Abstract
Background
Coronavirus disease 2019 (COVID-19) has again highlighted the crucial role of healthcare workers in case management, disease surveillance, policy development, and healthcare education and training. The ongoing pandemic demonstrates the importance of having an emergency response plan that accounts for the safety of frontline healthcare workers, including those working in critical care settings.
Objectives
The aim of the study was to explore Australian critical care nurses' knowledge, preparedness, and experiences of managing patients diagnosed with severe acute respiratory syndrome coronavirus 2 infection (SARS-CoV-2) and COVID-19.
Methods
An exploratory cross-sectional study of Australian critical care nurses was conducted between June and September 2020. An anonymised online survey was sent to Australian College of Critical Care Nurses' members to collect information about their knowledge, preparedness, and experiences during the COVID-19 pandemic. Descriptive statistics were used to summarise and report data.
Results
A total of 157 critical care nurses participated, with 138 fully complete surveys analysed. Most respondents reported ‘good’ to ‘very good’ level of knowledge about COVID-19 and obtained up-to-date COVID-19 information from international and local sources. Regarding managing patients with COVID-19, 82.3% felt sufficiently prepared at the time of data collection, and 93.4% had received specific education, training, or instruction. Most participants were involved in assessing (89.3%) and treating (92.4%) patients with COVID-19. Varying levels of concerns about SARS-CoV-2 infection were expressed by respondents, and 55.7% thought the pandemic had increased their workload. The most frequent concerns expressed by participants were a lack of appropriate personal protective equipment (PPE) and fear of PPE shortage.
Conclusions
While most nurses expressed sufficient preparedness for managing COVID-19 patients, specific education had been undertaken and experiential learning was evident. Fears of insufficient or lack of appropriate PPE made the response more difficult for nurses and the community. Preparedness and responsiveness are critical to successful management of the COVID-19 pandemic and future outbreaks of emerging infectious diseases.
Keywords: Critical care, COVID-19, SARS-CoV-2, Nurse, Preparedness, Knowledge acquisition, Clinical experience
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), began as a cluster of pneumonia-like cases identified in Wuhan, Hubei Province, in China in late December 2019.1 , 2 The World Health Organisation (WHO) declared the outbreak to be a Public Health Emergency of International Concern on January 30th, 2020, and issued recommendations to all countries that they should review their preparedness plans, including active surveillance, early detection, isolation, and case management, and contact tracing, to prevent further spread of COVID-19.3
Since January 25, 2020, when the first case of COVID-19 was confirmed in Australia,4 , 5 the country has experienced significant challenges in containing the outbreak. The intensified pressure on the healthcare system as well as the societal and socio-economic impacts driven by long lockdowns and stringent public health measures have had a significant toll on Australian federal and state governments and a range of industries, organisations, and communities.[6], [7], [8]
The COVID-19 global health emergency highlights the importance of having an agile and robust emergency response plan that deploys sustained infection prevention and disease control to ensure the safety of patients and health professionals, particularly those who are patient-facing such as those in infection prevention and control, infectious disease practice, emergency care, critical care, public health, and general practice. These and other health professionals perform critical functions including case management, disease surveillance, policy development, and education and training of clinicians and support staff.
Previous research that examined clinicians' experiences, knowledge, and perception in various outbreaks, including that of SARS-CoV-1,9 Ebola virus disease,10 and the Middle East respiratory syndrome coronavirus pandemic,11 , 12 helped to shape Australia's outbreak containment plan, response, and preparedness for COVID-19. In the context of critical care practice, successful management of outbreaks of emerging infectious diseases could be greatly influenced by whether a preparedness plan already existed and if the intensive care unit (ICU) functions are effectively integrated with hospital-wide plans.13 Learnings from previous outbreaks have highlighted the necessity for adherence to rigorous infection control practices, efficient management of staff and their exposure, and provision of sustained training and education for key clinical practices.[14], [15], [16]
On this basis, examining clinicians' knowledge, preparedness, and experiences of managing the COVID-19 response is anticipated to assist with successful outbreak management during the current pandemic and in future emerging infectious disease situations. This article reports the findings of an explorative study of critical care nurses' knowledge, preparedness, and experiences of managing SARS-CoV-2 infection and COVID-19 in the Australian healthcare setting.
2. Methods
2.1. Study design
An exploratory cross-sectional study of Australian critical care nurses was conducted between June 3 2020, and September 3 2020.
