Abstract
Introduction
Racial/ethnic and socioeconomic disparities in diabetes prevalence and management persist. Unmet basic needs such as food insecurity and unstable housing interfere with optimal diabetes self-management. Bridge to Health/Puente a la Salud is a randomized pilot trial designed to examine the feasibility of testing the effectiveness of addressing unmet basic needs via navigation services versus navigation plus diabetes self-management support (DSMS) on improving diabetes-related outcomes among racial/ethnic minority and low-income patients with uncontrolled diabetes.
Material and methods
We recruited and randomized 110 African American, Hispanic, and Medicaid patients (any race/ethnicity) with diabetes and recent hemoglobin A1C ≥ 8% to one of two 6-month interventions: 1) Navigation only; or 2) Navigation + DSMS. In both arms, practice-embedded patient navigators help participants navigate social services and community-based resources to address unmet basic needs. In Navigation + DSMS, participants are also assigned to a community health worker (CHW) embedded in a local community-based organization who provides additional navigation support and delivers DSMS. A1C and unmet basic needs data are collected via routine lab and survey, respectively, at baseline and 6-month follow-up. Qualitative interviews with participants, health system leaders, CHWs, and patient navigators are conducted to explore intervention acceptability and determinants of implementation in a health care setting.
Discussion
Findings from this pilot feasibility study will enhance understanding about acceptability, preliminary clinical effectiveness, and facilitators and barriers to implementation of the Navigation only and Navigation + DSMS interventions and inform refinements of the overall study design for the larger, randomized clinical trial.
Keywords: Diabetes, Unmet basic needs, Navigation, Diabetes self-management, And community health workers
1. Introduction
In the U.S., 11.7% of African Americans and 12.5% of Hispanics have type 2 diabetes, compared to only 7.5% of Whites [1]. In addition to disparities in prevalence of diabetes, racial/ethnic minorities and individuals with low socioeconomic status (SES) are less likely than White individuals and those with higher SES, respectively, to achieve diabetes-related clinical targets (e.g., A1C < 7.0%) [[1], [2], [3]], and are therefore at higher risk for diabetes complications and adverse cardiovascular outcomes [3]. These disparities are exacerbated by the presence of unmet basic needs, such as food insecurity, insufficient housing, difficulty paying for medical care, and lack of transportation. Unmet basic needs interfere with adequate diabetes self-management behaviors, including healthy eating, physical activity, self-monitoring of blood glucose, and medication adherence leading to poor glycemic control [[4], [5], [6], [7], [8], [9], [10], [11]], increased healthcare utilization, and higher health care costs [[12], [13], [14]]. Thus, there is a need for effective, comprehensive behavioral interventions that address the social, behavioral, and economic factors that impede optimal diabetes self-management among racial/ethnic minority and low-income patients.
Health system-based social health interventions to address unmet basic needs usually consist of helping patients navigate social services and community-based resources. Navigation, also known as “linkage interventions,” have been associated with reduction in food insecurity [15], homelessness [16], unnecessary healthcare utilization (e.g., emergency department visits) and costs [[17], [18], [19], [20]]. It has been suggested that alleviating the socioeconomic stressors that often supersede diabetes management, may result in improved self-care behaviors, followed by subsequent improved diabetes-related outcomes [21]. However, results from the few studies that have examined the effects of navigation programs on A1C [[22], [23], [24]], suggest that addressing unmet basic needs alone may not be sufficient to improve outcomes for a complex disease such as diabetes [25]. Findings from recent research indicated that when community health workers (CHWs) provided both navigation to community resources and disease self-management support, patients experienced an improvement in glycemic control, blood pressure, and self-rated mental health [26,27]. Thus, the overarching goal of our work is to determine the effectiveness of navigation alone compared to a combined diabetes self-management and social health intervention on diabetes-related outcomes. Before conducting a large, pragmatic, randomized trial, we sought to test the feasibility and acceptability of this study design in the target population.
Bridge to Health/Puente a la Salud (R34DK119853) is a two-year, randomized feasibility study funded in September 2018. Recruitment has been completed and 110 eligible participants were randomized to one of two 6-month study conditions: 1) navigation to community resources only (Navigation); or 2) navigation plus diabetes self-management support (Navigation + DSMS). The aims of the study are to:
-
1.
Determine intervention feasibility based on recruitment and retention rates as well as other intervention process measures;
-
2.
Assess intervention acceptability and determinants of sustainability based on semi-structured qualitative interviews with participants, patient navigators, CHWs, and health system leaders; and
-
3.
Examine preliminary effectiveness by comparing the two study arms on A1C and healthcare utilization at 6 months post-randomization.
This manuscript describes the study design and the protocols for recruitment, intervention delivery, data collection, and analyses.
2. Materials and methods
2.1. Design
Bridge to Health/Puente a la Salud is a two-arm, randomized pilot and feasibility study with a qualitative component to examine facilitators and barriers to intervention implementation and sustainability. This study was approved by the Institutional Review Board of Kaiser Permanente Northwest (Portland, OR).
2.2. Setting
Participants were members of Kaiser Permanente Northwest (KPNW), a large integrated non-profit health care system that provides comprehensive prepaid health care to its more than 620,000 members in Oregon and southwest Washington. Prior to this study being funded, racial/ethnic health disparities in diabetes management were present at KPNW, with a 3–15% gap in achieving the clinical target of A1C < 8% between Hispanic and non-Hispanic White members, and a 2–9% gap between African American and non-Hispanic White members across primary care clinics.
