Abstract
Background:
The treatment for borderline developmental dysplasia of the hip (BDDH) has historically been arthroscopic surgery or periacetabular osteotomy (PAO). As orthopaedic surgery is constantly evolving, a lack of comparison of outcomes for these 2 treatment methods could potentially be stalling the progression of treatment for patients with BDDH.
Purpose:
To evaluate the existing literature on patient characteristics, procedures, clinical outcomes, and failure rates for patients with BDDH and to determine whether PAO or hip arthroscopic surgery is a better treatment method for patients with BDDH.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Studies included were found using the following search words: “hip” and “borderline dysplasia,” “osteotomy” or “arthroscopy,” and “outcome” or “procedure.” Articles were included if they detailed participants of all sexes and ages, reported on isolated hips, and had patients diagnosed with BDDH.
Results:
A search was conducted across 3 databases, resulting in 469 articles for consideration, from which 12 total studies (10 on arthroscopic surgery and 2 on PAO) were chosen for a review. There were 6 studies that included patients with a lateral center-edge angle of 18° to 25°, while the remainder included patients with a lateral center-edge angle of 20° to 25°. All the studies reviewing arthroscopic surgery reported concomitant/accessory procedures, while the articles on the topic of PAO did not. It was determined that, whether treated using arthroscopic surgery or PAO, outcomes improved across all patient-reported outcome measures. Revision surgery was also common in both procedures.
Conclusion:
There is a lack of consensus in the literature on the best treatment option for patients with BDDH. Preoperative patient characteristics and concomitant injuries should be considered when evaluating which surgical procedure will result in the most favorable outcomes.
Keywords: borderline developmental dysplasia of the hip (BDDH), periacetabular osteotomy (PAO), hip arthroscopic surgery, systematic review
Developmental dysplasia of the hip (DDH) is a common musculoskeletal condition in newborns and is considered a precursor to osteoarthritis (OA).13,39 By definition, patients with DDH are described as having either a smaller, and therefore shallower, acetabulum or one that is abnormally vertical.5 Acetabular shallowness results in hip joint instability and may cause labral tearing with dysfunction in young patients.35 It has been reported that periacetabular osteotomy (PAO) and other procedures result in good clinical outcomes for patients with DDH and ultimately may prevent OA.9,11,26 This condition can be further defined based on the extent of acetabular coverage as borderline or mild (borderline DDH [BDDH]) largely using lateral center-edge angles (LCEAs) of either 20° to 25° or 18° to 25°, depending on the diagnosing physician. Because of the unique nature of the acetabulum and resultant capsular laxity in patients with BDDH, responses to surgical procedures aimed at treating the abnormality are mixed.45
Surgery for the treatment and diagnosis of hip abnormalities is constantly evolving, with hip arthroscopic surgery in the forefront of minimally invasive surgery,20,37 in which favorable clinical outcomes have been reported across multiple populations.28,33 Shown in the literature to be favorable in patients with femoroacetabular impingement, hip arthroscopy, along with PAO, was originally intended for the treatment of other conditions.43 Hip arthroscopic surgery is frequently indicated for the treatment of FAI, which has been recognized as a major cause of hip pain in young adults.1,2 However, patients diagnosed with BDDH have capsular laxity before a surgical intervention.16 Furthermore, increased capsular laxity is a poor outcome often associated with the arthroscopic treatment of hip disorders, which can be exacerbated in patients with BDDH and may result in subluxations and hip dislocations.41 In addition to this limitation of the arthroscopic treatment of BDDH, the following indications have shown poor outcomes in patients with BDDH: a broken Shenton line, an LCEA <19°, a femoral neck shaft angle >140°, cartilage injuries, a body mass index >23, and age >38 years.22 Arthroscopic surgery is preferred, as it is less invasive than are open procedures in the hip joint. However, because of the confined nature of only using portals for the procedure, arthroscopic surgery is not an option for patients who have a more severe classification of BDDH.47 Therefore, PAO is one of the most commonly indicated procedures for patients with more severe dysplasia. On the other hand, PAO is more invasive, and it requires extensive postsurgical rehabilitation, which limits returning to the same level of activity as before the surgical intervention.21
Both arthroscopic surgery and PAO of the hip joint have been shown to have favorable outcomes for patients with BDDH. Several studies have shown positive subjective and objective results in patients after hip arthroscopic surgery using capsular plication/closure in conjunction with labral repair.16,18,34 Moreover, some articles have shown that PAO also improves outcomes in patients with BDDH.29,32 However, each method has limits in producing the most favorable outcomes for patients.
While there appears to be a fair amount of research conducted on each treatment method, a direct comparison of articles reviewing PAO and hip arthroscopic surgery and their clinical outcomes has yet to be performed. There has, however, been a systematic review performed by Ding et al,13 who reviewed 9 studies composed of 425 patients with BDDH who underwent hip arthroscopic surgery and described that the mean reoperation rate was 8.5% and that the rate of conversion to total hip arthroplasty (THA) ranged from 4.4% to 26.9%. They concluded that hip arthroscopic surgery for patients with BDDH results in relatively good clinical outcomes.13 However, they did not discuss PAO and did not describe the details of arthroscopic surgery. Therefore, a systematic review detailing a comparison between hip arthroscopic surgery and PAO can help establish which is a better procedure for patients with BDDH.
The purpose of this systematic review was to evaluate the existing literature on patient characteristics, procedures, clinical outcomes, and failure rates for patients with BDDH to answer the following question: Which surgical intervention is best for treating patients with BDDH: hip arthroscopic surgery or PAO?
Methods
Search Strategy
Overall, 3 databases were used to search for qualifying articles (PubMed, Embase, and MEDLINE) using the following keywords: (hip) AND (borderline dysplasia) AND ((osteotomy) OR (arthroscopy)); (hip) AND (borderline dysplasia) AND ((outcome) OR (procedure)); (hip) AND (borderline dysplasia) AND ((arthroscopy) OR (open)). The search of the databases was carried out by 2 researchers (Y.M. and R.S.).
Inclusion and Exclusion Criteria
Articles were included in the study if they met the following inclusion criteria: included patients of all ages and sexes, reported the surgical outcomes of isolated hip procedures, and included patients having the diagnosis of BDDH. Furthermore, articles were excluded if they were written in a language other than English; included patients with previous or other hip deformities (eg, acetabular fractures, Legg-Calve-Perthes disease, inflammatory hip disorders, global morphologic abnormalities requiring surgical dislocation, generalized focal or neuromuscular disorders); or were review articles, diagnostic studies, case reports, technique reports, opinion articles, or articles that seemed to involve overlapping patients (Table 1). If there were inconsistencies in the articles proposed for inclusion by the 2 researchers, each potential article was read in full by each reviewer and discussed in terms of the criteria. Once a consensus was reached, the full-text review was complete.
TABLE 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
Data Collection
Data were collected by the primary author (Y.M.) and further evaluated by a co-author (M.M.) using spreadsheets. For each study, the following information was gathered into tables: basic characteristics of each study, concomitant/arthroscopic procedures performed, patient-reported outcome (PRO) scores, and failures in each study resulting in revision surgery or conversion to THA. Moreover, the Coleman methodology score10 was assigned to each article, and results were compiled using the same spreadsheet.
Quality Assessment
A quality assessment of the studies was performed separately by the 2 reviewers (Y.M. and M.M.) using the Coleman methodology score criteria.10 The Coleman methodology score was independently assigned in duplicate by 2 reviewers (Y.M. and M.M.).
