Abstract
Significant gender-based health inequalities have been observed across Europe, with women reporting worse health than men. Still, there has been little examination of how the gender–health gap has changed over time, and how it has been shaped by societal gender equality. We used data from the Statistics on Income and Living Conditions Eurostat database (EU-SILC), involving 2,931,081 participants aged 25–64, for 27 European countries. Logistic regressions were performed to model the association between self-reported bad health and gender, in general and over time. Analyses were stratified by employment, education, and clusters of countries according to levels of Gender Equality Index (GEI). Adjusting for age, year, and country, bad health was 17% more likely among women, but this disadvantage ceased after accounting for education and employment. Gender–health inequalities were larger among countries with higher GEI scores and among low-educated groups. The gender–health gap did not reduce significantly between 2004 and 2016, in general and within subgroups. Although societies are becoming more equal, persistent inequalities in employment and income still lead to sustained health differences between men and women.
Keywords: Europe, health inequalities, gender, socioeconomic factors
Gender accounts for significant differences in health outcomes, albeit paradoxically. Although women live longer, this advantage does not translate into healthier years,1,2 as they steadily report worse health status and suffer from a higher burden of non-fatal and debilitating conditions.3
Aside from biological characteristics, several factors underpin these differences. Men and women are differently influenced by the social determinants of health, with women particularly hit by unfavorable socioeconomic and psychosocial factors.4 Some authors have described women’s morbidity disadvantage as a consequence of the patriarchy, which restrains women’s access to social and employment-related privileges and economic resources.5–7
Several studies have focused on gender-based inequalities in health at the country level, as gender gaps vary cross-nationally, likely as a result of country-specific conditions.8 Still, little is known about how gender differences in Europe have evolved in recent years and which country-specific factors have been driving these differences.
According to previous literature, there are contradictory hypotheses. Gender inequality is decreasing in European societies in its various dimensions. Policies to promote gender equality through several spheres of society have been implemented6,9–11 and have been connected to decreased health inequalities.12 Gender differences in educational attainment have ended, with a current advantage for women in secondary and tertiary education.13
Notwithstanding, equality has not been achieved yet. Women are less employed than men and more often work part-time.14 Segregation persists, with some jobs considered exclusive for women, mirroring the traditional gendered division of work.15 Women are employed in lower-paid sectors and receive lower salaries.14Time-use is unfairly distributed, and women are more often faced with the double burden of paid job and household/caregiving tasks.14 These persistent inequalities may also harm women’s health, through psychosocial mechanisms, by disappointing their expectations of an equal society.16
Additionally, there is evidence showing that the Great Recession – and austerity – might have widened health inequalities.17,18 It has been shown that women were more affected than men in countries that experienced a severe recession, especially in those that implemented austerity, such as Greece, Portugal, Spain, and the United Kingdom.19–21
Finally, increased societal gender equality may promote the adoption of unhealthy, masculine health-related practices.8 Gender gaps on smoking and alcohol consumption have been closing,22,23 and the prevalence and mortality of diseases such as lung cancer and cardiovascular disease have been rising among women, thus increasing gender-based inequalities in morbidity.10,24
Studies have tried to understand the links between societal gender equality and the gender gap in health, but results have depended on the outcomes, the measure of equality, and the period under analysis.25 Previous research has largely been cross-sectional, with little examination of the interaction between gender-based health inequalities and socioeconomic status.5,26 In this article, we provide the first analysis of the evolution of gender-based inequalities in self-reported health for 27 European countries from 2004–2016 and examine any association with changes in societal gender equality. We also examine how the evolution of gender-based inequalities varies by socioeconomic status.
Methods
Data Sources
Repeated cross-sectional data from the Statistics on Income and Living Conditions Eurostat (EU-SILC) survey were used. This instrument collects annual micro-data on income, poverty, labor, education, and health, using representative samples of European countries.27 Data from EU-SILC has previously been used in comparative research about health inequalities.17,19
We used individual data spanning 13 years, from 2004 to 2016, for 27 countries (Austria, Belgium, Bulgaria, Cyprus, Czechia, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, the Netherlands, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, and the United Kingdom). We excluded data from Iceland, Norway, Serbia, and Switzerland, because the gender index was not available for non-E.U. countries, and from Croatia, as data was only available for a small subset of years.
We excluded subjects above age 64 (n = 1,246,131), to consider the employment status of the working-age population; those under age 25 (n = 706,279), as they may not have finished their education17; and other participants with inconsistent age-related information (n = 85). We excluded observations with missing information on self-reported health (n = 493,137) and other variables used in our models (n = 15,148). Finally, we excluded those who reported being students (n = 37,599), disabled (n = 128,158), or military (n = 288), as their health assessment was not representative of the general population.
