Abstract
High-altitude cerebral edema (HACE) is a rare condition of acute mountain sickness that manifests as consciousness disturbance and truncal ataxia. Neuroimaging shows vasogenic edema with microbleeds in the white matter and the corpus callosum. We herein report a case of HACE in which the patient showed widespread hyperintense signals with extensive microbleeds in the white matter and corpus callosum on MRI, as well as cognitive dysfunction. Rehabilitation to improve the higher brain function facilitated the recovery of the patient's cognitive impairment and was accompanied by improved MRI findings.
Keywords: high-altitude cerebral edema, mountain sickness, microbleeds, white matter high intensity, cognitive function
Introduction
Low atmospheric pressure causes low partial pressure of oxygen in the human body and may lead to difficulties in acclimatization to high-altitude areas. High-altitude cerebral edema (HACE) is a rare condition of acute mountain sickness that manifests as consciousness disturbance and truncal ataxia (1). Vasogenic edema causes these symptoms, and microbleeds in the white matter and corpus callosum are common MRI findings (2,3). Verbal and visual memory disturbances were observed in a patient with lesions in the splenium of the corpus callosum (4). Since HACE occurs under specific conditions, there are few studies that show its detailed clinical course and neuroimaging alterations. We herein report the case of a patient with HACE who had widespread hyperintense signals with extensive microbleeds in the white matter and cognitive dysfunction. Higher brain function rehabilitation facilitated the recovery of cognitive impairment and was accompanied with improvements in MRI findings.
Case Report
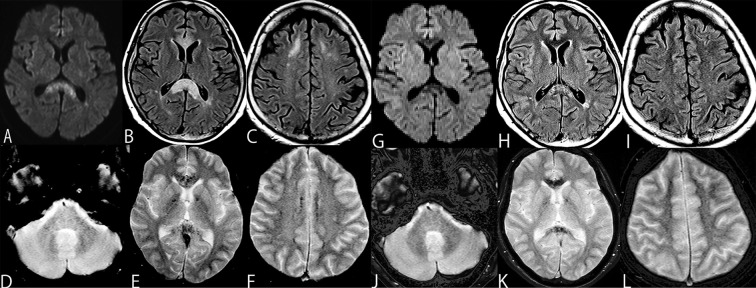
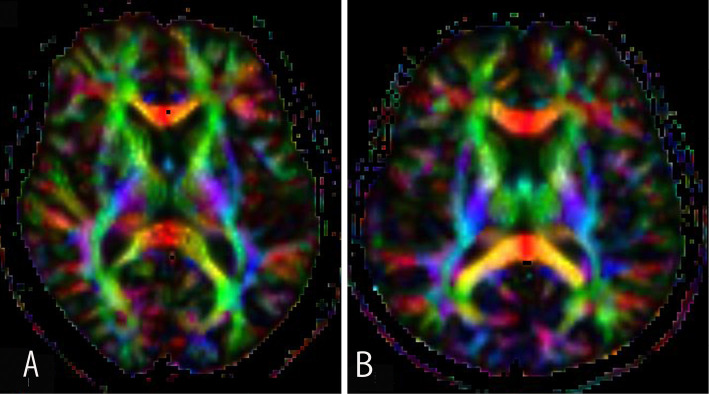
The patient was a 54-year-old woman who flew to Xining Caojiabao Airport in China (2,200 meters above sea level) to go sightseeing in Tibet (approximately 2,500-3,000 meters above sea level). After a 4-day stay in a hotel, she suddenly experienced nausea, vomiting, gait ataxia, and consciousness disturbance and was admitted to a local hospital (1,500 meters above sea level). At the time, her Glasgow Coma Scale was 14 (E3, V5, M6), with lethargy. Her memory and calculation acuity were normal. In addition, her cranial nerves, motor and sensory systems were also normal. Her blood pressure was 131/79 mmHg, and her heart rate was 76 beats/min. She had no fever and a physical examination revealed no abnormalities. Brain MRI DWI and FLAIR showed widespread areas of high intensity in the white matter of the centrum semiovale and the splenium of the corpus callosum. T2* imaging revealed extensive microbleeds, which were located symmetrically, anterior to the splenium of the corpus callosum, globus pallidus, widespread white matter in the centrum semiovale, and middle cerebral peduncle (Fig. 1A-F). There were no blood chemistry or cerebrospinal fluid abnormalities and cultures were negative. Her symptoms improved after hydration and rest, and she was able to walk. She was discharged from the hospital and returned home to Japan 7 days after the onset of symptoms. However, she experienced further memory disturbances and was admitted to hospital 12 days after a 4-day lucid interval. Although the results from physical and neurological examination were normal (e.g., normal reflexes in the extremities and a normal cerebellar function), attention disturbance as well as retrograde and antegrade amnesia were observed. Her Mini Mental State Examination (MMSE) score was 22 points, with slightly disturbed orientation, calculation, delayed recall and executive function. An examination using the Wechsler Adult Intelligence Scale 4th edition (WAIS IV) showed that her Full Scale IQ (FSIQ) was 82, her verbal comprehension index (VCI) was 106, her perceptional reasoning index (PRI) was 75, her working memory index (WMI) was 94, and her processing