Abstract
There is a recognized need to better understand “essential ingredients” of psychological treatments, and refine interventions to be more scalable and sustainable. The goal of the present study was to look within a specific modular, flexible, multi-problem transdiagnostic psychological intervention –the Common Elements Treatment Approach (CETA) - and examine questions that would lead to optimizing CETA for scale up and sustainment. Utilizing data from two trials of CETA in two different countries (Thailand and Iraq), this manuscript aims to: 1) determine the “active treatment dose” or how many sessions are needed to achieve clinically meaningful change overall, in CETA); and 2) test how trajectories of client symptom change varied based on client characteristics and/or on delivery of certain elements. Results showed that overall 50% of CETA clients show some improvement after 4–6 sessions (1 SD) and large improvement (2 SD) after 7–10 sessions. Trajectories of change show steady symptom decline over time. Results support gradual exposure as one of the “active ingredients”. Findings suggest that modular, flexible transdiagnostic models may allow for more efficient, targeted treatment as we gain more knowledge about key ingredients, their timing within treatment, and client outcomes.
Keywords: Transdiagnostic, Cognitive behavioral therapy, Low and middle income countries, Low resource settings, PTSD, Dismantling
1. Introduction
The estimated global burden of mental illness accounts for 32.4% of years lived with disability (YLDs) and 13.0% of disability-adjusted life-years (DALYs), which is even higher than earlier estimates suggesting 21.2% of YLDs and 7.1% of DALYs (Vigo, Thornicroft, & Atun, 2016). Over the past decade, there has been a rapidly growing body of research supporting the effectiveness of psychological treatments that address common mental health problems in low and middle income countries (LMIC) (e.g., Bass et al., 2013; Bolton et al., 2007, 2003; Murray et al., 2015; Murray et al., 2018; Papas et al., 2011; Patel et al., 2010; Rahman, Malik, Sikander, Roberts, & Creed, 2008; Weiss et al., 2015). Research from randomized controlled trials (RCT) demonstrate that certain mental health treatments are effective, acceptable, feasible and can be implemented in LMIC using a task-sharing approach, in which lay workers with limited formal mental health training function as counselors (van Ginneken, Tharyan, Lewin, Rao, Meera, Pian, Chandrashekar, 2013). Despite this progress, the treatment gap between those with mental health need and those who receive care remains substantial due to significant challenges with scale-up and sustainability of these interventions (Patel et al., 2016; Thornicroft et al., 2017).
One substantial barrier to scale-up and sustainability is reliance on “focal treatments”, that primarily target one disorder or mental health problem. Some focal treatments tested in LMIC include: (1) depression-focused: Interpersonal Psychotherapy (IPT), Behavioral Activation (BA), Thinking Healthy Program (THP), (Bolton et al., 2007; Bolton et al., 2003; Bolton, Bass, et al., 2014; Rahman et al., 2008); (2) trauma exposure sequelae: Narrative Exposure Therapy (NET, kidNET), Cognitive Processing Therapy (CPT; CPT-C), and Trauma-Focused Cognitive Behavioral Therapy for youth (TF-CBT) (Bass et al., 2013; Murray et al., 2015; Neuner et al., 2008; Neuner, Schauer, Klaschik, Karunakara, & Elbert, 2004; O’Callaghan, McMullen, Shannon, Rafferty, & Black, 2013; Ruf et al., 2010; Weiss et al., 2015), and (3) substance use-focused Cognitive Behavioral Therapy (Papas et al., 2011).
More recently, transdiagnostic psychological treatments have been proposed as a promising novel approach to overcome key challenges inherent in focal treatments (Mansell, Harvey, Watkins, & Shafran, 2009; McHugh, Murray, & Barlow, 2009; Pearl & Norton, 2017). Conceptually, transdiagnostic approaches enable a provider to be trained in one approach that works for multiple common mental health disorders or problems. Potential advantages of transdiagnostic approaches have been detailed elsewhere, but briefly include: a) capitalizing on similarities of symptoms across mental health disorders, as well as the similarities of elements within existing evidence-based treatments (EBTs); b) reducing the number of models in which providers need to be trained (and thus expenses) to treat the most common mental health problems; and c) allowing for, and providing guidance for flexibility based individual client presentation and clinical comorbidity (Chorpita & Daleiden, 2009; Chorpita, Daleiden, & Weisz, 2005b; Chu, Temkin, & Toffey, 2016; Insel, 2009; Mansell, Harvey, Watkins, & Shafran, 2008; Weisz, Krumholz, Santucci, Thomassin, & Ng, 2015; Weisz, Ugueto, Herren, Afienko, & Rutt, 2011). This last advantage is related to a specific type of transdiagnostic model known as “modular”. Modular approaches have elements that can be delivered in varying order and dose, and can act alone or in connection with other elements (Boustani, Gellatly, Westman, & Chorpita, 2017; Martin, Murray, Darnell, & Dorsey, 2018). The Common Elements Treatment Approach (CETA) is a modular, flexible, multi-problem transdiagnostic treatment developed specifically for LMIC and delivery by lay providers (Murray et al., 2014). Results from four completed studies indicates strong effectiveness for a range of problems (trauma, depression, anxiety, substance use, interpersonal violence, aggression) and the ability of lay providers to learn decision-making through the Apprenticeship model(Murray et al., 2011) (see Methods below for additional details) (Bolton, Lee, et al., 2014; Murray & Kane, 2018; Murray et al., 2018; Weiss et al., 2015).
Even with transdiagnostic models, there is a need to better understand how these psychological treatments work, and refine interventions that are more readily disseminated, implemented and potentially scalable and sustainable. This is not a new idea within the field of mental health – but a consistent call since the early 2000s (Kazdin, 2005, 2007, 2009; Murphy, Cooper, Hollon, & Fairburn, 2009; Weersing & Weisz, 2002). More recently, the U.S. Institute of Medicine again urged scientists to identify the key elements of psychosocial interventions that drive an intervention’s effect (Institute of Medicine, 2015). Despite this, the research on psychological treatments in LMIC over the past decade has largely relied on a pre/post-treatment design and/or follow-up assessments at fixed intervals, which has been noted as a barrier to moving the field forward on mechanism identification (Kazdin & Nock, 2003). As such, the global mental health field has answered important questions about “if” treatment packages work and, to a lesser extent, for whom it works in LMIC. Yet, very little is known about which elements within treatments are most associated with symptom improvement, required dose for any treatment or element within a treatment, and essential versus non-essential elements of multi-element treatments. Progress towards understanding “essential ingredients” within psychological treatments could lead to further refinement of existing treatments to aid in efficiency for greater public health impact (Hayes, Hope, & Hayes, 2007; Huebner & Tonigan, 2007). By understanding more about which elements help reduce symptoms, treatments could be optimized by: 1) a more focused use of elements, specific combinations of elements, and/or guidance on appropriate dosing ranges, 2) a reduction in the proliferation of manuals, which in turn would reduce the time and money to evaluate multiple new interventions, and 3) a reduction in time/resources required for training and supervision, if fewer elements are necessary for symptom reduction (e.g., 3–4 vs. 9 or more). Given the low-resource environments of LMIC and lay counselors’ lack of prior training and practice in providing mental health services, it is perhaps even more critical to delineate essential elements and streamline treatments to move to scale-up and sustainability quicker. This can help lessen the learning curve for lay counselors, possibly in preparation for more independence and complex treatment protocols in the future.
Various methods have been used to try to identify essential or “key” elements in psychological treatments delivered in high income country (HIC) settings including dismantling studies, meta-analyses, longitudinal methods to study individual trajectories over time, network analysis, and the identification of discontinuities and nonlinear patterns of change (e.g., sudden gains) (Laurenceau, Hayes, & Feldman, 2007; Singla, Hollon, Fairburn, Dimidjian, & Patel, 2019; Tang, Beberman, DeRubeis, & Pham, 2005). For example, a dismantling study was done by Cunningham and colleagues (Cunningham, Murphy, & Hendershot, 2015) on The Check Your Drinking intervention (CYD; www.CheckYourDrinking.net) which is a personalized feedback intervention for hazardous alcohol use. Results suggested that the personalized feedback element is the active component of the intervention compared to normative feedback (Ale, McCarthy, Rothschild, & Whiteside, 2015). utilized meta-analyses to examine treatment elements related to outcome across 35 RCTs for childhood anxiety disorders (CADs) and eight RCTs for childhood obsessive compulsive disorder (OCD). Results showed that introducing anxiety management elements (e.g., emotion identification, relaxation training, cognitive strategies) before beginning exposure did not improve outcomes. In contrast, this analysis indicated that use of more exposure earlier, with less relaxation (i.e., Exposure and Response Prevention for Obsessive Compulsive Disorder) was effective. Whiteside et al. (2015) found a similar outcome in their dismantling study of their intervention for CADs, emphasizing exposure earlier in treatment maintained its superiority while requiring fewer sessions. Pompoli et al. (2018) utilized a novel component network meta-analysis (NMA) to disentangle the effects of multiple components found in CBT for Panic disorder. The NMA led to similar conclusions as the CAD studies, that CBT approaches should include exposure (face-to-face and interoceptive), while excluding muscle relaxation and virtual-reality exposure. Others researchers have attempted to identify key elements by mapping out discontinuities and nonlinear change over time (Hayes, Laurenceau, Feldman, Strauss, & Cardaciotto, 2007; Kelly, Rizvi, Monson, & Resick, 2009), using approaches such as sudden gains analysis. For example, Tang and DeRubeis (Tang & DeRubeis, 1999) documented a nonlinear treatment course for a sizeable percentage of treatment responders, that is, occurrences of large sudden improvements from one session to the next within CBT for depression, which has been labeled a “sudden gain,” defined as a dramatic and stable reduction in symptom intensity that occurs over a short period of time. Sudden gains have been operationalized in a variety of ways, but one example is Singla et al. (Singla et al., 2019), who operationalized sudden gains as a decrease of a specified amount on an outcome measure from one clinical session to the next clinical session, a relative decrease of 25% of session-wise scores over two or three sessions, and no increase in outcome scores at sessions post sudden gain decrease.