Our final sample included 2,931,081 participants. To adjust for non-response, we used the personal weights provided with the database.
Dependent Variable
Self-reported health was obtained through the question “How is your health in general?” This variable has been shown to be associated with both physical and mental health problems28 and has been used in previous studies about gender–health inequalities.29 We recoded it as a binary variable and modeled bad health (original options “Bad” and “Very bad,” as opposed to “Very good,” “Good” and “Fair”).
Explanatory Variables
Gender was measured as male or female sex. Societal gender inequality was assessed by the Gender Equality Index (GEI),30 an index aiming to monitor the evolution of gender equality across E.U. countries. The core index is formed by 6 domains (Work, Money, Knowledge, Time, Power, and Health), varying between 1 (total inequality) and 100 (full equality). We used data from 2005 and 2015 to understand the evolution of gender equality over time. The Health domain was excluded to avoid correlation with our dependent variable, so we calculated an arithmetic mean of the other 5 domains.
Covariates
Age was used as a continuous variable for adjustments and categorically for characterization of the sample.
Socioeconomic status was measured by educational level and employment status. Educational level was coded as “Up to lower secondary education,” “Upper secondary education” (including post-secondary non-tertiary education), and “Tertiary education.” Employment status was coded as “Employed” (full-time or part-time), “Unemployed,” “Retired,” and “Out of labor” (those executing domestic tasks and other inactive persons).
Year of the survey and country were included as fixed effects. We added country-dummy variables to account for time-invariant, country-specific characteristics, such as cultural patterns,31 and year-dummy variables to estimate differences in our dependent variable over time.
Data Analysis
We performed logistic regression models to model bad health as function of gender, first adjusting for age, year, and country, and then also for educational level and employment status.
To test if gender differences have changed over time, we then added the gender × year interaction term and calculated the yearly odds ratio (OR) for women (versus men). To understand the role of educational level and employment status on shaping the evolution of gender differences, analyses were then stratified by these 2 variables.
Afterward, we used K-means clustering analysis to classify countries by their societal gender equality, using the GEI score of 2005 and the difference between 2015 and 2005. We opted for a 5-cluster solution, as this was the first in which significant differences (P < .05) were noted for both variables, and named the clusters according to the GEI scores of 2005 and 2015.
To assess gender-based inequalities for each cluster, models were performed with the gender × cluster interaction. Finally, logistic regression models with gender × year interaction were performed with data stratified by cluster, to assess the evolution of gender inequalities for each cluster.
Data analysis was performed with STATA-13 and SPSS. Results were statistically significant when P < .05. When appropriate, 95% confidence intervals (95%CI) are presented. For the interaction terms, we calculated the OR and 95%CI by sequentially changing the reference categories of the model.32
Ethics
Data collection respected the Helsinki Convention.33 All the analyses were performed with anonymized data, with no access to personal information.
Results
Description of the Sample
Women were slightly older than men, with a higher proportion among the 55–64 group (23.3%) and a lower representation among the 25–34 age group (23.2%) (Table 1). There were more women with up to lower secondary (26.2%) and tertiary education (28.2%) than men. There were more employed men (81.6%) than women (66.4%), whereas 17.9% of women were out of labor, against 1.9% of men.
Table 1.
Characterization of the sample (% Observations) (N = 2,931,081).
| Total sample | Men (48.9%) | Women (51.1%) | |
|---|---|---|---|
| Age groups | |||
| 25–34 | 23.4 | 23.6 | 23.2 |
| 35–44 | 27.5 | 27.8 | 27.2 |
| 45–54 | 26.4 | 26.5 | 26.3 |
| 55–64 | 22.7 | 22.1 | 23.3 |
| Age in years (mean ± SD) | 44.1 ± 11.0 | 44.2 ± 11.0 | 44.5 ± 11.1 |
| Educational level | |||
| Up to lower secondary | 25.1 | 24.7 | 26.2 |
| Upper secondary | 47.1 | 48.2 | 45.6 |
| Tertiary | 27.8 | 27.1 | 28.2 |
| Employment status | |||
| Employed | 73.9 | 81.6 | 66.4 |
| Unemployed | 8.5 | 9.0 | 8.1 |
| Retired | 7.6 | 7.5 | 7.6 |
| Out of labor | 10.1 | 1.9 | 17.9 |
Gender-Based Health Inequalities in Europe
Women were 17% (OR = 1.17, 95%CI = 1.15–1.19) more likely to report bad health than men, adjusting for age, year, and country. When education and employment were factored in, women became less likely to report bad health than men (OR = 0.97, 95%CI = 0.96–0.99). Supplemental Table 1 provides results stratified by country.