2.2. Setting and population
The study population was critical care nurses practising in Australia, who held current membership of the Australian College of Critical Care Nurses (ACCCN). The ACCCN is the peak national professional nursing association representing critical care nurses in Australia, with a membership of 1415 registered nurses.
2.3. Instrument
An anonymised online survey was generated using Research Electronic Data Capture (REDCap™). The survey questions were initially constructed from the previously published literature in line with the Capability, Opportunity, Motivation, Behaviour (COM-B) model of behaviour.17 A panel of experts comprising critical care nursing academics and infection prevention and control researchers reviewed the items gathered from similar surveys used in previous studies. The panel agreed on items to be included in this survey and validated the instrument. The final survey consisted of 37 multiple choice and free-text items over four sections exploring participants' demographics (three items), knowledge of COVID-19 and SARS-CoV-2 (four items), preparedness in relation to the current outbreak (13 items), and experiences of working during the ongoing COVID-19 outbreak (17 items) (see supplementary material).
2.4. Data collection and analysis
An electronic survey link was distributed in an invitation email via the ACCCN to invite members to participate in the study. Two follow-up reminder emails were sent to members. Collected data were cleaned and exported into SPSS (IBM Corp. Released 2019, version 26.0) for analysis. Descriptive statistics were used to summarise sample characteristics and results. Answers to open-ended questions were managed in Microsoft Excel and analysed using conventional content analysis technique.18 The first author performed axial coding of the data, grouped comparable codes into one code, and generated the codebook. The codes were discussed within the research team that led to emergence of the major themes that incorporated the significant challenges of critical care nurses during the COVID-19 pandemic.
2.5. Human research ethics
This study was approved by the Human Research Ethics Committee at the University of Sydney, Australia (HREC 2020/200).
3. Results
The survey was distributed via the ACCCN to reach out to the members of the college (1415 registered critical care nurses). A total of 157 responses were received from ACCCN members who participated in the study and provided demographic information. After excluding those whose survey records were incomplete, the data of 138 participants were included for analysis. Table 1 summarises the key characteristic information of the sample.
Table 1.
Demographic characteristics of the critical care nurse participants N = 157.
| Sample characteristics | n (%) |
|---|---|
| Current state or territory of work | |
| Australian Capital Territory | 6 (3.8) |
| New South Wales | 33 (21.0) |
| Northern Territory | 3 (1.9) |
| Queensland | 16 (10.2) |
| South Australia | 3 (1.9) |
| Tasmania | 3 (1.9) |
| Victoria | 65 (41.4) |
| Western Australia | 24 (15.3) |
| Currently working outside Australia | 4 (2.5) |
| Country of residency | |
| Australia | 153 (97.5) |
| New Zealand | 0 (0) |
| Other countries | 4 (2.5) |
| Member of the COVID-19 planning and response committee | |
| Not a member of a committee | 89 (65.4) |
| At the unit level | 37 (27.2) |
| At the hospital level | 14 (10.3) |
| At the health district level | 1 (0.7) |
| At the state level | 8 (5.9) |
| At the national level | 7 (5.1) |
| At the international level | 1 (0.7) |
| Mean (SD) | Range (years) | Median | |
|---|---|---|---|
| Years of professional work | 17.9 (12.5) | 1–66 | 15 |
COVID-19 = coronavirus disease 2019; SD = standard deviation.
