Abstract
Sexual violence exposure represents a serious public health issue among female youth given its association with female youths’ engagement in health-risk behaviours. Sexual minority female youth are particularly vulnerable to sexual violence exposure, alcohol use, suicidality, and sexual-risk behaviour. Using the population-based 2017 Youth Risk Behaviour Survey, we examined sexual violence as a mediator of sexual orientation disparities in health-risk behaviours among female youth. This study included 7,532 female students in grades 9 through 12 across the US. Participants identified their sexual orientation as heterosexual (73.5%); bisexual (12.2%); and, gay or lesbian (2.2%). Compared to heterosexual female youth, sexual violence exposure, alcohol use, binge drinking, and multiple sex partners were more common among bisexual female youth. The elevated risk of suicidality was most notable among gay or lesbian female youth relative to heterosexual female youth and bisexual female youth relative to heterosexual female youth. Mediation analyses showed that sexual violence exposure partially explained the sexual orientation disparity in these co-occurring health-risk behaviours between bisexual female youth and heterosexual female youth. Our findings highlight the need for clinical attention to be paid to assessing and treating the health effects of sexual violence, especially among bisexual female youth.
Keywords: Sexual minority youth, female youth, sexual violence, health-risk behaviours, youth risk behaviour survey (YRBS)
Sexual minority female youth (e.g. female youth who identify as gay, lesbian, or bisexual) report increased engagement in health-risk behaviours, namely alcohol use, suicidality, and sexual-risk behaviour, compared to heterosexual female youth (Hatzenbuehler, 2011; Marshal et al., 2011; Russell, Driscoll, & Truong, 2002; Saewyc et al., 2006). For example, compared to heterosexual female youth, lesbian female youth were 1.04 times as likely and bisexual female youth were 1.52 times as likely to report alcohol use compared to heterosexual female youth (Kerr, Ding, Burke, & Ott-Walter, 2015). Similarly, sexual minority female youth report a 1.92 greater likelihood of having suicidal ideation and 2.63 greater likelihood of having made a suicidal attempt compared to heterosexual female youth (Eisenberg & Resnick, 2006). Moreover, sexual minority female youth report more sexual partners relative to their heterosexual female counterparts (Goodenow, Szalacha, Robin, & Westheimer, 2008; Saewyc, Poon, Homma, & Skay, 2008; Tornello, Riskind, & Patterson, 2014). Sexual minority female youths’ greater exposure to sexual violence compared to heterosexual female youth may represent one contributor to sexual orientation disparities in alcohol use, suicidality, and sexual-risk behaviour among female youth (Drabble, Trocki, Hughes, Korcha, & Lown, 2013; Rhew, Stappenbeck, Bedard-Gilligan, Hughes, & Kaysen, 2017).
Sexual violence (i.e. being forced to engage in sexual acts against one’s wishes such as kissing, touching, or being physically forced to have sexual intercourse) represents one of the most traumatic forms of violence (Chen & Ullman, 2010). Although empirical and theoretical justifications for the disparity remain unclear (Rhew et al., 2017), sexual violence disproportionately affects sexual minority females compared to heterosexual females (Balsam, Lehavot, & Beadnell, 2011; Goodenow et al., 2008; Hughes, McCabe, Wilsnack, West, & Boyd, 2010a; Hughes et al., 2010b; Saewyc et al., 2006), with incidence rates peaking during adolescence (Snyder & Sickmund, 2000). For instance, one recent study found that lesbian female youth were six times more likely, and bisexual female youth were three times more likely, than heterosexual female youth to experience sexual violence (Tornello et al., 2014). There remains a dearth of literature, however, documenting the prevalence of sexual violence that occurs in dating contexts specifically among sexual minority female youth. Of the limited research that exists, one regional survey demonstrated that lesbian and bisexual female youth reported more sexual dating violence exposure compared to heterosexual female youth (Dank, Lachman, Zweig, & Yahner, 2014).
Sexual minority female youth may represent one group at particular risk of alcohol use, suicidality, and sexual-risk behaviour due to sexual violence exposure. For instance, previous findings demonstrated that sexual minority women exposed to sexual violence reported more alcohol misuse compared to heterosexual women exposed to sexual violence (Drabble et al., 2013; Sigurvinsdottir & Ullman, 2015; Stevens, 2012). Indeed, sexual violence exposure may disproportionately affect sexual minority women compared to heterosexual women due to diminished social support resources to cope with stress associated with sexual violence exposure (Balsam, Rothblum, & Beauchaine, 2005; Dunbar, 2006). While extant findings suggest that sexual minority female youth report higher rates of health-risk behaviours compared to heterosexual female youth (Hatzenbuehler, 2011; Marshal et al., 2011; Russell et al., 2002; Saewyc et al., 2006), sexual violence has not been explored as a mediator of sexual orientation disparities in alcohol use, suicidality, and sexual-risk behaviour. To the extent that sexual violence contributes to the sexual orientation disparity in alcohol use, suicidality, and sexual-risk behaviour among female youth, this would lend support to negative reinforcement models of health-risk behaviours (i.e. health-risk behaviours reduce stress associated with sexual violence exposure, which negatively reinforces continued and increased engagement in risk behaviours; Baker et al., 2004).
The present study takes advantage of the data available within a nationally representative US sample which provides a large enough sample size to address existing knowledge gaps regarding potential sexual orientation disparities in sexual violence exposure and health-risk behaviours among female youth. Specifically, the large sample size and representative data structure allowed us to examine: (1) whether sexual violence exposure in general, sexual dating violence exposure, alcohol use, binge drinking, suicidal ideation, having made a suicidal plan, having made a suicidal attempt, and multiple sex partners are more prevalent among sexual minority female youth than among heterosexual female youth and (2) whether greater exposure to sexual violence can explain or partially explain the elevated prevalence of alcohol use, suicidality, and sexual-risk behaviour among sexual minority female youth.
Method
Participants and procedures
Biennially since 1991, the US Centres for Disease Control and Prevention has conducted the national Youth Risk Behaviour Survey (YRBS). The YRBS is a school-based, cross-sectional survey that uses an independent three-stage cluster sample design to obtain a nationally representative sample of students in grades 9 through 12 who attend public and private schools in 50 states and the District of Columbia (Brener et al., 2013). Participation in the YRBS is anonymous and voluntary, and the YRBS adheres to local parental permission requirements. Students complete a self-administered questionnaire during a regular class period and record responses on an answer sheet or computer-scannable questionnaire booklet (Brener et al., 2013). For the 2017 YRBS, the school-level response rate was 75%, the student-level response rate was 81%, and the overall response rate was 60% (Johns et al., 2018). A weighting factor was applied to each student record to account for nonresponse and oversampling of Hispanic and Black students. The overall weights were then scaled so the weighted count of students was equal to the total sample size, and the weighted proportions of students in each grade matched population projections for each survey year (Johns et al., 2018). The national YRBS was reviewed and approved by an institutional review board at the Centres for Disease Control and Prevention in Atlanta, Georgia.