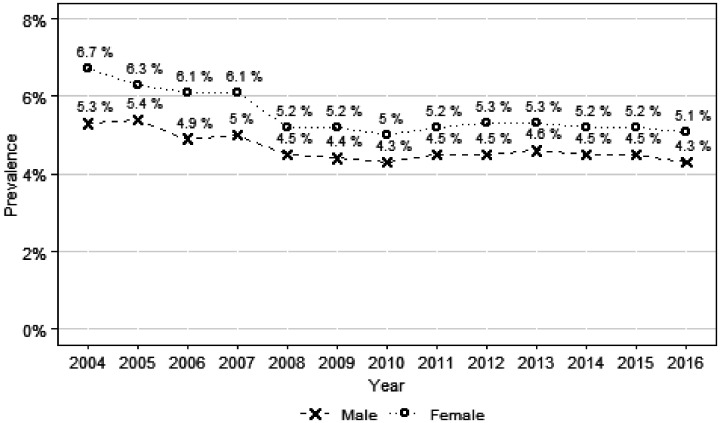
The prevalence of bad health has decreased between 2004 to 2016 (Figure 1), among women (from 6.7% to 5.1%) and men (from 5.3% to 4.3%). The lowest prevalence was achieved in 2010 for both genders.
Figure 1.
Prevalence of bad self-reported health, by gender, between 2004 and 2016.
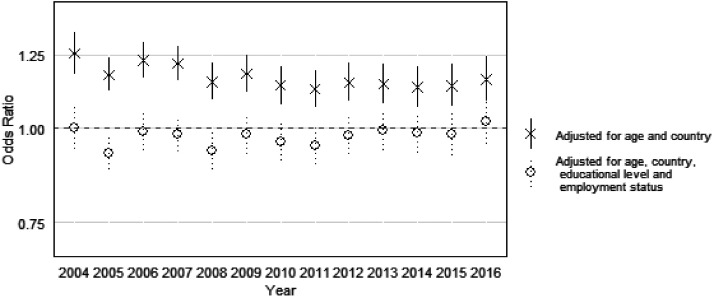
Figure 2 shows the yearly women’s OR (versus men) obtained by the gender × year interactions. When adjusting for age, country, and year, women have higher odds for reporting bad health in every year. The OR for women’s bad health were larger in 2004 and smaller in 2010. However, all CI overlapped, so differences between years were non-significant. When adding education and employment to our models, women’s disadvantage ceased to exist in all the years, but again, with no significant differences between the years.
Figure 2.
Risk of female bad self-reported health (OR, 95% CI), versus men (gender × year interaction), from 2004 to 2016.
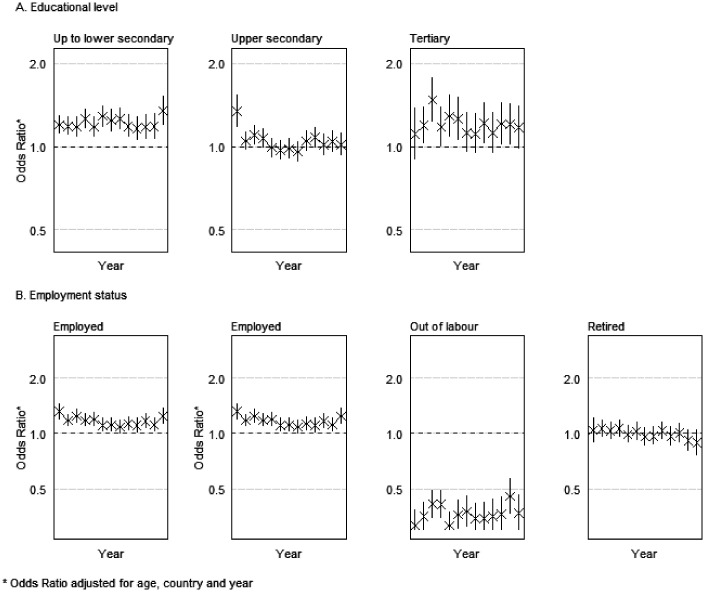
Gender-Based Health Inequalities by Socioeconomic Status
Women’s health disadvantage was higher among low-educated groups, and this has not significantly decreased since 2004 (Figure 3A). Among this group, differences were larger in 2016 (OR = 1.34, 95%CI = 1.19–1.51). Among the upper secondary group, differences were only significant in 2004 (OR = 1.34, 95%CI = 1.17–1.53) and 2006 (OR = 1.10, 95%CI = 1.01–1.19). No significant gender differences were observed thereafter, and all confidence intervals overlapped after 2005. Among the group with tertiary education, OR were significant in several of the years under study, being larger in 2006 (OR = 1.48, 95%CI = 1.23–1.77). Still, no significant changes were found from 2004 to 2016.
Figure 3.