3.1. Knowledge of SARS-CoV-2 and COVID-19
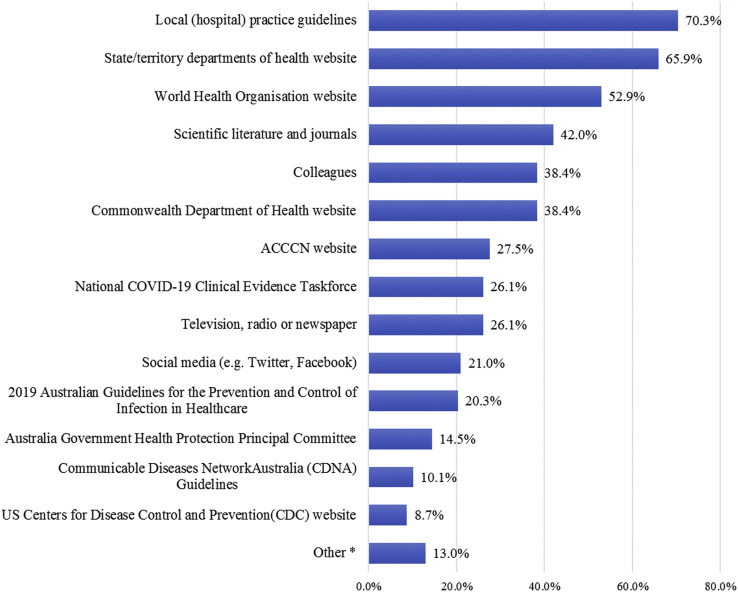
The majority of critical care nurses rated their current level of knowledge about COVID-19 as ‘good’ (n = 68, 49.3%) or ‘very good’ (n = 47, 34.1%) on a 5-point Likert scale. This was followed by those who rated their COVID-19 knowledge as ‘fair’ (n = 15, 10.9%), ‘excellent’ (n = 7, 5.1%), and ‘poor’ (n = 1, 0.7%). Information on participants' knowledge was drawn from a range of sources, including local (hospital) practice guidelines (n = 97, 70.3%), state/territory departments of health website (n = 91, 65.9%), and the WHO website (n = 73, 52.9%), as shown in Fig. 1 .
Fig. 1.
Critical care nurses' use of existing sources to obtain up-to-date information about COVID-19. COVID-19 = coronavirus disease 2019; ACCCN = Australian College of Critical Care Nurses.
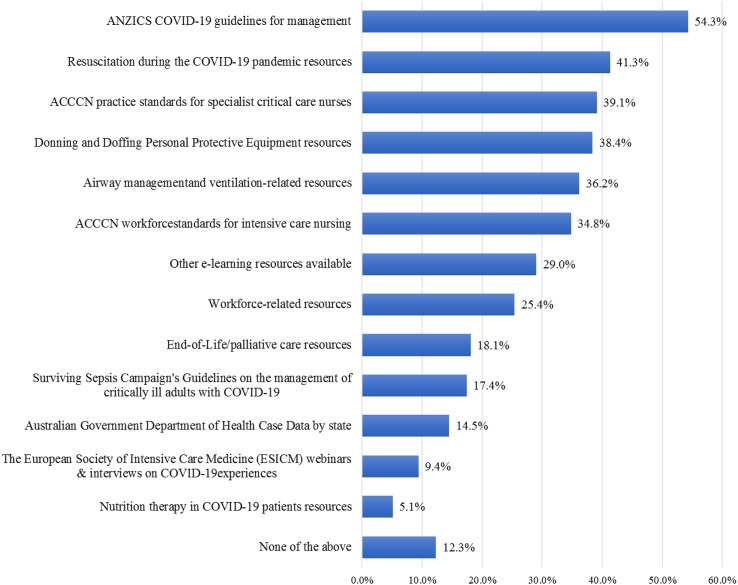
The ACCCN provided members with an array of resources during 2020 via its website as shown in Fig. 2 . Among these resources, the ‘ANZICS COVID-19 guidelines for management’ and the resources for ‘Resuscitation during COVID-19 pandemic’ were sourced and used more than any other resource.
Fig. 2.
Critical care nurses' use of ACCCN website COVID-19 resources. COVID-19 = coronavirus disease 2019; ACCCN = Australian College of Critical Care Nurses.
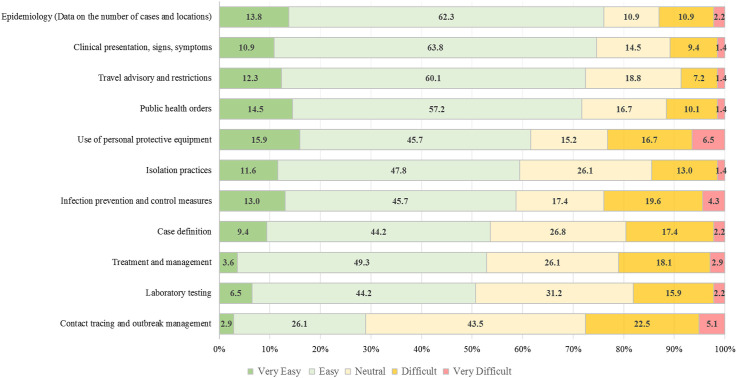
The participants were asked how easy or difficult it was to keep up to date with information about COVID-19 in 11 key areas, as shown in Fig. 3 . With the exception of the ‘Contact tracing and outbreak management’, the majority of participants felt it was ‘easy’ and ‘very easy’ to follow up and keep up to date with COVID-19 information across all fields.