In addition to providing comprehensive, integrated care, KPNW has a patient navigation program that has been in existence for five years. Patient navigators are embedded in the health system to assist with connecting patients to internal medical services and/or community-based resources. Thirty navigators are embedded in primary care clinics and emergency departments across the region, and they document their work in the electronic health record (EHR). Patient navigators come from diverse educational backgrounds, are trained in motivational interviewing and receive regular supervision by a Patient Navigator Program manager. Navigators engage with patient clinical teams in a variety of ways (e.g., documentation in the EHR, face-to-face case management) depending on the urgency and specificity of the unmet medical or social service need of the patient. In Bridge to Health/Puente a la Salud, KPNW patient navigators provided navigation services to participants in both study arms.
2.3. Community partners
Given that community health workers (CHWs) can play an effective role in addressing patient medical, social and economic needs [20,22,23,28] as well as enhancing diabetes self-management [[29], [30], [31]], we utilized CHWs to deliver diabetes self-management support and provide additional navigation to community-based resources to participants in the Navigation + DSMS arm. CHWs were embedded in six culturally-specific community-based organizations (CBOs) in Portland, Oregon that agreed to partner with us to implement this study – Familias en Acción, Latino Network, Northwest Family Services, Impact Northwest, Volunteers of America, and Portland Opportunities Industrialization Center. In addition, we collaborated with Project Access NOW (PANOW), another local CBO, that served as the hub in terms of facilitating referrals from our study team to their CHWs.
2.4. Participants
Study participants recruited from KPNW met the following inclusion criteria: 1) aged 18 years or older; 2) identified as African American or Hispanic, or a Medicaid recipient of any racial or ethnic background; 3) preferred language was English or Spanish; 4) had a diagnosis of type 2 diabetes with most recent hemoglobin A1C ≥ 8% measured on or after January 2017; and 5) at the time of eligibility screening endorsed one or more unmet basic needs. Medicaid health insurance coverage was used as a proxy for low-income status given that patient-level SES variables are not available in the KPNW EHR. Patients were ineligible if any of the above criteria were not met, had already worked with a KPNW patient navigator in the past two months prior to recruitment, or if they were unable to provide verbal informed consent due to cognitive or psychiatric impairment.
2.5. Procedures
2.5.1. Recruitment
The study team aimed to enroll 100 participants. KPNW members who met the demographic and clinical inclusion criteria were identified using the EHR. Study staff sent eligible patients targeted recruitment emails and letters that provided an overview of the study and a contact number for potential participants to call and screen for eligibility. After 2–3 business days, study staff followed up on the recruitment letter mailing/email with a phone call to potentially eligible participants to describe the study and further assess eligibility by confirming African American or Hispanic race/ethnicity or Medicaid coverage, as well as administering the Your Current Life Situation (YCLS), a 9-item social needs screener to determine if at least one unmet basic need was endorsed. The YCLS is administered in English or Spanish and assesses the following domains: living situation, concerns about living situation, financial hardship, food insecurity, transportation, and help with activities of daily living [32]. Respondents who met study criteria provided verbal informed consent prior to being enrolled. Recruitment took place from March to mid-October 2019 and is now complete with 110 participants enrolled. Exceeding the target enrollment rate was intentional, in an anticipation of participants being lost to follow-up or terminating the study early. Recruitment and referral data were managed using REDCap and Clara, a web-based client tracking tool and database application. REDCap was managed by our study team with PANOW having limited, shared access and Clara was managed by PANOW with our study team receiving monthly documentation reports.
2.5.2. Randomization
Eligible patients were randomized to the two study arms (Navigation vs. Navigation + DSMS) at a 1:1 ratio. Because there are significant differences in achievement of diabetes-related clinical targets by race/ethnicity [1,2], sex [2], and body mass index (BMI) [2], we stratified randomization by sex (female, male), race/ethnicity (White, non-White) and BMI (<30, ≥30). Given the nature of this trial, participants could not be blinded to randomization assignment.
2.5.3. Retention strategies
To retain participants in the study, we use some of the proven approaches described by Yancey et al. [33] for retaining racial/ethnic minorities in research. Specifically, patient navigators and CHWs maintain regular contact via phone or home visits with participants, and when possible, study staff, navigators, and CHWs match the target population in race/ethnicity, cultural background, and language. As an additional retention strategy, participants are sent birthday cards. Participants receive up to $50 for completing the 6- month follow-up visit, which include completing the YCLS (social needs screener) and an A1C test.
2.6. Interventions
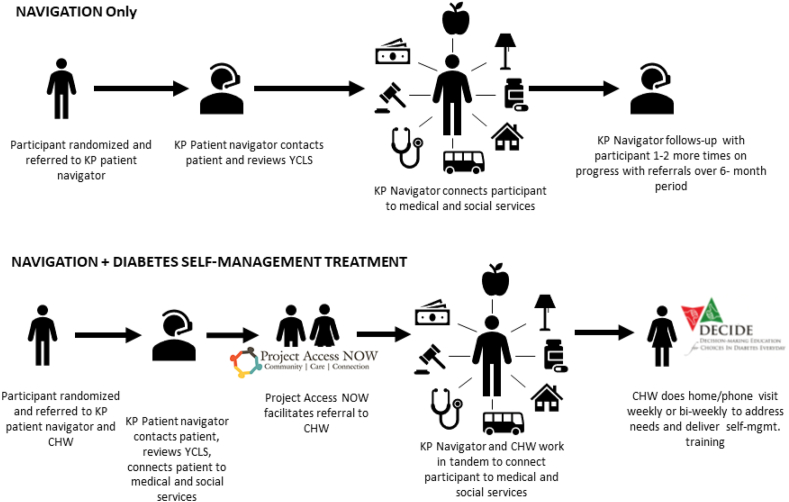
Participants in both study arms are sent diabetes educational materials from the American Diabetes Association (ADA), in English and Spanish, by mail every month for six months to provide basic diabetes management education and to keep them engaged in the study. In addition, participants were encouraged to continue receiving ‘usual care,’ which consisted of provider-prescribed diabetes treatment regimen including medication management, self-monitoring of blood glucose, and A1C checks every 3–6 months. Fig. 1 displays the flow diagram for each intervention arm.
