Abstract
The novel SARS-CoV-2 virus has affected children and adolescents throughout the world since its discovery in 2019. For many children, infection with SARS-CoV-2 presents as an asymptomatic to mild infection. However, in a small subset of children who become infected with the SARS-CoV-2 virus, a more severe post-infectious inflammatory illness has emerged, referred to as Multisystem Inflammatory Syndrome in Children (MIS-C). Since its discovery in 2020, the scientific community has learned a lot about the presentation, evaluation, treatment, and management of MIS-C.
Introduction
The novel SARS-CoV-2 virus has affected children and adolescents throughout the world since its discovery in 2019. For many children, infection with SARS-CoV-2 presents as an asymptomatic to mild infection.1 However, in a small subset of children who become infected with the SARS-CoV-2 virus, a more severe postinfectious inflammatory illness has emerged, called Multisystem Inflammatory Syndrome in Children (MIS-C). The Center for Disease Control (CDC) defines MIS-C as an illness in a pediatric patient less than 21 years of age that presents with a documented or subjective fever >38°C for ≥24 hours with laboratory evidence of inflammation and multisystem involvement (>2 organ systems), severe illness requiring hospitalization, no alternative diagnosis, and either a recent or current SARS-CoV-2 infection.2 MIS-C is defined by the World Health Organization (WHO) as an illness in a pediatric patient age 0 to 19 years old, with a fever for ≥ 3 days, with at least two clinical signs of multisystem involvement, elevated markers of inflammation, with no other obvious microbial cause of inflammation, and evidence of a SARS-CoV-2 infection3 (Table 1 ).
Table 1.
CDC Classification and WHO Classification Criteria for MIS-C
| CDC Definition of MIS-C |
WHO Definition of MIS-C |
||
|---|---|---|---|
| ALL 4 CRITERIA MUST BE MET: | ALL 6 CRITERIA MUST BE MET: | ||
| 1. Age | < 21 years of age | 1. Age | <19 years of age |
| 2A. Fever Criteria | Documented fever >38°C for ≥24 hours OR subjective fever ≥24 hours | 2. Fever Criteria | Fever for ≥ 3 days |
| 2B. Laboratory Evidence of Elevated Markers of Inflammation | Including but not limited to: • Elevated CRP • Elevated ESR • Elevated procalcitonin • Elevated fibrinogen • Elevated D-dimer • Elevated LDH • Elevated IL-6 level • Lymphocytopenia • Neutrophilia • Hypoalbuminemia |
3. Elevated Markers of Inflammation | • Elevated CRP • Elevated ESR • Elevated procalcitonin |
| 2C. Multisystem Involvement | Two or more organ systems involved: • Cardiovascular -Shock - Elevated troponin -Elevated BNP -Abnormal ECHO -Arrythmia • Dermatologic -Other rash -Erythroderma -Mucositis • Gastrointestinal -Abdominal pain -Vomiting -Diarrhea -GI bleed -Ileus -Elevated liver enzymes • Hematologic -Coagulopathy • Respiratory -Pneumonia -PE -ARDS • Renal -AKI -Renal failure |
4. Clinical signs of Multisystem Involvement | Two or more of the following: • Rash, bilateral non-purulent conjunctivitis or mucocutaneous inflammation (oral, hands or feet) • Hypotension or shock • Cardiac dysfunction, pericarditis, valvulitis or coronary abnormalities (including ECHO findings or elevated troponin/BNP) • Evidence of coagulopathy (example: abnormal PT, abnormal PTT, elevated D-dimer) • Acute gastrointestinal symptoms (diarrhea, vomiting or abdominal pain) |
| 2D. Severe Illness | • Severe illness requiring hospitalization | ||
| 3. Recent SARS-CoV-2Infection | • Any of the following: -Positive PCR test -Positive antigen test -Positive serology -Exposure to COVID-19 within 4 weeks of symptom onset |
5. Evidence of SARS-CoV-2 Infection | • Any of the following: -Positive PCR test -Positive antigen test -Positive serology -Contact with an individual with COVID-19 infection |
| 4. No alternative plausible diagnosis | 6. No other obvious microbial cause of inflammation (including bacterial sepsis and TSS) | ||
ECHO= echocardiogram
PE= pulmonary embolism
BNP= brain natriuretic peptide
LDH= lactate dehydrogenase
ARDS= acute respiratory distress syndrome
AKI= acute kidney injury
GI= gastrointestinal
PCR= polymerase chain reaction
PT= prothrombin time
PTT= partial prothrombin time
TSS= Toxic Shock Syndrome
Pathophyisiology
The pathophysiology of MIS-C is not yet well understood. The current theory behind the pathophysiology concludes that MIS-C is likely caused by an abnormal immune response to the SARS-CoV-2 virus. Other possibilities include macrophage activation syndrome (MAS) and cytokine release syndrome.4 Although MIS-C may mimic Kawasaki disease, it does appear to have a different immunophenotype. Of note,
