Abstract
Background:
The combination of lateral extra-articular tenodesis (LET) with primary single-bundle anterior cruciate ligament (ACL) reconstruction (ACLR) remains controversial.
Purpose:
To determine whether the combination of LET with single-bundle ACLR provides greater control of anterolateral rotatory instability and improved clinical outcomes compared with ACLR alone.
Study Design:
Systematic review; Level of evidence, 2.
Methods:
PubMed, Embase, and the Cochrane Central Register of Controlled Trials databases were searched between inception and July 1, 2020. Level 1 or 2 randomized controlled trials that compared isolated single-bundle ACLR with combined LET with ACLR were included. Data were meta-analyzed for the primary outcome measure of knee stability and the secondary outcome measures of patient-reported outcome scores, return to sports, and graft failure. Dichotomous variables were presented as relative risks (RRs), and continuous variables were presented as mean differences (MDs) and standardized MDs (SMDs).
Results:
A total of 6 studies involving 1010 patients were included. Pooled data showed that the ACLR+LET group had a lower incidence of the pivot shift (RR, 0.56 [95% CI, 0.45 to 0.69]; P < .00001), a higher postoperative activity level (MD, 0.47 [95% CI, 0.15 to 0.78]; P = .004), and a lower risk of graft failure (RR, 0.35 [95% CI, 0.21 to 0.59]; P < .00001) than did the ACLR group. However, there were no statistically significant differences in primary outcomes including positive Lachman test findings (RR, 0.76 [95% CI, 0.48 to 1.21]; P = .26) or side-to-side differences (SMD, –0.43 [95% CI, –0.95 to 0.09]; P = .11) or in secondary outcomes including International Knee Documentation Committee scores (SMD, 0.25 [95% CI, –0.06 to 0.56]; P = .11) or Lysholm scores (SMD, 0.28 [95% CI, –0.06 to 0.62]; P = .11). Although the overall rate of return to sports was not significantly different between the groups (RR, 0.97 [95% CI, 0.90 to 1.03]; P = .33), the activity level was higher in the ACLR+LET group.
Conclusion:
The addition of LET to primary single-bundle ACLR produced greater knee stability, a higher activity level, and a lower incidence of graft failure than did ACLR alone. There may be a role for adding LET to ACLR for the treatment of ACL injuries.
Keywords: Knee, lateral extra-articular tenodesis, anterior cruciate ligament reconstruction, anterolateral rotatory instability, pivot shift
Intra-articular anterior cruciate ligament (ACL) reconstruction (ACLR) is considered an effective treatment for ACL injuries. Despite the rapid evolution of ACLR techniques, an increasing subset of patients has residual anterolateral rotatory instability (ALRI) postoperatively.17,35,39,44 Such instability is usually assessed using the pivot-shift test. Residual pivot shift after ACLR is negatively correlated with functional outcomes and results in a higher risk of meniscal and cartilage injuries, graft ruptures, and osteoarthritis.5,10,26,28,37
Before intra-articular ACLR became the primary treatment for an ACL-deficient knee, isolated lateral extra-articular tenodesis (LET) was used as a solution to rotational instability.6,15 This approach became popular in the 1980s and was adopted by a number of surgeons as concomitant augmentation in ACLR,9,53 but it then fell out of favor because of unsatisfactory clinical outcomes27,47 and was eventually superseded by intra-articular ACLR. However, with increasing failure rates after single-bundle ACLR and intractable cases of ALRI continuously reported in recent studies,30,31 LET has regained its favor as an additional procedure for potentially reducing the rate of reinjuries and residual instability after ACLR.
Several randomized controlled trials (RCTs) have compared the combination of LET and ACLR with isolated ACLR,1,4,8,18,19,45,46,51 but many of these trials contained relatively small cohorts and demonstrated inconsistent outcomes. For example, 1 multicenter RCT18 reported that the addition of LET to single-bundle ACLR with a hamstring tendon autograft results in a statistically significant, clinically relevant reduction in the risk of graft ruptures and persistent rotatory laxity. However, this conclusion was contradicted by several other RCTs.4,8,45 Another study8 indicated a risk of lateral compartment osteoarthritis after 19 years when LET was combined with ACLR, but 2 other European studies with follow-up periods of over 20 years did not demonstrate an increased rate of osteoarthritis development with the addition of LET.36,52
Several systematic reviews with meta-analyses have also attempted to address which treatment plan is most beneficial.12,21,43,48 These meta-analyses produced inconsistent conclusions, and the quality of the included RCTs was low and contained methodologic shortcomings, characterized by high heterogeneity and a lack of outcome indicators.
To our knowledge, no quantitative meta-analysis on overall clinical outcomes has been conducted. These gaps in the literature make it unclear whether LET during primary ACLR can reduce the risk of postoperative ALRI. Thus, we conducted a meta-analysis to evaluate whether LET combined with ACLR could improve overall knee function with regard to knee stability, patient-reported outcome scores, the incidence of graft failure, and the ability to return to sports.
Methods
Search Strategy and Inclusion Criteria
This meta-analysis was conducted according to the 2010 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.33 A systematic review of the literature was performed using the electronic databases of PubMed, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) between inception and July 1, 2020. Two reviewers (Y.M. and K.Z.) independently searched each database using the following keywords: (“lateral extra-articular tenodesis” OR “lateral extra-articular procedure” OR “lateral augmentation procedures” OR “lateral extra-articular plasty” OR “lateral extra-articular sling”) AND (“knee”). The detailed search strategy is provided in the Appendix. A manual search of references from the included articles was also conducted to ensure the retrieval of articles on related topics.
Titles and abstracts were screened initially for relevance, and potentially eligible articles were read in their entirety. Disagreements on study selection were resolved through a discussion and consensus between the 2 reviewers. Only studies published in English were reviewed. The inclusion criteria were as follows: (1) level 1 or 2 prospective studies or RCTs that compared the combination of LET and ACLR with isolated ACLR; (2) single-bundle ACLR performed using autogenous grafts; (3) knee laxity measured using the pivot-shift test, Lachman test, and arthrometric side-to-side difference; (4) at least 1 postoperative patient-reported outcome score measured using either the International Knee Documentation Committee (IKDC) subjective score or Lysholm score; (5) rate of return to sports (return to preinjury levels) reported; (6) cases of graft failure or ruptures recorded; and (7) mean follow-up of at least 2 years. Studies were excluded if they involved any of the following: (1) ACLR performed using double-bundle techniques, (2) allogeneic or artificial grafts used for ACLR or LET, (3) patients with multiligament injuries, (4) concomitant surgery that affected knee function (eg, alignment knee surgery or fracture surgery), or (5) revision surgery. Biomechanical or animal studies as well as reviews were excluded.