CETA is well-suited for examining how elements affect symptoms due to its effectiveness across a wide range of common mental health problems through one approach. The goal of the present study was to look within a specific modular, flexible, multi-problem transdiagnostic psychological intervention (CETA) and examine questions that would lead to optimizing CETA for scale up and sustainment. Specifically, we examined how individual clients’ symptoms changed over time during receipt of a CETA, and the relative effectiveness of different elements included in CETA. We aimed to 1) determine the “active treatment dose” or how many sessions are needed to achieve clinically meaningful change overall in CETA); and 2) test how trajectories of client symptom change varied based on client characteristics and/or on delivery of certain elements. We used data from two trials of CETA in two different LMIC, Thailand and Iraq.
2. Methods
2.1. Intervention
Building on work by Chorpita & Weisz in HIC (Chorpita & Daleiden, 2009; Chorpita, Daleiden, & Weisz, 2005a; Weisz et al., 2012), our research group developed CETA as a common elements, modular, flexible, multi-problem approach (Murray et al., 2014) (for definitions and differentiation across trandiagnostic treatments, see Sauer-Zavala et al. (2017) and Boustani et al. (2017). To date, CETA includes 8 elements (see Table 1) that can be combined in different ways to address primary presenting problems. CETA has demonstrated strong effectiveness in multiple randomized RCTs in LMIC, and uniquely addresses a wide range of problems including depression, anxiety, trauma, relationship problems, violence, substance use (Bolton, Lee, et al., 2014; Kane et al., 2017; Murray & Kane, 2018; Weiss et al., 2015), and in an open trial, behavioral problems for youth (Murray et al., 2018). In a trial in Southern Iraq with adult survivors of systematic violence (including torture), CETA demonstrated large effect sizes for trauma (d = 2.40), anxiety, (d = 1.60), depression (d = 1.82), and dysfunction (d = 0.88) relative to waitlist control (WLC) (N = 149; Weiss et al., 2015). In a trial with trauma-exposed Burmese refugees in Thailand (N = 347), CETA demonstrated large effect sizes for PTS (d = 1.19), depression (d = 1.16), and anxiety (d = 0.79), with more moderate effect sizes for dysfunction (d = 0.63) relative to WLC (Bolton et al., 2014). In a non-randomized evaluation of CETA-Youth with displaced Somali children in refugee camps in Ethiopia, participants reported significant decreases in symptoms of internalizing (d = 1.37), externalizing (d = 0.85), and PTS (d = 1.71), as well as improvements in well-being (d = 0.75) (Murray et al., 2018; Murray and Kane, 2018). A recently completed trial of CETA in Zambia also showed strong effectiveness for reduction in violence and substance use (Murray and Kane, 2018).
Table 1.
Elements of CETA.
| Element | Simplified Name (Used in training) | Description |
|---|---|---|
| Psychoeducation and Engagement | Introduction and Encouraging | • Focus on obstacles to engagement |
| Participation | • Linking program to assisting with client’s problems | |
| • Includes family when appropriate | ||
| • Program information (duration, content, expectations) | ||
| • Normalization/validation of current symptoms/problems | ||
| Anxiety management strategies | Relaxation | Strategies to improve physiological stress |
| • Examples include: deep breathing, meditation, muscle relaxation, and imagery. Others added by local cultures. | ||
| Behavioral Activation | Getting Active (GA) | • Identifying and engaging in pleasurable, mood-boosting, or efficacy-increasing activities |
| Cognitive Coping/Restructuring | Thinking in a Different Way – Part I and Part II (TDW1 and TDW2) | • Understand association between thoughts, feelings, and behavior • Learn to restructure thinking to be more accurate and/or helpful |
| Imaginal Gradual Exposure | Talking about Trauma Memories (TDM) | • Facing feared and avoided memories in detail • Gradual desensitization/exposure |
| Problem Solving* | Problem Solving | • Step-by-step guidance on basic problem solving |
| Suicide/Homicide/Danger Assessment and Planning | Safety | • Assessing client risk for suicide, homicide, and domestic violence |
| • Developing a focused plan with the client and client’s family (when appropriate) | ||
| • Additional referral/reporting when needed | ||
| CBT for Substance Use and Relapse Prevention** | Substance Use Element (SU) | • Utilizes concepts of Motivational Interviewing to get client buy-in to change substance use/abuse behavior. |
Problem Solving was used only in Thailand.
CBT for substance use was added after these trials (not trails), and evaluated in Ukraine and Zambia
CETA training follows the Apprenticeship model or 10 day live training, practice groups run by local supervisors, very close supervision while providing CETA to a counselor’s first client, and weekly, ongoing supervision throughout CETA provision. CETA training also includes building skills in decision making via client vignette exercises and group discussion with trainer feedback around: a) what elements are appropriate for specific client presentations, b) the order of elements, c) the “dose” or number of sessions dedicated to each element, and d) how to use client’s in session and out of session practice to determine that the client has acquired requisite skills in each element (e.g., if the client does not complete homework or the homework suggests some skill deficits, more session time is dedicated to supporting the client in achieving the ability to independently use skills) (see (Murray et al., 2011) or more information on the vignette-based training activity). In the first two CETA RCTs, a “base flow” of trauma-focus was used as the starting point, given that the study designs had trauma exposure as inclusion criteria. CETA elements for the trauma “base flow” ordering are: Psychoeducation/Engagement, Cognitive Coping, Exposure, Cognitive Restructuring and Finishing Steps – with Safety utilized as needed throughout. In the two trials used, providers were taught to use three “data points” to decide any modifications to the trauma-flow including: a) client responses on the clinical assessment before starting treatment, b) what the client says and does in session, and c) consultation with a supervisor. During the training process, CETA providers practiced utilizing different data in the form of mini case vignettes to create various flows of CETA elements. In both studies, the local provider and supervisor would suggest a flow that needed to be agreed upon with a CETA trainer, who supported the local supervisor through weekly internet-based phone calls.
CETA is inherently flexible, in that if a provider needed additional time to complete the goals of an element, ensure a client could use a skill independently (typically demonstrated by review of client homework) or if the client presented with different symptoms that warranted a new/different element, the flow could be adjusted. For example, if a client, who was receiving a trauma-flow of elements, stated that they felt very depressed and had trouble getting out of bed, the element of Behavioral Activation could be inserted into the trauma flow to address these symptoms. In both RCTs, any adjustments were collective decisions by the provider, supervisor and trainer. This supervision structure also includes procedures designed to support CETA adherence and competency in providers in delivery of the elements. First, each element includes clear steps to follow (part of the CETA manual). Second, providers role played upcoming elements before delivering them, and received peer provider and supervisor feedback. Third, providers objectively report on their delivery of elements, providing a verbal narrative of their session. If any element (or certain steps within an element) was not delivered in a way the supervisor and trainer felt was adequate, the provider was asked to re-do that element or specific steps.
2.2. Data source
Data were from participants enrolled in two RCTs aimed at testing the effectiveness of CETA for mental health symptoms among violence-and torture-affected populations in Iraq and Thailand (displaced persons from Myanmar)(Bolton, Lee, et al., 2014; Weiss et al., 2015). Participants were enrolled in the RCTs if they had experienced a traumatic event had moderate to severe depression and/or posttraumatic stress symptoms as indicated by locally validated measurement instruments (Haroz et al., 2014; Weiss & Bolton, 2010). In Thailand, potential participants were screened using a modified version of a DSM-IV based algorithm applied to the Harvard Trauma Questionnaire (HTQ) and Hopkins Symptom Checklist for depression (see Bolton et al., 2014 for more details). In Iraq, participants were screened using an adapted version of the HTQ that included original HTQ items plus relevant local symptoms (e.g., feeling that one is being watched). Before the trial, the measure underwent validity testing using a psychiatrist diagnosis as a criterion. A score of 36, which was the value that maximized sensitivity and 1-specificity in validity testing, or higher on the measure was selected as the inclusion cutoff (see Weiss et al., 2015 for more details). Although we did not definitely know whether participants were receiving other treatments within these studies, in both locations the availability of CBT-based mental health services would be very rare if even available.
