Abstract
Protein glycation provides a biomarker in widespread clinical use, glycated hemoglobin HbA1c (A1C). It is a biomarker for diagnosis of diabetes and prediabetes and of medium-term glycemic control in patients with established diabetes. A1C is an early-stage glycation adduct of hemoglobin with glucose; a fructosamine derivative. Glucose is an amino group-directed glycating agent, modifying N-terminal and lysine sidechain amino groups. A similar fructosamine derivative of serum albumin, glycated albumin (GA), finds use as a biomarker of glycemic control, particularly where there is interference in use of A1C. Later stage adducts, advanced glycation endproducts (AGEs), are formed by the degradation of fructosamines and by the reaction of reactive dicarbonyl metabolites, such as methylglyoxal. Dicarbonyls are arginine-directed glycating agents forming mainly hydroimidazolone AGEs. Glucosepane and pentosidine, an intense fluorophore, are AGE covalent crosslinks. Cellular proteolysis of glycated proteins forms glycated amino acids, which are released into plasma and excreted in urine. Development of diagnostic algorithms by artificial intelligence machine learning is enhancing the applications of glycation biomarkers. Investigational glycation biomarkers are in development for: (i) healthy aging; (ii) risk prediction of vascular complications of diabetes; (iii) diagnosis of autism; and (iv) diagnosis and classification of early-stage arthritis. Protein glycation biomarkers are influenced by heritability, aging, decline in metabolic, vascular, renal and skeletal health, and other factors. They are applicable to populations of differing ethnicities, bridging the gap between genotype and phenotype. They are thereby likely to find continued and expanding clinical use, including in the current era of developing precision medicine, reporting on multiple pathogenic processes and supporting a precision medicine approach.
Keywords: Glycated hemoglobin, Fructosamine, Methylglyoxal, Diabetes, Chronic kidney disease, Machine learning
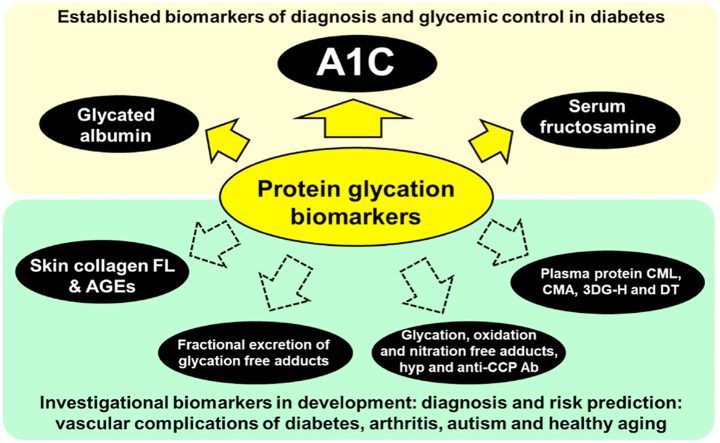
Graphical abstract
Highlights
-
•
Clinical glycation biomarkers are: A1C, glycated albumin and serum fructosamine.
-
•
Advanced glycation endproduct (AGE) biomarkers are in development.
-
•
Applications include: diabetes, diabetic complications, arthritis, autism and aging.
-
•
They are influenced by genetics, aging, glucose metabolism and other factors.
-
•
Applicable to all ethnicities, they bridge the gap between genotype and phenotype.
Abbreviations
- Ab
antibody
- A1C
glycated hemoglobin HbA1c
- ACE
angiotensin converting enzyme
- AGE
advanced glycation endproduct
- ARB
angiotensin receptor blocker
- ASD
autism spectrum disorder
- BMI
body mass index
- CAC
coronary artery calcification
- CCP
citrullinated cyclic peptide
- CEL
Nε-carboxyethyl-lysine
- CIMT
carotid intima-media thickness
- CKD
chronic kidney disease
- CMA
Nꞷ-carboxymethyl-arginine
- CML
Nε-carboxymethyl-lysine
- CVD
cardiovascular disease
- DCCT
Diabetes Control and Complications Trial
- 3DG-H
3-deoxyglucosone-derived hydroimidazolone
- DT
dityrosine
- EDRF
early decline in renal function
- ELOVL2
elongation of very long-chain fatty acids protein-2
- FADS
polymorphism of fatty acid desaturase
- FL
Nε-1-deoxyfructosyl-lysine
- FN3K
fructosamine 3-kinase
- G6PD
glucose-6-phosphate dehydrogenase
- GA
glycated albumin
- GCKR
glucokinase regulator
- GFR
glomerular filtration rate
- GG
glycosylation gap
- G-H1
glyoxal-derived hydroimidazolone
- Glo1
glyoxalase 1
- GSP
glucosepane
- GWAS
genome-wide association studies
- HDL
high density lipoprotein
- LC-MS/MS
liquid chromatography-tandem mass spectrometry
- LDL
low density lipoprotein
- LR
likelihood ratio
- MetSO
methionine sulfoxide
- MG
methylglyoxal
- MG-H1
methylglyoxal-derived hydroimidazolone
- NBT
nitroblue tetrazolium
- NFK
N-formylkynurenine
- 3-NT
3-nitrotyrosine
- OA
osteoarthritis
- PAD
peripheral artery disease
- PTC
renal proximal tubular epithelial cells
- SNP
single nucleotide polymorphism
- RA
rheumatoid arthritis
- ROS
reactive oxygen species
- T1DM
type 1 diabetes mellitus
- T2DM
type 2 diabetes mellitus
- TER
transcapillary escape rate
1. Introduction – protein glycation in the clinical setting
Protein glycation is the spontaneous, non-enzymatic reaction of proteins with simple reducing sugars and related metabolites. In the clinical setting, the major glycating agent is glucose which reacts with amino groups of N-terminal and lysine residues of proteins to form an initial Schiff's base, with following rearrangement to form N-(1-deoxy-D-fructos-1-yl)amino acids or fructosamines [1]. For lysine residues, the adduct is Nε-1-deoxyfructosyl-lysine (FL), with analytical surrogate, furosine [2] (Fig. 1a). Glycation of proteins by glucose to the fructosamine stage is classified as early glycation. In later stage reactions, fructosamine degrades to stable endstage adducts called advanced glycation endproducts (AGEs). Other important glycating agents are reactive α-oxoaldehyde metabolites, particularly methylglyoxal (MG), glyoxal and 3-deoxyglucosone. Dicarbonyls from mainly arginine-derived hydroimidazolone AGEs as the dominant product, typically accounting for >90% total glycation adducts formed [3,4]. Other minor glycation adducts include Nε-carboxymethyl-lysine (CML) and Nꞷ-carboxymethyl-arginine (CMA) formed from glyoxal, and Nε-carboxyethyl-lysine (CEL) from MG. Glucose and MG are precursors of major quantitative early-stage glycation adducts and AGEs, FL and hydroimidazolone MG-H1, respectively. The formation of AGEs, CML from FL and pentosidine from pentose precursors, involves oxidation and these processes are called glycoxidation (Fig. 1b). Glycation adducts are present as two major forms: glycation adduct residues of proteins – also called “protein-bound glycation adducts” and glycated amino acids or glycation free adducts. Cellular proteolysis forms glycation free adducts which are released into plasma and excreted in urine. There is also absorption of glycation free adducts and small glycated peptides from digestion of glycated proteins in food [5]. Processes of formation and metabolic transit of protein glycation are summarised schematically (Fig. 1c). Protein glycation occurs in the cellular and extracellular compartments. Glycated proteins are also ingested and those degraded to small glycated peptides and free adducts are absorbed in the portal vein. Albumin cycles from plasma into interstitial fluid, lymph and returns to plasma – with some leakage through renal glomeruli and return to venous circulation by the renal albumin retrieval pathway of proximal tubular epithelial cells (PTCs) [6]. The major route of excretion of glycation adducts is as free adducts in urine, with minor excretion in urinary albumin, other proteins and peptides. Glycation free adducts with molecular mass <500 Da pass readily through the glomerular filter into glomerular filtrate and are reabsorbed and secreted in the renal proximal tubules, likely by amino acid transporters, producing usually high and characteristic fractional excretions [7,8].
Fig. 1.
Protein glycation adducts (a. and b.)and formation, physiological processing and metabolic transit of glycated proteins(c.). Glycation adducts are shown as adduct residues with peptide bond linkage and ionization of glycation adducts at physiological pH, 7.4. For glycation free adducts, the peptide backbone N- and C-termini are –NH3+ and –CO2-, respectively. The square bracket round furosine indicates that it is an analytical surrogate (of FL), formed during acid hydrolysis in pre-analytic processing. Abbreviations: A1C, glycated hemoglobin HbA1c; PTC, proximal tubular epithelial cell; TER, transcapillary escape rate.
In this review, we describe the clinical diagnostic application of glycation adducts as biomarkers. Glycation adducts may be biomarkers used for diagnosis, risk of developing a health disorder or disease and monitoring of the response to treatment. The steady-state levels of glycation adduct residues of proteins reflect the rates of formation, degradation and repair of the glycated protein in the compartments where the protein substrate is located [9]. Glycation adducts provide reports on different aspects of metabolism [9] (Table 1). The levels of glycation free adducts in plasma reflects the balance between fluxes of free adducts released into the vasculature from tissues (including absorption from digested food in the portal vein) and renal clearance [10], increasing profoundly in experimental nephrectomy and clinical renal failure [7,11]. The urinary flux of glycation free adducts reflects the total body flux of formation of glycation adducts with a contribution from glycation free adducts absorbed from food [7,11,12]. Factors affecting the level of glycated protein biomarker are: concentration of the protein substrate, concentration of the glycating agent and duration of exposure to it, and turnover and repair and replacement of the glycated protein [5]. Other non-glycation based physiological factors provide interferences in biomarker reporting of physiological glycation [13]. Robust measurement of glycation adducts in the clinical chemistry laboratory has been challenging which recent advances in application of stable isotopic dilution analysis LC-MS/MS have overcome [9,14]. The strength and weakness of different analytical methods and overview of steps in development and validation for clinical use are summarised in Table 2. With optimized methodologies and protocols now available, protein glycation provides unique and valuable clinical and investigational biomarkers.
Table 1.
Biomarker characteristics of protein glycation adducts.
| Glycation adduct | Reporter feature (precursor) | Comment |
|---|---|---|
| FLa | Glycemic control (glucose) | Major early-stage glycation adduct. Repaired intracellularly by fructosamine 3-phosphokinase [24]. Free adduct absorbed after digestion of food proteins [121]. |
| MG-H1 | Dicarbonyl stress (methylglyoxal) | Major AGE. Linked to increased fasting and postprandial glucose exposure, unscheduled glycolysis, insulin resistance and cardiovascular disease [4,12,90,119,122]. Free adduct absorbed after digestion of food proteins [12]. Good stability in samples with delayed processing for epidemiological studies [73] |
| CML | Glycoxidation glycemic control/(FL and others) | Major AGE. Formed by the oxidative degradation of FL and other sources. CML/FL ratio is an indicator of oxidative stress [123]. Free adduct absorbed after digestion of food proteins [124]. |
| GSP | Glycemic control/glycation crosslinking (FL) | Major glycation crosslink [75]. Major glycation adduct released from joint proteins during early-stage development of osteoarthritis [116]. Good stability in samples with delayed processing for epidemiological studies [73]. |
| Pentosidine | Pentosephosphate pathway activity (pentose metabolite) | Low level pentose sugar-derived glycation crosslink and intense fluorophore. Considered to reflect pentosephosphate pathway activity [125]. Skin collagen pentosidine accounts for 30% variation in SAF [126] |
| Pyrraline | AGE exposure from food (cooked food) | Glucose-derived AGE formed at high temperatures of culinary processing; originating only from food [127,128]. Urinary pyrraline excretion is linked to amount of AGE absorbed from food [12]. |
Also applies to N-(1-deoxy-D-fructos-1-yl)amino acids (fructosamine). Abbreviation: SAF, skin autofluorescence.
Table 2.