Data Extraction
The same 2 reviewers independently extracted the following data from included studies: name of the first author, publication year, number of participants enrolled, mean age of participants, number of patients lost to follow-up, methods of randomization, methods of assessor/participant blinding, length of follow-up, ACLR technique, LET technique, and outcome measures. Disagreements on data extraction were resolved through a discussion. The primary outcome was knee stability, defined as follows: (1) positive knee ALRI (pivot-shift test grade ≥2), (2) positive anterior laxity (Lachman test grade ≥2), and (3) KT-1000/-2000 arthrometer side-to-side difference in anterior tibial translation between the injured and noninjured knees.
Secondary outcomes included patient-reported outcome scores: the IKDC subjective score, ranging from 0 (total limitation) to 100 (no limitations),24 and the Lysholm score, ranging from 0 (no function) to 100 (best function).7 The rate of return to sports was defined as the proportion of patients able to return to their preinjury sports of choice. Activity level was assessed at last follow-up using the Tegner scale, with 0 denoting disability and 10 denoting competitive sports,7 and the Marx scale, with 0 denoting exercise <1 time per month and 4 denoting exercise >4 times a week.32 Graft failure was defined as a postoperative rupture of the graft that was confirmed using either magnetic resonance imaging or an arthroscopic examination and required revision surgery.
Quality Assessment
Moreover, the 2 reviewers independently assessed the methodologic quality of the selected studies using the Cochrane Collaboration risk of bias tool,22 which comprises the following 7 items: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. Each of the included studies was rated as having a low, unclear, or high risk of bias. Disagreements were resolved through a discussion.
Statistical Analysis
Data analyses were performed using Review Manager Version 5.3 (Cochrane Collaboration). The relative risk (RR) and its corresponding 95% CI were calculated for dichotomous data including the pivot-shift test, Lachman test, and overall rate of return to sports. Standardized mean differences (SMDs) and 95% CIs were calculated for continuous variables of the IKDC subjective score, Lysholm score, and side-to-side difference. Activity levels were compared using mean differences (MDs) and 95% CIs. Heterogeneity across individual studies was assessed using the I 2 statistic, with I 2 >50% considered significant. If heterogeneity was significant, data were analyzed using a random-effects model; otherwise, a fixed-effects model was applied. Publication bias was not formally tested because the number of included studies was too small.
Results
Search Results
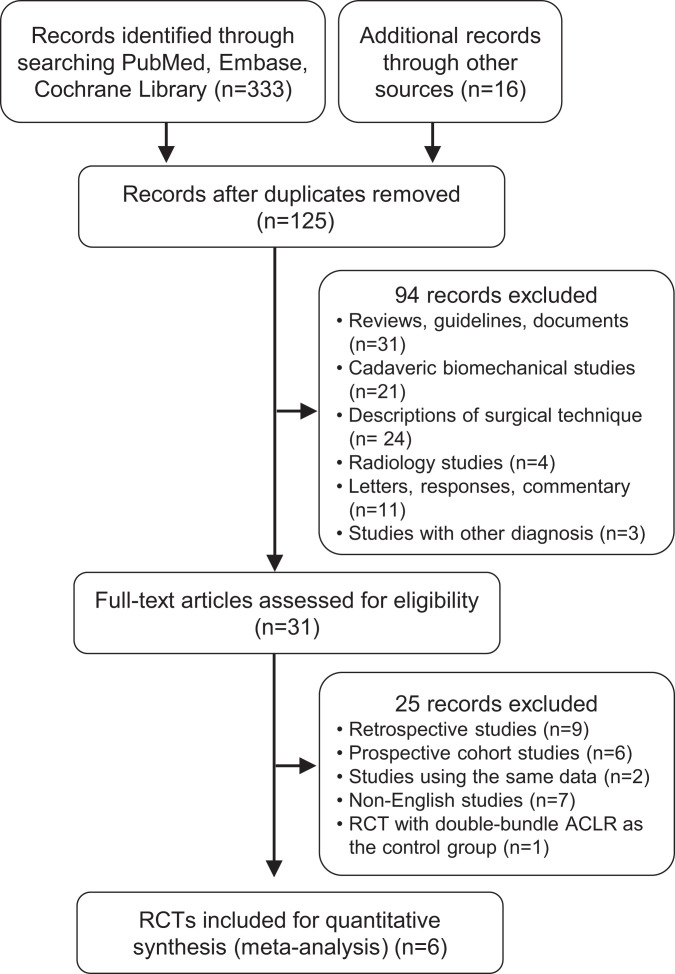
Our initial search of the online databases retrieved a total of 333 articles (Figure 1). After the screening and removal of duplicate articles, 125 remained. Titles and abstracts were reviewed, and the full text of 31 articles was examined. Ultimately, 6 RCTs4,8,18,45,46,51 were included in this review (Table 1).
Figure 1.
Flowchart of study search and selection. ACLR, anterior cruciate ligament reconstruction; RCT, randomized controlled trial.
Table 1.
Characteristics of Included Randomized Controlled Trialsa
| Lead Author (Year) | No. of Patients | Patient Age,b y | Surgical Technique | Follow-up,b y | Patients Lost to Follow-up, n (%) | |
|---|---|---|---|---|---|---|
| ACLR | LET | |||||
| Getgood18 (2020) | ACLR: 298; ACLR+LET: 291 | ACLR: 18.8 (14-25); ACLR+LET: 19.1 (14-25) | HA | Modified Lemaire | 2 | 29 (4.9) |
| Castoldi8 (2020) | ACLR: 61; ACLR+LET: 60 | Inclusion: 26.0 (15-40); last follow-up: 46.0 (35-59) | BPTB | Modified Lemaire | 19.4 (19.0-20.2) | 41 (33.9) |
| Trichine45 (2014) | ACLR: 60; ACLR+LET: 60 | ACLR: 27.7 (19-40); ACLR+LET: 28.6 (21-30) | BPTB | Modified Lemaire | 1.9 (0.5-5.2) | 13 (10.8) |
| Vadalà46 (2013) | ACLR: 32; ACLR+LET: 28 | ACLR: 28 (15-40); ACLR+LET: 26 (15-40) | HA | Modified Cocker-Arnold | 3.7 (3.0-4.2) | 5 (8.3) |
| Zaffagnini51 (2006) | ACLR: 25; ACLR+LET: 25 | ACLR: 31.3 (26-49); ACLR+LET: 26.7 (15-44) | BPTB and HA | “Over the top” | 5 | 0 (0.0) |
| Anderson4 (2001) | ACLR: 35; ACLR+LET: 35 | ACLR: 20.1 (14-38); ACLR+LET: 22.0 (14-40) | BPTB and HA | Losee | 2.9 (2.0-4.0) | 3 (4.3) |
aACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone autograft; HA, hamstring tendon autograft; LET, lateral extra-articular tenodesis.
bData are shown as mean (range).
