Abstract
Objectives:
Evaluate fall risk with the Short Physical Performance Battery (SPPB) and examine its application within the Stopping Elderly Accidents, Deaths, and Injuries (STEADI) tool advocated by the Centers for Disease Control.
Design:
Prospective longitudinal cohort study.
Setting and participants:
417 community-dwelling adults aged 65+ at risk for mobility decline, recruited from 9 primary care practices.
Methods:
The SPPB, a three-part performance-based test (gait time, chair stand, and balance) was assessed at baseline. Previously established cutpoints were used to categorize participant scores into three groups: low, middle, and best performers. Self-reported falls were assessed in-person at baseline and via phone interviews quarterly for four years. Multivariable negative binomial regression models were used to evaluate the relationship of the SPPB and each of its three components with fall rates over one and four years of follow-up. Additional analyses were stratified by fall risk screen status (+/−) based on self-reported fall history and balance self-efficacy using an adapted STEADI model.
Results:
Participants had median age 76 years [IQR 70-82] and were 67.2% female with mean baseline SPPB 8.7 ± 2.3. Poor performance on the SPPB and on each of its three components independently predicted higher fall risk in the first year. After four years, the low total baseline SPPB (RR 1.53; CI 1.09-2.17) and gait time performances (RR 1.61; CI 1.07-2.41) predicted higher fall risk. After stratifying the sample according to the STEADI model, we observed the highest one-year fall risk among those with a (+) fall risk screen who also scored lowest on the SPPB.
Conclusions and Implications:
The SPPB is a performance measure with clinical utility for fall risk stratification over one and four years of follow-up among older adults. It shows promise as a complement to the STEADI guidelines, but its full benefits should be confirmed within a larger study.
Keywords: SPPB, STEADI, performance measure, fall, geriatric assessment
Brief Summary
In this prospective cohort study, we demonstrate that the short physical performance battery (SPPB) is a useful tool for fall risk stratification of community dwelling, older adults at risk for mobility decline.
INTRODUCTION
Medicare mandates annual screening of older patients for preventable health risks. One common focus of these assessments is falls. The Stopping Elderly Accidents, Deaths, and Injuries (STEADI) tool is recommended by the Center for Disease Control and Prevention (CDC) for fall risk screening and prevention in older primary care patients. The STEADI tool was developed from consensus work; its application in prospective clinical studies is more limited.1-3
The STEADI guidelines advocate inquiring about fear of falling, feelings of unsteadiness, and fall history in the past year. Next, they recommend checking for orthostatic hypotension and evaluating three aspects of physical performance. Notably, the three physical performance measures assess similar functional domains as the Short Physical Performance Battery (SPPB) (walking task, chair stand, and balance test).
Physical performance measures have generally demonstrated a strong ability to predict falls; however, this has largely been based upon retrospective studies rather than prospective studies.4 The Berg Balance Scale (BBS), Timed Up and Go (TUG), and 5 Times Sit To Stand (5TSTS) have both retrospective and prospective evidence to support them.5-8 The SPPB is a three-part quick and objective physical function test with excellent test-retest reliability, predictive validity, and clinical applicability with defined clinically important difference values.9-11 It is distinguished from these other fall assessments and advocated for use in geriatric assessments because of its predictive validity for other important adverse health outcomes including all-cause mortality, disability, hospitalization, and institutionalization.12-14 Although the SPPB has predictive ability for in-hospital falls, prospective evidence for the SPPB test at predicting falls among community-dwelling older primary care patients is less clear.15 Practically speaking, given its unique ability to predict other important fall outcomes, demonstration that the SPPB is predictive of falls may strengthen its advocacy for widespread use in clinical settings.
We aimed to evaluate the association between the SPPB and its three components with falls over 1 and 4 years of follow-up and hypothesized that the worst SPPB total score would be associated with higher fall risk. As an exploratory analysis, we also evaluated whether the SPPB contributed to fall risk stratification in the context of the STEADI recommendations.