Results
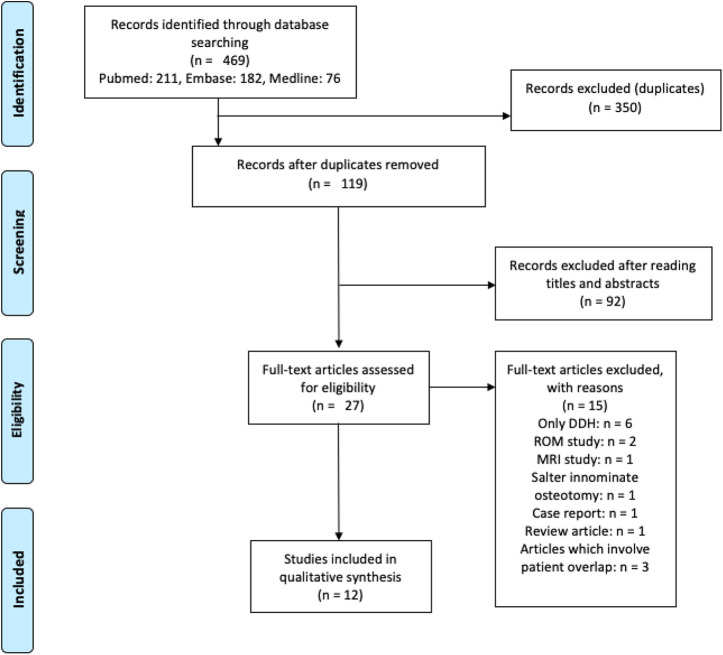
The original search yielded 469 articles. Duplicates were removed, resulting in 119 studies to be considered. Articles were then screened based on the titles and abstracts, leaving 27 full-text articles before applying the inclusion/exclusion criteria. There were 15 full-text articles excluded based on meeting certain exclusion criteria. As a result of our literature search findings, there was a significant overlap in authors and institutions across articles eligible for inclusion. This would result in a large patient overlap and, therefore, repeated data sets across studies. As a result, among the 15 excluded articles were 3 articles6,8,16 that were excluded in an attempt to limit excessive patient overlapping (Appendix Table A1). Finally, 12 articles were reviewed for a qualitative synthesis (Figure 1) and included in this study, resulting in a total of 674 patients, 581 of whom were patients in the arthroscopic surgery group and 93 of whom were in the PAO group.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of the search strategy. DDH, developmental dysplasia of the hip; MRI, magnetic resonance imaging; ROM, range of motion.
Definition of BDDH
Interestingly, 6 of the studies included in this review defined BDDH as an LCEA between 18° and 25°.7,12,14,27,29,34 The remaining 6 of the 12 studies4,17,18,22,32,48 examined in this review included patients clinically diagnosed with hip dysplasia presenting with an LCEA between 20° and 25° (Table 2).
TABLE 2.
Characteristics of Included Studiesa
| First author (Year) | Study Type (LOE) | Definition of BDDH | No. of Patients | Mean Age, y | Mean ± SD Follow-up, mo | Outcome Measures |
|---|---|---|---|---|---|---|
| Hip arthroscopic surgery | ||||||
| Beck4 (2019) | Cohort (3) | LCEA, 20°-25° | 112 | 33.6 ± 12.7 | 24 | mHHS, HOS-ADL, HOS-SSS, iHOT-12 |
| Chaharbakhshi7 (2017) | Cohort (3) | LCEA, 18°-25° | 40 | LT tear: 29.6 ± 12.2; no LT tear: 26.8 ± 11.5b | 54.3 | mHHS, NAHS, HOS-SSS, VAS pain, satisfaction |
| Cvetanovich12 (2017) | Cohort (3) | LCEA, 18°-25° | 36 | 31.5 ± 11.8 | 31.2 ± 7.2 | mHHS, HOS-SSS, HOS-ADL, satisfaction |
| Domb14 (2018) | Case series (4) | LCEA, 18°-25° | 19 (21 hips) | 22.9 | 68.8 ± 6.4 | mHHS, NAHS, HOS-SSS, VAS pain, satisfaction |
| Evans17 (2017) | Therapeutic (4) | LCEA, 20°-25° | 21 | 15.5 | 26.3 | mHHS, NAHS, HOS-SSS, HOS-ADL, VAS pain, satisfaction |
| Fukui18 (2015) | Therapeutic (4) | LCEA, 20°-25° | 102 | 35 | 40 | mHHS, HOS-ADL, HOS-SSS, SF-12 PCS, SF-12 MCS, WOMAC, satisfaction |
| Hatakeyama22 (2018) | Case-control (3) | LCEA, 20°-25° | 45 | 31.4 | 42.5 | mHHS, NAHS |
| Maldonado27 (2018) | Case-control (3) | LCEA, 18°-25° | 115 (122 hips) | Success: 23.5 ± 7.5; failure: 28.5 ± 7.8c | Success: 39.2 ± 17.3; failure: 42.8 ± 20.4 | mHHS, NAHS, HOS-SSS, VAS pain, satisfaction |
| Nawabi34 (2016) | Cohort (3) | LCEA, 18°-25° | 46 (55 hips) | 29.8 ± 9.4 | 31.3 ± 7.6 | mHHS, HOS-SSS, HOS-ADL, iHOT-33, satisfaction |
| Yoon48 (2019) | Therapeutic (4) | LCEA, 20°-25° | 45 (47 hips) | 39.2 ± 11.8 | 25.9 | mHHS, NAHS, VAS pain, satisfaction |
| PAO | ||||||
| McClincy29 (2019) | Therapeutic (4) | LCEA, 18°-25° | 49 | 26.5 ± 8 | 26.4 | mHHS, UCLA, HOOS, SF-12 |
| Mose32 (2019) | Cohort (3) | LCEA, 20°-25° | 44 | 34.1 | 24 | WOMAC, OHS, SF-36 |
aBDDH, borderline developmental dysplasia of the hip; HOOS, Hip disability and Osteoarthritis Outcome Score; HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; iHOT-12, 12-Item International Hip Outcome Tool; iHOT-33, 33-Item International Hip Outcome Tool; LCEA, lateral center-edge angle; LOE, level of evidence; LT, ligamentum teres; MCS, Mental Component Summary; mHHS, modified Harris Hip Score; NAHS, Nonarthritic Hip Score; OHS, Oxford Hip Score; PAO, periacetabular osteotomy; PCS, Physical Component Summary; SF-12, 12-Item Short Form Health Survey; SF-36, 36-Item Short Form Health Survey; UCLA, University of California, Los Angeles; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
bThe patients with LT tears were matched in a 1:1 ratio to patients without LT tears based on the following criteria: sex, age at surgery ±10 years, obesity (body mass index <30 vs ≥30), labral treatment type (repair vs selective debridement), and microfracture.
cThe “success” group consisted of all patients who achieved the Patient Acceptable Symptom State (PASS) of an mHHS score ≥74 and underwent no ipsilateral hip surgery subsequent to their index arthroscopic surgery. The “failure” group was composed of patients who did not achieve the PASS at latest follow-up or required secondary arthroscopic surgery or conversion to total hip arthroplasty.
Risk of Bias in Included Studies
Table 3 outlines the scores that each article received when undergoing the Coleman methodology score analysis.10 The highest score in the arthroscopic surgery articles was achieved by Hatakeyama et al,22 while the lowest was assigned to Maldonado et al.27 Of the 2 articles examining PAO, Mose et al32 was assigned the higher score of 63 compared with that of 38 for McClincy et al.29
TABLE 3.
