Abstract
Background: The United States continues to account for the highest proportion of the global Coronavirus Disease-2019 (COVID-19) cases and deaths. Currently, it is important to contextualize COVID-19 fatality to guide mitigation efforts.
Objectives: The objective of this study was to assess the ecological factors (policy, health behaviors, socio-economic, physical environment, and clinical care) associated with COVID-19 case fatality rate (CFR) in the United States.
Methods: Data from the New York Times’ COVID-19 repository and the Centers for Disease Control and Prevention Data (01/21/2020 - 02/27/2021) were used. County-level CFR was modeled using the Spatial Durbin model (SDM). The SDM estimates were decomposed into direct and indirect impacts.
Results: The study found percent positive for COVID-19 (0.057% point), stringency index (0.014% point), percent diabetic (0.011% point), long-term care beds (log) (0.010% point), premature age-adjusted mortality (log) (0.702 % point), income inequality ratio (0.078% point), social association rate (log) (0.014% point), percent 65 years old and over (0.055% point), and percent African Americans (0.016% point) in a given county were positively associated with its COVID-19 CFR. The study also found food insecurity, long-term beds (log), mental health-care provider (log), workforce in construction, social association rate (log), and percent diabetic of a given county as well as neighboring county were associated with given county’s COVID-19 CFR, indicating significant externalities.
Conclusion: The spatial models identified percent positive for COVID-19, stringency index, elderly, college education, race/ethnicity, residential segregation, premature mortality, income inequality, workforce composition, and rurality as important ecological determinants of the geographic disparities in COVID-19 CFR.
Keywords: spatial analysis, health status disparities, social determinants of health, public policy, coronavirus disease 2019, sars-cov-2
INTRODUCTION
The novel coronavirus of 2019 (COVID-19) pandemic continues to spread in the United States and around the world. The United States, as of April 11, 2021, recorded 31.1 million COVID-19 cases and 561 231 deaths.1 Cases and deaths in the United States continue to account for the largest share of global cases (23%) and global deaths (19%).2 Containing the COVID-19 pandemic in the United States was challenging due to virus contagion characteristics, its pathophysiology, and socio-political factors.3 In response to the pandemic, many states initially adopted safety measures such as mask mandates, social distancing and safety measures for operations of certain businesses.4,5 After implementing these restrictive measures including lockdowns, many states rolled back such policies in 2020.6 Despite these rollbacks, personal safety measures (mask mandates and social distancing) were continued into the year 2021. However, as of the writing of this study, 14 states in the United States have lifted mask mandates.7
Safety measures such as the closure of business establishments, stay-at-home orders, and social distancing mandates severely impacted the economy.8 In response to the pandemic, lawmakers passed three stimulus packages and the Coronavirus Aid, Relief, and Economic Security Act (CARES) Act, with additional relief legislation expected.9,10 As of April 11, 2021, Moderna, Pfizer, and Johnson & Johnson vaccines have received emergency use authorization by the US Food and Drug Administration and are being rolled out in phases. Other biopharmaceutical companies are conducting clinical trials for 60 COVID-19 vaccine candidates.11 The current vaccine rollout will continue to gain momentum while other COVID-19 vaccines may receive market approval in the near future. Despite this progress, experts recommend that the public follow COVID-19 safety measures due to slow initial rollout, uncertainties surrounding COVID-19 vaccines (virus mutations, duration of immunity, real world effectiveness, vaccine uptake, etc.) and vaccine hesitancy.12,13 In summary, the US government and the scientific community has undertaken various measures to address the needs of the population during the COVID-19 pandemic. However, the assessment of the impact of ecological contextual factors such as health behaviors, clinical care and burden, socio-economic, and physical environment-related characteristics on the course of the COVID-19 pandemic is necessary. The contextual understanding from such a study is required to gauge whether lock-down measures worked and to what extent. Moreover, the study also aids in identifying high-risk areas for targeting vaccine distribution. Therefore, having a thorough knowledge of these ecological contextual factors is critical to address the public health and economic challenges and prioritize resources.
Studies so far have generated predictive models for growth in COVID-19 incidence and mortality and estimated the impacts of some community-level factors on COVID-19 incidence and mortality. Millett et al. and Khanijahani et al. focused on assessing the ecological determinants of susceptibility to COVID-19 outcomes among predominantly African American counties, while Fielding-Miller et al. and Peters et al. performed a similar assessment along the rural-urban continuum.14–17 Few studies have assessed the spatial determinants of COVID-19 transmission.3,18,19 Recently, Sun et al. assessed the relationship between various county-level determinants and COVID-19 incidence while Andersen et al. also identified high prevalence clusters.3,18 These studies evaluated the incidence and prevalence during the initial phase of the pandemic and limited the analysis to a few county-level and policy-related factors.
Incidence and mortality were critical outcomes in shaping the initial pandemic response to reduce the contagion. However, to reduce fatalities in the current stage of the pandemic, an increasing focus is placed on mitigation strategies such as increasing vaccination rates and continuing safety precautions such as social distancing and mask use. Therefore, COVID-19 case-fatality rate (CFR) is a useful outcomes measure in the current stage of the pandemic. CFR, being less susceptible to testing and reporting biases, also reflects the disease severity. In a study led by author Cao, country-level demographic and socioeconomic characteristics on COVID-19 CFR were presented.20 However, to our knowledge, in the United States, no study has estimated the effect of county-level ecological factors, including policy-related factors, on COVID-19 CFR.
The objective of the current study was to assess the impact of county-level ecological factors, using spatial econometric analysis, on the COVID-19 CFR over one year of the pandemic.
METHODS
Data source and study design
The current study used county-level COVID-19 confirmed cases and deaths data from the New York Times repository extracted as of February 27, 2021, and included data up until that date.18 The study used county-level characteristics from 2020 County Health Rankings data and 2018-2019 Area Health Resource File data. State-level stringency index, percent positive for COVID-19, and social distancing score were obtained from Oxford COVID-19 government response tracker, the COVID Tracking Project, and Unacast, respectively.4,21–24 Alaska and Hawaii counties were excluded from the analysis. The US counties ESRI Shapefile was obtained from the US Census Bureau.25 The study employed a cross-sectional ecological study design to assess the association between county-level characteristics on the cumulative COVID-19 CFR.
Outcomes
The county-level US COVID-19 cumulative confirmed cases and deaths data from the New York Times repository was extracted as of February 27, 2021, data up until that date was included.18 The COVID-19 cumulative CFR was operationally defined as a ratio of the cumulative COVID-19 deaths by cumulative COVID-19 cases.20 The current analysis used CFR as the outcome of interest because it reflects the disease severity, treatment effectiveness, and responsiveness of the health-care system.20 Additionally, since the measure is a ratio, compared to incidence rate or mortality rate, the CFR is less sensitive to differences in testing rates across regions.