All participants randomized to CETA in the RCTs completed a weekly self-report measure, the Client Monitoring Form (CMF), at the beginning of each session. The CMF is a tool originally designed to help monitor client progress and guide clinical decisions. It includes 12 items taken from the locally validated assessment instruments (noted above at each site), which were delivered at baseline and post treatment in the RCTs. Items on the CMFs related to symptoms of depression, anxiety, and trauma. In both countries, participants were asked how often in the last week had they experienced each symptom. In Thailand, response options included 0 “None of the time,” 1 “A little of the time,” 2 “Some of the time,” 3 “Most of the time” and 4 “Almost all the time” (possible range (0–48). In Iraq, response options included 0 “Never or no,” 1 “Sometimes,” 2 “Often,” and 3 “Very often” (possible range 0–36). Weekly session scores in each site were calculated by taking the total score across the common 12 items on the CMF.
2.3. Setting
The trial in Thailand took place in the town of Mae Sot in Northwest Thailand among refugees, former political prisoners and migrants who had experienced past trauma when fleeing Myanmar and ongoing stressors related to living illegally in Thailand (Bolton, Lee, et al., 2014). The trial in Iraq was conducted in three rural areas of Southern Iraq – Hilla, Karbala and Najaf – areas that experienced ongoing bombings, political violence and military involvement during the RCT (Weiss et al., 2015).
2.4. Sample
The current analysis included N = 166 participants in Thailand who provided full CMF data (91% of the original CETA sample) and N = 98 participants in Iraq with complete CMF data (99% of original CETA sample). In Thailand, CMF data were analyzed up to 12 sessions because only one participant had CMF data for sessions 13 and 14. In Iraq CMF data were analyzed up to 14 sessions (Table 2).
Table 2.
Demographics and clinical symptoms.
| CETA-Iraq | CETA-Thailand | ||
|---|---|---|---|
| N (%) | N (%) | ||
| Sample Size | 98 | 166 | |
| Sex | Male | 67 (68.4) | 66 (39.8) |
| Female | 31 (31.6) | 100 (60.2) | |
| Marital Status | Not married | 26 (26.5) | 75 (45.2) |
| Married | 72 (73.5) | 89 (53.6) | |
| Missing | 0 | 2 (1.2) | |
| Ethnicity | Burman | - | 111 (66.9) |
| Other | - | 47 (28.3) | |
| Missing | - | 8 (4.8) | |
| Education | None | 15 (15.3) | 10 (6.0) |
| Primary/Middle | 29 (29.6) | 63 (38.0) | |
| school | |||
| High school | 33 (33.7) | 47 (28.3) | |
| More than high school | 21 (21.4) | 46 (27.7) | |
| Mean (SD) range | Mean (SD) range | ||
| Age | 41.9 (11.2) | 36.5 (12.9) | |
| 18-70 | 18-85 | ||
| PTS | 1.28 (0.23) | 1.08 (0.38) | |
| 0.93-2.0 | 0.20-2.24 | ||
| Depression | 1.22 (0.43) | 1.34 (0.41) | |
| 0.45-2.36 | 0.41-2.71 | ||
| Anxiety | 1.32 (0.47) | 1.18 (0.64) | |
| 0.33-2.67 | 0.09-3.46 | ||
| Function | 1.56 (0.6) | 0.97 (0.74) | |
| 0.32-2.81 | 0-3.18 | ||
| Aggression | - | 0.66 (0.39) | |
| 0-1.92 | |||
2.5. Statistical analyses
2.5.1. Aim 1
For Aim 1, determining the active dose of treatment in CETA, we defined clinically meaningful change as a relative measure in our sample – examining how long it took clients to achieve one or two standard deviation(s) in symptom improvement. We used time-to-event analysis (life tables) to calculate the number of sessions it took 25%, 50%, and 75% of clients to achieve one or two standard deviation(s) from baseline in symptom improvement. We chose these cutoffs because we were using a study-developed measure, which did not have established cutoff scores to gauge clinically significant improvement, or test-retest reliability statistics to permit approaches such as the Reliable Change Index. Our relative index of change using SD and percent of clients who improved is conceptually consistent with previous work such as sudden gains analyses in psychotherapy research (Tang & DeRubeis, 1999). For this analysis we explored two sub-populations of clients: all those in treatment with CMF data (n = 166 for Thailand; n = 97 for Iraq), and those who had high enough first-session scores to make a gain of either 1 or 2 SDs (n = 155 & 98, respectively for Thailand, n = 96 & 73, respectively, for Iraq). Clients who ended or dropped out of treatment were censored. We also calculated the percentage of clients that achieved symptom changes of 1 or 2 SDs by the end of treatment.
Sensitivity analyses.
We completed two sensitivity analyses. First, to test the robustness of our findings, we examined the percentage of participants who had scores that worsened while still in treatment after reaching one or two SDs of improvement. Second, during the previous effectiveness studies using this same dataset (see Bolton, Lee, et al., 2014; Weiss et al., 2015), for full details about RCTs) participants in the control groups in each country also improved, possibly due to regression to the mean. We sought to isolate the effect of the intervention on improvement and therefore determine the dose-response relationship above and beyond this naturally occurring improvement. The control groups did not have weekly CMF scores, but did have baseline and follow-up assessment data using the same items as the CMF. Using these scores, we predicted the number of sessions required to achieve improvement while adjusting for the difference between the average improvement slopes (baseline to follow-up) for each condition by country. This approach statistically removed the effects of naturally occurring improvement (i.e. regression to the mean) to estimate a pure treatment effect.
2.5.2. Aim 2
Our examination of how client symptom changed varied based on client characteristics and CETA elements received consisted of several steps. Step 1. Exploratory data analysis we examined trajectories of symptom change based on CMF score using spaghetti and scatter plots. To select our baseline model we explored whether a linear growth model with random intercept, a quadratic growth model with random intercept, or a linear growth model with random intercept and random slope, best fit the data in each site. Step 2. Model fit and selection: Each model was fit with an independent correlation structure, maximum likelihood estimation, and compared using Akaike information criterion (AIC) and Bayesian information criteria (BIC)(Akaike, 1974; Schwarz, 1978). All models also included the random effects of counselor (clients nested within counselor) and client (time pointes nested within individual client). The model with the lowest AIC and BIC was selected as the most appropriate baseline model from which to build.
Step 3. Examination of client characteristics: Using this model building strategy, we next explored the association between baseline client characteristics on symptom trajectories. Based on previous research indicating that sex (Girgus & Yang, 2015; Mirza & Jenkins, 2004), exposure to traumatic events (Alim et al., 2006; O’Donnell, Creamer, & Pattison, 2004), and education (Mirza & Jenkins, 2004; Scarinci et al, 2002) are associated with worse symptoms of depression, anxiety and PTS, we explored whether these variables had an impact on the level of client symptoms and the slope of symptom change. These characteristics were entered into the baseline model independently as covariates and then as an interaction term between covariate and time.
Step 4. Examination of the impact of certain CETA elements: We then investigated the association between treatment element delivery and changes in the trajectory of client symptoms by comparing a series of alternative discontinuous change models for Cognitive Coping, Gradual Exposure, and Cognitive Restructuring. Separate models tested if the addition of the element was associated with a change in client symptom trajectory level, slope, or both. Shift in level is analogous to the “sudden gains” approach, whereby an immediate decrease in average scores for clients occurred after the element was delivered, but differs from some other operationalizing used in research in LIMC countries (e.g. Singla et al., 2019) by being based solely on the statistical significance of average response, and not based on the proportion of individuals who demonstrate a decrease of absolute value, relative change, and subsequent absence of increased scores. Psychoeducation was excluded because it was the first element delivered in all settings and therefore lacked pre-delivery trajectories. Due to prohibitively small samples sizes of individuals who received two elements, we did not explore behavioral activation (n = 28 in Thailand; n = 12 in Iraq) or relaxation (n = 10 in Thailand; n = 26 in Iraq).
Changes in symptom severity and change trajectories (i.e. level, slope, and both level and slope) were estimated using the procedure outlined in Raudenbush & Byrk (Raudenbush & Bryk, 2002). Change in deviance statistics were used to compare the models and select the most appropriate model to reflect discontinuous change in each setting (Singer & Willett, 2003) Change in deviance values were large enough to be considered noteworthy if the value was above 2 indicating positive evidence of model superiority and values above 10 indicating strong evidence (Singer & Willett, 2003).