METHODS
Participants
We analyzed a prospective cohort study of 430 community-dwelling older adults, which was designed to identify modifiable risk factors for decline in mobility skills. The Institutional Review Board approved the study, and participants provided written informed consent. Study details are published.16 Participants were recruited from 9 primary care practices. Inclusion criteria were age ≥65 years, difficulty or task modification with walking one-half mile and/or climbing 1 flight of stairs. Exclusion criteria were major surgery or myocardial infarction in the prior 6 months, Mini Mental State Exam (MMSE) score <18, and SPPB score <4. In-person assessments were conducted at baseline and annually for 2 years. Quarterly phone calls were conducted for 4 years after baseline. Out of 430 participants enrolled, only those with complete baseline data were included in the analyses (n=417). Missing baseline characteristics included Body Mass Index (BMI) (n=1), Physical Activity Scale for the Elderly (PASE) (n=1), vision (n= 6), psychotropic drug use (n=2), and Activities-Specific Balance Confidence (ABC) scale (n=3).
Characteristics
Baseline demographics and clinical characteristics linked to falls included in this analysis were age, gender, race, education, number of comorbid conditions, visual impairment, cognition, BMI, psychotropic medications, physical activity, depression, pain, and self-efficacy. Number of comorbid conditions was assessed using a validated self-report questionnaire.17 Comorbid conditions included heart disease, hypertension, lung disease, diabetes, ulcer or stomach disease, kidney disease, liver disease, anemia or other blood disease, cancer, osteoarthritis, back pain, and rheumatoid arthritis. Visual impairment was defined as the inability to correctly read the 20/50 line of the Snellen eye chart from 20 feet (with corrective vision used for distances).18 Cognition was assessed using the Mini Mental State Exam (MMSE).19 BMI was calculated as body weight in kilograms divided by height in meters squared (kg/m2). Any medications classified under the Iowa Drug Information Service (IDIS) as psychotherapeutic agents or anxiolytics were characterized as psychotropic drugs. Physical activity was measured using the PASE; higher scores indicate greater activity.20 Depressive symptoms were measured with the Patient Health Questionnaire 9 (PHQ-9); depression was classified as any score ≥10.21 Pain was measured with the Brief Pain Inventory (BPI), a validated measure of non-malignant pain.22 Balance self-efficacy was measured using the ABC scale, a validated self-report measure associated with fall risk with scores <67 out of 100 indicating increased risk.23
Falls
At baseline, one-year fall history was assessed. At baseline and follow-up assessments, falls were defined as unintentionally coming to rest on the ground or other lower level, not as a result of a major intrinsic event (e.g. myocardial infarction, stroke, seizure), or an overwhelming hazard (e.g. hit by vehicle).24 During quarterly phone calls, participants were asked “Have you fallen to the ground in the past 3 months?” and “If so, how many times?” In the four years of quarterly follow-up, 91% completed a quarterly assessment during the first year (90% female, 94% male, p=0.20), 85% during the second year (83% female, 88% male, p=0.13), 77% during the third year (77% female, 77% male, p=0.99), and 54% during the fourth year (57% female, 50% male, p=0.17).
Short Physical Performance Battery
Two study personnel were trained in SPPB assessment and audited by the same trainer for accurate execution. At baseline, all participants completed the SPPB (ICC 0.81), which consists of 3 timed components: 1) a 4-meter usual pace walk, 2) a five-repetition chair stand without using one’s arms, and 3) a progressive test of standing balance.10 Study personnel demonstrated each component ahead of participant testing. The walking component was performed by the participant two times and the best trial was used. Times from each component were scored from 0-4, with higher scores corresponding to better performance. We characterized these scores in subgroups as “low,” “low-middle,” “high-middle,” and “best” performers.11 Gait time performance groups “low” and “low-middle” were combined in to one “low performers” group in this study due to small sub-group numbers. When all three component scores were added together, final total SPPB scores ranged between 4 and 12, with 4-6 representing the low, 7-9 the middle, and 10-12 the best performances based on previously established clinical cutpoints.11
Stopping Elderly Accidents, Deaths, and Injuries
We employed an adapted version of the STEADI algorithm to stratify participants at baseline into positive and negative fall risk screen groups based on two criteria: self-reported fall history and balance self-efficacy. At baseline, participants were asked “How many times have you fallen to the ground in the past year?” and were considered positive for this criterion if they reported 1 or more falls. Participants were characterized as being in the (+) fall screen group if they had a positive prior fall history or poor balance self-efficacy (baseline ABC score <67) and being in the (−) fall screen group if they fulfilled neither of these criteria.