All studies reported on single-bundle ACLR using either a hamstring tendon autograft or bone–patellar tendon–bone (BPTB) autograft. Overall, 3 studies reported on LET using the modified Lemaire technique.8,18,45 The modified Cocker-Arnold technique46 and the Losee technique4 were reported by 1 study each.4,46 These 2 techniques are biomechanically similar to the modified Lemaire technique in which the lateral articular capsule is enhanced using an iliotibial band strip. One study51 incorporated the tails of hamstring tendon grafts for ACLR in an “over-the-top” technique; the graft was looped back and fixed at the end of the lateral condyle in the cortical bone of the femur, and then, the remaining part of the graft was fixed using a single staple in manual maximum tension to the Gerdy tubercle. The fixation points are similar to those used in the MacIntosh technique.3
Characteristics of Included Studies
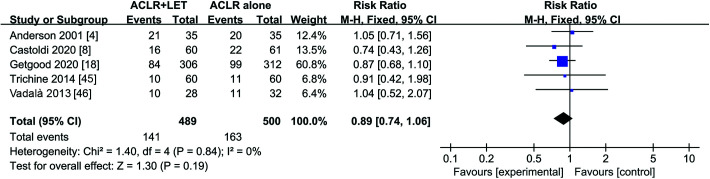
A total of 1010 patients were included in our analysis. The inclusion criteria of patients were slightly different among studies but can be summarized as follows: (1) an isolated primary ACL rupture with no comorbidities other than meniscal injuries,4,8,18,45,46,51 (2) age younger than 40 to 50 years4,18,46,51 (very few participants [<5%] were over the age of 40-50), (3) the presence of a grade ≥2 pivot shift,18,45,46 and (4) cutting sports at a competitive or amateur level.18,46,51 There were no statistically significant differences in the proportion of participants with concomitant partial meniscectomy between the ACLR+LET and ACLR groups (RR, 0.89 [95% CI, 0.74-1.06]; P = .19) (Figure 2). A single study included only male patients,45 while another included only female patients.46 Furthermore, 2 studies compared 3 techniques: isolated ACLR with a BPTB autograft, isolated ACLR with a hamstring tendon autograft, and ACLR+LET with a hamstring tendon autograft.4,51 To minimize heterogeneity, only the data from the latter 2 groups were extracted.
Figure 2.
Forest plot comparing the rates of patients with concomitant partial meniscectomy between the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; LET, lateral extra-articular tenodesis; M-H, Mantel-Haenszel.
Quality Assessment
Results from the quality assessment of included studies are summarized in Figure 3. One study8 was rated as having a high risk of selection bias because it reported unblinded block randomization for group allocation. Also, 2 studies46,51 reported that participants were allocated randomly but did not adequately describe the randomization method, thus resulting in an unclear risk of bias rating. All studies failed to clearly describe the blinding of patients regarding the surgery type. There were 3 studies8,18,46 rated as having a low risk of bias that mentioned the blinding methods used to measure outcome data: all participants wore a Tubigrip sleeve over the operative knee during functional testing to conceal the incisions, or an independent assessor completed clinical assessments. In contrast, the remaining studies were rated as having an unclear risk of bias because they provided insufficient data.
Figure 3.
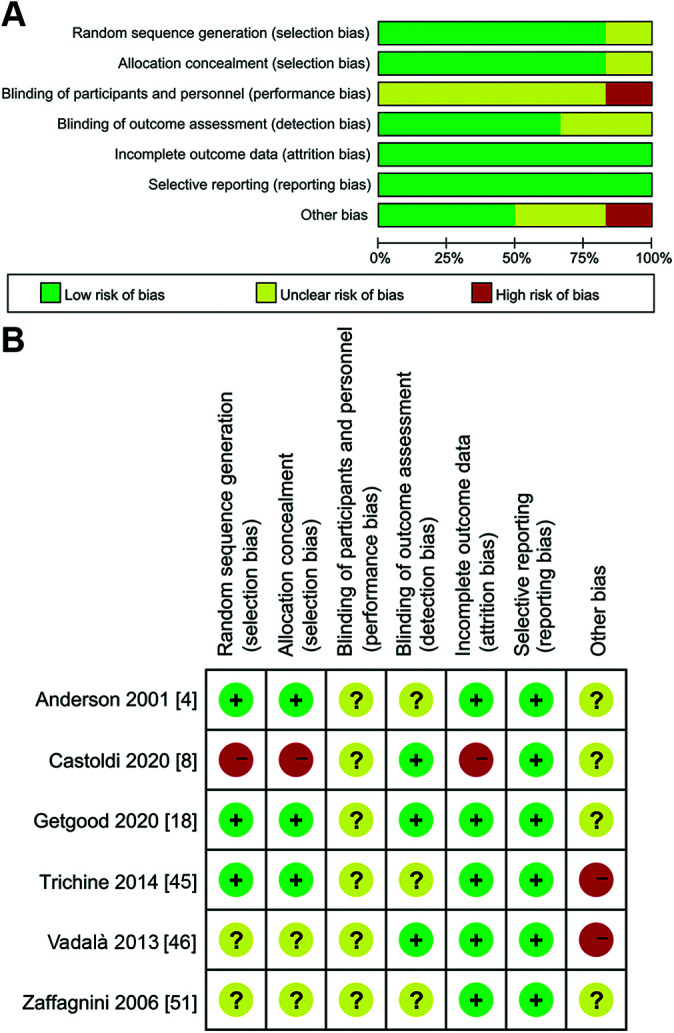
Quality assessment of the included studies. (A) Graph of the risk of different types of bias. (B) Summary of bias risk. + = low risk of bias; − = high risk of bias; ? = unclear or unknown risk of bias.