Measures
Sexual orientation
Sexual orientation was classified based on self-identification using the following item: ‘Which of the following best describes you?’ Response options were categorical and included: heterosexual; gay or lesbian; bisexual; and, not sure. We excluded the 347 (4.6%) individuals who responded that they were uncertain of their sexual orientation, as previous studies have shown that this group often consists of a heterogenous mix of respondents in terms of sexual identity (Badgett, 2009). In addition, while some people do not know their sexual orientation because they are undecided, studies have indicated that the majority of people who choose such responses may not understand the question (Sell, Wells, & Wypij, 1995). Those who responded that they were ‘not sure’ of their sexual orientation did not significantly differ regarding age, race, or grade as compared to those reporting being gay or lesbian, bisexual, or heterosexual. For all analyses, two dummy coded sexual orientation variables were used (gay or lesbian, coded 1, with heterosexual as the reference group, coded 0) and (bisexual, coded 1, with heterosexual as the reference group, coded 0).
Socio-demographic variables
Participants reported their age, race, and school grade. All socio-demographic variables were collected in categorical form. Race was assessed with the following question, ‘What is your race?’ Response options included: American Indian or Alaska Native; Asian; Black or African American; Native Hawaiian or Pacific Islander; and White. Race was dichotomised as racial minority (i.e. American Indian or Alaska Native; Asian; Black or African American; Native Hawaiian or Pacific Islander), coded 0, and White, coded 1, in tests of bivariate associations.
Alcohol use
Alcohol use was assessed with the following question: ‘During the past 30 days, on how many days did you have at least one drink of alcohol?’ Response options ranged from 0 (0 days) to 6 (all 30 days). Binge drinking was assessed with the following question: ‘During the past 30 days, on how many days did you have 4 or more drinks of alcohol in a row (if you are female)?’ Response options ranged from 0 (0 days) to 6 (20 or more days). Because of a high number of zeroes across alcohol use (37.5%) and binge drinking (80.1%), alcohol use during the past 30 days was dichotomised as 0 days, coded 0, and 1 or more days, coded 1; and, binge drinking was dichotomised as 0 days, coded 0, and 1 or more days, coded 1, as recommended by Fletcher, MacKenzie, and Villouta (2005).
Suicidality
Suicidal ideation was assessed with the following question: ‘During the past 12 months, did you ever seriously consider attempting suicide?’ This item was answered yes (1) or no (0). Past 12 months suicidal ideation was dichotomised as no, coded 0, and yes, coded 1. Having made a suicidal plan was assessed with the following question: ‘During the past 12 months, did you make a plan about how you would attempt suicide?’ This item was answered yes (1) or no (0). Past 12 months suicidal plan was dichotomised as no, coded 0, and yes, coded 1. Having made a suicidal attempt was assessed with the following question: ‘During the past 12 months, how many times did you actually attempt suicide?’ Response options ranged from 0 (0 times) to 4 (6 or more times). Past 12 months suicidal attempt was dichotomised as no, coded 0, and yes, coded 1.
Sexual-risk behaviour
Sexual-risk behaviour over the past 3 months was assessed using one item that measures individuals’ self-reports of having multiple sex partners. Having multiple sex partners was assessed with the following question: ‘During the past 3 months, with how many people have you had sexual intercourse?’ Response options ranged from 0 (I have never had sexual intercourse) to 6 (6 or more people). Having multiple sex partners was dichotomised as never had sexual intercourse/1 person, coded 0, and 2 or more people, coded 1, following Garofalo, Mustanski, McKirnan, Herrick, and Donenberg (2007).
Sexual violence exposure
Sexual violence exposure was assessed with the following question: ‘During the past 12 months, how many times did anyone force you to do sexual things that you did not want to do? Count such things as kissing, touching, or being physically forced to have sexual intercourse.’ Response options ranged from 0 (0 times) to 4 (6 or more times). Past-12-month sexual violence was dichotomised as 0 times, coded 0, and 1 or more times, coded 1. Sexual dating violence was assessed with the following question: ‘During the past 12 months, how many times did someone you were dating or going out with force you to do sexual things that you did not want to do? Count such things as kissing, touching, or being physically forced to have sexual intercourse.’ Response options ranged from 0 (I did not go out with anyone during the past 12 months/0 times) to 5 (6 or more times). Past-12-month sexual dating violence was dichotomised as I did not go out with anyone during the past 12 months/0 times, coded 0, and 1 or more times, coded 1.
Statistical analysis
SPSS version 24 (IBM Corporation, 2016) was used to analyse descriptive statistics and assess for sexual orientation differences in sexual violence exposure and health-risk behaviours between gay or lesbian female youth and heterosexual female youth and between bisexual female youth and heterosexual female youth using logistic regression. We first tested for bivariate associations among the study variables and demographic covariates using binary logistic regressions. Examining bivariate associations allows us to better estimate associations between variables in our measurement and structural models (Anderson & Gerbing, 1988). In all analyses, post-stratification weights were used to adjust for nonresponse and oversampling of Hispanic and Black students to generate nationally representative estimates of prevalence and associations. We then performed the logistic regression analyses which were adjusted for age, race, and grade. Missing data for demographic characteristics ranged from 0.01% for age to 7.49% for sexual orientation. Missing data for other study variables ranged from 1.10% for suicidal plan to 13.46% for suicidal attempt. Imputation for missing data is not recommended for studies using the YRBS (Brener et al., 2013); thus, we used complete case analysis.
Next, we examined whether sexual violence exposure explained or partially explained sexual orientation disparities in alcohol use, suicidality, and sexual-risk behaviour using mediation analyses. To statistically test mediation, we calculated the indirect effect of sexual orientation on alcohol use, suicidality, and sexual-risk behaviour through sexual violence exposure. Subpopulation effects were examined by performing mediation analyses separately for gay or lesbian female youth and bisexual female youth. Specifically, we conducted a path analysis using Mplus version 8.1 (Muthén & Muthén, 2018) with robust maximum likelihood (MLR) estimation, which is the optimal method for analyses with missing data, with the requisite Montecarlo integration (Muthén & Muthén, 2018). Structural equation modelling allows for the simultaneous testing of multiple linear regressions as well as the computation of both direct and indirect effects and their corresponding standard errors (Anderson & Gerbing, 1988). As recommended (Anderson & Gerbing, 1988), we first tested a measurement model, in which co-variances among factors of our independent, mediator, and dependent variables were freely estimated and measurement errors were not allowed to correlate.
