Key Points
Question
Is internet-delivered cognitive behavioral therapy (CBT) implemented in a stepped-care model noninferior to in-person CBT for children and adolescents with obsessive-compulsive disorder?
Findings
In this randomized, noninferiority clinical trial, 152 children and adolescents with obsessive-compulsive disorder were treated with an internet-delivered CBT program followed by traditional in-person CBT if necessary vs in-person CBT alone. After 6 months, the mean Children’s Yale-Brown Obsessive-Compulsive Scale score was 11.57 in those treated with internet-delivered CBT vs 10.57 in those treated with in-person CBT, a difference that met the noninferiority criterion of 4 points.
Meaning
Treating children and adolescents with obsessive-compulsive disorder with an internet intervention followed by traditional face-to-face therapy if necessary was noninferior to in-person therapy alone.
Abstract
Importance
In most countries, young people with obsessive-compulsive disorder have limited access to specialist cognitive behavioral therapy (CBT), a first-line treatment.
Objective
To investigate whether internet-delivered CBT implemented in a stepped-care model is noninferior to in-person CBT for pediatric obsessive-compulsive disorder.
Design, Setting and Participants
A randomized clinical noninferiority trial conducted at 2 specialist child and adolescent mental health clinics in Sweden. Participants included 152 individuals aged 8 to 17 years with obsessive-compulsive disorder. Enrollment began in October 2017 and ended in May 2019. Follow-up ended in April 2020.
Interventions
Participants randomized to the stepped-care group (n = 74) received internet-delivered CBT for 16 weeks. Nonresponders at the 3-month follow-up were then offered a course of traditional face-to-face treatment. Participants randomized to the control group (n = 78) immediately received in-person CBT for 16 weeks. Nonresponders at the 3-month follow-up received additional face-to-face treatment.
Main Outcomes and Measures
The primary outcome was the masked assessor–rated Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) score at the 6-month follow-up. The scale includes 10 items rated from 0 (no symptoms) to 4 (extreme symptoms), yielding a total score range of 0 to 40, with higher scores indicating greater severity. Assessors were masked to treatment allocation at pretreatment, posttreatment, 3-month follow-up, and 6-month follow-up assessments. The predefined noninferiority margin was 4 points on the CY-BOCS.
Results
Among the 152 randomized participants (mean age, 13.4 years; 94 [62%] females), 151 (99%) completed the trial. At the 3-month follow-up, 34 participants (46%) in the stepped-care group and 23 (30%) in the in-person CBT group were nonresponders. At the 6-month follow-up, the CY-BOCS score was 11.57 points in the stepped-care group vs 10.57 points in the face-to-face treatment group, corresponding to an estimated mean difference of 0.91 points ([1-sided 97.5% CI, −∞ to 3.28]; P for noninferiority = .02). Increased anxiety (30%-36%) and depressive symptoms (20%-28%) were the most frequently reported adverse events in both groups. There were 2 unrelated serious adverse events (1 in each group).
Conclusions and Relevance
Among children and adolescents with obsessive-compulsive disorder, treatment with an internet-delivered CBT program followed by in-person CBT if necessary compared with in-person CBT alone resulted in a noninferior difference in symptoms at the 6-month follow-up. Further research is needed to understand the durability and generalizability of these findings.
Trial Registration
ClinicalTrials.gov Identifier: NCT03263546
This noninferiority trial compares the effects of an internet-delivered cognitive behavioral therapy (CBT) program followed by traditional in-person CBT if necessary vs in-person CBT alone on symptoms of obsessive compulsive disorder (OCD) in children and adolescents.
Introduction
Obsessive-compulsive disorder (OCD) is a relatively common psychiatric disorder (the lifetime prevalence was estimated to be 1.3% in a meta-analysis including all worldwide studies until 20171) that is associated with marked functional impairment2,3 and increased mortality risk.4,5 Because the disorder typically develops in childhood or adolescence6 and tends to run a chronic course if untreated,7 early intervention should be prioritized.8
Evidence-based treatments for young people with OCD include cognitive behavioral therapy (CBT) and selective serotonin-reuptake inhibitors, but guidelines typically recommend in-person CBT as the first-line treatment for mild to moderate OCD due to its favorable adverse effect profile and greater acceptability.9 CBT for OCD is a highly specialized treatment that may be difficult to access and is time-consuming, typically requiring regular appointments with a qualified therapist over several weeks or months.9,10 One possible solution to the limited availability of specialized CBT is to deliver a low-intensity version of the treatment online with minimal remote support from a clinician, akin to a guided self-help intervention.11 This kind of guided internet-delivered CBT differs from standard telepsychiatry in that the therapist does not actively deliver the treatment content in real time. Instead, the therapist provides minimal support asynchronously via a messaging system built in the online platform. Research has supported the potential efficacy and cost-effectiveness of this approach for managing pediatric OCD.12,13,14,15 However, questions remain regarding the feasibility of implementing such low-intensity interventions in regular health care.
It may be possible to effectively use internet-delivered CBT in a stepped-care fashion, in which patients are first offered a low-intensity intervention and higher-intensity treatments (eg, face-to-face CBT) are reserved for patients who do not benefit sufficiently from the low-intensity intervention. Stepped-care approaches are heralded as the ideal model of psychiatric service delivery, but they have rarely been evaluated. The current trial aimed to evaluate whether a stepped-care model could be as efficacious as (ie, not inferior to) traditional in-person CBT for children and adolescents with OCD.
Methods
Trial Design
This was a 2-site single-blinded randomized clinical noninferiority trial comparing stepped care with in-person CBT treatment for children and adolescents with OCD. The principal investigator and outcome assessors were blinded to group allocation, but treatment condition was not blinded for participants or therapists. Masked rater assessments were conducted at pretreatment (week 0), posttreatment (week 16), 3-month follow-up, and 6-month follow-up (primary end point) visits. The study was approved by the regional ethical review board in Stockholm, Sweden (DNR 2017/1070-31/1). All participants and their parents/legal guardians received verbal and written information about the study and provided written informed consent before inclusion. The full trial protocol is published16 and available in Supplement 1. A full heath economic evaluation will be published separately.
Participants
Participants were recruited from 2 specialist pediatric OCD clinics in Stockholm and Gothenburg, Sweden. Families could also self-refer to the study via a dedicated website. After an initial screening, eligible participants were invited to participate in an in-person clinician appointment for a full psychiatric assessment that included the Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS)17 and the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID).18 Following the initial assessment, and discussion with the multidisciplinary team in cases of uncertainty, families who fulfilled the inclusion criteria and provided informed consent were included in the study.
Eligible participants were children and adolescents with a primary diagnosis of OCD according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,19 a total score of at least 16 on the CY-BOCS,17 age between 7 and 17 years, ability to read and write in Swedish, and daily access to a computer with internet connection. Participants were excluded if they had changed any psychotropic medication in the 6 weeks before the pretreatment assessment; had a comorbid diagnosis of organic brain disorder, global learning disabilities, autism spectrum disorder, psychosis, bipolar disorder, or severe eating disorder; had suicidal ideation; were housebound or in need of intensive or inpatient treatment; completed a course of CBT for OCD in the past 12 months; or were receiving ongoing psychological treatment for OCD or an anxiety disorder.