Risk of female bad self-reported health (OR, 95% CI), versus men (gender × year interaction), from 2004 to 2016, stratified by educational level and employment status.
Gender-based health inequalities among those employed have been stable (Figure 3B) and significant in every year but 2011. Among the unemployed, women had lower odds for reporting bad health between 2005 and 2008, with no significant differences since 2009. However, differences between years were not significant.
Evolution of the Gender Equality Index
GEI’s mean score was 59.78 in 2005 and 63.44 in 2015. Greece scored worst in both years (49.2 and 51.38), whereas Sweden scored best (78.92 and 82.5). All countries had a higher GEI score in 2015, with the smallest increases observed in Hungary (0.32) and the United Kingdom (0.4), and the largest in Italy (7.94) and Cyprus (7.6).
K-means cluster analysis returned 5 clusters (Supplemental Figure 1). The cluster “Low-Low” (Bulgaria, Czechia, Estonia, Greece, Hungary, Lithuania, Poland, Romania, and Slovakia) had low equality in 2005 (52.93) and a small increase (2.12) until 2015. Cyprus, Italy, Latvia, Malta, and Portugal formed the cluster “Low-Medium.” This cluster had the lowest mean value in 2005 (52.87) and the largest increase to 2015 (6.02). The cluster “Medium-Medium” was formed by Austria, Germany, France, Ireland, Slovenia and Spain. This group’s mean GEI evolved from 62.42 to 67.71. Belgium, Finland, Luxembourg, Netherlands, and the United Kingdom composed the cluster “High-High,” with mean GEI of 69.04 in 2005 and growth of 2.42. The cluster “Very high-Very high” (Denmark and Sweden) had the highest equality (mean of 76.73 in 2005 and 79.65 in 2015).
Table 2 shows the results of the interaction gender × cluster. Women were more likely to report bad health in all clusters, adjusting for age, country, and year. Inequalities were larger in the cluster “Very high-Very high” (OR = 1.36, 95%CI = 1.26–1.48) and smaller in the cluster “Medium-Medium” (OR = 1.09, 95%CI = 1.06–1.12). After adjusting for employment and education, women’s disadvantage persisted in all clusters other than “Low-Low” and “Medium-Medium.” The largest inequalities remained in the cluster “Very high-Very high.”
Table 2.
Distribution of bad self-reported health by gender (%) and risk of female bad self-reported health (OR and 95%CI), versus men (gender × cluster interaction), by cluster of Gender Equality Index (2004–2016).
| Bad self-reported health(%) |
Risk of female bad self-reported health (OR, 95% CI) |
||||
|---|---|---|---|---|---|
| Cluster | Countries | Men | Women | Adjusted for agea | Adjusted for age, educational level, and employment statusa |
| Low–Low | Bulgaria, Czechia, Estonia, Greece, Hungary, Lithuania, Poland, Romania, Slovakia | 5.5 | 6.7 | 1.18 (1.15–1.20)* | 0.97 (0.95–1.00)* |
| Low–Medium | Cyprus, Italy, Latvia, Malta, Portugal | 5.2 | 6.6 | 1.27 (1.23–1.31) | 1.04 (1.01–1.08)* |
| Medium–Medium | Austria, Germany, Spain, France, Ireland, Slovenia | 4.9 | 5.4 | 1.09 (1.06–1.12)* | 0.91 (0.88–0.94)* |
| High–High | Belgium, Finland, Luxembourg, Netherlands, United Kingdom | 2.7 | 3.4 | 1.28 (1.22–1.36) | 1.07 (1.01–1.13)* |
| Very high–Very high | Denmark, Sweden | 3.0 | 4.1 | 1.36 (1.26–1.48) | 1.37 (1.26–1.48) |
Abbreviations: CI, confidence interval; OR, odds ratio.
All OR are also adjusted for country and year (fixed effects).
P value < .05 (“Very high-Very high” as the reference category).
Evolution of Gender Inequalities by Gender Equality Index Groups
Gender–health inequalities were significant in both 2004 and 2016 among clusters “Low-Low,” “Low-Medium,” and “High-High.” Among the cluster “Medium-Medium,” gender-based inequalities were only significant between 2004 and 2007. Regarding the cluster “Very high-Very high,” the gender–health gap started being significant in 2008, with the largest health inequalities in 2015. Overall, 95%CI overlapped in all clusters, so differences between years were not significant (Supplemental Figure 2).
Discussion
This study aimed to understand the evolution of gender differences in self-reported health from 2004 to 2016 and to analyze how levels of societal gender equality might have shaped these changes. Women were more likely to report bad health, without any significant decrease of gender-based inequalities, in general and by sub-groups. Those in the least educated groups experienced the highest gender-related inequalities, whereas countries with greater societal gender equality did not experience a smaller health gap.