Model indices were used to determine which parameters could be freely estimated to significantly improve model fit (i.e. based on the model chi-square statistic). A modification index represents the numerical amount that the model chi-square would decrease if a parameter was freely estimated. We added a covariance between the measurement errors of two variables if a modification index for that parameter was 10 or greater (Lewis, Milletich, Derlega, & Padilla, 2014; Muthén & Muthén, 2018). In the final measurement model, the observed indicators were constrained to load onto their respective factor. The latent mediator (i.e. sexual violence) was indicated by the measures of sexual violence and sexual dating violence. The latent alcohol use factor was indicated by the measures of alcohol use and binge drinking. The latent suicidality factor was indicated by the measures of suicidal ideation, having made a suicidal plan, and having made a suicidal attempt. We used a dichotomous manifest variable for sexual-risk behaviour operationalised as multiple sex partners.
We then tested the hypothesised structural path model to examine the direct relationships between sexual orientation with sexual violence exposure and health-risk behaviours as well as the indirect effect of sexual orientation on health-risk behaviours through sexual violence exposure. Alcohol use was allowed to co-vary with sexual-risk behaviour and suicidality, and suicidality was allowed to co-vary with sexual-risk behaviour, given their associations at the bivariate level. Each endogenous variable (i.e. each regression) in the model was adjusted for the impact of age, race, and grade. Studies using the YRBS to examine sexual orientation disparities have used similar demographic covariates (e.g. Fish & Baams, 2018). Finally, bias-corrected bootstrapping procedures were used to calculate indirect effect estimates with 95% confidence intervals from 1,000 samples drawn from the original dataset.
A significant indirect effect (p < 0.05) was interpreted as evidence of mediation. We assessed the model fit using the comparative fit index (CFI), Tucker-Lewis Index (TLI), standardised root-mean-square residual (SRMR), and root-mean-square error of approximation (RMSEA) and its 90% confidence interval to the data. Values of at least .95 for the CFI and TLI indicate that the model is a good fit to the data (Kline, 1998), while SRMR and RMSEA values of .08 or lower are acceptable (Hu & Bentler, 1999).
Results
We first examined the demographic characteristics of the sample and then tested for bivariate associations among study variables using the full sample. Sexual orientation differences (gay or lesbian versus heterosexual; bisexual versus heterosexual) in sexual violence in general, sexual dating violence, alcohol use, binge drinking, suicidal ideation, having made a suicidal plan, having made a suicidal attempt, and sexual-risk behaviour were analysed using logistic regression. Finally, we used structural equation modelling to assess whether sexual minority female youths’ (i.e. gay or lesbian, bisexual) disproportionate risk of sexual violence exposure mediated the anticipated sexual orientation differences in engagement in health-risk behaviours.
Sample description
Table 1 presents full demographic information, including response options and sample characteristics, in the total sample and stratified by sexual orientation. Participants were 7,532 female youth. Most participants were 16 years old (25.5%) and in 9th grade (26.6%). Participants identified their sexual orientation as heterosexual (73.5%), bisexual (12.2%), and gay or lesbian (2.2%). The majority of participants identified as White (53.1%), followed by Black or African American (12.9%), Multiracial Hispanic (12.2%), Hispanic/Latino (9.2%), Multiracial non-Hispanic (5.6%), Asian (3.5%), Native Hawaiian/Pacific Islander (0.8%), and American Indian/Alaska Native (0.3%).
Table 1.
Frequencies of demographic variables by sexual orientation among female youtha.
| Total sample n = 7,532 |
Heterosexual n = 5,533 (73.5%) |
Gay or Lesbian n = 168 (2.2%) |
Bisexual n = 921 (12.1%) |
|
|---|---|---|---|---|
| N (%)b | N (%)b | N (%)b | N (%)b | |
| Race | ||||
| American Indian/Alaska Native | 26 (0.3%) | 17 (0.3%) | 1 (0.7%) | 3 (0.4%) |
| Asian | 265 (3.5%) | 224 (4.1%) | 1 (0.7%) | 18 (2.0%) |
| Black or African American | 976 (12.9%) | 681 (12.3%) | 43 (25.9%) | 165 (17.9%) |
| Native Hawaiian/Pacific Islander | 57 (0.8%) | 47 (0.8%) | 1 (0.7%) | 5 (0.6%) |
| White | 4,003 (53.1%) | 2,863 (51.7%) | 79 (47.2%) | 443 (48.1%) |
| Hispanic/Latino | 693 (9.2%) | 552 (10.0%) | 12 (6.9%) | 82 (8.9%) |
| Multiracial Hispanic | 920 (12.2%) | 723 (13.1%) | 18 (10.7%) | 105 (11.4%) |
| Multiracial non-Hispanic | 425 (5.6%) | 317 (5.7%) | 8 (4.8%) | 80 (8.7%) |
| Grade | ||||
| 9th grade | 2,009 (26.6%) | 1,472 (26.6%) | 33 (19.6%) | 227 (24.7%) |
| 10th grade | 1,916 (25.4%) | 1,369 (24.8%) | 55 (32.6%) | 252 (27.4%) |
| 11th grade | 1,787 (23.7%) | 1,329 (24.0%) | 42 (24.9%) | 226 (24.6%) |
| 12th grade | 1,739 (23.1%) | 1,303 (23.6%) | 37 (21.8%) | 205 (22.3%) |
| Age | ||||
| 12 years old or younger | 15 (0.2%) | 7 (0.1%) | 1 (0.8%) | 1 (0.1%) |
| 13 years old | 8 (0.1%) | 4 (0.1%) | 2 (1.0%) | 2 (0.2%) |
| 14 years old | 937 (12.4%) | 686 (12.4%) | 18 (10.8%) | 108 (11.7%) |
| 15 years old | 1,868 (24.8%) | 1,344 (24.3%) | 33 (19.4%) | 225 (24.4%) |
| 16 years old | 1,921(25.5%) | 1,399 (25.3%) | 50 (29.9%) | 252 (27.3%) |
| 17 years old | 1,787 (23.7%) | 1,337 (24.2%) | 32 (18.9%) | 221 (24.0%) |
| 18 years old or older | 931(12.3%) | 704 (12.7%) | 31 (18.2%) | 100 (10.9%) |
Note.
Percentages may not equal 100 due to missing data.
Weighted percentages.
Preliminary analyses
Table 2 presents the bivariate associations among study variables. In tests of bivariate associations between demographic covariates adjusted within the mediation model, older age was significantly associated with a lower likelihood of having made a suicidal attempt and higher grade was significantly associated with a greater likelihood of alcohol use and sexual-risk behaviour (i.e. having multiple sex partners). Female youth who identified as White were more likely to report sexual violence exposure and alcohol use, and less likely to report having made a suicidal attempt compared to female youth who identified as racial minorities.