Fig. 3.
Critical care nurses' opinion about the ease or difficulty of knowledge acquisition in 11 key information areas of COVID-19. COVID-19 = coronavirus disease 2019.
3.2. Preparedness for the COVID-19 outbreak
The majority of respondents (n = 102, 75%) reported they were not prepared for COVID-19 when the WHO was formally notified about the initial cluster of cases in Wuhan, China, on December 31, 2019. However, a sizable majority (n = 112, 82.3%) believed they were ‘moderately’ or ‘extremely’ prepared for managing patients with COVID-19 by the time they responded to this survey (June 3 to September 3, 2020). Most participants (n = 126, 92.6%) thought their workplace was prepared to manage COVID-19 in the future.
Most participants (n = 127, 93.4%) reported that they had received specific education, training, or instruction about COVID-19 within their workplace via different education and training programs including ‘In-service education’ (n = 113, 89%), ‘PPE training and certification’ (n = 86, 63.2%), ‘Written materials’ (n = 81, 63.8%), ‘ICU-specific e-learning modules’ (n = 66, 52%), and ‘Lectures or Grand Rounds’ (n = 36, 28.3%). A majority (n = 93, 73.2%) rated these education and training programs ‘mostly’ or ‘entirely’ adequate. Two-thirds of participants (n = 86, 63.2%) had completed outbreak management education and training, either via internal programs run within their workplace (n = 77, 89.5%) or through external programs (n = 24, 27.9%). A large proportion of participants (n = 121, 89%) reported receiving training or certification in the use of PPE for managing COVID-19, and 76.9% of them rated the PPE training as ‘mostly’ or ‘entirely’ adequate. A majority of participants agreed that they were provided with clear, timely, and authoritative information about COVID-19 in their workplace (n = 95, 69.8%), by their respective state or territory health department (n = 107, 78.7%), or by the federal health department (n = 93, 68.4%) (see supplementary material).
Most participants (n = 114, 83.8%) indicated that their workplace had COVID-19 guidelines and some form of outbreak response plan, and a large proportion of these participants (n = 79/114, 69.3%) were ‘moderately’ or ‘entirely’ familiar with those guidelines and response plans. Although the majority of these participants (59.6%) indicated that it was easy to adhere to guidelines and response plans, some found it to be more difficult (n = 16, 14%). A smaller proportion of participants (n = 19, 14%) were unsure as to whether such guidelines and response plans existed in their workplace, and a few (n = 3, 2.2%) stated that their workplace had no COVID-19 response plans or guidelines.
3.3. Experiences of working during the COVID-19 outbreak
The majority (n = 117/131, 89.3%) reported working in settings wherein assessments of suspected cases of COVID-19 occurred, and the vast majority (n = 121/131, 92.4%) reported treating suspected or confirmed COVID-19 cases. The number of critical care nurses who were directly involved in caring for COVID-19 cases (suspected or confirmed) was more than twice the number of those who did not have direct involvement with those cases (70.2% versus 29.8%, respectively). Most participants (n = 116, 88.5%) reported being involved in some form of COVID-19 outbreak response activity (see supplementary material).
Varying levels of concerns about contracting SARS-CoV-2 were reported, with higher proportions being ‘slightly concerned’ (n = 43, 32.8%), ‘somewhat concerned’ (n = 38, 29%), and ‘moderately concerned’ (n = 31, 23.7%). There were only a few participants who were either ‘not concerned’ (n = 13, 9.9%) or ‘extremely concerned’ (n = 6, 4.6%) about being infected with the virus. In relation to concerns about contracting SARS-CoV-2 infection at work, none, except one participant, had taken annual leave, and only a few participants (n = 7, 5.3%) had taken sick leave. Just more than one quarter of respondents (n = 35, 26.7%) indicated that they had, or would have, avoided telling others about their involvement in the delivery of care for patients with COVID-19 because they were afraid of negative reactions from others. About one-third of the participants felt their family or friends were avoiding contact with them as a response to the nature of their work (n = 44, 33.6%). A minority (n = 18, 13.7%) had experienced or witnessed racial or other forms of discrimination at work in relation to the COVID-19 outbreak.
