Abstract
Among Uterine Artery Embolization (UAE) complications, vaginal discharge is considered very frequent, especially for submucosal fibroids. Until now, it was reported as clear odorless viscous material. To our knowledge, we describe the first report of intrauterine microsphere migration after UAE. A 45-year-old-woman was admitted to our hospital complaining metromenorrhagia, menstrual cramping, pelvic pain and dyspareunia. After a preprocedural Magnetic Resonance Imaging (MRI) study, she underwent a superselective transradial UAE using 500-700 µm and 700-900 µm microspheres with a good morphological results. At 2-month follow-up, she complained viscous vaginal discharge with “strange pink stiff sphere of about 2 mm in diameter”. A post-procedural-MRI showed fibroid migration towards the uterine cavity, a frequent occurrence especially for submucosal fibroids. The microspheres transvascular migration outside the vessel wall was already reported in a study performed in sheep. Our hypothesis is that the phenomenon of transvascular migration along with the fibroid migration towards the uterine cavity after UAE, may have led the migration of the microspheres directly into the vaginal cavity causing chronic vaginal discharge with pink stiff sphere. Vaginal discharge mixed with “sphere of particles” should be included among the UAE late complication especially for intramural and/or submucosal fibroids with distance to the endometrium less than 2.4 mm at pre-procedural MRI.
Keywords: Uterine artery embolization, Complications, Vaginal discharge, Microsphere, Uterine fibroids, MRI
Introduction
Uterine Artery Embolization (UAE) is considered a safe and feasible treatment, alternative to surgery, for symptomatic fibroids [1]. During procedural planning, MRI imaging plays an important role providing information about fibroids vascularization, size and location (submucosal and/or intramural and/or subserosal) [1], [2], [3].
At post-procedural MRI, performed typically 3-6 months after UAE, in addition to reduction in fibroids and uterine sizes, we can also track fibroids changing location [4].
Some fibroids location can be associated with higher risk of post-procedural complication occurrence; for example, an higher risk of UAE complication such as intracavitary migration and/or expulsion or vaginal discharge, was reported for submucosal fibroids [2], [3], [4].
Among the complication, chronic vaginal discharge is considered very frequent despite being poorly reported spontaneously by women affected; it can be secondary to the development of a sinus tract between the uterine cavity and a necrotic fibroid, resulting in drainage of necrotic material [5].
The vaginal discharge reported in literature was described as clear odorless viscous material [6]. In our case the patient has complained also the presence of “strange small pink stiff spheres”.
This is the first report to describe intrauterine microsphere migration as a complication of UAE for fibroids using microspheres particles.
Case report
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
A 45-year-old woman with uterine fibroids was admitted to our hospital complaining metromenorrhagia, menstrual cramping, pelvic pain and dyspareunia. The patient has a cardiac MRI-compatible Pace-Maker; in order to assess UAE indication, she was scheduled for a pelvic Contrast-enhancement MRI exam. This latter was performed with a 1.5 T MRI scanner and following sequences: axial T1-weighted 3D gradient echo, Contrast-Enhanced T1-weighted 3D gradient echo fat-suppressed, axial and sagittal FSE T2-weighted.
MRI showed multiple intramural fibroids including two deserving particular attention. The first one was a well-defined fibroid measuring 3 cm in diameter which showed an intramural and/or submucosal location with 1.9 mm distance to the endometrium; moderately T2-hyperintense signal in respect to the myometrium and strong contrast enhancement were typical for hypercellular leiomyoma. The second one was a large (7 × 5 × 5 centimeters) non-degenerated subserosal fundal fibroid, displaying isointense signal in T1w and low signal in T2w (Fig. 1). These MRI findings, along with her symptoms, confirmed that she was a good candidate for UAE.
Fig. 1.
Pre-procedural MRI findings. Sagittal (A) and axial FSE T2-weighted (B ,C), axial T1-weighted 3D gradient echo (D) and Contrast-Enhanced T1-weighted 3D gradient echo fat-suppressed (EF) images show: an intramural/submucosal fibroid (arrowhead), up to 3 centimeters, with 1.9 mm distance to the endometrium (C) moderately T2-hyperintense signal in respect to the myometrium and strong contrast enhancement suspect for hypercellular leiomyoma; a large (up to 7 centimeters) non-degenerated subserosal fundal fibroid (*), displaying isointense signal in T1 and low signal in T2.
Therefore, the patient was admitted electively for bilateral UAE. The UAE technique was performed as follow: after placement of 4F hydrophilic sheat at left radial artery, a 4 F MPA catheter was placed into the left right internal iliac artery; a 2.4 F microcatheter (Direxion 2.4 F microcatheter, Boston Scientific Corporation) was placed subselectively into the left uterine artery and contrast digital subtraction angiography (DSA) studies was performed to confirm the anatomy (Fig. 2). After exclusion of uterine-to-ovarian artery collaterals, a superselective UAE was performed with two syringe of 500-700 µm EmboGold particles (S620EG Merit Medical, Jordan, Utah) and one of 700-900 µm EmboGold particles (S820EG Merit Medical, Jordan, Utah) (Fig. 2). In detail 4 ml of 500-700 µm and 2 ml of 700-900 µm EmboGold particles were injiected. The embolic suspension of EmboGold microspheres is obtained mixing with 50/50 saline and/or contrast media solution.