Randomization and Masking
Participants were randomly assigned in a 1:1 ratio to receive either stepped care or in-person CBT through an online automated randomization system (randomize.net). This was done by several assigned clinicians according to a delegation list. The system was provided and monitored by an independent clinical trials unit, the Karolinska Trial Alliance (https://karolinskatrialalliance.se/en/), and the randomization sequence was inaccessible to the research team. The randomization sequence (block sizes of 6 individuals) was stratified by age (children aged 7-12 years or adolescents aged 13-17 years) and source of participant referral (clinician-referred or self-referred).
The group allocation was concealed from the masked raters who conducted the pretreatment, posttreatment, 3-month follow-up, and 6-month follow-up assessments. To test masking integrity, the raters were asked to note if participants had inadvertently revealed their allocated group and to guess treatment allocation after each assessment. Assessors who became unblinded were replaced and the recorded CY-BOCS interview was re-rated by a new rater. The trial was unblinded after the last participant completed the 6-month follow-up assessment.
Interventions
Participants in the stepped-care group first underwent an internet-delivered CBT program for 16 weeks.12,14,20 Two age-adapted versions of the program were used: one for children aged 7 to 12 years and another for adolescents aged 13 to 17 years. Both versions had 14 modules that consisted of text, movies, and exercises that were presented in an engaging and varied way. The treatment components were the same as in the face-to-face CBT treatment manuals: education, exposure with response prevention, and relapse prevention. The parents had access to a parallel online intervention that focused specifically on reducing family accommodation and the use of positive reinforcement. Each family was assigned a personal therapist throughout the whole treatment. Communication was in the form of asynchronous, written messages through the encrypted online platform. Additional telephone support was provided on demand. A video illustrating the main features of the program can be found at https://vimeo.com/355965105/b3d5d1c439.
Participants in the control group received manualized in-person CBT21 with up to 14 sessions delivered over 16 weeks by a personally assigned therapist. Adaptations regarding degree of parental involvement, home visits, and longer sessions were made depending on individual needs. The sessions were audiotaped, and a random 20% of the sessions were selected and rated by independent clinical psychologists to ensure therapists’ adherence to the treatment manual. The ratings indicated excellent therapist adherence (eMethods 2 in Supplement 2).
Participants in either group who were classified as nonresponders at the 3-month follow-up were offered up to 12 sessions of in-person CBT between the 3-month follow-up and 6-month follow-up. The reason for waiting until the 3-month follow-up was to capture the full effect of internet-delivered CBT, because previous trials have indicated a continued improvement beyond completion of the treatment.14,22
The therapists involved in the trial were highly experienced and treated participants in both groups (eTable 2 in Supplement 2); had training in the trial protocol; and received supervision by senior clinicians during the weekly team meetings and, occasionally, during the treatment session. A more detailed description of the interventions is in the study protocol16 and in eMethod 1, eTable 1, and the eFigure in Supplement 2.
Outcome Measures
The primary outcome measure was the masked assessor–rated CY-BOCS score, a semi-structured clinician-administered interview that assesses OCD symptom severity in children and young adults. The CY-BOCS consists of 10 items that are rated on a 5-point Likert scale, ranging from 0 (no symptoms) to 4 (extreme symptoms), that are summed to yield a total score ranging from 0 to 40, with higher scores indicating greater symptom severity.17 All therapists and assessors received both initial and regular (quarterly) training in the use of the measure. The interrater reliability for the CY-BOCS during the trial was high (intraclass correlation coefficient, 0.99 [95% CI, 0.98-1.00]).
Secondary outcome measures were the masked assessor–rated Clinical Global Impressions (CGI) Severity (CGI-S) and Improvement (CGI-I) scales,23 the masked assessor–rated Children’s Global Assessment Scale,24 the Obsessive-Compulsive Inventory-Child version,25 the Children’s Obsessional Compulsive Inventory-Revised-Parent version,26 the Family Accommodation Scale-Self Rated,27 the Work and Social Adjustment Scale-Youth version and Work and Social Adjustment Scale-Parent version,28 the Mood and Feelings Questionnaire Child and Parent versions,29 the Insomnia Severity Index,30 and the Child Health Utility 9D.31 The findings of the Trimbos/iMTA Questionnaire for Costs Associated With Psychiatric Illness will be published separately. Detailed information on these secondary outcome measures, anchors, score ranges, and interpretation can be found in eMethod 3 and eTable 3 in Supplement 2. All self-rated and parent-rated measures were completed online.
Safety Procedures
Adverse events were recorded online at midtreatment (week 8), posttreatment (week 16), and 6-month follow-up assessments (eMethod 3 in Supplement 2). Safety aspects and data quality were monitored quarterly by the Karolinska Trial Alliance.
Sample Size
Power was estimated based on repeated measures (each participant being assessed 4 times), using a linear random intercept model with 1000 bootstrap samples using data from a previous randomized clinical trial.15 The enrollment of 152 participants provided an estimated power greater than 95% to reject the null hypothesis that stepped-care treatment would be inferior to in-person CBT alone, after allowing for 10% data attrition.
The noninferiority margin was set at 4 points, which was decided a priori based on clinical judgement and following recommendations to use half of the mean controlled effect size from historical trials.32 A 4-point margin corresponds to approximately half of the effect of CBT vs pill and psychological placebo conditions from a meta-analysis.33 From a clinical perspective, the chosen margin is considered to be a small clinical difference in the CY-BOCS score and is more conservative than previous noninferiority trials in OCD.21,34
Statistical Methods
Primary Analysis
The noninferiority analysis was based on the CY-BOCS score at the 6-month follow-up (primary end point) and was determined by a 1-sided 97.5% CI of the mean difference between the 2 groups using mixed-effect regression analyses for repeated measures (all assessment points included), which are valid under the assumption that the data are missing at random.35
All randomized participants were analyzed according to their randomization groups and included in the primary prespecified analysis (Figure 1). No data imputation method was used because the percentage of missing data was less than 10%.16,36 The mixed-effect regression model included fixed effects of time, treatment group, and site (Stockholm vs Gothenburg) and an interaction effect of group × time, as well as random intercept and random slope to account for individual differences. An interaction effect of group, time, and source of referral was included in the model to explore whether source of referral was a meaningful moderator of treatment effect. A planned sensitivity analysis was conducted in which participants who violated protocol (ie, made medication changes or received additional psychological treatment for OCD) were excluded.