Coleman Methodology Scores of Included Studiesa
| First author (Year) | Categoryb | Total Score (of 100) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Hip arthroscopic surgery | ||||||||||||
| Beck4 (2019) | 10 | 0 | 5 | 10 | 0 | 5 | 5 | 5 | 10 | 6 | 15 | 71 |
| Chaharbakhshi7 (2017) | 4 | 3 | 5 | 10 | 0 | 5 | 3 | 3 | 10 | 6 | 15 | 64 |
| Cvetanovich12 (2017) | 10 | 0 | 3 | 10 | 0 | 5 | 5 | 3 | 10 | 6 | 15 | 67 |
| Domb14 (2018) | 0 | 3 | 3 | 10 | 0 | 5 | 3 | 3 | 10 | 11 | 15 | 63 |
| Evans17 (2017) | 4 | 0 | 3 | 10 | 0 | 5 | 5 | 3 | 10 | 6 | 15 | 61 |
| Fukui18 (2015) | 7 | 3 | 3 | 10 | 0 | 5 | 5 | 3 | 10 | 6 | 15 | 67 |
| Hatakeyama22 (2018) | 4 | 0 | 5 | 10 | 0 | 5 | 5 | 3 | 10 | 15 | 15 | 72 |
| Maldonado27 (2018) | 7 | 0 | 0 | 10 | 0 | 5 | 3 | 0 | 10 | 6 | 10 | 51 |
| Nawabi34 (2016) | 10 | 0 | 0 | 10 | 0 | 5 | 5 | 0 | 10 | 6 | 15 | 61 |
| Yoon48 (2019) | 4 | 0 | 0 | 10 | 0 | 5 | 5 | 0 | 10 | 11 | 10 | 55 |
| PAO | ||||||||||||
| McClincy29 (2019) | 4 | 0 | 3 | 5 | 0 | 5 | 3 | 0 | 7 | 6 | 5 | 38 |
| Mose32 (2019) | 7 | 0 | 5 | 10 | 10 | 5 | 0 | 0 | 10 | 6 | 10 | 63 |
aPAO, periacetabular osteotomy.
b1 = study size; 2 = mean follow-up; 3 = percentage of patients with follow-up; 4 = number of interventions per group; 5 = study type; 6 = diagnostic certainty; 7 = description of surgical technique; 8 = description of postoperative rehabilitation; 9 = outcome criteria; 10 = procedure for assessing outcomes; 11 = description of participant selection process.
Surgical Procedures
The procedure for the arthroscopic treatment of BDDH varies slightly among surgeons; however, an in-depth description of the procedure was provided in the study by Menge et al.31 In summary, labral repair involves suturing the torn labral fragments back to their approximated anatomic origin to restore the labral seal function. In addition, procedures such as osteoplasty for the correction of bony abnormalities can be performed, along with soft tissue release (ie, psoas or gluteus medius) and other accessory procedures.
An in-depth description of PAO can be found in the study by Ganz et al.19 The main protocols of this procedure include 3 separate osteotomy procedures performed to reposition the acetabulum to approximate a normal angle of acetabular coverage.
Arthroscopic Procedures
Concomitant and accessory arthroscopic procedures performed during surgery along with percentages are recorded in Table 4. All arthroscopic surgery articles provided data on additional procedures, but no such data were reported in the PAO articles.§ The most frequently reported accessory procedures were labral debridement7,14,17,27,34,48 and repair,∥ femoroplasty,4,7,12,14,17,18,22,27 and capsular closure.4,12,18,34,48 The reported rates for labral debridement were as high as 38%17 and as low as 5%,14 while the reported rates for labral repair were much higher, with the lowest reported rate being 26%.17 The studies that provided capsular closure rates all reported that 100% of patients underwent this procedure.4,12,18,34 Furthermore, the reported rates of capsular plication were nearly as high, with all but 3 articles reporting that 100% of patients underwent plication of the capsule.7,14,17,18,22,27,48
TABLE 4.
Arthroscopic Procedures of Included Studiesa
| Beck4 (2019) | Chaharbakhshi7 (2017) | Cvetanovich12 (2017) | Domb14 (2018) | Evans17 (2017) | Fukui18 (2015) | Hatakeyama22 (2018) | Maldonado27 (2018) | Nawabi34 (2016) | Yoon48 (2019) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of hips | 112 | LT tear: 20 | No LT tear: 20 | 36 | 21 | 21 | 102 | 45 | Success: 97 | Failure: 25 | 55 | 47 |
| Acetabular chondroplasty | NR | NR | NR | NR | 6 (29) | 0 (0) | 18 (18) | NR | NR | NR | NR | NR |
| Acetabular decortication | NR | 7 (35) | 8 (40) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Acetabular rim trimming | 95 (85) | NR | NR | 4 (11) | NR | NR | 5 (5) | NR | NR | NR | NR | NR |
| Acetabuloplasty | NR | NR | NR | NR | NR | NR | NR | NR | 43 (44) | 12 (48) | NR | NR |
| Cam and rim decompression | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 5 (9) | NR |
| Cam and subspinal decompression | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 25 (46) | NR |
| Cam decompression | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 54 (98) | NR |
| Cam, rim, and subspinal decompression | NR | NR | NR | NR | NR | NR | 80 (78) | NR | NR | NR | 10 (18) | NR |
| Capsular closure | 112 (100) | NR | NR | 36 (100) | NR | NR | 102 (100) | NR | NR | NR | 55 (100) | NR |
| Capsular plication | NR | 20 (100) | 20 (100) | NR | 21 (100) | 21 (100) | 38 (37) | 45 (100) | 97 (100) | 25 (100) | NR | 15 (32) |
| Capsular shift | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 3 (6) | NR |
| Femoroplasty | 112 (100) | 12 (60) | 16 (80) | 36 (100) | 11 (52) | 15 (71) | 17 (17) | 42 (93) | 79 (81) | 20 (80) | NR | NR |
| Iliopsoas bursectomy | NR | NR | NR | NR | 1 (5) | 3 (14) | NR | NR | NR | NR | NR | NR |
| Iliopsoas fractional lengthening | NR | 9 (45) | 9 (45) | NR | 11 (52) | NR | NR | NR | 67 (69) | 17 (68) | NR | NR |
| Iliopsoas release | NR | NR | NR | 0 (0) | NR | 15 (71) | NR | NR | NR | NR | NR | NR |
| Isolated cam decompression | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 14 (26) | NR |
| Iliotibial band release | NR | NR | NR | 1 (3) | NR | NR | NR | NR | NR | NR | NR | NR |
| Labral debridement | NR | 7 (35) | 7 (35) | NR | 1 (5) | 8 (38) | NR | NR | 20 (21) | 6 (24) | 17 (31) | 3 (6) |
| Labral reconstruction | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Labral repair | 112 (100) | 13 (65) | 13 (65) | 32 (89) | 20 (95) | 13 (62) | 102 (100) | 42 (93) | 76 (78) | 17 (68) | 38 (69) | 12 (26) |
| LT debridement | NR | 20 (100) | 0 (0) | NR | 12 (57) | 3 (14) | 95 (93) | NR | NR | NR | 13 (24) | 9 (19) |
| Microfracture | NR | 1 (5) | 1 (5) | 0 (0) | NR | NR | NR | NR | 5 (5) | 1 (4) | NR | NR |
| Notchplasty | NR | 0 (0) | 1 (5) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Osteochondroplasty | NR | NR | NR | NR | NR | NR | 4 (4) | 42 (93) | NR | NR | 40 (73) | NR |
| Rim decompression | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 15 (27) | NR |
| Rim trimming | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Subspinal decompression | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 35 (64) | NR |
| Synovectomy | NR | 0 (0) | 2 (10) | NR | NR | 3 (14) | NR | NR | NR | NR | NR | 3 (6) |
| Trochanteric bursectomy | NR | NR | NR | 1 (3) | NR | NR | NR | NR | 2 (2) | 2 (8) | NR | NR |
aThis study reported values for both “cam decompression” and “isolated cam decompression.” As there was no explanation for the distinction(s) between the two accessory procedures, both were recorded for the purpose of this review. Studies are presented as first author (year). Values are presented as n (%). LT, ligamentum teres; NR, not reported.