speed index (PSI) was 71. With the exception of her VCI value, her other index scores were low. She underwent rehabilitation to improve her calculation, auditory word comprehension, and concentration using card games and underwent memory training using complex figures. At 30 days after onset, her MMSE score recovered to 30. Her WAIS IV scores also improved: FSIQ 113, VCI 119, PRI 107, WMI 109. However, her PSI score remained at 87. An MRI examination 41 days after the onset showed the disappearance of high intensity lesions in the white matter and corpus callosum, except for the lesions in the splenium. The widespread and marked appearance of microbleeds had decreased; however, some microbleeds remained (Fig. 1G-L). Since the PSI index is associated with the executive function and information processing speed, the residual white matter and globus pallidus lesions delayed the recovery of PSI in comparison to other brain cortical function indexes (5,6). Diffusion tensor tractography at day 24 showed decreased commissural fibers in the corpus callosum (Fig. 2).
Figure 1.
MRI findings on the 12th day, DWI and FLAIR showed widespread areas of high intensity in the splenium of the corpus callosum (A, B) and white matter in the centrum semiovale (C). T2* revealed extensive microbleeds that were symmetrically located in the middle cerebral peduncle (D) and anterior to the splenium of the corpus callosum and globus pallidus (E), and the white matter in the centrum semiovale (F). At 41 days after the onset of symptoms, DWI and FLAIR showed improvement in the high intensity lesions in the corpus callosum and the splenium lesion (G, H), as well as the disappearance of the white matter lesions (I). The widespread and marked appearance of microbleeds was decreased; however, some microbleeds remained (J-L).
Figure 2.
Comparison of diffusion tensor tractography between our case (A) and an age- and sex- matched control (B). Simens Magnetome Avanto (1.5 T, TR/TE=7,000/102 ms, FOV=230×230 mm, matrix=128×128, b-value=1,000, diffusion direction=12); Fujifilm Synapse Vincent (Craniotomy Simulator/Tensor analysis V 5.3). Eye closed steady state without tasks. Image of the decreased commissural fibers in the corpus callosum on day 24. TR: time of repetition, TE: time of echo, FOV: field of view
Discussion
In the present case, prominent hyperintense signals with extensive microbleeds were observed in the corpus callosum and white matter. The pathophysiology of HACE is reversible, and vasogenic brain edema leads to microbleeds. The collapse of the blood brain barrier due to vasodilation with increased cerebral blood flow under low oxygen pressure and high-altitude erythrocytosis causes unique distributions and distinct MRI findings (7,8). These structures are anatomically classified as white matter, which is more vulnerable to vasogenic brain edema in comparison to gray matter. The blood supply of the splenium of the corpus callosum and middle cerebellar peduncle comprise the posterior circulation. Adrenergic regulation is weak in the posterior circulation vessels (7). Under these conditions, we found a severe case of HACE by MRI.
Hemorrhage in the globus pallidus due to CO intoxication and hypoxemia is often observed. The globus pallidus is a structure composed of gray matter that is located in the deep cerebrum; the end portion is perfused by a single artery system (9,10). These mechanisms may have caused the globus pallidus to be vulnerable to HACE in our case. The re-exacerbation of symptoms after a lucid interval is more likely to occur in pure hypoxia, such as is observed in patients with CO poisoning. Although delayed exacerbations are rare in high-altitude illness, a case with a one-month lucid interval was reported in a patient with acute mountain illness with bilateral globus pallidus lesions (11). Hypoxic factors and microbleed lesions in the bilateral globus pallidus may have been associated with the re-exacerbation of her symptoms.
