Abstract
Background
Substantial concern exists regarding the impact of the COVID-19 pandemic on substance use behaviors. This is especially true for subpopulations like young men who have sex with men and young transgender women (YMSM-YTW) who report higher rates of substance use. This study examines changes in prevalence and frequency of marijuana and non-marijuana drug use among YMSM-YTW following the onset of the pandemic.
Method
Data for this analysis (n = 458 participants, 1356 observations) come from an ongoing longitudinal cohort study of YMSM-YTW. A series of Bayesian multilevel models were used to examine change in prevalence and frequency of use for marijuana and non-marijuana drugs.
Results
Results indicated no systematic change in prevalence or frequency of marijuana use. However, a decrease in non-marijuana drug use was observed (OR = 0.60, 95 % CrI: [0.37, 0.94]) following the onset of the pandemic. Furthermore, a small increase in the frequency of non-marijuana drug use was observed (OR = 1.79, 95 % CrI: [1.02, 3.21]) among individuals who used these substances.
Conclusions
These findings concur with a small number of studies identifying a decrease in drug use prevalence but increase in frequency among those who continue to use drugs. Despite the protective effect of lower drug use prevalence, higher frequency of use may lead to additional negative health outcomes of drug use, particularly among groups facing multiple health challenges such as YMSM-YTW. However, the pandemic likely has a unique impact on substance use behaviors across subpopulations.
Keywords: Drug use frequency, Young men who have sex with men, Transgender women, COVID-19, SARS-CoV-2
1. Introduction
Global health experts have raised substantial concern regarding the impact of the COVID-19 pandemic on substance use due to increased social isolation and elevated stress (McKay and Asmundson, 2020). Yet, the impact of the pandemic is unclear given the reduction in social gatherings where substances are commonly consumed and the potential difficulty physically obtaining or financially affording substances (Chiappini et al., 2020; Dietze and Peacock, 2020). The pandemic may also impact the severity of substance use disorders due to changes in frequency of substance use and the disruption of substance use treatment (Dunlop et al., 2020; Marsden et al., 2020).
A small number of studies have examined changes in substance use behavior following the onset of the pandemic. One study found substance use decreased but frequency of use increased among adolescents following the implementation of social distancing in Canada (Dumas et al., 2020). Similarly, another study found decreases in the likelihood of using alcohol but increases in frequency among those who continued to use alcohol during the pandemic among US adults (Boschuetz et al., 2020). However, the impact of COVID-19 may also vary across subpopulations. Studies have observed an increase in cannabis use among casino gamblers (Xuereb et al., 2020), no increase in cannabis use among a sample of people living with HIV (Hochstatter et al., 2020), and decreases in both cannabis and other illegal drug use among sexual minority men (Starks et al., 2020).
Given these findings, it is important to examine changes in substance use behaviors among groups at high risk for negative health outcomes. For example, young adults may be particularly vulnerable to the pandemic’s detrimental impact on mental health (Elmer et al., 2020; Shanahan et al., 2020). Furthermore, sexual and gender minorities report higher rates of substance use (Schuler et al., 2019) and prevalence of substance use disorders (Chaudhry and Reisner, 2019; Connolly and Gilchrist, 2020) than their peers. For example, two studies found lifetime marijuana use was 40.4 % among transgender youth (Day et al., 2017) and 65.0 % among young gay men (Schuler et al., 2019), 1.5–1.9 times greater than peers. Accordingly, sexual and gender minority young adults are uniquely vulnerable to negative health outcomes during the pandemic given existing high rates of substance use (Salerno et al., 2020). This study leverages a cohort with longitudinal observations of the same individuals before and after the pandemic onset to examine changes in both prevalence and frequency of drug use among young men who have sex with men and young transgender women (YMSM-YTW).