Covariates
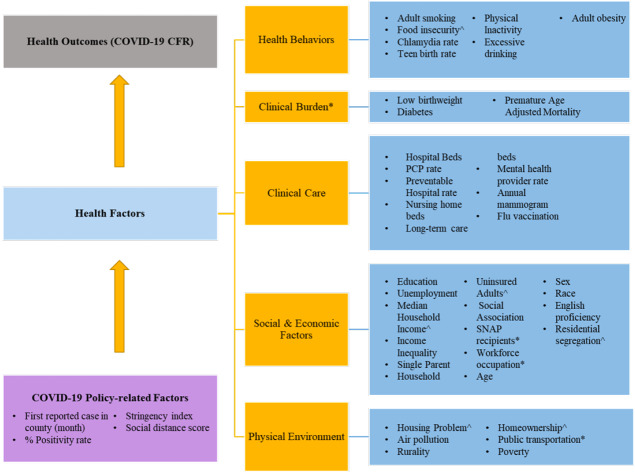
The covariates selected within the model to predict the county-level CFR were adapted from the County Health Ranking Framework (CHRF).26 The framework categorizes health factors into four sub-categories, namely health behaviors, clinical care, socioeconomic factors, and physical environment (Figure 1). Each of the sub-categories is further divided into individual factors. The CHRF model was used in the current analysis because it provides a well-established theoretical framework for studying ecological determinants of health outcomes. The current analysis augmented the CHRF by including additional covariates based on additional demographic measures from county health ranking, and prior ecological studies on COVID-19. Firstly, an additional sub-category of “clinical burden” was added, which included measures such as low- birth weight, percent diabetes prevalence, and premature age-adjusted mortality. Secondly, nursing home beds, long-term care beds, and total hospital beds were added to the clinical care sub-category.3 Thirdly, population characteristics such as rurality, poverty, age distribution, population, population density, supplemental nutritional assistance program (SNAP) eligibility, and percentage of workforce in various occupational categories were added to the social and economic factors sub-category.3,15,18,27,28 Additionally, physical environmental factors such as percentage of workers using public transport, were added to the respective sub-category.28 Finally, COVID-19 related factors were added to the model, which included month of first infection in the county, positivity rate for COVID-19 at the state-level, social distancing score, and stringency index.3,4,20–23,29 The final list of potential county-level covariates and corresponding rationale are described in Table 1. Although the CHRF model assigns weight to each of the components, they were not utilized in the current analysis as no composite rank score was calculated.
Figure 1: Theoretical Framework Based on the County Health Rankings Model To Establish a Relationship Between COVID-19 Case Fatality Rate and County-level Ecological Factors.
Abbreviations: CFR, Case fatality rate; SNAP, supplemental nutritional assistance program.
^ indicates that the data was obtained from additional resources and supplementary files of the County Health Rankings26; * indicates that the data was obtained from sources other than those in the County Health Rankings data.
Table 1: Ecological Factors Used in the Analysis: Source Definitions and Modifications.
| Factors | Definitions & Rationale | Source |
|---|---|---|
| Calendar Month of the First Reported Case in the State | Generated as the month when the first COVID-19 case was reported in the county. Based on the frequency distribution the following categories were created: January, February, March, April, May, and June to December. Month of first reported case has been used in previous studies. Earlier studies have included this variable due to its significant impact on the cumulative cases and deaths during the early phases of the pandemic.30 | 2020-2021 New York Times COVID-19 & Centers for Disease Control and Prevention Data1 |
| Percent Positive for COVID-19* | This factor was defined as the proportion of all COVID-19 tests performed that are positive. Positivity rate = (positive tests)/(total tests) x 100%. Percent positivity rate is a proxy measure for extent of under/over testing and has been included to control for impact of geographic differences in testing rates.31 |
The COVID Tracking Project21 |
| Social Distance Score |
It is defined as the average numerical score based on the following three metrics:
During the initial phases of the pandemic, social distances scores were found to be associated with lower COVID-19 mortality.23 |
Unacast22 |
| Stringency Index | Composite measure based on 9 response indicators, including school closures, workplace closures, testing policy and travel bans, rescaled to a value from 0 to 100 (100=strictest response). Stringency index has been previously used in ecological research on COVID-19 CFR.20 | Oxford COVID-19 Government Response Tracker4 |
| Percent Adult Smokers | Percentage of adults who are current smokers. | CHRF Data25 |
| Percent of Poor or Fair Health | Percentage of adults reporting fair or poor health (age-adjusted). | |
| Percent Low Birthweight | Percentage of live births with low birthweight (< 2500 grams). | |
| Teen Birth Rate | Births per 1000 females ages 15-19 | |
| Percent Adult Obesity | Percentage of the adult population (age 20 and older) who report a body mass index greater than or equal to 30 kg/m.2 | |
| Percent Excessive Drinking | Percentage of adults reporting binge or heavy drinking. | |
| Percent Flu Vaccine | Percentage of fee-for-service Medicare enrollees who had an annual flu vaccination. | |
| Percent with Annual Mammogram | Percentage of female Medicare enrollees having an annual mammogram (age 65- 74). | |
| Percent Physical Inactivity | Percentage of adults age 20 and over reporting no leisure-time physical activity. | |
| Income Inequality Ratio | Ratio of household income at the 80th percentile to income at the 20th percentile. | |
| Primary Care Physicians Rate (log)* | Log of ratio of population to primary care physicians. | |
| Preventable Hospitalization Rate (log)* | Rate of hospital stays for ambulatory-care sensitive conditions per 100 000 Medicare enrollees. | |
| Percent Educated at Some College | Percentage of adults aged 25-44 with some post-secondary education. | |
| Percent Unemployment | Number of people aged 16 years and above unemployed and looking for work. | |
| Percent Single Parent | Percentage of children who live in single-parent households. | |
| Social Association Rate | Number of membership associations per 10 000 population. | |
| Pollution Level: PM 2.5 | Average daily density of fine particulate matter in micrograms per cubic meter (PM2.5). | |
| Percent Severe Housing Problem | Percentage of households with at least 1 of 4 housing problems: overcrowding, high housing costs, lack of kitchen facilities, or lack of plumbing facilities. | |
| Percent Homeownership | Percentage of occupied housing units that are owned. | |
| Percent Uninsured Adult | Percentage of adults under age 65 without health insurance. | |
| Premature Age-adjusted Mortality | Number of deaths among residents under age 75 per 100 000 population (age-adjusted). | |
| Median Household Income (in Thousands) | The income where half of households in a county earn more and half of households earn less. | |
| Percent Over 65 | Percentage of population aged 65 and older. | |
| Percent Less Than 18 | Percentage of population below 18 years of age. | |
| Percent Black | Percentage of population who are non-Hispanic African American. | |
| Percent Native American | Percentage of population who are American Indian or Alaska Native. | |
| Percent Hispanic | Percentage of population who are Hispanic. | |
| Percent Female | Percentage of population who are female. | |
| Segregation Index: White/Non-White | Index of dissimilarity where higher values indicate greater residential segregation between non-White and White county residents. | |
| Percent Rural | Percentage of population living in a rural area. | |
| Percent Not Proficient in English | Percentage of population who are not proficient in English. | |
| Percent Diabetics | Percentage of adults aged 20 and above with diagnosed diabetes. | |
| Percent with Food Insecurity | Percentage of population who lack adequate access to food. | |
| Mental Health Provider Rate | Mental health providers per 100 000 population. | |
| Chlamydia Rate (Log) | Chlamydia cases per 100 000 population | |
| Percent SNAP Recipients | Percentage of the population on food stamps or SNAP. | 2019-2020 AHRF |
| Percent Public Transportation | Percentage of the population using public transportation. | |
| Percent of Workforce in Education, Health-care and Social Assistance Field | Percentage of the population in the occupation of education/health-care/social assistance. | |
| Percent of Workforce in Construction | Percentage of the population who work in construction. | |
| Percent of Workforce in Manufacturing | Percentage of the population who are manufacturing workers. | |
| Percent Poverty | Percentage of the population below poverty level. | |
| Hospital Bed Rates (log) | Number of beds regularly maintained (set up and staffed for use) for inpatients. | |
| Nursing Home Beds | Number of nursing home unit beds in hospitals. | |
| Long-term Care Beds (log) | Number of long-term care beds in hospitals. | |
| Population | Resident population. | |
| Population Density (log) | Persons per 100 square mile area. |
Abbreviations: AHRF, Area Health Resource Files; CHRF, County Health Ranking Framework; SNAP, supplemental nutritional assistance program.