Table 2.
Bivariate associations among the study variables in the full sample of female youth.
| Age OR (95% CI) | Grade OR (95% CI) | Race OR (95% CI) | Sexual violence OR (95% CI) | Sexual dating violence OR (95% CI) | Alcohol use OR (95% CI) | Binge drinking OR (95% CI) | Suicidal ideation OR (95% CI) | Suicidal plan OR (95% CI) | Suicidal attempt OR (95% CI) | Multiple sex partners OR (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | N/A | 0.99 (0.90, 1.10) | 0.89 (0.73, 1.10) | 1.24 (0.95, 1.63) | 0.99 (0.86, 1.16) | 1.18 (0.98, 1.42) | 1.05 (0.89, 1.23) | 1.15 (0.96, 1.39) | 0.87* (0.75, 0.99) | 1.18 (0.90, 1.55) |
| 2. Grade | – | 1.01 (0.91, 1.13) | 1.04 (0.83, 1.30) | 0.84 (0.63, 1.13) | 1.29** (1.10, 1.52) | 0.98 (0.80, 1.20) | 0.95 (0.79, 1.13) | 0.90 (0.73, 1.10) | 0.99 (0.86, 1.16) | 1.53** (1.13, 2.05) | |
| 3. Race | – | 1.45** (1.15, 1.83) | 1.11 (0.99, 1.24) | 1.09** (1.03, 1.15) | 1.07 (0.99, 1.16) | 1.02 (0.95, 1.08) | 1.06 (0.99, 1.14) | 0.88*** (0.83, 0.93) | 1.00 (0.90, 1.12) | ||
| 4. Sexual violence | – | N/A | 1.91*** (1.42,2.58) | 1.21 (0.86, 1.69) | 2.10*** (1.52, 2.88) | 1.92*** (1.38,2.68) | 1.39* (1.06, 1.81) | 2.37*** (1.56, 3.62) | |||
| 5. Sexual dating violence | – | 0.57* (0.37, 0.88) | 1.59* (1.00,2.53) | 1.22 (0.82, 1.81) | 1.01 (0.68, 1.52) | 0.94 (0.66, 1.33) | 1.10 (0.66, 1.82) | ||||
| 6. Alcohol use | – | N/A | 1.04 (0.80, 1.35) | 1.46** (1.10, 1.94) | 0.88 (0.70, 1.10) | 3.37*** (2.27, 4.99) | |||||
| 7. Binge drinking | – | 1.08 (0.79, 1.48) | 1.17 (0.84, 1.62) | 1.31 (0.99, 1.72) | 1.58* (1.09, 2.29) | ||||||
| 8. Suicidal ideation | – | 33.03*** (26.75, 40.77) | 3.17*** (2.58, 3.88) | 1.39 (0.91, 2.12) | |||||||
| 9. Suicidal plan | – | 2.64*** (2.13, 3.28) | 1.14 (0.73, 1.78) | ||||||||
| 10. Suicidal attempt | – | 0.96 (0.66, 1.40) | |||||||||
| 11. Multiple sex partners | – |
Note. ORs with 95% confidence intervals. Associations between the study variables and demographic covariates were tested using a bivariate logistic regression. Race (0 = racial minority; 1 = White); Sexual violence (0 = 0 times and 1 = 1 or more times); Sexual dating violence (0 = I did not go out with anyone during the past 12 months/0 times and 1 = 1 or more times); Alcohol use (0 = 0 days; 1 = 1 or more days); Binge drinking (0 = 0 days; 1 = 1 or more days); Suicidal ideation (0 = no; 1 = yes); Suicidal plan (0 = no; 1 = yes); Suicidal attempt (0 = no; 1 = yes); Multiple sex partners (0 = never had sexual intercourse/1 person; 1 = 2 or more people).
OR = odds ratio; CI = confidence interval
p < .10,
p < .05,
p < .01,
p < .001.
As expected, sexual violence exposure was positively associated with alcohol use, suicidal ideation, having made a suicidal plan, having made a suicidal attempt, and having multiple sex partners. Sexual dating violence was negatively associated with alcohol use and positively associated with binge drinking. Alcohol use was positively associated with having made a suicidal plan and having multiple sex partners. Binge drinking was positively associated with having multiple sex partners. Finally, variables for suicidality were positively associated with each other (i.e. suicidal ideation, having made a suicidal plan, and having made a suicidal attempt).
Sexual orientation differences across study variables
Table 3 presents sexual orientation disparities in sexual violence in general, sexual dating violence, alcohol use, binge drinking, suicidal ideation, having made a suicidal plan, having made a suicidal attempt, and multiple sex partners among female youth. Bisexual female youth had elevated risk of sexual violence in general (adjusted odds ratio [AOR] = 2.17; 95% CI 1.82 2.58), sexual dating violence (AOR = 2.10; 95% CI 1.67, 2.65), alcohol use (AOR = 1.45; 95% CI 1.24, 1.69), binge drinking (AOR = 1.38; 95% CI 1.14, 1.68), and multiple sex partners (AOR = 2.38; 95% CI 1.79, 3.16) compared to heterosexual female youth. The elevated risk of suicidality was most notable among gay or lesbian female youth relative to heterosexual female youth (AOR for suicidal ideation: 5.19; 95% CI 3.78, 7.12; AOR for having made a suicidal plan: 4.72; 95% CI 3.42, 6.51; AOR for having made a suicidal attempt: 2.30; 95% CI 1.65, 3.21); and bisexual female youth relative to heterosexual female youth (AOR for suicidal ideation: 5.23; 95% CI 4.50, 6.08; AOR for having made a suicidal plan: 4.82; 95% CI 4.13, 5.64; AOR for having made a suicidal attempt: 2.06; 95% CI 1.77, 2.41).
Table 3.