2. Method
2.1. Participants and procedures
All data for this study come from an ongoing longitudinal cohort study of YMSM-YTW (Mustanski et al., 2019a, b). Data collection for this cohort began in February 2015 and remains ongoing. Participants included recruitment from two prior cohorts, Project Q2 (Mustanski et al., 2010) and Crew 450 (Mustanski et al., 2013), as well as new enrollment with participants recruited via venue-based, online, and peer recruitment. All cohort members were required to meet the following criteria: 16–29 years old at enrollment, male assigned at birth (non-cisgender identified individuals were eligible), speak English, report a sexual encounter with a man in the previous year or identify as gay or bisexual, and willing to attend in-person research visits in Chicago. Comprehensive details regarding the cohort can be found elsewhere (Mustanski et al., 2019a). Cohort participants were eligible for one study visit every six months. Participants were eligible for the current analysis if they completed a visit after the shelter in place order in Illinois took effect on March 21 st, 2020 (Dave et al., 2020) by the date of analysis (October 1 st, 2020) and also had at least one other visit within the last year and a half (i.e., 78 weeks) prior to the order. Data were included for up to the two most recent visits before the onset of the pandemic and one observation after the pandemic’s onset. Accordingly, the analysis included 458 participants (43.6 % of 1051 cohort members) of which 440 provided data on 3 visits and 18 provided data on 2 visits, for a total of and 1356 visits.
2.2. Measures
2.2.1. Drug use
Participants reporting drug use in the past six months indicated how many occasions they used the following substances in the past 30 days (1 = 0; 2 = 1–2; 3 = 3–5; 4 = 6–9; 5 = 10–19; 6 = 20–39, 7 = 40 or more): marijuana, cocaine or crack, heroin, ecstasy, methamphetamines, prescription stimulants or amphetamines, prescription painkillers, and prescription depressants or tranquilizers. Only prescription drug use taken without a prescription was included. Drug use was categorized as marijuana use or non-marijuana drug use. This categorization scheme was used because individual drug categories were too sparse to compare changes in specific drug categories (Li et al., 2019; Swann et al., 2017), recreational marijuana was legalized in Illinois starting January 1 st, 2020, and marijuana use is extremely common in the current cohort (Li et al., 2019).
2.2.2. Covariates
We included HIV status and age as covariates given the documented associations with drug use during the pandemic (Dumas et al., 2020; Hochstatter et al., 2020). HIV status was measured using Alere™ Determine™ 4th Generation HIV-1/HIV-2 Ab/Ag Combo rapid test and confirmatory testing according to CDC guidance. Self-report data were used for visits where participants had not previously tested positive and were missing HIV test data. Age represented the number of years from age 16. Gender identity was indicated as male, transgender female, or other.
2.3. Analysis
We examined descriptive statistics regarding past 30-day drug use prevalence by drug category across visits. We also examined alluvial plots (Brunson, 2020) to examine transition between frequencies across visits. Subsequently, we modeled changes in past 30-day prevalence and changes in frequency of use. All models were Bayesian multilevel models and included a random intercept to account for multiple observations per participant, using the default improper flat priors for fixed effects (Bürkner et al., 2019). Change in prevalence was examined using a logistic model. Change in frequency was examined using a sequential ordinal model (Bürkner et al., 2019) with a logistic distribution, commonly known as a continuation ratio model (Liu and Bai, 2020). Frequency of drug use was only examined among individuals who reported past 30-day drug use. Participants were assigned their highest indicated frequency for non-marijuana drug use. The main exposure variable of interest was a dichotomous indicator designating observations following the onset of the pandemic (i.e., shelter in place order). First, we examined a model with independent association of the pandemic. Second, we examined models with age, HIV status, and gender identity as covariates. Finally, we conducted a two-part sensitivity analysis for non-marijuana drug use frequency to ensure participants changing drug types did not bias results. First, we excluded participants that changed their most frequently used non-marijuana drug across visits. Second, we utilized a sum score of frequency across all non-marijuana drugs as the outcome by summing the midpoints number of occasions for each drug.