More than half of the respondents reported that the COVID-19 outbreak had increased their workload (n = 73, 55.7%), whereas a few indicated that their workload was lessened (n = 9, 6.9%) or remained constant (n = 10, 7.6%). A slightly higher proportion of respondents reported they felt ‘moderately’ or ‘extremely’ stressed at work as a result of the current outbreak (n = 58, 44.3%) compared with those who were only ‘slightly’ or ‘somewhat stressed’ (n = 54, 41.2%) and those who were ‘not stressed at all’ (n = 19, 14.5%).
Although a majority (n = 95, 72.6%) indicated that their workplace provided support services (e.g., debriefing and/or staff psychological support services), only a small proportion of participants attended debriefings (n = 30, 22.9%) and/or accessed psychological services (n = 6, 4.6%). Those who used these services rated them useful (n = 28/30, 93.3% for debriefing and n = 5/6, 83.3% for psychological services).
The participants were invited to list their most significant challenges during the COVID-19 outbreak. The most common challenge reported was in relation to PPE supply and use (n = 31/131, 23.7%). Lack of appropriate PPE (including the training for use of PPE), frequent changes to PPE guidelines, and fear of PPE shortage were the most dominant concerns, as illustrated by the following quotes:
“PPE is a major factor. We have very limited supplies of N95 masks that actually pass a fit check. We have plenty of Chinese made masks that will not pass a fit check.” (Participant 57)
The continuous change in what kind of PPE to wear when providing care for COVID-19 suspected or confirmed patients, without providing feedback on whether what we were wearing was actually providing us coverage and giving usadded stress about being exposed because of the changing PPE rules. (Participant 166)
Staff anxiety and mental exhaustion were the second greatest challenge (n = 17/131, 13%), which was reported in association with increased stress levels and high burnout rates, as summarised in the following quote:
“The sheer workload involved in testing, isolating, caring for and transferring every person who was swabbed (who are overwhelmingly COVID-19 negative) adds to the stressful nature of my work and adds many additional steps and tasks to every nursing action … We have been running on anxiety and fear for the past three months and we're exhausted andburned out.” (Participant 129)
The third most common challenge reported was the communication challenges (n = 14/131, 10.7%). Poor communication between management and clinicians during the course of the outbreak was a common concern, as signified in the following participants' remarks:
“The mixed or unclear messages and inconsistencies given by management.” (Participant 48)
“The lack of preparedness, slow response and lack of timely communication of management strategies while often completely ignoring the concerns raised by clinical staff”. (Participant 131)
These excerpts illustrate the importance of communication in outbreak response.
4. Discussion
This study explored the knowledge, preparedness, and experiences of critical care nurses in Australian healthcare settings during the COVID-19 outbreak. Our findings suggest that the critical care nurses in this study had access to a variety of sources of local, national, and international information about COVID-19. Since the start of the COVID-19 pandemic, the ACCCN has played an active role in helping to facilitate knowledge acquisition of critical care nurses and supporting them as one of the core clinical craft groups at the forefront of Australia's defence against the pandemic. The ACCCN's collaboration with the ANZICS led to the development of a national set of guidelines for the management of patients requiring intensive care during the COVID-19 outbreak.19 , 20 These efforts may have contributed to the high level of COVID-19 literacy in this sample, and highlight the importance of timely interdisciplinary collaboration with relevant professional bodies.
Critical care nurses in this study indicated they could easily follow up and keep up to date with information about most of the key areas relating to COVID-19. However, it appears some nurses had difficulty keeping up with the latest information in the areas of contact tracing, outbreak management, infection prevention and control measures, and the use of PPE. As such, the challenges pertaining to these areas had the biggest potential to impact clinical practice. This suggests that potential planning directives are needed to ensure that all critical care nurses are well informed and effectively communicated about changing measures and guidelines in the aforementioned areas during the COVID-19 pandemic.
Our findings demonstrated a significant shift in the perceived level of preparedness during the trajectory of the COVID-19 pandemic. The vast majority believed they were less prepared in the early phase of the COVID-19 outbreak in Australia, but they were well prepared to manage the COVID-19 outbreak currently and in future. Such a drastic shift in preparedness could be partly explained by the multitude of efforts made by nurses themselves, along with health authorities and key stakeholders at different levels locally and nationally to support Australian critical care nurses during the COVID-19 pandemic.