Adjusted odds ratios for sexual orientation disparities in sexual violence exposure and health-risk behaviours.
| Descriptive results |
Logistic regression results |
|||||
|---|---|---|---|---|---|---|
| Heterosexual |
Gay or Lesbian |
Bisexual |
Heterosexual |
Gay or Lesbian |
Bisexual |
|
| n (%)a | n (%)a | n (%)a | (Reference) | AORb (95% CI) | AORb (95% CI) | |
| Sexual violence exposure | ||||||
| Sexual violence in general | 714 (12.9) | 23 (13.5) | 214 (23.3) | 1 | 0.93 (0.58, 1.50) | 2.17*** (1.82, 2.58) |
| Sexual dating violence | 340 (6.1) | 15 (9.2) | 108 (11.7) | 1 | 1.39 (0.79, 2.44) | 2.10*** (1.67,2.65) |
| Alcohol use | ||||||
| Alcohol use | 1,578 (28.5) | 56 (33.2) | 319 (34.6) | 1 | 1.27 (0.90, 1.79) | 1.45*** (1.24, 1.69) |
| Binge drinking | 720 (13.0) | 28 (16.5) | 154 (16.7) | 1 | 1.25 (0.81, 1.92) | 1.38*** (1.14, 1.68) |
| Suicidality | ||||||
| Suicidal ideation | 928 (16.8) | 87 (51.6) | 463 (50.3) | 1 | 5.19*** (3.78, 7.12) | 5.23*** (4.50, 6.08) |
| Suicidal plan | 710 (12.8) | 69 (40.9) | 369 (40.1) | 1 | 4.72*** (3.42, 6.51) | 4.82*** (4.13, 5.64) |
| Suicidal attempt | 1,081 (19.5) | 62 (36.9) | 311 (33.8) | 1 | 2.30*** (1.65, 3.21) | 2.06*** (1.77,2.41) |
| Sexual-risk behaviour | ||||||
| Multiple sex partners | 201 (3.6) | 8 (4.5) | 73 (7.9) | 1 | 1.36 (0.64, 2.88) | 2.38*** (1.79,3.16) |
Weighted percentages.
Analyses were adjusted for age, grade, and race.
Note. AOR = adjusted odds ratios; CI = confidence interval. Sexual violence (0 = 0 times and 1 = 1 or more times); Sexual dating violence (0 = I did not go out with anyone during the past 12 months/0 times and 1 = 1 or more times); Alcohol use (0 = 0 days; 1 = 1 or more days); Binge drinking (0 = 0 days; 1 = 1 or more days); Suicidal ideation (0 = no; 1 = yes); Suicidal plan (0 = no; 1 = yes); Suicidal attempt (0 = no; 1 = yes); Multiple sex partners (0 = never had sexual intercourse/1 person; 1 = 2 or more people).
p < .10,
p < .05,
p < .01,
p < .001.
Path model of associations between sexual orientation with sexual violence exposure and health-risk behaviours
To examine whether sexual violence exposure mediated the anticipated sexual orientation disparities in health-risk behaviours, a path analysis was conducted. Overall, the measurement model demonstrated good fit (CFI = 0.97; TLI = 0.96; SRMR = 0.04; RMSEA = 0.04, 90% CI [0.03, 0.04]). The latent factor measuring sexual violence had high standardised loadings for both sexual violence (λ = 0.97) and sexual dating violence (λ = 0.68). Similarly, the latent factor measuring alcohol use had strong factor loadings for alcohol use (λ = 0.83) and binge drinking (λ = 0.79). Finally, the latent factor measuring suicidality had adequate standardised loadings for suicidal ideation (λ = 0.82), suicidal plan (λ = 0.79), and suicidal attempt (λ = 0.32). Overall, the latent structural model also demonstrated good fit (CFI = 0.99; TLI = 0.98; SRMR = 0.02; RMSEA = 0.03, 90% CI [0.02, 0.03]).
As displayed in Figure 1, the mediating effect of sexual violence exposure on health-risk behaviours was only significant for bisexual female youth, suggesting that sexual violence exposure partially mediated the sexual orientation disparity between bisexual and heterosexual female youth in alcohol use, suicidality, and sexual-risk behaviour. This overall model explained 8.2% of the variability in alcohol use, 17.9% of the variance in suicidality, and 3.5% of the variability in sexual-risk behaviour. We also calculated the unique proportion of the sexual orientation disparity mediated by sexual violence exposure, separately for gay or lesbian and bisexual female youth, using calculation of risk differences as suggested by Vanderweele (2015). In analyses examining the disparities between gay or lesbian female youth compared to heterosexual female youth, sexual violence exposure explained 7.9% of the disparity in alcohol use, 9.8% of the disparity in suicidality, and 3.3% of the disparity in sexual-risk behaviour. In analyses examining the disparities between bisexual female youth compared to heterosexual female youth, sexual violence exposure explained 8.0% of the disparity in alcohol use, 15.9% of the disparity in suicidality, and 3.5% of the variance in sexual-risk behaviour.
Figure 1.
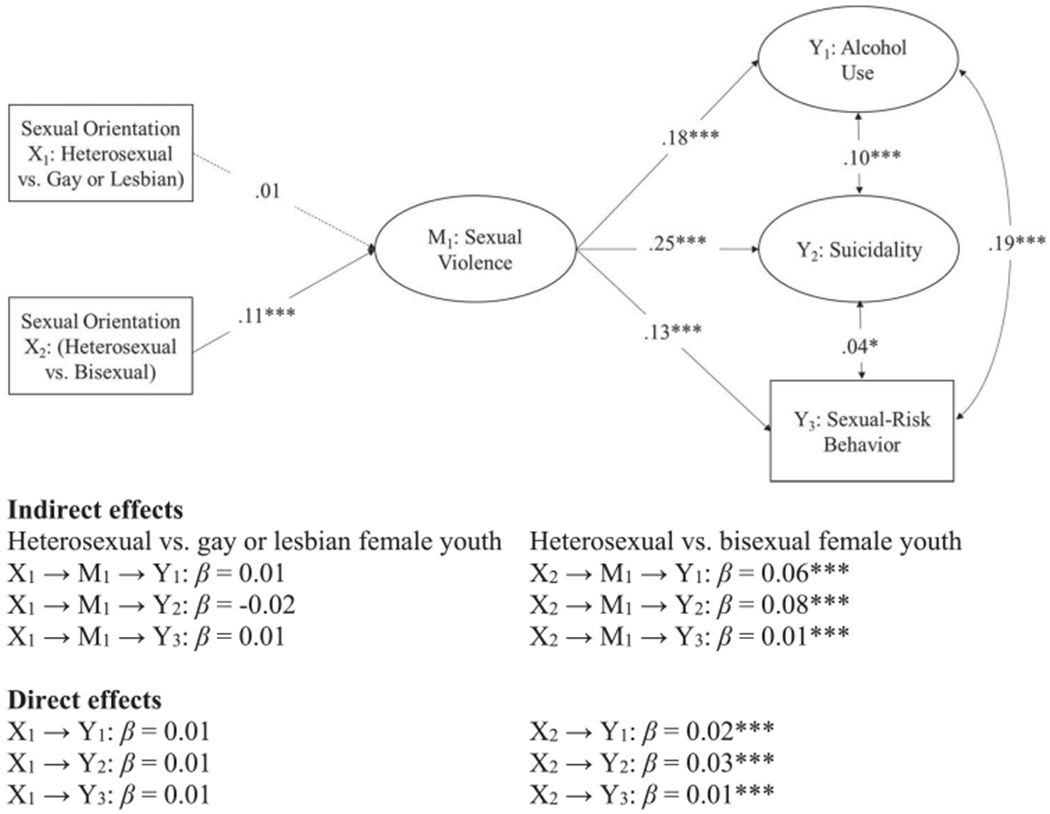
Indirect and direct effect of sexual orientation differences in alcohol use, suicidality, and sexual-risk behaviour mediated through sexual violence exposure.