Statistical Analysis
Participants were characterized by SPPB total score; group differences in baseline characteristics were analyzed with chi-square tests for categorical variables and Kruskall-Wallis tests for continuous variables. Rate ratios (RR) and 95% CI from multivariable-adjusted negative binomial regression models were used to evaluate the relationships of total SPPB score categories and SPPB component score categories with fall rates over one and four years of follow-up. An offset variable for log total years of follow-up was used. To assess one-year performance of the SPPB with stratification by the adapted STEADI, RR and 95% CI were calculated among the (+) fall screen subcohort and the (−) fall screen subcohort, separately. For each analysis, the highest performers served as the reference group. Models were initially adjusted for demographic variables (age, gender, race, and education). Then, iterative multivariable models were constructed using baseline characteristics that had confounding potential, based upon the literature and statistical criteria for association with the outcome (p<0.1). Cumulative four-year fall rates were derived directly and adjusted for age, gender, race, and education. Analyses were performed using SAS version 9.4.
RESULTS
As shown in Table 1, participants were 67.2% female, 82.3% white, and had a median age of 76 years. The mean baseline SPPB score was 8.7 ± 2.3. The low SPPB performers were older and manifested greater comorbidity, more visual impairment, and lower scores on the MMSE. They were also more likely to be on one psychotropic drug, to have lower physical activity, more chronic pain, to have fallen in the past year, and to have poor falls self-efficacy. Other baseline characteristics did not significantly differ between SPPB performance groups (Table 1).
Table 1.
Baseline Participant Characteristics by SPPB Performance
| Demographics with Value Ranges |
Overall (n=417) |
SPPB* Low (n=83) |
SPPB* Middle (n=153) |
SPPB Best* (n=181) |
p – value† |
|---|---|---|---|---|---|
| No. (%) of Participants or Median (IQR) Value | |||||
| Age (years) (65-96) | 76 (70-82) | 80 (73-85) | 76 (71-82) | 74 (70-80) | <0.0001 |
| Female Gender | 280 (67.2%) | 57 (68.7%) | 98 (64.1%) | 125 (69.1%) | 0.60 |
| White Race | 343 (82.3%) | 63 (76.0%) | 129 (84.3%) | 151 (83.4%) | 0.23 |
| Education | |||||
| < High School | 53 (12.7%) | 13 (15.7%) | 20 (13.1%) | 20 (11.1%) | |
| High School Graduate | 125 (30.0%) | 32 (38.6%) | 40 (26.1%) | 53 (29.3%) | 0.33 |
| College Graduate | 135 (32.4%) | 24 (28.9%) | 52 (34.0%) | 59 (32.6%) | |
| Graduate or Professional School | 104 (24.9%) | 14 (16.9%) | 41 (26.8%) | 49 (27.1%) | |
| Chronic Condition | 4 (2-5) | 4 (3-6) | 4 (3-6) | 3 (2-5) | <0.0001 |
| Count | |||||
| Visual Impairment‡ | 18 (4.3%) | 8 (9.6%) | 6 (3.9%) | 4 (2.2%) | 0.02 |
| Cognition§ (18-30) | 28 (26-29) | 27 (26-29) | 28 (26-29) | 28 (27-29) | 0.0001 |
| Body Mass Index∥ | |||||
| <25 | 98 (23.5%) | 23 (27.7%) | 35 (22.9%) | 40 (22.1%) | |
| 25-29.9 | 163 (39.1%) | 34 (41.0%) | 56 (36.6%) | 73 (40.3%) | 0.66 |
| ≥30 | 156 (37.4%) | 26 (31.3%) | 63 (40.5%) | 68 (37.6%) | |
| Psychotropic Drugs | |||||
| None | 290 (69.5%) | 47 (56.6%) | 105 (68.6%) | 138 (76.2%) | |
| Single Agent | 73 (17.5%) | 20 (24.1%) | 29 (19.0%) | 24 (13.3%) | 0.03 |
| 2+ Agents | 54 (13.0%) | 16 (19.3%) | 19 (12.4%) | 19 (10.5%) | |
| Physical Activity** (36.4 - 636.9) | 166 (126-212) | 130.1 (110-167) | 165.0 (127-200) | 180.4 (141-246) | <0.0001 |
| Depression†† (0-27) | 16 (3.8%) | 7 (8.4 %) | 4 (2.6%) | 5 (2.8%) | 0.05 |
| Pain‡‡ (0-10) | 2.3 (1.0-3.5) | 2.8 (1.8-4.0) | 2.5 (1.3-4.3) | 2.0 (0.8-3.3) | 0.0004 |
| Fell in Past Year | 176 (42.2%) | 47 (56.6%) | 62 (40.5%) | 67 (37.0%) | 0.01 |
| Self Efficacy§§ (0-100) | 79 (67-89) | 65 (51-74) | 76 (68-88) | 86 (75-93) | <0.0001 |
Note. SPPB=Short Physical Performance Battery.