*These variables are derived or converted for use within the regression model.
Statistical Analyses
Descriptive univariate statistics of the weighted county-level characteristics were generated. Firstly, all covariates in Table 1, selected as potential covariates, underwent a two-step covariate selection process. In the first step, multicollinearity was assessed and factors with variance inflation factor >7 were excluded.31 In the second step, Pearson correlation between remaining factors was tested (Supplemental Table 1) and factors with correlation greater than 0.7 were excluded.20 All remaining factors were used in regression analysis. Secondly, the presence of spatial correlation was confirmed by performing Moran’s I test for spatial correlation. Two island counties were excluded because spatial regression analysis necessitates that the data contains no island counties. Based on prior research, the LeSage and Pace method was used to determine the best fit spatial regression model.30 A first-order queen spatial weight matrix was employed for all spatial models. The queen matrix defines neighbor relationships if the counties either share a border or a vertex. All analysis was performed in RStudio (R) v 4.0.3 (Boston, Massachusetts) and QGIS v 3.16.0 (Berne, Switzerland).
RESULTS
The final analysis included data from 3101 counties from the mainland United States. Between January 20, 2020 to February 27, 2021, the population-weighted COVID-19 CFR for the mainland United States was 1.82%. Table 2 demonstrates the descriptive statistics of the COVID-19 CFR and county-level determinants, namely, COVID-19 policy-related factors, health behaviors, clinical burden, clinical care, socio-economic, and physical environment factors. Some 2097 counties reported their first case in March 2020. The percent positivity for COVID-19 was 9%. The mean social distance score and stringency index at the county-level was 1.75 and 49.14, respectively. The proportion of adult smokers, those with physical inactivity, obesity, and Medicare enrollees who were administered influenza vaccines were 15%, 23%, 29%, and 46%, respectively. At the county- level, the average ratio of population to primary care physicians was 74 and the average preventable hospitalization rate was 4545 per 10 000 Medicare enrollees. Premature age-adjusted mortality was 342 per 100 000. Among socio-economic factors, the proportion of the workforce in education/health-care/social assistance field, construction, and manufacturing comprised 23%, 7%, and 10% of the population, respectively. Additionally, unemployment was 4%, 12% of adults were uninsured, the mean income inequality ratio was 5 and adults with some college education made up 65% of the population. About 13% were African Americans, 18% Hispanics, 1% Native Americans, 51% females, 33% of the children lived in single-parent households, and 4% of the population was not proficient in English. The percentage of the population older than 65 years and less than 18 years were 16% and 22%, respectively. On average, 19% of counties were rural, the homeownership rate was 64%, 18% used public transportation and 18% of households had severe housing problems. Lastly, population density/100 sq. miles was found to be 2067.
Table 2: Descriptive Statistics of Ecological Factors (N=3101).