Major analytical methodologies for glycation biomarkers in clinical practice and research. Steps to clinical translation.
| MAJOR ANALYTICAL METHODOLOGIES | |||
|---|---|---|---|
| Glycation analyte | Analytical methodology | Comment | Reference |
| Clinical practice application | |||
| Glycated hemoglobin HbA1c | Immunoassay (recognizing glycated N-terminus of β-chain). | Rapid and high sample throughput. Automated in clinical chemistry analyzers. | [129] |
| Cation exchange chromatography with absorbance spectrophotometric detection | Moderate sample throughput. Automated in clinical chemistry analyzers. Interference from rare hemoglobin variants. | [130] | |
| Glycated hemoglobin HbA1 | Boronate affinity chromatography with absorbance spectrophotometric detection | Moderate sample throughput. Measures sum of HbA1a, HbA1b and HbA1c. Automated in clinical chemistry analyzers. Minimal interference from hemoglobin variants. | [131] |
| Glycated albumin | Enzymatic chromogenic assay (ketoamine oxidase/peroxidase) | Moderate sample throughput. Requires prior processing of glycated amino acids followed by proteolytic digestion. | [132] |
| Glycated albumin | Boronate affinity chromatography with absorbance spectrophotometric detection | Moderate throughput. Measures percentage albumin with fructosamine residues | [133] |
| Serum fructosamine | Absorbance spectrophotometry | Rapid and high sample throughput. Automated in clinical chemistry analyzers. Interferences: hemoglobin, bilirubin, glutathione, cysteine. | [63,134] |
| Research application | |||
| All glycation analytes | Stable isotopic dilution analysis LC-MS/MS | Reference method. Moderate throughput. Multiplexing at minimal additional cost and without interference. Prior enzymatic hydrolysis for glycated proteins. Not yet fully automated. Limited commercial availability of analytical standards. | [9,14,96] |
| All glycation analytes | Immunoassay | High throughput. Different response for glycation adduct residues of proteins and glycation free adducts, requiring separation in pre-analytic processing. Often incomplete characterization of epitope specificity and calibration standards. Masked epitopes and other sample matrix effects. Interference from analyte in blocking proteins – advise use of polythreonine. Expensive to multiplex and risk of interference. Limited commercial availability of specific antibodies other than for CML. Preferably corroborated by LC-M/MS. | [92,[135], [136], [137]] |
| Fluorescent AGEs | HPLC with fluorimetric detection | Medium throughput. Prior enzymatic hydrolysis for glycated proteins. Limited commercial availability of calibration standards. Can be run in-line with LC-MS/MS. | [9,14,96] |
| Fluorimetry: excitation 350 nm, emission 440 nm “AGE fluorescence”. | Multiple fluorophores. Interference from non-AGE fluorophores. Excitation 328 nm, emission 378 nm wavelengths have also been used. | [[68], [138]] | |
| STEPS TO CLINICAL TRANSLATION OF PROTEIN GLYCATION BIOMARKERS – including application of machine learning to develop classifier algorithms. | |
|---|---|
| Step | Requirements |
| 1. Analytical method development and standard operating procedure. | Analytical sensitivity and specificity – including investigation of interferences; linearity and dynamic range; internal and calibration standards; limits of detection and quantification; intrabath and interbatch coefficients of variation; conditions for clinical sample collection, storage and pre-analytic processing; protocol for data analysis and quality control. |
| 2. Application to clinical studies. | Determine reference interval in control study group. |
| 3. Development of classifier algorithms. | Assay protein glycation biomarkers in case and control study groups, with power analysis for appropriate sample number.a Train and test algorithms with analytical data from independent subject groups, optimizing for accuracy of case and control classification. |
| 4. Further validation studies. | Applicability to subjects of different age, gender, ethnicity and effect of co-morbidities and treatment. Algorithms for diagnosis, risk of severity progression and response to therapy of a health disorder or disease. |
An introduction to power analysis in clinical diagnostics was given by Xia et al. [139].
2. Glycated hemoglobin A1C
Glycated hemoglobin, HbA1c or A1C, is widely used for the diagnosis and monitoring of glycemic control of diabetes, in both patients with type 1 diabetes mellitus (T1DM) and patients with type 2 diabetes mellitus (T2DM). Current guidelines advise A1C is measured at least biannually in patients with diabetes [15]. A1C is also used for the diagnosis of prediabetes – a condition that precedes development of T2DM [16]. It is formed by the reaction of glucose with unglycated hemoglobin, HbA0. The major adduct formed is the fructosamine derivative of the N-terminal valine residue of the beta-chain, ßval-1, with also glucose modification at αlys-61 and βlys-66 [[17], [18], [19]]. There are other minor forms of glycated hemoglobin resolved from A1C in conventional cation exchange chromatography analysis used in clinical chemistry, representing <1% total Hb: HbA1a1, HbA1a2 and HbA1b, which are ßval-1 adducts of fructose-1,6-bisphosphate, glucose-6-phosphate and pyruvate, respectively, and HbA1d (aldimine Schiff's base) and HbA1e (fructosamine adduct of αval-1) [[20], [21], [22]]. The steady-state level of A1C in vivo is influenced by deglycation of glycation adducts by fructosamine 3-kinase (FN3K) [23,24], red blood cell lifespan (mean 120 days) and glycemic control over the previous 90–120 days [25]. A1C is a weighted measure of mean blood glucose concentration during the 120 days prior to measurement; blood glucose levels in the 30 days immediately prior to blood sampling contribute approximately 50%, whereas levels in prior 90–120 contribute only 10% [[26], [27], [28]]. A1C is a valuable biomarker of medium-term glycemic control, with the disadvantage that intervention trials to improve dysglycemia in prediabetes and hyperglycemia in diabetes must be at least 3 months duration for responsiveness of A1C [29]. The validity of A1C as a biomarker of glycemic control is impaired when non-glycemic factors influence levels: such as impaired red blood cell synthesis in renal failure [30], unstable hemoglobin variants [31] and dysregulated iron and red blood cell metabolism [32] – including in pregnancy [33]. Good control of hyperglycemia is important in the clinical care of patients with diabetes which, together with control of blood pressure and lipids, decreases the risk of developing debilitating vascular complications of diabetes: diabetic nephropathy, diabetic retinopathy, diabetic neuropathy and increased risk of cardiovascular disease (CVD). As a biomarker of glycemic control, A1C is considered a modifiable risk factor for the chronic vascular complications of diabetes. Decrease of A1C by intensive treatment with hypoglycemic drugs is associated with decreased risk of development of diabetic microvascular complications [[34], [35], [36]] and decreased progression of CVD in patients with T1DM [37,38] (Table 3). A1C was also associated with all-cause mortality in non-diabetic and diabetic subjects [39].
Table 3.
Glycated proteins and free adducts as clinical biomarkers.
| Health decline or disease (Type of biomarker) | Glycation analyte (adduct) | Diagnostic indication and biomarker characteristics | Reference |
|---|---|---|---|
| Proteins with early-stage glycation by glucose | |||
| Diabetes and prediabetes (Diagnostic biomarker and therapeutic monitoring - glycemic control) | Glycated hemoglobin A1C (fructosamine) | Diagnosis: normal, A1C <5.7% (<39 mmol/mol); prediabetes, A1C 5.7–6.4% (39–47 mmol/mol); diabetes, A1C ≥ 6.5% (≥48 mmol/mol). Therapeutic monitoring (glycemic control): good, <7% (53 mmol/mol); moderate, <8% (53 mmol/mol); poor, ≥8% (53 mmol/mol). In widespread clinical use. | [15,16,19] |
| Glycated albumin (fructosamine) | Diagnosis: normal glycemia 11–16%. In widespread clinical use, particularly where there are interferences in use of A1C. Likely interference from change in albumin synthesis, catabolism, TER and glomerular filtration. | [42,140] | |
| Microvascular and macrovascular complications of diabetes (Risk predictor) | Glycated skin collagen (fructosamine) | Risk prediction: increased furosine linked to worsening of diabetic retinopathy, nephropathy and neuropathy and increased CAC and left ventricular mass/end diastolic volume ratio. | [71,72] |
| Cardiovascular disease (Risk predictor) | LDL (fructosamine) | Apolipoprotein B100 major protein; half-life 3 days. Glycated in 6 domains. Difficult to quantify at all sites. May be risk predictor of myocardial infarction and surrogate of small dense LDL | [[141], [142], [143], [144], [145]] |
| HDL (fructosamine) | Apolipoprotein A-1 major protein; half-life 3.3 days. 3–5% glycation; sites - lys-12, lys-96, lys-133, lys-205 and lys-239 Difficult to quantify. May be surrogate marker of HDL instability | [91,[146], [147], [148]] | |
| Advanced glycation endproducts-modified proteins | |||
| Healthy aging (Diagnostic marker) | Plasma protein (GSP) | Correlates positively with age. | [73] |
| Skin collagen (CML, CEL, GSP, MG-H1, pentosidine) | AGEs increase with donor age. May be linked to skin aging and age-linked decline in glucose tolerance and dysglycemia | [68,74] | |
| Diabetes (Diagnostic marker; glycemic control) | Plasma protein (CML, GSP) | CML correlated positively with A1C and mean 24 h plasma glucose. Plasma protein GSP increased with T2DM. | [4,73] |
| Microvascular and macrovascular complications of diabetes (Risk predictor) | Plasma protein (CML, CEL and pentosidine) | T1DM: Increased plasma protein AGEs associated with increased risk of CVD and all-cause mortality. T2DM: inverse link to PAD. | [80,83] |
| Skin collagen (CML, CEL, G-H1, GSP MG-H1 and pentosidine) | Predicted risk of diabetic retinopathy, diabetic neuropathy and increased risk of CVD (CIMT, increased left ventricular mass, and increased LV mass/end diastolic volume ratio). | [71,72[71,72] | |
| CKD (Risk predictor) | Plasma protein and free adduct (pentosidine) | Risk predictor of all-cause mortality. | [87] |
| CVD (Risk predictor) | Plasma protein (MG-H1) | Increased mortality in nondiabetic women | [90] |
| Glycation endproduct free adducts | |||
| Chronic kidney disease (Risk predictor) | Fractional excretion of free adducts (FL, CML, CEL MG-H1, CMA and Pentosidine) |
Fractional excretion of glycation free adduct is increased in patients with diabetes at high risk of EDRF, supporting a precision medicine approach. | [8] |
| Plasma free adducts (CML, CEL and MG-H1) | Logistic regression model for progression of diabetic kidney disease | [106] | |
There is a strong genetic influence of A1C. Genes influencing A1C are in metabolic pathways influencing glycemic status, red blood cells and others – including FN3K which catalyzes the deglycation of glycated hemoglobin [23,32]. In non-diabetic subjects, 62% of population variation in A1C is explained by genetics and the remainder is attributable to the influence of environment (23%) and age (14%). Genetic influence of A1C also extended in patients with diabetes [40]. A1C may underestimate the glycemic status of subjects with sickle cell anemia and patients with renal failure on dialysis [30,31] (Table 4).
Table 4.
Influence of genetics on protein glycation.
| Glycated protein(s) | Type of study | Observation | Reference |
|---|---|---|---|
| Glycated hemoglobin A1C | Twin study (non-diabetic subjects) | Population variation: 62% genetics; 23% environment; 14% age. Genetic influence extended to patients with T1DM. | [40] |
| GWAS study (non-diabetic subjects) | 60 loci influencing A1C, explaining 4%–14% of the trait variance: 19 genes of glycemic status, 22 genes of red blood cell pathways, 19 genes unclassified. | [32] | |
| Glycated albumin GA | First degree relatives and GWAS (non-diabetic subjects) | Population variation: 48% genetics. Associated SNP: GCKR - SNPs identified accounted for 3.2% of the variation. | [44,45] |
| Glycation gap (GG) | Twin study (non-diabetic subjects) | Population variation: 69% genetics; 31% environment. Twenty percent heritability of A1C was common to GG. | [149] |
| Serum protein CML | Twin study (non-diabetic subjects) | Population variation: 74% genetics. | [150] |
3. Glycated albumin and serum fructosamine
Glycation of serum albumin by glucose produces glycated albumin (GA) which is also a clinical biomarker of glycemic control. It is increasingly preferred where interferences in A1C apply – see above. The major sites of glycation are, in order of reactivity: asp-1, lys-525, lys-199 and lys-439 [41]. The extent of albumin glycation in healthy human subjects is 11–16%, increasing 2–3 fold in patients with diabetes [42]. Albumin has a half-life of ca. 20 days, and provides a report on glucose control over 14–20 days prior to blood sampling [43]. GA shows 48% genetic influence in population variation [44,45] (Table 3, Table 4).