PRO Scores
PRO scores are recorded for the following measures in Tables 5 and 6: modified Harris Hip Score, Hip Outcome Score–Activities of Daily Living, Hip Outcome Score–Sport-Specific Subscale, Nonarthritic Hip Score, visual analog scale for pain, and patient satisfaction. Of significance, only 1 study17 reported on all these measures. Although the articles covering PAO for the treatment of BDDH used different PRO measures than did the arthroscopic surgery articles, values improved across both studies, regardless of the measure.29,32
TABLE 5.
Patient-Reported Outcome Scores of Included Studies: Hip Arthroscopic Surgerya
| First author (Year) | mHHS | HOS-ADL | HOS-SSS | NAHS | VAS Pain | Satisfaction | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | ||
| Beck4 (2019) | 55.6 ± 14.5 | 78.6 ± 17.1 | 63.8 ± 18.7 | 85.5 ± 17.4 | 41.7 ± 20.5 | 72.6 ± 27.1 | NR | NR | 67.2 ± 18.3 | 18.9 ± 21.5 | 77.1 ± 28.5 |
| Chaharbakhshi7 (2017) | LT tear: 64.1 ± 13.5; no LT tear: 66.9 ± 14.3 | LT tear: 81.3 ± 13.7; no LT tear: 87.4 ± 8.9 | NR | NR | LT tear: 44.1 ± 22.8; no LT tear: 50.4 ± 23.9 | LT tear: 68.1 ± 28.9; no LT tear: 75.6 ± 19.6 | LT tear: 63.9 ± 16.2; no LT tear: 67.7 ± 15.4 | LT tear: 81.7 ± 13.9; no LT tear: 88.4 ± 8.9 | LT tear: 5.3 ± 2.6; 5.5 ± 1.9 | LT tear: 2.7 ± 2.5; no LT tear: 2.1 ± 2.1 | LT tear: 8.1; no LT tear: 7.9 |
| Cvetanovich12 (2017) | 57.2 ± 12.3 | 79.9 ± 13.8 | 65.4 ± 16.0 | 88.6 ± 15.2 | 44.5 ± 20.9 | 73.6 ± 26.7 | NR | NR | 7.6 ± 2.4 | 1.4 ± 1.6 | 81.1 ± 22.3 |
| Domb14 (2018) | 70.3 ± 9.8 | 85.9 ± 12.1 | NR | NR | 52.1 ± 15.9 | 70.8 ± 19.5 | 68.3 ± 13.2 | 87.3 ± 9.8 | 5.6 ± 2.5 | 1.8 ± 1.3 | 7.9 ± 1.7 |
| Evans17 (2017) | 59.71 | 88.04 | 62.91 | 94.74 | 42.13 | 81.59 | 62.75 | 91.94 | 6.29 | 1.31 | 7.89 |
| Fukui18 (2015) | 63.5 ± 14 | 84.9 ± 14 | 70.9 ± 13 | 84.7 ± 17 | 51.4 ± 22 | 75.7 ± 25 | NR | NR | NR | NR | 8 |
| Hatakeyama22 (2018) | Success: 72.1; failure: 68.1 | 100 | NR | NR | NR | NR | Success: 72.1; failure: 68.1 | 98.8 | NR | NR | NR |
| Maldonado27 (2018) | 65.4 ± 16.1 | 90.9 ± 7.6 | NR | NR | 45.1 ± 24.8 | 84.7 ± 15.6 | 64.6 ± 18.0 | 90.9 ± 7.6 | 5.2 ± 2.4 | 1.4 ± 1.7 | 8.5 ± 1.7 |
| Nawabi34 (2016) | 61.7 ± 10.9 | 86.2 ± 14.6 | 76 ± 14.4 | 93.2 ± 11.3 | 54.6 ± 23 | 85.4 ± 22.1 | NR | NR | NR | NR | NR |
| Yoon48 (2019) | 61.0 ± 7.6 | 78.6 ± 19.5 | NR | NR | NR | NR | 62.1 ± 7.5 | 80.0 ± 18.5 | 6.1 ± 1.6 | 3.5 ± 2.8 | NR |
aValues are presented as mean ± SD. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; LT, ligamentum teres; mHHS, modified Harris Hip Score; NAHS, Nonarthritic Hip Score; NR, not reported; VAS, visual analog scale.
TABLE 6.
Patient-Reported Outcome Scores of Included Studies: PAOa
| First author (Year) | Preoperative | Postoperative |
|---|---|---|
| McClincy29 (2019) | ||
| mHHS | 64 ± 19 | 86 ± 13 |
| HOOS Pain | 52 ± 23 | 78 ± 25 |
| HOOS Symptoms | 58 ± 22 | 76 ± 22 |
| HOOS Activities of Daily Living | 69 ± 23 | 87 ± 22 |
| HOOS Sport/Recreation | 47 ± 29 | 76 ± 26 |
| HOOS Quality of Life | 32 ± 24 | 66 ± 28 |
| HOOS total | 261 ± 117 | 386 ± 128 |
| SF-12 PCS | 39 ± 12 | 47 ± 11 |
| SF-12 MCS | 51 ± 11 | 52 ± 8 |
| UCLA | 6 ± 2 | 7 ± 2 |
| Mose32 (2019) | ||
| WOMAC total | 69 (57-80) | 90 (78-99) |
| WOMAC pain | 13 (11-15) | 16 (14-20) |
| OHS | 31 (27-35) | 40 (30-47) |
| SF-36 PCS | 38.9 ± 7.9 | 45.5 ± 12.2 |
| SF-36 MCS | 49.5 ± 10.4 | 53.4 ± 10.7 |
aValues are presented as mean ± SD or median (interquartile range). HOOS, Hip disability and Osteoarthritis Outcome Score; MCS, Mental Component Summary; mHHS, modified Harris Hip Score; OHS, Oxford Hip Score; PAO, periacetabular osteotomy; PCS, Physical Component Summary; SF-12, 12-Item Short Form Health Survey; SF-36, 36-Item Short Form Health Survey; UCLA, University of California, Los Angeles; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Revision Arthroscopic Surgery or Conversion to THA
Only 2 articles48 on arthroscopic surgery did not report failure rates, as demonstrated in Appendix Table A2. Furthermore, only 1 of the 2 PAO studies outlined the failure rates resulting in revision arthroscopic surgery or conversion to THA,32 as demonstrated in Appendix Table A3. Across the 12 studies (excluding 3 studies27,29,48), patients in the control, PAO, or arthroscopic surgery group had revision arthroscopic surgery or conversion to THA. The highest rate of revision was 22.2% (22/99; included dysplasia and BDDH) of patients, as seen in the population that underwent PAO in 1 study32 with only 1 case of conversion to THA. The lowest reported rates of revision arthroscopic surgery and conversion to THA were seen in the study with the youngest reported population.17
Discussion
Through our search, 12 articles were identified as fitting our inclusion criteria: 2 studies reviewed the outcomes after PAO, while 10 covered the topic of arthroscopic surgery for the treatment of BDDH. The main findings of this review are the following: (1) When confirming the diagnosis of BDDH, authors used 1 commonly recurring method, which was the LCEA. (2) Concomitant/accessory hip arthroscopic procedures were performed for the treatment of BDDH. (3) It was determined that, whether arthroscopic surgery or PAO was used, outcomes improved across all PRO measures. (4) Revision surgery was common in both procedures.
