Abstract
Introduction and importance
Gastrointestinal stromal tumors (GIST) are rare mesenchymal tumors originating in the wall of the gastrointestinal tract. Jejunal GIST is the rarest subtype. Large GIST can present with an abdominopelvic mass which can be preoperatively misdiagnosed as a gynecological tumor.
Case history
A 44-year regularly menstruating woman presented with lower abdominal pain which was diagnosed as a malignant ovarian tumor preoperatively with an MRI. However, intraoperatively, a lobulated mass was present in the abdominal cavity arising from a jejunal portion of the small intestine. With an intraoperative diagnosis of jejunal GIST, the mass was excised and jejunum anastomosed. Histopathology examination report showed GIST which was further confirmed by immunohistochemistry.
Discussion
GIST presenting as a large abdominopelvic mass can mimic a gynecological tumor. Contrast-enhanced CT scan is the preferred imaging modality for the evaluation of patients with suspected GIST to determine the extent of the tumor, the presence or absence of metastatic disease alongside evaluation of the possibility of complete resection. Adjuvant imatinib therapy following complete excision can decrease the disease recurrence.
Conclusion
Gynecologists should keep in mind that primary gastrointestinal tumors can present as a pelvic mass. A proper histopathological examination helps to confirm the diagnosis. Complete surgical removal of the tumor should be obtained as it determines the prognosis of the disease.
Keywords: Gastrointestinal stromal tumors, GIST, Ovarian neoplasm, Case report
Highlights
-
•
If a pelvic mass is detected, a non-gynecological tumor like a gastrointestinal stromal tumor (GIST) has to be considered.
-
•
Every effort should be made to identify the origin of the tumor and related anatomic structures, especially the ovaries.
-
•
Misdiagnoses may have significant therapeutic implications because of the availability of targeted imatinib-based therapy.
1. Introduction
Gastrointestinal stromal tumors (GISTs) are rare mesenchymal tumors of the alimentary tract and comprise 0.2% of all gastrointestinal tumors and only 0.04% of small intestinal tumors.
GIST can occur in any part of the GI tract and GIST of the jejunum is considered the rarest subtype [1,2]. Herein, We present an unusual case of GIST originating from the jejunum, which was preoperatively misdiagnosed as a pelvic mass arising from the ovary with magnetic resonance imaging (MRI) and ultrasonography (USG) during gynecologic evaluation. As these two entities completely differ from one another, misdiagnosis may have significant therapeutic and prognostic implications. This case has been reported in line with SCARE criteria [3].
2. Case history
A 44-year P2+1 L1 Mongolian regularly menstruating non-alcoholic and non-smoker without any prior surgical history or any family history of malignancy presented to our center with a complaint of insidious onset, continuous and non-radiating left lower abdominal pain for 15 days relieved by analgesics. She didn't have nausea, vomiting, fever, hematochezia/melena, abdominal distension, weight loss, or trauma to the abdomen before the onset of the symptom.
On examination, she was afebrile with a BP of 100/60 mm Hg, pulse rate of 80 bpm, respiratory rate of 15breaths per minute, and Sp02 of 98% in the room air.
On abdominal examination, the lower abdomen was distended. On deep palpation, approximately 18 cm × 20 cm mobile, non-tender cystic mass with a smooth surface was felt occupying bilateral iliac fossa, lumbar region, and hypogastric region with no fluid thrill. These findings were further confirmed via per vaginal examination. Examination of all other systems was grossly intact.