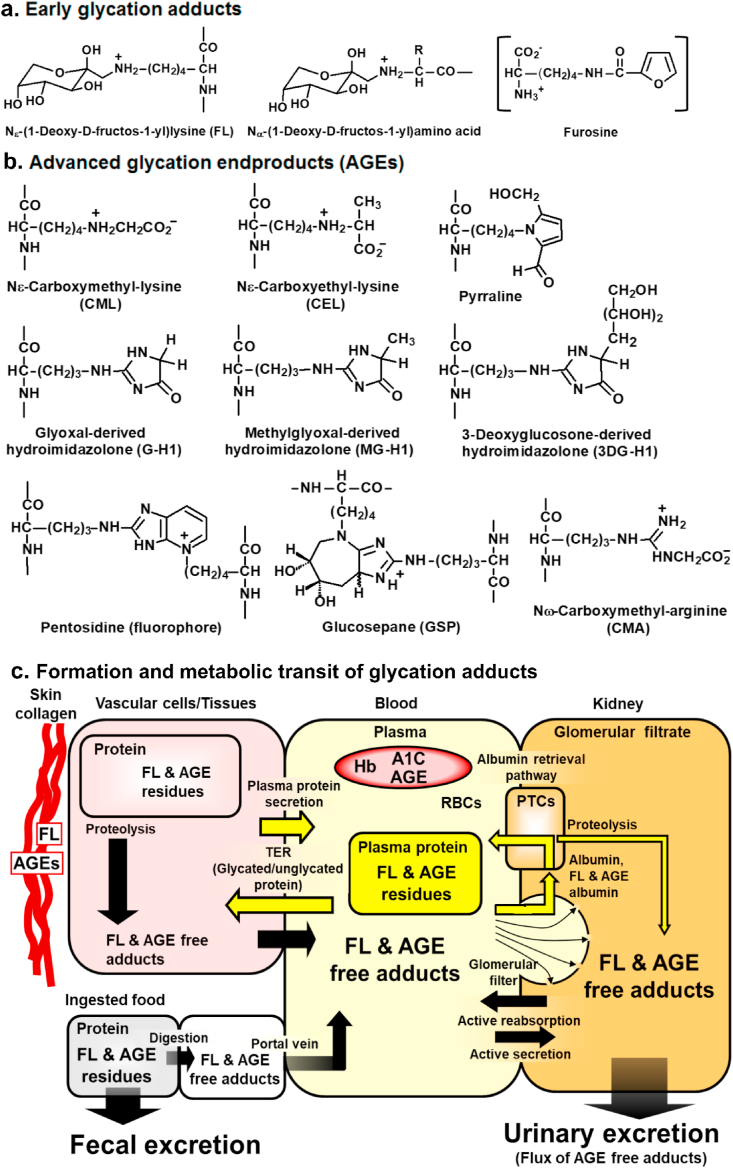
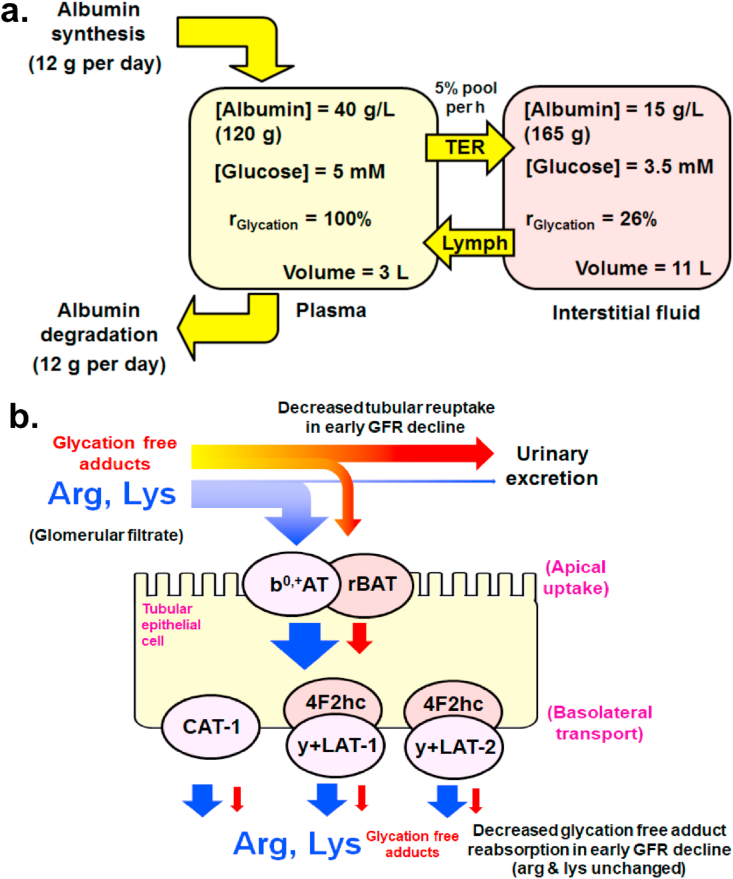
Albumin is secreted into plasma by the liver. It leaks from the vascular into interstitial fluid at 5% of total plasma pool per h – the albumin transcapillary escape rate (TER). It returns to plasma via lymph. Albumin leaking through renal glomeruli is returned to the venous circulation by the renal albumin retrieval pathway where GA may be preferentially excreted [6,46,47] (Fig. 1c). Given the decreased concentrations of albumin and glucose in the interstitial fluid compared to plasma, the rate of glycation of albumin by glucose is ca. 4-fold lower in the interstitial fluid compared to plasma (Fig. 2a) [48]. Change in albumin TER in hypertension, obesity, diabetes, acute inflammatory disease and peripheral artery disease (PAD) may provide an interference in use of GA as a biomarker of glycemic control [[49], [50], [51], [52], [53], [54]]. Decreased synthesis, plasma concentration and catabolism of albumin in patients with cirrhosis likely explains the 2-fold increase of GA without change in glycemic status [10,46]. It was initially proposed from experimental studies that AGE-modified albumin is extracted from plasma by the liver [55]. Clinical studies of levels of endogenous AGE-modified albumin in hepatic artery, portal vein and hepatic vein did not support this [10]. Albumin ligands used in experimental studies had high, supraphysiological extents of glycation and abnormally high increased net negative charge which bind hepatic scavenger receptors for cellular uptake [[55], [56], [57]]. Endogenous AGE-modified albumin clinically or albumin modified by AGEs in vitro to physiological extent showed no binding of the scavenger receptor and limited extraction in the liver [10,58,59]. The cellular uptake and proteolysis of FL- and AGE-modified albumin is rather proposed to occur in multiple tissues, similar to that of unglycated albumin [10]. Recent studies suggest glycated proteins are directed for cellular proteolysis by the unfolded protein response [60,61].
Fig. 2.
Compartmentalization of albumin glycation in plasma and interstitial fluid and impaired renal tubular reuptake of glycation free adducts in early-stage diabetic kidney disease. a. Glycation of albumin by glucose – glycation kinetics and dynamics in vascular and extravascular compartments. Physiological data from Refs. [6,152]. Relative glycation kinetics deduced from: rGlycation = k [Glucose][albumin], k is the glycation rate constant and assuming rGlycation in the plasma compartment = 100%. Albumin TER is increased (5.6–7.6% per h) and plasma volume decreases by up to 10% in hypertension and overweight/obese subjects with metabolic syndrome; obesity increases total body interstitial fluid volume [49,50,153]. b. Schematic diagram of amino acid transporters of arginine and lysine uptake in the renal tubular epithelium and engagement with glycation free adducts. Renal proximal tubular reuptake by low affinity binding to cation transporter proteins: heterodimeric complex b0,+AT/rBAT on the apical surface (gene names SLC7A9 and SLC3A1, respectively) and high affinity cationic amino acid transporter 1 (CAT-1) and heterodimeric complexes of y + LAT1, y + LAT2 with 4F2hc on the basolateral surface (gene names SLC7A1, SLC7A7, SLC7A6 and SLC3A2, respectively) [[99], [100], [101], [102], [103]]. Reproduced from Refs. [8,48] with permission. Abbreviations: GRF, glomerular filtration rate; TER, transcapillary escape rate.
A further interference is through effects of renoprotective drug treatment on leakage of albumin through the renal glomerular filter (Fig. 1c). Patients with early-stage diabetic nephropathy, microalbuminuria, are treated with angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs). This decreases the size of the pores of the renal glomeruli filter, decreasing leakage of albumin and particularly GA into the glomerular filtrate. Treatment with ARB, Irbesartan, increased in GA by 66–72% without change in A1C [62].
A glycation biomarker related to GA is serum fructosamine – a measure of total serum protein glycation by glucose. It is determined as the rate of reduction of serum protein using nitroblue tetrazolium (NBT) at pH 10.8 [63], reports on glycemic control over 10–14 days prior to sampling [43] and likely has similar interferences to GA. The concentration of serum fructosamine in healthy human subjects was 230 ± 26 μM [64] but the absolute calibration is challenging; different fructosamines reducing NBT at different rates [63,65]. Measurement of serum fructosamines or “Fructosamine test” is low cost and in widespread clinical use.
Both serum fructosamine and GA correlate positively with A1C [64]. Cohen et al. introduced a derivative variable called the glycosylation gap (GG) which is the difference between measured A1C and A1C predicted from the fructosamine based on the A1C-fructosamine regression equation [66]. GG may predict progression of diabetic nephropathy [67]. From the above considerations, increased albumin TER and renoprotective drug treatment may produce negative and positive GGs, respectively [48,62]. GG also has strong genetic influence (Table 4).
4. Glycated skin collagen and other fructosamine-modified proteins
FL residue content of skin collagen increases with age of healthy subjects, increasing ca. 45% from 20 to 80 years of age [68]. This may reflect age-dependent decrease of glucose tolerance [69]. There was no age-dependent link to skin collagen FL in patients with T1DM, although levels correlated positively with A1C and were decreased with therapeutic improvement of glycemic control [68,70]. In patients with T1DM of the Diabetes Control and Complications Trial (DCCT), increased skin collagen furosine was associated with worsening of diabetic retinopathy, nephropathy and neuropathy [71]. A similar study explored association with measures of subclinical CVD, finding furosine predicted future increased coronary artery calcification (CAC) and change of left ventricular mass/end diastolic volume ratio [72]. This may reflect the progression of CVD with increased hyperglycemia [37,38].
Other fructosamine-modified proteins studied are glycated low density lipoprotein (LDL) and high density lipoprotein (HDL). They are investigational risk predictors of atherosclerosis and coronary heart disease (Table 3).
5. Proteins modified by advanced glycation endproducts
Proteins modified by AGEs are currently investigational clinical biomarkers, typically measured in plasma protein and skin collagen. In a validation study for application to epidemiological investigations, plasma protein GSP and MG-H1 showed the highest reliability in replicate samples and greatest stability with delayed processing and storage [73].
In healthy subjects, plasma protein GSP correlated positively with subject age [73]. In skin collagen, CML, CEL, MG-H1, GSP, pentosidine and “AGE fluorescence” (excitation 328 nm, emission 378 nm) correlated positively with age in healthy subjects [68,74]. GSP is a stable degradation product of FL and may provide an improved cumulative measure of glucose exposure and dysglycemia, relative to FL [75]. It is the major glycation crosslink in skin collagen and may contribute to age-related impairment of elastic properties in skin [76]. MG-H1 has a half-life of only 12 days under physiological conditions so its increase with age is likely reflecting exposure to increased MG or dicarbonyl stress with age [77,78].
In patients with T1DM, plasma protein CML correlated positively with A1C and mean 24 h plasma glucose, consistent with glycemic control biomarker FL being often the major precursor of CML [4]. Increased plasma protein CML and CEL were positively associated with arterial pulse pressure [79], increased CML, CEL and pentosidine were associated with increased risk of CVD and all-cause mortality [80] but CML and other AGEs were not linked to the risk of developing diabetic nephropathy [81,82]. In skin collagen, glycation-related analytes including CML, CEL, G-H1, GSP, MG-H1 and pentosidine were risk predictors of progression of retinopathy and neuropathy but not nephropathy, with GSP and MG-H1 major contributors [71]; and CML, MG-H1, GSP and pentosidine also predictors of surrogate clinical endpoints of CVD [72].
In patients with T2DM, an increased AGE score computed from plasma protein CML, CEL and pentosidine was inversely linked to BMI, risk of PAD and GFR [62,83]. These associations may be due to increased albumin TER in obesity and PAD and increased loss of AGE-modified albumin through the glomerular filter with increased GFR [50,54]. Increased MG-H1 residue content of serum protein was associated with diabetic retinopathy in patients with T2DM [84]. Plasma protein CML was inversely associated with BMI in a large cohort of obese and insulin resistance subjects – some with T2DM [85], which may be due to increased albumin TER in obesity and insulin resistance [[50], [51], [52]] (Table 3).
Protein glycation biomarkers in CKD were recently reviewed elsewhere [86]. Total plasma pentosidine (protein-bound + free adduct), was a risk predictor of mortality in CKD after adjusting for all confounders [87] and may be reporting increased pentosephosphate pathway activity in response to oxidative stress induced by rapid decline in renal function and associated increased mortality [8]. CML residue contents of plasma protein was investigated as a biomarker of mortality risk in renal failure in patients receiving hemodialysis therapy in two studies with contrary outcomes [88,89]. Whilst formation of AGEs likely has a role in the etiology of renal disease [86], there is interference in application of plasma protein glycation biomarkers from changes in albumin synthesis and protein loss in dialysis.
For CVD, plasma protein MG-H1 was associated with increased mortality in nondiabetic women [90]. These observations suggest dicarbonyl stress may have a key role in CVD, particularly through formation of MG-modified small, dense LDL and MG modified HDL with decreased stability and half-life in pro-atherogenic dyslipidemia [91,92]. Supporting this, a genome wide association study found expression of glyoxalase 1 (Glo1) which metabolizes MG was negatively linked to risk of coronary heart disease [93]. Increased plasma protein CML and pentosidine were associated with poor diastolic and systolic heart function [94], which may be due to interference of decreased albumin TER [95].
6. Glycation free adducts
Assay of glycation free adducts requires minimal pre-analytic processing and is robust with short analysis time using stable isotopic dilution analysis LC-MS/MS [9,14]. Increased glycation free adducts in plasma and urine may be biomarkers of increased exposure to protein glycation and/or increased proteolysis of long-lived extracellular matrix proteins that have accumulated long-lived, chemically stable glycation adducts throughout life [96]. Recent studies suggest renal handling of glycation free adducts provides a very sensitive measure of patients who develop rapid loss of renal function or “early decline in renal function” (EDRF).
Diabetic kidney disease (DKD) occurs in about 40% patients with diabetes [97]. In a subset of patients with EDRF, renal function declines rapidly such that after 5–20 years, patients require renal dialysis and with median survival thereafter of only 3 years. During renal function decline, there is also a progressive increase in risk of fatal CVD, 3 to 20-fold higher than the healthy population. It is estimated that 19% patients with T1DM and 28% patients with T2DM develop EDRF [98]. Improved treatment and care could be provided if patients at risk of future development of EDRF could be identified. In an investigation of glycation free adducts in plasma and urine of patients with T1DM, with and without future development of EDRF (assessed during 12 years of follow-up), we found urinary excretion of pentosidine was increased in patients with EDRF, compared to patients with stable renal function. Remarkably, fractional excretions of 6 lysine and arginine-derived glycation free adducts were higher in patients with EDRF, compared to patients with stable renal function. Lysine and arginine-derived glycation free adducts are thought to be taken up and moved across the renal tubular epithelium by low affinity binding to cation transporter proteins which also take up arginine and lysine. These are: heterodimeric complex b0,+AT/rBAT on the apical surface and CAT-1 and heterodimeric complexes of y + LAT1, y + LAT2 with 4F2hc on the basolateral surface [[99], [100], [101], [102], [103]]. Interestingly, in genome-wide association studies genetic polymorphism of y + LAT1, y + LAT2, b0,+AT (genes SLC7A7, SLC7A6, and SLC7A9) was associated with variation in eGFR and development of CKD [104,105]. Impaired tubular reuptake of glycation free adducts by lysine and arginine transporter proteins in patients with EDRF is likely involved (Fig. 2b). Increased fractional excretions of glycation adducts are potential risk predictors for EDRF in diabetes and possibly progression of non-diabetic CKD [8]. In an alternative approach, a logistic regression model indicated that plasma concentrations of CML, CEL and MG-H1 free adducts, but not A1C, were linked to progression of diabetic kidney disease in patients with T1DM, assessed by thickening of the renal glomerular basement membrane [106] (Table 3).
