Abstract
Digital contact tracing provides an expeditious and comprehensive way to collect and analyze data on people’s proximity, location, movement, and health status. However, this technique raises concerns about data privacy and its overall effectiveness. This paper contributes to this debate as it provides a systematic review of digital contact tracing studies between January 1, 2020, and March 31, 2021. Following the PRISMA protocol for systematic reviews and the CHEERS statement for quality assessment, 580 papers were initially screened, and 19 papers were included in a qualitative synthesis. We add to the current literature in three ways. First, we evaluate whether digital contact tracing can mitigate COVID-19 by either reducing the effective reproductive number or the infected cases. Second, we study whether digital is more effective than manual contact tracing. Third, we analyze how proximity/location awareness technologies affect data privacy and population participation. We also discuss proximity/location accuracy problems arising when these technologies are applied in different built environments (i.e., home, transport, mall, park). This review provides a strong rationale for using digital contact tracing under specific requirements. Outcomes may inform current digital contact tracing implementation efforts worldwide regarding the potential benefits, technical limitations, and trade-offs between effectiveness and privacy.
Keywords: Digital contact tracing, manual contact tracing, SARS-CoV-2, location-awareness, proximity awareness, smartphone
1. Introduction
The coronavirus disease 2019 (COVID-19) is probably the most severe public health crisis our world has faced in the last decades (Maiti et al., 2021; Velraj & Haghighat, 2020). It has not only posed a serious threat against human life, but it has significantly impacted every aspect of social and economic activity (Ge et al., 2020, Rahmani and Mirmahaleh, 2020). Considering its unprecedented scale, the United Nations declared the pandemic as a social, human, and economic crisis that threatens human wellbeing and society’s sustainability (United Nations, 2020). The COVID-19 pandemic created the worst recession since the Great Depression, lasting from 1929 to 1939 (International Monetary Fund, 2020). As a consequence, people are likely to become poorer in the mid-to-long term (Batty, 2020), with an anticipated increase in suicide rates, substance abuse, domestic violence, homelessness, and food insecurity (DeLuca, Papageorge, Mitchel, & Kalish, 2020). Moreover, the psychological impact of social distancing and other non-pharmaceutical interventions (i.e., lockdowns) is likely to worsen due to the post-traumatic disorder effect (Fokas, Cuevas-Maraver, & Kevrekidis, 2020).
The COVID-19 pandemic with a multiple hit to health, economy, and society directly threatens the achievement of various Sustainable Development Goals (SDGs) (Zhou et al., 2020). The United Nations SDGs aim to achieve a better and more sustainable future for all societies by addressing global challenges (United Nations Development Programme, 2015). For example, SGD-3 (one of the 17 goals of the United Nations program) aims to ensure good health and wellbeing for everyone (United Nations Development Programme, 2015). Specifically, target SDG 3.3 aims to end epidemics (i.e., AIDS, malaria) or other communicable diseases. However, in the absence of medicines, or widespread vaccination, controlling an epidemic needs careful management and targeted interventions to alleviate its severe impact on society (Rahmani and Mirmahaleh, 2020). Many strategies have been introduced to mitigate the effects of COVID-19 pandemic, based on the concept of sustainable cities and environments (Jadidi et al., 2021). These include city management (Elavarasan, Pugazhendhi, Shafiullah, Irfan, & Anvari-Moghaddam, 2021; Zhou et al., 2020), lockdown management (Rahmani and Mirmahaleh, 2020), and digital contact tracing through the use of proximity awareness technologies, geospatial technologies, and wireless communication infrastructure (Jadidi et al., 2021).