Hip dysplasia is largely defined based on radiographic evidence of abnormal lateral acetabular coverage, which is assessed by determining the LCEA of a given hip joint. Over the course of this review, BDDH was defined using angles of acetabular coverage ranging from 18° to 25°. Disagreement on the angles of inclusion (18°-25° or 20°-25°) when making a clinically diagnosis was about whether the acetabular abnormality was mild, moderate, or severe. Severe acetabular coverage falls under the definition of a pincer deformity, classifying the disorder as FAI. Wilkin et al45 described the challenge in the treatment of BDDH as being the “variability in its definition,” as supported by their recent review that included LCEAs ranging from 18° to 27° across 18 studies. The study further cited Wiberg44 as describing the initial classification, using an LCEA <20°, of patients having dysplastic hips, and to this day, this is one of the most influential studies on the topic. The consensus across studies over multiple decades is that the lower the LCEA, the greater the risk that dysplastic hips will generate arthritic changes.45 The challenge is that the LCEA is only 1 measurement of a disorder that is multifaceted. Hatakeyama et al22 assessed patients using both the LCEA and the vertical-center-anterior (VCA) angle as diagnostic criteria, and those who had low VCA angles had poorer outcomes than did those with higher VCA angles. However, another study29 included in the current review consisted of patients with BDDH who met the inclusion criteria on >1 measure in addition to the LCEA: the Femoro-Epiphyseal Acetabular Roof index,46 anterior center-edge angle,24 and anterior and posterior wall indices. Of note, other measures that can be used in addition to the LCEA to confirm BDDH diagnoses are the following: an acetabular index >15, a femoral head extrusion index >25%, a Sharp angle >45°, and an acetabular depth ratio <250.45 However, the methods of confirmation for BDDH are not limited to radiographic/imaging findings. The Barlow3 and Ortolani36 methods have been used to identify dislocated hips, indicating laxity, and relocated lax hips as a result, respectively. Moreover, ligamentum teres (LT) ruptures are associated with BDDH because of the hypermobile joints in patients with these ruptures, and the clinical diagnosis for this injury can be used to diagnose BDDH in patients and refer surgeons to the proper surgical method.31 The axial traction apprehension test and the dial test can be used to confirm LT tears in conjunction with other methods to confirm BDDH diagnoses.31 As many other injuries are associated with BDDH and require repair, the use of 1 criterion for diagnostic confirmation to determine which of the 2 surgical methods to use poses a challenge. In conclusion, the use of the LCEA as the main diagnostic criterion is not enough to direct the course of treatment in patients with BDDH.
All studies,¶ except the 2 articles about PAO,29,32 reported concomitant or accessory procedures performed in conjunction with the original arthroscopic surgical procedure for patients with BDDH. As discussed, BDDH is more than just altered acetabular coverage of the femur, and more should be considered when determining the proper procedure used for treatment. A study7 included in the current review considered PAO as a viable option for those who present with BDDH in conjunction with an LT rupture, as such patients have poor outcomes after arthroscopic surgery. Because of this report, it seems that a procedure combining the 2 surgical methods would be a favorable alternative in patients who require more extensive acetabular rim remodeling as well as accessory procedures. Furthermore, as previously mentioned, patients with BDDH have capsular laxity before a surgical intervention, and capsular laxity is often a result of undergoing arthroscopic surgery. Therefore, the high rates of capsular plication and closure across the studies included in the current review indicate that this is a necessary step in the surgical management of BDDH. Targeted treatment of capsular laxity is important to ensure good patient outcomes and reduce the risk of subluxations or dislocations after surgery when treating BDDH. There have been 2 previously published articles that outlined the methods for capsular plication and closure. If the methods described by Uchida et al43 and Menge et al30 are stronger than are standard suturing of the capsule, we should use these techniques to prevent the potential resultant instability in patients with BDDH undergoing arthroscopic surgery.
Moreover, several surgeons reported labral debridement in addition to labral repair, ranging from 5% to 38% across studies.7,14,17,27,34,48 Intraoperative procedures/findings such as debridement and insufficient seal reproduction may lead to the progression of OA. Though hip arthroscopic surgery is aimed at reducing or halting the progression of arthritic changes in the joint, in the setting of patients with FAI, 20% of patients continue to show progression of arthritic changes in the joint at 2 years postoperatively, and it is stipulated that this rate underestimates the actual prevalence.38 This is an indication that hip arthroscopy may not halt the progression of OA in all patients. On the other hand, at 30 years postoperatively, using PAO to treat DDH resulted in 70% of patients progressing to THA because of pain and OA.25 However, there are no comparative studies describing the progression of OA between arthroscopic surgery and PAO for patients with BDDH. Considerations should be taken with either surgical procedure to limit poor outcomes as a result of progressed OA through the identification of risk factors. Additionally, in their systematic review, Kemp et al23 reported the outcomes after hip arthroscopic surgery in patients with OA and concluded that, although patients with hip OA report positive outcomes after hip arthroscopic surgery, this effect may be inflated as a result of methodologic limitations. Comparative studies are required to confirm the effects of both PAO and hip arthroscopic surgery before a surgical intervention for the treatment of patients with OA and BDDH.
Domb et al15 proposed combining arthroscopic surgery and PAO to utilize the best of both methods and improve outcomes. In support of this approach, it may be concluded that PAO does not allow for the assessment of LT ruptures or for their repair. For this, surgeons should recommend that patients with an LCEA <19° undergo treatment that involves a combination of arthroscopic surgery and osteotomy. In the formerly described circumstances, the PAO portion of the surgical procedure could account for rim remodeling, while the arthroscopic portion could repair the LT. In patients with milder dysplasia who do not require as extensive remodeling of the rim (LCEA, 20°-25°), arthroscopic surgery would result in good outcomes as long as emphasis is placed on the proper structures. Arthroscopic surgery used alone for the treatment of BDDH should focus on LT repair, labral repair, minimal rim decompression, and capsular plication in the place of capsular closure. This conclusion is supported by research published by Menge et al,31 who reported the procedure of anatomic arthroscopic LT reconstruction for hip instability.
It is unknown whether it is more imperative to perform bony coverage correction or soft tissue repair (LT, labrum, capsule, etc) in patients with BDDH. In an attempt to determine whether one injury is of more importance than is the other, surgeons have begun to use new surgical methods to rectify BDDH abnormalities and injuries. In 2018, Yamada et al47 reported on using endoscopic shelf acetabuloplasty for the treatment of BDDH. This treatment method involves the repair of intra-articular chondrolabral abnormalities, cam or pincer impingement, and anterolateral acetabular shelf coverage. The method of Yamada et al mimics that of the one described by Uchida et al42 in their study covering endoscopic shelf acetabuloplasty. This particular method of treating patients with BDDH is of consequence because it combines all the effective portions of the different surgical interventions used in the past to treat patients with BDDH: labral repair, cam osteochondroplasty, capsular plication, and shelf acetabuloplasty. On postoperative imaging, patients showed improvements in the LCEA, while PRO scores improved significantly on the modified Harris Hip Score from 70.4 to 97.5.42 The advantages of this procedure are that it is minimally invasive, involves fewer severe complications, and allows for early rehabilitation and, therefore, a quicker recovery. However, the surgical procedure is very technically demanding, it involves the risk of graft fractures and displacement, and it is difficult to treat posterior acetabular cysts because of the portals used for access.47 As the previously mentioned studies by Yamada et al and Uchida et al42 were only recently published in 2018 and 2016, respectively, reports on the procedure and its outcomes are still developing. Long-term outcomes are required to determine if this surgical method is effective for patients suffering from BDDH.
PRO scores were reported across all 12 studies. All studies showed an improvement in scores across all PRO measures. However, the rates of revision hip arthroscopic surgery (0.0%-25.0%) and conversion to THA (0.0%-15.0%) were inconsistent for hip arthroscopic surgery in patients with BDDH. Shah et al40 reported that the failure rate of hip arthroscopic surgery for patients with dysplasia was 25.8% (192/743) at an average of 28.1 months after index arthroscopic surgery and concluded that a smaller LCEA, larger Tönnis angle, broken Shenton line, and decreased joint space (≤2 mm) were the radiographic predictors of failure. Furthermore, Hatakeyama et al22 reported revision rates of up to 25% in patients treated using arthroscopic surgery for BDDH, although the failure rate in the same study for patients aged <42 years was only 6.2%. When choosing the surgical intervention for BDDH, age, the Shenton line (broken), the VCA angle (<17°), femoral head damage (severe), Tönnis grade (>1), and acetabular rim chondral damage should be considered for the mentioned values.22
As a result of this review, we believe that it is imperative that surgeons explore all potential surgical options, considering the indications stemming from individual patients and their associated intra-/extra-articular abnormalities.