An overwhelming majority of participants believed they were provided with clear, timely, and authoritative information about COVID-19 in their workplace, by their state or territory health department and by federal health department. In most cases, critical care nurses were familiar with, and adhered to, their workplace COVID-19 guidelines or outbreak response plans and had some forms of engagement in COVID-19–specific education and training. Our findings suggest that a combination of the high level of support from stakeholders and authorities together with ongoing engagement of clinicians could have contributed to improve the level of the Australian healthcare system's preparedness for COVID-19. However, there are several ongoing practice challenges in this group, some of which are precipitated by the very nature of the COVID-19 outbreak. The rapid nature of the COVID-19 pandemic mandated the adoption of a ‘learn as we go’ pattern for most health sectors in Australia and around the world. That said, experiential learning shared openly with colleagues internationally as seen during 2020 has been unprecedented, all with the aim of skilling staff to save the lives of patients and themselves. Multiple variations to the emergency response plan, public health orders, and practice guidelines were unavoidable, yet necessary for the sake of ensuring the safety of patients and frontline healthcare workers. Nonetheless, an unintended consequence of these continuous updates and changes created new challenges for critical care nurses—to keep up to date with the most recent instructions and practice guidelines.
Since the start of this pandemic, critical care nurses have been heavily involved in managing and treating COVID-19 cases in all the states and jurisdictions.21 , 22 Our findings show that more than two-thirds of critical nurses in this study were directly involved in caring for patients with suspected or confirmed COVID-19 in the country. The two dominant COVID-19 outbreak response activities of critical care nurses were in relation to PPE donning and doffing training and provision of support for healthcare professionals. Notwithstanding the intense exposure and involvement in COVID-19-related activities, there appeared to be high levels of concern about contracting SARS-CoV-2 which was reflected in participants' coping practices and behaviours. For instance, some used emotion-focused strategies (e.g., reducing social contacts and avoiding communications about their involvement in caring for patients with COVID-19) to minimise the risk of negative reactions and potential discrimination from others. Some used the available resources provided in their workplace (e.g., debriefing and employee psychological support) to practice problem-focused coping techniques to counteract their anxiety and mental exhaustion. These are consistent with the findings reported in other studies in previous outbreaks.23 , 24
This article identified several key elements in the domains of knowledge, preparedness, and experiences of a group of Australian critical care nurses who were involved in managing patients with COVID-19. To the best of our knowledge, there has been no similar study with the same aims and scope. The sample size in this study prohibited subanalyses that could have highlighted different challenges specific to work context. There was also likely to be some elements of selection bias among respondents, culminated by the convenient recruitment method and advertising the study via the ACCCN. For instance, those who chose to participate in the study are likely to have more involvement and interest in COVID-19 outbreak management. Nevertheless, the findings reported in this article provide insight into multiple key facets of practice of a cohort of Australian critical care nurses and can be used in planning for successful outbreak management during the current pandemic and in future emerging infectious disease outbreaks.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Shizar Nahidi: Methodology, Validation, Formal analysis, Investigation, Resources, Data curation, Writing – original draft, Writing – review and editing, Project administration; Cristina Sotomayor-Castillo: Methodology, Validation, Investigation, Resources, Data curation, Writing – original draft, Writing – review and editing, Project administration; Cecilia Li: Methodology, Validation, Resources, Data curation, Investigation, Writing – review and editing; Judy Currey: Validation, Resources, Writing – review and editing; Rosalind Elliott: Validation, Resources, Writing – review and editing; Ramon Z. Shaban: Conceptualisation, Methodology, Validation, Formal analysis, Investigation, Resources, Writing – review and editing, Project administration.
Conflict of interest
The authors have no conflict of interest to declare.