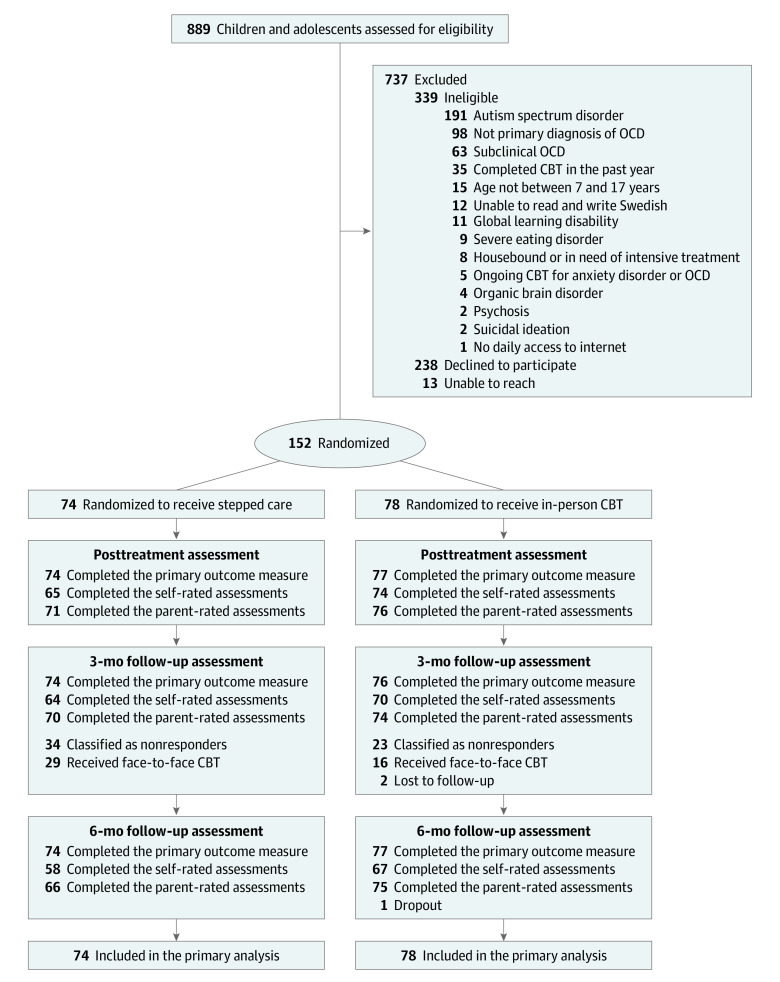
Figure 1. Patient Flow in a Study of the Effect of Internet-Delivered Stepped Care vs In-Person Cognitive Behavioral Therapy (CBT) on Obsessive-Compulsive Disorder Symptoms in Children and Adolescents.
See eResult 3 in Supplement 2 for detailed reasons on not receiving face-to-face CBT when being classified as a nonresponder at the 3-month follow-up assessment.
Secondary Analyses
Secondary outcomes were analyzed with the above-mentioned regression model using 2-sided tests with α = .05. Because of the potential for type I error due to multiple comparisons, findings for analyses of secondary outcomes should be considered exploratory. Ordinal variables (CGI-I and CGI-S) were analyzed with ordinal logistic regression. Other outcome measures (eg, treatment credibility and satisfaction) were analyzed with independent t tests. Between-group effect sizes were estimated with bootstrapped Cohen d (eMethod 4 in Supplement 2). χ2 tests were used to determine whether the masked assessors’ guesses on treatment allocation were better than chance.
Post Hoc Analyses
The percentage of participants classified as responders and remitters was compared using logistic regression. Responder status was defined as at least 35% reduction on the CY-BOCS and a CGI-I score of 1 or 2, and remitter status was defined as a score of 12 or less on the CY-BOCS and a CGI-S score of 1 or 2.37
All statistical analyses were conducted using Stata, version 16.1. The final data set, statistical analysis plan, and Stata code were locked at the Karolinska Institutet electronic laboratory notebook system prior to unblinding and data analysis.
Results
Participants
Of the 889 children and adolescents screened, 152 were enrolled in the trial (74 randomized to receive stepped-care treatment and 78 to receive in-person CBT) between October 6, 2017, and May 24, 2019 (Figure 1). The mean (SD) age at baseline was 13.4 (2.5) years, 94 participants (62%) were females, and 52 (34%) had at least 1 psychiatric comorbidity. A total of 110 participants (72%) were clinician referrals to the 2 study sites and the remainder were self-referrals. Sociodemographic and clinical characteristics of the participants are shown in Table 1. Baseline characteristics were similar across study sites (eTable 4 in Supplement 2).
Table 1. Sociodemographic and Clinical Characteristics in a Study of the Effect of Internet-Delivered Stepped Care vs In-Person Cognitive Behavioral Therapy on Obsessive-Compulsive Disorder Symptoms in Children and Adolescents (N = 152).
| Characteristic | No. (%) | |
|---|---|---|
| Stepped care (n = 74) | In-person CBT (n = 78) | |
| Site | ||
| Stockholm | 52 (70.3) | 54 (69.2) |
| Gothenburg | 22 (29.7) | 24 (30.8) |
| Patient characteristics | ||
| Sex | ||
| Female | 46 (62.2) | 48 (61.5) |
| Male | 28 (37.8) | 30 (38.5) |
| Age, mean (SD) [range], y | 13.4 (2.6) [8-17] | 13.4 (2.5) [8-17] |
| Age stratification | ||
| Children (7-12 y) | 28 (37.8) | 32 (41.0) |
| Adolescents (13-17 y) | 46 (62.2) | 46 (59.0) |
| Living arrangement | ||
| Lives with both parents | 52 (70.3) | 62 (79.5) |
| Alternating residence | 13 (17.6) | 10 (12.8) |
| Lives with one parent | 8 (10.8) | 6 (7.7) |
| Other | 1 (1.4) | 0 |
| Symptom onset, mean (SD), ya | 9.5 (3.1) | 9.0 (3.2) |
| Onset OCD, mean (SD), ya | 12.0 (2.7) | 11.5 (2.5) |
| Parent educational levelb | ||
| Primary school | 2 (2.7) | 0 |
| Secondary school | 8 (10.8) | 8 (10.3) |
| College/university (<2 y) | 8 (10.8) | 8 (10.3) |
| College/university (≥2 y) | 53 (71.6) | 60 (76.9) |
| Doctorate | 3 (4.1) | 2 (2.6) |
| Parent occupational statusb | ||
| Working | 68 (91.9) | 75 (96.3) |
| Student | 0 | 3 (3.9) |
| On sick leave | 6 (8.1) | 0 |
| Comorbidity | ||
| None | 50 (67.6) | 50 (64.1) |
| Depressive episode | 6 (8.1) | 12 (15.4) |
| Anxiety disorders | ||
| Specific phobia | 9 (12.2) | 6 (7.7) |
| Social phobia | 4 (5.4) | 4 (5.1) |
| Generalized anxiety disorder | 4 (5.4) | 3 (3.9) |
| Panic disorder | 1 (1.4) | 2 (2.6) |
| Separation anxiety | 1 (1.4) | 2 (2.6) |
| Health anxiety | 0 | 1 (1.3) |
| Tic disorder | 6 (8.1) | 8 (10.3) |
| ADHD | 6 (8.1) | 4 (5.1) |
| Eating disorder | 1 (1.4) | 0 |
| Ongoing medication | ||
| None | 69 (93.2) | 74 (94.9) |
| SSRI | 2 (2.6) | 3 (3.8) |
| Sleep hormone | 2 (2.6) | 2 (2.3) |
| Central stimulants | 2 (2.6) | 0 |
| Antihistamine | 0 | 0 |
| Previous psychological treatment | ||
| None | 39 (52.7) | 55 (70.5) |
| CBT for OCD | 6 (8.1) | 9 (11.5) |
| CBT for other | 9 (12.2) | 8 (10.3) |
| Otherc | 19 (25.7) | 6 (7.7) |
| CY-BOCS baseline score, mean (SD) [range]d | 23.0 (3.6) [16-32] | 23.0 (3.7) [17-33] |
| AQ-10 score >5 pointse | 15 (20.3) | 10 (12.8) |
| Source of referral to the study | ||
| Clinician | 54 (73.0) | 56 (71.8) |
| Self | 20 (27.0) | 22 (28.2) |
Abbreviations: ADHD, attention deficit/hyperactivity disorder; CBT, cognitive behavioral therapy; OCD, obsessive-compulsive disorder; SSRI, selective serotonin-reuptake inhibitors.