SPPB Low Performance Group Total Score 4-6, Middle Performance Group Total Score 7-9, and Best Performance Group Total Score 10-12.
Chi Square and Kruskal-Wallis H test for p-values reflect overall differences between SPPB categories.
Visual impairment defined inability to successfully read the 20/50 line of the Snellen eye chart.
Cognition measured with the Mini Mental State Exam (MMSE).
Body mass index is calculated as weight in kilograms divided by height in meters squared.
Physical activity measured using the Physical Activity Scale for the Elderly.
Depression characterized as a Patient Health Questionnaire-9 (PHQ-9) scores ≥10.
Pain measured with the Brief Pain Inventory.
Balance self efficacy measured with the Activities-Specific Balance Confidence Scale (ABC).
During the first year of follow up, 53% (n=222) reported falling at least once. After adjustment for demographics, number of comorbid conditions, and fall risk factors, compared to those with high performance, older adults in the low SPPB performance group (RR 3.03; CI 2.04-4.49), and in the low performance groups for gait (RR 2.90; CI 1.85-4.55), chair stand (RR 1.77; CI 1.11-2.84), and balance (RR 2.86; CI 1.82-4.50), each manifested the highest fall risk over the first year of follow-up. The low-middle performers on the chair stand (RR 1.70; CI 1.07-2.70) and balance tests (RR 1.68; CI 1.14-2.49) also had significantly higher fall risk over the first year of follow-up compared to those in the high performance groups, while the middle SPPB and gait time performance groups had borderline associations with fall risk (Figure 1).
Figure 1.
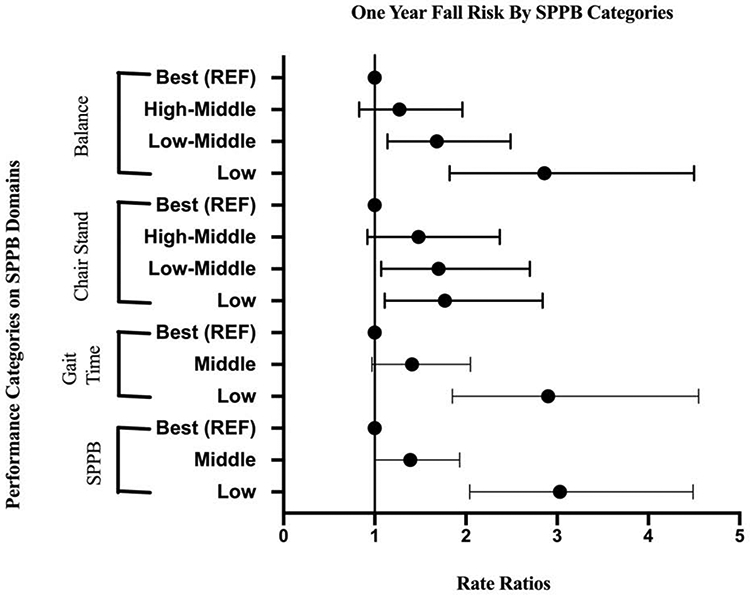
One Year Fall Risk By SPPB Categories
Rate ratios and 95% confidence intervals from negative binomial regression models, adjusted for age, gender, race, education level, number of comorbid conditions, BMI, psychotropic drugs, physical activity, pain, and depression
*Short Physical Performance Battery (SPPB) Low Performance Group Total Score 4-6, Middle Performance Group Total Score 7-9, and Best Performance Group used as reference (REF) Total Score 10-12.
†Gait Time Low Performance Group walked 4 meters in ≥6.21 seconds, Middle Performance Group in 4.82-6.20 seconds and Best Performance Group in <4.82 seconds.