most children that are diagnosed with MIS-C have a negative PCR for SARS-CoV-2
Alt-text: Unlabelled box
(indicating an active infection is not likely).4 Most affected children have positive serologies for SARS-CoV-2 antibodies, a finding that further supports the hypothesis that MIS-C is related to immune dysregulation that appears after an acute infection.4 MIS-C most commonly presents approximately 3-4 weeks after the initial SARS-CoV-2 infection.1
Evaluation
Prompt evaluation is recommended if MIS-C is suspected in a pediatric patient. The diagnostic testing required for MIS-C varies, but typically includes laboratory testing, radiographic imaging, and other diagnostic testing. A tiered diagnostic approach to testing is recommended for children without life threatening manifestations.5 Initial work up for patients with non-life-threatening symptoms includes complete blood count (CBC) with differential, comprehensive metabolic panel (CMP), erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), SARS-CoV-2 testing (PCR and/or serology).5 If the initial tier of testing confirms suspicions for MIS-C, further diagnostic and laboratory testing is indicated.5 An electrocardiogram (EKG) and echocardiogram (ECHO) should be performed as part of the work up for a patient with suspected or confirmed MIS-C.5 Cardiac laboratory testing may include troponin T and B-type natriuretic peptide (BNP)/N-terminal proBNP.5 D-dimer level, ferritin level, procalcitonin level and LDH level may also be indicated.5 A chest radiograph and consultation with pediatric infectious disease, pediatric cardiology and rheumatology are recommended.4 Most case reports and retrospective case studies indicate that blood cultures were obtained during the initial evaluation because patients with severe forms of MIS-C present with the signs and symptoms that mimic septic shock or toxic shock syndrome.4
Presentation of MIS-C
Clinical findings in MIS-C vary amongst pediatric patients. A recent meta-analysis of 39 papers on MIS-C published from January 2020 through July 2020 revealed that
fever, abdominal pain, diarrhea, and vomiting were the most common symptoms in patients diagnosed with MIS-C.1
Alt-text: Unlabelled box
Conjunctivitis and rash were also frequently observed in the patients.1
In the meta-analysis,
approximately 60% of patients that were diagnosed with MIS-C presented with shock.1
Alt-text: Unlabelled box
Cardiac involvement is prominent in children diagnosed with MIS-C.5 Left ventricular dysfunction, coronary artery dilatation or coronary artery aneurysm and conduction abnormalities have been reported in every retrospective cohort study examined by the American College of Rheumatology.5 Valvular dysfunction and pericardial effusions were reported less frequently.5 In one case series, 22% to 64% of children diagnosed with MIS-C met criteria for Kawasaki Disease, and 51% to 90% presented with myocardial dysfunction (diagnosed by ECHO, elevated troponin or elevated BNP).4
Additionally, 24% to 57% of patients presented with serositis (pleural, pericardial and ascitic effusions), and 28% to 52% of presented with acute kidney injury.4
Children with MIS-C demonstrate significant laboratory abnormalities. Many children with MIS-C were found to have significantly elevated cardiac markers including troponin and brain natriuretic peptide (BNP).1 Abnormal coagulation laboratory results included elevated D-dimer, fibrinogen and erythrocyte sedimentation rate (ESR).1 An increased risk of thrombosis also remains a concern for patients diagnosed with MIS-C.5
C-reactive protein (CRP), ferritin, and procalcitonin were significantly elevated in patients with MIS-C.1 When compared with a COVID-19 infection, patients with MIS-C had an 18-fold higher ferritin level and a significantly higher procalcitonin level.1 Fibrinogen, D-dimer and IL-6 were also elevated.5
Patients with MIS-C presented with elevated white blood cell count with elevated mean neutrophil count and low mean lymphocyte count.1 Patients with MIS-C had other notable laboratory abnormalities including hypoalbuminemia, and slightly elevated alanine transaminase (ALT) and aspartate aminotransferase (AST).4
Of note, children that presented with more severe illness (who developed shock and other severe symptoms) were found to have higher CRP values, lower lymphocyte counts and lower serum albumin4
Alt-text: Unlabelled box
(Table 2 ).
Table 2.