All elements were treated as fixed effects. Client level covariates found to be statistically significantly related to symptom change trajectories (p < 0.10) were then added to the most appropriate discontinuous change model, resulting in models that explored the impact of each treatment element while adjusting for any measured baseline confounding.
Finally, in order to determine whether any treatment elements had an association with trajectory change above and beyond the other elements, all elements (parameters for both level and slope for each element) were included in a final model with the significant client characteristic baseline covariates. Similar model selection procedures were performed for this analysis to look at the most appropriate discontinuous change model with all time-varying covariates included in the model. All analyses for Aim 1 were done using Stata 13.0 (StataCorp, 2013).
Sensitivity analysis.
Based on the exploratory analysis, client symptom change trajectories for select counselors (n = 6) in Thailand suggested unlikely uniformity across clients. All of these counselors’ clients improved at nearly uniform rates (e.g. improving at 2–3 points per session with no worsening), unlike all other counselors who had clients with scores that varied over time (e.g. overall consistent improvement but some sessions revealed worsening). To explore the effects of these counselors on symptom change trajectories we compared coefficients from final models that excluded the client data from these counselors to models that included this client data.
3. Results
3.1. Aim 1
Baseline (first session) CMF scores averaged 16.2 (SD = 6.8, range = 0–39) in Thailand and 15.8 in Iraq (SD = 5.8, range = 5–29). Fig. 1 demonstrates the average CMF score at each session. In Thailand, by the end of treatment 138 clients (85.2% of the total sample) improved by 1 SD and 83 (51.2%) improved by 2 SD. Seven clients (4.2%) had baseline scores below 1 SD (6.8) and 66 clients (39.8%) had baseline scores below 2 SD (13.6). Therefore, it was impossible for these clients to “improve” below their respective deviations, as operationalized in this study (this challenge is a common limitation in measuring clinical significance (Hansen, Lambert, & Forman, 2002). In Iraq, by the end of treatment 86 (88.7%) improved by 1 SD and 47 (48.5%) improved by 2 SD. One client (1%) had a baseline score below 1 SD (5.8) and 23 (23.7%) were below 2 SD (11.6). Therefore, we ran separate analyses, including all clients and only those with high enough scores as baseline to show improvement.
Fig. 1.
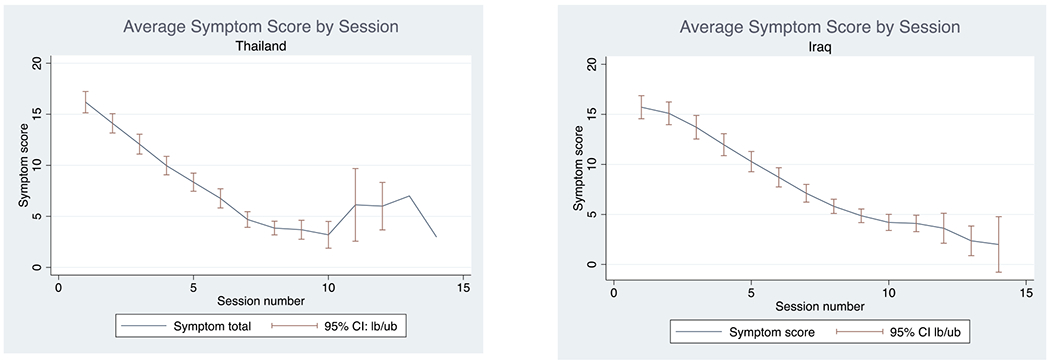
Average symptom score by session in Thailand and Iraq.
Table 3 shows the results of a time-to-event analysis depicting the number of sessions until 25%, 50%, and 75% of clients reached either 1 or 2 SD improvement, censoring cases that left treatment before improving. Results for Thailand found that the median number of sessions to make 1 SD improvement was 4–5, and to make 2 SD was 7–8. In Iraq, the median sessions needed to make a 1 SD improvement was 6 and to make a 2 SD improvement was 8–10.
Table 3.
Number of sessions until improvement or censored.
| Thailand | Improvement | N | 25% | 50% | 75% |
|---|---|---|---|---|---|
| Of all those who remained in treatmenta | 1 SD | 162 | 3 | 5 | 7 |
| 2 SD | 162 | 6 | 8 | - | |
| Of those remaining in treatment and who had high enough first-session scores to make againa | 1 SD | 155 | 3 | 4 | 6 |
| 2 SD | 98 | 5 | 7 | 8 | |
| Iraq | Improvement | Nb | 25% | 50% | 75% |
| Of all those who remained in treatmenta | 1 SD | 97 | 5 | 6 | 7 |
| 2 SD | 97 | 7 | 10 | - | |
| Of those remaining in treatment and who had high enough first-session scores to make a gaina | 1 SD | 96 | 5 | 6 | 7 |
| 2 SD | 73 | 6 | 8 | 13 | |
Survival analysis with right censored cases.
One person removed from analysis due to missing data at baseline.
3.2. Aim 1 sensitivity analyses
In Thailand, of those who improved by 1 SD, 18 (14.1%) had a subsequent CMF score that worsened, but only 3 (2.3%) had a subsequent CMF score that was equivalent to or worse than their first session score. Of those who improved by 2 SD, 13 (19.7%) subsequently had worse scores, but n = 10 of these were essentially plateaus, with changes of 3 points or less, suggestive of statistical noise. In Iraq, of those who made 1 SD improvement, 12 (14.3%) had a subsequent score that worsened, but none had a subsequent score equivalent to or worse than their first session score. Of those with 2 SD improvement, 3 (7.1%) had a subsequent score that worsened, but worsening was small in magnitude (1–2 points), suggestive of statistical noise.
In Thailand, from pre-assessment to follow-up and assuming linear change, the CETA group improved at an average of 1.2 points per week (SD = 0.76). The control group improved at an average of 0.54 points per week (SD = 0.57), which is 45.8% of the rate of the CETA group. In Iraq, the CETA group improved at an average of 0.45 points per week (SD = 0.19), while the control group improved at an average of 0.28 points per week (SD = 0.28) or 62.2% of the rate of the CETA group. After statistically adjusting for differences in slopes between the intervention and control groups to remove the effect of naturally occurring change, the CETA group in Thailand was predicted to require 5.8 to 7.3 sessions to make 1 SD improvement and 10.2 to 11.7 sessions to make 2 SD improvement. The CETA group in Iraq was predicted to require 9.7 sessions to make 1 SD improvement and 13.0 to 16.2 sessions to make 2 SD improvement.
3.3. Aim 2
In Thailand 24% (95% Cl: 0.13, 0.41) of the variance in client change trajectory was at the clinician level; while in Iraq 44% (95% Cl: 0.25, 0.65) was at the clinician level. Model fit statistics identified that the use of linear time trends, random intercepts, and random slopes were most appropriate in the baseline model for representing the effect of time (session) on client symptom change trajectories. The sensitivity analysis found no significant difference in point estimates when removing data from Thailand counselors with questionable client change trajectories.
In Thailand, women had higher symptoms at every timepoint compared to men (β = 1.97, p < 0.001). In Iraq, clients with higher education had lower symptom scores at every timepoint (β = −1.17, p < 0.05). No significant associations were found for trauma exposure in either site. None of the baseline client level characteristics investigated were significantly associated with the rate of change in symptom scores in either site.
Results showed that inclusion of time-varying parameters representing discontinuities in level and slope as random effects were not significant; therefore, these parameters were fixed in all models. Results of baseline linear time trend models indicated that there was consistent improvement in symptoms throughout treatment. In Thailand, the average client improved 1.92 points on the CMF at each session (SE = 0.15); in Iraq, the average client improved 1.53 points per session (SE = 0.15) (Tables 4 and 5).
Table 4.