‡Chair Stand Low Performance Group unable to stand or completed 5 stands >16.7 seconds, Low-Middle Performance Group in 13.7-16.6 seconds, High-Middle Performance Group in 11.2-13.6 seconds, and Best Performance Group in <11.2 seconds.
§Balance Test Low Performance Group performed Side-by-Side Stand <10 seconds, Low-Middle Performance Group Semi Tandem Stand <10 seconds, High-Middle Performance Group Full Tandem Stand 3-9 seconds, and Best Performance Group Full Tandem Stand ≥10 seconds.
Table 2 expands the follow up time frame to four years and provides both fall rates as well as rate ratios. One or more falls was reported among 310 participants (74%) during the four-year follow-up. The low SPPB, gait time, chair stand, and balance test performers had the highest cumulative fall rates over four years. The low-middle balance test performers also had statistically significant higher four-year fall rates. Within multivariable models, the low SPPB performers, (RR 1.53; CI 1.09-2.17), and gait time performers, (RR 1.61; CI 1.07-2.41), had higher rate ratios over four years of follow-up in comparison to the reference groups. The lowest chair stand and balance test performers did not have significantly higher 4-year fall risk after adjusting for fall risk factors compared to those in the highest performance groups.
Table 2.
Four-Year Fall Rates and Fall Risk by SPPB Performance Categories
| Performance Categories |
n | Number of Falls |
Number of Person- Years |
Fall Rate (95% CI)* |
Fall Risk (95% CI)† |
|---|---|---|---|---|---|
| SPPB Performance | |||||
| Low | 83 | 470 | 235 | 2.10 (1.61-2.76) | 1.53 (1.09-2.17) |
| Middle | 153 | 567 | 484 | 1.17 (0.96-1.43) | 1.22 (0.92-1.60) |
| Best | 181 | 519 | 603 | 0.85 (0.70-1.03) | 1.00 (REF) |
| Gait Time Performance | |||||
| Low | 48 | 329 | 137 | 2.61 (1.82-3.73) | 1.61 (1.07-2.41) |
| Middle | 107 | 379 | 322 | 1.26 (0.98-1.62) | 0.91 (0.68-1.23) |
| Best | 262 | 848 | 864 | 0.95 (0.81-1.24) | 1.00 (REF) |
| Chair Stand Performance | |||||
| Low | 121 | 500 | 358 | 1.47 (1.16-1.86) | 0.98 (0.67-1.42) |
| Low-Middle | 114 | 426 | 362 | 1.19 (0.93-1.51) | 1.04 (0.73-1.49) |
| High-Middle | 110 | 392 | 364 | 1.06 (0.82-1.36) | 0.93 (0.65-1.33) |
| Best | 72 | 238 | 238 | 1.02 (0.75-1.39) | 1.00 (REF) |
| Balance Test Performance | |||||
| Low | 50 | 241 | 152 | 1.67 (1.17-2.37) | 1.37 (0.93-2.03) |
| Low-Middle | 98 | 443 | 295 | 1.61 (1.24-2.09) | 1.47 (1.07-2.03) |
| High-Middle | 69 | 295 | 222 | 1.35 (1.00-1.82) | 1.38 (0.98-1.95) |
| Best | 200 | 577 | 654 | 0.86 (0.72-1.04) | 1.00 (REF) |
Fall rates and 95% confidence intervals derived using the direct method, adjusted for age, gender, race, and education level.
Rate ratios and 95% confidence intervals from negative binomial regression models, adjusted for age, gender, race, education level, number of comorbid conditions, BMI, psychotropic drugs, physical activity, pain, and depression.
To evaluate the SPPB within STEADI guidelines, our adapted version was modeled with one year of falls (Table 3). Balance self-efficacy screening was missing for one participant and they were left out of the model. Two hundred twenty-six participants were noted to have a (+) fall screen with a (+) fall history or poor balance self-efficacy. When compared to the (−) fall screen group, the (+) fall screen group had a significantly high fall rate (RR 10.05; CI 7.03-14.37).
Table 3.