One study8 lost more than 20% of enrolled patients during follow-up and was regarded as having a high risk of attribution bias. All studies reported the same outcome measures and were thus rated as having a low risk of reporting bias. Notably, a single study included only male patients,45 while another included only female patients,46 which resulted in a high risk of other bias.
Primary Outcomes
Knee Stability
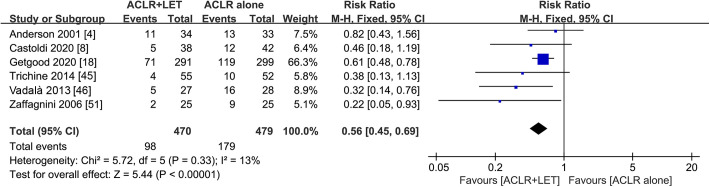
Pivot-Shift Test
The pivot-shift test is purportedly the most specific measure of rotational instability of all clinical ACL tests.42 All studies4,8,18,45,46,51 in our meta-analysis reported postoperative pivot-shift test findings (Figure 4). Among the patients, 479 were treated using isolated single-bundle ACLR (with either a hamstring tendon or BPTB autograft), and 470 were treated using ACLR+LET. The pivot shift was dichotomized into positive (grades 2 or 3) or negative (grades 0 or 1) for meta-analysis. There was a 56% risk reduction for positive knee ALRI with ACLR+LET (RR, 0.56 [95% CI, 0.45-0.69]; P < .00001), and low heterogeneity was detected (I 2 = 13%; P = .33).
Figure 4.
Forest plot of the incidence of positive knee anterolateral rotatory instability in the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; LET, lateral extra-articular tenodesis; M-H, Mantel-Haenszel.
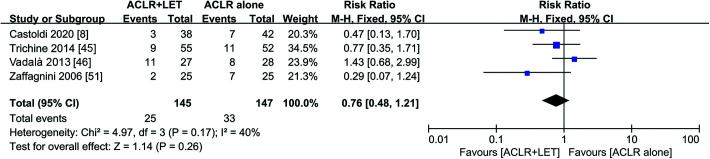
Lachman Test
Two-thirds of the studies reported Lachman test results.8,45,46,51 A total of 145 patients treated using ACLR+LET were compared to 147 patients treated using isolated ACLR (Figure 5). Lachman test results were dichotomized into positive (grades 2 and 3) or negative (grades 0 and 1) for meta-analysis. The results revealed no significant differences in terms of positive anterior laxity between the ACLR+LET and ACLR groups (RR, 0.76 [95% CI, 0.48-1.21]; P = .26). There was low to moderate heterogeneity among the studies (I 2 = 40%; P = .17).
Figure 5.
Forest plot of the incidence of positive anterior laxity in the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; LET, lateral extra-articular tenodesis; M-H, Mantel-Haenszel.
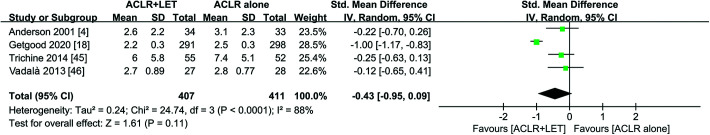
Side-to-Side Difference in Anterior Translation
Data on 818 patients, including 407 who underwent ACLR+LET and 411 who underwent ACLR, were pooled from 4 studies4,18,45,46 that reported the postoperative side-to-side difference as measured using a KT-1000/-2000 arthrometer (Figure 6). At last follow-up, this measurement was not significantly different between the 2 groups (SMD, –0.43 [95% CI, –0.95 to 0.09]; P = .11), although heterogeneity was high for this outcome (I 2 = 88%; P < .00001).
Figure 6.
Forest plot of the side-to-side difference between the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; IV, inverse variance; LET, lateral extra-articular tenodesis; Std, standardized.
Secondary Outcomes
Return to Sports
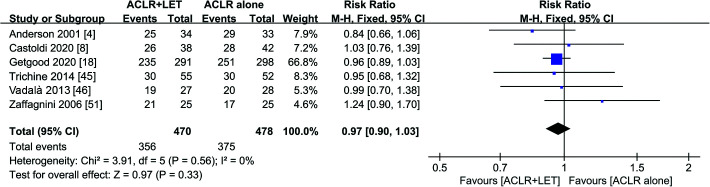
Overall Rate
Data on 470 patients treated using ACLR+LET and 478 treated using isolated ACLR were extracted from all 6 studies4,8,18,45,46,51 (Figure 7). The overall rates of return to sports, defined as the ability of patients to return to their primary sport of choice and their activity level before trauma, were evaluated at last follow-up. The data were dichotomized into “able to return” or “not able to return” for meta-analysis. No differences in overall rates of return to sports were found (RR, 0.97 [95% CI, 0.90-1.03]; P = .33), and no heterogeneity was detected (I 2 = 0%; P = .56).
Figure 7.
Forest plot of the overall rate of return to sports in the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; LET, lateral extra-articular tenodesis; M-H, Mantel-Haenszel.
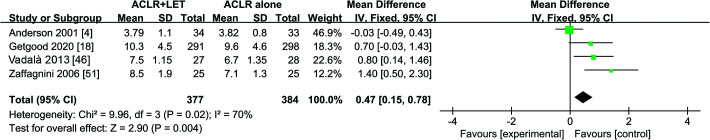
Activity Level
The Tegner scale and Marx scale are validated scoring systems to measure patient-reported activity levels.7,32 Data on 761 patients were pooled from 4 studies4,18,46,51 (Figure 8). Patients treated using ACLR+LET had significantly higher postoperative activity levels compared with patients who underwent ACLR (MD, 0.47 [95% CI, 0.15-0.78]; P = .004), with moderate to high heterogeneity among the studies (I 2 = 70%; P = .02).
Figure 8.
Forest plot comparing activity levels at last follow-up between the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; IV, inverse variance; LET, lateral extra-articular tenodesis.