Comparison of fitting alternative discontinuous change trajectories to client symptom scores in Thailand (N = 166)a.
| β (Robust SE) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model | Intercept | Time | Female | Level | Slope | AIC | BIC | ▵ Deviance |
| Model A | 13.53 (1.03)** | −1.92 (0.15)** | 2.20 (0.52)** | - | - | 7223.2 | 7259.3 | - |
| Cognitive Coping (Model B is best fitting) | ||||||||
| Model B | 13.57 (1.05)** | −2.09 (0.22)** | 2.18 (0.52)** | 1.02 (0.65) | 7215.6 | 7256.9 | 9.6 | |
| Model C | 13.44 (0.84)** | −1.83 (0.36)** | 2.20 (0.52)** | - | −0.34 (0.34) | 7224.4 | 7265.7 | 0.8 |
| Model D | 13.46 (0.85)** | −1.99 (0.29)** | 2.18 (0.52)** | 1.03 (0.69) | −0.36 (0.34) | 7216.7 | 7263.1 | 10.5 |
| Gradual Exposure (Model B is best fitting) | ||||||||
| Model B | 13.30 (0.91)** | −1.75 (0.16)** | 2.19 (0.52)** | −1.14 (1.19) | - | 7212.7 | 7254.0 | 12.5 |
| Model C | 13.38 (0.89)** | −1.82 (0.17)** | 2.19 (0.52)** | - | −0.30 (0.58) | 7221.06 | 7262.4 | 4.1 |
| Model D | 13.32 (0.88)** | −1.76 (0.19)** | 2.19 (0.52)** | −1.25 (0.68) | 0.07 (0.42) | 7214.6 | 7261.0 | 12.6 |
| Cognitive Restructuring (Model D is best fitting) | ||||||||
| Model B | 13.54 (1.00)** | −1.92 (0.14)** | 2.20 (0.51)** | 0.03 (0.58) | - | 7225.2 | 7266.5 | 0.01 |
| Model C | 13.54 (1.00)** | −1.92 (0.14)** | 2.20 (0.51)** | - | 0.07 (0.52) | 7225.1 | 7266.4 | 0.05 |
| Model D | 13.54 (1.00)** | −1.92 (0.14)** | 2.20 (0.51)** | −0.74 (0.75 | 0.75 (0.33)* | 7226.9 | 7273.3 | 0.30 |
p < 0.05.
p < 0.001.
Deviance calculated as -2*loglikelihood/AIC or BIC and compared using chi-squared difference tests with 1 degree of freedom for Models B & C; and 2 degrees of freedom for Model Ds. If no highlight, Model A is considered the best fitting model.
Model A = Baseline model; Model B = Discontinuity in level (not slope); Model C = Discontinuity in slope (not level); Model D = Discontinuity in level and slope.
Table 5.
Comparison of fitting alternative discontinuous change trajectories to client symptom scores in Iraq (N = 98)a.
| β (Robust SE) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Element | Intercept | Time | Female | Level | Slope | AIC | BIC | Δ Deviance |
| Model A | 18.31 (1.61)** | −1.53 (0.15)** | −1.10(0.34)** | - | - | 4881.8 | 4915.8 | - |
| Cognitive Coping (Model A is best fitting) | ||||||||
| Model B | 18.31 (1.60)** | −1.51 (0.14)** | −1.10 (0.43)** | −0.18 (0.44) | - | 4883.5 | 4922.3 | 0.37 |
| Model C | 17.95 (1.34)** | −1.28 (0.26)** | −1.09 (0.34)** | - | −0.33 (0.34) | 4876.8 | 4915.7 | 7.00 |
| Model D | 17.93 (1.32)** | −1.22 (0.25)** | −1.09 (0.34)** | −0.30 (0.43) | −0.35 (0.34) | 4877.8 | 4921.5 | 8.07 |
| Gradual Exposure (Model A is best fitting) | ||||||||
| Model B | 18.06 (1.49)** | −1.39 (0.14)** | −1.10 (0.34)** | −1.01 (0.66) | - | 4871.6 | 4910.51 | 12.19 |
| Model C | 18.28 (1.51)** | −1.52 (0.17)** | −1.10 (0.34)** | - | −0.04 (0.28) | 4883.7 | 4922.58 | 0.12 |
| Model D | 18.18 (1.48)** | −1.43 (0.16)** | −1.10 (0.34)** | −1.43 (0.57)* | 0.28 (0.27) | 4869.3 | 4913.09 | 16.47 |
| Cognitive Restructuring (Model A is best fitting) | ||||||||
| Model B | 18.33 (1.59)** | −1.54 (0.15)** | −1.10 (0.34)** | 0.20 (0.44) | - | 4883.41 | 4922.30 | 0.41 |
| Model C | 18.33 (1.59)** | −1.54 (0.15)** | −1.10 (0.34)** | - | 0.20 (0.44) | 4883.41 | 4922.30 | 0.41 |
| Model D | 16.58 (1.48)** | −1.54 (0.15)** | −1.10 (0.34)** | 0.20 (0.44) | NA | 4883.41 | 4922.30 | 0.41 |
p < 0.05.
p < 0.001.
CC: Model B
GE: Model B
CR: Model D
Deviance calculated as -2*logliklihood/AIC/BIC and compared using chi-squared difference tests with 1 degree of freedom for Models B & C; and 2 degrees of freedom for Model Ds. If no highlight, Model A is considered the best fitting model.
Model A = Baseline model; Model B = Discontinuity in level (not slope); Model C = Discontinuity in slope (not level); Model D = Discontinuity in level and slope.
In both Thailand and Iraq, cognitive coping was not significantly associated with symptom change trajectories. Gradual exposure was associated with symptom change in both settings. In Thailand, gradual exposure was associated with an immediate, although not statistically significant, decrease in symptoms (β = −1.14; p = 0.07) and a slight flattening of improvement trajectory. In Iraq, gradual exposure was significantly associated with an immediate drop in symptoms (β = −1.43, p < 0.05) followed by a slight attenuation of improvement trajectory (Tables 4 and 5).
Cognitive restructuring was related to more rapid symptom decrease in Thailand (β = 0.75), but was not related to change in Iraq. However, cognitive restructuring most often happened late in treatment (commonly delivered by the 6th session in Thailand, and by 10th session in Iraq) and therefore we may have lacked power to detect slope change following completion of the element (Tables 4 and 5).
To determine whether any treatment elements had an impact above and beyond the other elements, we included all elements (parameters for both level and slope) in a single model for each site. In both Thailand and Iraq, completion of gradual exposure resulted in an immediate decrease in symptom levels (Thailand: β = −1.18, p = 0.001; Iraq: β = −1.31, p < 0.05). None of the other elements examined were associated with improvement in symptom level or trajectory when included in a complete model featuring the other elements (Table 6).
Table 6.
Final outcome models with all elements included.
| Thailand (N = 166) | Iraq (N = 98) | |||
|---|---|---|---|---|
| β | Robust SE | β | Robust SE | |
| Intercept | 13.46** | 0.85 | 17.94** | 1.32 |
| Time | −1.99** | 0.29 | −1.21** | 0.24 |
| Gender | 2.18** | 0.52 | - | - |
| Education | - | - | −1.10** | 0.34 |
| Cognitive Coping | ||||
| Level | 0.99 | 0.60 | 0.01 | 0.31 |
| Slope | 0.01 | 0.55 | −0.44 | 0.34 |
| Gradual Exposure | ||||
| Level | −1.18** | 0.37 | −1.31* | 0.59 |
| Slope | 0.19 | 0.34 | 0.59 | 0.36 |
| Cognitive Restructuring | ||||
| Level | −0.44 | 0.50 | −0.32 | 0.41 |
| Slope | 0.66 | 0.60 | Colinear | |
| Variance Elements | ||||
| Level-1: Within-person | 3.86 | 0.24 | 3.10 | 0.37 |
| Level-2: Counselor | 3.55 | 0.79 | 4.33 | 0.88 |
| Goodness-of-fit | ||||
| -2LL | 7189.20 | 4845.174 | ||
| AIC | 7215.20 | 4869.175 | ||
| BIC | 7282.32 | 4927.503 | ||
p < 0.05.
p < 0.001.
4. Discussion
This study is the first, to our knowledge, to explore the essential elements, dose, and trajectories of change within a modular, flexible, multi-problem transdiagnostic treatment implemented by non-professionals in two LMIC settings. Advancements in identifying “key elements” as well as an “active dose” of psychological treatments have great potential to aid scalability and sustainability. In LMIC specifically, the dearth of resources for mental health care necessitate close attention to getting the most out of our treatments in the shortest amount of time. Understanding which elements of an intervention empirically contribute to positive outcomes increases treatment efficiency and potential reach (Abry, Hulleman, & Rimm-Kaufman, 2015; Blase & Fixsen, 2013).
In our examination of “active dose” or how many treatment sessions are needed to achieve clinically meaningful change overall, 50% of CETA clients show some improvement after 4–6 sessions (1 SD) and large improvement (2 SD) after 7–10 sessions. Although we cannot make direct comparisons to clinical trials of psychotherapy in HIC (e.g., differences in symptom presentation cross-culturally, appropriateness/use of western diagnoses), this number of sessions is seemingly shorter than many CBT-based psychotherapies in HIC. In a review of dose-response effects, Hansen and colleagues (Hansen et al., 2002) indicate that in trials of focal disorder treatments, between 57.6% and 67.6% of clients improve by 12.7 sessions of treatment, but that in the United States the average number of sessions receive was less than 5 with only a 20% rate of improvement. Currently, most manualized focal treatments that have been tested in LMIC are designed to have around 12–16 structured sessions and show strong effects (e.g., CPT-C, IPT), which is in line with our calculated predictions of the number of sessions needed for meaningful change for these two trial sites. Our results also suggest that the more severe the symptoms (e.g., Iraq versus Thailand), on average the more sessions needed for meaningful change. For those presenting with common mental health disorders, there may be a cut point for too few sessions to render clinically meaningful change. The lower number of sessions shown for CETA versus focal treatments may also suggest that which elements are provided in early sessions, or how soon treatments deliver potentially key elements, may drive outcomes.