7. Application of artificial intelligence machine learning for the development of diagnostic algorithms with protein glycation features
Combination of multiple measurements as features in trained and tested algorithms is a recently developed strategy to improve clinical diagnostic performance of glycation adduct biomarkers. Plasma protein content of AGEs, CML, CMA, 3-deoxyglucosone-derived hydroimidazolone (3DG-H) and oxidative damage marker, dityrosine (DT), provided features in a diagnostic algorithm for autism spectrum disorder (ASD) or autism [101]. Autism is a developmental disorder of childhood that affects 12 million people worldwide with a global prevalence of 0.62% [107], with higher prevalence in the USA (2.47%) [108] and Europe (1.15%) [109]. Plasma protein contents of CML, CMA and DT were higher and plasma protein content of 3DG-H lower in children with ASD, compared to children with normal development. A diagnostic algorithm combining these analytes gave a test with 88% accuracy. An important indicator of diagnostic performance is positive likelihood ratio LR+, which is the ratio of subjects with a positive test who have a health disorder or disease, compared to number of subjects with a positive test who do not. Similarly, negative likelihood ratio LR− is the ratio of subjects with a negative test who have a health disorder or disease, compared to number of subjects with a negative test who do not. LR+ >10 and LR− <0.1 is considered strong, often conclusive evidence for positive and negative diagnosis, respectively; and LR+ of 5–10 and LR− of 0.1–0.2 provides moderate evidence of positive and negative diagnosis, respectively [110]. For the autism blood test, LR+ = 5.7 and LR− = 0.095, suggesting moderate and strong, often conclusive evidence of presence and absence of ASD, respectively [101]. Regarding algorithm features, increased CML and CMA residues in plasma protein may reflect increased plasma protein glycation by glyoxal, sourced mainly from lipid peroxidation [14]. Recent studies have associated genetic polymorphism of fatty acid desaturase (FADS) 1/2 and elongation of very long-chain fatty acids protein-2 (ELOVL2) with risk of ASD [111]. This may indicate a disturbance of long chain polyunsaturated fatty acid metabolism with increased lipid peroxidation in ASD. DT residue content of plasma proteins, a marker of protein oxidative damage, was increased in subjects with ASD whereas other oxidative damage markers were not. DT residue formation occurs by reaction of tyrosine residues in proteins with ROS and dual oxidase DUOX [112]. DUOX has an important role in gut mucosal immunity, host–microbe homeostasis and signaling for neutrophil recruitment into allergic airways [113]. Gut microbiota may be influential in development of the behavioral phenotype in ASD [114]. Decrease of 3DG-H content of plasma protein in subjects with ASD may reflect decreased concentration of plasma 3-DG due to increased 3-DG reductase activity, as discussed [101]. With further validation, this may provide the basis of a simple blood test for autism diagnosis. This is an example of combination of biomarkers of protein glycation and oxidative damage.
Application of glycation free adducts for clinical diagnosis is best developed for diagnosis and classification of early-stage arthritis. Protein glycation and oxidative damage accumulates in articular cartilage with age [[115], [116], [117]]. From the earliest stages, pathogenesis of arthritis involves increased proteolysis of articular cartilage. There are three main types of arthritis clinically: osteoarthritis (OA), rheumatoid arthritis (RA) and other inflammatory joint disease which is often self-resolving (non-RA). Arthritis type is often difficult to discern at the early stages. Early-stage detection may enable effective treatment of RA with disease-modifying anti-arthritic drugs and OA with beneficial lifestyle and therapeutic interventions. Early-stage arthritis was detected and type assigned with diagnostic algorithms based on features of plasma glycation, oxidation and nitration free adducts in combination with hydroxyproline. LR+ and LR− for early-stage diagnosis was 10.2 and 0.09 respectively, indicating conclusive evidence for presence or absence of early-stage arthritis (any type). The type of arthritis could also be discerned where anti-citrullinated cyclic peptide (CCP) antibody positivity status was a feature [118]. This illustrates how combination of protein glycation, oxidative and nitration damage markers with the bone resorption biomarker, hyp, and anti-CCP antibody status – a clinical RA-biomarker requiring refinement, may provide high performance diagnosis.
A urinary health screen with age, BMI, FL free adduct and valine as features was also recently developed providing moderate, weak and strong evidence for early-stage decline in metabolic, vascular and renal health respectively (Table 5).
Table 5.
Application of artificial intelligence machine learning for the development of diagnostic algorithms involved glycation adducts.
| Disorder or disease (Type of biomarker) | Analytes (adduct) | Diagnostic indication | Reference |
|---|---|---|---|
| Autism spectrum disorder (Diagnostic marker) | Glycated plasma protein (CML, CMA, 3DG-H and DT) | Combined in a diagnostic algorithm, gave moderate evidence for presence and borderline moderate/conclusive evidence for absence of ASD; LR+ = 5.7, LR− = 0.095. | [101] |
| Early-stage arthritis (Diagnosis marker) | Plasma free adducts (FL, CML, CEL, G-H1, MG-H1, 3DG-H, CEL, CMA, GSP, pentosidine; and MetSO, DT, NFK, 3-NT; and hyp and anti-CCP antibody status) | Diagnostic algorithm for early-stage arthritis (any type) vs good skeletal health: LR+ = 8.3 and LR− = 0.11. Diagnostic algorithm for classification of early-stage arthritis type (OA, RA or non-RA): for OA, RA and non-RA, LR+ = 16.1, 7.7 and 5.0 and LR− = 0.06, 0.34 and 0.36, respectively. | [116] |
| Early-stage decline in metabolic, vascular and renal health. | Urinary free adduct (FL; and val, age and BMI) | Diagnostic algorithm classifying good health vs early-stage health decline. LR+, 8.0.2.8 and 13.2, and LR− 0.24, 0.43 and 0.13 for metabolic, vascular and renal health respectively. | [151] |
Interpretation of level of evidence from likelihood ratios: LR+: 1–2, minimal; 2–5, small; 5–10, moderate; >10, large and conclusive. LR−: 0.5–1.0, minimal; 0.2–0.5, small; 0.1–0.2, moderate; <0.1, large and conclusive [110].
8. Overview and concluding remarks
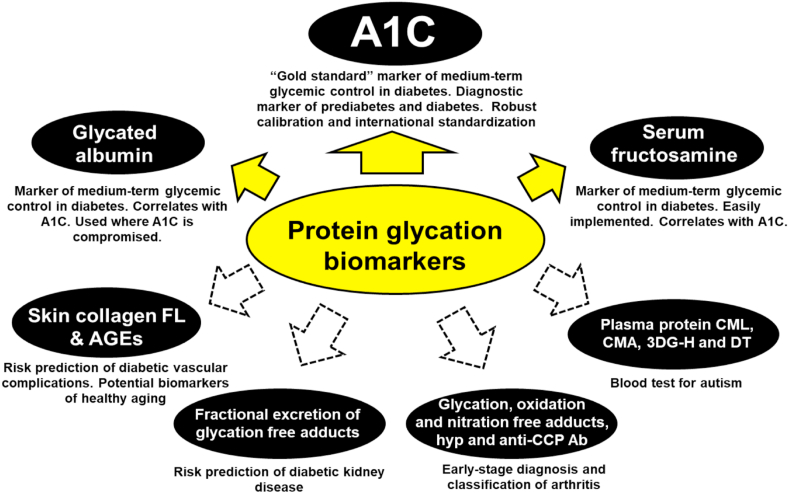
A1C, GA and serum fructosamine are important clinical biomarkers in widespread use for assessment of glycemic control in patients with diabetes and A1C for also diagnosis of prediabetes and diabetes. Measurement of AGE residue content of skin collagen may provide an assessment of aging of skin and healthy aging, an indicator of glycemic control and risk prediction of vascular complication of diabetes. These are valuable clinical biomarkers because they reflect pathways mechanistically linked to the health disorder and disease phenotype: fructosamine, GSP and CML - hyperglycemia and glycemic control; MG-H1, CEL and G-H1 - dicarbonyl stress and metabolic dysfunction of unscheduled glycolysis linked mechanistically to the development of T2DM and diabetic vascular complications; and pentosidine - increased pentosephosphate pathway activity [9,28,119] (Table 1). Increased plasma glycation, oxidation and nitration free adducts combined with hyp and increased fractional excretion of glycation free adducts in diabetes with microalbuminuria may also be valuable diagnostic biomarkers of early-stage arthritis and risk predictors of DKD because they are close to the early-stage disease phenotype – increased joint proteolysis and decline in renal tubular function, respectively. Such biomarkers are likely to provide valuable diagnostic information and support a precision medicine approach. Protein glycation biomarkers are influenced by heritability, aging and decline in metabolic, vascular, renal and skeletal health and other factors. They are therefore applicable to populations of differing ethnicities, bridging the gap between genotype and phenotype [120], and thereby likely to find continued and expanding clinical use. A summary of established and emerging applications of protein glycation biomarkers is given: established biomarkers of glycemic control – A1C, glycated albumin and serum fructosamine; emerging biomarkers of risk prediction of vascular complications of diabetes, early-stage detection and classification of arthritis, a blood test for diagnosis of autism and, potentially, biomarkers of healthy aging (Fig. 3). For future research, with increased availability of analytical standards and LC-MS/MS assay platform for use or reference validation of immunoassays, and application of machine learning algorithm development for optimum biomarker combination and weighting, we call on collaborative efforts from the glycation research community with custodians of large clinical sample collections and computational scientists to develop and validate emerging and further innovate applications of protein glycation biomarkers for clinical diagnosis and screening, disease progression and therapeutic monitoring.
Fig. 3.
Biomarkers of glycation in clinical use and investigational development. See text for details. Key: solid line bordered filled arrows – glycation biomarkers in clinical use; dotted line bordered unfilled arrows - glycation biomarkers in investigational development. Abbreviations: A1C, glycated hemoglobin HbA1c; anti-CCP Ab, anti-cyclic citrullinated peptide antibody; CMA, Nꞷ-carboxymethyl-arginine; 3DG-H, 3-deoxyglucosone-derived hydroimidazolone; and DT, dityrosine.
Declaration of competing interest
The authors declare that they have no conflict of interest in relation to the above manuscript.
Acknowledgements
The authors thank Qatar University and the Qatar Foundation for support for their glycation research.
Contributor Information
Naila Rabbani, Email: n.rabbani@qu.edu.qa.
Paul J. Thornalley, Email: pthornalley@hbku.edu.qa.