1.1. Digital contact tracing
Given the life-saving importance of rapid action against a novel pathogen, tracing the contacts of infected individuals is critical for controlling its spread (Rahmani and Mirmahaleh, 2020). Contact tracing is a well-established method to interrupt chains of infection transmission by locating and isolating those in close contact with an infected individual (Braithwaite, Callender, Bullock, & Aldridge, 2020). Successful contact tracing is a powerful tool to keep the virus spread at manageable levels. However, a precondition should be met; finding active cases as soon as possible (World Health Organization, 2020). Failing to trace asymptomatic infected individuals or newly infected patients rapidly results in silent spread of the virus in the community for days before a significant number of patients have been diagnosed and health services become aware. In particular, for viruses such as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) where more than half of the transmissions (70%) occur before someone is symptomatic (Mizumoto, Kagaya, Zarebski, & Chowell, 2020), contact tracing should be as fast as possible. For a 3-day delay in notification, models show that the COVID-19 epidemic cannot be controlled (Ferretti, Wymant, & Kendall, 2020; Kretzschmar & Rozhnova, 2020). In such cases, manual contact tracing cannot significantly assist in containing the virus, especially when the epidemic is accelerating exponentially (Hellewell, Abbott, & Gimma, 2020; Peak Corey, Childs Lauren, Grad Yonatan, & Buckee Caroline, 2017). This emphasizes the need for rapid and effective contact tracing. By the same token, the World Health Organization (WHO), urges to “shift from reliance on existing surveillance networks to system of rapid, population-level active surveillance” (World Health Organization, 2020).
Digital contact tracing responds to this need and may overcome the problems mentioned above (Ferretti et al., 2020). Digital contact tracing uses a variety of technologies such as, location-based services, geospatial technologies, proximity awareness technology, machine learning algorithms, and automated decision making to scrutinize individual’s digital footprint and trace those who are potentially infected, locate their close contacts and enforce specific health protocols or social distancing (Calvo, Deterding, & Ryan, 2020). With digital contact tracing, many of the logistic challenges of massive contact tracing following the traditional approach are eased (Aleta, Martín-Corral, & Piontti, 2020). Through proximity awareness technology, mobile apps, and in some case GIS analysis and mapping (Geographical Information Systems), digital contact tracing decreases the response time compared to manual tracing, allowing for quicker tracing of individuals exposed to the virus. Therefore, a rapid assessment of close contacts through digital contact tracing can break the chain of infection earlier, curbing the virus spread (Ferretti et al., 2020). For a more thorough review of digital contact tracing and related apps against COVID-19, one may refer to Gasser, Ienca, Scheibner, Sleigh, and Vayena (2020); Salehinejad, Niakan Kalhori, Hajesmaeel Gohari, Bahaadinbeigy, and Fatehi (2021), or Fagherazzi, Goetzinger, Rashid, Aguayo, and Huiart (2020).
1.2. Research gaps and contribution of this review
Despite the initial enthusiasm for novel technologies to contain COVID-19, especially in the spring of 2020, there is no widespread integration of digital contact tracing strategies within governmental response plans across the world. Current digital tracing endeavors portray heterogeneities on preferred system architecture (i.e., decentralized vs. centralized) (Gasser et al., 2020), proximity or location awareness technologies (i.e., Bluetooth vs. GPS) (Rosenkrantz, Schuurman, Bell, & Amram, 2020), and data privacy (privacy first vs. public safety first) (Cohen, Gostin, & Weitzner, 2020), while their overall usefulness and effectiveness are debated (Braithwaite et al., 2020). Therefore, a systematic review is needed to summarize the key findings of digital contact tracing-related studies
Currently, there are two reviews on a similar subject (Anglemyer, Moore, & Parker, 2020; Braithwaite et al., 2020). The first review studied automated, and non-automated contact tracing approaches applied for COVID-19, SARS, MERS, influenza, and Ebola published up to April 14, 2020 (Braithwaite et al., 2020). The second review studied digital contact tracing in various epidemics (Anglemyer et al., 2020). Only four papers are related to COVID-19, out of which two report the impact of digital contact tracing on the Reff. Hence, conclusions are difficult to be drawn.
The above two reviews offer a valuable understanding of multiple aspects of digital contact tracing. Yet, they fail to address some critical questions in the context of a systematic literature review, which can be attributed to the early analysis of a limited number of studies published up to May 5, 2020. First, they do not study whether digital contact tracing reduces the effective reproductive number (Reff). The Reff represents the average number of secondary cases generated by a single infection case and is one of the most important metrics to monitor an epidemic (Flaxman et al., 2020). A value of Reff under one would indicate that the epidemic is controlled. As Reff is a measure of virus transmission in the community, it is widely used to assess the effectiveness of pharmaceutical and non-pharmaceutical interventions over time (Flaxman et al., 2020). On this account, interventions like digital contact tracing, are commonly evaluated based on their ability to drop the Reff metric preferrable below one. Current reviews neglect to study this aspect.