| Ecological Factors | Overall | VIF | |
| Sample size | 326 Million (population of 3101 counties) | ||
| Mean | SD | ||
| Cases | 110 257.75 | 214 169.92 | |
| Deaths | 1991.70 | 3956.85 | |
| Case fatality rate# | 1.82 | 0.82 | |
| Census Region [n, %] ^ | |||
| Northeast | 217.00 | 7.00 | |
| Midwest | 1055.00 | 33.90 | |
| South | 1422.00 | 45.80 | |
| West | 414.00 | 13.30 | |
| COVID-19 Policy-related Factors | |||
| Calendar Month of the First Reported Case in the State [n, %] ^ | n | % | 2.71 |
| January | 6.00 | 0.20 | |
| February | 16.00 | 0.50 | |
| March | 2097.00 | 67.50 | |
| April | 692.00 | 22.30 | |
| May | 133.00 | 4.30 | |
| June to December | 164.00 | 5.30 | |
| % Positive for COVID-19 | 9.30 | 4.10 | 1.99 |
| Social Distance Score | 1.75 | 0.63 | 3.30 |
| Stringency Index | 49.14 | 11.21 | 2.03 |
| Health Behaviors | |||
| % Adult Smoking | 15.31 | 3.43 | 8.85 |
| Food Insecurity | 7.83 | 0.85 | 3.20 |
| Chlamydia Rate* | 520.05 | 236.40 | 3.09 |
| % Fair or Poor Health | 16.74 | 3.83 | 15.65 |
| Teen Birth Rate | 22.81 | 11.11 | 5.11 |
| % Physical Inactivity | 23.31 | 5.37 | 2.50 |
| % Excessive Drinking | 18.76 | 2.80 | 3.09 |
| % Adult Obesity | 29.06 | 5.53 | 2.06 |
| Clinical Burden | |||
| % Low Birthweight | 8.07 | 1.42 | 3.07 |
| % Diabetic | 10.25 | 2.77 | 1.91 |
| Premature Age Adjusted Mortality* | 341.61 | 93.01 | 4.95 |
| Clinical Care | |||
| Primary Care Physicians Rate* | 75.41 | 30.36 | 2.17 |
| Preventable Hospitalization Rate | 4545.01 | 1270.42 | 1.63 |
| Hospital Beds* | 3200.65 | 5035.30 | 1.84 |
| Nursing Home Beds* | 77.79 | 187.85 | 1.13 |
| Long-term Care Beds* | 128.89 | 260.27 | 1.28 |
| Mental Health Provider Rate* | 247.42 | 161.55 | 2.09 |
| % With Annual Mammogram | 41.15 | 6.19 | 2.29 |
| % Influenza Vaccinations | 46.11 | 6.91 | 2.05 |
| Socio-economic Factors | |||
| % SNAP Recipients | 12.43 | 5.92 | 7.25 |
| % of Workforce in Education/Health-care/Social Assistance Field | 23.12 | 3.92 | 1.92 |
| % of Workforce in Construction | 6.52 | 1.81 | 1.53 |
| % of Workforce in Manufacturing | 10.23 | 5.40 | 2.30 |
| Income Inequality Ratio | 4.72 | 0.78 | 2.24 |
| % Adults with Some College Education | 65.33 | 9.81 | 3.97 |
| % Unemployment | 3.96 | 1.12 | 2.42 |
| % Children in Single-parent Households | 33.15 | 8.68 | 3.67 |
| Social Association Rate* | 9.01 | 3.60 | 1.67 |
| % Uninsured Adults | 10.25 | 4.81 | 3.40 |
| Median Income* | US$65 045.85 | US$17 989.94 | 11.00 |
| % 65 Years Old and Over | 16.02 | 4.04 | 5.78 |
| % Less Than 18 Years of Age | 22.44 | 2.94 | 4.70 |
| % African American | 12.55 | 12.56 | 5.19 |
| % Native Americans | 1.24 | 3.18 | 2.64 |
| % Hispanic | 18.35 | 17.18 | 7.80 |
| % Female | 50.76 | 1.23 | 2.70 |
| % Not Proficient in English | 4.41 | 4.38 | 4.17 |
| Residential Segregation Non-White/White | 37.03 | 11.27 | 1.47 |
| % Poverty | 13.05 | 4.82 | 11.57 |
| Physical Environment | |||
| Air Pollution-particulate Matter (2.5) | 10.08 | 2.11 | 2.94 |
| % Severe Housing Problem | 18.09 | 5.85 | 2.82 |
| % Rural | 18.68 | 24.06 | 4.58 |
| % Homeownership | 63.77 | 10.82 | 3.21 |
| % Public Transportation | 18.24 | 3.95 | 1.31 |
| Population* | 1 172 722.28 | 1 940 307.84 | 8.34 |
| Population Density per 100 sq. miles* | 2067.26 | 6497.01 | 9.12 |
Abbreviations: SD, Standard Deviation; SNAP, supplemental nutritional assistance program; VIF, Variance Inflation Factor.
# Cumulative case fatality rate calculated as of February 27, 2021.
* VIF was calculated on the log transformed values.
^ Unweighted estimates, as this represents the number of counties
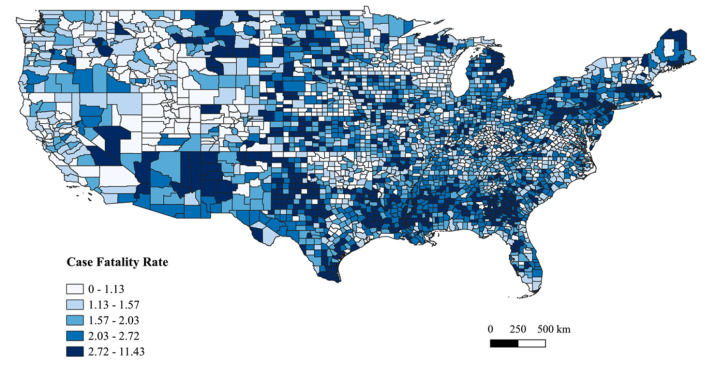
Figure 2 presents the spatial distribution (quintiles) of COVID-19 CFR. In the West, Washington’s Spokane area and Nevada’s Las Vegas area had high COVID-19 CFR. High COVID-19 CFR clusters were found in border counties of Arizona’s Phoenix area and in New Mexico. In Montana, all major cities such as Helena, Butte, and Billings and along the border of Wyoming (specifically near Yellow Stone National Park) had high COVID-19 CFR. In the Midwestern region, barring the high COVID-19 CFR clusters in Michigan’s Upper Peninsula area, there were many scattered counties with high CFR. The Deep South states of Mississippi, Louisiana, Tennessee, central Alabama, and Arkansas had clusters of high COVID-19 CFR. The Texas panhandle region, the Corpus Christie, Texas, area and the area along the US-Mexico border had clusters of high COVID-19 CFR. In the Northeastern region, high COVID-19 CFR clusters were found between the large parts of Pennsylvania and New Jersey, and in the Boston, Massachusetts, area. Additionally, in Maine, clusters of high COVID-19 CFR were found around Acadia National Park and the northeastern parts of the state.
Figure 2: Spatial Distribution of the Cumulative COVID-19 Case Fatality Rate by Quintiles as of February 27, 2021.
The first step in the factor selection process identified and excluded percent adult smokers, percent fair/poor health, log population density, log population, percent under poverty, median income, percent eligible for SNAP benefits due to multicollinearity, which is shown in Table 2. Similarly, percent smokers, teen birth rate, percent SNAP eligible, log population, log population density, percent speaking language other than English were excluded based on high correlation with other factors (Supplemental Table 1). The presence of spatial autocorrelation was confirmed based on a significant Moran’s I test statistic (Moran’s I=0.256, P-value<0.001). The LeSage and Pace method identified that Spatial Durbin Model (SDM) was a better fit to the data compared with other spatial regression models. The significant Rho parameter of the SDM model indicates that (Rho=0.447, P-value<0.001), a 1% increase in a neighboring county’s CFR, also results in 0.447% increase in CFR rate in the particular county.
The multivariable SDM results are presented in Table 3. The factors significantly associated with CFR included percent positive for COVID-19 (β=0.059), stringency index (β=0.015), log nursing home beds (β=-0.005), log long-term care beds (β=0.008), percent workforce in construction (β=-0.019), log premature age-adjusted mortality (β=0.711), income inequality ratio (β=0.076), percent population 65 years and older (β=0.055), and percent severe housing problem (β=-0.023). Additionally, the spatial lag term for factors such as percent positive for COVID-19 (lag β=-0.048), stringency index (lag β=- 0.017), social distancing score (lag β=-0.136), adult obesity (lag β=-0.026), log long-term care bed (lag β=0.025), log mental health provider rate (lag β=-0.080), percent workforce in education/health-care/social assistance (lag β=0.018), log social association rate (lag β=0.038), percent female (lag β=-0.057), and percent rurality (lag β=0.005) were also associated with COVID-19 CFR.