References
- 1.Hodge J.E. The Amadori rearrangement. Adv. Carbohydr. Chem. 1955;10:169–205. doi: 10.1016/s0096-5332(08)60392-6. [DOI] [PubMed] [Google Scholar]
- 2.Schleicher E., Scheller L., Wieland O.H. Quantitation of lysine bound glucose of normal and diabetic erythrocyte membranes by HPLC analysis of furosine [ε-N(L-furoylmethyl)-L-lysine] Biochem. Biophys. Res. Commun. 1981;99:1011–1019. doi: 10.1016/0006-291x(81)91262-6. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed N., Dobler D., Dean M., Thornalley P.J. Peptide mapping identifies hotspot site of modification in human serum albumin by methylglyoxal involved in ligand binding and esterase activity. J. Biol. Chem. 2005;280:5724–5732. doi: 10.1074/jbc.M410973200. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed N., Babaei-Jadidi R., Howell S.K., Beisswenger P.J., Thornalley P.J. Degradation products of proteins damaged by glycation, oxidation and nitration in clinical type 1 diabetes. Diabetologia. 2005;48:1590–1603. doi: 10.1007/s00125-005-1810-7. [DOI] [PubMed] [Google Scholar]
- 5.Rabbani N., Thornalley P.J. Glycation research in Amino Acids: a place to call home. Amino Acids. 2012;42:1087–1096. doi: 10.1007/s00726-010-0782-1. [DOI] [PubMed] [Google Scholar]
- 6.Margarson M.P., Soni N. Serum albumin: touchstone or totem? Anaesthesia. 1998;53:789–803. doi: 10.1046/j.1365-2044.1998.00438.x. [DOI] [PubMed] [Google Scholar]
- 7.Agalou S., Ahmed N., Babaei-Jadidi R., Dawnay A., Thornalley P.J. Profound mishandling of protein glycation degradation products in uremia and dialysis. J. Am. Soc. Nephrol. 2005;16:1471–1485. doi: 10.1681/ASN.2004080635. [DOI] [PubMed] [Google Scholar]
- 8.Perkins B.A., Rabbani N., Weston A., Adaikalakoteswari A., Lee J.A., Lovblom L.E., Cardinez N., Thornalley P.J. High fractional excretion of glycation adducts is associated with subsequent early decline in renal function in type 1 diabetes. Sci. Rep. 2020;10:12709. doi: 10.1038/s41598-020-69350-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rabbani N., Thornalley Paul J. Reading patterns of proteome damage by glycation, oxidation and nitration: quantitation by stable isotopic dilution analysis LC-MS/MS. Essays Biochem. 2020;64:169–183. doi: 10.1042/EBC20190047. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed N., Thornalley P.J., Luthen R., Haussinger D., Sebekova K., Schinzel R., Voelker W., Heidland A. Processing of protein glycation, oxidation and nitrosation adducts in the liver and the effect of cirrhosis. J. Hepatol. 2004;41:913–919. doi: 10.1016/j.jhep.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Rabbani N., Sebekova K., Sebekova K., Jr., Heidland A., Thornalley P.J. Protein glycation, oxidation and nitration free adduct accumulation after bilateral nephrectomy and ureteral ligation. Kidney Int. 2007;72:1113–1121. doi: 10.1038/sj.ki.5002513. [DOI] [PubMed] [Google Scholar]
- 12.Xue M., Weickert M.O., Qureshi S., Ngianga-Bakwin K., Anwar A., Waldron M., Shafie A., Messenger D., Fowler M., Jenkins G., Rabbani N., Thornalley P.J. Improved glycemic control and vascular function in overweight and obese subjects by glyoxalase 1 inducer formulation. Diabetes. 2016;65:2282–2294. doi: 10.2337/db16-0153. [DOI] [PubMed] [Google Scholar]
- 13.Leong A., Wheeler E. Genetics of HbA1c: a case study in clinical translation. Curr. Opin. Genet. Dev. 2018;50:79–85. doi: 10.1016/j.gde.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Thornalley P.J., Rabbani N. Detection of oxidized and glycated proteins in clinical samples using mass spectrometry - a user's perspective. Biochim. Biophys. Acta. 2014;1840:818–829. doi: 10.1016/j.bbagen.2013.03.025. [DOI] [PubMed] [Google Scholar]
- 15.American-Diabetes-Association 6. Glycemic targets: standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S66–S76. doi: 10.2337/dc20-S006. [DOI] [PubMed] [Google Scholar]
- 16.American-Diabetes-Association, 2 Classification and diagnosis of diabetes: standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S14–S31. doi: 10.2337/dc20-S002. [DOI] [PubMed] [Google Scholar]
- 17.Shapiro R., McManus M.J., Zalut C., Bunn H.F. Sites of nonenzymatic glycosylation of human hemoglobin A. J. Biol. Chem. 1980;255:3120–3127. [PubMed] [Google Scholar]
- 18.Roberts N.B., Amara A.B., Morris M., Green B.N. Long-term evaluation of electrospray ionization mass spectrometric analysis of glycated hemoglobin. Clin. Chem. 2001;47:316–321. [PubMed] [Google Scholar]
- 19.Wang S.H., Wang T.F., Wu C.H., Chen S.H. In-depth comparative characterization of hemoglobin glycation in normal and diabetic bloods by LC-MSMS. J. Am. Soc. Mass Spectrom. 2014;25:758–766. doi: 10.1007/s13361-014-0830-2. [DOI] [PubMed] [Google Scholar]
- 20.Flückiger R., Mortensen H.B. Glycated haemoglobins. J. Chromatogr. B Biomed. Sci. Appl. 1988;429:279–292. doi: 10.1016/s0378-4347(00)83874-8. [DOI] [PubMed] [Google Scholar]
- 21.Prome D., Blouquit Y., Ponthus C., Prome J.C., Rosa J. Structure of the human adult hemoglobin minor fraction-A1b by electrospray and secondary ion mass-spectrometry - pyruvic-acid as amino-terminal blocking group. J. Biol. Chem. 1991;266:13050–13054. [PubMed] [Google Scholar]
- 22.Al-Abed Y., VanPatten S., Li H., Lawson J.A., FitzGerald G.A., Manogue K.R., Bucala R. Characterization of a novel hemoglobin-glutathione adduct that is elevated in diabetic patients. Mol. Med. 2001;7:619–623. [PMC free article] [PubMed] [Google Scholar]
- 23.Delpierre G., Collard F., Fortpied J., Van Schaftingen E. Fructosamine 3-kinase is involved in an intracellular deglycation pathway in human erythrocytes. Biochem. J. 2002;365:801–808. doi: 10.1042/BJ20020325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Delpierre G., Vertommen D., Communi D., Rider M.H., Van Schaftingen E. Identification of fructosamine residues deglycated by fructosamine-3-kinase in human hemoglobin. J. Biol. Chem. 2004;279:27613–27620. doi: 10.1074/jbc.M402091200. [DOI] [PubMed] [Google Scholar]
- 25.Nathan D.M., Kuenen J., Borg R., Zheng H., Schoenfeld D., Heine R.J. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31:1473–1478. doi: 10.2337/dc08-0545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tahara Y., Shima K. The response of ghb to stepwise plasma-glucose change over time in diabetic-patients. Diabetes Care. 1993;16:1313–1314. doi: 10.2337/diacare.16.9.1313. [DOI] [PubMed] [Google Scholar]
- 27.Beach K.W. A theoretical model to predict the behavior of glycosylated hemoglobin levels. J. Theor. Biol. 1979;81:547–561. doi: 10.1016/0022-5193(79)90052-3. [DOI] [PubMed] [Google Scholar]
- 28.Goldstein D.E., Little R.R., Lorenz R.A., Malone J.I., Nathan D., Peterson C.M., Sacks D.B. Tests of glycemia in diabetes. Diabetes Care. 2004;27:1761–1773. doi: 10.2337/diacare.27.7.1761. [DOI] [PubMed] [Google Scholar]
- 29.Feskens E., Brennan L., Dussort P., Flourakis M., Lindner L.M.E., Mela D., Rabbani N., Rathmann W., Respondek F., Stehouwer C., Theis S., Thornalley P., Vinoy S. Potential markers of dietary glycemic exposures for sustained dietary interventions in populations without diabetes. Advances in Nutrition. 2020;11:1221–1236. doi: 10.1093/advances/nmaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freedman B.I. A critical evaluation of glycated protein parameters in advanced nephropathy: a matter of life or death. Time to dispense with the hemoglobin A1C in end-stage kidney disease. Diabetes Care. 2012;35:1621–1624. doi: 10.2337/dc12-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lacy M.E., Wellenius G.A., Sumner A.E., Correa A., Carnethon M.R., Liem R.I., Wilson J.G., Sacks D.B., Jacobs D.R., Jr., Carson A.P., Luo X., Gjelsvik A., Reiner A.P., Naik R.P., Liu S., Musani S.K., Eaton C.B., Wu W.-C. Association of sickle cell trait with hemoglobin A1c in african Americans. J. Am. Med. Assoc. 2017;317:507–515. doi: 10.1001/jama.2016.21035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wheeler E., Leong A., Liu C.-T., Hivert M.-F., Strawbridge R.J., Podmore C., Li M., Yao J., Sim X., Hong J., Chu A.Y., Zhang W., Wang X., Chen P., Maruthur N.M., Porneala B.C., Sharp S.J., Jia Y., Kabagambe E.K., Chang L.-C., Chen W.-M., Elks C.E., Evans D.S., Fan Q., Giulianini F., Go M.J., Hottenga J.-J., Hu Y., Jackson A.U., Kanoni S., Kim Y.J., Kleber M.E., Ladenvall C., Lecoeur C., Lim S.-H., Lu Y., Mahajan A., Marzi C., Nalls M.A., Navarro P., Nolte I.M., Rose L.M., Rybin D.V., Sanna S., Shi Y., Stram D.O., Takeuchi F., Tan S.P., van der Most P.J., Van Vliet-Ostaptchouk J.V., Wong A., Yengo L., Zhao W., Goel A., Martinez Larrad M.T., Radke D., Salo P., Tanaka T., van Iperen E.P.A., Abecasis G., Afaq S., Alizadeh B.Z., Bertoni A.G., Bonnefond A., Böttcher Y., Bottinger E.P., Campbell H., Carlson O.D., Chen C.-H., Cho Y.S., Garvey W.T., Gieger C., Goodarzi M.O., Grallert H., Hamsten A., Hartman C.A., Herder C., Hsiung C.A., Huang J., Igase M., Isono M., Katsuya T., Khor C.-C., Kiess W., Kohara K., Kovacs P., Lee J., Lee W.-J., Lehne B., Li H., Liu J., Lobbens S., Luan J.a., Lyssenko V., Meitinger T., Miki T., Miljkovic I., Moon S., Mulas A., Müller G., Müller-Nurasyid M., Nagaraja R., Nauck M., Pankow J.S., Polasek O., Prokopenko I., Ramos P.S., Rasmussen-Torvik L., Rathmann W., Rich S.S., Robertson N.R., Roden M., Roussel R., Rudan I., Scott R.A., Scott W.R., Sennblad B., Siscovick D.S., Strauch K., Sun L., Swertz M., Tajuddin S.M., Taylor K.D., Teo Y.-Y., Tham Y.C., Tönjes A., Wareham N.J., Willemsen G., Wilsgaard T., Hingorani A.D., Consortium E.-C., Consortium E.P.-I., Lifelines Cohort S., Egan J., Ferrucci L., Hovingh G.K., Jula A., Kivimaki M., Kumari M., Njølstad I., Palmer C.N.A., Serrano Ríos M., Stumvoll M., Watkins H., Aung T., Blüher M., Boehnke M., Boomsma D.I., Bornstein S.R., Chambers J.C., Chasman D.I., Chen Y.-D.I., Chen Y.-T., Cheng C.-Y., Cucca F., de Geus E.J.C., Deloukas P., Evans M.K., Fornage M., Friedlander Y., Froguel P., Groop L., Gross M.D., Harris T.B., Hayward C., Heng C.-K., Ingelsson E., Kato N., Kim B.-J., Koh W.-P., Kooner J.S., Körner A., Kuh D., Kuusisto J., Laakso M., Lin X., Liu Y., Loos R.J.F., Magnusson P.K.E., März W., McCarthy M.I., Oldehinkel A.J., Ong K.K., Pedersen N.L., Pereira M.A., Peters A., Ridker P.M., Sabanayagam C., Sale M., Saleheen D., Saltevo J., Schwarz P.E.H., Sheu W.H.H., Snieder H., Spector T.D., Tabara Y., Tuomilehto J., van Dam R.M., Wilson J.G., Wilson J.F., Wolffenbuttel B.H.R., Wong T.Y., Wu J.-Y., Yuan J.-M., Zonderman A.B., Soranzo N., Guo X., Roberts D.J., Florez J.C., Sladek R., Dupuis J., Morris A.P., Tai E.S., Selvin E., Rotter J.I., Langenberg C., Barroso I., Meigs J.B. Impact of common genetic determinants of Hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: a transethnic genome-wide meta-analysis. PLoS Med. 2017;14 doi: 10.1371/journal.pmed.1002383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American-Diabetes-Association 14. Management of diabetes in pregnancy: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S183–S192. doi: 10.2337/dc20-S014. [DOI] [PubMed] [Google Scholar]
- 34.D.-C.-C.-T.R. Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New Engl. J. Med. 1993;327:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 35.Nathan D.M., Cleary P.A., Backlund J.-Y.C., Genuth S.M., Lachin J.M., Orchard T.J., Raskin P., Zinman B., Diabetes C. I. Complications Trial/Epidemiology of Diabetes, G. Complications Study Research, Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N. Engl. J. Med. 2005;353:2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stratton I.M., Adler A.I., Neil H.A.W., Matthews D.R., Manley S.E., Cull C.A., Hadden D., Turner R.C., Holman R.R. Association of glycaemic with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2002;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carson A.P., Steffes M.W., Carr J.J., Kim Y., Gross M.D., Carnethon M.R., Reis J.P., Loria C.M., Jacobs D.R., Lewis C.E. Hemoglobin A1c and the progression of coronary artery calcification among adults without diabetes. Diabetes Care. 2015;38:66–71. doi: 10.2337/dc14-0360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aepfelbacher F.C., Yeon S.B., Weinrauch L.A., D'Elia J., Burger A.J. Improved glycemic control induces regression of left ventricular mass in patients with type 1 diabetes mellitus. Int. J. Cardiol. 2004;94:47–51. doi: 10.1016/j.ijcard.2003.04.012. [DOI] [PubMed] [Google Scholar]
- 39.Khaw K.T., Wareham N., Bingham S., Luben R., Welch A., Day N. Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann. Intern. Med. 2004;141:413–420. doi: 10.7326/0003-4819-141-6-200409210-00006. [DOI] [PubMed] [Google Scholar]