Conversely, the fact that half the clients showed some improvement after only 4–6 sessions is encouraging from a public health standpoint. Modular, flexible transdiagnostic models that allow flexibility in dosing may be advantageous in allowing for brief treatment for those that recover more quickly, and only increasing treatment duration (adding sessions and/or elements) for those with poorer treatment response (Martin et al., 2018). This approach fits with stepped-care models in global public health in which there is a need to improve efficiency in treatment and find lower-cost/resource options that show some improvement (e.g. Glasgow, Klesges, Dzewaltowski, Estabrooks, & Vogt, 2006; Glasgow, Vogt, & Boles, 1999; Murray & Jordans, 2016).
Our trajectories of client symptom change would be described as smoothly decreasing over the course of therapy, which is commonly hypothesized in skills-based interventions (Laurenceau et al, 2007). Research suggests that exposure-based interventions may be expected to have an initial increase in symptoms, or perhaps an increase during the exposure elements before ultimate symptom improvement (i.e., a “S” shaped curve). Although CETA included exposure in both RCTs, we did not see this S curve. One explanation may be that “worsening before improvement” may be contextual in that both settings were wrought with ongoing violence/war or displacement challenges. Another may be that given inherent flexibility in CETA, exposure was started in different sessions for different clients, which may have washed out detecting mean-level differences in symptoms by session number.
Our examination of the impact of individual therapeutic elements in CETA supported gradual exposure as one of the “active ingredients” significantly associated with decreasing client symptoms almost immediately upon completion. Identifying Gradual Exposure as a key ingredient in CETA is consistent with the literature showing effectiveness of exposure therapy for trauma affected populations (Foa, Keane, Friedman, & Cohen, 2009; Pompoli et al., 2018; Watts et al., 2013; Whiteside et al., 2015). Notably, CETA implementation did not consistently include the relaxation element that other dismantling studies have shown to be non-additive, so we were not able to examine this element. We did not find evidence to support the effectiveness of Cognitive Restructuring and Cognitive Coping on their own. While this is inconsistent with literature showing substantial effect sizes for more cognitively focused CBT approaches to treating trauma and related symptoms, (e.g., Bass et al., 2013b) we believe our findings are due to is limited power as there were fewer post-sessions for cognitive processing (as one of the later elements in the base trauma flow) compared to exposure, meaning that those slopes could not be estimated as precisely. A larger study, with manipulation to control for time in treatment, wider variation in delivery timing for each element, or experimental assignment to element ordering would increase our power to detect change and also permit examining whether these elements were effective for certain subsets of clients with specific presenting issues.
This study was able to leverage a routine outcome monitoring clinical tool used to guide delivery of care, the Client Monitoring Form (CMF), to better understand how a treatment was working. This was based on the literature on measurement based care models that suggests this allows for better treatment planning, changes based on emergent needs, and improvement in clinical outcomes (Fortney et al., 2017; Scott & Lewis, 2015) The CMF was developed from a longer instrument, which was locally validated in each site. The CMF is important for multiple reasons including: (1) ability to encourage longitudinal data collection to advance our understanding of core mechanisms in psychological treatments, and (2) in the use of modular, flexible, multi-problem transdiagnostic models wherein clinicians are routinely evaluating symptoms and responding to symptom fluctuation, and comorbidity. In essence, using the clinical CMF as a research tool and our longitudinal modeling of trajectories allowed us to use an embedded quasi-experimental design and interrupted time-series approach, to better understand the impact of each element in CETA on client level outcomes (Penfold & Zhang, 2013). While a limitation is that the CMF was not itself a psychometrically tested instrument in these two trials, our work since this study has included use of Item Response Theory methods to shorten instruments and create reliable, valid and pragmatic CMFs that can serve both clinical and research purposes and replace longer baseline assessments. Using IRT to create a short, validated clinical tool with other treatments would build our greater collective knowledge about individual elements, like exposure, to optimize a broader range of treatments.
This study has a number of limitations. By capitalizing on the flexible, modular, common-elements-based delivery approach, certain confounds may be present. For instance, time in treatment is associated with the delivery of certain elements that nearly always precede the delivery of other elements (e.g. psychoeducation always precedes other elements) and elements that usually do not begin until other elements have been delivered (e.g. exposure in CETA always follows Cognitive Coping. This limits our ability to test for the effects of these elements in isolation, and may have contributed to the fact that we did not identify cognitive restructuring as statistically significant, in contrast with other studies. Similarly, elements such as psychoeducation may be necessary but insufficient, serving as an essential foundation for building to effective treatment but replace itself produce significant symptom reduction. It may be that the lack of methodological control for element delivery resulted in greater or lesser effects attributed to certain elements than would have been found in the absence of other elements. These studies also did not include any measurement of actual skill acquisition by the clients, although this was monitored in supervision. Additional limitations concern measurement. Because no clinical cutoff exists for the weekly measurement score (CMF), we could not incorporate the Reliable Change Index into our analyses, and instead we used cutoffs of 1 and 2 SDs from baseline. Therefore, while this study found the median number of sessions necessary to achieve change of a certain size, we cannot describe the median number of sessions necessary until clients had subclinical symptomatology. Another limitation common to utilizing two trials is that the methods varied slightly (e.g., substance use offered in Thailand and not Iraq), and there are a number of cultural and implementation differences rendering some analyses more difficult. Finally, given enrollment criteria for both studies (based on funding), all participants were trauma-exposed and received elements designated in CETA as essential when clients have trauma exposure and trauma-related symptoms. Current research on CETA has included broader enrollment criteria, resulting in greater variance in element choice, dosing, and order. This variance will allow for better examining of how treatment works based on client differences and how it is delivered.
Although the current literature highlights the need for better understanding of essential elements and sudden gains, there are methodological challenges that would be important to address in the future. Many reviews are unable to draw conclusions due to poor study quality and/or low statistical power (Cuijpers, Cristea, Karyotaki, Reijnders, & Hollon, 2017). Other study designs that could better unpack and disentangle the association between element and effect often are more complex and require larger sample sizes (e.g. Multiphase Optimization Strategy Testing; Sequential Multiple Assignment Randomized Trials) (Collins, Murphy, & Strecher, 2007). Other promising approaches may include micro-randomized trials (Klasnja et al., 2015) and element network meta-analysis (Pompoli et al, 2018). Central to this work is the need for short validated measures (e.g. CMF), that can be used longitudinally and with clinical cutoff indications which could be embedded in large global implementation projects to better inform treatment and understand how people change over the course of treatment. Finally, future work will include use of transdiagnostic approaches when client inclusion criteria are more broad and varied.
In summary, our study showed that individuals with common mental health disorders demonstrated meaningful change in less than 12 sessions, which is the average session length for most manualized focal treatments. This suggests that transdiagnostic models that are specifically modular and flexible (versus a set number of structured sessions for all) may allow for more efficient treatment. Our analyses also showed that for these trauma-affected populations, a key ingredient that reduced symptoms was exposure. This aligns with other research related to anxiety disorders, and suggests that while some feel this ingredient may be more challenging (for either the client and/or counselor) it may be a necessary and efficient method to reduce suffering.
Acknowledgements
The authors would like to thank those that have contributed to the development and refinement of the CETA model including Ms. Lucy Berliner, Dr. John Weisz, Dr. David Barlow and Dr. Richard Spates.
Funding/support
The original trials were supported by USAID, Victims of Support Fund DFD-A-00-08-00308-00. The funding for Emily E. Haroz from the National Insitute of Mental Health (NIMH).
Role of the sponsor
The funder had no role in study design, data collection and analysis, interpretation of data, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest
The authors declare that they have no competing interests.
Additional contributions
None.