Table 3: Spatial Durbin Model for the Case Fatality Rates as of February 27, 2021 Using NYT1, AHRF24, and CHRF26 Datasets.
| Ecological Factors | Spatial Durbin Model | Decomposition Estimates | |||
| Estimate | Lag Estimate | Direct | Indirect | Total | |
| COVID-19 Policy-related Factors | |||||
| Calendar Month of the First Reported Case in the State [n, %]* | |||||
| January | Reference | ||||
| February | -0.253 | -0.288 | -0.253 | -0.673 | -0.927 |
| March | -0.375 | 0.380 | -0.345 | 0.333 | -0.011 |
| April | -0.407 | 0.231 | -0.396 | 0.048 | -0.348 |
| May | -0.368 | 0.026 | -0.378 | -0.257 | -0.635 |
| June to December | -0.586 | 0.845 | -0.521 | 0.955 | 0.434 |
| % Positive for COVID-19 | 0.059 *** | -0.048 *** | 0.057 *** | -0.035 ** | 0.022 ** |
| Social Distance Score | 0.062 | -0.136 * | 0.056 | -0.185 | -0.129 |
| Stringency Index | 0.015 ** | -0.017 ** | 0.014 ** | -0.017 ** | -0.003 |
| Health Behaviors | |||||
| Food Insecurity | 0.000 | 0.086 | 0.011 | 0.148 * | 0.160 * |
| Chlamydia Rate (log) | -0.034 | 0.173 | -0.024 | 0.260 | 0.236 |
| % Physical Inactivity | 0.002 | -0.009 | 0.002 | -0.013 | -0.011 |
| % Excessive Drinking | -0.002 | 0.025 | 0.000 | 0.043 | 0.043* |
| % Adult Obesity | -0.009 * | -0.026 * | -0.013 ** | -0.054 *** | -0.066 *** |
| Clinical Burden | |||||
| % Low Birthweight | -0.022 | 0.002 | -0.023 | -0.008 | -0.031 |
| % Diabetic | 0.008 | 0.022 | 0.011 * | 0.044 * | 0.055 * |
| Premature Age Adjusted Mortality (log) | 0.711 *** | -0.469 * | 0.702 *** | -0.234 | 0.467 |
| Clinical Care | |||||
| Primary Care Physicians Rate (log) | -0.003 | -0.005 | -0.003 | -0.009 | -0.011 |
| Preventable Hospitalization Rate | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Hospital Beds (log) | 0.003 | 0.001 | 0.003 | 0.003 | 0.006 |
| Nursing Home Beds | -0.005 * | -0.001 | -0.005 * | -0.006 | -0.011 |
| Long-term Care Beds (log) | 0.008 * | 0.025 *** | 0.010 ** | 0.048 *** | 0.058 *** |
| Mental Health Provider Rate (log) | -0.001 | -0.080 *** | -0.010 | -0.136 *** | -0.146 *** |
| % With Annual Mammogram | -0.001 | -0.003 | -0.001 | -0.004 | -0.005 |
| % Influenza Vaccinations^ | -0.004 | 0.003 | -0.004 | 0.002 | -0.002 |
| Socio-economic Factors | |||||
| % of Workforce in Education/Health-care/Social Assistance Field | 0.006 | 0.018 * | 0.009 | 0.036 ** | 0.045 ** |
| % of Workforce in Construction | -0.019 * | -0.027 | -0.024 ** | -0.063 * | -0.086 ** |
| % of Workforce in Manufacturing | 0.001 | 0.006 | 0.002 | 0.011 | 0.012 |
| Income Inequality Ratio | 0.076 * | -0.063 | 0.078 ** | -0.056 | 0.022 |
| % Adults with Some College Education | -0.004 | -0.001 | -0.004 ** | -0.005 * | -0.009 ** |
| % Unemployment | 0.039 | 0.040 | 0.045 | 0.096 | 0.141 |
| % Children in Single-parent Households | 0.003 | 0.004 | 0.003 | 0.008 | 0.011 |
| Social Association Rate (log) | 0.011 | 0.038 ** | 0.014 ** | 0.073 ** | 0.087 ** |
| % Uninsured Adults | 0.014 | 0.001 | 0.015 | 0.014 | 0.028 * |
| % 65 Years Old and Over | 0.055 *** | -0.009 | 0.055 *** | 0.024 | 0.079 ** |
| % Less Than 18 Years of Age | 0.016 | 0.020 | 0.018 | 0.044 | |
| % African American | 0.006 | 0.002 | 0.007 * | 0.009 | 0.016 * |
| % Native Americans | -0.007 | 0.000 | -0.007 | -0.006 | -0.013 |
| % Hispanic | -0.003 | 0.008 | -0.002 | 0.011 * | 0.009 |
| % Female | 0.018 | -0.057 ** | 0.013 | -0.081* | -0.068 |
| Residential Segregation Non-White/White | 0.001 | 0.007 * | 0.002 | 0.013 ** | 0.015 ** |
| Physical Environment | |||||
| Air Pollution-particulate Matter (2.5) | 0.012 | -0.035 | 0.009 | -0.050 | -0.041 |
| % Severe Housing Problem | -0.023 *** | 0.005 | -0.024 *** | -0.009 | -0.033 |
| % Rural | -0.001 | 0.005 * | 0.000 | 0.008 ** | 0.007 * |
| % Homeownership | 0.004 | -0.005 | 0.004 | -0.006 | -0.003 |
| % Public Transportation | 0.001 | 0.000 | 0.001 | -0.001 | 0.000 |
| Rho^ | 0.447*** | ||||
Abbreviations: AHRF, Area Health Resource Files; NYT, New York Times; CHR: County Health Rankings.
Level of significance: *P-value<0.05, **P-value<0.01, ***P-value<0.001.