Common Laboratory Trends In Pediatric Patients With MIS-C.
| • Leukocytosis |
| -Neutrophilia |
| -Lymphocytopenia |
| • Elevated Procalcitonin |
| • Elevated Ferritin |
| • Elevated CRP |
| • Elevated Troponin |
| • Elevated BNP |
| • Elevated D-Dimer |
| • Elevated Fibrinogen |
| • Elevated ESR |
| • Hypoalbuminemia |
| • Elevated AST and ALT |
The differentiation between severe acute COVID-19 infection and MIS-C can be difficult to detect because they have overlapping features.4 Most children with severe COVID-19 had significant pulmonary disease without cardiovascular involvement.4 On the other hand, children with MIS-C present more commonly with cardiovascular, gastrointestinal and mucocutaneous involvement.4 When comparing laboratory test results, patients with MIS-C were more likely to have thrombocytopenia, lymphopenia and a significantly elevated CRP when compared to patients with severe COVID-19 infections.4
Spectrum & Subtypes of MIS-C
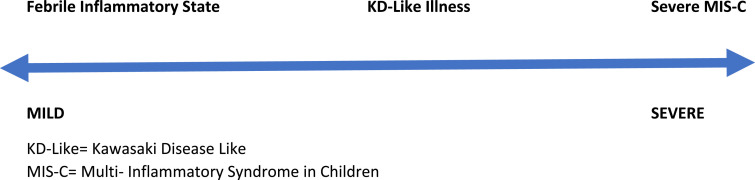
A spectrum of severity for the diagnosis of MIS-C has been created to categorize the variation in presentation. On the less severe end of the spectrum is “Febrile MIS-C” which is described as a child with persistent fevers, mild symptoms (i.e. headache, fatigue), and elevated inflammatory markers without signs of severe multisystem involvement.4 “Kawasaki-Like” MIS-C is described as a child that meets criteria for complete or incomplete KD but does not have signs of severe multisystem involvement or shock.4 Severe MIS-C is described as a child with markedly elevated inflammatory markers and severe multisystem involvement.4 In severe MIS-C cases, cardiac involvement and shock are common4 (Fig. 1 ).
Fig. 1.
Severity Spectrum of MIS-C.
In a recent study conducted on 570 patients with a diagnosis of MIS-C reported through July 2020 to the CDC, the investigators used latent class analysis to identify three different subtypes of MIS-C and were able to compare and contrast aspects of each subtype4 (Table 3 ).
Table 3.
Current Subtypes of MIS-C.
| Percentage of Cohort | Patient Demographics | Symptoms/Signs | SARS-CoV-2 Serology | |
|---|---|---|---|---|
| MIS-C without KD | 35% |
|
|
|
| MIS-C Overlapping with Severe Acute COVID-19 | 30% |
|
|
|
| MIS-C Overlapping with KD | 35% |
|
|
|
MIS-C, Multi-Inflammatory Syndrome in Children; KD, Kawasaki Like Disease; PCR, polymerase chain reaction; CRP, c-reactive protein.
Distinction between MIS-C's Kawasaki-like disease (MIS-C KLD) presentation and Kawasaki Disease (KD) has proven difficult, although specific trends have enabled differentiation among patients that present with similar symptoms.4 One key distinction between MIS-C's KLD and KD is that MIS-C KLD typically affects older children and adolescents, whereas classic KD typically affects infants and young children.4 In addition, gastrointestinal complaints, shock, and myocardial dysfunction are more common in MIS-C KLD than KD.4 When comparing laboratory testing, the inflammatory markers are more elevated in MIS-C KLD when compared with KD (most notably c- reactive protein (CRP), ferritin and D-dimer) and the absolute lymphocyte count and platelets tend to be lower in MIS-C KLD when compared to KD.4
Based on current data, the risk of developing MIS-C appears to vary by both race and gender. Males appear to be more at risk than females, and patients of African American/Afro-Caribbean descent are at greater risk for developing MIS-C.1
Treatment
Although the treatment for MIS-C is not standardized in the U.S. at this time, many pediatric hospitals have been utilizing similar treatment regimens and protocols to treat children with MIS-C. Initial stabilization and treatment of patients with presumed or confirmed MIS-C that present with hyperinflammatory shock or other severe clinical symptoms involves hospital admission with a possible need for admission to an intensive care unit.1 Vasopressor administration, ventilator support, and/or extracorporeal membrane oxygenation (ECMO) may be indicated.1 Admission to the hospital for monitoring of inflammatory markers, cardiac markers and supportive care are recommended.5
Supportive care for children admitted with MIS-C is based on severity of symptoms. Those presenting with shock often require ionotropic support with vasopressors like epinephrine, norepinephrine, dopamine, dobutamine and milrinone.6 The use of extracorporeal membrane oxygenation varies among patients with severe MIS-C.6 Patients with MIS-C require varying levels of respiratory support including non-invasive and invasive mechanical ventilation.1 Fluid resuscitation is commonly necessary for patients admitted with MIS-C.1
The American College of Rheumatology has published recommendations regarding the treatment of MIS-C that includes a stepwise approach to immunomodulatory therapy.5