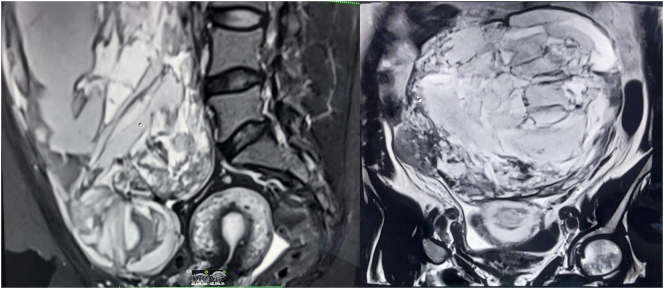
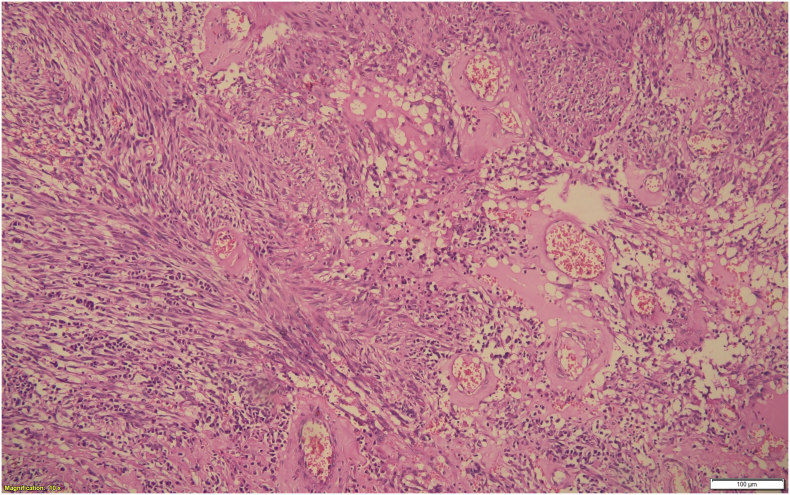
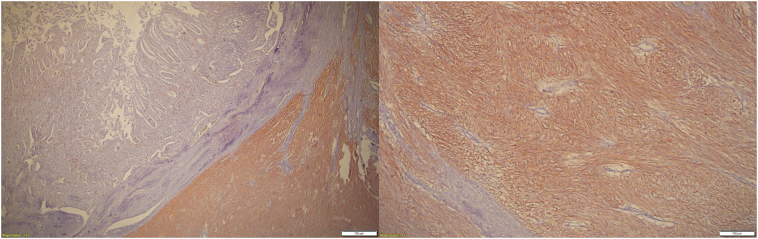
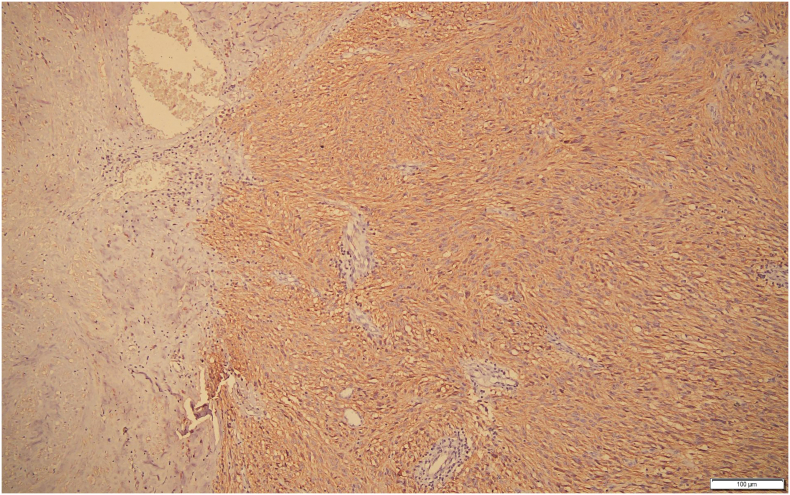
Blood counts were within normal limits however the patient was anemic (Hemoglobin-8.3 g/dl, PCV-27 g%). All other blood investigations including tumor markers; CEA and CA-125, Beta-HCG, and alpha-fetoprotein were within normal limits along with her urinalysis and urine culture. Transabdominal USG revealed a large heterogeneous cystic solid mass with multiple septations and mild vascularity measuring 29 cm × 16 cm × 10 cm arising from the right ovary. With the suspicion of malignant pathology, MRI of abdomen and pelvis was done which revealed a 17.1 cm × 11.7 cm × 19.4 cm multilocular solid cystic mass with inferior aspect contagious with right ovary along with multiple enlarged lymph nodes along iliac vessels and in bilateral inguinal regions; features suggestive of malignant ovarian pathology likely mucinous cystadenoma (Fig. 1). Fine needle aspiration cytology (FNAC) of the right inguinal lymph node was compatible with reactive lymphadenitis. Since a routine FNAC is contraindicated in patients with suspected ovarian tumors to prevent upstaging of disease, FNAC was not performed and she was planned for staging laparotomy by the team of treating gynecologists. An infraumbilical midline incision was given. To our surprise, around 25 cm × 20 cm lobulated mass was present in the abdominal cavity arising from a jejunal portion of the small intestine around 170 cm proximal to the ileocecal junction along with an enlarged right lymph node (Fig. 2). The GI surgery team was called and the mass was excised with the suspicion of a