Fig. 1.
Bridge to Health/Puente a la Salud Intervention Arms. KP = Kaiser Permanente; YCLS = Your Current Life Situation (social needs screener); CHW = Community Health Worker; DECIDE = Decision-making Education for Choices in Diabetes Everyday.
2.6.1. Navigation only
In the Navigation Only arm, KPNW navigators embedded within primary care clinics help connect participants to social services and community-based resources to address identified unmet basic needs. After randomization, study staff place a referral to the patient navigators using a standard EHR-based referral process. Once patient navigators receive the referral, they follow up within 14–21 days by phone or secure email through the patient portal to address the identified unmet basic needs by providing referrals to community-based resources or assisting with enrollment in Medicaid or the Supplemental Nutrition Assistance Program (SNAP), for example. During the course of the 6-month intervention period, patient navigators follow up with the participant 1–3 times by phone or in person regarding progress with referrals and help address additional needs that may develop during that timeframe.
2.6.2. Navigation plus diabetes self-management support
Participants randomized to the Navigation + DSMS arm are also referred to a KPNW patient navigator similar to participants in the Navigation only arm. However, in addition, participants in this arm are assigned to a trained CHW who delivers the DSMS curriculum and provides additional navigation support in collaboration with the KPNW patient navigator, as needed, over the 6-month intervention period. Specifically, once a participant is randomized to this arm, study staff notify PANOW via email that a new participant has been enrolled. PANOW would then assign a CHW to the participant considering the participant's cultural background, preference, previous experience with the CBO the CHW is embedded in, and geographical location, as well as the CHW's current caseload. Once an assignment is made, study staff inform the participant of the CHW's name and contact information to deliver a warm hand-off for the referral. Furthermore, study staff provide the CHWs name and contact information to the clinical care team by sending a staff message to the primary care provider, and adding the CHW as an additional care team member as well as placing a progress note with CHW contact information in the patient's EHR. CHWs also receive contact information for the patient's primary care provider and could engage with the patient's care team via the patient navigator or directly by phone. However, CHWs do not have access to document directly in the patient's EHR.
Upon receipt of a participant referral, CHWs are expected to contact participants within a week to schedule an initial meeting either in the participant's home or another public setting (e.g., library, church, café). During the initial visit, the CHW follows up on community-based referrals already placed by the KPNW patient navigator and assesses for additional unmet basic needs. CHWs apply the Pathways to Health Model [34], a step-by-step process to efficiently track activities and progress towards addressing participant unmet basic needs during the 6-month intervention period. There are 31 possible Pathways (e.g., Food Access, Employment, Health Insurance Coverage, Housing, Transportation), each involving a 3-step process (referral, check-in at 2 weeks, check-in at 30 days) that need to be achieved to ‘close’ or ‘resolve the Pathway.’
In addition to addressing unmet basic needs, during weekly and bi-weekly visits (in person or over the phone) CHWs deliver the American Diabetes Association approved DSMS program, Decision-making Education for Choices In Diabetes Everyday (DECIDE). DECIDE is a nine-module, low-literacy- adapted diabetes and cardiovascular disease (CVD) education and problem-solving training program [34,35]. It uses problem-solving training as an evidence-based behavior change skill to facilitate identifying and managing barriers to diabetes self-management [36]. In the first session of DECIDE participants are taught the clinical targets for diabetes-related outcomes (i.e., A1C, fasting blood glucose, blood pressure, LDL, and HDL) and self-management behaviors needed to achieve those targets (i.e., healthy eating, engagement in physical activity, medication adherence, and attending medical appointments). The remaining eight sessions focus on teaching participants the five steps of problem solving within the context of diabetes management: 1) identify the problem; 2) brainstorm possible strategies for problem resolution; 3) select the most appropriate strategy; 4) apply the strategy; and 5) evaluate the effectiveness of the strategy [[34], [35], [36]]. In a previous randomized clinical trial, participants with poorly managed diabetes who received DECIDE experienced significant reduction in A1C immediately post-intervention and had significant, sustained improvement in diabetes knowledge, problem-solving skills, and diabetes self-care behaviors [37]. In Bridge to Health/Puente a la Salud, the timing of the delivery of DECIDE is based on the needs of the participant: for example, the CHW could choose to prioritize navigation services prior to delivering DECIDE; address unmet basic needs and deliver the DECIDE intervention content simultaneously; or deliver DECIDE and continue to be available to address any new identified needs. Each participant receives a binder with materials for the nine DECIDE modules, available in English and Spanish.