Both glucocorticoids and intravenous immunoglobulin (IVIG) are considered the most common first line treatment modalities for immunomodulatory treatment in MIS-C.5 Although there is minimal research on the efficacy of IVIG and glucocorticoids in combination when compared with IVIG or glucocorticoids alone, a recent retrospective cohort study found that the combination of IVIG with glucocorticoids demonstrated a more favorable fever course than IVIG alone.7 Respondents in a recent international survey reported steroid use most often in patients with severe clinical presentation (64%).6
IL-1 & IL-6 inhibitors can be used in MIS-C patients that are refractory to IVIG and/or glucocorticoids.5 Anakinra, a recombinant human IL-1 receptor antagonist, is often administered, especially in particularly severe or refractory cases of MIS-C.6
Anti-coagulation has been utilized in the treatment of MIS-C due to the concern for hypercoagulability.5 Antiplatelet agents such as low dose aspirin are recommended for MIS-C patients with Kawasaki Disease-like features, coronary artery aneurysms and thrombocytosis.5 In children with higher coronary artery Z-scores or moderate-to-severe left ventricular dysfunction, the use of anticoagulation agents like enoxaparin or warfarin is advised.5
Antimicrobial therapy with broad spectrum antibiotics is indicated for patients that present with septic shock or toxic shock syndrome while blood culture results are pending.8 An appropriate empiric regimen consists of ceftriaxone plus vancomycin or for an alternative regimen, ceftaroline plus piperacillin-tazobactam.8 Clindamycin can be added if the clinical presentation is consistent with a toxin-mediated process.8
Antiviral therapies (like remdesivir) have not been well studied in the management of MIS-C.8
Future Directions
Follow up and long-term monitoring for children with MIS-C has not been standardized to date. Overall, most children will survive MIS-C.1 However, many pediatric hospitals are currently studying the short- and long-term outcomes for children with this condition.1 Future research is needed to assess both the short- and long-term effects and outcomes on the pediatric population and to standardize the treatment for Multisystem Inflammatory Syndrome in Children.
More research is also necessary to assess the full scope of the different subtypes and the spectrum of illness related to MIS-C.
Footnotes
Dr. Matic has no competing interests to disclose.
References
- 1.Ahmed M, Advani S, Moreira A, Zoretic S, Martinez J, et al. Multisystem inflammtory syndrome in children: a systemic review. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention. Multisystem Inflammatory Syndrome (MIS-C). Center for Disease Control and Prevention (cdc.gov). 2021. Available at: https://www.cdc.gov/mis-c/hcp/.
- 3.World Health Organization. Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19. World Health Organization (www.WHO.int). 2021. Available at: https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19.
- 4.Son MBF, Friedman K. COVID-19: Multisystem inflammatory syndrome in children (MIS-C) clinical features, evaluation, and diagnosis. UpToDate. 2021 Available at: https://www.uptodate.com/contents/covid-19-multisystem-inflammatory-syndrome-in-children-mis-c-clinical-features-evaluation-and-diagnosis?search=misc&source=search_result&selectedTitle=2~80&usage_type=default&display_rank=2#H2726712857. [Google Scholar]
- 5.Henderson LA, Canna SW, Friedman KG, Gorelik M, et al. American College of Rheumatology Clinical Guidance for Multisystem Inflammatory Syndrome in Children Associated with SARS-COV-2 and Hyperinflammation in Pediatric COVID-19: Version 1. Am College Rheumatol. 2020;73(4):e13–e29. doi: 10.1002/art.41616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elias MD, McCrindle BW, Larios G, et al. Management of multisystem inflammatory sydrome in children associated with COVID-19: a survey from the International Kawaski Disease Registry. CJC Open. 2020;2(6):632–640. doi: 10.1016/j.cjco.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ouldali N, Toubiana J, Antona D, et al. Association of Intravenous immunoglobulins plus methylprednisolone vs. immunoglobulins alone with course of fever in multisystem inflammatory syndrome in children. J Am Med Assoc (JAMA) 2021;325(9):855–864. doi: 10.1001/jama.2021.0694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Son MBF, Friedman K. Coronavirus disease 2019 (COVID-19): Multisystem inflammatory syndrome in children (MIS-C) management and outcome. UpToDate. 2021 https://www.uptodate.com/contents/covid-19-multisystem-inflammatory-syndrome-in-children-mis-c-management-and-outcome?search=misc&source=search_result&selectedTitle=1~50&usage_type=default&display_ rank=1 Available at. [Google Scholar]