primary gastrointestinal tumor along with subsequent functional jejunojejunal anastomosis. Uterus, Bilateral fallopian tubes, and ovaries were normal and free of any mass. Further, a peritoneal wash was done and sent for cytology which was negative for malignancy. Histopathological examination of the excised mass showed spindle-shaped cells arising from the muscularis propria and arranged in fascicles with oval to elongated nuclei with mild infiltration of lymphocytes in the intervening stroma (Fig. 3). Mitotic figures constitute 2 per 5 mm2. CD117 (c-KIT) and DOG-1 immunostains were strongly positive in the tumor cells confirming the diagnosis of GIST, spindle cell type with high-risk category (Fig. 4, Fig. 5).
Fig. 1.
MRI abdomen and pelvis showing complex multilocular solid cystic abdominopelvic mass.
Fig. 2.
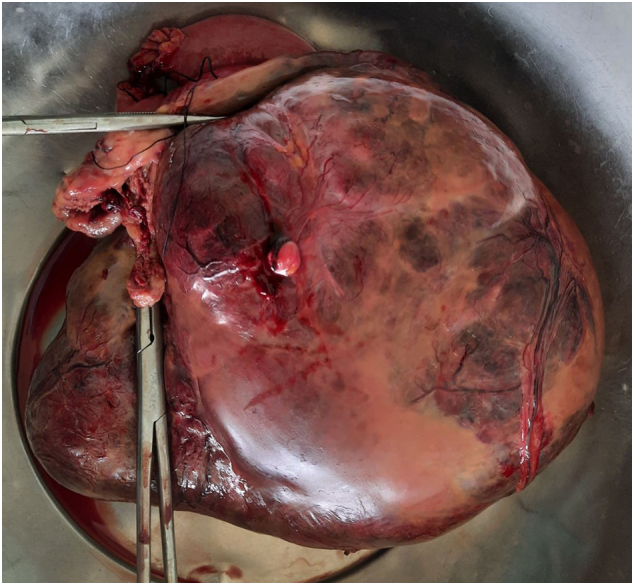
Huge mass excised from the jejunum.
Fig. 3.
Section of the excised mass shows spindle-shaped tumor cells with oval nuclei arranged in fascicles (H&E 200× magnification).
Fig. 4.
Section shows tumor cells arising from muscularis propria (left) with strong cytoplasmic positivity for CD117(right and left). (Immunohistochemistry, X100 magnification).
Fig. 5.
Tumor cells membrane and cytoplasm staining positive for DOG-1 stain.
The post-operative period was uneventful and the patient recovered well. After a tumor board discussion with gynecologists, GI surgeons, and medical oncologists, the patient was started on imatinib considering the large size of the tumor with high-risk assessment. The patient is doing well, happy with the treatment she received, remains disease-free at 6 months of follow-up, and is advised for follow-up every 6 months.