Extensive microbleeds in subcortical U-fibers were another characteristic in our case. U-fibers are usually doubly supplied from the cortical and white matter vessels and are resistant to hypoxia (9,10). However, since these U-fiber structures consist of nerve fibers, they may be as vulnerable to vasogenic edema as the corpus callosum and the middle cerebellar peduncle.
Lesions in the splenium of the corpus callosum disrupt the connection between the anterior thalamic nucleus and hippocampus (Papez circuit) and cause visual and verbal memory disturbances (12). Our patient showed decreased visual and verbal IQ 12 days after the onset of symptoms; however, her scores returned to normal with rehabilitation. To our knowledge, this is the first report use the WAIS IV to show the improvement of visual and verbal memory impairment in the follow-up of a patient with HACE. Diffusion tensor tractography indicated that these extensive microbleeds corresponded to a decrease in nerve fibers. Observation studies regarding longitudinal improvement in PSI, retrograde amnesia and microbleeds are necessary to understand the course of HACE.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We are grateful to Dr. Luo Yang and Dr. Chen Jun in the First Hospital of Lanzhou University Department of Neurology for the referral forms.
References
- 1. Wilson MH, Newman S, Imray CH. The cerebral effects of ascent to high altitudes. Lancet Neurol 8: 175-191, 2009. [DOI] [PubMed] [Google Scholar]
- 2. Hackett PH, Yarnell PR, Hill R, Reynard K, Heit J, McCormick J. High-altitude cerebral edema evaluated with magnetic resonance imaging: clinical correlation and pathophysiology. JAMA 280: 1920-1925, 1998. [DOI] [PubMed] [Google Scholar]
- 3. Marussi VHR, Pedroso JL, Piccolo AM, et al. Teaching neuroimages: typical neuroimaging features in high-altitude cerebral edema. Neurology 89: e176-e177, 2017. [DOI] [PubMed] [Google Scholar]
- 4. Yanagawa Y, Madokoro S, Matsunami T, et al. Mountain sickness with delayed signal changes in the corpus callosum on magnetic resonance imaging: a case report. J Rural Med 14: 253-257, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cummings JL, Benson DF. Subcortical dementia: review of an emerging concept. Arch Neurol 41: 874-879, 1984. [DOI] [PubMed] [Google Scholar]
- 6. Black S, Gao F, Bilbao J. Understanding white matter disease: imaging-pathological correlations in vascular cognitive impairment. Stroke 40: S48-S52, 2009. [DOI] [PubMed] [Google Scholar]
- 7. Hackett PH. The cerebral etiology of high-altitude cerebral edema and acute mountain sickness. Wilderness Environ Med 10: 97-109, 1999. [DOI] [PubMed] [Google Scholar]
- 8. Tremblay JC, Hoiland RL, Howe CA, et al. Global REACH 2018 high blood viscosity and hemoglobin concentration contribute to reduced flow-mediated dilation in high-altitude excessive erythrocytosis. Hypertension 73: 1327-1335, 2019. [DOI] [PubMed] [Google Scholar]
- 9. Moody DM, Bell MA, Challa VR. Features of the cerebral vascular pattern that predict vulnerability to perfusion or oxygenation deficiency: an anatomic study. AJNR 11: 431-439, 1990. [PMC free article] [PubMed] [Google Scholar]
- 10. Chang KH, Han MH, Kim HS, Wie BA, Han MC. Delayed encephalopathy after acute carbon monoxide intoxication: MR imaging features and distribution of cerebral white matter lesions. Radiology 184: 117-122, 1992. [DOI] [PubMed] [Google Scholar]
- 11. Usui C, Inoue Y, Kimura M, et al. Irreversible subcortical dementia following high altitude illness. High Alt Med Biol 5: 77-81, 2004. [DOI] [PubMed] [Google Scholar]
- 12. Maeshima S, Osawa A, Yamane F, Yoshihara T, Kanazawa R, Ishihara S. Retrosplenial amnesia without topographic disorientation caused by a lesion in the nondominant hemisphere. J Stroke Cerebrovasc Dis 23: 441-445, 2014. [DOI] [PubMed] [Google Scholar]