2.6.3. Treatment fidelity
To ensure standardized delivery of the study intervention, all CHWs completed a 20-h in-person training that was co-facilitated by the Principal Investigator (Fitzpatrick) and a DECIDE trainer from Johns Hopkins School of Medicine. A Popular Educacion (empowerment education) approach was used throughout the training, which involves connecting the CHWs' lived experiences to social determinants of health and supporting collective action for social justice [38]. Use of this approach has been associated with an enhanced sense of empowerment both among the CHWs and the families and communities they serve and the empowerment translates into improved health [38,39]. Specific content covered during the training consisted of the following: an overview of diabetes and the racial/ethnic disparities in optimal disease management; information about study implementation and research ethics; an in-depth review of the DECIDE materials; and role-play exercises of the nine DECIDE sessions. A refresher training was provided midway through the 6-month recruitment period to support the existing CHWs and train a new CHW who joined the team. The CHWs receive regular supervision and bi-monthly case management from the Principal Investigator. In addition, a random selection of CHW visits are audio-recorded (with verbal consent from the study participants) and reviewed by the Principal Investigator as another check for fidelity. The KPNW patient navigators are in regular contact with their direct supervisors, and the study team met as needed with the Patient Navigator Program manager to provide pertinent study updates and modify the referral process as needed based on navigators’ caseloads.
2.7. Study measures
2.7.1. Feasibility
The primary outcome of this pilot trial is feasibility, which will be determined by: a) recruitment and retention rate; b) percent of successful referrals to patient navigators and CHWs; c) mean number of days to connect patients to navigators and CHWs; d) proportion of participants whose unmet basic needs are met at the end of the 6-month intervention; and e) DECIDE session completion. Table 1 provides the definition and goals for each feasibility measure. Referral data (i.e., to navigators, CHWs, and community-based resources), completion of DECIDE sessions, and additional intervention contacts, are obtained from the EHR or through Clara, a web-based client tracking tool and database application that is used by PANOW and the CHWs for case management.
Table 1.
Feasibility measure definitions.
| Measure | Definition/Calculation | Study Goal |
|---|---|---|
| Recruitment rate | Number of eligible participants recruited/Total number of eligible patients | Recruit 100 participants over a 6-month perioda |
| Retention rate | Number of participants with 6-month outcome data (i.e., an A1C test and completed social needs screener)/Number of enrolled participants | Retain at least 80% of participants at the end of the study with 6-month outcome data |
| Percent of successful referrals to community health worker and/or patient navigator | Number of participants with at least one encounter (via phone or in person) with a community health worker and/or patient navigator/Total number of participants randomized and referred | Connect 50% or more participants to a community health worker and/or patient navigator |
| Mean number of days to connect participant to patient navigator or CHW | Mean number of days between the date of referral to the date of first encounter (via phone or in person) with a community health worker and/or patient navigator across participants per study arm | 7-14 days |
| Proportion of participants with unmet basic needs met at the end of the 6-month intervention | Based on responses to the social needs screener at the 6- month follow-up in both study arms and the number of Pathways closed by the CHW in the Navigation + DSMS arm | Resolve at least one unmet basic need during the 6- month intervention per participant |
| DECIDE session completion | Number of DECIDE sessions (total of 9) successfully delivered to a participant by the CHW | At least 8 sessions |
Recruitment has been completed and 110 participants were recruited over a 9-month period.
2.7.2. Acceptability
Semi-structured qualitative interviews with 20 randomly selected participants and 5 senior health system administrators as well as focus groups with 5 or more CHWs and KPNW patient navigators each are being conducted to assess intervention acceptability and identify determinants of implementation and sustainability. Formal qualitative interviews with clinical care team members are not being conducted due to their limited time and bandwidth; however, the Principal Investigator (Fitzpatrick) did solicit feedback on the study design and recruitment methods during informal conversations with providers and at care team huddles at the beginning of the study. Interviews with patients, health system administrators, CHWs, and patient navigators are conducted by phone and focus groups in-person following interview guides developed using the Tailored Implementation for Chronic Diseases (TICD) [40] and the Practical, Robust Implementation and Sustainability Model (PRISM) [41] frameworks. Specifically, using the TICD framework, interview questions cover the following domains: a) intervention factors (e.g., Is intervention delivery feasible for the patient navigators and CHWs?); b) individual health professional factors (e.g., What skills are needed to effectively deliver the interventions and do the navigators and CHWs have those skills?); c) professional interactions (e.g., What referral processes and communication are needed between the different levels of care and what changes are needed to facilitate adherence to these processes?); d) incentives and resources (e.g., How do the information systems (EHR and Clara) facilitate or hinder the referral process and communication between the different levels of care?); e) capacity for organizational change (e.g., What organizational changes are needed to implement and sustain the intervention?); and f) social, political, and legal factors (e.g., Do economic constraints on the healthcare budget facilitate or hinder implementation and sustainability of the intervention?). To further examine intervention acceptability from the participant perspective, based on the PRISM framework, interview guides are designed to assess the degree to which the Navigation and Navigation + DSMS arms are: a) patient centered; b) provide patient with choices; c) addresses patient barriers; d) involves a seamless transition between program elements; e) easy to access; f) burdensome; and g) provides feedback of results.
2.7.3. Diabetes-related clinical measures
Hemoglobin A1C values obtained during routine care within a 60-day window around the 6-month post-randomization date and entered in the EHR will be extracted. We will use this data to determine the proportion of participants with an A1C test and an A1C < 8% in each arm at the 6-month follow-up.