Second, there is a gap in comparing manual contact tracing to digital contact tracing. Only one study has been reported in previous reviews that compared digital to manual contact tracing effectiveness for COVID-19 (Kucharski, Klepac, & Edmunds, 2020). Third, as underlined by Braithwaite et al. (2020), there is a gap in studying how technology affects data privacy, community uptake, and the overall effectiveness of digital contact tracing. Although the above questions have been studied from individual studies, a systematic literature review that summarizes the findings is missing.
This work aims to fill these gaps by systematically reviewing digital contact tracing papers for controlling COVID-19 from January 1, 2020, to March 31, 2021. The contributions of this paper are threefold:
-
•
First, opposed to existing studies that analyze the number of contacts identified through digital contact tracing (Braithwaite et al., 2020), we focus on the actual effect of digital contact tracing on reducing the effective reproductive number, or the number of infected individuals, an outcome extremely important for drawing related health policies. Hence, our review includes studies that numerically present the reduction in the Reff or the number of infections. We also report this finding in relation to contact tracing app uptake (percentage of people using the app) and we search for functional relations between app uptake and the effectiveness of digital contact tracing. Braithwaite et al. (2020) reported one study that compared digital to manual contact. Here, we report eight studies that compare digital to manual tracing. This provides a better understanding of which strategy outperforms the other.
-
•
Second, manual contact tracing is compared to digital contact regarding their ability to reduce the Reff or the number of infected cases. At least to our knowledge, this is the first time of such comparison in a systematic review for COVID-19.
-
•
Third, we respond to another research gap as underlined by Braithwaite et al. (2020): how technology affects digital contact tracing effectiveness. Specifically, we also analyze how the system architecture (i.e., centralized vs. decentralized) may affect data privacy and subsequently the community uptake. We also examine the suitability of proximity awareness sensors, from the perspective of proximity and location accuracy, across different spaces as this has a direct impact on the effectiveness of digital contact tracing. Low proximity/location accuracy may lead to false alerts and exposure notifications. Such an aspect of the problem has not been considered in previous reviews.
In conclusion, early reviews evaluating digital contact tracing did not consider the quantitative impact of digital contact tracing in reducing either the Reff or the number of cases infected. Other essential features were neglected, such as how the proximity awareness technology infers inaccuracies in contact tracing and potential infringement of privacy. By evaluating the necessity, effectiveness, proximity/location accuracy, and personal data privacy concerns of such systems, this review offers vital information that can support decision making and guide future contact tracing endeavors.
2. Methods
2.1. Research objectives
This review attempts to assess the effect of digital contact tracing and balance the potential technological and ethical concerns in containing COVID-19. Specifically, the review analyzes a set of studies to provide evidence on:
-
•
The effect of digital contact tracing in reducing the effective reproductive number (Reff) or the number of COVID-19 infections
-
•
The necessary contact-tracing app adoption rate by the population to ensure control of the epidemic (Reff<1)
-
•
The functional relation, if any, between the contact-tracing app uptake by the public and the effectiveness of digital contact tracing
-
•
Whether digital contact tracing is more effective (decreasing Reff or the number if infections more) than manual contact tracing
-
•
How technical aspects such as the system architecture or the proximity/location accuracy affect data privacy, community uptake, and the overall effectiveness of digital contact tracing.
2.2. Eligibility criteria
We considered studies that reported a direct effect on mitigating the epidemic. Specifically, we only included studies that reported either the reduction in the effective reproductive number Reff (average number of secondary cases generated by a single infection case) or the reduction in the number of infections.
Studies that did not report any numerical effect of digital contact tracing in mitigating the epidemic or were purely qualitative, were excluded. We also excluded papers that focus on the ethical and privacy concerns of digital contact tracing from a conceptual perspective only. We did not compare digital contact tracing to all potential combinations with other interventions, such as isolation, social distancing, and quarantine. Currently, many countries have developed various types of digital contact-tracing apps. We do not review such apps. For a more thorough presentation of such systems, one may refer to Salehinejad et al. (2021) and Skoll, Miller, and Saxon (2020)). This paper is not a review of the limitations of digital or manual contact tracing strategies, although we discuss some of them. Further evaluation of security and privacy considerations related to hardware (i.e., data servers, firewalls) and software used (i.e., operating system) are beyond the scope of this review, but readers may refer to Nguyen et al. (2020) for a recent review. All reviewed manuscripts were in English.