Fall Risk Stratification by Fall Screen and SPPB Performance
| − Fall Screen (n=190) | + Fall Screen (n=226) | ||||
|---|---|---|---|---|---|
| − Fall History or Good Balance Self Efficacy* |
+ Fall History or Poor Balance Self Efficacy* |
||||
| REFERENCE | 10.05 [7.03-14.37] | ||||
| SPPB Low Performers† (n=19) | SPPB Middle Performers† (n=72) | SPPB Best Performers† (n=99) | SPPB Low Performers† (n=64) | SPPB Middle Performers† (n=80) | SPPB Best Performers† (n=82) |
| 1.35 [0.39-4.71] | 1.23 [0.56-2.70] | REFERENCE | 1.48 [1.03-2.12] | 1.21 [0.88-1.68] | REFERENCE |
Poor self-efficacy was categorized as an Activities Balance Specific Confidence Scale <67 (out of 100).
Short Physical Performance Battery (SPPB) Low Performance Group Total Score 4-6, Middle Performance Group Total Score 7-9, and Best Performance Group used as reference (REF) Total Score 10-12.
Rate ratios and 95% confidence intervals from negative binomial regression models, adjusted for age, gender, race, education level, comorbid conditions, BMI, psychotropic drugs, physical activity, pain, and depression
The largest SPPB groups were the best performers (score 10-12) regardless of a (+/−) fall screening at baseline. After adjusting for potential confounders, the (+) fall screen group with the worst SPPB performances had the highest risk of falls (RR 1.48; CI 1.03-2.12) compared to the best SPPB performers within this STEADI category. We did not observe an increased risk of falls according to SPPB group among those with a (−) fall screen.
DISCUSSION
The main finding of our study was that low scores on the SPPB and all three subcomponents predicted higher one-year fall risk. Further, over the four-year time period, low SPPB score and gait time predicted higher fall risk, including adjustment for other fall risk factors. Chair stand performance was not predictive of falls over 4 years. Within the adapted STEADI model we observed benefit of the SPPB at predicting one-year falls among those who screened positive for fall risk at baseline.
Evidence suggests that physical performance measures are an important method for predicting future falls.4 To our knowledge, this is the most robust prospective investigation evaluating the SPPB performance measure and its three components as predictors of falls among community-dwelling older primary care patients. The SPPB has been investigated in a large hospital cohort; however, much of the prior evidence for SPPB performance and falls has come from cross-sectional studies.9-15,25-27 Our findings suggest that primary care patients with total SPPB scores of 4-6 are at three times the risk for falls in the following year compared to those with high SPPB scores (10-12). Our findings contrast with an Italian population-based cohort study (n=561) that demonstrated total SPPB score did not predict fall risk after one year.12 This difference could likely be attributed to differences in the methods of falls ascertainment. Whereas we evaluate fall rates over time during quarterly phone calls, the aforementioned study asked participants to report whether they fell in the prior 12 months. Thus there was a one-year delay between the SPPB test and the fall assessment.
The STEADI guidelines advocate that clinicians prioritize a dynamic walking test over the balance and chair stand tests in evaluating fall risk; although their recommended walking test is the Timed Up and Go. Our findings support the recommendation of an assessment of dynamic walking given the most consistent predictor of fall risk in our cohort was gait time over 4 meters. It predicted a future fall over one and four years of follow up in those requiring ≥6.2 seconds to walk 4 meters.
Within our cohort, those at the lowest level of chair stand performance (unable or taking >16.7 seconds to perform) had the highest one-year fall risk. However, this relationship did not hold up over four years. Our chair stand findings complement a growing body of evidence suggesting that being unable to rise from a chair efficiently is an important marker for one-year fall outcomes.28 As for the SPPB balance component, our findings suggest that those unable to hold a side-by-side stance for 10 seconds (the worst category) are at the highest risk for falls in the following year while those unable to semi-tandem stand for 10 seconds (the low-middle category) had a higher four-year fall risk. This shows that short-term (one-year) fall risk can be predicted well by very poor balance, and that long-term (four-year) fall risk can be predicted by subtle, possibly pre-clinical, balance problems.