^ spatial lag parameter
As the β from SDM are not directly interpretable, the estimates from the SDM were decomposed into direct and indirect effects using the Impacts command from spdep package as shown in Table 3.30,32 Several factors had significant direct impact on the county’s COVID-19 CFR. Firstly, two of the COVID-19 related factors, namely, percent positive for COVID-19 (direct impact: 0.057% point), and stringency index (direct impact: 0.014% point) were positively associated were higher COVID-19 CFR in that county. Secondly, among health behavior related factors, percent adult obesity (direct impact: -0.013% point) was negatively associated with COVID-19 CFR. Thirdly, among the clinical burden and clinical care related factors, percent diabetics (direct impact: 0.011% point), log premature age-adjusted mortality (direct impact: 0.702% point), and log long-term care beds (direct impact: 0.010% point) were positively associated with COVID-19 CFR, while log nursing home beds (direct impact: -0.005% point) was negatively associated with COVID-19 CFR. Several socio-economic factors, importantly, income inequality (direct impact: 0.078% point), log social association rate (direct impact: 0.014% point), and percentage African Americans (direct impact: 0.007% point) were positively associated with COVID-19 CFR, while percentage workforce in construction (direct impact: -0.024% point) and percentage adults with some college education (direct impact: -0.004% point) were negatively associated with COVID-19 CFR.
The decomposition estimates also demonstrated strong indirect effects of spatial lag terms indicating externality associated with ecological factors from surrounding counties on COVID-19 CFR. The directionality of the direct and indirect associations was similar for the majority of the factors. However, some of the factors demonstrated divergent direct and indirect effects on COVID-19 CFR. For illustration, among COVID-19 policy-related factors, both percent positive for COVID-19 (direct: 0.057% point; indirect impact: -0.035% point) and stringency index (direct impact: 0.014% point; indirect impact: -0.017% point) of neighboring counties were negatively associated with COVID-19 CFR in a given county. Interestingly, the magnitude of the indirect associations were larger than the direct associations for the majority of the factors, except for percent 65 years old and over (direct: 0.055% point; indirect: 0.024% point), and percent severe housing problem (direct: -0.024% point; indirect: -0.009% point).
It is noteworthy that for some of the factors, while either the direct or indirect impacts were insignificant, the total impact was found to be significant: for example, food insecurity (total impact: 0.160), log of mental health provider rate (total impact: -0.146% point), percent of workforce in education/health-care/social assistance field (total impact: 0.045% point), percent uninsured adults (total impact: 0.028% point), percent 65 years old and over (total impact: 0.079% point), residential segregation non-White/White (total impact: 0.015% point), and percent rural (total impact: 0.007% point). For percent excessive drinking factor, although the direct and indirect impacts were found to be insignificant, the overall total impact (0.043% point) was significant.
DISCUSSION
To the best of our knowledge, this is the first spatial analysis study that captured and assessed the COVID-19 CFR through the year 2020-2021 (January 20, 2020 to February 27, 2021) of the COVID-19 pandemic in the United States. The study found that both direct and indirect impacts of food insecurity, diabetes, long-term care beds, and social association rate on COVID-19 CFR was positive. However, only the direct impact of stringency index, premature age-adjusted rate, income inequality ratio, population aged 65 years or more, and African Americans on COVID-19 CFR was significant and positive. Conversely, both the direct and indirect impacts of proportion of adults with obesity, mental health provider rate, workforce in construction, and adults with some college education on COVID-19 CFR was negative. While factors such as nursing home beds and severe housing problem had a negative direct impact on COVID-19 CFR, stringency index and percent females were found to have a negative indirect impact on COVID-19 CFR.
Only one study by Cao et al has assessed the ecological determinants of COVID-19 CFR but that study used country-level data.20 Similar to our study, Cao et al reported that stringency index and diabetes prevalence were associated with higher CFR. Although no US-based studies have assessed an association between county-level ecological factors and COVID-19 CFR, some studies have reported on the ecological determinants on COVID-19 mortality. A few studies have reported high deaths in counties with greater proportions of racial minorities (Hispanics and African Americans) and found results similar to the present study.15,33 Stokes et al found that greater proportions of income inequality ratio and African American population was associated with high death rates, which is similar to the relationship this study found with CFR as an outcome.29
Aside from the similarities with already published literature on COVID-19, this study adds to the literature on ecological determinants of COVID-19 CFR. Firstly, this study demonstrated a positive association between percent positive for COVID-19 and COVID-19 CFR. Percent positive for COVID-19 captures both community level transmission rate and inadequacy of testing.34 Hence, increased community-level testing and timely local-level lockdown policies may be needed to improve CFR. Surprisingly, the indirect impact of percent positive for COVID-19 was negative, which warrants further research. Secondly, unlike Cao et al, this study found that a higher stringency index in neighboring counties was significantly associated with lower COVID-19 CFR in a given county. However, unlike the indirect association, the direct association between stringency index and COVID-19 CFR was positive due to endogeneity. For illustration, states such as New York and Washington were the early hotspots for COVID-19 cases and deaths.4 As a result, due to early lockdown policies that lasted for a long duration, these states had higher stringency index values.6 Thirdly, workforce composition in a given county and its surrounding counties were also associated with COVID-19 CFR. Finally, our study found very strong positive association between premature age-adjusted mortality and COVID-19 CFR in a given county. Numerous studies have assessed determinants of premature age-adjusted mortality. Based on the research, public health interventions aimed at reducing premature age-adjusted mortality would also play a vital role in reducing COVID-19 CFR. The study has important limitations. Given the study is cross-sectional and ecological in nature no causal inferences or inferences at the individual level can be made. Although our study included percent positive for COVID-19, there are considerable differences in the testing rates across regions. Relative to incidence and mortality rates, the CFR is less sensitive to testing rates. However, if differential bias in testing of incidence and mortality rates persists then CFR may be biased. Even though stringency index and social distancing scores are included in the study, these measurements were taken at a specific time point. Further, the list of variables is by no means comprehensive and does not include several other factors such as local safety policies (county or city level), and compliance with local and federal prevention guidelines.
CONCLUSION
The findings of this study are more insightful than the mere coronavirus count meters and data visualizations that depict the spread of the COVID-19 pandemic. The current spatial models incorporated a comprehensive list of factors to ensure that the results, when parsed, offer a multi-faceted explanatory power. For illustration, these models helped identify factors including COVID-19 policy-related factors (stringency index, social distancing score, and percent positive for COVID-19), health behaviors (example: excessive drinking), clinical burden (example: percent diabetic, premature age-adjusted mortality), clinical care (example: mental health provider rates), socio-economic factors (example: race/ethnicity, income inequality, segregation index, education, workforce composition), and physical environment (example: rurality) as some of the important determinants of the geographic disparities in COVID-19 CFR. This study highlights the plausible effect of one’s residential location, vicinity, local state policy and the connectivity to the neighboring counties on COVID-19 CFR. The United States is facing the next set of challenges in limiting fatalities and COVID-19 mutations, while undertaking mass immunization for COVID-19. At this crucial juncture, the current study findings provide guidance on identifying areas at greater risk of COVID-19 CFR.
CONFLICTS OF INTEREST
The authors declare no competing interests.