2.3. Search strategy and study selection
Similar to others (Braithwaite et al., 2020), we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol. The PRISMA protocol has been the standard way of reporting systematic reviews and meta-analysis of studies evaluating the effects of interventions (Moher, Liberati, Tetzlaff, & Altman, 2009; refer to Supplementary Table S1 for the PRISMA statement). Further reading on other protocols used for systematic reviews and their comparisons is provided by Booth et al. (2020).
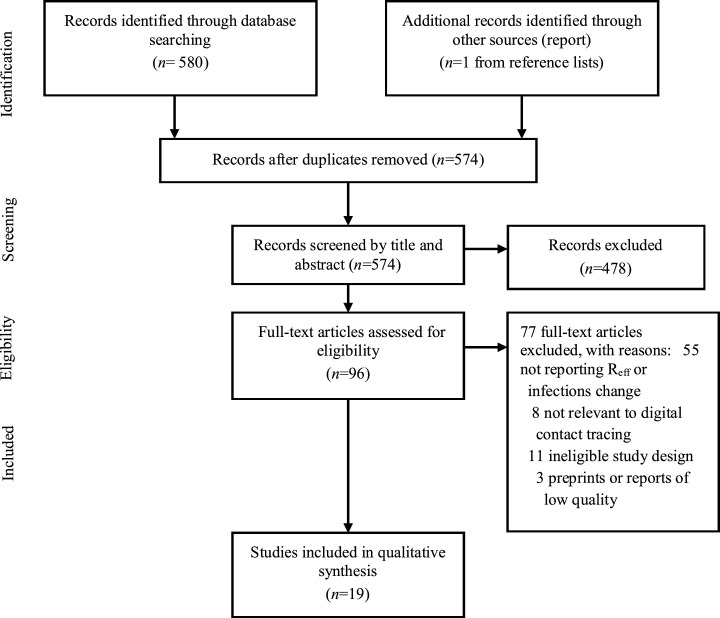
We searched PubMed, bioRxiv, medRxiv, and arXiv for articles published between January 1, 2020, and March 31, 2021. Search terms included “SARS-CoV-2” OR “COVID-19” AND “digital contact tracing” OR “automated contact tracing” OR “smartphone.” The complete query (with additional keywords) used to search the databases is presented in Supplementary Text S1. A total of 580 papers were retrieved (Fig. 1 ). The screening process was conducted independently by two authors and any disagreements were discussed. The initial screening of the titles and abstracts, and exclusion of duplicates, yielded 96 papers. The full text of these papers was meticulously reviewed. Those not meeting the primary criteria (i.e., reporting reduction either in Reff or the number of infected cases resulting from digital contact tracing) were excluded. A final set of 19 papers was used for qualitative synthesis. Due to the high heterogeneity in the studies design, variations in technologies, and outputs, no meta-analysis has been conducted. For this reason, we synthesized study findings narratively.
Fig. 1.
PRISMA flowchart.
2.4. Data extraction
Data were extracted manually using a Microsoft Excel spreadsheet. The following data were collected: year, authors, study sample, system architecture, proximity/location awareness technology used, proximity/location accuracy, data privacy risks, app uptake, Reff change for digital contact tracing, Reff change for manual contact tracing, infections change for digital contact tracing, infections change for manual contact tracing, description of the intervention.
2.5. Risk of bias
The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement was used to assess the quality of the studies included in this review and reduce the risk of bias, an additional checkpoint of the PRISMA protocol (Husereau et al., 2020). The CHEERS statement aims to evaluate the quality of modelling studies related to health interventions and has been used in other systematic reviews (Braithwaite et al., 2020). Questions 1,6-7,9-17 and 22-25 from this statement were omitted here as they refer to the economic output of a study, and were not relevant to the modeling studies included in this review (refer to Supplementary Table S2 for the CHEERS summary). The assessment of risk of bias was conducted by the authors independently, and any conflicting opinions were resolved through discussion.
3. Results
We identified 19 papers on digital contact tracing, all of which were modeling studies (Table 1 ). Similar to others (Braithwaite et al., 2020), and due to this research topic’s high importance and timeliness, we included five preprints, while the rest fourteen papers have been peer-reviewed. The results vary significantly across studies, as different modeling and scenario settings are applied.