3. Results
3.1. Descriptives
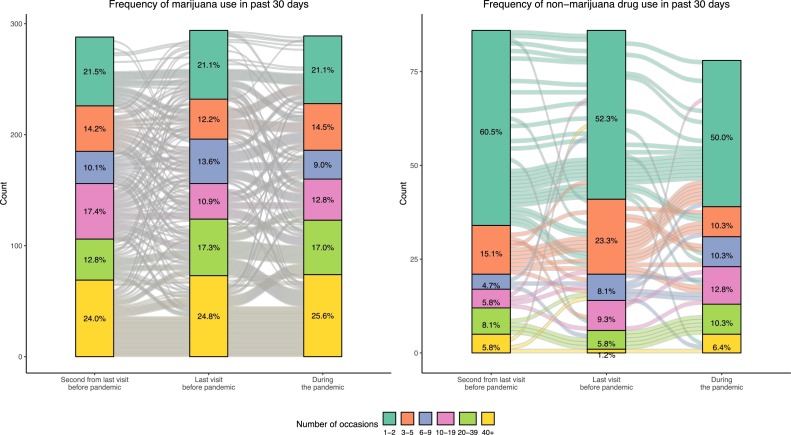
Participants predominantly identified as male (93.2 %; 3.3 % transgender female; 3.5 % another gender identity), were mostly HIV negative (83.8 %), and had a mean age of 21.3 years old. For marijuana, 65.4 %, 64.3 %, and 63.0 % of participants reported use in the second from last visit before the pandemic, last visit before the pandemic, and during the pandemic, respectively. These percentages were 19.5 %, 18.8 %, and 17.0 % for non-marijuana drug use. Fig. 1 presents the frequency of use for each drug type. For drugs other than marijuana, there is a notable decrease in the percentage of individuals using these substances on 3–5 occasions (23.3%–10.3%) and an increase in all categories between 6–9 to 40+ occasions.
Fig. 1.
Alluvial plot of changes in frequency of use for marijuana and non-marijuana drug use.
3.2. Bayesian multilevel models
3.2.1. Prevalence of drug use
For marijuana use, the baseline model (Table 1 ) indicated that marijuana use did not change following the onset of the pandemic (OR = 0.84; 95 % Credible Interval (CrI): 0.60, 1.19). Similar results were also found for the model with covariates included (OR = 0.83, 95 % CrI: 0.58, 1.20). For non-marijuana drug use, the baseline model indicated that drug use was less common during the pandemic (OR = 0.61, 95 % CrI: 0.37, 0.96). Again, similar results were found (OR = 0.60, 95 % CrI: 0.37, 0.94) from the full model after accounting for covariates.
Table 1.
Models results for marijuana and other drug use and frequency of use among users.
| Use |
Frequency |
|||
|---|---|---|---|---|
| Marijuana (n = 458; nobs = 1356) |
Other Drugs (n = 458; nobs = 1356) |
Marijuana (n = 363; nobs = 871) |
Other Drugs (n = 141; nobs = 250) |
|
| OR [95 % CrI] | OR [95 % CrI] | OR [95 % CrI] | OR [95 % CrI] | |
| During Pandemic | 0.84 [0.60, 1.19] | 0.61 [0.37, 0.96] | 1.21 [0.94, 1.55] | 1.75 [1.01, 3.05] |
| With Covariates | ||||
| During Pandemic | 0.83 [0.58, 1.20] | 0.60 [0.37, 0.94] | 1.22 [0.94, 1.57] | 1.79 [1.02, 3.21] |
| Age | 0.86 [0.75, 0.98] | 0.98 [0.85, 1.14] | 0.99 [0.89, 1.12] | 1.17 [0.97, 1.41] |
| HIV Positive | 5.26 [1.8, 15.62] | 0.94 [0.29, 3.26] | 8.46 [3.53, 20.67] | 0.23 [0.03, 1.36] |
| Gender Identity | ||||
| Male (Reference) | – | – | – | – |
| Transgender Female | 0.38 [0.05, 3.00] | 4.62 [0.46, 48.96] | 1.69 [0.24, 12.22] | 2.38 [0.21, 31.32] |
| Other | 1.32 [0.17, 10.99] | 3.43 [0.34, 29.56] | 4.58 [0.79, 29.10] | 3.51 [0.30, 46.90] |
Note. All models include a random intercept to account for multiple observations of participants. Model intercepts are not shown. nobs indicates the number of observations provided by participants for each analysis.