Limitations
This review had several limitations. First, there was a risk of publication bias because cases clearly diagnosed as BDDH were published and listed in medical literature search engines, whereas underdiagnosed cases were probably less likely published in the medical literature. A second limitation was that the diagnostic pathway was not validated. Each diagnostic procedure should be assessed to confirm whether it, in fact, exhibits test sensitivity. More research should be conducted on larger sample sizes to determine if the benefits outweigh the risks of these procedures for patients with BDDH. Third, only 2 articles reported on PAO as a treatment method, while 10 reported on arthroscopic surgery for the treatment of BDDH. Fourth, there was a possibility of partial overlapping patients; however, it was minimized to the best of our ability. Fifth, there was a significant difference in the number of patients in both groups. It may have been insufficient to adequately conduct a review, as it is preferable to compare equal amounts of data for accurate extrapolation to the general population. Sixth, variability existed not only in the technique but also in the terminology; a limitation of this study was its ability to effectively categorize concomitant procedures, as each surgeon may have defined the same procedure different from the way another surgeon may have. This could have effectively skewed the results and should therefore be noted as a limitation when interpreting the data.
Conclusion
In conclusion, there is a lack of consensus in the literature on the best treatment method for patients with BDDH. Preoperative patient characteristics and concomitant injuries should be considered when evaluating which surgical procedure will result in the most favorable outcomes. In addition, new surgical methods require further research to determine their efficacy in the treatment of patients with BDDH.
Appendix
TABLE A1.
Institution, Overlapping Authors, and Extraction Period of Included Studiesa
| First author (Year) | Institution | Overlapping Authors | Extraction Period |
|---|---|---|---|
| Beck4 (2019) | Department of Orthopaedic Surgery, Rush University Medical Center | None | 1/2012 to 1/2017 |
| Chaharbakhshi6 (2019)a | American Hip Institute | Domb, Perets | 4/2010 to 11/2014 |
| Chaharbakhshi7 (2017) | American Hip Institute | Domb, Perets | 2/2008 to 4/2014 |
| Chandrasekaran8 (2017)a | American Hip Institute and Hinsdale Orthopaedics | Domb | 4/2008 to 4/2013 |
| Cvetanovich12 (2017) | Rush University Medical Center | None | 1/2012 to 1/2014 |
| Domb14 (2018) | American Hip Institute and Hinsdale Orthopaedics | Chaharbakhshi, Perets | 2/2008 to 12/2010 |
| Domb16 (2013)b | American Hip Institute and Hinsdale Orthopaedics | None | 4/2008 to 11/2010 |
| Evans17 (2017)c | Larner College of Medicine, University of Vermont; Southeast Orthopedic Specialists; University of Illinois College of Medicine; Pritzker School of Medicine, University of Chicago; Stritch School of Medicine, Loyola University Chicago; and American Hip Institute | Chaharbakhshi, Domb | 1/2008 to 1/2013 |
| Fukui18 (2015) | Steadman Philippon Research Institute | None | 6/2005 to 3/2011 |
| Hatakeyama22 (2018) | Wakamatsu Hospital, University of Occupational and Environmental Health | None | 3/2009 to 12/2014 |
| Maldonado27 (2018)d | American Hip Institute | Domb, Perets | 11/2008 to 1/2015 |
| Nawabi34 (2016) | Hospital for Special Surgery | None | 3/2009 to 7/2012 |
| Yoon48 (2019) | Department of Orthopedic Surgery, Jeonbuk National University Medical School | None | 3/2015 to 12/2017 |
| McClincy29 (2019) | Child and Young Adult Hip Preservation Program, Department of Orthopedic Surgery, Boston Children’s Hospital | None | 1/2010 to 12/2014 |
| Mose32 (2019) | Department of Orthopedics, School of Medical Sciences, Örebro University | None | 1/2010 to 8/2011 |
aChaharbakhshi et al6 (2019) and Chandrasekaran et al8 (2017) were excluded because the authors were affiliated with the same institution as Chaharbakhshi et al7 (2017) and had a shorter duration of inclusion.
bDomb et al16 (2013) was excluded because the authors were affiliated with the same institution as those of Domb et al14 (2018) and had shorter follow up from an older period (i.e. less recent results).
cEvans et al17 (2017) was included because more institutions other than the American Hip Institute were involved; this could have been a result of multisite research and, therefore, a multisite patient population. Additionally, this study involved a younger patient population (<18 years); again, more likely there was less overlap, as no other included study had this inclusion/exclusion criterion.
dMaldonado et al27 (2018) was included because it had different and more precise inclusion/exclusion criteria than did the other studies included; this could also have minimized patient overlap before publication, and thus, this article was included.
TABLE A2.
Failure Rate of Included Studies: Hip Arthroscopic Surgerya
| First author (Year) | Follow-up,b mo | No. of Hips | Revision Hip Arthroscopic Surgery | Conversion to THA | ||
|---|---|---|---|---|---|---|
| n (%) | Description | n (%) | Description | |||
| Beck4 (2019) | 24 | 112 | 1 (0.9) | NR | 1 (0.9) | NR |
| Chaharbakhshi7 (2017) | 54.3 (24.2-83.8) | LT tear: 20; no LT tear: 20 | LT tear: 5 (25.0); no LT tear: 1 (5.0) | The mean time to revision was 22.9 mo (range, 4.1-48.1 mo). One case of revision consisted of loose body removal and recurrent LT debridement for partial tearing. There were 2 patients who each required 2 revisions: (1) One of these patients underwent revision arthroscopic surgery at 7.1 and 47.9 mo from the index arthroscopic procedure and ultimately underwent THA. (2) The remaining 2 revisions in the LT tear group were performed in 1 patient at 7.1 and 48.1 mo for recurrent chondral defects and labral tearing. One patient in the control group underwent revision at 1.8 mo from the index procedure for an underresected femoral neck deformity and recurrent labral tearing, which resulted in the alleviation of symptoms. | LT tear: 3 (15.0); no LT tear: 0 (0.0) |
Patient 1: age, 51.7 y; female;
BMI, 30.6; index arthroscopic findings of Seldes type I,
ALAD grade 1, acetabular Outerbridge grade 1, and
femoral head Outerbridge grade 0; primary procedure of
labral debridement; time to THA, 62.0 mo. Patient 2: age, 44.2 y; female; BMI, 29.1; index arthroscopic findings of Seldes type I, ALAD grade 2, acetabular Outerbridge grade 1 with a 2.5-cm2 defect, femoral head Outerbridge grade 0, and a cam lesion; primary procedure of labral repair, femoroplasty, and microfracture; time to THA, 16.6 mo. Patient 3: age, 48.2 y; female; BMI, 21.4; index arthroscopic findings of Seldes type II, ALAD grade 1, acetabular Outerbridge grade 1, femoral head Outerbridge grade 0, and a cam lesion; primary procedure of labral debridement and femoroplasty; time to THA, 48.5 mo. |
| Cvetanovich12 (2017) | 31.2 ± 7.2 | 36 | 1 (2.8) | NR | 0 (0.0) | NR |
| Domb14 (2018) | 68.8 ± 6.4 (60.0-93.8) | 21 | 4 (19.0) | The mean time to revision was 25.1 ± 19.2 mo (range, 4.1-50.1 mo). There were 2 hips that underwent loose body removal, 1 of which was for heterotopic ossification measuring >5 mm and the other was for residual suture material related to a rupture from previous capsular plication. All patients were noted to have improvements in PRO scores at a mean of 42.3 mo after revision. | 0 (0.0) | NR |