Table 1.
Papers studied and outcomes of interest
| Study | Data | Arch/re | Tech/ogy | Privacy risks | App |
Reff / Infections |
Key finding | |
|---|---|---|---|---|---|---|---|---|
| Uptake | Digital | Manual | ||||||
| Abueg et al. (2021) | USA | Not reported | Not reported | Not examined | 75% | 73-79% reduction in infections | 30% more infections compared to digital | 50% fewer infections for digital and manual combined |
| Almagor and Picascia (2020) | 103,000 agents from 2011 UK Census | Not reported | Not reported | Not examined | 80% | 89% reduction in cases at the peal of the epidemic | Not reported | Digital contact tracing can contribute to reducing infection rates when accompanied by a sufficient testing capacity |
| Barrat et al. (2020) | Copenhagen Networks Study | Decentralized | BLE | Not examined | 60% | 36% reduction in epidemic size | 60% reduction in epidemic size only with manual tracing | Digital and manual combined leads to an 80% reduction in the epidemic size |
| Bradshaw et al. (2021) | Hypothetical population | Decentralized | Not reported | Not examined | 90% | Reff reduction close to 1 | Reff reduction close to 1 | Digital exposure notification alone is unlikely to control the epidemic |
| Bulchandani et al. (2020) | Hypothetical population | Not reported | Not reported | Not examined | 75%-95% | Reff <1 | Not reported | Digital immunity is possible with uptake of 75%-95% |
| Currie et al. (2020) | Australia COVIDSafe app | Centralised | BLE | Examined | 61% | 50% less infected | Not reported | COVIDSafe app an important tool adjunct to testing and social distancing |
| Ferretti et al. (2020) | 40 source-recipient pairs | Decentralized | BLE | Not examined | High | Reff <1 | Reff cannot get below 1 for a 3-day delay | A three-day delay assumed in manual tracing leads to an out of control epidemic |
| Hinch et al. (2020) | 1 million/UK | Decentralized | BLE | Not examined | 56% | Reff <1 | Not reported | High rates of app uptake lead to epidemic containment. |
| Kim and Paul (2021) | Hypothetical population | Not reported | Not reported | Not examined | High | Able to reduce infections if uptake is high | Not reported | Uptake rate has a quadratic relationship with digital contact tracing effectiveness |
| Kretzschmar and Rozhnova (2020) | Polymod study for the Netherlands | Not reported | Not reported | Not examined | 20% | 17.6% reduction in Reff | 2.5% reduction in Reff | Digital more effective than manual tracing even with low uptake |
| Kucharski et al. (2020) | 40,162 individuals/UK | Not reported | Not reported | Not examined | 53% | 47% reduction in Reff | 64% reduction in Reff | 66% reduction for manual and digital combined |
| López et al. (2021) | Demographic social-contact data/France | Not reported | Not reported | Not examined | 60% | 67% decrease at peak incidents | Not reported | For R0>2, digital contact tracing alone can not control the epidemic |
| Nakamoto et al. (2020) | Japan/ COCOA app Japan |
Decentralized | BLE | Examined | 90% | Reff <1 | Not reported | Data privacy first |
| Nuzzo et al. (2020) | Hypothetical population | Not reported | Not reported | Not examined | 50% | 90% decease in peak number of infections | Not reported | Digital contact tracing successfully mitigates infection spread |
| Plank et al. (2020) | Hypothetical population | Centralized | BLE | Not examined | 80% | Reff reduction from 2.4 to 1.46 | Manual contact tracing alone reduction from 2.4 to 1.5 | Reff reduced from 2.4 to 1.12 for digital and manual combined |
| b) | Hypothetical population | Decentralized | BLE | Not examined | 80% | Not reported | Not reported | Reff reduced from 2.4 to 1.40 for digital and manual combined |
| c) | Hypothetical population | Not reported | QR | Not examined | 80% | Not reported | Not reported | Reff reduced from 2.4 to 1.41 for digital and manual combined |
| Pollmann et al. (2020) | Hypothetical population | Not reported | BLE | Not examined | 90% | Reff <1 | Not reported | Random testing and social distancing necessary to push Reff below 1 |
| Wilmink et al. (2020) | Hypothetical population in nursing homes | Centralized | Wearable device/ BLE Beacons | Not examined | 100% | 12% fewer infections compared to manual | Digital contact tracing essential for nursing homes and long-term care facilities | |