3.2.2. Frequency of drug use
Among users in the past 30 days, there was no association between the onset of the pandemic and frequency of marijuana use (OR = 1.21, 95 % CrI: 0.94, 1.55) in the baseline model and inclusion of covariates did not substantially impact this estimate (OR = 1.22, 95 % CrI: 0.94, 1.57). Among individuals that used non-marijuana drugs in the past 30 days, the baseline model indicated slightly higher frequency of use (OR = 1.75, 95 % CrI: 1.01, 3.05) during the pandemic and was unchanged when including covariates (OR = 1.79, 95 % CrI: 1.02, 3.21). The sensitivity analysis indicated the results appeared robust to the alternative model specifications.
4. Discussion
This study found little evidence of changes in marijuana prevalence or frequency of use in a large cohort of YMSM-YTW. However, a decrease in non-marijuana drug use and a slight increase in the frequency of drug use was observed among individuals who continued to use these substances. These findings highlight the complexity of changes in drug use behaviors during the COVID-19 pandemic that may uniquely impact individuals with different levels of substance use.
While the observed decrease in non-marijuana drug use could be driven by reduced social occasions to use drugs (Chiappini et al., 2020), studies observing related but distinct groups from the current sample have found inconsistent results. One study in an older sample of MSM observed declines in drug use (Starks et al., 2020) and a different study of people living with HIV finding no significant differences in drug use (Hochstatter et al., 2020). Yet, studies of general sample adolescents reported a decrease in prevalence of alcohol and marijuana use (Dumas et al., 2020). Therefore, accumulating evidence suggests the pandemic may differentially impact drug use behaviors among certain subpopulations. Future studies should consider the potential for heterogeneity in response to the pandemic across age, sexual identity, and HIV status.
In addition, two prior studies have observed decreases in prevalence but increases in frequency of use among alcohol and marijuana (Boschuetz et al., 2020; Dumas et al., 2020) during the COVID-19 pandemic. Although we observed no changes in marijuana use, these findings considered together may indicate the COVID-19 pandemic is particularly detrimental to habitual substance users (Daly and Robinson, 2020; Jackson et al., 2020) but be less influential to casual users. Accordingly, there is an urgent need for further data on substance use disorders which may also be impacted by barriers to substance use treatment and harm reduction services during the pandemic (Melamed et al., 2020; Radfar et al., 2020). Indeed, the increased frequency of non-marijuana drug use may indicate an extended need for substance use treatment, even following the widespread adoption of COVID-19 vaccines and these services will be particularly important for subpopulations such as YMSM-YTW with higher prevalence of use.
This study had a number of limitations. The impact of the pandemic cannot be disentangled from the recent legalization of recreational marijuana use in Illinois. Drug use frequency was measured with an ordinal scale that could not capture subtle changes in drug use. Drugs were categorized in broad groups that do not reflect risk differences across specific drugs. We could not provide separate estimates by gender identity due to small cell counts. Finally, these data come from a large and diverse sample important to drug use epidemiology but was not a probability sample.
Despite these limitations, we believe this study provides important initial evidence documenting decreases in prevalence but potential increases in frequency of non-marijuana drug use among YMSM-YTW. Future studies should continue to explore the impact the pandemic may have on substance use behaviors and the potential for heterogeneity in the pandemic’s effects across important subpopulations.
Contributors
PJ developed the research question, conducted the analysis, and drafted the manuscript. BM and MN provided feedback on the analysis plan and also reviewed and edited the entire manuscript.