Symptom onset was defined as the time when the participant first experienced any OCD symptom; onset OCD was defined as when the symptoms became time-consuming and impairing.
The parent mainly responsible for study participation.
Defined as supportive therapy, treatment for OCD or anxiety disorders that did not include (or included less than 5 sessions of) exposure and response prevention, or anger management training.
Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) scores range from 0 to 40, with higher scores indicating more severe symptoms. A score of 23 corresponds to moderate/severe OCD.
Autism Spectrum Quotient 10 items (AQ-10) scores range from 0 to 10, with higher scores indicating more autistic symptoms. A score greater than 5 is considered indication for further assessment of neuropsychiatric difficulties.
Primary End Points
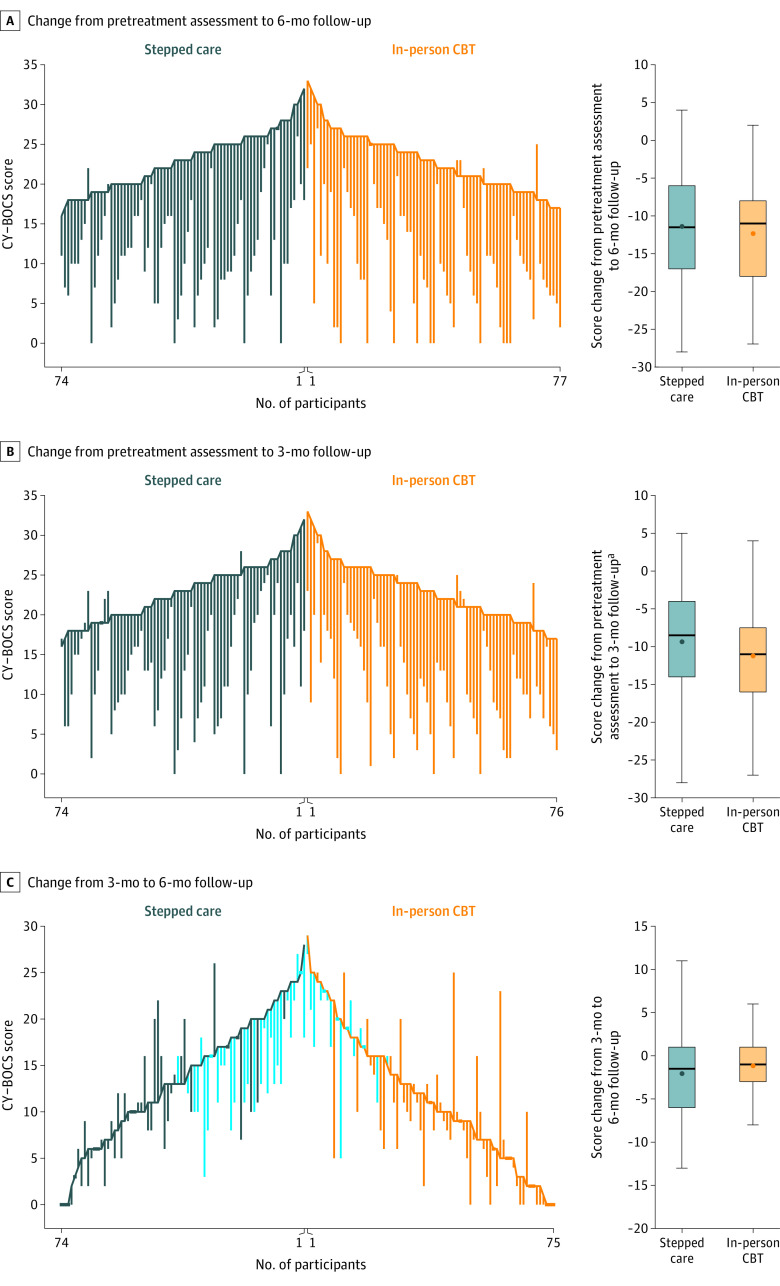
The data attrition on the primary outcome was very low, with CY-BOCS scores available for 151 of 152 participants (99%) at the 6-month follow-up (primary end point; Figure 1). The mean CY-BOCS score at the pretreatment assessment was 22.96 in the stepped-care group and 22.95 in the in-person CBT group. At the 6-month follow-up, the mean CY-BOCS score was 11.57 points in the stepped-care group and 10.57 points in the in-person CBT group (Table 2; Figure 2A); the estimated mean difference was 0.91 points (1-sided 97.5% CI, −∞ to 3.28), which met the 4-point criterion for noninferiority (P value for noninferiority = .02; Figure 2B). Individual participant outcomes are shown in Figure 3. There was no significant effect of referral source (clinician-referred vs self-referred; B = 0.07; Z = 0.86; P = .39).