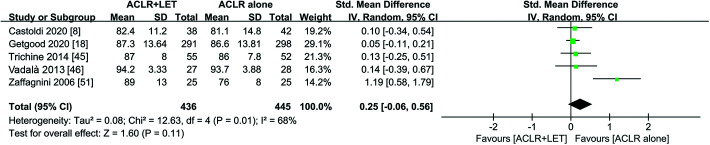
Patient-Reported Outcome Scores
IKDC Score
All 6 studies4,8,18,45,46,51 reported postoperative scores on the IKDC subjective evaluation form, but 1 study4 was excluded from the meta-analysis of IKDC scores because it used the 1994 version rather than the most recent 2000 version. While 1 study51 reported significantly higher IKDC scores for the ACLR+LET group than for the ACLR group, our meta-analysis revealed no significant differences (SMD, 0.25 [95% CI, –0.06 to 0.56]; P = .11) (Figure 9). Moderate to high heterogeneity was observed for this outcome (I 2 = 68%; P = .01).
Figure 9.
Forest plot comparing postoperative International Knee Documentation Committee scores (based on the 2000 subjective evaluation form) between the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; IV, inverse variance; LET, lateral extra-articular tenodesis; Std, standardized.
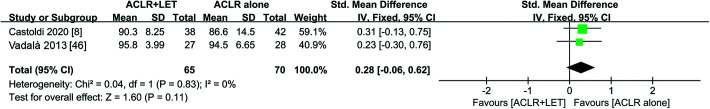
Lysholm Score
The Lysholm score is effective for evaluating overall knee function, but only 2 studies8,46 reported postoperative Lysholm scores. No statistically significant differences were detected between the ACLR+LET group (n = 65) and ACLR group (n = 70) (SMD, 0.28 [95% CI, –0.06 to 0.62]; P = .11), and no heterogeneity was observed for this outcome (I 2 = 0%; P = .83) (Figure 10).
Figure 10.
Forest plot comparing postoperative Lysholm scores between the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; IV, inverse variance; LET, lateral extra-articular tenodesis; Std, standardized.
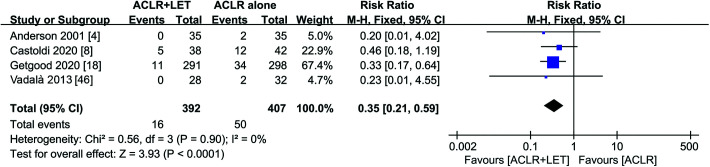
Graft Failure
Data on 799 patients, including 392 who underwent ACLR+LET and 407 who underwent ACLR, were pooled from 4 studies.4,8,18,46 The data were dichotomized into “confirmed graft rupture” or “no graft rupture” for meta-analysis. Patients treated using ACLR+LET had a significantly lower risk of postoperative graft failure compared with patients who underwent ACLR (RR, 0.35 [95% CI, 0.21-0.59]; P < .00001) (Figure 11), and no heterogeneity was detected (I 2 = 0%; P = .90).
Figure 11.
Forest plot of graft failure between the ACLR and ACLR+LET groups. ACLR, anterior cruciate ligament reconstruction; LET, lateral extra-articular tenodesis; M-H, Mantel-Haenszel.
Sensitivity Analysis
Given the potential for heterogeneity across studies because of patient and method differences, including the use of different LET techniques (iliotibial band graft or continuous hamstring tendon graft), we repeated the meta-analyses after excluding certain studies. The results were similar to those of the original meta-analyses (data not shown). In addition, as the number of included studies was relatively small, the random-effects model may not have been reliable. Therefore, all meta-analyses initially performed using a random-effects model were repeated using the fixed-effects model. Again, the results were similar to those of the original meta-analyses (data not shown).
Discussion
To determine differences in knee stability after the treatment of injured ACLs using ACLR+LET or ACLR alone, we performed a meta-analysis including 6 RCTs involving 1010 patients who were followed up for at least 24 months after surgery. We found that adding LET to ACLR provided no additional anterior knee stability compared with using ACLR alone based on the Lachman test or arthrometer testing. However, the addition of LET did reduce the incidence of the pivot shift and postoperative graft failure. While the addition of LET did not increase the overall rate of return to preinjury sports, it was associated with higher postoperative activity levels. Patient-reported outcome scores did not differ significantly between the ACLR and ACLR+LET groups.
The findings of our meta-analysis are consistent with those from several prospective controlled cohort studies.11,41,49 For example, a controlled cohort study41 of 277 patients treated using single-bundle ACLR with or without extra-articular augmentation using an iliotibial band also reported a significantly lower pivot shift at 2-year follow-up in the group that underwent tenodesis. Another study11 observed superior correction of the pivot shift in patients who underwent single-bundle ACLR using BPTB autografts in addition to modified Lemaire extra-articular tenodesis compared with in patients who underwent ACLR alone. We conclude that combining single-bundle ACLR with LET can further reduce the risk of postoperative ALRI in the long term (>2 years).
LET is aimed at restoring stability of the injured anterolateral complex including the anterolateral ligament, lateral capsule, and lateral collateral ligament, which together act as a secondary restraint to internal rotation of the tibia.29,38,40 Therefore, we were not surprised to find that LET did not affect anterior laxity of the knee in patients undergoing ACLR, as measured using the Lachman test or in terms of the side-to-side difference. Consistent with our findings, several biomechanical studies13,16,20,25 not included in this meta-analysis have reported no significant differences in anterior tibial translation of ACL-reconstructed knees between patients who underwent LET and those who did not.
Although adding LET to ACLR did not significantly increase the rate of return to sports in our meta-analysis, it did appear to increase the activity level during sports. There were 2 included studies18,46 that reported that the addition of LET enabled a larger subset of patients to return to strenuous, high pivot-shift sports such as skiing, soccer, and football. In fact, 1 study2 reported that the addition of LET led to postoperative activity levels that were similar to preinjury levels. Regardless of whether these discrepancies from our meta-analysis are genuine, the literature supports adding LET to ACLR for athletes in demanding sports.
We and others did not detect differences in the IKDC subjective score or Lysholm score between patients who underwent ACLR and those who underwent ACLR+LET.2,11,49 Both scoring systems have been carefully validated to assess patient knee function,7,14,23 but items assessing quality of life contribute only 10% to the overall IKDC score and only 5% to the overall Lysholm score. In fact, the IKDC score fails to reflect differences in quality of life after ACLR because of, for example, differences in postoperative activity levels.50 Therefore, a more disease-specific measurement with better structural validity, such as the ACL Quality of Life Questionnaire,34 may be needed. IKDC subjective scores and Lysholm scores may not be sufficient for comprehensively assessing outcomes after the addition of LET or other ACLR modifications.