CONSENT FOR PUBLICATION
All authors have consented for this manuscript to be published.
COMPETING INTERESTS
None.
AUTHORS’ CONTRIBUTIONS
NK and RW conceived and designed the study; NK and RW collected, cleaned, and curated the data; NK and RW conducted the statistical analysis. NK and RW discussed the results, interpreted the data, and modified the first manuscript. NK and RW supervised the data collection and interpreted the data. Both the authors have read and gave final approval for publication.
Supplementary Material
Acknowledgments
ACKNOWLEDGEMENTS
We would like to thank the New York Times for providing us with the data, which was based on reports from state and local health agencies.
Funding Statement
The study received no funding.
References
- The New York Times Coronavirus (COVID-19) Data in the United States. [2021-2-28]. https://github.com/nytimes/covid-19-data
- See Coronavirus Restrictions and Mask Mandates for All 50 States. The New York Times [2021-4-14]; https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html
- Analyzing the spatial determinants of local Covid-19 transmission in the United States. Andersen Lauren M., Harden Stella R., Sugg Margaret M., Runkle Jennifer D., Lundquist Taylor E. Feb;2021 Science of The Total Environment. 754:142396. doi: 10.1016/j.scitotenv.2020.142396. doi: 10.1016/j.scitotenv.2020.142396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blavatnik School of Government. University of Oxford Oxford COVID-19 Government Response Tracker. [2021-4-13]. https://www.bsg.ox.ac.uk/research/research-projects/covid-19-government-response-tracker#data
- Ballotpedia States that did not issue stay-at-home orders in response to the coronavirus (COVID-19) pandemic, 2020. [2020-11-15]. https://ballotpedia.org/Status_of_lockdown_and_stay-at-home_orders_in_response_to_the_coronavirus_(COVID-19)_pandemic,_2020
- Ballotpedia Travel restrictions issued by states in response to the coronavirus (COVID-19) pandemic, 2020-2021. [2021-4-11]. https://ballotpedia.org/Travel_restrictions_issued_by_states_in_response_to_the_coronavirus_(COVID-19)_pandemic,_2020-2021#Travel_restrictions.2C_advisories.2C_and_recommendations_by_state
- MultiState COVID-19 Mask Mandates by State. [2021-4-13]. https://www.multistate.us/issues/covid-19-mask-mandates-by-state
- International Monetary Fund Policy Responses to COVID-19. [2021-4-13]. https://www.imf.org/en/Topics/imf-and-covid19/Policy-Responses-to-COVID-19#U
- Investopedia Coronavirus Aid, Relief, and Economic Security (CARES) Act. [2021-4-13]. https://www.investopedia.com/coronavirus-aid-relief-and-economic-security-cares-act-4800707
- Peter G. Peterson Foundation What to Know About all Three Rounds of Coronavirus Stimulus Checks. [2021-4-13]. https://www.pgpf.org/blog/2021/03/what-to-know-about-all-three-rounds-of-coronavirus-stimulus-checks
- Covid-19 Vaccine Tracker. Corum J., Wee S.-L., Zimmer C. [2021-4-11];The New York Times. https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html?auth=login-google
- Dr. Fauci says masks, social distancing will still be needed after a Covid-19 vaccine—here’s why. Scipioni J. Nov 16;2020 [2020-11-27];CNBC Make it. https://www.cnbc.com/2020/11/16/fauci-why-still-need-masks-social-distancing-after-covid-19-vaccine.html
- Wehbi Nizar K., Wani Rajvi J., Klepser Donald G., Murry Janice, Khan Ali S. Vaccine. 1. Vol. 37. Elsevier BV; Impact of implementing a technology platform in community pharmacies to increase adult immunizations rates; pp. 56–60. [DOI] [PubMed] [Google Scholar]
- Assessing differential impacts of COVID-19 on Black communities. Millett Gregorio A., Jones Austin T., Benkeser David, Baral Stefan, Mercer Laina, Beyrer Chris, Honermann Brian, Lankiewicz Elise, Mena Leandro, Crowley Jeffrey S., Sherwood Jennifer, Sullivan Patrick S. Jul;2020 Annals of Epidemiology. 47:37–44. doi: 10.1016/j.annepidem.2020.05.003. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- County-level proportions of Black and Hispanic populations, and socioeconomic characteristics in association with confirmed COVID-19 cases and deaths in the United States. Preprint: Posted online June 5, 2020. Khanijahani Ahmad. medRxiv. 2020:1-23 doi: 10.1101/2020.06.03.20120667. [DOI] [Google Scholar]
- Social determinants of COVID-19 mortality at the county level. Preprint: Posted online July 1, 2020. Fielding-Miller Rebecca K., Sundaram Maria E., Brouwer Kimberly. medRxiv. 2020.05.03.20089698 doi: 10.1101/2020.05.03.20089698. doi: 10.1101/2020.05.03.20089698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Community susceptibility and resiliency to COVID-19 across the rural-urban continuum in the United States. Peters David J. Jun;2020 The Journal of Rural Health. 36(3):446–456. doi: 10.1111/jrh.12477. doi: 10.1111/jrh.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A spatial analysis of the COVID-19 period prevalence in U.S. counties through June 28, 2020: where geography matters? Sun Feinuo, Matthews Stephen A., Yang Tse-Chuan, Hu Ming-Hsiao. Dec;2020 Annals of Epidemiology. 52:54–59.e1. doi: 10.1016/j.annepidem.2020.07.014. doi: 10.1016/j.annepidem.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taking the inner route: Spatial and demographic factors affecting vulnerability to COVID-19 among 604 cities from inner São Paulo State, Brazil. Fortaleza C. M. C. B., Guimarães R. B., De Almeida G. B., Pronunciate M., Ferreira C. P. 2020Epidemiology and Infection. 148:e118. doi: 10.1017/s095026882000134x. doi: 10.1017/s095026882000134x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 case-fatality rate and demographic and socioeconomic influencers: worldwide spatial regression analysis based on country-level data. Cao Yang, Hiyoshi Ayako, Montgomery Scott. Nov;2020 BMJ Open. 10(11):1–12. doi: 10.1136/bmjopen-2020-043560. doi: 10.1136/bmjopen-2020-043560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Atlantic Monthly Group The COVID Tracking Project. [2021-4-13]. https://covidtracking.com/data/download