Table 2. Outcomes in a Study of the Effect of Internet-Delivered vs In-Person Cognitive Behavioral Therapy (CBT) on Obsessive-Compulsive Disorder Symptoms in Children and Adolescents (N = 152)a.
| Outcome | Mean (SD) | Estimated absolute difference (CI)b | P value | |
|---|---|---|---|---|
| Stepped care (n = 74) | In-person CBT (n = 78) | |||
| Primary outcome | ||||
| CY-BOCS score | ||||
| Pretreatment | 23.9 (3.6) | 23.0 (3.7) | ||
| Posttreatment | 13.6 (5.9) | 12.8 (7.1) | ||
| 3-mo follow-up | 13.6 (6.7) | 11.8 (7.1) | ||
| 6-mo follow-up | 11.6 (6.4) | 10.6 (7.6) | 0.9 (−∞ to 3.3) | .02c |
| Secondary outcomes | ||||
| Clinician-rated | ||||
| Children’s Global Assessment Scale score | ||||
| Pretreatment | 55.1 (8.6) | 56.29 (7.2) | ||
| Posttreatment | 64.0 (10.5) | 66.61 (11.5) | ||
| 3-mo follow-up | 64.1 (11.5) | 66.96 (10.8) | ||
| 6-mo follow-up | 66.3 (11.5) | 67.99 (12.3) | −1.7 (−5.2 to 1.8) | .33 |
| Child-rated | ||||
| Obsessive-Compulsive Inventory-Child version | ||||
| Pretreatment | 18.7 (7.5) | 20.4 (6.4) | ||
| Posttreatment | 9.6 (6.4) | 11.2 (8.4) | ||
| 3-mo follow-up | 9.6 (7.6) | 11.1 (8.6) | ||
| 6-mo follow-up | 8.1 (5.67) | 8.8 (7.8) | −0.9 (−3.6 to 1.9) | .53 |
| Mood and Feelings Questionnaire-Child version | ||||
| Pretreatment | 8.9 (5.6) | 9.9 (6.3) | ||
| Posttreatment | 5.4 (5.1) | 6.3 (6.2) | ||
| 3-mo follow-up | 5.5 (5.4) | 5.5 (6.2) | ||
| 6-mo follow-up | 4.8 (4.9) | 5.0 (5.7) | 0.03 (−2.2 to 2.2) | .98 |
| Work and Social Adjustment Scale-Youth version | ||||
| Pretreatment | 15.1 (8.0) | 17.2 (8.7) | ||
| Posttreatment | 8.7 (6.7) | 9.9 (8.6) | ||
| 3-mo follow-up | 7.3 (7.0) | 8.0 (6.9) | ||
| 6-mo follow-up | 6.1 (5.5) | 7.5 (7.7) | −0.9 (−3.8 to 2.1) | .57 |
| Child Health Utility 9D | ||||
| Pretreatment | 19.9 (5.7) | 20.0 (5.5) | ||
| Posttreatment | 16.9 (5.7) | 16.7 (6.2) | ||
| 3-mo follow-up | 17.3 (6.2) | 15.8 (5.8) | ||
| 6-mo follow-up | 16.1 (5.2) | 14.8 (4.9) | 1.7 (−0.4 to 3.7) | .12 |
| Insomnia Severity Index | ||||
| Pretreatment | 7.0 (5.7) | 5.8 (4.9) | ||
| Posttreatment | 4.8 (4.5) | 4.4 (4.2) | ||
| 3-mo follow-up | 5.1 (5.3) | 4.8 (5.8) | ||
| 6-mo follow-up | 4.8 (4.5) | 4.0 (5.0) | 1.3 (−0.5 to 3.1) | .15 |
| Parent-rated | ||||
| Children’s Obsessional Compulsive Inventory-Revised-Parent version | ||||
| Pretreatment | 27.7 (6.6) | 28.5 (7.8) | ||
| Posttreatment | 16.1 (9.1) | 15.5 (9.9) | ||
| 3-mo follow-up | 15.3 (9.6) | 14.1 (10.0) | ||
| 6-mo follow-up | 13.3 (7.9) | 13.5 (9.7) | −0.5 (−3.8 to 2.9) | .78 |
| Family Accommodation Scale-Self Rated | ||||
| Pretreatment | 19.5 (14.4) | 21.4 (16.0) | ||
| Posttreatment | 7.0 (9.1) | 8.9 (11.8) | ||
| 3-mo follow-up | 8.8 (13.2) | 7.7 (11.1) | ||
| 6-mo follow-up | 5.2 (7.4) | 8.2 (10.7) | −2.4 (−6.4 to 1.5) | .23 |
| Mood and Feelings Questionnaire-Parent version | ||||
| Pretreatment | 9.2 (5.6) | 10.3 (5.9) | ||
| Posttreatment | 5.7 (4.6) | 6.4 (5.9) | ||
| 3-mo follow-up | 5.4 (5.2) | 5.8 (6.2) | ||
| 6-mo follow-up | 4.7 (4.7) | 5.6 (6.0) | −1.1 (−3.1 to 0.9) | .28 |
| Work and Social Adjustment Scale-Parent version | ||||
| Pretreatment | 16.6 (8.5) | 17.6 (8.3) | ||
| Posttreatment | 8.9 (7.1) | 10.0 (8.8) | ||
| 3-mo follow-up | 8.7 (8.3) | 7.9 (8.2) | ||
| 6-mo follow-up | 7.5 (7.4) | 7.8 (8.5) | −0.3 (−3.3 to 2.7) | .83 |
Data were analyzed according to the randomization groups and all participants were included in the analyses. The Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) scores range from 0 to 40, with higher scores indicating more severe symptoms. See eMethod 3 in Supplement 2 for detailed information about the secondary outcome measures.
Group × time interaction from mixed-effect regression analyses. 1-sided 97.5% CI is reported for the primary outcome measure (CY-BOCS score) and 2-sided 95% CIs are reported for the secondary outcome measures.
P value reported for the CY-BOCS score is for the test of noninferiority. A significant P value indicates noninferiority.
Figure 2. Primary Outcome in a Study of the Effect of Internet-Delivered vs In-Person Cognitive Behavioral Therapy (CBT) on Obsessive-Compulsive Disorder Symptoms in Children and Adolescents.