The results from our meta-analysis are strengthened by the fact that we performed a comprehensive review of level 1 evidence with strict inclusion criteria. In addition, this study included 2 new, high-quality RCTs and a larger sample than a similar previous meta-analysis included.12,21 This, together with our sensitivity analysis, supports the robustness of our conclusions.
Despite these advantages, our meta-analysis has several limitations. First, the number of included studies was yet still small. Second, the follow-up duration varied widely from 2 to 19 years, which may have contributed to heterogeneity. Third, patients across the studies varied in their baseline characteristics, including age, sex, and family history, all of which are regarded as risk factors for residual ALRI. Fourth, surgical methods differed across the studies, which can affect outcomes. Other limitations may include the following: >50% of patients in this meta-analysis came from a single study,18 we could not assess other anterolateral ligament procedures, there were no data on long-term results, and there were limited data on LET using BPTB grafts. Further RCTs with larger sample sizes and longer follow-ups (>10 years) are required to ascertain the necessity of adding LET to ACLR.
Conclusion
The addition of LET to single-bundle ACLR appeared to be associated with a statistically significant, clinically relevant reduction in postoperative ALRI in the long term (>2 years) relative to ACLR alone. The adoption of LET may also lead to higher postoperative activity levels and a lower incidence of graft failure. For these reasons, the LET procedure should be considered in combination with isolated single-bundle ACLR, particularly in patients involved in strenuous sports.
APPENDIX
Search Strategy of PubMed Databasea
Search string:
((((((Lateral Extra-articular Tenodesis) OR (Lateral Extra-articular procedure)) OR (Lateral Augmentation Procedures)) OR (Lateral Extra-articular Plasty)) OR (Lateral Extra-articular sling) AND (Knee) Sort by: Most Recent
((((((((((((((((((((((((“functional laterality”[MeSH Terms] OR (“functional”[All Fields] AND “laterality”[All Fields])) OR “functional laterality”[All Fields]) OR “laterality”[All Fields]) OR “lateral”[All Fields]) OR “lateralisation”[All Fields]) OR “lateralisations”[All Fields]) OR “lateralise”[All Fields]) OR “lateralised”[All Fields]) OR “lateralises”[All Fields]) OR “lateralising”[All Fields]) OR “lateralities”[All Fields]) OR “lateralization”[All Fields]) OR “lateralizations”[All Fields]) OR “lateralize”[All Fields]) OR “lateralized”[All Fields]) OR “lateralizes”[All Fields]) OR “lateralizing”[All Fields]) OR “laterally”[All Fields]) OR “laterals”[All Fields]) AND “Extra-articular”[All Fields] AND ((((“tenodesed”[All Fields] OR “tenodesing”[All Fields]) OR “tenodesis”[MeSH Terms]) OR “tenodesis”[All Fields]) OR “tenodeses”[All Fields])) OR ((((((((((((((((((((“functional laterality”[MeSH Terms] OR (“functional”[All Fields] AND “laterality”[All Fields])) OR “functional laterality”[All Fields]) OR “laterality”[All Fields]) OR “lateral”[All Fields]) OR “lateralisation”[All Fields]) OR “lateralisations”[All Fields]) OR “lateralise”[All Fields]) OR “lateralised”[All Fields]) OR “lateralises”[All Fields]) OR “lateralising”[All Fields]) OR “lateralities”[All Fields]) OR “lateralization”[All Fields]) OR “lateralizations”[All Fields]) OR “lateralize”[All Fields]) OR “lateralized”[All Fields]) OR “lateralizes”[All Fields]) OR “lateralizing”[All Fields]) OR “laterally”[All Fields]) OR “laterals”[All Fields]) AND “Extra-articular”[All Fields] AND (((((((“methods”[MeSH Terms] OR “methods”[All Fields]) OR “procedure”[All Fields]) OR “methods”[MeSH Subheading]) OR “procedures”[All Fields]) OR “procedural”[All Fields]) OR “procedurally”[All Fields]) OR “procedure s”[All Fields]))) OR ((((((((((((((((((((“functional laterality”[MeSH Terms] OR (“functional”[All Fields] AND “laterality”[All Fields])) OR “functional laterality”[All Fields]) OR “laterality”[All Fields]) OR “lateral”[All Fields]) OR “lateralisation”[All Fields]) OR “lateralisations”[All Fields]) OR “lateralise”[All Fields]) OR “lateralised”[All Fields]) OR “lateralises”[All Fields]) OR “lateralising”[All Fields]) OR “lateralities”[All Fields]) OR “lateralization”[All Fields]) OR “lateralizations”[All Fields]) OR “lateralize”[All Fields]) OR “lateralized”[All Fields]) OR “lateralizes”[All Fields]) OR “lateralizing”[All Fields]) OR “laterally”[All Fields]) OR “laterals”[All Fields]) AND (((((“augment”[All Fields] OR “augmentation”[All Fields]) OR “augmentations”[All Fields]) OR “augmented”[All Fields]) OR “augmenting”[All Fields]) OR “augments”[All Fields]) AND (((((((“methods”[MeSH Terms] OR “methods”[All Fields]) OR “procedure”[All Fields]) OR “methods”[MeSH Subheading]) OR “procedures”[All Fields]) OR “procedural”[All Fields]) OR “procedurally”[All Fields]) OR “procedure s”[All Fields]))) OR ((((((((((((((((((((“functional laterality”[MeSH Terms] OR (“functional”[All Fields] AND “laterality”[All Fields])) OR “functional laterality”[All Fields]) OR “laterality”[All Fields]) OR “lateral”[All Fields]) OR “lateralisation”[All Fields]) OR “lateralisations”[All Fields]) OR “lateralise”[All Fields]) OR “lateralised”[All Fields]) OR “lateralises”[All Fields]) OR “lateralising”[All Fields]) OR “lateralities”[All Fields]) OR “lateralization”[All Fields]) OR “lateralizations”[All Fields]) OR “lateralize”[All Fields]) OR “lateralized”[All Fields]) OR “lateralizes”[All Fields]) OR “lateralizing”[All Fields]) OR “laterally”[All Fields]) OR “laterals”[All Fields]) AND “Extra-articular”[All Fields] AND (“plasties”[All Fields] OR “plasty”[All Fields]))) OR ((((((((((((((((((((“functional laterality”[MeSH Terms] OR (“functional”[All Fields] AND “laterality”[All Fields])) OR “functional laterality”[All Fields]) OR “laterality”[All Fields]) OR “lateral”[All Fields]) OR “lateralisation”[All Fields]) OR “lateralisations”[All Fields]) OR “lateralise”[All Fields]) OR “lateralised”[All Fields]) OR “lateralises”[All Fields]) OR “lateralising”[All Fields]) OR “lateralities”[All Fields]) OR “lateralization”[All Fields]) OR “lateralizations”[All Fields]) OR “lateralize”[All Fields]) OR “lateralized”[All Fields]) OR “lateralizes”[All Fields]) OR “lateralizing”[All Fields]) OR “laterally”[All Fields]) OR “laterals”[All Fields]) AND “Extra-articular”[All Fields] AND (“sling”[All Fields] OR “slings”[All Fields]))) AND ((((“knee”[MeSH Terms] OR “knee”[All Fields]) OR “knee joint”[MeSH Terms]) OR (“knee”[All Fields] AND “joint”[All Fields])) OR “knee joint”[All Fields])
aMeSH, Medical Subject Headings.