- Unacast Covid-19 Social Distancing Scoreboard. [2021-4-13]. https://www.unacast.com/covid19/social-distancing-scoreboard#scoreboard
- Effect of social distancing on COVID-19 incidence and mortality in the US. Preprint: Posted online June 12, 2020. VoPham Trang, Weaver Matthew D., Hart Jaime E., Ton Mimi, White Emily, Newcomb Polly A. medRxiv. 2020.06.10.20127589 doi: 10.1101/2020.06.10.20127589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources & Services Administration Area Health Resources File. [2021-4-13]. https://data.hrsa.gov/data/download?data=AHRF#AHRF
- United States Census Bureau Cartographic Boundary Files - Shapefile. [2020-10-27]. https://www.census.gov/geographies/mapping-files/time-series/geo/carto-boundary-file.html files/time-series/geo/carto-boundary-file.html. Updated 2019. Accessed October 27,
- The County Health Rankings: rationale and methods. Remington Patrick L, Catlin Bridget B, Gennuso Keith P. Apr 17;2015 Population Health Metrics. 13(1):1–12. doi: 10.1186/s12963-015-0044-2. doi: 10.1186/s12963-015-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Pollán Marina, Pérez-Gómez Beatriz, Pastor-Barriuso Roberto, Oteo Jesús, Hernán Miguel A, Pérez-Olmeda Mayte, Sanmartín Jose L, Fernández-García Aurora, Cruz Israel, Fernández de Larrea Nerea, Molina Marta, Rodríguez-Cabrera Francisco, Martín Mariano, Merino-Amador Paloma, León Paniagua Jose, Muñoz-Montalvo Juan F, Blanco Faustino, Yotti Raquel, Blanco Faustino, Gutiérrez Fernández Rodrigo, Martín Mariano, Mezcua Navarro Saturnino, Molina Marta, Muñoz-Montalvo Juan F., Salinero Hernández Matías, Sanmartín Jose L., Cuenca-Estrella Manuel, Yotti Raquel, León Paniagua José, Fernández de Larrea Nerea, Fernández-Navarro Pablo, Pastor-Barriuso Roberto, Pérez-Gómez Beatriz, Pollán Marina, Avellón Ana, Fedele Giovanni, Fernández-García Aurora, Oteo Iglesias Jesús, Pérez Olmeda María Teresa, Cruz Israel, Fernandez Martinez Maria Elena, Rodríguez-Cabrera Francisco D., Hernán Miguel A., Padrones Fernández Susana, Rumbao Aguirre José Manuel, Navarro Marí José M., Palop Borrás Begoña, Pérez Jiménez Ana Belén, Rodríguez-Iglesias Manuel, Calvo Gascón Ana María, Lou Alcaine María Luz, Donate Suárez Ignacio, Suárez Álvarez Oscar, Rodríguez Pérez Mercedes, Cases Sanchís Margarita, Villafáfila Gomila Carlos Javier, Carbo Saladrigas Lluis, Hurtado Fernández Adoración, Oliver Antonio, Castro Feliciano Elías, González Quintana María Noemí, Barrasa Fernández José María, Hernández Betancor María Araceli, Hernández Febles Melisa, Martín Martín Leopoldo, López López Luis-Mariano, Ugarte Miota Teresa, De Benito Población Inés, Celada Pérez María Sagrario, Vallés Fernández María Natalia, Maté Enríquez Tomás, Villa Arranz Miguel, Domínguez-Gil González Marta, Fernández-Natal Isabel, Megías Lobón Gregoria, Muñoz Bellido Juan Luis, Ciruela Pilar, Mas i Casals Ariadna, Doladé Botías Maria, Marcos Maeso M. Angeles, Pérez del Campo Dúnia, Félix de Castro Antonio, Limón Ramírez Ramón, Elías Retamosa Maria Francisca, Rubio González Manuela, Blanco Lobeiras María Sinda, Fuentes Losada Alberto, Aguilera Antonio, Bou German, Caro Yolanda, Marauri Noemí, Soria Blanco Luis Miguel, del Cura González Isabel, Hernández Pascual Montserrat, Alonso Fernández Roberto, Merino-Amador Paloma, Cabrera Castro Natalia, Tomás Lizcano Aurora, Ramírez Almagro Cristóbal, Segovia Hernández Manuel, Ascunce Elizaga Nieves, Ederra Sanz María, Ezpeleta Baquedano Carmen, Bustinduy Bascaran Ana, Iglesias Tamayo Susana, Elorduy Otazua Luis, Benarroch Benarroch Rebeca, Lopera Flores Jesús, Vázquez de la Villa Antonia. Aug;2020 The Lancet. 396(10250):535–544. doi: 10.1016/s0140-6736(20)31483-5. doi: 10.1016/s0140-6736(20)31483-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A spatial analysis of the effect of neighborhood contexts on cumulative number of confirmed cases of COVID-19 in U.S. Counties through October 20 2020. Sung Baksun. Jun;2021 Preventive Medicine. 147:217–225. doi: 10.1016/j.ypmed.2021.106457. doi: 10.1016/j.ypmed.2021.106457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assessing the impact of the Covid-19 pandemic on US mortality: A county-level analysis. Preprint: Posted online September 26, 2020. Stokes Andrew C., Lundberg Dielle J., Hempstead Katherine, Elo Irma T., Preston Samuel H. medRxiv. 2020:2020.08.31.20184036 doi: 10.1101/2020.08.31.20184036. doi: 10.1101/2020.08.31.20184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeSage James P., Pace Robert Kelley. Introduction to Spatial Econometrics. Chapman & Hall/CRC; Boca Raton, FL: [DOI] [Google Scholar]
- James G., Witten D., Hastie T., Tibshirani R. An Introduction to Statistical Learning. Springer-Verlag; New York, NY: [Google Scholar]
- Package 'spdep'. Bivand R., Altman M., Anselin L.., et al. 2015 [2021-4-13];The Comprehensive R Archive Network. https://cran.r-project.org/web/packages/spdep/spdep.pdf Accessed: April 13, 2021.
- Risk for COVID-19 infection and death among Latinos in the United States: examining heterogeneity in transmission dynamics. Rodriguez-Diaz Carlos E., Guilamo-Ramos Vincent, Mena Leandro, Hall Eric, Honermann Brian, Crowley Jeffrey S., Baral Stefan, Prado Guillermo J., Marzan-Rodriguez Melissa, Beyrer Chris, Sullivan Patrick S., Millett Gregorio A. Dec;2020 Annals of Epidemiology. 52:46–53.e2. doi: 10.1016/j.annepidem.2020.07.007. doi: 10.1016/j.annepidem.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The impact of changes in diagnostic testing practices on estimates of COVID-19 transmission in the United States. Preprint: Posted online April 24, 2020. Pitzer Virginia E., Chitwood Melanie, Havumaki Joshua, Menzies Nicolas A., Perniciaro Stephanie, Warren Joshua L., Weinberger Daniel M., Cohen Ted. medRxiv. 2020;2020.04.20.20073338 doi: 10.1101/2020.04.20.20073338. doi: 10.1101/2020.04.20.20073338. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.