| Xia and Lee (2020) | Hypothetical population | Decentralized | Wearable BLE |
Examined | >90% | Reff <1 | Not reported | Uptake between 90%-95% to return to full normalcy |
| Yasaka et al. (2020) | Hypothetical population | Centralized and peer to peer | QR | Examined | 25% | 25% fewer infections compared to zero uptake | Not reported | Even a low adoption of 25% contributes to lower transmissions |
Note: BLE = Bluetooth, QR = Quick Response, Reff =effective reproductive number, APP = mobile application
3.1. Digital contact tracing effect on the number of infections and Reff
Nine studies reported the effect of digital contact tracing on the number of infections. Abueg et al. (2021) reported that if a digital tracing app is used by 75% of the population, the number of infections is reduced by 73–79%. Another study showed that an 80% uptake leads to 89% reduction in cases at the peak of the epidemic (Almagor & Picascia, 2020), while Barrat, Cattuto, Kivelä, Lehmann, & Saramäki (2020) revealed that a 60% uptake produces a 36% reduction in epidemic size. Further, COVIDSafe, an existing tracing app created by the Australian government, was assessed for its effectiveness (Currie, Peng, Jameson, Frommer, & Lyle, 2020). The model indicated that a 61% uptake of the app would reduce the total number of new cases by almost 50%. Another study estimated that a 50% adoption rate of digital contact tracing results in a 90% decrease in the peak number of infections (Nuzzo et al., 2020). López et al. (2021) calibrated an agent-based model on the French population integrating demographic and social-contact data simulated how digital contact tracing impacted COVID-19 transmission. Assuming Reff = 2.6, digital tracing at a 60% adoption rate would produce a 67% reduction in peak incidence. Finally, Wilmink, Summer, and Marsyla (2020)) reported 12% fewer infections for 100% uptake. This study refers to nursing homes and long-term care facilities, and population uptake refers only to personnel, residents, and visitors. Meanwhile, the former studies used different metrics to assess the epidemic containment due to digital contact tracing (i.e., total infections, new infections, peak infections), and the results are not comparable. However, they provide evidence that a high uptake leads to the mitigation of the epidemic.
Another four studies reported a decrease in Reff at various uptake levels (Bradshaw, Alley, Huggins, Lloyd, & Esvelt, 2021; Kretzschmar & Rozhnova, 2020; Kucharski et al., 2020; Plank et al., 2020). With an uptake value ranging from 20% to 90%, a reduction in Reff was estimated between 17.6% and 47%. An additional set of seven papers also reported that digital contact tracing could reduce Reff below one under various uptake values and are presented in the following section.
3.2. Minimum uptake to control the epidemic
A critical question from both a policy and a feasibility perspective is how many people should use a digital contact tracing app to control the epidemic. For this reason, we searched if a specific threshold value in uptake would be necessary to reduce Reff to less than one, that is, to control the epidemic (excluding manual tracing, but including isolation of contacts and quarantine of infected people). One study called this as “digital herd immunity” to emphasize the transition to the smartphone era (Bulchandani, Shivam, Moudgalya, & Sondhi, 2020). Digital herd immunity is defined as a population that “can be immune to epidemics even if not a single one of its members is immune to the disease.” According to this work, digital immunity is possible due to smartphone capabilities, regardless of the share of non-symptomatic transmission. To achieve digital herd immunity, the fraction of the population that needs to use a contact tracing app ranges between 75% and 95% for R0 = 3 (basic reproductive number). For smaller R0 values resulting from social distancing or other interventions, this fraction further decreases. Five additional studies also converged to a nearly 90% uptake needed to control the epidemic (Bradshaw et al., 2021; Kucharski et al., 2020; Nakamoto, Jiang, & Zhang, 2020; Pollmann, Pollmann, & Wiesinger, 2020; Xia & Lee, 2020). Finally, Hinch, Probert, and Nurtay (2020)) estimated that an epidemic could be suppressed if 80% of smartphone owners (corresponding to 56% of the overall population) use the app.