3. Discussion
GISTs are believed to arise from interstitial cells of Cajal or their stem cell precursors [4]. Majority of GISTs are diagnosed in adults over 40 years of age with a peak age at 60–65 years and show a slight male preponderance [5]. Most of them are benign and only 10–30% progress to malignant GISTs [6]. Most common presentations of GISTs include Gastrointestinal (GI) bleeding followed by abdominal pain and GI obstruction. Other presenting symptoms are hematemesis, melena, abdominal distention, palpable mass, and features of perforation, intussusception, and obstruction. Abdominal pain and/or GI bleeding are seen more often in large GISTs owing to the vascular nature of the tumor [7]. Our patient presented with lower abdominal pain and a palpable mass.
Because GISTs don't have a distinct appearance on ultrasound, a contrast-enhanced CT scan is the preferred imaging modality for the evaluation of patients with suspected GIST [8]. Though a CECT cannot distinguish GIST from a gynecologic mass, it helps determine the extent of the tumor and the presence or absence of metastatic disease, and thus, evaluation of the possibility of complete resection [9]. MRI was done in our case because of a suspected malignant ovarian mass in the USG abdomen. It is difficult to distinguish GIST of the small bowel and rectosigmoid areas from ovarian tumors based on clinical features and imaging studies [10]. Moreover, leiomyoma and leiomyosarcoma of the small intestine can mimic primary ovarian neoplasm [11]. Various other differential diagnoses of large pelvic mass are listed in Table 1. Supporting the aforementioned facts, GIST was a difficult diagnosis as the mass was large and appeared to be arising from the right ovary which made the recognition of the origin of the tumor very difficult.
Table 1.
Differential diagnoses of large pelvic mass.
| Uterine neoplasm | Endometrial carcinoma Mesenchymal tumors |
| Cervical neoplasm | Leiomyoma, Squamous cell carcinoma cervix, Adenocarcinoma cervix |
| Fallopian tube neoplasm | Leiomyoma, Teratoma, Adenocarcinoma |
| Ovarian neoplasm | Clear cell adenocarcinoma, Metastatic tumor |
| Gastrointestinal neoplasm | Colorectal carcinoma Gastrointestinal stromal Tumor Soft tissue neoplasm- Hemangiopericytoma, Rhabdomyosarcoma, Liposarcoma, Neurofibroma, Leiomyosarcoma. |
Preoperative diagnosis of GIST is difficult because of its unusual and non-specific symptoms which occurred in our case as well. The tumor is frequently misdiagnosed as a gynecological condition if it exists in the pelvis which can have a significant therapeutic and prognostic implication after the discovery of novel agents [12]. Similarly, our patient was suspected of having a malignant ovarian mass even after an MRI and was diagnosed as GIST intraoperatively and after the histopathological examination of the excised mass.
The treatment modality for non-metastatic GISTs is surgical resection with negative margins without lymph node resection [7]. To minimize the risk of local recurrence and metastatic expansion of GISTs, it is critical to achieving complete excision of localized disease with tumor spillage being prevented [13]. The definitive diagnosis of GIST is based on histology and immunohistochemistry. Positive immunohistochemical staining for CD117 is a defining characteristic of GISTs and currently, it is considered the most specific and sensitive marker for GIST [14]. The immunohistochemistry of the excised mass in our case was positive for CD117 and DOG1 as well, confirming the diagnosis of jejunal GIST. An algorithm to diagnose an intestinal tumor with clinical suspicion of an ovarian mass has been given in Fig. 6.
Fig. 6.
Flowchart showing a diagnostic approach to an abdominopelvic mass with obscure imaging findings.
The prognosis of the tumor depends on the age at presentation, anatomic location, size, histomorphology, immunohistochemistry, and molecular genetics, with tumor size considered the most important [15]. Tumor size and mitotic activity are the two most powerful and well-documented criteria for assessment of the biologic potential of GIST. Irrespective of the mitotic rate, all intestinal GISTs of more than 5 cm have at least moderate risk for metastasis, and all 5 mitoses per 50 high power fields have a high risk for metastases [16].