Role of funding source
This study was supported by a grant from the National Institute on Drug Abuse (U01DA036939; PI: Brian Mustanski). The article is the responsibility of the authors and does not necessarily reflect the views of the National Institutes of Health or the National Institute on Drug Abuse.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- Boschuetz N., Cheng S., Mei L., Loy V.M. Changes in alcohol use patterns in the United States during COVID-19 pandemic. Wisconsin Med. J. 2020;119(3):171–176. [PubMed] [Google Scholar]
- Brunson J. Ggalluvial: layered grammar for alluvial plots. J. Open Source Softw. 2020;5(49):1–6. doi: 10.21105/joss.02017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bürkner P.-C., Bürkner P.-C., Vuorre M. Ordinal regression models in psychology: a tutorial. Adv. Methods Pract. Psychol. Sci. 2019;2:77–101. [Google Scholar]
- Chaudhry A.B., Reisner S.L. Disparities by sexual orientation persist for major depressive episode and substance abuse or dependence: findings from a national probability study of adults in the United States. LGBT Health. 2019;6:261–266. doi: 10.1089/lgbt.2018.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiappini S., Guirguis A., John A., Corkery J.M., Schifano F. COVID-19: the hidden impact on mental health and drug addiction. Front. Psychiatry. 2020;11:767. doi: 10.3389/fpsyt.2020.00767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly D., Gilchrist G. Prevalence and correlates of substance use among transgender adults: a systematic review. Addict. Behav. 2020;111 doi: 10.1016/j.addbeh.2020.106544. [DOI] [PubMed] [Google Scholar]
- Daly M., Robinson E. medRxiv; 2020. Problem Drinking Before and During the COVID-19 Crisis in US and UK Adults: Evidence From Two Population-based Longitudinal Studies. [Google Scholar]
- Dave D., Friedson A.I., Matsuzawa K., Sabia J.J. When do shelter-in-place orders fight COVID-19 best? Policy heterogeneity across states and adoption time. Econ. Inq. 2020;59(1):29–52. doi: 10.1111/ecin.12944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day J.K., Fish J.N., Perez-Brumer A., Hatzenbuehler M.L., Russell S.T. Transgender youth substance use disparities: results from a population-based sample. J. Adolesc. Health. 2017;61:729–735. doi: 10.1016/j.jadohealth.2017.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietze P.M., Peacock A. Illicit drug use and harms in Australia in the context of COVID-19 and associated restrictions: anticipated consequences and initial responses. Drug Alcohol Rev. 2020;39:297–300. doi: 10.1111/dar.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas T.M., Ellis W., Litt D.M. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J. Adolesc. Health Care. 2020;67:354–361. doi: 10.1016/j.jadohealth.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop A., Lokuge B., Masters D., Sequeira M., Saul P., Dunlop G., Ryan J., Hall M., Ezard N., Haber P., Lintzeris N., Maher L. Challenges in maintaining treatment services for people who use drugs during the COVID-19 pandemic. Harm Reduct. J. 2020;17:26. doi: 10.1186/s12954-020-00370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmer T., Mepham K., Stadtfeld C. Students under lockdown: comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One. 2020;15 doi: 10.1371/journal.pone.0236337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochstatter K.R., Akhtar W.Z., Dietz S., Pe-Romashko K., Gustafson D.H., Shah D.V., Krechel S., Liebert C., Miller R., El-Bassel N., Westergaard R.P. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: experience from a pilot mHealth intervention. AIDS Behav. 2020;25(2):354–359. doi: 10.1007/s10461-020-02976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson S.E., Garnett C., Shahab L., Oldham M., Brown J. medRxiv; 2020. Association of the Covid-19 Lockdown With Smoking, Drinking, and Attempts to Quit in England: an Analysis of 2019-2020 Data. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D.H., Janulis P., Mustanski B. Predictors of correspondence between self-reported substance use and urinalysis screening among a racially diverse cohort of young men who have sex with men and transgender women. Addict. Behav. 2019;88:6–14. doi: 10.1016/j.addbeh.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Bai H. Forward and backward continuation ratio models for ordinal response variables. J. Mod. Appl. Stat. Methods. 2020;18:4. [Google Scholar]