- 40.Snieder H., Sawtell P.A., Ross L., Walker J., Spector T.D., Leslie R.D.G. HbA1c Levels are genetically determined even in type 1 diabetes: evidence from healthy and diabetic twins. Diabetes. 2001;50:2858–2863. doi: 10.2337/diabetes.50.12.2858. [DOI] [PubMed] [Google Scholar]
- 41.Barnaby O.S., Cerny R.L., Clarke W., Hage D.S. Quantitative analysis of glycation patterns in human serum albumin using 16O/18O-labeling and MALDI–TOF MS. Clin. Chim. Acta. 2011;412:1606–1615. doi: 10.1016/j.cca.2011.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shimizu I., Kohzuma T., Koga M. A proposed glycemic control marker for the future: glycated albumin. Journal of Laboratory and Precision Medicine. 2019;4 [Google Scholar]
- 43.Sacks D.B., Nathan D.M., Lachin J.M. Gaps in the glycation gap hypothesis. Clin. Chem. 2011;57:150–152. doi: 10.1373/clinchem.2010.158071. [DOI] [PubMed] [Google Scholar]
- 44.Loomis S.J., Tin A., Coresh J., Boerwinkle E., Pankow J.S., Köttgen A., Selvin E., Duggal P. Heritability analysis of nontraditional glycemic biomarkers in the atherosclerosis risk in communities study. Genet. Epidemiol. 2019;43:776–785. doi: 10.1002/gepi.22243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Loomis S.J., Li M., Maruthur N.M., Baldridge A.S., North K.E., Mei H., Morrison A., Carson A.P., Pankow J.S., Boerwinkle E., Scharpf R., Rasmussen-Torvik L.J., Coresh J., Duggal P., Köttgen A., Selvin E. Genome-wide association study of serum fructosamine and glycated albumin in adults without diagnosed diabetes: results from the atherosclerosis risk in communities study. Diabetes. 2018;67:1684–1696. doi: 10.2337/db17-1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Levitt D.G., Levitt M.D. Human serum albumin homeostasis: a new look at the roles of synthesis, catabolism, renal and gastrointestinal excretion, and the clinical value of serum albumin measurements. Int. J. Gen. Med. 2016;9:229–255. doi: 10.2147/IJGM.S102819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cha T., Tahara Y., Yamoto E., Yoneda H., Ikegami H., Noma Y., Shima K., Ogihara T. Renal handling of glycated albumin in non-insulin-dependent diabetes mellitus with nephropathy. Diabetes Res. Clin. Pract. 1991;12:149–156. doi: 10.1016/0168-8227(91)90071-k. [DOI] [PubMed] [Google Scholar]
- 48.Masania J., Malczewska-Malec M., Razny U., Goralska J., Zdzienicka A., Kiec-Wilk B., Gruca A., Stancel-Mozwillo J., Dembinska-Kiec A., Rabbani N., Thornalley P.J. Dicarbonyl stress in clinical obesity. Glycoconj. J. 2016;33:581–589. doi: 10.1007/s10719-016-9692-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parving H.-H., Gyntelberg F. Transcapillary escape rate of albumin and plasma volume in essential hypertension. Circ. Res. 1973;32:643–652. doi: 10.1161/01.res.32.5.643. [DOI] [PubMed] [Google Scholar]
- 50.Dell'Omo G., Penno G., Pucci L., Mariani M., Del Prato S., Pedrinelli R. Abnormal capillary permeability and endothelial dysfunction in hypertension with comorbid Metabolic Syndrome. Atherosclerosis. 2004;172:383–389. doi: 10.1016/j.atherosclerosis.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 51.Nestler J.E., Barlascini C.O., Tetrault G.A., Fratkin M.J., Clore J.N., Blackard W.G. Increased transcapillary escape rate of albumin in nondiabetic men in response to hyperinsulinemia. Diabetes. 1990;39:1212–1217. doi: 10.2337/diab.39.10.1212. [DOI] [PubMed] [Google Scholar]
- 52.O'Hare J.A., Ferriss J.B. Transcapillary escape rate of albumin and extracellular fluid volume in diabetes. Diabetologia. 1985;28:937–938. doi: 10.1007/BF00703142. [DOI] [PubMed] [Google Scholar]
- 53.Ballmer P.E., Ochsenbein A.F., Schutzhofmann S. Transcapillary escape rate of albumin positively correlates with plasma-albumin concentration in acute but not in chronic inflammatory disease. Metabolism-Clinical and Experimental. 1994;43:697–705. doi: 10.1016/0026-0495(94)90117-1. [DOI] [PubMed] [Google Scholar]
- 54.Kornerup K., Nordestgaard B.G., Jensen T.K., Feldt-Rasmussen B., Eiberg J.P., Jensen K.S., Jensen J.S. Transendothelial exchange of low-density lipoprotein is unaffected by the presence of severe atherosclerosis. Cardiovasc. Res. 2004;64:337–345. doi: 10.1016/j.cardiores.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 55.Matsumoto K., Sano K., Nagai R., Suzuki H., Kodama T., Yoshida M., Ueda S., Smedsrod B., Horiuchi S. Endocytic uptake of advanced glycation end products by mouse liver sinusoidal endothelial cells is mediated by a scavenger receptor distinct from the macrophage scavenger receptor class A. Biochem. J. 2000;352:233–240. [PMC free article] [PubMed] [Google Scholar]
- 56.Tsutsui A., Ogura A., Tahara T., Nozaki S., Urano S., Hara M., Kojima S., Kurbangalieva A., Onoe H., Watanabe Y., Taniguchi N., Tanaka K. In vivo imaging of advanced glycation end products (AGEs) of albumin: first observations of significantly reduced clearance and liver deposition properties in mice. Org. Biomol. Chem. 2016;14:5755–5760. doi: 10.1039/c6ob00098c. [DOI] [PubMed] [Google Scholar]
- 57.Svistounov D., Oteiza A., Zykova S.N., Sørensen K.K., McCourt P., McLachlan A.J., McCuskey R.S., Smedsrød B. Hepatic disposal of advanced glycation end products during maturation and aging. Exp. Gerontol. 2013;48:549–556. doi: 10.1016/j.exger.2013.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nagai R., Mera K., Nakajou K., Fujiwara Y., Iwao Y., Imai H., Murata T., Otagiri M. The ligand activity of AGE-proteins to scavenger receptors is dependent on their rate of modification by AGEs. Biochim. Biophys. Acta. 2007;1772:1192–1198. doi: 10.1016/j.bbadis.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 59.Nagai R., Mera K., Fujiwara Y., Nagai M., Otagiri M. Comparison of pharmacokinetics between highly and mildly modified AGE proteins in mice. Ann. N. Y. Acad. Sci. 2008;1126:325–327. doi: 10.1196/annals.1433.002. [DOI] [PubMed] [Google Scholar]
- 60.Irshad Z., Xue M., Ashour A., Larkin J.R., Thornalley P.J., Rabbani N. Activation of the unfolded protein response in high glucose treated endothelial cells is mediated by methylglyoxal. Sci. Rep. 2019;9:7889. doi: 10.1038/s41598-019-44358-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ashour A., Xue M., Al-Motawa M., Thornalley P.J., Rabbani N. Glycolytic overload-driven dysfunction of periodontal ligament fibroblasts in high glucose concentration, corrected by glyoxalase 1 inducer. BMJ Open Diabetes Research & Care. 2020;8 doi: 10.1136/bmjdrc-2020-001458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rabbani N., Adaikalakoteswari A., Rossing K., Rossing P., Tarnow L., Parving H.-H., Thornalley P.J. Effect of Irbesartan treatment on plasma and urinary markers of protein damage in patients with type 2 diabetes and microalbuminuria. Amino Acids. 2012;42:1627–1639. doi: 10.1007/s00726-011-0857-7. [DOI] [PubMed] [Google Scholar]
- 63.Johnson R.N., Metcalf P.A., Baker J.R. Fructosamine: a new approach to the estimation of serum glycosyl protein. An index of diabetic control, Clin. Chim. Acta. 1982;127:87–95. doi: 10.1016/0009-8981(83)90078-5. [DOI] [PubMed] [Google Scholar]
- 64.Juraschek S.P., Steffes M.W., Selvin E. Associations of alternative markers of glycemia with hemoglobin A(1c) and fasting glucose. Clin. Chem. 2012;58:1648–1655. doi: 10.1373/clinchem.2012.188367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thornalley P.J., Langborg A., Minhas H.S. Formation of glyoxal, methylglyoxal and 3-deoxyglucosone in the glycation of proteins by glucose. Biochem. J. 1999;344:109–116. [PMC free article] [PubMed] [Google Scholar]
- 66.Cohen R.M., Holmes Y.R., Chenier T.C., Joiner C.H. Discordance between HbA1c and fructosamine. Diabetes Care. 2003;26:163–167. doi: 10.2337/diacare.26.1.163. [DOI] [PubMed] [Google Scholar]
- 67.Rodríguez-Segade S., Rodríguez J., Cabezas-Agricola J.M., Casanueva F.F., Camiña F. Progression of nephropathy in type 2 diabetes: the glycation gap is a significant predictor after adjustment for glycohemoglobin (Hb A1c) Clin. Chem. 2011;57:264–271. doi: 10.1373/clinchem.2010.144949. [DOI] [PubMed] [Google Scholar]
- 68.Dyer D.G., Dunn J.A., Thorpe S.R., Bailie K.E., Lyons T.J., McCance D.R., Baynes J.W. Accumulation of Maillard reaction products in skin collagen in diabetes and aging. J. Clin. Invest. 1993;91:2463–2469. doi: 10.1172/JCI116481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Reaven G.M., Chen N., Hollenbeck C., Chen Y.-D.I. Effect of age on glucose tolerance and glucose uptake in healthy individuals. J. Am. Geriatr. Soc. 1989;37:735–740. doi: 10.1111/j.1532-5415.1989.tb02235.x. [DOI] [PubMed] [Google Scholar]
- 70.Lyons T.J., Bailie K.E., Dyer D.G., Dunn J.A., Baynes J.W. Decrease in skin collagen glycation with improved glycemic control in patients with insulin-dependent diabetes mellitus. J. Clin. Invest. 1991;87:1910–1915. doi: 10.1172/JCI115216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Genuth S., Sun W., Cleary P., Gao X., Sell D.R., Lachin J., Group t.D.E.R., Monnier V.M. Skin advanced glycation endproducts (AGEs) glucosepane and methylglyoxal hydroimidazolone are independently associated with long-term microvascular complication progression of type I diabetes. Diabetes. 2015;64:266–278. doi: 10.2337/db14-0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Monnier V.M., Sun W., Gao X., Sell D.R., Cleary P.A., Lachin J.M., Genuth S., The D.E.R.G. Skin collagen advanced glycation endproducts (AGEs) and the long-term progression of sub-clinical cardiovascular disease in type 1 diabetes. Cardiovasc. Diabetol. 2015;14:118. doi: 10.1186/s12933-015-0266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chiu C.-J., Rabbani N., Rowan S., Chang M.-L., Sawyer S., Hu F.B., Willett W., Thornalley P.J., Anwar A., Bar L., Kang J.H., Taylor A. Studies of advanced glycation end products and oxidation biomarkers for type 2 diabetes. Biofactors. 2018;44:281–288. doi: 10.1002/biof.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fan X., Sell D.R., Zhang J., Nemet I., Theves M., Lu J., Strauch C., Halushka M.K., Monnier V.M. Anaerobic vs aerobic pathways of carbonyl and oxidant stress in human lens and skin during aging and in diabetes: a comparative analysis. Free Radic. Biol. Med. 2010;49:847–856. doi: 10.1016/j.freeradbiomed.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Biemel K.M., Friedl D.A., Lederer M.O. Identification and quantification of major Maillard cross-links in human serum albumin and lens protein - evidence for glucosepane as the dominant compound. J. Biol. Chem. 2002;277:24907–24915. doi: 10.1074/jbc.M202681200. [DOI] [PubMed] [Google Scholar]
- 76.Schulze C., Wetzel F., Kueper T., Malsen A., Muhr G., Jaspers S., Blatt T., Wittern K.P., Wenck H., Kas J.A. Stiffening of human skin fibroblasts with age. Clin. Plast. Surg. 2012;39:9–20. doi: 10.1016/j.cps.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 77.Ahmed N., Argirov O.K., Minhas H.S., Cordeiro C.A., Thornalley P.J. Assay of advanced glycation endproducts (AGEs): surveying AGEs by chromatographic assay with derivatisation by aminoquinolyl-N-hydroxysuccimidyl-carbamate and application to Nε-carboxymethyl-lysine- and Nε-(1-carboxyethyl)lysine-modified albumin. Biochem. J. 2002;364:1–14. doi: 10.1042/bj3640001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rabbani N., Xue M., Thornalley P.J. Methylglyoxal-induced dicarbonyl stress in aging and disease: first steps towards glyoxalase 1-based treatments. Clin Sci. 2016;130:1677–1696. doi: 10.1042/CS20160025. [DOI] [PubMed] [Google Scholar]
- 79.Schram M.T., Schalkwijk C.G., Bootsma A.H., Fuller J.H., Chaturvedi N., Stehouwer C.D.A. Advanced glycation end products are associated with pulse pressure in type 1 diabetes - the EURODIAB Prospective Complications Study. Hypertension. 2005;46:232–237. doi: 10.1161/01.HYP.0000164574.60279.ba. [DOI] [PubMed] [Google Scholar]