| Evans17 (2017) | 26.3 | 21 | 0 (0.0) | NR | 0 (0.0) | NR |
| Fukui18 (2015) | 40 (24-97) | 80 | 7 (8.8) |
Patient 1: Primary arthroscopic
procedure: pincer impingement, debridement of the LT,
and closure of capsulotomy; revision arthroscopic
procedure: adhesions and labral reconstruction. Patient 2: Primary arthroscopic procedure: cam impingement, pincer impingement, debridement of the LT, and closure of capsulotomy; revision arthroscopic procedure: adhesions and trochanteric bursitis. Patient 3: Primary arthroscopic procedure: cam impingement, pincer impingement, microfracture of the acetabulum, debridement of the LT, and closure of capsulotomy; revision arthroscopic procedure: adhesions and cam regrowth. Patient 4: Primary arthroscopic procedure: cam impingement, pincer impingement, debridement of the LT, and closure of capsulotomy; revision arthroscopic procedure: adhesions. Patient 5: Primary arthroscopic procedure: cam impingement, pincer impingement, debridement of the LT, and closure of capsulotomy; revision arthroscopic procedure: adhesions, iliotibial band and psoas release, trochanteric bursitis, and new acetabular chondral defect. Patient 6: Primary arthroscopic procedure: cam impingement, pincer impingement, microfracture of the acetabulum, debridement of the LT, and closure of capsulotomy; revision arthroscopic procedure: adhesions, unaddressed cam impingement, and new acetabular chondral defect. Patient 7: Primary arthroscopic procedure: cam impingement, pincer impingement, debridement of the LT, and closure of capsulotomy; revision arthroscopic procedure: adhesions and small labral injury. |
5 (6.3) | There were 4 men and 1 woman with a mean age of 42 y at a mean of 2 y (range, 11-48 mo) after arthroscopic surgery. |
| Hatakeyama22 (2018) | 42.5 (24.0-72.6) | 45 | 7 (15.6) | There were 2 patients who underwent revision arthroscopic surgery (trimming for osteophytes at the cotyloid fossa, labral repair, cam osteochondroplasty, and microfracture at the acetabulum) because of the progression of OA and labral retearing, and 5 underwent arthroscopic shelf acetabuloplasty. | 2 (4.4) | THA performed because of progressive OA with lateral migration of the femoral head. |
| Maldonado27 (2018) | Success: 39.2 ± 17.3; failure: 42.8 ± 20.4 | 122 | NR | NR | NR | NR |
| Nawabi34 (2016) | 31.3 ± 7.6 (23.1-67.3) | 46 | 2 (4.3) | At a mean of 9.6 and 23.8 mo after arthroscopic surgery, 1 patient underwent revision for painful adhesions, and 1 patient underwent it for recurrent labral tearing, respectively. | 0 (0.0) | NR |
| Yoon48 (2019) | 25.9 | 47 | NR | NR | NR | NR |
aALAD, acetabular labrum articular disruption; BMI, body mass index; LT, ligamentum teres; NR, not reported; OA, osteoarthritis; PRO, patient-reported outcome; THA, total hip arthroplasty.
bValues are presented as mean ± SD (and range, if shown).
TABLE A3.
Failure Rate of Included Studies: PAOa
| First author (Year) | Mean Follow-up, mo | No. of Patients | Revision Hip Arthroscopic Surgery | Conversion to THA | ||
|---|---|---|---|---|---|---|
| n (%) | Description | n (%) | Description | |||
| McClincy29 (2019) | 26.4 | 49 | NR | NR | NR | NR |
| Mose32 (2019) | 24 | 99b | 22 (22.2)b | There were 14 patients with type 3a tears, 1 patient with a type 3b tear, and 1 patient with a type 1 tear. Also, 4 patients were preoperatively classified as having type 0 tears, but during arthroscopic surgery, the labrum was found to be affected in 3 patients and was treated accordingly. | 1 (1.0)b | NR |
aNR, not reported; PAO, periacetabular osteotomy; THA, total hip arthroplasty.
bThere were 44 patients with borderline dysplasia (lateral center-edge angle of 20°-25°) and 55 with dysplasia (lateral center-edge angle <20°), which we could not distinguish.
Footnotes
Final revision submitted May 15, 2020; accepted June 8, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.J.P. has received educational support from Linvatec; speaking fees and consulting fees from Smith & Nephew; royalties from DJO, Linvatec, and Smith & Nephew; and hospitality payments from Siemens. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72(6):918–923. [DOI] [PubMed] [Google Scholar]
- 2. Agricola R, Waarsing JH, Arden NK, et al. Cam impingement of the hip: a risk factor for hip osteoarthritis. Nat Rev Rheumatol. 2013;9(10):630–634. [DOI] [PubMed] [Google Scholar]
- 3. Barlow TG. Congenital dislocation of the hip: early diagnosis and treatment. Lond Clin Med J. 1964;5:47–58. [PubMed] [Google Scholar]
- 4. Beck EC, Nwachukwu BU, Chahla J, et al. Patients with borderline hip dysplasia achieve clinically significant outcome after arthroscopic femoroacetabular impingement surgery: a case-control study with minimum 2-year follow-up. Am J Sports Med. 2019;47(11):2636–2645. [DOI] [PubMed] [Google Scholar]
- 5. Bialik V, Bialik GM, Blazer S, Sujov P, Wiener F, Berant M. Developmental dysplasia of the hip: a new approach to incidence. Pediatrics. 1999;103(1):93–99. [DOI] [PubMed] [Google Scholar]
- 6. Chaharbakhshi EO, Hartigan DE, Perets I, Domb BG. Is hip arthroscopy effective in patients with combined excessive femoral anteversion and borderline dysplasia? A match-controlled study. Am J Sports Med. 2019;47(1):123–130. [DOI] [PubMed] [Google Scholar]
- 7. Chaharbakhshi EO, Perets I, Ashberg L, Mu B, Lenkeit C, Domb BG. Do ligamentum teres tears portend inferior outcomes in patients with borderline dysplasia undergoing hip arthroscopic surgery? A match-controlled study with a minimum 2-year follow-up. Am J Sports Med. 2017;45(11):2507–2516. [DOI] [PubMed] [Google Scholar]
- 8. Chandrasekaran S, Darwish N, Martin TJ, Suarez-Ahedo C, Lodhia P, Domb BG. Arthroscopic capsular plication and labral seal restoration in borderline hip dysplasia: 2-year clinical outcomes in 55 cases. Arthroscopy. 2017;33(7):1332–1340. [DOI] [PubMed] [Google Scholar]
- 9. Clohisy JC, Ackerman J, Baca G, et al. Patient-reported outcomes of periacetabular osteotomy from the prospective ANCHOR cohort study. J Bone Joint Surg Am. 2017;99(1):33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10(1):2–11. [DOI] [PubMed] [Google Scholar]
- 11. Coobs BR, Xiong A, Clohisy JC. Contemporary concepts in the young adult hip patient: periacetabular osteotomy for hip dysplasia. J Arthroplasty. 2015;30(7):1105–1108. [DOI] [PubMed] [Google Scholar]
- 12. Cvetanovich GL, Levy DM, Weber AE, et al. Do patients with borderline dysplasia have inferior outcomes after hip arthroscopic surgery for femoroacetabular impingement compared with patients with normal acetabular coverage? Am J Sports Med. 2017;45(9):2116–2124. [DOI] [PubMed] [Google Scholar]
- 13. Ding Z, Sun Y, Liu S, Chen J. Hip arthroscopic surgery in borderline developmental dysplastic hips: a systematic review. Am J Sports Med. 2019;47(10):2494–2500. [DOI] [PubMed] [Google Scholar]
- 14. Domb BG, Chaharbakhshi EO, Perets I, Yuen LC, Walsh JP, Ashberg L. Hip arthroscopic surgery with labral preservation and capsular plication in patients with borderline hip dysplasia: minimum 5-year patient-reported outcomes. Am J Sports Med. 2018;46(2):305–313. [DOI] [PubMed] [Google Scholar]