As expected, bad health was more common among women.3,8,29 Gender inequalities were fully explained by socioeconomic disparities between men and women, and, when educational level and employment were factored in, women even had a small health advantage compared to men. Previous research has stressed how gender differences in health measures are impacted by inequalities in the distribution of social determinants of health,4,8,34 especially the overrepresentation of women in groups with lower social resources.4
The prevalence of bad self-reported health has decreased for both genders, but no large gains were obtained, for men or women, since 2008. This is consistent with previous studies in Europe that show that the Great Recession terminated the positive trend in self-reported health,35,36 although some evidence has shown that the evolution depends on gender and age.35,37
Our main results show that gender inequalities in health persisted between 2004 and 2016, with a non-significant decrease. This happened regardless of the educational level, employment status, or cluster of societal gender equality. This may be related to the persistence of inequalities in society. Our data show that in 2016, women were still less likely to be employed than men, even though the proportion of women out of the labor force has been decreasing since 2004 (Supplemental Table 2). The employment gap has already been described as one of the main factors underlying gender inequalities in health and is associated with differences in outcomes such as chronic diseases and self-reported health.3,4 Female participation in the workforce may indeed have beneficial health effects for women, promoting their economic empowerment, social interaction, and self-esteem.38,39
Still, inequalities remain after women enter the workforce, as gender-based inequalities persist when solely employed people are included. This may be due to the enduring gender wage gap, regardless of women’s higher educational attainment,40 or the persistence of labor segregation, despite the increase of women in high-skilled, male-dominated occupations.15 Women are also burdened by combining their paid jobs with unequally distributed household and family-related activities.14
Gender-based health inequalities have persisted despite the increase of societal gender equality in all countries, as measured by the GEI. Gender equality typically involves 2 opposite movements toward non-traditional territories: women’s entrance into the job market and men’s increased participation in domestic and family-related tasks.39 Alone, the entrance of women in the job market may not be enough to end gender-based inequalities, as women may become more burdened by inequalities in the division of household labor.25,39
Our results also indicate larger gender differences among the group with lowest education, consistent with previous findings.41 Women with lower socioeconomic status may face specific threats to their health status. Gender gaps in employment rate and income are larger among low-educated persons.42 The domestic autonomy and bargaining power of these women may be limited by their lower individual income,43 increasing their vulnerability to intimate partner abuse.44 These women are also more likely to experience single parenthood and to raise children with less contact with the fathers.45 These women’s health disadvantage may create a vicious circle, in which poor health is influenced by low socioeconomic status and in turn contributes to it via downward social mobility or limited job opportunities/pay.41,46
Gender-based inequalities were significant for all the clusters of countries and larger in the cluster with higher societal gender equality. Previous research has shown that gender health inequalities persist in Scandinavian countries (particularly Sweden), despite the improvement in societal gender equality.16 This is the only cluster in which relative gender-based inequalities did not decrease after educational level and employment status were factored in, showing the limited explanatory relevance of these factors. This could be due to other structural factors such as the gender pay gap,47 labor market segregation,15 or women’s unfulfilled expectations of an equalitarian society.16 This paradox has some similarities with the Nordic public health puzzle, whereby despite having greater income equality, Scandinavian countries have larger relative health inequalities.48
Strengths and Limitations
Our study provides information about the evolution of gender health inequalities by using a dataset of almost 3 million observations, with comparable longitudinal data from 27 countries.
To our knowledge, this is the first study using GEI to assess gender-based inequalities. Although some studies have used other measures of societal gender equality (Gender Inequality Index, Gender Empowerment Measure, or Gender Development Index),25 GEI provides a quantification of gender equality based on a much wider set of indicators. Although the index is not available for every year, we were able to capture the evolution of gender equality by using data from 2005 and 2015. Measures of gender equality are believed to differ among regions of the same country, particularly in decentralized states such as Germany and Spain.49 Still, no disaggregated data were available regarding the GEI or its components.
Self-reported health has been proven a reliable tool to assess health for both men and women,28,34 but it largely differs among countries and cultural settings.8,26,50 We believe that this bias may have been controlled by focusing on a measure of relative inequality (OR), instead of the prevalence of bad self-reported health.
Conclusions
This study examined the evolution of gender inequalities in self-reported health in Europe between 2004 and 2016, in general and by socioeconomic status, and how levels of societal gender equality might have shaped any changes. Results show that women are more likely to report bad health, without any significant decrease of relative gender-based inequalities over time. Women in the least educated groups experience the highest gender–health gap. Differences in education and employment appear to be important in shaping gender-related inequalities in health, while countries with greater societal gender equality do not experience a smaller health gap. That is, our results do not support that higher levels of gender-equality inevitably lead to a smaller gender–health gap. Future research should examine why this is the case.