- 80.Nin J.W., Jorsal A., Ferreira I., Schalkwijk C.G., Prins M.H., Parving H.H., Tarnow L., Rossing P., Stehouwer C.D. Higher plasma levels of advanced glycation end products are associated with incident cardiovascular disease and all-cause mortality in type 1 diabetes A 12-year follow-up study. Diabetes Care. 2011;34:442–447. doi: 10.2337/dc10-1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Klein R., Horak K., Lee K.E., Danforth L., Cruickshanks K.J., Tsai M.Y., Gangnon R.E., Klein B.E.K. The relationship of serum soluble receptor for advanced glycation end products (sRAGE) and carboxymethyl lysine (CML) to the incidence of diabetic nephropathy in persons with type 1 diabetes. Diabetes Care. 2017;40:e117–e119. doi: 10.2337/dc17-0421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Perkins B.A., Rabbani N., Weston A., Ficociello L.H., Adaikalakoteswari A., Niewczas M., Warram J., Krolewski A.S., Thornalley P. Serum levels of advanced glycation endproducts and other markers of protein damage in early diabetic nephropathy in type 1 diabetes. PloS One. 2012;7 doi: 10.1371/journal.pone.0035655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hanssen N.M.J., Beulens J.W.J., van Dieren S., Scheijen J.L.J.M., van der A D.L., Spijkerman A.M.W., van der Schouw Y.T., Stehouwer C.D.A., Schalkwijk C.G. Plasma advanced glycation end products are associated with incident cardiovascular events in individuals with type 2 diabetes: a case-cohort study with a median follow-up of 10 Years (EPIC-NL) Diabetes. 2015;64:257–265. doi: 10.2337/db13-1864. [DOI] [PubMed] [Google Scholar]
- 84.Fosmark D.S., Torjesen P.A., Kilhovd B.K., Berg T.J., Sandvik L., Hanssen K.F., Agardh C.D., Agardh E. Increased serum levels of the specific advanced glycation end product methylglyoxal-derived hydroimidazolone are associated with retinopathy in patients with type 2 diabetes mellitus. Metabolism-Clinical and Experimental. 2006;55:232–236. doi: 10.1016/j.metabol.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 85.Gaens K.H.J., Ferreira I., van de Waarenburg M.P.H., van Greevenbroek M.M., van der Kallen C.J.H., Dekker J.M., Nijpels G., Rensen S.S., Stehouwer C.D.A., Schalkwijk C.G. Protein-bound plasma N-epsilon-(Carboxymethyl) lysine is inversely associated with central obesity and inflammation and significantly explain a part of the central obesity-related increase in inflammation the hoorn and CODAM studies. Arterioscler. Thromb. Vasc. Biol. 2015;35:2707–2713. doi: 10.1161/ATVBAHA.115.306106. [DOI] [PubMed] [Google Scholar]
- 86.Rabbani N., Thornalley P.J. Advanced glycation end products in the pathogenesis of chronic kidney disease. Kidney Int. 2018;93:803–813. doi: 10.1016/j.kint.2017.11.034. [DOI] [PubMed] [Google Scholar]
- 87.Machowska A., Sun J., Qureshi A.R., Isoyama N., Leurs P., Anderstam B., Heimburger O., Barany P., Stenvinkel P., Lindholm B. Plasma pentosidine and its association with mortality in patients with chronic kidney disease. PloS One. 2016;11 doi: 10.1371/journal.pone.0163826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Schwedler S.B., Metzger T., Schinzel R., Wanner C. Advanced glycation end products and mortality in hemodialysis patients. Kidney Int. 2002;62:301–310. doi: 10.1046/j.1523-1755.2002.00423.x. [DOI] [PubMed] [Google Scholar]
- 89.Wagner Z., Molnar M., Molnar G.A., Tamasko M., Laczy B., Wagner L., Csiky B., Heidland A., Nagy J., Wittmann I. Serum carboxymethyllysine predicts mortality in hemodialysis patients. Am. J. Kidney Dis. 2006;47:294–300. doi: 10.1053/j.ajkd.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 90.Kilhovd B.K., Juutilainen A., Lehto S., Ronnemaa T., Torjesen P.A., Hanssen K.F., Laakso M. Increased serum levels of methylglyoxal-derived hydroimidazolone-AGE are associated with increased cardiovascular disease mortality in nondiabetic women. Atherosclerosis. 2009;205:590–594. doi: 10.1016/j.atherosclerosis.2008.12.041. [DOI] [PubMed] [Google Scholar]
- 91.Godfrey L., Yamada-Fowler N., Smith J.A., Thornalley P.J., Rabbani N. Arginine-directed glycation and decreased HDL plasma concentration and functionality. Nutr. Diabetes. 2014;4:e134. doi: 10.1038/nutd.2014.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rabbani N., Godfrey L., Xue M., Shaheen F., Geoffrion M., Milne R., Thornalley P.J. Conversion of low density lipoprotein to the pro-atherogenic form by methylglyoxal with increased arterial proteoglycan binding and aortal retention. Diabetes. 2011;60:1973–1980. doi: 10.2337/db11-0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mäkinen V.-P., Civelek M., Meng Q., Zhang B., Zhu J., Levian C., Huan T., Segrè A.V., Ghosh S., Vivar J., Nikpay M., Stewart A.F.R., Nelson C.P., Willenborg C., Erdmann J., Blakenberg S., O'Donnell C.J., März W., Laaksonen R., Epstein S.E., Kathiresan S., Shah S.H., Hazen S.L., Reilly M.P., Lusis A.J., Samani N.J., Schunkert H., Quertermous T., McPherson R., Yang X., Assimes T.L. The-coronary-ARtery-DIsease-genome-wide-replication-Meta-analysis-consortium, integrative genomics reveals novel molecular pathways and gene networks for coronary artery disease. PLoS Genet. 2014;10 doi: 10.1371/journal.pgen.1004502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Linssen P.B., Henry R.M., Schalkwijk C.G., Dekker J.M., Nijpels G., Rocca H.-P.B.-L., Stehouwer C.D. Serum advanced glycation endproducts are associated with left ventricular dysfunction in normal glucose metabolism but not in type 2 diabetes: the Hoorn Study. Diabetes Vasc. Dis. Res. 2016;13:278–285. doi: 10.1177/1479164116640680. [DOI] [PubMed] [Google Scholar]
- 95.Hesse B., Parving H., Lund-Jacobsen H., Noer I. Transcapillary escape rate of albumin and right atrial pressure in chronic congestive heart failure before and after treatment. Circ. Res. 1976;39:358–361. doi: 10.1161/01.res.39.3.358. [DOI] [PubMed] [Google Scholar]
- 96.Thornalley P.J., Battah S., Ahmed N., Karachalias N., Agalou S., Babaei-Jadidi R., Dawnay A. Quantitative screening of advanced glycation endproducts in cellular and extracellular proteins by tandem mass spectrometry. Biochem. J. 2003;375:581–592. doi: 10.1042/BJ20030763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pugliese G., Penno G., Natali A., Barutta F., Di Paolo S., Reboldi G., Gesualdo L., De Nicola L. Diabetic kidney disease: new clinical and therapeutic issues. Joint position statement of the Italian Diabetes Society and the Italian Society of Nephrology on “The natural history of diabetic kidney disease and treatment of hyperglycemia in patients with type 2 diabetes and impaired renal function”. Nutr. Metabol. Cardiovasc. Dis. 2019;29:1127–1150. doi: 10.1016/j.numecd.2019.07.017. [DOI] [PubMed] [Google Scholar]
- 98.Krolewski A.S., Skupien J., Rossing P., Warram J.H. Fast renal decline to end-stage renal disease: an unrecognized feature of nephropathy in diabetes. Kidney Int. 2017;91:1300–1311. doi: 10.1016/j.kint.2016.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Grunwald S., Krause R., Bruch M., Henle T., Brandsch M. Transepithelial flux of early and advanced glycation compounds across Caco-2 cell monolayers and their interaction with intestinal amino acid and peptide transport systems. Br. J. Nutr. 2006;95:1221–1228. doi: 10.1079/bjn20061793. [DOI] [PubMed] [Google Scholar]
- 100.Hellwig M., Geissler S., Matthes R., Peto A., Silow C., Brandsch M., Henle T. Transport of free and peptide-bound glycated amino acids: synthesis, transepithelial flux at Caco-2 cell monolayers, and interaction with apical membrane transport proteins. Chembiochem. 2011;12:1270–1279. doi: 10.1002/cbic.201000759. [DOI] [PubMed] [Google Scholar]
- 101.Anwar A., Abruzzo P.M., Pasha S., Rajpoot K., Bolotta A., Ghezzo A., Marini M., Posar A., Visconti P., Thornalley P.J., Rabbani N. Advanced glycation endproducts, dityrosine and arginine transporter dysfunction in autism - a source of biomarkers for clinical diagnosis. Mol. Autism. 2018;9:3. doi: 10.1186/s13229-017-0183-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fotiadis D., Kanai Y., Palacín M. The SLC3 and SLC7 families of amino acid transporters. Mol. Aspect. Med. 2013;34:139–158. doi: 10.1016/j.mam.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 103.Makrides V., Camargo S.M.R., Verrey F. American Physiological Society; New York: 2014. Transport of Amino Acids in the Kidney, Comprehensive Physiology; pp. 367–403. [DOI] [PubMed] [Google Scholar]
- 104.Chambers J.C., Zhang W., Lord G.M., van der Harst P., Lawlor D.A., Sehmi J.S., Gale D.P., Wass M.N., Ahmadi K.R., Bakker S.J.L., Beckmann J., Bilo H.J.G., Bochud M., Brown M.J., Caulfield M.J., Connell J.M.C., Cook H.T., Cotlarciuc I., Smith G.D., de Silva R., Deng G., Devuyst O., Dikkeschei L.D., Dimkovic N., Dockrell M., Dominiczak A., Ebrahim S., Eggermann T., Farrall M., Ferrucci L., Floege J., Forouhi N.G., Gansevoort R.T., Han X., Hedblad B., van der Heide J.J.H., Hepkema B.G., Hernandez-Fuentes M., Hypponen E., Johnson T., de Jong P.E., Kleefstra N., Lagou V., Lapsley M., Li Y., Loos R.J.F., Luan J.a., Luttropp K., Maréchal C., Melander O., Munroe P.B., Nordfors L., Parsa A., Peltonen L., Penninx B.W., Perucha E., Pouta A., Prokopenko I., Roderick P.J., Ruokonen A., Samani N.J., Sanna S., Schalling M., Schlessinger D., Schlieper G., Seelen M.A.J., Shuldiner A.R., Sjögren M., Smit J.H., Snieder H., Soranzo N., Spector T.D., Stenvinkel P., Sternberg M.J.E., Swaminathan R., Tanaka T., Ubink-Veltmaat L.J., Uda M., Vollenweider P., Wallace C., Waterworth D., Zerres K., Waeber G., Wareham N.J., Maxwell P.H., McCarthy M.I., Jarvelin M.-R., Mooser V., Abecasis G.R., Lightstone L., Scott J., Navis G., Elliott P., Kooner J.S. Genetic loci influencing kidney function and chronic kidney disease. Nat. Genet. 2010;42:373–375. doi: 10.1038/ng.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chasman D.I., Fuchsberger C., Pattaro C., Teumer A., Böger C.A., Endlich K., Olden M., Chen M.-H., Tin A., Taliun D., Li M., Gao X., Gorski M., Yang Q., Hundertmark C., Foster M.C., O'Seaghdha C.M., Glazer N., Isaacs A., Liu C.-T., Smith A.V., O'Connell J.R., Struchalin M., Tanaka T., Li G., Johnson A.D., Gierman H.J., Feitosa M.F., Hwang S.-J., Atkinson E.J., Lohman K., Cornelis M.C., Johansson A., Tönjes A., Dehghan A., Lambert J.-C., Holliday E.G., Sorice R., Kutalik Z., Lehtimäki T., Esko T., Deshmukh H., Ulivi S., Chu A.Y., Murgia F., Trompet S., Imboden M., Coassin S., Pistis G., Consortium C.A., Consortium I., Consortium C.A., Wtccc T.B. Harris, Launer L.J., Aspelund T., Eiriksdottir G., Mitchell B.D., Boerwinkle E., Schmidt H., Cavalieri M., Rao M., Hu F., Demirkan A., Oostra B.A., de Andrade M., Turner S.T., Ding J., Andrews J.S., Freedman B.I., Giulianini F., Koenig W., Illig T., Meisinger C., Gieger C., Zgaga L., Zemunik T., Boban M., Minelli C., Wheeler H.E., Igl W., Zaboli G., Wild S.H., Wright A.F., Campbell H., Ellinghaus D., Nöthlings U., Jacobs G., Biffar R., Ernst F., Homuth G., Kroemer H.K., Nauck M., Stracke S., Völker U., Völzke H., Kovacs P., Stumvoll M., Mägi R., Hofman A., Uitterlinden A.G., Rivadeneira F., Aulchenko Y.S., Polasek O., Hastie N., Vitart V., Helmer C., Wang J.J., Stengel B., Ruggiero D., Bergmann S., Kähönen M., Viikari J., Nikopensius T., Province M., Ketkar S., Colhoun H., Doney A., Robino A., Krämer B.K., Portas L., Ford I., Buckley B.M., Adam M., Thun G.-A., Paulweber B., Haun M., Sala C., Mitchell P., Ciullo M., Kim S.K., Vollenweider P., Raitakari O., Metspalu A., Palmer C., Gasparini P., Pirastu M., Jukema J.W., Probst-Hensch N.M., Kronenberg F., Toniolo D., Gudnason V., Shuldiner A.R., Coresh J., Schmidt R., Ferrucci L., Siscovick D.S., van Duijn C.M., Borecki I.B., Kardia S.L.R., Liu Y., Curhan G.C., Rudan I., Gyllensten U., Wilson J.F., Franke A., Pramstaller P.P., Rettig R., Prokopenko I., Witteman J., Hayward C., Ridker P.M., Parsa A., Bochud M., Heid I.M., Kao W.H.L., Fox C.S., Köttgen A. Integration of genome-wide association studies with biological knowledge identifies six novel genes related to kidney function. Hum. Mol. Genet. 2012;21:5329–5343. doi: 10.1093/hmg/dds369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Beisswenger P.J., Howell S.K., Russell G.B., Miller M.E., Rich S.S., Mauer M. Early progression of diabetic nephropathy correlates with methylglyoxal-derived advanced glycation end products. Diabetes Care. 2013;36:3234–3239. doi: 10.2337/dc12-2689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Elsabbagh M., Divan G., Koh Y.-J., Kim Y.S., Kauchali S., Marcín C., Montiel-Nava C., Patel V., Paula C.S., Wang C., Yasamy M.T., Fombonne E. Global prevalence of autism and other pervasive developmental disorders. Autism Res. 2012;5:160–179. doi: 10.1002/aur.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Xu G., Strathearn L., Liu B., Bao W. Prevalence of autism spectrum disorder among US children and adolescents. J. Am. Med. Assoc. 2018;319:81–82. doi: 10.1001/jama.2017.17812. 2014-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Narzisi A., Posada M., Barbieri F., Chericoni N., Ciuffolini D., Pinzino M., Romano R., Scattoni M.L., Tancredi R., Calderoni S., Muratori F. Prevalence of Autism Spectrum Disorder in a large Italian catchment area: a school-based population study within the ASDEU project. Epidemiol. Psychiatr. Sci. 2018;29:1–10. doi: 10.1017/S2045796018000483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jaeschke R., Guyatt G.H., Sackett D.L., Guyatt G., Bass E., Brill-Edwards P., Browman G., Cook D., Farkouh M., Gerstein H., Haynes B., Hayward R., Holbrook A., Juniper E., Lee H., Levine M., Moyer V., Nishikawa J., Oxman A., Patel A., Philbrick J., Richardson W.S., Sauve S., Sackett D., Sinclair J., Trout K.S., Tugwell P., Tunis S., Walter S., Wilson M. Users' guides to the medical literature: III. How to use an article about a diagnostic test B. What are the results and will they help me in caring for my patients? J. Am. Med. Assoc. 1994;271:703–707. doi: 10.1001/jama.271.9.703. [DOI] [PubMed] [Google Scholar]