- 15. Domb BG, LaReau JM, Hammarstedt JE, Gupta A, Stake CE, Redmond JM. Concomitant hip arthroscopy and periacetabular osteotomy. Arthroscopy. 2015;31(11):2199–2206. [DOI] [PubMed] [Google Scholar]
- 16. Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41(11):2591–2598. [DOI] [PubMed] [Google Scholar]
- 17. Evans PT, Redmond JM, Hammarstedt JE, Liu Y, Chaharbakhshi EO, Domb BG. Arthroscopic treatment of hip pain in adolescent patients with borderline dysplasia of the hip: minimum 2-year follow-up. Arthroscopy. 2017;33(8):1530–1536. [DOI] [PubMed] [Google Scholar]
- 18. Fukui K, Briggs KK, Trindade CA, Philippon MJ. Outcomes after labral repair in patients with femoroacetabular impingement and borderline dysplasia. Arthroscopy. 2015;31(12):2371–2379. [DOI] [PubMed] [Google Scholar]
- 19. Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 20. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 21. Gray BL, Stambough JB, Baca GR, Schoenecker PL, Clohisy JC. Comparison of contemporary periacetabular osteotomy for hip dysplasia with total hip arthroplasty for hip osteoarthritis. Bone Joint J. 2015;97-B(10):1322–1327. [DOI] [PubMed] [Google Scholar]
- 22. Hatakeyama A, Utsunomiya H, Nishikino S, et al. Predictors of poor clinical outcome after arthroscopic labral preservation, capsular plication, and cam osteoplasty in the setting of borderline hip dysplasia. Am J Sports Med. 2018;46(1):135–143. [DOI] [PubMed] [Google Scholar]
- 23. Kemp JL, MacDonald D, Collins NJ, Hatton AL, Crossley KM. Hip arthroscopy in the setting of hip osteoarthritis: systematic review of outcomes and progression to hip arthroplasty. Clin Orthop Relat Res. 2015;473(3):1055–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lequesne MG, Laredo JD. The faux profil (oblique view) of the hip in the standing position: contribution to the evaluation of osteoarthritis of the adult hip. Ann Rheum Dis. 1998;57(11):676–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lerch TD, Steppacher SD, Liechti EF, Tannast M, Siebenrock KA. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res. 2017;475(4):1154–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Leunig M, Ganz R. The evolution and concepts of joint-preserving surgery of the hip. Bone Joint J. 2014;96-B(1):5–18. [DOI] [PubMed] [Google Scholar]
- 27. Maldonado DR, Perets I, Mu BH, et al. Arthroscopic capsular plication in patients with labral tears and borderline dysplasia of the hip: analysis of risk factors for failure. Am J Sports Med. 2018;46(14):3446–3453. [DOI] [PubMed] [Google Scholar]
- 28. Malviya A, Stafford GH, Villar RN. Is hip arthroscopy for femoroacetabular impingement only for athletes? Br J Sports Med. 2012;46(14):1016–1018. [DOI] [PubMed] [Google Scholar]
- 29. McClincy MP, Wylie JD, Kim YJ, Millis MB, Novais EN. Periacetabular osteotomy improves pain and function in patients with lateral center-edge angle between 18 degrees and 25 degrees, but are these hips really borderline dysplastic? Clin Orthop Relat Res. 2019;477(5):1145–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Menge TJ, Chahla J, Soares E, Mitchell JJ, Philippon MJ. The Quebec City Slider: a technique for capsular closure and plication in hip arthroscopy. Arthrosc Tech. 2016;5(5):e971–e974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Menge TJ, Mitchell JJ, Briggs KK, Philippon MJ. Anatomic arthroscopic ligamentum teres reconstruction for hip instability. Arthrosc Tech. 2016;5(4):e737–e742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mose FB, Mechlenburg I, Hartig-Andreasen C, Gelineck J, Soballe K, Jakobsen SS. High frequency of labral pathology in symptomatic borderline dysplasia: a prospective magnetic resonance arthrography study of 99 patients. J Hip Preserv Surg. 2019;6(1):60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Murata Y, Uchida S, Utsunomiya H, Hatakeyama A, Nakamura E, Sakai A. A comparison of clinical outcome between athletes and nonathletes undergoing hip arthroscopy for femoroacetabular impingement. Clin J Sport Med. 2017;27(4):349–356. [DOI] [PubMed] [Google Scholar]
- 34. Nawabi DH, Degen RM, Fields KG, et al. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med. 2016;44(4):1017–1023. [DOI] [PubMed] [Google Scholar]
- 35. Nishii T, Sugano N, Tanaka H, Nakanishi K, Ohzono K, Yoshikawa H. Articular cartilage abnormalities in dysplastic hips without joint space narrowing. Clin Orthop Relat Res. 2001;383:183–190. [DOI] [PubMed] [Google Scholar]
- 36. Ortolani M. Congenital hip dysplasia in the light of early and very early diagnosis. Clin Orthop Relat Res. 1976;119:6–10. [PubMed] [Google Scholar]
- 37. Philippon MJ, Arnoczky SP, Torrie A. Arthroscopic repair of the acetabular labrum: a histologic assessment of healing in an ovine model. Arthroscopy. 2007;23(4):376–380. [DOI] [PubMed] [Google Scholar]
- 38. Rhon DI, Greenlee TA, Sissel CD, Reiman MP. The two-year incidence of hip osteoarthritis after arthroscopic hip surgery for femoroacetabular impingement syndrome. BMC Musculoskelet Disord. 2019;20(1):266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Saberi Hosnijeh F, Zuiderwijk ME, Versteeg M, et al. Cam deformity and acetabular dysplasia as risk factors for hip osteoarthritis. Arthritis Rheumatol. 2017;69(1):86–93. [DOI] [PubMed] [Google Scholar]
- 40. Shah A, Kay J, Memon M, et al. Clinical and radiographic predictors of failed hip arthroscopy in the management of dysplasia: a systematic review and proposal for classification. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1296–1310. [DOI] [PubMed] [Google Scholar]
- 41. Stone AV, Mehta N, Beck EC, et al. Comparable patient-reported outcomes in females with or without joint hypermobility after hip arthroscopy and capsular plication for femoroacetabular impingement syndrome. J Hip Preserv Surg. 2019;6(1):33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Uchida S, Hatakeyama A, Kanezaki S, et al. Endoscopic shelf acetabuloplasty can improve clinical outcomes and achieve return to sports-related activity in active patients with hip dysplasia. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):3165–3177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Uchida S, Pascual-Garrido C, Ohnishi Y, et al. Arthroscopic shoelace capsular closure technique in the hip using Ultratape. Arthrosc Tech. 2017;6(1):e157–e161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83(suppl 58):7–38. [Google Scholar]
- 45. Wilkin GP, Ibrahim MM, Smit KM, Beaule PE. A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. J Arthroplasty. 2017;32(9)(suppl):S20–S27. [DOI] [PubMed] [Google Scholar]
- 46. Wyatt M, Weidner J, Pfluger D, Beck M. The Femoro-Epiphyseal Acetabular Roof (FEAR) index: a new measurement associated with instability in borderline hip dysplasia? Clin Orthop Relat Res. 2017;475(3):861–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yamada K, Matsuda DK, Suzuki H, Sakai A, Uchida S. Endoscopic shelf acetabuloplasty for treating acetabular large bone cyst in patient with dysplasia. Arthrosc Tech. 2018;7(7):e691–e697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yoon SJ, Lee SH, Jang SW, Jo S. Hip arthroscopy of a painful hip with borderline dysplasia. Hip Pelvis. 2019;31(2):102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]