Footnotes
Final revision submitted December 3, 2020; accepted January 5, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Acquitter Y, Hulet C, Locker B, et al. Patellar tendon-bone autograft reconstruction of the anterior cruciate ligament for advanced-stage chronic anterior laxity: is an extra-articular plasty necessary? A prospective randomized study of 100 patients with five year follow-up. Article in French. Rev Chir Orthop Reparatrice Appar Mot. 2003;89(5):413–422. [PubMed] [Google Scholar]
- 2. Alessio-Mazzola M, Formica M, Russo A, et al. Outcome after combined lateral extra-articular tenodesis and anterior cruciate ligament revision in professional soccer players. J Knee Surg. 2019;32(9):906–910. [DOI] [PubMed] [Google Scholar]
- 3. Amirault J, Cameron J, MacIntosh D, Marks P. Chronic anterior cruciate ligament deficiency: long-term results of MacIntosh’s lateral substitution reconstruction. J Bone Joint Surg Br. 1988;70(4):622–624. [DOI] [PubMed] [Google Scholar]
- 4. Anderson AF, Snyder RB, Lipscomb AB, Jr. Anterior cruciate ligament reconstruction: a prospective randomized study of three surgical methods. Am J Sports Med. 2001;29(3):272–279. [DOI] [PubMed] [Google Scholar]
- 5. Ayeni O, Chahal M, Tran M, Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):767–777. [DOI] [PubMed] [Google Scholar]
- 6. Benum P. Anterolateral rotary instability of the knee joint: results after stabilization by extraarticular transposition of the lateral part of the patellar ligament. A preliminary report. Acta Orthop Scand. 1982;53(4):613–617. [DOI] [PubMed] [Google Scholar]
- 7. Briggs K, Lysholm J, Tegner Y, et al. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. [DOI] [PubMed] [Google Scholar]
- 8. Castoldi M, Magnussen R, Gunst S, et al. A randomized controlled trial of bone--patellar tendon--bone anterior cruciate ligament reconstruction with and without lateral extra-articular tenodesis: 19-year clinical and radiological follow-up. Am J Sports Med. 2020;48(7):1665–1672. [DOI] [PubMed] [Google Scholar]
- 9. Clancy W, Nelson D, Reider B, Narechania R. Anterior cruciate ligament reconstruction using one-third of the patellar ligament, augmented by extra-articular tendon transfers. J Bone Joint Surg Am. 1982;64(3):352–359. [PubMed] [Google Scholar]
- 10. Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(9):1566–1571. [DOI] [PubMed] [Google Scholar]
- 11. Dejour D, Vanconcelos W, Bonin N, Saggin P. Comparative study between mono-bundle bone-patellar tendon-bone, double-bundle hamstring and mono-bundle bone-patellar tendon-bone combined with a modified Lemaire extra-articular procedure in anterior cruciate ligament reconstruction. Int Orthop. 2013;37(2):193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Devitt B, Bouguennec N, Barfod K, et al. Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis does not result in an increased rate of osteoarthritis: a systematic review and best evidence synthesis. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1149–1160. [DOI] [PubMed] [Google Scholar]
- 13. Devitt BM, Lord BR, Williams A, Amis AA, Feller JA. Biomechanical assessment of a distally fixed lateral extra-articular augmentation procedure in the treatment of anterolateral rotational laxity of the knee. Am J Sports Med. 2019;47(9):2102–2109. [DOI] [PubMed] [Google Scholar]
- 14. Ebrahimzadeh MH, Makhmalbaf H, Golhasani-Keshtan F, Rabani S, Birjandinejad A. The International Knee Documentation Committee (IKDC) subjective short form: a validity and reliability study. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3163–3167. [DOI] [PubMed] [Google Scholar]
- 15. Ellison AE. Distal iliotibial-band transfer for anterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1979;61(3):330–337. [PubMed] [Google Scholar]
- 16. Geeslin AG, Moatshe G, Chahla J, et al. Anterolateral knee extra-articular stabilizers: a robotic study comparing anterolateral ligament reconstruction and modified Lemaire lateral extra-articular tenodesis. Am J Sports Med. 2018;46(3):607–616. [DOI] [PubMed] [Google Scholar]
- 17. Georgoulis A, Ristanis S, Chouliaras V, Moraiti C, Stergiou N. Tibial rotation is not restored after ACL reconstruction with a hamstring graft. Clin Orthop Relat Res. 2007;454:89–94. [DOI] [PubMed] [Google Scholar]
- 18. Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY study randomized clinical trial. Am J Sports Med. 2020;48(2):285–297. [DOI] [PubMed] [Google Scholar]
- 19. Giraud B, Besse J, Cladière F, et al. Intra-articular reconstruction of the anterior cruciate ligament with and without extra-articular supplementation by quadricipital tendon plasty: seven-year follow-up. Article in French. Rev Chir Orthop Reparatrice Appar Mot. 2006;92(8):788–797. [DOI] [PubMed] [Google Scholar]
- 20. Herbst E, Arilla F, Guenther D, et al. Lateral extra-articular tenodesis has no effect in knees with isolated anterior cruciate ligament injury. Arthroscopy. 2018;34(1):251–260. [DOI] [PubMed] [Google Scholar]
- 21. Hewison C, Tran M, Kaniki N, et al. Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: a systematic review of the literature. Arthroscopy. 2015;31(10):2022–2034. [DOI] [PubMed] [Google Scholar]
- 22. Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Higgins LD, Taylor MK, Park D, et al. Reliability and validity of the International Knee Documentation Committee (IKDC) subjective knee form. Joint Bone Spine. 2007;74(6):594–599. [DOI] [PubMed] [Google Scholar]
- 24. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 25. Jette C, Gutierrez D, Sastre S, Llusa M, Combalia A. Biomechanical comparison of anterolateral ligament anatomical reconstruction with a semi-anatomical lateral extra-articular tenodesis: a cadaveric study. Knee. 2019;26(5):1003–1009. [DOI] [PubMed] [Google Scholar]