The mitotic figure in our case is 2 per 5 square mm2 (reported as per CAP protocol on GIST v4.0.1.0) which corresponds to about 22 high power fields in our modern microscopes and the size was more than 10 cm indicating its high risk of metastasis or tumor-related death. Adjuvant imatinib therapy following surgery is necessary for patients with intermediate and high-risk GIST [17].
Recurrence of GIST is common in the majority of patients despite full resection of the tumor with negative margins. This emphasizes the need for regular follow-up examinations and investigations [18]. FDA has approved the use of imatinib as adjuvant chemotherapy for tumors with KIT-positive mutations among adults who have undergone complete resection due to the aforementioned reasons [19]. Our patient received adjuvant imatinib considering the size of the tumor and risk of recurrence. An increase in tumor size or new lesions at the local or distant sites on imaging is indicative of recurrence or progression of the disease [6]. In unresectable, recurrent, or metastatic disease, imatinib is the first-line therapy, the use of which has improved the quality of life and survival of the patients together with fewer recurrent events [20]. However, the optimal duration of this therapy following complete resection remains unclear.
Misdiagnosis of this entity, though common, has significant diagnostic and therapeutic implications. Thus, the treating gynecologist must be aware of this entity along with other gastrointestinal tumors that can potentially mimic an ovarian tumor.
4. Conclusion
GIST is a rare tumor and poses a diagnostic dilemma in women with abdominopelvic mass. As it may mimic gynecologic tumors like an ovarian tumor, gynecologists need to be aware of this condition and consider it in the differential diagnosis of patients presenting with an abdominopelvic mass.
Funding
None.
Ethical approval
Not required.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CRediT authorship contribution statement
Bikal Ghimire (BG), Jayant Sah (JS), Janardan Prasad Joshi (JPJ), and Sansar Babu Tiwari (ST) = Study concept, Data collection, and surgical therapy for the patient.
Bibek Man Shrestha (BMS), Suraj Shrestha (SS), and Sanjeev Kharel (SK) = Writing- original draft preparation.
BMS, Suraj Shrestha (SS), Sanjeev Kharel (SK), and Yasoda Rijal (YR) = Editing and writing.
BG, ST, and JS = senior author and manuscript reviewer.
All the authors read and approved the final manuscript.
Registration of research studies
Not Applicable.
Guarantor
Suraj Shrestha.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None.
Acknowledgment
None.
References
- 1.Kramer K., Siech M., Sträter J., Aschoff A.J., Henne-Bruns D. GI hemorrhage with fulminant shock induced by jejunal gastrointestinal stromal tumor (GIST) coincident with duodenal neuroendocrine carcinoma (NET) + neurofibromatosis (NF) – case report and review of the literature. Z. Gastroenterol. 2005;43(3):281–288. doi: 10.1055/s-2004-813810. [DOI] [PubMed] [Google Scholar]
- 2.Sankey R.E., Maatouk M., Mahmood A., Raja M. Case Report: jejunal gastrointestinal stromal tumour, a rare tumour, with a challenging diagnosis and a successful treatment. J Surg Case Rep. 2015;2015(5) doi: 10.1093/jscr/rjv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Miettinen M., Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med. 2006;130(10):1466–1478. doi: 10.1043/1543-2165(2006)130[1466:GSTROM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Sornmayura P. Gastrointestinal stromal tumors (GISTs): a pathology view point. J. Med. Assoc. Thail. 2009;92(1):124–135. https://www.ncbi.nlm.nih.gov/pubmed/19260254 [PubMed] [Google Scholar]