Supplemental Material
Supplemental material, sj-pdf-1-joh-10.1177_0020731420960344 for Gender Equality and Gender Inequalities in Self-Reported Health: A Longitudinal Study of 27 European Countries 2004 to 2016 by Luis Roxo, Clare Bambra and Julian Perelman in International Journal of Health Services
Supplemental material, sj-pdf-2-joh-10.1177_0020731420960344 for Gender Equality and Gender Inequalities in Self-Reported Health: A Longitudinal Study of 27 European Countries 2004 to 2016 by Luis Roxo, Clare Bambra and Julian Perelman in International Journal of Health Services
Acknowledgments
The authors thank the European Commission for providing the access to the dataset (RPP 134/2020-EU-SILC) and declare that the results and conclusions are not those of Eurostat, the European Commission, or any of the national statistical authorities whose data have been used.
Author Biographies
Luis Roxo is a PhD candidate in the Global Public Health PhD Programme at NOVA National School of Public Health, Universidade NOVA de Lisboa, Portugal. He holds a master’s degree in clinical psychology from the University of Lisbon. His research interests are in the areas of gender, health inequalities, and mental health.
Clare Bambra, PhD, FAcSS, is a professor of public health in the Population Health Sciences Institute, Newcastle University, United Kingdom. She is an interdisciplinary social scientist working at the interface of public health, health politics and policy, health geography, and social epidemiology. Her mixed-methods research focuses on understanding and reducing health inequalities. She has published widely, including several books. She is a senior investigator in several large collaborations: CHAIN: Centre for Global Health Inequalities Research, NIHR Policy Research Unit in Behavioural Science, SIPHER: UKPRP Consortium on Systems Science in Public Health, NIHR Applied Research Collaboration – North East and North Cumbria (NE-NC-ARC), NIHR Communities in Control Study, and NIHR School for Public Health Research and Fuse: The Centre for Translational Research in Public Health. She is a director of the Equal England: Health Inequalities Knowledge Exchange Network. She works regularly with policy and practice organizations, including Public Health England, the European Union, and the World Health Organization.
Julian Perelman holds a PhD in economics from Université Catholique de Louvain, Belgium. He is an associate professor at the Portuguese National School of Public Health, NOVA University of Lisbon, and vice president of the Portuguese Commission for Health Technology Evaluation, CATS. He coordinated the Mission Framework for the Sustainability of the Health Budget Program (Ministry of Health and Ministry of Finance) from 2018 to 2020. He has authored more than 80 publications in indexed scientific journals, mainly related to economic evaluation in health, socioeconomic determinants of health, and payment systems and incentives.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: L. R. is a PhD student funded by the Portuguese Foundation for Science and Technology – FCT [PD/BD/135591/2018].
ORCID iDs: Luis Roxo https://orcid.org/0000-0001-6946-6501
Julian Perelman https://orcid.org/0000-0001-6634-9000
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Solé-Auró A, Jasilionis D, Li P, Oksuzyan A. Do women in Europe live longer and happier lives than men? Eur J Public Health. 2018; 28(5):847–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Oyen H, Nusselder W, Jagger C, Kolip P, Cambois E, Robine JM. Gender differences in healthy life years within the EU: an exploration of the “health-survival” paradox. Int J Public Health. 2013; 58(1):143–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boerma T, Hosseinpoor AR, Verdes E, Chatterji S. A global assessment of the gender gap in self-reported health with survey data from 59 countries. BMC Public Health. 2016; 16: 675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Denton M, Prus S, Walters V. Gender differences in health: a Canadian study of the psychosocial, structural and behavioural determinants of health. Soc Sci Med. 2004; 58(12):2585–2600. [DOI] [PubMed] [Google Scholar]
- 5.Gkiouleka A, Huijts T, Beckfield J, Bambra C. Understanding the micro and macro politics of health: inequalities, intersectionality & institutions – a research agenda. Soc Sci Med. 2018; 200:92–98. [DOI] [PubMed] [Google Scholar]
- 6.Palència L, De Moortel D, Artazcoz L, et al. Gender policies and gender inequalities in health in Europe: results of the SOPHIE project. Int J Health Serv. 2017; 47(1):61–82. [DOI] [PubMed] [Google Scholar]