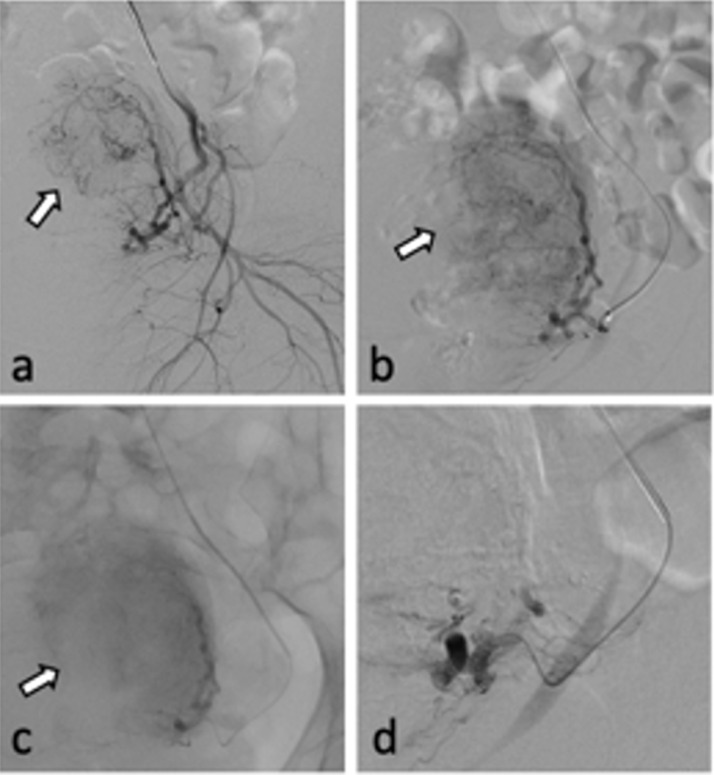
Fig. 2.
Angiographic findings of UAE. Before embolization, selective (A) and superselective angiography (B) from left uterine artery showed large uterine fibroids (arrow);(C) embolization of large fibroid (arrow) with 500-700 µm EmboGold particles injiection; (D) final angiography showed the disappearance of the hypervascularity and fibroid.
During the procedure an episode of radial artery spasm was promptly resolved with an injection of a solution of 100-300 mcg of nitroglycerine through the sheath. Final fluoroscopic acquisitions through bilateral uterine arteries were performed to confirm adequate embolization (Fig. 2). Sheath removal was followed by a radial pressure-assisted compression device (Safeguard, Merit Medical System Inc., Europe) placement.
The trans-radial approach allows patients to flex their legs, walk and sit from a few hours after procedure [7]. She was admitted for overnight observation and discharged on postoperative day 2.
At 1-month follow-up, she had no complaints. She called 2 months after UAE complaining a single episode of viscous vaginal discharge with some “strange pink stiff sphere of about 2 mm in diameter ” containing few particle which have stopped spontaneously (Fig. 3). She denied fever and abdominal pain. The interventional radiology team suggested performing an MRI exam. This latter (Fig. 3) shows a migration of hypercellular leiomyoma from intramural to submucosal location and reduction in size (from 3 to 2.4 centimeters), displaying now T2-hypointense signal in respect to the myometrium and mild contrast enhancement; no significant changes of the non-degenerated subserosal fundal fibroid was noted.
Fig. 3.
Images of macroscopic findings and post-procedural MRI. (A) (B) Pictures of vaginal discharge provided by patient with a sphere of particles of about 2 mm which show changes over time (from 3 to5” to 2 minutes); (C) from top to down sagittal (1) and axial FSE T2-weighted (2-3), axial T1-weighted 3D gradient echo (4-5) and Contrast-Enhanced T1-weighted 3D gradient echo fat-suppressed (6) MRI images show: a submucosal fibroid (arrowhead), up to 2.4 centimeters, with an intracavitary component displaying T2-hypointense signal in respect to the myometrium and mild contrast enhancement; a large (up to 7 centimeters) non-degenerated subserosal fundal fibroid (*), displaying isointense signal in T1 and low signal in T2.
Discussion
Chronic vaginal discharge is a well-known complication of UAE [6]. According to previous study, chronic vaginal discharge can be secondary to the development of a sinus tract between the uterine cavity and a necrotic fibroid, resulting in drainage of necrotic material [5]. These chronic vaginal discharge post-UAE can be more frequent for submucosal or intracavitary fibroids (especially when distant from the endometrium less than 2.4 mm at pre-procedural MRI) treated with UAE and also in case of post-UAE changing location [1], [2], [3], [4]. In our case, post-procedural MRI showed fibroid migration from intramural to submucosal location: in detail the distance of fibroid from the endometrium before UAE were 1.9 mm; after UAE this distance could no longer be calculated since the fibroid has become completely submucosal.