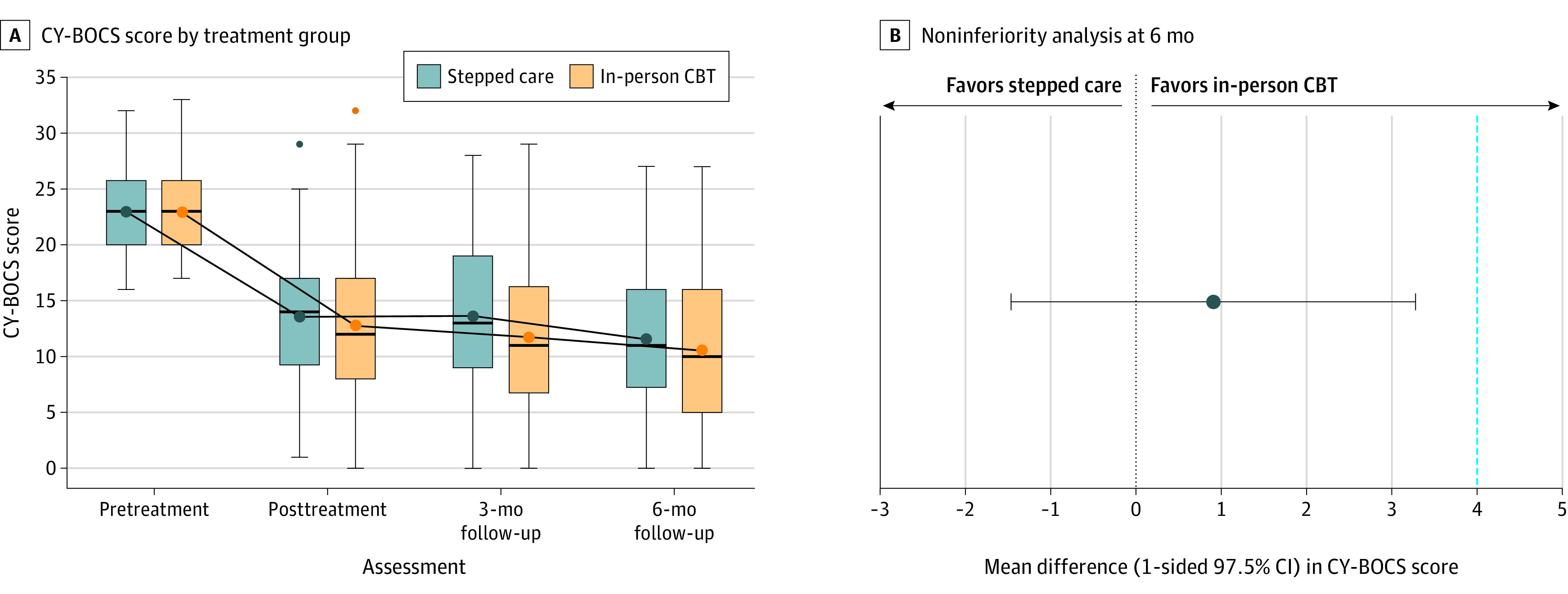
A, Boxes represent the interquartile range of the 25th and 75th percentiles, the middle line represents the median, the circles with connecting lines represent the mean values, the whiskers extend to the highest and lowest values within 1.5 times the interquartile range, and dots represent outliers. Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) scores range from 0 to 40, with higher scores indicating more severe symptoms. The posttreatment assessment was 16 weeks after the pretreatment assessment, and the follow-up assessments were 3 months and 6 months after the posttreatment assessment. Nonresponders at the 3-month follow-up were offered additional in-person CBT between the 3-month follow-up and the 6-month follow-up. B, Stepped-care treatment was considered noninferior to in-person CBT because the 1-sided 97.5% CI of the mean difference was below the prespecified margin of 4 points (dotted line) on the CY-BOCS.
Figure 3. Individual Participant CY-BOCS Outcomes in a Study of the Effect of Internet-Delivered vs In-Person Cognitive Behavioral Therapy (CBT) on Obsessive-Compulsive Disorder Symptoms in Children and Adolescents.
Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) scores range from 0 to 40, with higher scores indicating more severe symptoms. The boxplots indicate the interquartile range of the 25th and 75th percentiles, the middle line represents the median, circles represent the mean value, and the whiskers extend to the highest and lowest values within 1.5 times the interquartile range. C, The light blue vertical lines represent the nonresponders at the 3-month follow-up who received additional in-person treatment.
In a sensitivity analysis, the main analysis was repeated excluding 10% (n = 16 [8 in each group]) of participants who broke protocol due to clinical needs (made changes in concomitant medication and/or received additional psychological treatment for OCD during the study period). The inference of noninferiority was robust to these protocol deviations (mean [SD] CY-BOCS score of 11.20 [6.18] points in the stepped-care treatment group vs 10.39 [7.39] in the face-to-face treatment group; estimated mean difference, 0.75 [1-sided 97.5% CI, ∞ to 3.20]).
Secondary End Points
No significant between-group differences were found in any of the secondary outcome measures (Table 2; eTable 5 and eTable 6 in Supplement 2).
Post Hoc Analyses
At the 6-month follow-up, 50 participants (68%) in the stepped-care group and 52 (68%) in the face-to-face treatment group were classified as responders (odds ratio, 1.00 [95% CI, 0.51-1.98]; P = .99). At the same time point, 36 participants (49%) in the stepped-care group were in remission, compared with 46 (60%) in the face-to-face treatment group (odds ratio, 0.64 [95% CI, 0.34-1.22]; P = .17) (eTable 7 in Supplement 2).
Process Measures
Participants randomized to the stepped-care group completed a mean (SD) of 10.49 (3.69) online modules, and parents of participants in that group completed a mean of 10.97 (3.44) modules. Participants in the face-to-face treatment group received a mean (SD) of 11.65 (2.74) CBT sessions during the first step of treatment. The mean (SD) therapist time for the first treatment step was 336.84 (217.56) minutes per family for internet-delivered CBT and 741.81 (263.54) minutes per family in the in-person CBT group.
At the 3-month follow-up, 40 participants (54%) in the stepped-care group and 53 (71%) in the in-person CBT group were responders (Figure 1). The 29 nonresponders in the stepped-care group who accepted the offer of face-to-face CBT received a mean (SD) of 7.76 (3.15) additional in-person therapy sessions. The 16 nonresponders in the in-person CBT group received a mean (SD) of 7.56 (2.68) additional face-to-face sessions during the second step of treatment. In total, the mean (SD) therapist time for the entire study period was 526.18 (370.99) minutes per family in the stepped-care group and 849.10 (398.55) minutes in the in-person CBT group (eTable 8 in Supplement 2).
The participants deemed the face-to-face treatment more credible than internet-delivered CBT in early stages of treatment (week 2), but reported equal working alliance and satisfaction (eTable 9 in Supplement 2). Adherence to treatment was high in both groups (eTable 9 in Supplement 2). Four participants revealed their group allocation at the 6-month follow-up (eResult 1 in Supplement 2). The masked raters’ guesses of group allocation were correct in 58% of the cases, which is not significantly different from chance (X2(1) = 3.73; P = .053).
Adverse Events
The percentage of participants with adverse events was comparable between the groups (47 [64%] in stepped-care group and 52 [67%] in face-to-face treatment group). Most events were mild and subsided between the assessments (eTable 10 in Supplement 2). Two serious adverse events (1 in each group) were reported and judged to be unrelated to the treatment: 1 participant was admitted to inpatient care due to rapid weight loss (anorexia) and 1 was admitted due to increased anxiety, suicidal thoughts, and self-harm following a stressful psychosocial situation.
Discussion
Among children and adolescents with OCD, treatment with a low-intensity digital intervention followed by a course of in-person CBT if necessary resulted in a noninferior difference in OCD symptoms compared with in-person CBT alone. Improvements in all secondary outcomes were observed, including self- and parent-reported OCD symptoms, depression, insomnia, general function, quality of life, and parental accommodation of OCD symptoms, with no statistically differences between the groups at the primary end point.
Fifty-four percent of the participants were classified as treatment responders 3 months after receiving internet-delivered CBT and did not require further in-person treatment. Thus, by first offering a low-intensity intervention in a stepped-care fashion, it was possible to reduce the number of patients requiring face-to-face CBT. A health economic evaluation of this trial will be published separately.
The results extend the findings of the previous waitlist-controlled trial in adolescents with OCD15 by improving the treatment protocol, expanding the parental support modules, including both children and adolescents, and using a noninferiority design.