- Marsden J., Darke S., Hall W., Hickman M., Holmes J., Humphreys K., Neale J., Tucker J., West R. Mitigating and learning from the impact of COVID‐19 infection on addictive disorders. Addiction. 2020;115:1007–1010. doi: 10.1111/add.15080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay D., Asmundson G.J.G. COVID-19 stress and substance use: current issues and future preparations. J. Anxiety Disord. 2020;74 doi: 10.1016/j.janxdis.2020.102274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melamed O.C., Hauck T.S., Buckley L., Selby P., Mulsant B.H. COVID-19 and persons with substance use disorders: inequities and mitigation strategies. Subst. Abus. 2020;41:286–291. doi: 10.1080/08897077.2020.1784363. [DOI] [PubMed] [Google Scholar]
- Mustanski B., Garofalo R., Emerson E.M. Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual, and transgender youths. Am. J. Public Health. 2010;100:2426–2432. doi: 10.2105/AJPH.2009.178319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B., Johnson A.K., Garofalo R., Ryan D., Birkett M. Perceived likelihood of using HIV pre-exposure prophylaxis medications among young men who have sex with men. AIDS Behav. 2013;17:2173–2179. doi: 10.1007/s10461-012-0359-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B., Morgan E., D’Aquila R., Birkett M., Janulis P., Newcomb M.E. Individual and network factors associated with racial disparities in HIV among young men who have sex with men: results from the RADAR cohort study. J. Acquired Immune Deficiency Syndr. 2019;80(1):24–30. doi: 10.1097/QAI.0000000000001886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B., Ryan D.T., Newcomb M.E., Richard T.D., Matson M. Very high HIV incidence and associated risk factors in a longitudinal cohort study of diverse adolescent and young adult men who have sex with men and transgender women. AIDS Behav. 2019;24:1975–1996. doi: 10.1007/s10461-019-02766-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radfar S.R., De Jong C.A.J., Farhoudian A., Ebrahimi M., Rafei P., Vahidi M., Yunesian M., Kouimtsidis C., Arunogiri S., Massah O., Others . medRxiv; 2020. Reorganization of Substance Use Treatment and Harm Reduction Services During the COVID-19 Pandemic: A Global Survey. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno J.P., Williams N.D., Gattamorta K.A. LGBTQ populations: psychologically vulnerable communities in the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy. 2020;12(S1):S239–S242. doi: 10.1037/tra0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler M.S., Stein B.D., Collins R.L. Differences in substance use disparities across age groups in a national cross-sectional survey of lesbian, gay, and bisexual adults. LGBT Health. 2019;6:68–76. doi: 10.1089/lgbt.2018.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L., Steinhoff A., Bechtiger L., Murray A.L., Nivette A., Hepp U., Ribeaud D., Eisner M. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020:1–10. doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks T.J., Jones S.S., Sauermilch D., Benedict M., Adebayo T., Cain D., Simpson K.N. Evaluating the impact of COVID-19: a cohort comparison study of drug use and risky sexual behavior among sexual minority men in the USA. Drug Alcohol Depend. 2020 doi: 10.1016/j.drugalcdep.2020.108260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swann G., Bettin E., Clifford A., Newcomb M.E., Mustanski B. Trajectories of alcohol, marijuana, and illicit drug use in a diverse sample of young men who have sex with men. Drug Alcohol Depend. 2017;178:231–242. doi: 10.1016/j.drugalcdep.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xuereb S., Kim H.S., Clark L., Wohl M.J.A. 2020. Substitution Behaviors Among Casino Gamblers During COVID-19 Precipitated Casino Closures. [DOI] [Google Scholar]