- 6.Choi H. Response evaluation of gastrointestinal stromal tumors. Oncologist. 2008;13(Suppl. 2):4–7. doi: 10.1634/theoncologist.13-S2-4. [DOI] [PubMed] [Google Scholar]
- 7.Marcella C., Shi R.H., Sarwar S. Clinical overview of GIST and its latest management by endoscopic resection in upper GI: a literature review. Gastroenterol. Res. Pract. 2018;2018:6864256. doi: 10.1155/2018/6864256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hong X., Choi H., Loyer E.M., Benjamin R.S., Trent J.C., Charnsangavej C. Gastrointestinal stromal tumor: role of CT in diagnosis and in response evaluation and surveillance after treatment with imatinib. Radiographics. 2006;26(2):481–495. doi: 10.1148/rg.262055097. [DOI] [PubMed] [Google Scholar]
- 9.Choi H. Imaging modalities of gastrointestinal stromal tumors. J. Surg. Oncol. 2011;104(8):907–914. doi: 10.1002/jso.21871. [DOI] [PubMed] [Google Scholar]
- 10.Ijeri S.K., Rathod P.S., Kundargi R. Gastrointestinal stromal tumor mimicking as ovarian tumor in gynaecologic oncology. Indian J Surg Oncol. 2016;7(1):56–61. doi: 10.1007/s13193-015-0479-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawagoe H., Kataoka A., Sugiyama T., Nishida T., Yakushiji M., Shirouzu K. Leiomyosarcoma of the small intestine presenting as a pelvic mass. Eur. J. Obstet. Gynecol. Reprod. Biol. 1996;66(2):187–191. doi: 10.1016/0301-2115(96)02389-5. [DOI] [PubMed] [Google Scholar]
- 12.Pinto V., Ingravallo G., Cicinelli E. Gastrointestinal stromal tumors mimicking gynecological masses on ultrasound: a report of two cases. Ultrasound Obstet. Gynecol. 2007;30(3):359–361. doi: 10.1002/uog.4097. [DOI] [PubMed] [Google Scholar]
- 13.Romic I., Pavlek G., Romic M. Urgent surgical treatment of GIST of esophago-gastric junction in a patient with giant hiatal hernia. Klin Onkol. 2019;32(4):306–309. doi: 10.14735/amko2019306. [DOI] [PubMed] [Google Scholar]
- 14.González-Cámpora R., Delgado M.D., Amate A.H., Gallardo S.P., León M.S., Beltrán A.L. Old and new immunohistochemical markers for the diagnosis of gastrointestinal stromal tumors. Anal. Quant. Cytol. Histol. 2011;33(1):1–11. https://www.ncbi.nlm.nih.gov/pubmed/22125840 [PubMed] [Google Scholar]
- 15.Huang C.-C., Yang C.-Y., Lai I.-R., Chen C.-N., Lee P.-H., Lin M.-T. Gastrointestinal stromal tumor of the small intestine: a clinicopathologic study of 70 cases in the postimatinib era. World J. Surg. 2009;33(4):828–834. doi: 10.1007/s00268-009-9918-4. [DOI] [PubMed] [Google Scholar]
- 16.Miettinen M., Makhlouf H., Sobin L.H., Lasota J. Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am. J. Surg. Pathol. 2006;30(4):477–489. doi: 10.1097/00000478-200604000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Yin X., Shen C., Yin Y., Cai Z., Chen Z., Zhang B. Giant gastric stromal tumor mimicking as a posterior mediastinal mass: a case report and literature review. Medicine. 2018;97(41) doi: 10.1097/MD.0000000000012816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panbude S.N., Ankathi S.K., Ramaswamy A.T., Saklani A.P. Gastrointestinal stromal tumor (GIST) from esophagus to anorectum - diagnosis, response evaluation and surveillance on computed tomography (CT) scan. Indian J Radiol Imaging. 2019;29(2):133–140. doi: 10.4103/ijri.IJRI_354_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee T. Gastrointestinal stromal tumor (GIST) presenting as a huge pelvic mass. Geburtshilfe Frauenheilkd. 2013;73(1):70–73. doi: 10.1055/s-0032-1328039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Balachandran V.P., DeMatteo R.P. Gastrointestinal stromal tumors: who should get imatinib and for how long? Adv. Surg. 2014;48:165–183. doi: 10.1016/j.yasu.2014.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]