Although the majority of participants responded to treatment at the 6-month follow-up, about one-third still did not benefit sufficiently (some having received 2 courses of in-person CBT). The percentage of participants in remission ranged from 49% to 60%. A logical next step would be to attempt a course of a selective serotonin reuptake inhibitor, because there is some support for the efficacy of sequentially offering selective serotonin reuptake inhibitor medication to patients who do not benefit sufficiently from an initial course of CBT.38 These results highlight the importance of continuous research into effective ways to further augment the effects of CBT for pediatric OCD.
Some strengths of this trial were a low rate of data loss, a narrower noninferiority margin compared with previous trials,21,34 and the consideration of the source of participant referrals. Previous internet-delivered CBT trials have primarily recruited self-referred individuals,12,14,20 raising concerns about the generalizability of the results to clinic-referred participants.39 In the current study, only 28% of the participants were self-referred and the source of referral (clinician referral vs self-referral) did not moderate the results. The current trial had a long controlled study phase of 10 months in total, which is unusual in trials of psychological interventions.
Limitations
This study has several limitations. First, the study was conducted in Sweden, where there is a very limited number of specialist OCD clinics. Although the results may generalize to countries with similar shortages and health care systems, they may translate less well to other health care settings. In countries in which specialist treatment for OCD is more widely available, a stepped-care approach would be less likely to be of value because it would mean delaying symptom remission. In the current study, specialist treatment was delayed 7 months for those who did not respond to the initial low-intensity intervention. Second, the presence of co-occurring conditions, such as autism spectrum disorder, were exclusion criteria. Additional studies are needed to evaluate whether these findings apply to patients with these conditions.
Conclusions
Among children and adolescents with OCD, treatment with an internet-delivered CBT program followed by in-person CBT if necessary compared with in-person CBT alone resulted in a noninferior difference in symptoms at the 6-month follow-up. Further research is needed to understand the durability and generalizability of these findings.
Trial protocol
eMethod 1. Interventions
eMethod 2. Assessment of therapist adherence
eMethod 3. Outcome measures (continued)
eMethod 4. Statistical analysis (continued)
eResult 1. Blinding integrity
eResult 2. Reasons not receiving additional treatment as a non-responder
eTable 1. Content of the internet-delivered CBT program for children and adolescents with OCD
eTable 2. Description of therapists
eTable 3. Measures and assessment points
eTable 4. Demographics and clinical characteristics by site
eTable 5. Between-group effect sizes at 6-month follow-up
eTable 6. Observed values and estimated treatment efficacy for ordinal secondary measurements
eTable 7. Treatment response and remission rates across measurement points
eTable 8. Therapist time
eTable 9. Treatment adherence, credibility and satisfaction
eTable 10. Reported adverse events by study group
eFigure 1. Screenshots of the internet-delivered cognitive behavioral therapy program
eReferences
Data sharing statement
References
- 1.Fawcett EJ, Power H, Fawcett JM. Women are at greater risk of OCD than men: a meta-analytic review of OCD prevalence worldwide. J Clin Psychiatry. 2020;81(4):19r13085. doi: 10.4088/JCP.19r13085 [DOI] [PubMed] [Google Scholar]
- 2.Pérez-Vigil A, Fernández de la Cruz L, Brander G, et al. Association of obsessive-compulsive disorder with objective indicators of educational attainment: a nationwide register-based sibling control study. JAMA Psychiatry. 2018;75(1):47-55. doi: 10.1001/jamapsychiatry.2017.3523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pérez-Vigil A, Mittendorfer-Rutz E, Helgesson M, Fernández de la Cruz L, Mataix-Cols D. Labour market marginalisation in obsessive-compulsive disorder: a nationwide register-based sibling control study. Psychol Med. 2019;49(6):1015-1024. doi: 10.1017/S0033291718001691 [DOI] [PubMed] [Google Scholar]
- 4.Fernández de la Cruz L, Rydell M, Runeson B, et al. Suicide in obsessive-compulsive disorder: a population-based study of 36 788 Swedish patients. Mol Psychiatry. 2017;22(11):1626-1632. doi: 10.1038/mp.2016.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Isomura K, Brander G, Chang Z, et al. Metabolic and cardiovascular complications in obsessive-compulsive disorder: a total population, sibling comparison study with long-term follow-up. Biol Psychiatry. 2018;84(5):324-331. doi: 10.1016/j.biopsych.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 6.Taylor S. Early versus late onset obsessive-compulsive disorder: evidence for distinct subtypes. Clin Psychol Rev. 2011;31(7):1083-1100. doi: 10.1016/j.cpr.2011.06.007 [DOI] [PubMed] [Google Scholar]
- 7.Pinto A, Mancebo MC, Eisen JL, Pagano ME, Rasmussen SA. The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake. J Clin Psychiatry. 2006;67(5):703-711. doi: 10.4088/JCP.v67n0503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fineberg NA, Dell’Osso B, Albert U, et al. Early intervention for obsessive compulsive disorder: an expert consensus statement. Eur Neuropsychopharmacol. 2019;29(4):549-565. doi: 10.1016/j.euroneuro.2019.02.002 [DOI] [PubMed] [Google Scholar]
- 9.Geller DA, March J. Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(1):98-113. doi: 10.1016/j.jaac.2011.09.019 [DOI] [PubMed] [Google Scholar]
- 10.Goodwin R, Koenen KC, Hellman F, Guardino M, Struening E. Helpseeking and access to mental health treatment for obsessive-compulsive disorder. Acta Psychiatr Scand. 2002;106(2):143-149. doi: 10.1034/j.1600-0447.2002.01221.x [DOI] [PubMed] [Google Scholar]
- 11.Babiano-Espinosa L, Wolters LH, Weidle B, et al. Acceptability, feasibility, and efficacy of internet cognitive behavioral therapy (iCBT) for pediatric obsessive-compulsive disorder: a systematic review. Syst Rev. 2019;8(1):284. doi: 10.1186/s13643-019-1166-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aspvall K, Andrén P, Lenhard F, Andersson E, Mataix-Cols D, Serlachius E. Internet-delivered cognitive behavioural therapy for young children with obsessive-compulsive disorder: development and initial evaluation of the BIP OCD Junior programme. BJPsych Open. 2018;4(3):106-112. doi: 10.1192/bjo.2018.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aspvall K, Lenhard F, Melin K, et al. Implementation of internet-delivered cognitive behaviour therapy for pediatric obsessive-compulsive disorder: lessons from clinics in Sweden, United Kingdom and Australia. Internet Interv. 2020;20:100308. doi: 10.1016/j.invent.2020.100308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lenhard F, Ssegonja R, Andersson E, et al. Cost-effectiveness of therapist-guided internet-delivered cognitive behaviour therapy for paediatric obsessive-compulsive disorder: results from a randomised controlled trial. BMJ Open. 2017;7(5):e015246. doi: 10.1136/bmjopen-2016-015246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lenhard F, Andersson E, Mataix-Cols D, et al. Therapist-guided, internet-delivered cognitive-behavioral therapy for adolescents with obsessive-compulsive disorder: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2017;56(1):e10-e19. doi: 10.1016/j.jaac.2016.09.515 [DOI] [PubMed] [Google Scholar]