References
- Abry T, Hulleman CS, & Rimm-Kaufman SE (2015). Using indices of fidelity to intervention core components to identify Program active ingredients. American Journal of Evaluation, 36(3), 320–338. 10.1177/1098214014557009. [DOI] [Google Scholar]
- Akaike H (1974). A new look at the statistical model identification. IEEE transactions on automatic control 10.1109/TAC.1974.1100705. [DOI] [Google Scholar]
- Ale CM, McCarthy DM, Rothschild LM, & Whiteside SPH (2015). Components of cognitive behavioral therapy related to outcome in childhood anxiety disorders. Clinical Child and Family Psychology Review, 18(3), 240–251. 10.1007/s10567-015-0184-8. [DOI] [PubMed] [Google Scholar]
- Alim TN, Graves E, Mellman T. a, Aigbogun N, Gray E, Lawson W, et al. (2006). Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. Journal of the National Medical Association, 98(10), 1630–1636. 10.1037/t00072-000;M4-Citavi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass JK, Annan J, McIvor Murray S, Kaysen D, Griffiths S, Cetinoglu T, … Bolton P. a. (2013). Controlled trial of psychotherapy for Congolese survivors of sexual violence. New England Journal of Medicine, 368(23), 2182–2191. 10.1056/NEJMoa1211853. [DOI] [PubMed] [Google Scholar]
- Blase K, & Fixsen DL (2013). Core intervention components: Identifying and operationalizing. ASPE Research Brief 10.1177/1049731509335549. [DOI] [Google Scholar]
- Bolton P, Bass J, Betancourt T, Speelman L, Onyango G, Clougherty KF, … Verdeli H (2007). Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: A randomized controlled trial. Journal of the American Medical Association: The Journal of the American Medical Association, 298(5), 519–527. 10.1001/jama.298.5.519. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, … Weissman M (2003). Group interpersonal psychotherapy for depression in rural Uganda: A randomized controlled trial. JAMA: The Journal of the American Medical Association, 289(23), 3117–3124. 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass JK, Zangana GAS, Kamal T, Murray SM, Kaysen D, … Rosenblum M (2014). A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, Northern Iraq. BMC Psychiatry, 14(1), 360. 10.1186/s12888-014-0360-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, Robinson C, … Bass J (2014). A transdiagnostic community-based mental health treatment for comorbid disorders: Development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Medicine, 11(11) 10.1371/journal.pmed.1001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boustani MM, Gellatly R, Westman JG, & Chorpita BF (2017). Advances in cognitive behavioral treatment design: Time for a glossary. The Behavior Therapist, 40(6), 199–208. [Google Scholar]
- Chorpita BF, & Daleiden EL (2009). Mapping evidence-based treatments for children and adolescents: Application of the distillation and matching model to 615 treatments from 322 randomized trials. Journal of Consulting and Clinical Psychology, 77(3), 566–579. 10.1037/a0014565. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, & Weisz JR (2005a). Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Mental Health Services Research, 7(1), 5–20. 10.1007/s11020-005-1962-6. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, & Weisz JR (2005b). Modularity in the design and application of therapeutic interventions. Applied and Preventive Psychology, 11 (3), 141–156. 10.1016/j.appsy.2005.05.002. [DOI] [Google Scholar]
- Chu BC, Temkin AB, & Toffey K (2016). Transdiagnostic mechanisms and treatment for children and adolescents, Vol. 1 10.1093/oxfordhb/9780199935291.013.10. [DOI] [Google Scholar]
- Collins LM, Murphy SA, & Strecher V (2007). The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART). New methods for more potent eHealth interventions. American Journal of Preventive Medicine, 32(5), S112–S118. 10.1016/j.amepre.2007.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Cristea IA, Karyotaki E, Reijnders M, & Hollon SD (2017). Component studies of psychological treatments of adult depression: A systematic review and meta-analysis. Psychotherapy Research, 0(0), 1–15. 10.1080/10503307.2017.1395922. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Murphy M, & Hendershot CS (2015). Treatment dismantling pilot study to identify the active ingredients in personalized feedback interventions for hazardous alcohol use: Randomized controlled trial. Addiction Science & Clinical Practice, 10, 1. 10.1186/s13722-014-0022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, & Cohen JA (2009). Effective treatments for PTSD: Practice guidelines from the international society for traumatic stress studies (2nd ed.). In effective treatments for PTSD: Practice guidelines from the international society for traumatic stress studies (2nd ed. ). [Google Scholar]
- Fortney JC, Unutzer J, Wrenn G, Pyne JM, Smith GR, Schoenbaum M, et al. (2017). A tipping point for measurement-based care. Psychiatric Services 10.1176/appi.ps.201500439. [DOI] [PubMed] [Google Scholar]
- van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera SM, Plan J, et al. (2013). Non-specialist health worker interventions for the care ofmental, neurological and substance-abuse disorders in low- and middle-income countries. Cochrane Database OfSystematic Reviews (11). [DOI] [PubMed] [Google Scholar]
- Girgus JS, & Yang K (2015). Gender and depression. Current Opinion in Psychology, 4, 53–60. 10.1016/j.copsyc.2015.01.019. [DOI] [Google Scholar]
- Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, & Vogt TM (2006). Evaluating the impact of health promotion programs: Using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Education Research, 21(5), 688–694. 10.1093/her/cyl081. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, & Boles SM (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89(9), 1322–1327. 10.2105/AJPH.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen NB, Lambert MJ, & Forman EM (2002). The psychotherapy dose-response effect and its implications for treatment delivery services. Clinical Psychology: Science and Practice. 10.1093/clipsy/9.3.329. [DOI] [Google Scholar]
- Haroz EE, Bass JK, Lee C, Murray LK, Robinson C, & Bolton P (2014). Adaptation and testing of psychosocial assessment instruments for cross-cultural use: An example from the Thailand Burma border. BMC Psychology, 2(31), 1–9. 10.1186/s40359-014-0031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A, Hope DA, & Hayes S (2007a). Towards an understanding of the process and mechanisms of change in cognitive behavioral therapy: Linking innovative methodology with fundamental questions. Clinical Psychology Review, 10.1016/j.cpr.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AM, Laurenceau JP, Feldman G, Strauss JL, & Cardaciotto LA (2007b). Change is not always linear: The study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review. 10.1016/j.cpr.2007.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebner RB, & Tonigan JS (2007). The search for mechanisms of behavior change in evidence-based behavioral treatments for alcohol use disorders: Overview. Alcoholism: Clinical and Experimental Research, 31 (s3), 1s–3s. 10.1111/j.1530-0277.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- Insel TR (2009). Translating scientific opportunity into public health impact. Archives of General Psychiatry, 66(2), 128. 10.1001/archgenpsychiatry.2008.540. [DOI] [PubMed] [Google Scholar]
- Kane JC, Skavenski Van Wyk S, Murray SM, Bolton P, Melendez F, Danielson CK, … Murray LK (2017). Testing the effectiveness of a transdiagnostic treatment approach in reducing violence and alcohol abuse among families in Zambia: Study protocol of the violence and alcohol treatment (VATU) trial. Global Mental Health, 4, e18. 10.1017/gmh.2017.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE (2005). Treatment outcomes, common factors, and continued neglect of mechanisms of change. Clinical Psychology: Science and Practice, 10.1093/clipsy/bpi023. [DOI] [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kazdin AE (2009). Understanding how and why psychotherapy leads to change. Psychotherapy Research, 19(4–5), 418–428. 10.1080/10503300802448899. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Nock MK (2003). Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, 44(8), 1116–1129. 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kelly KA, Rizvi SL, Monson CM, & Resick PA (2009). The impact of sudden gains in cognitive behavioral therapy for posttraumatic stress disorder. Journal of Traumatic Stress, 22(4), 287–293. 10.1002/jts.20427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klasnja P, Hekler EB, Shiftman S, Boruvka A, Almirall D, Tewari A, et al. (2015). Microrandomized trials: An experimental design for developing just-in-time adaptive interventions. Health Psychology, 34(supplement), 1220–1228. 10.1037/hea0000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurenceau J-P, Hayes AM, & Feldman GC (2007). Some methodological and statistical issues in the study of change processes in psychotherapy. Clinical Psychology Review, 10.1016/j.cpr.2007.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansell W, Harvey A, Watkins ER, & Shafran R (2008). Cognitive behavioral processes across psychological disorders: A review of the utility and validity of the transdiagnostic approach. International Journal of Cognitive Therapy, 1(3), 181–191. 10.1680/ijct.2008.1.3.181. [DOI] [Google Scholar]
- Mansell W, Harvey A, Watkins E, & Shafran R (2009). Conceptual foundations of the transdiagnostic approach to CBT. Journal of Cognitive Psychotherapy, 23(1), 6–19. 10.1891/0889-8391.23.1.6. [DOI] [Google Scholar]
- Martin P, Murray LK, Darnell D, & Dorsey S (2018). Transdiagnostic treatment approaches for greater public health impact: Implementing principles of evidence-based mental health interventions. Clinical psychology: Science and practice, 25, e12270. 10.1111/cpsp.12270. [DOI] [Google Scholar]