Note. Values are standardised coefficient estimates. Dashed lines represent significant paths. Two dummy coded sexual orientation variables were used (gay or lesbian = 1, heterosexual = 0) and (bisexual = 1, heterosexual = 0). The model controls for age, race, and grade. †p < .10, *p < .05, **p < .01, ***p < .001.
Discussion
Sexual minority female youth disproportionately report higher rates of health-risk behaviours, including alcohol use, suicidality, and sexual-risk behaviour, relative to heterosexual female youth (Dank et al., 2014; Eisenberg & Resnick, 2006; Hatzenbuehler, 2011; Marshal et al., 2011; Russell et al., 2002; Saewyc et al., 2006). This US population-based study extends these findings by demonstrating that alcohol use, binge drinking, and multiple sex partners was most notable among bisexual female youth relative to heterosexual female youth. No such elevated risk existed among gay or lesbian female youth compared to heterosexual female youth. Further, in line with our hypotheses, all sexual minority female youth (i.e. gay or lesbian, bisexual) consistently reported elevated risk of suicidal ideation, having made a suicidal plan, and having made a suicidal attempt compared to heterosexual female youth. In addition to demonstrating evidence of elevated health-risk behaviours among sexual minority female youth compared to heterosexual female youth, our findings indicate that sexual violence exposure may serve as one mechanism that partially explains sexual orientation disparities in health-risk behaviours between bisexual and heterosexual female youth. Specifically, we found that experiences of sexual violence, measured both as sexual violence in general and as occurring in dating relationships, were elevated among bisexual female youth, and partially explained the substantially elevated risk of alcohol use, suicidality, and sexual-risk behaviour among bisexual female youth compared to heterosexual female youth. Together, findings suggest the need to enhance targeted relationship-, school-, and community-based clinical services to assess for and treat the mental health and behavioural effects of sexual violence exposure among all female youth in general and in particular, bisexual female youth.
Notably, for all youth, adolescence represents a developmental period of forming personal identities and navigating dating and sexual relationships (Ryan & Futterman, 1997). For sexual minority female youth, developing a positive sexual identity, often in the context of minority stress (e.g. discrimination, prejudice), may directly affect their ability to establish healthy sexual and dating relationships, leading to their increased risk of experiencing sexual violence (Balsam & Szymanski, 2005; Gillum & DiFulvio, 2012). This study extends previous findings by illustrating preliminary support that engaging in risky behaviour, such as alcohol use, may be motivated by the need to assuage the stress that can follow sexual violence exposure, especially among bisexual female youth (Hughes et al., 2010a, 2010b; Saewyc et al., 2006). Discerning the aetiology of targeted sexual violence against bisexual female youth is especially critical given that sexual violence exposure during adolescence is a risk factor for re-victimisation in adulthood (Martin, Fisher, Warner, Krebs, & Lindquist, 2011).
We extend the sexual minority and trauma literature by providing evidence that the substantially elevated risk of alcohol use, suicidality, and sexual-risk behaviour among bisexual female youth in comparison to heterosexual female youth can be partially explained by bisexual female youths’ increased exposure to sexual violence (i.e. sexual violence in general and sexual dating violence). Prior work focuses on sexual minority female youths’ engagement in health-risk behaviours as a maladaptive coping response to persistent experiences of stigma-related stressors, such as peer victimisation (Burton, Marshal, Chisolm, Sucato, & Friedman, 2013; Eisenberg & Resnick, 2006), with limited attention to sexual violence. The present study’s findings underscore the mental health and behavioural effects of sexual violence exposure and suggest the need for future studies to investigate psychosocial mechanisms, such as emotion regulation and shame, that may further explain the association between sexual violence exposure and health-risk behaviours particularly among bisexual female youth.
Research and clinical implications
Sexual violence exposure represents an under-investigated mechanism that partially explains the sexual orientation disparity in health-risk behaviours, namely alcohol use, suicidality, and sexual-risk behaviour, between bisexual female youth and heterosexual female youth. The sexual orientation disparities in violence exposure and health-risk behaviours documented in this large study of US-based female youth have several implications for future research. For example, in the present study, sexual violence exposure was associated with every indicator of alcohol use, suicidality, and sexual-risk behaviour among all female youth, regardless of sexual orientation, age, race, or grade. As these findings broadly indicate, female youth survivors of trauma may attempt to cope with the negative effects of sexual violence by engaging in risky behaviour. Longitudinal research is needed to better examine the causal influences of the relationship between sexual violence and health-risk behaviours in this population. Future research should also incorporate other explanatory mechanisms into the tested model that may account for additional explained variance in suicidality among sexual minority female youth with sexual violence exposure. Finally, our findings of variability in risk of sexual violence exposure, alcohol use, suicidality, and sexual-risk behaviour among different subgroups of sexual minority female youth (i.e. gay or lesbian, bisexual) highlight the importance of including multiple options for sexual identity in national surveys.
This study’s findings expand our current understanding of sexual violence exposure as a mechanism that may explain sexual orientation disparities in health-risk behaviours among female youth and therefore could inform clinical interventions targeting health-risk behaviours particularly among bisexual female youth. For instance, assessing sexual violence exposure when working with female youth in general, and especially with bisexual female youth, could help identify individuals who may be particularly vulnerable to health-risk behaviours. Existing sexual violence prevention programmes should ensure their inclusivity of sexual minorities and effectiveness for vulnerable subgroups of sexual minority female youth. Additionally, health professionals and educators should ensure that prevention efforts are directed towards the full range of health-risk behaviours experienced by sexual minority female youth with sexual violence exposure, including alcohol use, suicidality, and sexual-risk behaviour. School-based prevention and intervention efforts should work to promote sexual violence awareness among adolescents, including dating violence. Schools should also work to implement a referral system for female students who disclose experiences of sexual violence to community-based resources specifically for youth exposed to sexual violence to circumvent their increased risk for engaging in maladaptive coping behaviours. Implementation of these interventions should occur in lesbian, gay, bisexual, transgender, and queer (LGBTQ) community settings and organisations, including school-based gender-sexuality alliances, as connectedness to the broader LGBTQ community serves as a protective factor against minority stress and bias-based victimisation (Poteat, Scheer, Marx, Calzo, & Yoshikawa, 2015; Shilo, Antebi, & Mor, 2015).