- 16.Aspvall K, Andersson E, Lenhard F, et al. Stepped care internet-delivered vs face-to-face cognitive-behavior therapy for pediatric obsessive-compulsive disorder: a trial protocol for a randomized noninferiority trial. JAMA Netw Open. 2019;2(10):e1913810. doi: 10.1001/jamanetworkopen.2019.13810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scahill L, Riddle MA, McSwiggin-Hardin M, et al. Children’s Yale-Brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(6):844-852. doi: 10.1097/00004583-199706000-00023 [DOI] [PubMed] [Google Scholar]
- 18.Sheehan DV, Sheehan KH, Shytle RD, et al. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J Clin Psychiatry. 2010;71(3):313-326. doi: 10.4088/JCP.09m05305whi [DOI] [PubMed] [Google Scholar]
- 19.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Publishing; 2013. [Google Scholar]
- 20.Lenhard F, Vigerland S, Andersson E, et al. Internet-delivered cognitive behavior therapy for adolescents with obsessive-compulsive disorder: an open trial. PLoS One. 2014;9(6):e100773. doi: 10.1371/journal.pone.0100773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner CM, Mataix-Cols D, Lovell K, et al. Telephone cognitive-behavioral therapy for adolescents with obsessive-compulsive disorder: a randomized controlled non-inferiority trial. J Am Acad Child Adolesc Psychiatry. 2014;53(12):1298-1307.e2. doi: 10.1016/j.jaac.2014.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jolstedt M, Wahlund T, Lenhard F, et al. Efficacy and cost-effectiveness of therapist-guided internet cognitive behavioural therapy for paediatric anxiety disorders: a single-centre, single-blind, randomised controlled trial. Lancet Child Adolesc Health. 2018;2(11):792-801. doi: 10.1016/S2352-4642(18)30275-X [DOI] [PubMed] [Google Scholar]
- 23.Guy W. The ECDEU Assessment Manual for Psychopharmacology-Revised Volume. National Institute of Mental Health; 1976. [Google Scholar]
- 24.Shaffer D, Gould MS, Brasic J, et al. A children’s global assessment scale (CGAS). Arch Gen Psychiatry. 1983;40(11):1228-1231. doi: 10.1001/archpsyc.1983.01790100074010 [DOI] [PubMed] [Google Scholar]
- 25.Aspvall K, Cervin M, Andrén P, Perrin S, Mataix-Cols D, Andersson E. Validity and clinical utility of the obsessive compulsive inventory-child version: further evaluation in clinical samples. BMC Psychiatry. 2020;20(1):42. doi: 10.1186/s12888-020-2450-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uher R, Heyman I, Turner CM, Shafran R. Self-, parent-report and interview measures of obsessive-compulsive disorder in children and adolescents. J Anxiety Disord. 2008;22(6):979-990. doi: 10.1016/j.janxdis.2007.10.001 [DOI] [PubMed] [Google Scholar]
- 27.Pinto A, Van Noppen B, Calvocoressi L. Development and preliminary psychometric evaluation of a self-rated version of the Family Accommodation Scale for Obsessive-Compulsive Disorder. J Obsessive Compuls Relat Disord. 2013;2(4):457-465. doi: 10.1016/j.jocrd.2012.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jassi A, Lenhard F, Krebs G, et al. The Work and Social Adjustment Scale, youth and parent versions: psychometric evaluation of a brief measure of functional impairment in young people. Child Psychiatry Hum Dev. 2020;51(3):453-460. doi: 10.1007/s10578-020-00956-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatric Res. 1995;5(4):237-249. [Google Scholar]
- 30.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297-307. doi: 10.1016/S1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 31.Stevens K. Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy. 2011;9(3):157-169. doi: 10.2165/11587350-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 32.Guideline on the Choice of the Non-inferiority Margin. European Medicines Agency Committee For Medicinal Products For Human Use ; 2005. Accessed April 15, 2021. https://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003636.pdf
- 33.Öst L-G, Riise EN, Wergeland GJ, Hansen B, Kvale G. Cognitive behavioral and pharmacological treatments of OCD in children: a systematic review and meta-analysis. J Anxiety Disord. 2016;43:58-69. doi: 10.1016/j.janxdis.2016.08.003 [DOI] [PubMed] [Google Scholar]
- 34.Lovell K, Cox D, Haddock G, et al. Telephone administered cognitive behaviour therapy for treatment of obsessive compulsive disorder: randomised controlled non-inferiority trial. BMJ. 2006;333(7574):883. doi: 10.1136/bmj.38940.355602.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rubin DB. Inference and missing data. ETS Research Bulletin Series. 1975;1975(1):i-19. doi: 10.1002/j.2333-8504.1975.tb01053.x [DOI] [Google Scholar]
- 36.Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons; 1987. doi: 10.1002/9780470316696 [DOI] [Google Scholar]
- 37.Mataix-Cols D, Fernández de la Cruz L, Nordsletten AE, Lenhard F, Isomura K, Simpson HB. Towards an international expert consensus for defining treatment response, remission, recovery and relapse in obsessive-compulsive disorder. World Psychiatry. 2016;15(1):80-81. doi: 10.1002/wps.20299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Skarphedinsson G, Weidle B, Ivarsson T. Sertraline Treatment of Nonresponders to Extended Cognitive-Behavior Therapy in Pediatric Obsessive-Compulsive Disorder. J Child Adolesc Psychopharmacol. 2015;25(7):574-579. doi: 10.1089/cap.2015.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mataix-Cols D, Cameron R, Gega L, Kenwright M, Marks IM. Effect of referral source on outcome with cognitive-behavior therapy self-help. Compr Psychiatry. 2006;47(4):241-245. doi: 10.1016/j.comppsych.2005.11.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial protocol
eMethod 1. Interventions
eMethod 2. Assessment of therapist adherence
eMethod 3. Outcome measures (continued)
eMethod 4. Statistical analysis (continued)
eResult 1. Blinding integrity
eResult 2. Reasons not receiving additional treatment as a non-responder
eTable 1. Content of the internet-delivered CBT program for children and adolescents with OCD
eTable 2. Description of therapists
eTable 3. Measures and assessment points
eTable 4. Demographics and clinical characteristics by site
eTable 5. Between-group effect sizes at 6-month follow-up
eTable 6. Observed values and estimated treatment efficacy for ordinal secondary measurements
eTable 7. Treatment response and remission rates across measurement points
eTable 8. Therapist time
eTable 9. Treatment adherence, credibility and satisfaction
eTable 10. Reported adverse events by study group
eFigure 1. Screenshots of the internet-delivered cognitive behavioral therapy program
eReferences
Data sharing statement