2.7.4. Healthcare utilization
Primary care, emergency department, and pharmacy utilization data will also be extracted from the EHR. We will particularly examine the number of no shows to scheduled primary care appointments, emergency department visits, and refills of diabetes-related prescriptions 6 months prior to randomization and 6 months post-randomization.
2.8. Statistical and qualitative analysis plan
Before we carry out any analyses, we will audit the data for quality and completeness, and evaluate missing data patterns. We will examine variable distributions for outliers and assess them to ensure that they meet the assumptions of the planned analysis. We will present the baseline characteristics as means and standard deviations for continuous variables and as percentages for categorical variables. Nominal variables will be coded as categorical variables for inclusion as predictors in multivariate analyses. All inferential tests will be carried out at a two-tailed alpha level of 0.05. We will examine group differences on important baseline factors using a student t-test (or the nonparametric Mann-Whitney U test) for continuous variables and chi-square test (or the Fisher's exact test) for categorical variables. Significant variables will be included as covariates in the models.
Recruitment and retention rate, proportion of participants with a successful referral to a patient navigator and CHW, mean number of days to connect each participant to a navigator and CHW, and proportion of participants with unmet basic needs met at 6-month follow-up will be calculated as described in Table 1. For the qualitative analysis, a coding dictionary will be developed based on review of the transcripts’ content and interview questions. Codes will denote content of questions, TICD and PRISM domains, and concepts naturally emerging from the discussions. During the coding process, inter-rater reliability will be established by comparing the agreement in coded text with 20% of the transcripts between two coders. Any differences in coding will be resolved through discussion, and the two coders will meet regularly to discuss and refine the coding process. A qualitative database will be compiled, coded, and analyzed using a qualitative software program (Dedoose). Once all transcripts are coded within the software program, we will use text retrieval and grouping functions on specific codes and combinations of codes for a particular topic and summarize the issues, agreements, and disagreements in the content for each item. This process will result in a list of themes relating to intervention acceptability [42] and determinants (barriers and facilitators) of implementation and sustainability. As we summarize and interpret, we will identify findings or patterns among themes and will review data for statements that directly confirm or discredit our interpretations [[43], [44], [45]].
To assess preliminary effectiveness, using a chi-square test, we will compare the two study arms on proportion of participants with A1C < 8% at 6-month follow-up. In addition, we will conduct a logistic regression analysis to assess the association between the study arms and A1C < 8% at 6-month follow-up, coding the study arms as a binary variable (Navigation only as the reference) as the predictor of interest. We will control for factors that are not balanced between the two arms (e.g., age, sex) in the model. We will conduct similar analyses for the binary outcome, A1C test completed (yes or no).
To analyze the number of emergency department (ED) visits by each participant, we will count and then summarize the distribution of the ED count with means, medians, standard deviations, quartiles, frequency, and proportion of participants with 0, 1, 2+ ED visits, by study arm. We will use the Poisson model (or negative binomial model when appropriate) to analyze the relationship between study arms and the number of ED visits adjusting for the covariates that are significantly different between the two arms. We will report the estimated rate ratio (RR) associated with the study arm binary variable and the 95% CI.
The primary care no-show visit rate will be calculated as the number of primary care visits a participant missed divided by the total number of primary care visits scheduled during the 6-month follow-up period. The time to refill a medication will be based on number of days between the diabetes medication being dispensed and the previous supply running out. Delayed refills will be defined as medication not being dispensed for 7 days or more after the previous supply ran out. For each participant, number of delays or gaps in refills and number of days without a refill will be calculated. Both no-show visit rate and number of delays in refills are continuous variables. We will summarize the distributions with means, medians, standard deviations, and quartiles for each study arm. Assuming normal distribution, we will use the two-sample t-tests to compare the means of these two outcomes between the two study arms. We will use multiple linear regression modeling to examine the association between study arms and these two outcomes. Based on expectations of fairly well-balanced study arms for these two outcomes we will adjust for all unbalanced factors in the models. We will report the coefficients and the 95% CIs associated with the study arm binary variable.
3. Discussion
As the Centers for Medicare and Medicaid Services (CMS) move toward a value-based payment model accounting for social risks [46], healthcare systems and community-based settings across the U.S. are gradually implementing procedures to increase the screening of unmet basic needs and other social risks [[47], [48], [49], [50]]. Furthermore, the CMS Accountable Health Communities initiative is a demonstration project to increase social risks screening followed by navigation to social services or community-based resources to address those needs in clinical care settings across the U.S [51]. As a result of these policies and demonstration projects, navigation is emerging as an enhanced standard of care; however, protocols for effective navigation within healthcare settings, particularly as it relates to diabetes management, still needs to be established, which findings from this study will inform. Findings from this trial will contribute to the limited literature on the effect of navigation programs on diabetes-related outcomes and acceptability of this intervention from the participant perspective based on qualitative interviews. Furthermore, we will be able to examine if combining diabetes self-management support with navigation to address the unmet basic needs that interfere with diabetes self-management may help reduce the persistent racial/ethnic disparities in glycemic control.