- 7.Stanistreet D, Bambra C, Scott-Samuel A. Is patriarchy the source of men’s higher mortality? J Epidemiol Community Heal. 2005; 59(10):873–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dahlin J, Härkönen J. Cross-national differences in the gender gap in subjective health in Europe: does country-level gender equality matter? Soc Sci Med. 2013; 98:24–28. [DOI] [PubMed] [Google Scholar]
- 9.Beckfield J, Morris KA, Bambra C. How social policy contributes to the distribution of population health: the case of gender health equity. Scand J Public Health. 2018; 46(1):6–17. [DOI] [PubMed] [Google Scholar]
- 10.Morris KA, Beckfield J, Bambra C. Who benefits from social investment? The gendered effects of family and employment policies on cardiovascular disease in Europe. J Epidemiol Community Health. 2019; 73(3):206–213. [DOI] [PubMed] [Google Scholar]
- 11.Pascall G, Lewis J. Emerging gender regimes and policies for gender equality in a wider Europe. J Soc Policy. 2004; 33(3):373–394. [Google Scholar]
- 12.Borrell C, Palència L, Muntaner C, Urquía M, Malmusi D, O’Campo P. Influence of macrosocial policies on women’s health and gender inequalities in health. Epidemiol Rev. 2014; 36(1):31–48. [DOI] [PubMed] [Google Scholar]
- 13.Organisation for Economic Co-operation and Development. Education at a Glance 2018. Paris, France: OECD; 2018. [Google Scholar]
- 14.European Commission. 2018 Report on Equality Between Women and Men in the EU; Brussels, Belgium: European Commission; 2018. [Google Scholar]
- 15.Gonäs L, Wikman A, Vaez M, Alexanderson K, Gustafsson K. Changes in the gender segregation of occupations in Sweden between 2003 and 2011. Scand J Public Health. 2019; 47(3):344–347. [DOI] [PubMed] [Google Scholar]
- 16.Olafsdottir S. Gendered health inequalities in mental well-being? The Nordic countries in a comparative perspective. Scand J Public Health. 2017; 45(2):185–194. [DOI] [PubMed] [Google Scholar]
- 17.Leão T, Campos-Matos I, Bambra C, Russo G, Perelman J. Welfare states, the Great Recession and health: trends in educational inequalities in self-reported health in 26 European countries. PLoS One. 2018; 13(2):e0193165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suhrcke M, Stuckler D. Will the recession be bad for our health? It depends. Soc Sci Med. 2012; 74(5):647–653. [DOI] [PubMed] [Google Scholar]
- 19.Abebe DS, Tøge AG, Dahl E. Individual-level changes in self-rated health before and during the economic crisis in Europe. Int J Equity Health. 2016; 15:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bambra C, ed. Health in Hard Times: Austerity and Health Inequalities. Bristol, England: Bristol University Press; 2019. [Google Scholar]
- 21.Greer Murphy A. Austerity in the United Kingdom: the intersections of spatial and gendered inequalities. Area. 2017; 49(1):122–124. [Google Scholar]
- 22.World Health Organization. European Tobacco Use Trends Report 2019. Geneva, Switzerland: World Health Organization; 2019. [Google Scholar]
- 23.Bratberg GH, Wilsnack SC, Wilsnack R, et al. Gender differences and gender convergence in alcohol use over the past three decades (1984-2008), The HUNT Study, Norway. BMC Public Health. 2016; 16:723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malvezzi M, Carioli G, Bertuccio P, et al. European cancer mortality predictions for the year 2018 with focus on colorectal cancer. Ann Oncol. 2018; 29(4):1016–1022. [DOI] [PubMed] [Google Scholar]
- 25.King TL, Kavanagh A, Scovelle AJ, Milner A. Associations between gender equality and health: a systematic review. Health Promot Int. 2018; 35(1):27–41. [DOI] [PubMed] [Google Scholar]
- 26.Bambra C, Pope D, Swami V, et al. Gender, health inequalities and welfare state regimes: a cross-national study of 13 European countries. J Epidemiol Community Heal. 2009; 63:38–44. [DOI] [PubMed] [Google Scholar]
- 27.Arora VS, Karanikolos M, Clair A, Reeves A, Stuckler D, Mckee M. Data resource profile: the European Union Statistics on Income and Living Conditions (EU-SILC). Int J Epidemiol. 2015; 44(2):451–461. [DOI] [PubMed] [Google Scholar]
- 28.Baćak V, Ólafsdóttir S. Gender and validity of self-rated health in nineteen European countries. Scand J Public Health. 2017; 45(6):647–653. [DOI] [PubMed] [Google Scholar]
- 29.Palencia L, Malmusi D, De Moortel D, et al. The influence of gender equality policies on gender inequalities in health in Europe. Soc Sci Med. 2014; 117:25–33. [DOI] [PubMed] [Google Scholar]
- 30.European Institute for Gender Equality. Gender Equality Index 2017: Measuring Gender Equality in the European Union 2005-2015. Vilnius, Lithuania: European Institute for Gender Equality; 2017. [Google Scholar]