Limitations
While this study is among the first to examine whether sexual violence exposure may serve as an explanatory mechanism for sexual orientation disparities in health-risk behaviours among female youth using a large, population-based sample, results must be interpreted in light of several limitations related to study design and measurement. This study’s cross-sectional design precludes causal inference and limits understanding temporal ordering of sexual violence exposure and health-risk behaviours. As such, we cannot rule out competing models that may explain these findings. For instance, although having multiple recent sex partners following sexual violence exposure may result from an attempt to modulate psychological distress or negative arousal associated with sexual violence exposure, it is possible that having multiple recent sex partners increases one’s risk of sexual violence exposure (Booth, Mengeling, Torner, & Sadler, 2011). Future longitudinal designs can verify the temporal sequence of experiences reported here and provide stronger evidence for the indirect pathways and direction of associations between sexual violence exposure and health-risk behaviours among female youth.
Additionally, given that the YRBS is solely a school-based survey, many at-risk youths who may be particularly vulnerable to sexual violence and health-risk behaviours may be excluded. This is especially relevant given the higher rates of school absences, dropout, and homelessness among sexual minority youth relative to their heterosexual counterparts (Kosciw, Palmer, Kull, & Greytak, 2013). Also, this study did not account for other forms of sexual violence (e.g. childhood sexual abuse) or the severity and frequency of sexual violence, which would be important factors to consider in future research in order to identify female youth at greatest risk for engaging in health-risk behaviours. This study also did not examine the sexual violence perpetrator’s gender identity which may have contributed to important nuances in the demonstrated associations. For example, the extent to which sexual minority female youth engage in health-risk behaviours may relate to their perceptions of whether their exposure to sexual violence was motivated by heterosexism (Cannon, 2015). It should also be noted that while our analyses can only infer the presence of stigma based on female youths’ sexual minority identity (Meyer, 2003), the mediating role of violence exposure could be due to factors other than stigma such as prior exposure to sexual violence in childhood or adolescence.
Results should also be interpreted in light of limitations in the measurement of some study constructs. Because the YRBS uses self-report data, there exists a possibility for biased reporting in health-risk behaviours; however, prior research has demonstrated the reliability of the data collected by the YRBS (Kann et al., 2014). We also used sexual identity as a marker of sexual orientation, thus limiting our generalisability to sexual minority female youth who do not identify as gay, lesbian, or bisexual, but may have same-gender sexual partners or experience same-gender sexual attraction. In addition, the YRBS does not assess for gender identity of respondents; as such, the percentage of sexual minority female youth participants who identify as transgender or gender non-binary remains unknown. Thus, future iterations of the YRBS should assess for gender identity in an inclusive and affirming manner to increase the generalisability of the association between sexual violence exposure and health-risk behaviours in this gender-diverse population.
Conclusion
In conclusion, this study tested potential differences in sexual violence exposure and health-risk behaviours among female youth who identify as heterosexual and those who identify as gay, lesbian, or bisexual. In this large population-based sample, sexual minority female youth were more likely to report sexual violence exposure in general and in dating relationships specifically, alcohol use, suicidality, and sexual-risk behaviour than heterosexual female youth. Further, this study provides evidence for sexual violence exposure as an explanatory mechanism of sexual orientation disparities in alcohol use, suicidality, and sexual-risk behaviour among female youth. As such, comprehensive interventions targeting health-risk behaviours among sexual minority female youth should assess for and treat traumatic stress associated with sexual violence exposure in this population. Future studies can extend findings from the current study by further investigating mechanisms, such as shame, that could help explain the short- and long-term consequences of sexual violence exposure among sexual minority female youth.
Acknowledgments
Manuscript preparation was supported in part by grant number T32MH020031-20 from the National Institute of Mental Health at the National Institutes of Health in support of Jillian Scheer.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Anderson JC, & Gerbing DW (1988). Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin, 103(3), 411–423. [Google Scholar]
- Badgett MV (2009). Best practices for asking questions about sexual orientation on surveys. Los Angeles: The Williams Institute. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51. [DOI] [PubMed] [Google Scholar]
- Balsam KF, Lehavot K, & Beadnell B (2011). Sexual revictimization and mental health: A comparison of lesbians, gay men, and heterosexual women. Journal of Interpersonal Violence, 26(9), 1798–1814. [DOI] [PubMed] [Google Scholar]
- Balsam KF, Rothblum ED, & Beauchaine TP (2005). Victimization over the life span: A comparison of lesbian, gay, bisexual, and heterosexual siblings. Journal of Consulting and Clinical Psychology, 73(3), 477–487. [DOI] [PubMed] [Google Scholar]
- Balsam KF, & Szymanski DM (2005). Relationship quality and domestic violence in women’s same-sex relationships: The role of minority stress. Psychology of Women Quarterly, 29(3), 258–269. [Google Scholar]
- Booth BM, Mengeling M, Torner J, & Sadler AG (2011). Rape, sex partnership, and substance use consequences in women veterans. Journal of Traumatic Stress, 24(3), 287–294. [DOI] [PubMed] [Google Scholar]
- Brener ND, Kann L, Shanklin S, Kinchen S, Eaton DK, Hawkins J, & Flint KH (2013). Methodology of the youth risk behavior surveillance system—2013. Morbidity and Mortality Weekly Report: Recommendations and Reports, 62(1), 1–20. [PubMed] [Google Scholar]
- Burton CM, Marshal MP, Chisolm DJ, Sucato GS, & Friedman MS (2013). Sexual minority-related victimization as a mediator of mental health disparities in sexual minority youth: A longitudinal analysis. Journal of Youth and Adolescence, 42(3), 394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon C (2015). Illusion of inclusion: The failure of the gender paradigm to account for intimate partner violence in LGBT relationships. Partner Abuse, 6(1), 65–77. [Google Scholar]
- Chen Y, & Ullman SE (2010). Women’s reporting of sexual and physical assaults to police in the national violence against women survey. Violence against Women, 16(3), 262–279. [DOI] [PubMed] [Google Scholar]
- Corporation, I. B. M. (2016). IBM SPSS statistics for windows, version 24.0. Armonk, NY: IBM Corp. [Google Scholar]
- Dank M, Lachman P, Zweig JM, & Yahner J (2014). Dating violence experiences of lesbian, gay, bisexual, and transgender youth. Journal of Youth and Adolescence, 43(5), 846–857. [DOI] [PubMed] [Google Scholar]