- 111.Sun C., Zou M., Wang X., Xia W., Ma Y., Liang S., Hao Y., Wu L., Fu S. FADS1-FADS2 and ELOVL2 gene polymorphisms in susceptibility to autism spectrum disorders in Chinese children. BMC Psychiatr. 2018;18:283. doi: 10.1186/s12888-018-1868-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lévigne D., Modarressi A., Krause K.-H., Pittet-Cuénod B. NADPH oxidase 4 deficiency leads to impaired wound repair and reduced dityrosine-crosslinking, but does not affect myofibroblast formation. Free Radic. Biol. Med. 2016;96:374–384. doi: 10.1016/j.freeradbiomed.2016.04.194. [DOI] [PubMed] [Google Scholar]
- 113.Bae Y.S., Choi M.K., Lee W.-J. Dual oxidase in mucosal immunity and host-microbe homeostasis. Trends Immunol. 2010;31:278–287. doi: 10.1016/j.it.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 114.Mussap M., Noto A., Fanos V. Metabolomics of autism spectrum disorders: early insights regarding mammalian-microbial cometabolites. Expert Rev. Mol. Diagn. 2016;16:869–881. doi: 10.1080/14737159.2016.1202765. [DOI] [PubMed] [Google Scholar]
- 115.Verzijl N., DeGroot J., Oldehinkel E., Bank R.A., Thorpe S.R., Baynes J.W., Bayliss M.T., Bijlsma J.W.J., Lafeber F.P.J.G., TeKoppele J.M. Age-related accumulation of Maillard reaction products in human articular cartilage collagen. Biochem. J. 2000;350:381–387. [PMC free article] [PubMed] [Google Scholar]
- 116.Legrand C., Ahmed U., Anwar A., Rajpoot K., Pasha S., Lambert C., Davidson R.K., Clark I.M., Thornalley P.J., Henrotin Y., Rabbani N. Glycation marker glucosepane increases with the progression of osteoarthritis and correlates with morphological and functional changes of cartilage in vivo. Arthritis Res. Ther. 2018;20:131. doi: 10.1186/s13075-018-1636-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wells-Knecht M.C., Lyons T.J., McCance D.R., Thorpe S.R., Baynes J.W. Age-dependent increases in ortho-tyrosine and methionine sulfoxide in human skin collagen is not accelerated in diabetes. J. Clin. Invest. 1997;100:839–846. doi: 10.1172/JCI119599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ahmed U., Anwar A., Savage R.S., Thornalley P.J., Rabbani N. Protein oxidation, nitration and glycation biomarkers for early-stage diagnosis of osteoarthritis of the knee and typing and progression of arthritic disease. Arthritis Res. Ther. 2016;18:250. doi: 10.1186/s13075-016-1154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rabbani N., Thornalley P.J. Hexokinase-2 glycolytic overload in diabetes and ischemia–reperfusion injury. Trends in Endocrinology & Metabolism. 2019;30:419–431. doi: 10.1016/j.tem.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 120.Jenkinson C.P., Göring H.H.H., Arya R., Blangero J., Duggirala R., DeFronzo R.A. Transcriptomics in type 2 diabetes: bridging the gap between genotype and phenotype. Genomics Data. 2016;8:25–36. doi: 10.1016/j.gdata.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Erbersdobler H.F., Faist V. Metabolic transit of Amadori products. Nahrung-Food. 2001;45:177–181. doi: 10.1002/1521-3803(20010601)45:3<177::AID-FOOD177>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 122.Ahmed N., Babaei-Jadidi R., Howell S.K., Thornalley P.J., Beisswenger P.J. Glycated and oxidized protein degradation products are indicators of fasting and postprandial hyperglycemia in diabetes. Diabetes Care. 2005;28:2465–2471. doi: 10.2337/diacare.28.10.2465. [DOI] [PubMed] [Google Scholar]
- 123.Knecht K.J., Dunn J.A., McFarland K.F., McCance D.R., Lyons T.J., Thorpe S.R., Baynes J.W. Effect of diabetes and aging on carboxymethyllysine levels in human urine. Diabetes. 1991;40:190–196. doi: 10.2337/diab.40.2.190. [DOI] [PubMed] [Google Scholar]
- 124.Liardon R., de Weck-Gaudard D., Philipossian G., Finot P.A. Identification of Nε-carboxymethyllysine: a new Maillard reaction product, in rat urine. J. Agric. Food Chem. 1987;35:427–431. [Google Scholar]
- 125.Wang F., Zhao Y., Niu Y., Wang C., Wang M., Li Y., Sun C. Activated glucose-6-phosphate dehydrogenase is associated with insulin resistance by upregulating pentose and pentosidine in diet-induced obesity of rats. Horm. Metab. Res. 2012;44:938–942. doi: 10.1055/s-0032-1323727. [DOI] [PubMed] [Google Scholar]
- 126.Meerwaldt R., Graaff R., Oomen P.H.N., Links T.P., Jager J.J., Alderson N.L., Thorpe S.R., Baynes J.W., Gans R.O.B., Smit A.J. Simple non-invasive assessment of advanced glycation endproduct accumulation. Diabetologia. 2004;47:1324–1330. doi: 10.1007/s00125-004-1451-2. [DOI] [PubMed] [Google Scholar]
- 127.Foerster A., Henle T. Glycation in food and metabolic transit of dietary AGEs (advanced glycation end-products): studies on the urinary excretion of pyrraline. Biochem. Soc. Trans. 2003;31:1383–1385. doi: 10.1042/bst0311383. [DOI] [PubMed] [Google Scholar]
- 128.Hohmann C., Liehr K., Henning C., Fiedler R., Girndt M., Gebert M., Hulko M., Storr M., Glomb M.A. Detection of free advanced glycation end products in vivo during hemodialysis. J. Agric. Food Chem. 2017;65:930–937. doi: 10.1021/acs.jafc.6b05013. [DOI] [PubMed] [Google Scholar]
- 129.John W.G., Gray M.R., Bates D.L., Beacham J.L. Enzyme immunoassay--a new technique for estimating hemoglobin A1c. Clin. Chem. 1993;39:663–666. [PubMed] [Google Scholar]
- 130.Eckerbom S., Bergqvist Y., Jeppsson J.-O. Improved method for analysis of glycated haemoglobin by ion exchange chromatography. Ann. Clin. Biochem. 1994;31:355–360. doi: 10.1177/000456329403100409. [DOI] [PubMed] [Google Scholar]
- 131.John W.G., Little R., Sacks D.B., Weykamp C., Lenters-Westra E., Hornsby T., Zhao Z., Siebelder C., Tennill A., English E. Multicentre evaluation of the premier Hb9210 HbA1c analyser. Clin. Chem. Lab. Med. 2015;53:319–327. doi: 10.1515/cclm-2014-0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kohzuma T., Yamamoto T., Uematsu Y., Shihabi Z.K., Freedman B.I. Basic performance of an enzymatic method for glycated albumin and reference range determination. J. Diabetes Sci. Technol. 2011;5:1455–1462. doi: 10.1177/193229681100500619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Shima K., Ito N., Abe F., Hirota M., Yano M., Yamamoto Y., Uchida T., Noguchi K. High-performance liquid-chromatographic assay of serum glycated albumin. Diabetologia. 1988;31:627–631. doi: 10.1007/BF00264772. [DOI] [PubMed] [Google Scholar]
- 134.Hill R.P., Hindle E.J., Howey J.E., Lemon M., Lloyd D.R. Recommendations for adopting standard conditions and analytical procedures in the measurement of serum fructosamine concentration. Ann. Clin. Biochem. 1990;27:413–424. doi: 10.1177/000456329002700502. [DOI] [PubMed] [Google Scholar]
- 135.Nagai R., Horiuchi S. Application of monoclonal antibody libraries for the measurement of glycation adducts. Biochem. Soc. Trans. 2003;31:1438–1440. doi: 10.1042/bst0311438. [DOI] [PubMed] [Google Scholar]
- 136.Koito W., Araki T., Horiuchi S., Nagai R. Conventional antibody against Nε-(carboxymethyl)lysine (CML) shows cross-reaction to Nε-(carboxyethyl)lysine (CEL): immunochemical quantification of CML with a specific antibody. J. Biochem. 2004;136:831–837. doi: 10.1093/jb/mvh193. [DOI] [PubMed] [Google Scholar]
- 137.Zhang X., Frischmann M., Kientsch-Engel R., Steinmann K., Stopper H., Niwa T., Pischetsrieder M. Two immunochemical assays to measure advanced glycation end-products in serum from dialysis patients. Clin. Chem. Lab. Med. 2005;43:503. doi: 10.1515/CCLM.2005.089. [DOI] [PubMed] [Google Scholar]
- 138.Monnier V.M., Kohn R.R., Cerami A. Accelerated AGE-related browning of human collagen in diabetes- mellitus. Proc. Natl. Acad. Sci. U.S.A. 1984;81:583–587. doi: 10.1073/pnas.81.2.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Xia J., Broadhurst D.L., Wilson M., Wishart D.S. Translational biomarker discovery in clinical metabolomics: an introductory tutorial. Metabolomics. 2012:1–20. doi: 10.1007/s11306-012-0482-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Anguizola J., Matsuda R., Barnaby O.S., Hoy K.S., Wa C., DeBolt E., Koke M., Hage D.S. Review: glycation of human serum albumin. Clin. Chim. Acta. 2013;425:64–76. doi: 10.1016/j.cca.2013.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Misciagna G., Logroscino G., De Michele G., Guerra V., Cisternino A.M., Caruso M.G., Trevisan M. Glycated apolipoprotein B and myocardial infarction. Nutr. Metabol. Cardiovasc. Dis. 2007;17:6–12. doi: 10.1016/j.numecd.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 142.Rabbani N., Varma Chittari M., Bodmer C.W., Zehnder D., Ceriello A., Thornalley P.J. Increased glycation and oxidative damage to apolipoprotein B100 of LDL in patients with type 2 diabetes and effect of metformin. Diabetes. 2010;59:1038–1045. doi: 10.2337/db09-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Schleicher E., Deufel T., Wieland O.H. Non-enzymatic glycation of human serum lipoproteins: elevated epsilon-lysine glycosylated low-density lipoprotein in diabetic patients. FEBS Lett. 1981;129:1–4. doi: 10.1016/0014-5793(81)80741-7. [DOI] [PubMed] [Google Scholar]
- 144.Wang X., Bucala R., Milne R. Epitopes close to the apolipoprotein B low density lipoprotein receptor-binding site are modified by advanced glycation end products. Proc. Natl. Acad. Sci. USA. 1998;95:7643–7647. doi: 10.1073/pnas.95.13.7643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Younis N., Charlton-Menys V., Sharma R., Soran H., Durrington P.N. Glycation of LDL in non-diabetic people: small dense LDL is preferentially glycated both in vivo and in vitro. Atherosclerosis. 2009;202:162–168. doi: 10.1016/j.atherosclerosis.2008.04.036. [DOI] [PubMed] [Google Scholar]
- 146.Calvo C., Ulloa N., Campos M., Verdugo C., Ayrault-Jarrier M. The preferential site of non-enzymatic glycation of human apolipoprotein A-I in vivo. Clin. Chim. Acta. 1993;217:193–198. doi: 10.1016/0009-8981(93)90165-z. [DOI] [PubMed] [Google Scholar]
- 147.Kashyap S.R., Osme A., Ilchenko S., Golizeh M., Lee K., Wang S., Bena J., Previs S.F., Smith J.D., Kasumov T. Glycation reduces the stability of ApoAI and increases HDL dysfunction in diet-controlled type 2 diabetes. J. Clin. Endocrinol. Metab. 2017;103:388–396. doi: 10.1210/jc.2017-01551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Calvo C., Talussot C., Ponsin G., Berthezene F. Non enzymatic glycation of apolipoprotein A-I. Effects on its self-association and lipid binding properties. Biochem. Biophys. Res. Commun. 1988;153:1060–1067. doi: 10.1016/s0006-291x(88)81336-6. [DOI] [PubMed] [Google Scholar]
- 149.Cohen R.M., Snieder H., Lindsell C.J., Beyan H., Hawa M.I., Blinko S., Edwards R., Spector T.D., Leslie R.D. Evidence for independent heritability of the glycation gap (glycosylation gap) fraction of HbA1c in nondiabetic twins. Diabetes Care. 2006;29:1739–1743. doi: 10.2337/dc06-0286. [DOI] [PubMed] [Google Scholar]
- 150.Leslie R.D.G., Beyan H., Sawtell P., Boehm B.O., pector T.D., nieder H. Level of an advanced glycated end product is genetically determined: a study of normal twins. Diabetes. 2003;52:2441–2444. doi: 10.2337/diabetes.52.9.2441. [DOI] [PubMed] [Google Scholar]
- 151.Masania J., Faustmann G., Anwar A., Hafner-Giessauf H., Rajpoot R., Grabher J., Rajpoot K., Tiran B., Obermayer-Pietsch B., Winklhofer-Roob B.M., Roob J.M., Rabbani N., Thornalley P.J. 2019. Urinary Metabolomic Markers of Protein Glycation, Oxidation and Nitration in Early-Stage Decline in Metabolic, Vascular and Renal Health, Oxidative Medicine and Cellular Longevity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Maggs D.G., Jacob R., Rife F., Lange R., Leone P., During M.J., Tamborlane W.V., Sherwin R.S. Interstitial fluid concentrations of glycerol, glucose, and amino acids in human quadricep muscle and adipose tissue. Evidence for significant lipolysis in skeletal muscle. J. Clin. Invest. 1995;96:370–377. doi: 10.1172/JCI118043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bhave G., Neilson E.G. Body fluid dynamics: back to the future. J. Am. Soc. Nephrol. 2011;22:2166–2181. doi: 10.1681/ASN.2011080865. [DOI] [PMC free article] [PubMed] [Google Scholar]