Our findings contribute to the overall growing body of evidence supporting the use of performance-based measures for fall risk stratification. While other measures such as the Berg Balance Scale, Timed Up and Go, and 5 Times Sit to Stand are predictive of falls, they are not predictive of other important adverse outcomes.5-8 In the case of the Berg Balance Scale it is less clinically practical (~20 minutes to complete), This study contributes prospective evidence for the SPPB in the community-dwelling older adult population with a follow-up timeframe up to four years. This is logical as the SPPB comprises three functional domains as advocated by the CDC within the STEADI guidelines. The CDC’s STEADI tool advocates screening older adults at primary care visits with the following three questions: 1) Have you fallen in the past year? 2) Do you feel unsteady when standing or walking? 3) Do you worry about falling? These questions have clinical importance and are well supported in the falls literature.29 In the STEADI algorithm, fall risk screening would stop in individuals that answer no to these questions. Our study differed in that all participants underwent performance testing with the SPPB thereafter. When we stratified our analysis based on the STEADI fall screen questions, several older adults with a (−) fall screen still performed poorly on the SPPB. This highlights that there are degrees of risk according to the SPPB, even among those with a (−) STEADI fall screen. It may make sense to consider use of physical performance testing earlier in the STEADI protocol. Previous studies suggest that using a combination of self-report and physical performance measures is critical for assessing older adult function, and our study corroborates that notion.30 These findings contribute to the growing body of evidence informing STEADI.
There are limitations to this study, which must be considered. Our study sample was a cohort of community dwelling older adults; findings may not be generalizable to other populations. As part of the protocol, falls were collected via quarterly phone calls and not by monthly fall calendars. Also, some participants could not be reached at each quarter. Together this may have led to an underestimation of fall numbers. Our adapted STEADI screening criteria did not include a question about “worry about falls”, although we did have the fall history question and a validated scale on balance self-efficacy. In addition, the study inclusion criteria already required that participants self-report difficulty or task modification with walking long distances. This may have caused our adapted STEADI criteria to be less discriminative at identifying participants upfront with a (+) fall screen. When analyzing fall risk stratified by STEADI fall screen status, we likely had limited statistical power to detect associations due to small numbers within groups. Larger studies are needed for definitive conclusions regarding STEADI and the optimal sequence and timing of performance-based testing in fall risk assessments.
CONCLUSION AND IMPLICATIONS
In summary, we demonstrated that the SPPB, and its components, independently stratify community dwelling older adults at risk for falls including confounders but not fall history in our models. Strengths of this study are the well-characterized cohort of older primary care patients and clinically relevant follow-up time frames of one and four years. Our results indicate that the SPPB is a promising screening tool for predicting future falls at an annual visit. Although we did not observe an increased risk of falls according to SPPB group among those with a (−) STEADI fall screen, our findings suggest that older adults with poor physical performance could be missed by this approach. Furthermore, this study shows that adding SPPB to a (+) STEADI fall screen provides improved fall risk prediction, which is an important finding. Future work should focus on applying the combination of self-reported fall screening and performance-based measures in larger and more representative samples of older adults using rigorous falls ascertainment methods.
Acknowledgements:
The authors wish to thank all participants for their involvement in the study, Laura Griffith Kurlinski, and other staff for their contributions to the data collection.
Funding Sources: This work was supported by the National Institute on Aging (R01 AG032052-03) and the National Center for Research Resources in a grant to the Harvard Clinical and Translational Science Center (1 UL1 RR025758-01); and in part by a National Institutes of Health K24 award (4K24HD070966-05).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Stevens JA, Phelan EA. Development of STEADI: a fall prevention resource for health care providers. Health Promot Pract. 2013;14(5):706–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lohman MC, Crow RS, DiMilia PR, Nicklett EJ, Bruce ML, Batsis JA. Operationalisation and validation of the Stopping Elderly Accidents, Deaths, and Injuries (STEADI) fall risk algorithm in a nationally representative sample. J Epidemiol Community Health. 