- Drabble L, Trocki KF, Hughes TL, Korcha RA, & Lown AE (2013). Sexual orientation differences in the relationship between victimization and hazardous drinking among women in the national alcohol survey. Psychology of Addictive Behaviors, 27(3), 639–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar E (2006). Race, gender, and sexual orientation in hate crime victimization: Identity politics or identity risk? Violence and Victims, 21, 323–337. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, & Resnick MD (2006). Suicidality among gay, lesbian and bisexual youth: The role of protective factors. Journal of Adolescent Health, 39(5), 662–668. [DOI] [PubMed] [Google Scholar]
- Fish JN, & Baams L (2018). Trends in alcohol-related disparities between heterosexual and sexual minority youth from 2007 to 2015: Findings from the youth risk behavior survey. LGBT Health, 5(6), 359–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher D, MacKenzie D, & Villouta E (2005). Modelling skewed data with many zeros: A simple approach combining ordinary and logistic regression. Environmental and Ecological Statistics, 12(1), 45–54. [Google Scholar]
- Garofalo R, Mustanski BS, McKirnan DJ, Herrick A, & Donenberg GR (2007). Methamphetamine and young men who have sex with men: Understanding patterns and correlates of use and the association with HIV-related sexual risk. Archives of Pediatrics & Adolescent Medicine, 161 (6), 591–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillum TL, & DiFulvio G (2012). “There’s so much at stake:” Sexual minority youth discuss dating violence. Violence against Women, 18(7), 725–745. [DOI] [PubMed] [Google Scholar]
- Goodenow C, Szalacha LA, Robin LE, & Westheimer K (2008). Dimensions of sexual orientation and HIV-related risk among adolescent females: Evidence from a statewide survey. American Journal of Public Health, 98(6), 1051–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2011). The social environment and suicide attempts in lesbian, gay, and bisexual youth. Pediatrics, 127(5), 896–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Hughes T, McCabe SE, Wilsnack SC, West BT, & Boyd CJ (2010a). Victimization and substance use disorders in a national sample of heterosexual and sexual minority women and men. Addiction, 105(12), 2130–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Szalacha LA, Johnson TP, Kinnison KE, Wilsnack SC, & Cho Y (2010b). Sexual victimization and hazardous drinking among heterosexual and sexual minority women. Addictive Behaviors, 35(12), 1152–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns MM, Lowry R, Rasberry CN, Dunville R, Robin L, Pampati S, & Mercer Kollar LM (2018). Violence victimization, substance use, and suicide risk among sexual minority high school students—United States, 2015–2017. Morbidity and Mortality Weekly Report, 67(43), 1211–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, Kinchen S, Shanklin SL, Flint KH, Hawkins J, Harris WA, … Whittle L (2014). Youth risk behavior surveillance—United States, 2013. Morbidity and Mortality Weekly Report: Surveillance Summaries, 63(4), 1–168. [PubMed] [Google Scholar]
- Kerr D, Ding K, Burke A, & Ott-Walter K (2015). An alcohol, tobacco, and other drug use comparison of lesbian, bisexual, and heterosexual undergraduate women. Substance Use & Misuse, 50(3), 340–349. [DOI] [PubMed] [Google Scholar]
- Kline RB (1998). Principles and practices of structural equation modeling. New York: Guilford Press. [Google Scholar]
- Kosciw JG, Palmer NA, Kull RM, & Greytak EA (2013). The effect of negative school climate on academic outcomes for LGBT youth and the role of in-school supports. Journal of School Violence, 12(1), 45–63. [Google Scholar]
- Lewis RJ, Milletich RJ, Derlega VJ, & Padilla MA (2014). Sexual minority stressors and psychological aggression in lesbian women’s intimate relationships: The mediating roles of rumination and relationship satisfaction. Psychology of Women Quarterly, 38(4), 535–550. [Google Scholar]
- Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, … Brent DA (2011). Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. Journal of Adolescent Health, 49(2), 115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin SL, Fisher BS, Warner TD, Krebs CP, & Lindquist CH (2011). Women’s sexual orientations and their experiences of sexual assault before and during university. Women’s Health Issues, 21(3), 199–205. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2018). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Poteat VP, Scheer JR, Marx RA, Calzo JP, & Yoshikawa H (2015). Gay-straight alliances vary on dimensions of youth socializing and advocacy: Factors accounting for individual- and setting-level differences. American Journal of Community Psychology, 55, 422–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhew IC, Stappenbeck CA, Bedard-Gilligan M, Hughes T, & Kaysen D (2017). Effects of sexual assault on alcohol use and consequences among young adult sexual minority women. Journal of Consulting and Clinical Psychology, 85 (5), 424–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell ST, Driscoll AK, & Truong N (2002). Adolescent same-sex romantic attractions and relationships: Implications for substance use and abuse. American Journal of Public Health, 92(2), 198–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan C, & Futterman D (1997). Lesbian and gay youth: Care and counseling. Journal of Adolescent Medicine, 8(2), 207–374. [PubMed] [Google Scholar]
- Saewyc E, Skay C, Richens K, Reis E, Poon C, & Murphy A (2006). Sexual orientation, sexual abuse, and HIV-risk behaviors among adolescents in the Pacific Northwest. America Journal of Public Health, 96(6), 1104–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saewyc EM, Poon CS, Homma Y, & Skay CL (2008). Stigma management? The links between enacted stigma and teen pregnancy trends among gay, lesbian, and bisexual students in British Columbia. The Canadian Journal of Human Sexuality, 17(3), 123–139. [PMC free article] [PubMed] [Google Scholar]
- Sell RL, Wells JA, & Wypij D (1995). The prevalence of homosexual behavior and attraction in the United States, the United Kingdom and France: Results of national population-based samples. Archives of Sexual Behavior, 24(3), 235–248. [DOI] [PubMed] [Google Scholar]
- Shilo G, Antebi N, & Mor Z (2015). Individual and community resilience factors among lesbian, gay, bisexual, queer and questioning youth and adults in Israel. American Journal of Community Psychology, 55(1–2), 215–227. [DOI] [PubMed] [Google Scholar]
- Sigurvinsdottir R, & Ullman SE (2015). The role of sexual orientation in the victimization and recovery of sexual assault survivors. Violence and Victims, 30, 636–648. [DOI] [PubMed] [Google Scholar]
- Snyder H, & Sickmund M (2000, July). Sexual assault of young children as reported to law enforcement: Victim, incident, and offender characteristics. National Centre for Juvenile Justice. Retrieved from www.unh.edu/ccrc/factsheet.htmW3 [Google Scholar]
- Stevens S (2012). Meeting the substance abuse treatment needs of lesbian, bisexual and transgender women: Implications from research to practice. Substance Abuse and Rehabilitation, 3(Suppl 1), 27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tornello SL, Riskind RG, & Patterson CJ (2014). Sexual orientation and sexual and reproductive health among adolescent young women in the United States. Journal of Adolescent Health, 54(2), 160–168. [DOI] [PubMed] [Google Scholar]
- Vanderweele TJ (2015). Explanation in causal inference: Methods for mediation and interaction. New York: Oxford University Press. [Google Scholar]