Even at this pilot phase we decided to utilize existing healthcare staff, particularly patient navigators, as well as CHWs embedded in culturally specific CBOs to pragmatically test the feasibility of implementing the interventions. The novel approach of pairing patient navigators with CHWs to deliver the Navigation + DSMS intervention facilitates key linkages among the patient, care team, and the community and fosters a unique form of partnership between the health care system and community-based organizations. Qualitative interviews and focus groups with participants, senior health system administrators, navigators, and CHWs will provide pertinent information on the facilitators and barriers to implementation as well as determinants of sustainability. These qualitative findings will shed light on the best approaches for integrating CHWs in healthcare settings to address unmet basic needs and improve diabetes self-management as well as how to maximize the coordination among the care team.
There are some limitations to the study design in that there was no ‘usual care’ only arm to pilot test the effect of Navigation only. We thought it to be unethical to assess for unmet basic needs and not provide any support, in addition to the challenge of successfully recruiting and randomizing vulnerable, socially complex participants to ‘usual care.’ Adding a diabetes self-management support intervention only arm was also considered, yet the findings from this design may be minimal as there is already numerous studies demonstrating the effectiveness of diabetes self-management interventions in the literature [52]. Also, we designed this trial applying a health equity lens, which involves going beyond the traditional clinical and self-management context to also acknowledge the social context in which these participants are trying to manage their diabetes and make behavioral changes [53,54]. Another limitation is that we did not enroll patients who were delayed or completely disengaged from routine care for their diabetes as patients were required to have a recent A1C test documented in the EHR prior to recruitment and randomization. For future work, this particular population would be important to incorporate in the delivery of the intervention, yet we would have to consider effective strategies for successfully engaging them in the study.
Despite advances in treatment, racial/ethnic and socioeconomic disparities in the prevalence and management of diabetes persist. These disparities are exacerbated by unmet basic needs that interfere with optimal diabetes self-management. Social health interventions such as navigation to social services and community-based resources to address unmet basic needs are necessary but may not be sufficient to improve diabetes-related outcomes. The Bridge to Health/Puente a la Salud pilot study is designed to test the feasibility of a pragmatic, two-arm randomized trial to compare the effectiveness of navigation only to navigation + evidence-based diabetes self-management support on diabetes-related outcomes among racial/ethnic minority and low-income patients with poor glycemic control. Quantitative and qualitative findings from this pilot study will enhance understanding about acceptability, preliminary clinical effectiveness, and facilitators and barriers to implementation of these two intervention conditions and inform refinements of the interventions and overall study design for the larger, randomized clinical trial.
Funding
This work is supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (R34DK119853).
CRediT authorship contribution statement
Dea Papajorgji-Taylor: Writing – original draft, Project administration. Melanie Francisco: Formal analysis, Data curation, Writing – review & editing. Jennifer L. Schneider: Writing – review & editing. Katie Vaughn: Writing – review & editing. Nangel Lindberg: Writing – review & editing. Stephanie L. Fitzpatrick: Conceptualization, Funding acquisition, Investigation, Writing – review & editing, Supervision.
Acknowledgements
We also acknowledge the community-based organizations that partnered on the study: Project Access NOW, Familias en Acción, Northwest Family Services, Latino Network, Volunteers of America, Portland Opportunities Industrialization Center, Immigrant and Refugee Community Organization, El Programa Hispano, and Impact Northwest. Also, we would like to thank Dr. Felicia Hill-Briggs, developer of DECIDE, and Dr. Elizabeth Vrany, DECIDE trainer, for their contributions to interventionist training and study design implementation.
References
- 1.McWilliams J.M., Meara E., Zaslavsky A.M., Ayanian J.Z. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Ann. Intern. Med. 2009;150(8):505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 2.Bae J.P., Lage M.J., Mo D., Nelson D.R., Hoogwerf B.J. Obesity and glycemic control in patients with diabetes mellitus: analysis of physician electronic health records in the US from 2009-2011. J. Diabetes Complicat. 2016;30(2):212–220. doi: 10.1016/j.jdiacomp.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 3.Spanakis E.K., Golden S.H. Race/ethnic difference in diabetes and diabetic complications. Curr. Diabetes Rep. 2013;13(6):814–823. doi: 10.1007/s11892-013-0421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gucciardi E., Vahabi M., Norris N., Del Monte J.P., Farnum C. The intersection between food insecurity and diabetes: a review. Curr. Nutr. Rep. 2014;3(4):324–332. doi: 10.1007/s13668-014-0104-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnard L.S., Wexler D.J., DeWalt D., Berkowitz S.A. Material need support interventions for diabetes prevention and control: a systematic review. Curr. Diabetes Rep. 2015;15(2):574. doi: 10.1007/s11892-014-0574-1. [DOI] [PubMed] [Google Scholar]