- 26. Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5-9 years after surgery. Acta Orthop Scand. 2004;75(5):594–599. [DOI] [PubMed] [Google Scholar]
- 27. Kennedy JC, Stewart R, Walker DM. Anterolateral rotatory instability of the knee joint: an early analysis of the Ellison procedure. J Bone Joint Surg Am. 1978;60(8):1031–1039. [PubMed] [Google Scholar]
- 28. Kocher M, Steadman J, Briggs K, Sterett W, Hawkins R. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):629–634. [DOI] [PubMed] [Google Scholar]
- 29. Kosy JD, Mandalia VI. Revisiting the anterolateral ligament of the knee. J Knee Surg. 2016;29(7):571–579. [DOI] [PubMed] [Google Scholar]
- 30. Leroux T, Wasserstein D, Dwyer T, et al. The epidemiology of revision anterior cruciate ligament reconstruction in Ontario, Canada. Am J Sports Med. 2014;42(11):2666–2672. [DOI] [PubMed] [Google Scholar]
- 31. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 32. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 33. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. [DOI] [PubMed] [Google Scholar]
- 34. Mohtadi N. Development and validation of the quality of life outcome measure (questionnaire) for chronic anterior cruciate ligament deficiency. Am J Sports Med. 1998;26(3):350–359. [DOI] [PubMed] [Google Scholar]
- 35. Noyes FR, Huser LE, West J, et al. Two different knee rotational instabilities occur with anterior cruciate ligament and anterolateral ligament injuries: a robotic study on anterior cruciate ligament and extra-articular reconstructions in restoring rotational stability. Arthroscopy. 2018;34(9):2683–2695. [DOI] [PubMed] [Google Scholar]
- 36. Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P. Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med. 2010;38(6):1094–1102. [DOI] [PubMed] [Google Scholar]
- 37. Pinczewski LA, Lyman J, Salmon LJ, et al. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. [DOI] [PubMed] [Google Scholar]
- 38. Pomajzl R, Maerz T, Shams C, Guettler J, Bicos J. A review of the anterolateral ligament of the knee: current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy. 2015;31(3):583–591. [DOI] [PubMed] [Google Scholar]
- 39. Ristanis S, Giakas G, Papageorgiou CD, et al. The effects of anterior cruciate ligament reconstruction on tibial rotation during pivoting after descending stairs. Knee Surg Sports Traumatol Arthrosc. 2003;11(6):360–365. [DOI] [PubMed] [Google Scholar]
- 40. Roessler P, Schüttler K, Heyse T, Wirtz D, Efe T. The anterolateral ligament (ALL) and its role in rotational extra-articular stability of the knee joint: a review of anatomy and surgical concepts. Arch Orthop Trauma Surg. 2016;136(3):305–313. [DOI] [PubMed] [Google Scholar]
- 41. Rowan F, Huq S, Haddad F. Lateral extra-articular tenodesis with ACL reconstruction demonstrates better patient-reported outcomes compared to ACL reconstruction alone at 2 years minimum follow-up. Arch Orthop Trauma Surg. 2019;139(10):1425–1433. [DOI] [PubMed] [Google Scholar]
- 42. Scholten RJ, Opstelten W, van der Plas CG, et al. Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: a meta-analysis. J Fam Pract. 2003;52(9):689–694. [PubMed] [Google Scholar]
- 43. Song GY, Hong L, Zhang H, et al. Clinical outcomes of combined lateral extra-articular tenodesis and intra-articular anterior cruciate ligament reconstruction in addressing high-grade pivot-shift phenomenon. Arthroscopy. 2016;32(5):898–905. [DOI] [PubMed] [Google Scholar]
- 44. Tashman S, Collon D, Anderson K, Kolowich P, Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(4):975–983. [DOI] [PubMed] [Google Scholar]
- 45. Trichine F, Alsaati M, Chouteau J, et al. Patellar tendon autograft reconstruction of the anterior cruciate ligament with and without lateral plasty in advanced-stage chronic laxity: a clinical, prospective, randomized, single-blind study using passive dynamic X-rays. Knee. 2014;21(1):58–65. [DOI] [PubMed] [Google Scholar]
- 46. Vadalà AP, Iorio R, De Carli A, et al. An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. Int Orthop. 2013;37(2):187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Warren R, Marshall J. Injuries of the anterior cruciate and medial collateral ligaments of the knee: a long-term follow-up of 86 cases, part II. Clin Orthop Relat Res. 1978;136:198–211. [PubMed] [Google Scholar]
- 48. Weber AE, Zuke W, Mayer EN, et al. Lateral augmentation procedures in anterior cruciate ligament reconstruction: anatomic, biomechanical, imaging, and clinical evidence. Am J Sports Med. 2019;47(3):740–752. [DOI] [PubMed] [Google Scholar]
- 49. Williams A, Ball S, Stephen J, et al. The scientific rationale for lateral tenodesis augmentation of intra-articular ACL reconstruction using a modified “Lemaire” procedure. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1339–1344. [DOI] [PubMed] [Google Scholar]
- 50. Williams T, Burley D, Evans L, et al. The structural validity of the IKDC and its relationship with quality of life following ACL reconstruction. Scand J Med Sci Sports. 2020;30(9):1748–1757. [DOI] [PubMed] [Google Scholar]
- 51. Zaffagnini S, Marcacci M, Lo Presti M, et al. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1060–1069. [DOI] [PubMed] [Google Scholar]
- 52. Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, et al. Over-the-top ACL reconstruction plus extra-articular lateral tenodesis with hamstring tendon grafts: prospective evaluation with 20-year minimum follow-up. Am J Sports Med. 2017;45(14):3233–3242. [DOI] [PubMed] [Google Scholar]
- 53. Zarins B, Rowe C. Combined anterior cruciate-ligament reconstruction using semitendinosus tendon and iliotibial tract. J Bone Joint Surg Am. 1986;68(2):160–177. [PubMed] [Google Scholar]