Acknowledgements
The authors extend their sincere thanks to all the critical care nurses who participated in this study. The authors also thank the Australian College of Critical Care Nurses for their support in this study and their assistance in distributing the survey to the college members.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.aucc.2021.04.008.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization (WHO) World Health Organization; Geneva: 21 January 2020. Novel coronavirus (2019-nCoV): situation report-1. [Google Scholar]
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel Coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) World Health Organization; Geneva: 2020. WHO Director-General’s statement on IHR Emergency Committee on novel coronavirus (2019-nCoV) [Google Scholar]
- 4.Australia Department of Health . 2020. First confirmed case of novel coronavirus in Australia.https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/first-confirmed-case-of-novel-coronavirus-in-australia Available from: [Google Scholar]
- 5.Caly L., Druce J., Roberts J., Bond K., Tran T., Kostecki R., et al. Isolation and rapid sharing of the 2019 novel coronavirus (SARS-CoV-2) from the first patient diagnosed with COVID-19 in Australia. Med J Aust. 2020;212(10):459–462. doi: 10.5694/mja2.50569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blecher G.E., Blashki G.A., Judkins S. Crisis as opportunity: how COVID-19 can reshape the Australian health system. Med J Aust. 2020;213(5):196–198.e1. doi: 10.5694/mja2.50730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desborough J., Hall Dykgraaf S., de Toca L., Davis S., Roberts L., Kelaher C., et al. Australia's national COVID-19 primary care response. Med J Aust. 2020;213(3):104–106.e1. doi: 10.5694/mja2.50693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Sullivan D., Rahamathulla M., Pawar M. The Impact and implications of COVID-19: an Australian perspective. Int J Comm Soc Develop. 2020;2(2):134–151. [Google Scholar]
- 9.Deng J.F., Olowokure B., Kaydos-Daniels S.C., Chang H.J., Barwick R.S., Lee M.L., et al. Severe acute respiratory syndrome (SARS): knowledge, attitudes, practices and sources of information among physicians answering a SARS fever hotline service. Publ Health. 2006;120(1):15–19. doi: 10.1016/j.puhe.2005.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jalloh M.F., Li W.S., Bunnell R.E., Ethier K.A., O'Leary A., Hageman K.M., et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. 2018;3(2) doi: 10.1136/bmjgh-2017-000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan M.U., Shah S., Ahmad A., Fatokun O. Knowledge and attitude of healthcare workers about middle east respiratory syndrome in multispecialty hospitals of Qassim, Saudi Arabia. BMC Publ Health. 2014;14:1281. doi: 10.1186/1471-2458-14-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alsahafi A.J., Cheng A.C. Knowledge, attitudes and behaviours of healthcare workers in the kingdom of Saudi Arabia to MERS Coronavirus and other emerging infectious diseases. Int J Environ Res Publ Health. 2016;13(12):1214. doi: 10.3390/ijerph13121214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Dorzi H.M., Aldawood A.S., Khan R., Baharoon S., Alchin J.D., Matroud A.A., et al. The critical care response to a hospital outbreak of Middle East respiratory syndrome coronavirus (MERS-CoV) infection: an observational study. Ann Intensive Care. 2016;6(1):101. doi: 10.1186/s13613-016-0203-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arabi Y.M., Murthy S., Webb S. COVID-19: a novel coronavirus and a novel challenge for critical care. Intensive Care Med. 2020;46(5):833–836. doi: 10.1007/s00134-020-05955-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson S.S., Barranta N., Chertow D. Ebola at the National Institutes of Health: perspectives from critical care nurses. AACN Adv Crit Care. 2015;26(3):262–267. doi: 10.4037/NCI.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 16.El-Masri M.M., Williamson K.M., Fox-Wasylyshyn S.M. Severe acute respiratory syndrome: another challenge for critical care nurses. AACN Adv Crit Care. 2004;15(1):150–159. doi: 10.1097/00044067-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Michie S., van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6 doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 19.The Australian and New Zealand Intensive Care Society (ANZICS) 2020. COVID-19 guidelines.https://mcusercontent.com/03cbd5b8a6d36c351c46c235e/files/86e36972-a552-45da-8eab-8fd8c52a788d/ANZICS_COVID_19_Guidelines_Version_1.pdf?fbclid=IwAR2IPlq7SV3tWgG4_T6Xxz9XglMD1CxO1kHJSsAucqrXOjL_EVJZVK6InOw Available from: [Google Scholar]
- 20.Australian and New Zealand Intensive Care Society . 2020. ANZICS COVID-19 guidelines.https://www.anzics.com.au/coronavirus-guidelines/ Available from: [Google Scholar]
- 21.Marshall A.P., Austin D.E., Chamberlain D., Chapple L.-A.S., Cree M., Fetterplace K., et al. A critical care pandemic staffing framework in Australia. Aust Crit Care. 2020;S1036–7314(20):30300–30303. doi: 10.1016/j.aucc.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Litton E., Bucci T., Chavan S., Ho Y.Y., Holley A., Howard G., et al. Surge capacity of intensive care units in case of acute increase in demand caused by COVID-19 in Australia. Med J Aust. 2020;212(10):463–467. doi: 10.5694/mja2.50596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khalid I., Khalid T.J., Qabajah M.R., Barnard A.G., Qushmaq I.A. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016;14(1):7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S., et al. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. Can Med Assoc J. 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.