- 6.Heerman W.J., Wallston K.A., Osborn C.Y. Food insecurity is associated with diabetes self-care behaviours and glycaemic control. Diabet. Med. 2016;33(6):844–850. doi: 10.1111/dme.12896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayer V.L., McDonough K., Seligman H., Mitra N., Long J.A. Food insecurity, coping strategies and glucose control in low-income patients with diabetes. Publ. Health Nutr. 2016;19(6):1103–1111. doi: 10.1017/S1368980015002323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berkowitz S.A., Gao X., Tucker K.L. Food-insecure dietary patterns are associated with poor longitudinal glycemic control in diabetes: results from the Boston Puerto Rican Health study. Diabetes Care. 2014;37(9):2587–2592. doi: 10.2337/dc14-0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Billimek J., Sorkin D.H. Food insecurity, processes of care, and self-reported medication underuse in patients with type 2 diabetes: results from the California Health Interview Survey. Health Serv. Res. 2012;47(6):2159–2168. doi: 10.1111/j.1475-6773.2012.01463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knight C.K., Probst J.C., Liese A.D., Sercye E., Jones S.J. Household food insecurity and medication "scrimping" among US adults with diabetes. Prev. Med. 2016;83:41–45. doi: 10.1016/j.ypmed.2015.11.031. [DOI] [PubMed] [Google Scholar]
- 11.Seligman H.K., Davis T.C., Schillinger D., Wolf M.S. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J. Health Care Poor Underserved. 2010;21(4):1227–1233. doi: 10.1353/hpu.2010.0921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkowitz S.A., Meigs J.B., DeWalt D. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern. Med. 2015;175(2):257–265. doi: 10.1001/jamainternmed.2014.6888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berkowitz S.A., Kalkhoran S., Edwards S.T., Essien U.R., Baggett T.P. Unstable housing and diabetes-related emergency department visits and hospitalization: a nationally representative study of safety-net clinic patients. Diabetes Care. 2018;41(5):933–939. doi: 10.2337/dc17-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Becerra M.B., Allen N.L., Becerra B.J. Food insecurity and low self-efficacy are associated with increased healthcare utilization among adults with type II diabetes mellitus. J. Diabetes Complicat. 2016;30(8):1488–1493. doi: 10.1016/j.jdiacomp.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Mabli J.O.J., Dragoset L., Castner L., Santos B. Mathematica Policy Research; August, 2013. Measuring the Effect of Supplemental Nutrition Assistance Program (SNAP) Participation on Food Security. [Google Scholar]
- 16.Shinn M., Brown S.R., Wood M., Gubits D. Housing and service interventions for families experiencing homelessness in the United States: an experimental evaluation. Eur. J. Homelessness. 2016;10(1):13–30. [PMC free article] [PubMed] [Google Scholar]
- 17.Shier G., Ginsburg M., Howell J., Volland P., Golden R. Strong social support services, such as transportation and help for caregivers, can lead to lower health care use and costs. Health Aff. 2013;32(3):544–551. doi: 10.1377/hlthaff.2012.0170. [DOI] [PubMed] [Google Scholar]
- 18.Sadowski L.S., Kee R.A., VanderWeele T.J., Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. J. Am. Med. Assoc. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 19.Pruitt Z., Emechebe N., Quast T., Taylor P., Bryant K. Expenditure reductions associated with a social service referral program. Popul. Health Manag. 2018;21(6):469–476. doi: 10.1089/pop.2017.0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Enard K.R., Ganelin D.M. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. J. Healthc. Manag. 2013;58(6):412–427. discussion 428. [PMC free article] [PubMed] [Google Scholar]
- 21.Goodridge D., Bandara T., Marciniuk D. Promoting chronic disease management in persons with complex social needs: a qualitative descriptive study. Chron. Respir. Dis. 2019;16 doi: 10.1177/1479973119832025. 1479973119832025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loskutova N.Y., Tsai A.G., Fisher E.B. Patient navigators connecting patients to community resources to improve diabetes outcomes. J. Am. Board Fam. Med. 2016;29(1):78–89. doi: 10.3122/jabfm.2016.01.150048. [DOI] [PubMed] [Google Scholar]
- 23.Horny M., Glover W., Gupte G., Saraswat A., Vimalananda V., Rosenzweig J. Patient navigation to improve diabetes outpatient care at a safety-net hospital: a retrospective cohort study. BMC Health Serv. Res. 2017;17(1):759. doi: 10.1186/s12913-017-2700-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berkowitz S.A., Hulberg A.C., Hong C. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual. Saf. 2016;25(3):164–172. doi: 10.1136/bmjqs-2015-004521. [DOI] [PubMed] [Google Scholar]
- 25.Hessler D., Bowyer V., Gold R., Shields-Zeeman L., Cottrell E., Gottlieb L.M. Bringing social context into diabetes care: intervening on social risks versus providing contextualized care. Curr. Diabetes Rep. 2019;19(6):30. doi: 10.1007/s11892-019-1149-y. [DOI] [PubMed] [Google Scholar]
- 26.Kangovi S., Mitra N., Grande D., Huo H., Smith R.A., Long J.A. Community health worker support for disadvantaged patients with multiple chronic diseases: a randomized clinical trial. Am. J. Publ. Health. 2017;107(10):1660–1667. doi: 10.2105/AJPH.2017.303985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nelson K., Taylor L., Silverman J. Randomized controlled trial of a community health worker self-management support intervention among low-income adults with diabetes, seattle, Washington, 2010-2014. Prev. Chronic Dis. 2017;14:E15. doi: 10.5888/pcd14.160344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valaitis R.K., Carter N., Lam A., Nicholl J., Feather J., Cleghorn L. Implementation and maintenance of patient navigation programs linking primary care with community-based health and social services: a scoping literature review. BMC Health Serv. Res. 2017;17(1):116. doi: 10.1186/s12913-017-2046-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trump L.J., Mendenhall T.J. Community health workers in diabetes care: a systematic review of randomized controlled trials. Fam. Syst. Health. 2017;35(3):320–340. doi: 10.1037/fsh0000283. [DOI] [PubMed] [Google Scholar]