2017;71(12): 1191–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crow RS, Lohman MC, Pidgeon D, Bruce ML, Bartels SJ, Batsis JA. Frailty Versus Stopping Elderly Accidents, Deaths and Injuries Initiative Fall Risk Score: Ability to Predict Future Falls. J Am Geriatr Soc. 2018;66(3):577–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lusardi MM, Fritz S, Middleton A, et al. Determining Risk of Falls in Community Dwelling Older Adults: A Systematic Review and Meta-analysis Using Posttest Probability. J Geriatr Phys Ther. 2017;40(1):1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LeClerc B, Begin C, Cadieux E, et al. A classification and regression tree for predicting recurrent falling among community-dwelling seniors using homecare services. Can J Public Health. 2009;100(4):263–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Brien K, Pickles B, Culham E. Clinical measures of balance in community-dwelling elderly female fallers and nonfallers. Physiother Can.1998;50(3): 212–217. [Google Scholar]
- 7.Tiedemann A, Shimada H, Sherrington C, et al. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing. 2008;37(4):430–435. [DOI] [PubMed] [Google Scholar]
- 8.Buatois S, Manckoundia P, Gueguen R, et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J Am Geriatr Soc. 2008;56(8):1575–1577. [DOI] [PubMed] [Google Scholar]
- 9.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and r esponsiveness in common physical performance measures in older adults. J Am Geriatr S oc. 2006;54(5):743–749. [DOI] [PubMed] [Google Scholar]
- 10.Mangione KK, Craik RL, McCormick AA, et al. Detectable changes in physical performance measures in elderly African Americans. Phys Ther. 2010;90(6):921–927. [DOI] [PubMed] [Google Scholar]
- 11.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minneci C, Mello AM, Mossello E, et al. Comparative study of four physical performance measures as predictors of death, incident disability, and falls in unselected older persons: the insufficienza Cardiaca negli Anziani Residenti a Dicomano Study. J Am Geriatr Soc. 2015;63 (1):136–141. [DOI] [PubMed] [Google Scholar]
- 13.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. [DOI] [PubMed] [Google Scholar]
- 14.Pavasini R, Guralnik J, Brown JC, et al. Short Physical Performance Battery and all-cause mortality: systematic review and meta-analysis. BMC Med. 2016;14(1):215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hars M, Audet MC, Herrmann F, et al. Functional Performances on Admission Predict In-Hospital Falls, Injurious Falls, and Fractures in Older Patients: A Prospective Study. J Bone Miner Res. 2018;33(5):852–859. [DOI] [PubMed] [Google Scholar]
- 16.Holt NE, Percac-Lima S, Kurlinski LA, et al. The Boston Rehabilitative Impairment Study of the Elderly: a description of methods. Arch Phys Med Rehabil. 2013;94(2):347–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49(2):156–163. [DOI] [PubMed] [Google Scholar]
- 18.Kaiser PK. Prospective evaluation of visual acuity assessment: a comparison of snellen versus ETDRS charts in clinical practice (An AOS Thesis). Trans Am Ophthalmol Soc. 2009;107:311–324. [PMC free article] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. [DOI] [PubMed] [Google Scholar]
- 20.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain. 2004;5(2):133–137. [DOI] [PubMed] [Google Scholar]
- 23.Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the activities-specific balance confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1998;53(4):M287–294. [DOI] [PubMed] [Google Scholar]
- 24.The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan Med Bull. 1987;34 Suppl 4:1–24. [PubMed] [Google Scholar]
- 25.Lauretani F, Ticinesi A, Gionti L, et al. Short-Physical Performance Battery (SPPB) score is associated with falls in older outpatients. Aging Clin Exp Res. 2018. [DOI] [PubMed] [Google Scholar]
- 26.Singh DK, Pillai SG, Tan ST, Tai CC, Shahar S. Association between physiological falls risk and physical performance tests among community-dwelling older adults. Clin Interv Aging. 2015;10:1319–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park WC, Kim M, Kim S, et al. Introduction of Fall Risk Assessment (FRA) System and Cross-Sectional Validation Among Community-Dwelling Older Adults. Ann Rehabil Med. 2019;43(1):87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shea CA, Ward RE, Welch SA, Kiely DK, Goldstein R, Bean JF. Inability to Perform the Repeated Chair Stand Task Predicts Fall-Related Injury in Older Primary Care Patients. Am J Phys Med Rehabil. 2018;97(6):426–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mänty M, Heinonen A, Viljanen A, et al. Self-reported preclinical mobility limitation and fall history as predictors of future falls in older women: prospective cohort study. Osteoporos Int. 2010;21(4):689–693. [DOI] [PubMed] [Google Scholar]
- 30.Bean JF, Olveczky DD, Kiely DK, LaRose SI, Jette AM. Performance-based versus patient-reported physical function: what are the underlying predictors? Phys Ther. 2011;91(12):1804–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]