- McHugh RK, Murray HW, & Barlow DH (2009). Balancing fidelity and adaptation in the dissemination of empirically-supported treatments: The promise of transdiagnostic interventions. Behaviour Research and Therapy, 47(11), 946–953. 10.1016/j.brat.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicine Institute of, T. (2015). Psychosocial interventions for mental and substance use disorders: A framework for establishing evidence-based standards. Washington DC. 10.17226/19013. [DOI] [PubMed] [Google Scholar]
- Mirza I, & Jenkins R (2004). Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: Systematic review. BMJ. (Clinical Research Ed.) 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy R, Cooper Z, Hollon SD, & Fairburn CG (2009). How do psychological treatments work? Investigating mediators of change. Behaviour research and therapy. 10.1016/j.brat.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Bolton P, Jordans MJ, Rahman A, Bass J, … Verdeli H (2011). Building Capacity in Mental Health Interventions in Low-resource countries: An Apprenticeship Model for Training Local Providers. International Journal of Mental Health Systems, 5(1), 30. 10.1186/1752-4458-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Haroz E, Lee C, Alsiary MM, Haydary A, … Bolton P (2014). A common elements treatment approach for adult mental health problems in low- and middle-income countries. Cognitive and Behavioral Practice, 21(2), 111–123. 10.1016/j.cbpra.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, Hall B, Dorsey S, Ugeuto A, Puffer E, Ismael A, … Akiba C (2018). An evaluation of a common elements treatmentapproach for youth in Somali refugee camps. Global Mental Health, 5, 1–15. 10.1017/gmh.2018.7. e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, & Jordans MJD (2016). Rethinking the service delivery system of psychological interventions in low and middle income countries. BMC Psychiatry, 16(1) 10.1186/s12888-016-0938-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, & Kane J (2018). Results from a randomized trial on CETA for violence and substance use in Zambia. Zambia ministry of health dissemination meeting. Lusaka. [Google Scholar]
- Murray LK, Skavenski S, Kane JC, Mayeya J, Dorsey S, Cohen JA, … Bolton PA (2015). Effectiveness of trauma-focused cognitive behavioral therapy among trauma-affected children in lusaka, Zambia: A randomized clinical trial. JAMA Pediatrics, 169(8), 1–9. 21205 10.1001/jamapediatrics.2015.0580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, & Elbert T (August 2008). Treatment of posttraumatic stress disorder by trained lay counselors in an african refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 76(4), 686–694. 10.1037/0022-006X.76.4.686. [DOI] [PubMed] [Google Scholar]
- Neuner F, Schauer M, Klaschik C, Karunakara U, & Elbert T (August 2004). A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology, 72(4), 579–587. 10.1037/0022-006X.72.4.579. [DOI] [PubMed] [Google Scholar]
- O’Callaghan P, McMullen J, Shannon C, Rafferty H, & Black A (2013). A randomized controlled trial of trauma-focused cognitive behavioral therapy for sexually exploited, war-affected Congolese girls. Journal of the American Academy of Child & Adolescent Psychiatry, 52(4), 359–369. 10.1016/j.jaac.2013.01.013. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer M, & Pattison P (2004). Posttraumatic stress disorder and depression following trauma: Understanding comorbidity. American Journal of Psychiatry, 161, 1390–1396. 10.1176/appi.ajp.161.8.1390. [DOI] [PubMed] [Google Scholar]
- Papas RK, Sidle JE, Gakinya BN, Baliddawa JB, Martino S, Mwaniki MM, … Maisto SA (2011). Treatment outcomes of a stage 1 cognitive-behavioral trial to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction, 106(12), 2156–2166. 10.1111/j.1360-0443.2011.03518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, … Whiteford H (April 16, 2016). Addressing the burden of mental, neurological, and substance use disorders: Key messages from Disease Control Priorities. The Lancet, 387(10028), 1672–1685. 3rd ed. 10.1016/S0140-6736(15)00390-6. [DOI] [PubMed] [Google Scholar]
- Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, … Kirkwood BR (2010). Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): A cluster randomised controlled trial. The Lancet, 376, 2086–2095. 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl SB, & Norton PJ (2017). Transdiagnostic versus diagnosis specific cognitive behavioural therapies for anxiety: A meta-analysis. Journal of Anxiety Disorders, 46, 11–24. 10.1016/j.janxdis.2016.07.004. [DOI] [PubMed] [Google Scholar]
- Penfold RB, & Zhang F (2013). Use of interrupted time series analysis in evaluating health care quality improvements. Academic Pediatrics 10.1016/j.acap.2013.08.002. [DOI] [PubMed] [Google Scholar]
- Pompoli A, Furukawa TA, Efthimiou O, Imai H, Tajika A, & Salanti G (2018). Dismantling cognitive-behaviour therapy for panic disorder: A systematic review and component network meta-analysis. Psychological Medicine, 1–9 10.1017/S0033291717003919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Malik A, Sikander S, Roberts C, & Creed F (2008). Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: A cluster-randomised controlled trial. Lancet, 372(9642), 902–909. 10.1016/S0140-6736(08)61400-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods. Advanced quantitative techniques in the social sciences, 1. [Google Scholar]
- Ruf M, Schauer M, Neuner F, Catani C, Schauer E, & Elbert T (2010). Narrative exposure therapy for 7- to 16-year-olds: A randomized controlled trial with traumatized refugee children. Journal of Traumatic Stress, 23(4), 437–445. 10.1002/jts.20548. [DOI] [PubMed] [Google Scholar]
- Sauer-Zavala S, Gutner CA, Farchione TJ, Boettcher HT, Bullis JR, & Barlow DH (2017). Current definitions of “transdiagnostic” in treatment development: A search for consensus. Behavior Therapy, 48(1), 128–138. 10.1016/j.beth.2016.09.004. [DOI] [PubMed] [Google Scholar]
- Scarinci IC, Beech BM, Naumann W, Kovach KW, Pugh L, & Fapohunda B (2002). Depression, socioeconomic status, age, and marital status in black women: A national study. Ethnicity & Disease. [PubMed] [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. The Annals of Statistics, 10.1214/aos/1176344136. [DOI] [Google Scholar]
- Scott K, & Lewis CC (2015). Using measurement-based care to enhance any treatment. Cognitive and Behavioral Practice, 22(1), 49–59. 10.1016/j.cbpra.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data Analysis : Modeling change and event occurrence. ISBN0195152964 10.1093/acprof. [DOI] [Google Scholar]
- Singla DR, Hollon SD, Fairburn CG, Dimidjian S, & Patel V (2019). The roles of early response and sudden gains on depression outcomes: Findings from a randomized controlled trial of behavioral activation in Goa, India. Clinical Psychological Science, 10.1177/2167702619825860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp (2013). Stata statistical software: Release 13. 2013 10.2307/2234838. [DOI]
- Tang TZ, Beberman R, DeRubeis RJ, & Pham T (February 2005). Cognitive changes, critical sessions, and sudden gains in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology, 73(1), 168–172. 10.1037/0022-006X.73.1.168. [DOI] [PubMed] [Google Scholar]
- Tang TZ, & DeRubeis RJ (December 1999). Sudden gains and critical session in cognitive-behavioural therapy for depression. Journal of Consulting and Clinical Psychology, 67(6), 894–904. 10.1037/0022-006X.67.6.894. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Chatterji S, Evans-Laeko S, Gruber M, Sampson N, Aguilar-Gaxiola S, … Kessler RC (2017). Undertreatment of people with major depressive disorder in 21 countries. British Journal of Psychiatry, 210(2), 119–124. 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigo D, Thornicroft G, & Atun R (2016). Estimating the true global burden of mental illness. The Lancet Psychiatry, 3(2), 171–178. 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, & Friedman MJ (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. Journal of Clinical Psychiatry, 74(6), e541–e550. 10.4088/JCP.12r08225. [DOI] [PubMed] [Google Scholar]
- Weersing VR, & Weisz JR (2002). Mechanisms of action in youth psychotherapy. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 43(1), 3–29. 10.1111/1469-7610.00002. [DOI] [PubMed] [Google Scholar]
- Weiss W, & Bolton P (2010). Assessment of torture survivors in Southern Iraq: Development and testing of a locally-adapted assessment instrument. [Google Scholar]
- Weiss WM, Murray LK, Zangana GAS, Mahmooth Z, Kaysen D, Dorsey S, … Bolton P (2015). Community-based mental health treatments for survivors of torture and militant attacks in southern Iraq: A randomized control trial. BMC Psychiatry, 15, 249. 10.1186/s12888-015-0622-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, Bearman SK, … Mayberg S (2012). Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives of General Psychiatry, 69(3), 274–282. 10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Krumholz LS, Santucci L, Thomassin K, & Ng MY (2015). Shrinking the gap between research and practice: Tailoring and testing youth psychotherapies in clinical care contexts. Annual Review of Clinical Psychology, 11, 139–163. 10.1146/annurev-clinpsy-032814-112820. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Ugueto AM, Herren J, Afienko SR, & Rutt C (2011). Kernels vs. Ears, and other questions for a science of treatment dissemination. Clinical Psychology: Science and Practice, 18(1), 41–46. 10.1111/j.1468-2850.2010.01233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SPH, Ale CM, Young B, Dammann JE, Tiede MS, & Biggs BK (2015). The feasibility of improving CBT for childhood anxiety disorders through a dismantling study. Behaviour Research and Therapy, 73, 83–89. 10.1016/j.brat.2015.07.011. [DOI] [PubMed] [Google Scholar]