Until now, the vaginal discharge reported in literature was described as clear odorless viscous material [6]. Our patient has complained also the presence of “strange small pink stiff sphere” probably related to particles migration. To our knowledge, this is the first report to describe intrauterine microsphere migration as a complication after UAE for uterine fibroids using microspheres particles.
EmboGold microspheres are non-resorbable red-colored spheres produced from an acrylic polymer and impregnated with porcine gelatin [8]. The pink color of stiff sphere discharged can be associated to the red-color of original embolic microsphere.
The microspheres transvascular migration outside the vessel wall was already reported in a study performed in sheep; in fact about 50% of them were partially or totally excluded from the vessel [9]. The explanation for this phenomenon lies in the inability of microspheres to form aggregates with consequently more distally penetration and possible rupture of the elastic limitans induced by the foreign body inflammatory reaction [9]. The smaller are the microspheres, the easier they migrate outside the vessel [9]. Our hypothesis is that the phenomenon of transvascular migration along with the fibroid migration towards the uterine cavity after UAE, may have led the migration of the microspheres directly into the vaginal cavity causing chronic vaginal discharge with pink stiff sphere.
In conclusion, as already demonstrate in literature, chronic vaginal discharge after UAE is a frequent occurrence especially in case of intramural and/or submucosal fibroids with distance to the endometrium less than 2.4 mm at pre-procedural MRI. Vaginal discharge mixed with sphere of particles should be included among the late complication after UAE especially for intramural and/or submucosal fibroids.
Footnotes
Authors’ contributions:
CG: collecting data, drafting the work, literature analysis/search;
GF, FV, RIR, SL: data acquisition and interpretation;
AGM and PVF: data analysis and interpretation;
SP and AB: Study design/planning and final approval.
Funding. This study was not supported by any funding.
Ethical approval. “All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Patient consent. Written informed consent was obtained from all individuals included in the case report.
Consent for publication. Written consent for publication was obtained for every individual person's data included in the case report.
Contributor Information
Cecilia Gozzo, Email: ceciliagozzo91@gmail.com.
Giovanni Failla, Email: failla.giovanni@gmail.com.
Andrea Musumeci, Email: andreagiovannimusumeci@gmail.com.
Francesco Vacirca, Email: f.va77@libero.it.
Rosa Ida Romeo, Email: rossellaromeo@hotmail.it.
Salvatore Lamberto, Email: slamberto@hotmail.it.
Pietro Valerio Foti, Email: pietrofoti@hotmail.com.
Stefano Palmucci, Email: spalmucci@sirm.org.
Antonio Basile, Email: basile.antonello73@gmail.com.
Reference
- 1.Mailli L, Auyoung EY, Angileri SA. Predicting the fibroid-migratory impact of UAE: role of pre-embolization MRI characteristics. Cardiovasc Intervent Radiol. 2020;43(3):453–458. doi: 10.1007/s00270-019-02348-w. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keung JJ, Spies JB, Caridi TM. Uterine artery embolization: a review of current concepts. Best Pract Res Clin Obstet Gynaecol. 2018;46:66–73. doi: 10.1016/j.bpobgyn.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 3.Foti PV, Tilocca C, Sigona A, Palmucci S, Farina R, Caltabiano R. Benign neoplasms of the uterus: MR imaging of leiomyomas with radiologic pathologic correlation. WCRJ. 2015;2(2):E516. [Google Scholar]
- 4.Verma SK, Gonsalves CF, Baltarowich OH. Spectrum of imaging findings on MRI and CT after uterine artery embolization. Abdom Imaging. 2010;35(1):118–128. doi: 10.1007/s00261-008-9483-6. [DOI] [PubMed] [Google Scholar]
- 5.Walker WJ, Carpenter TT, Kent AS. Persistent vaginal discharge after uterine artery embolization for fibroid tumors: cause of the condition, magnetic resonance imaging appearance, and surgical treatment. Am J Obstet Gynecol. 2004;190 doi: 10.1016/j.ajog.2003.12.010. 1230–1203. [DOI] [PubMed] [Google Scholar]
- 6.Morris DV, Shekhani H, Peters G. Chronic vaginal discharge after uterine fibroid embolization. J Vasc Interv Radiol. 2018;29(9):1319–1321. doi: 10.1016/j.jvir.2018.01.764. [DOI] [PubMed] [Google Scholar]
- 7.Basile A, Rebonato A, Failla G. Early post-procedural patients compliance and VAS after UAE through transradial versus transfemoral approach: preliminary results. Radiol Med. 2018;123(11):885–889. doi: 10.1007/s11547-018-0920-5. [DOI] [PubMed] [Google Scholar]
- 8.EmboGold merit brochure, merit medical
- 9.Laurent A, Wassef M, Namur J, Martal J, Labarre D, Pelage JP. Recanalization and particle exclusion after embolization of uterine arteries in sheep: a long-term study. Fertil Steril. 2009;91(3):884–892. doi: 10.1016/j.fertnstert.2007.12.015. [DOI] [PubMed] [Google Scholar]