- 30.Gary T.L., Batts-Turner M., Yeh H.C. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch. Intern. Med. 2009;169(19):1788–1794. doi: 10.1001/archinternmed.2009.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rothschild S.K., Martin M.A., Swider S.M. Mexican American trial of community health workers: a randomized controlled trial of a community health worker intervention for Mexican Americans with type 2 diabetes mellitus. Am. J. Publ. Health. 2014;104(8):1540–1548. doi: 10.2105/AJPH.2013.301439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sundar K.R. Universal screening for social needs in a primary care clinic: a quality improvement approach using the Your current Life situation survey. Perm. J. 2018;22:18–89. doi: 10.7812/TPP/18-089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yancey A.K., Ortega A.N., Kumanyika S.K. Effective recruitment and retention of minority research participants. Annu. Rev. Publ. Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 34.Hill-Briggs F., Lazo M., Peyrot M. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J. Gen. Intern. Med. 2011;26(9):972–978. doi: 10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schumann K., Sutherland J.A., Majid H.M., Hill-Briggs F. Evidence-based behavioral treatments for diabetes: problem-solving therapy. Diabetes Spectr. 2011;24:64–69. [Google Scholar]
- 36.Hill-Briggs F. Problem solving in diabetes self-management: a model of chronic illness self-management behavior. Ann. Behav. Med. : Publ. Soc. Behav. Med. 2003;25(3):182–193. doi: 10.1207/S15324796ABM2503_04. [DOI] [PubMed] [Google Scholar]
- 37.Fitzpatrick S.L., Golden S.H., Stewart K. Effect of DECIDE (Decision-making education for choices in diabetes Everyday) program delivery modalities on clinical and behavioral outcomes in urban African Americans with type 2 diabetes: a randomized trial. Diabetes Care. 2016;39(12):2149–2157. doi: 10.2337/dc16-0941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wiggins N. Popular education for health promotion and community empowerment: a review of the literature. Health Promot. Int. 2012;27(3):356–371. doi: 10.1093/heapro/dar046. [DOI] [PubMed] [Google Scholar]
- 39.Wallerstein N. 2006. What Is the Evidence on Effectiveness of Empowerment to Improve Health? Copenhagen. [Google Scholar]
- 40.Flottorp S.A., Oxman A.D., Krause J. A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement. Sci. 2013;8:35. doi: 10.1186/1748-5908-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Feldstein A.C., Glasgow R.E. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Joint Comm. J. Qual. Patient Saf. 2008;34(4):228–243. doi: 10.1016/s1553-7250(08)34030-6. [DOI] [PubMed] [Google Scholar]
- 42.Ayala G.X., Elder J.P. Qualitative methods to ensure acceptability of behavioral and social interventions to the target population. J. Publ. Health Dent. 2011;71(Suppl 1):S69–S79. doi: 10.1111/j.1752-7325.2011.00241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bernard R., Ryan G.W. Sage Publications; Thousand Oaks, CA: 2009. Analyzing Qualitative Data: Systematic Approaches. [Google Scholar]
- 44.Patton M.Q. third ed. Sage Publications; Thousand Oaks, CA: 2002. Qualitative Research & Evaluation Methods. [Google Scholar]
- 45.Strauss A., Corbin J. Sage Publications; Thousand Oaks, CA: 2008. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. [Google Scholar]
- 46.Integrating N.A.S.E.M. The National Academies Press; Washington, DC: 2019. Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation's Health. [PubMed] [Google Scholar]
- 47.Frier A., Devine S., Barnett F., Dunning T. Utilising clinical settings to identify and respond to the social determinants of health of individuals with type 2 diabetes-A review of the literature. Health Soc. Care Community. 2020;28(4):1119–1133. doi: 10.1111/hsc.12932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Davidson K.W., McGinn T. Screening for social determinants of health: the known and unknown. J. Am. Med. Assoc. 2019;322(11):1037–1038. doi: 10.1001/jama.2019.10915. [DOI] [PubMed] [Google Scholar]
- 49.Gottlieb L.M., DeSalvo K., Adler N.E. Healthcare sector activities to identify and intervene on social risk: an introduction to the American journal of preventive medicine supplement. Am. J. Prev. Med. 2019;57(6 Suppl 1):S1–S5. doi: 10.1016/j.amepre.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 50.Fichtenberg C.M., Alley D.E., Mistry K.B. Improving social needs intervention research: key questions for advancing the field. Am. J. Prev. Med. 2019;57(6 Suppl 1):S47–S54. doi: 10.1016/j.amepre.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 51.Alley D.E., Asomugha C.N., Conway P.H., Sanghavi D.M. Accountable health communities--addressing social needs through medicare and Medicaid. N. Engl. J. Med. 2016;374(1):8–11. doi: 10.1056/NEJMp1512532. [DOI] [PubMed] [Google Scholar]
- 52.Ricci-Cabello I., Ruiz-Perez I., Rojas-Garcia A., Pastor G., Rodriguez-Barranco M., Goncalves D.C. Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: a systematic review, meta-analysis and meta-regression. BMC Endocr. Disord. 2014;14:60. doi: 10.1186/1472-6823-14-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thornton P.L., Kumanyika S.K., Gregg E.W. New research directions on disparities in obesity and type 2 diabetes. Ann. N. Y. Acad. Sci. 2020;1461(1):5–24. doi: 10.1111/nyas.14270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kumanyika S.K. A framework for increasing equity Impact in obesity prevention. Am. J. Publ. Health. 2019;109(10):1350–1357. doi: 10.2105/AJPH.2019.305221. [DOI] [PMC free article] [PubMed] [Google Scholar]