- 31.Gardiner JC, Luo Z, Roman LA. Fixed effects, random effects and GEE: what are the differences? Stat Med. 2009; 28(2):221–239. [DOI] [PubMed] [Google Scholar]
- 32.Figueiras A, Domenech-Massons JM, Cadarso C. Regression models: calculating the confidence interval of effects in the presence of interactions. Stat Med. 1998; 17(18):2099–2105. [DOI] [PubMed] [Google Scholar]
- 33.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013; 310(20):2191–2194. [DOI] [PubMed] [Google Scholar]
- 34.Zajacova A, Huzurbazar S, Todd M. Gender and the structure of self-rated health across the adult life span. Soc Sci Med. 2017; 187:58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Põld M, Pärna K, Ringmets I. Trends in self-rated health and association with socioeconomic position in Estonia: data from cross-sectional studies in 1996–2014. Int J Equity Health. 2016; 15(1):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reile R, Helakorpi S, Klumbiene J, Tekkel M, Leinsalu M. The recent economic recession and self-rated health in Estonia, Lithuania and Finland: a comparative cross-sectional study in 2004–2010. J Epidemiol Community Health. 2014; 68(11):1072–1079. [DOI] [PubMed] [Google Scholar]
- 37.Sperlich S, Tetzlaff J, Geyer S. Trends in good self-rated health in Germany between 1995 and 2014: do age and gender matter? Int J Public Health. 2019; 64(6):921–933. [DOI] [PubMed] [Google Scholar]
- 38.Artazcoz L, Borrell C, Benach J, Cortès I, Rohlfs I. Women, family demands and health: the importance of employment status and socio-economic position. Soc Sci Med. 2004; 59(2):263–274. [DOI] [PubMed] [Google Scholar]
- 39.Backhans MC, Lundberg M, Månsdotter A. Does increased gender equality lead to a convergence of health outcomes for men and women? A study of Swedish municipalities. Soc Sci Med. 2007; 64(9):1892–1903. [DOI] [PubMed] [Google Scholar]
- 40.Boye K, Halldén K, Magnusson C. Stagnation only on the surface? The implications of skill and family responsibilities for the gender wage gap in Sweden, 1974-2010. Br J Sociol. 2017; 68(4):595–619. [DOI] [PubMed] [Google Scholar]
- 41.Mwinyi J, Pisanu C, Castelao E, Stringhini S, Preisig M, Schiöth HB. Anxiety disorders are associated with low socioeconomic status in women but not in men. Women’s Heal Issues. 2017; 27(3):302–307. [DOI] [PubMed] [Google Scholar]
- 42.Organisation for Economic Co-operation and Development. The Pursuit of Gender Equality. Paris, France: OECD; 2017. [Google Scholar]
- 43.Malmusi D, Vives A, Benach J, Borrell C. Gender inequalities in health: exploring the contribution of living conditions in the intersection of social class. Glob Health Action. 2014; 7(1):23189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reichel D. Determinants of intimate partner violence in Europe: the role of socioeconomic status, inequality, and partner behavior. J Interpers Violence. 2017; 32(12):1853–1873. [DOI] [PubMed] [Google Scholar]
- 45.Jalovaara M, Andersson G. Disparities in children’s family experiences by mother’s socioeconomic status: the case of Finland. Popul Res Policy Rev. 2018; 37:751–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kröger H, Pakpahan E, Hoffmann R. What causes health inequality? A systematic review on the relative importance of social causation and health selection. Eur J Public Health. 2015; 25(6):951–960. [DOI] [PubMed] [Google Scholar]
- 47.European Union. A Decomposition of the Unadjusted Gender Pay Gap Using Structure of Earnings Survey Data. Luxembourg: European Union; 2018. [Google Scholar]
- 48.Bambra C. Health inequalities and welfare state regimes: theoretical insights on a public health “puzzle”. J Epidemiol Community Heal. 2011; 65(9):740–745. [DOI] [PubMed] [Google Scholar]
- 49.Vives-Cases C, Álvarez-Dardet C, Carrasco-Portiño M, Torrubiano-Domínguez J. El impacto de la desigualdad de género en la violencia del compañero íntimo en España. Gac Sanit. 2007; 21(3):242–246. [DOI] [PubMed] [Google Scholar]
- 50.Burgard SA, Chen PV. Challenges of health measurement in studies of health disparities. Soc Sci Med. 2014; 106:143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-joh-10.1177_0020731420960344 for Gender Equality and Gender Inequalities in Self-Reported Health: A Longitudinal Study of 27 European Countries 2004 to 2016 by Luis Roxo, Clare Bambra and Julian Perelman in International Journal of Health Services
Supplemental material, sj-pdf-2-joh-10.1177_0020731420960344 for Gender Equality and Gender Inequalities in Self-Reported Health: A Longitudinal Study of 27 European Countries 2004 to 2016 by Luis Roxo, Clare Bambra and Julian Perelman in International Journal of Health Services