3.3. Relation between app uptake level and effectiveness
Four studies quantified the relation between the effectiveness of digital contact and mitigating COVID-19. Kim and Paul (2021) defined the effectiveness of digital contact tracing as the ratio of the number of individuals notified to the minimum number that should be notified to control the epidemic. Under specific assumptions, digital contact tracing effectiveness drops drastically, having a quadratic relation to the population uptake rate. For example, a 70% uptake will result in 49% effectiveness, while 50% uptake will result in a 25% effectiveness. Consequently, for digital contact tracing to succeed, most of the population should enroll. A similar finding was reported in another study, which identified that the reduction in the epidemic size grows quadratically with the app adoption uptake (Barrat et al., 2020). This may be attributed to the fact that the infected case and the contacts need to use the app. Based on this fact, Kucharski et al. (2020) found a quadratic relation between uptake and Reff reduction. However, Hinch et al. (2020) reported a nearly linear relation between the cumulative deaths and app usage. This nearly linear dependence is explained by the combined effect of two non-linear effects in opposite directions: the quadratic proportion of contacts that use the app and the non-linear relation of epidemic size to R0 (Hinch et al., 2020).
3.4. Comparing digital and manual contact tracing
The studies in the previous section presented convincing evidence that digital contact tracing can reduce the epidemic spread at various levels depending on the uptake rate and even control it, if the uptake surpasses the 90% threshold level. Nonetheless, this conclusion is based on the modeling assumption that no manual contact tracing is conducted concurrently. Hence, there is no direct comparison between the effectiveness of digital-to-manual contact tracing. We identified eight studies that compared digital contact tracing to manual contact tracing (a detailed description of these studies is given in Supplementary Table S3). However, they draw contradictory outcomes on whether digital contact tracing is better than manual tracing.
Of the eight papers, four reported that digital contact tracing alone (i.e., without manual tracing) reduces significantly infections or Reff more than manual tracing (Abueg et al., 2021; Ferretti et al., 2020; Kretzschmar & Rozhnova, 2020; Wilmink et al., 2020), and two reported only a marginal improvement of Reff (Bradshaw et al., 2021; Plank et al., 2020). For example, without manual contact tracing, digital tracing reduces Reff from 2.4 to 1.46, while manual contact tracing (in the absence of digital) reduces Reff to 1.5 (Plank et al., 2020). On the other hand, two out of eight papers reported that manual contact tracing reduces Reff or infections more than digital tracing alone (Barrat et al., 2020; Kucharski et al., 2020). For instance, Barrat et al. (2020) estimated a nearly double reduction in the epidemic size with manual contact tracing (60%) compared to digital (36%), while Kucharski et al. (2020) reported a 64% reduction in Reff attributed only to manual tracing and 47% reduction if only digital tracing was applied. The above heterogeneous outcomes indicate that more evidence is needed to decide on the effectiveness of each strategy when applied alone.
Furthermore, we searched for studies that assessed the combined effect of manual and digital contact tracing on either Reff or the number of infections. One study showed that both policies combined reduced new infections by 50% (Abueg et al., 2021). Another study showed that manual and digital tracing combined, at the same 60% coverage/uptake level, would result in a nearly 80% reduction in the epidemic size (Barrat et al., 2020). This is a significant improvement compared to a 60% reduction if only manual tracing is applied, or 36% if digital contact tracing is the only tracing policy. One study showed that, with manual and digital tracing combined (uptake of 80%), Reff decreased from 2.4 to 1.12 (Plank et al., 2020). Bradshaw et al. (2021) showed that the hybrid use of manual contact tracing with bidirectional digital tracing, assuming 80% population uptake, led to an additional 0.26 lower Reff. Finally, Kucharski et al. (2020) estimated only a slight improvement (from 64% to 66% Reff reduction) of manual tracing once digital contact tracing was added.
3.5. System architecture, proximity awareness technology, and privacy
Ten out of the 19 papers reported information about the system architecture and the proximity/location awareness technology used. There are two main system architecture approaches in digital contact tracing: centralized and decentralized (Cohen et al., 2020). The centralized approach, reported in four papers in this review (Currie et al., 2020; Plank et al., 2020; Wilmink et al., 2020; Yasaka, Lehrich, & Sahyouni, 2020), is a top-down architecture where data are collected from the smartphone through an app and are stored at a central remote server. Therefore, the centralized approach has been criticized for potential privacy infringement (Cohen et al., 2020). Data are analyzed, and in the case of a confirmed case, all close contacts are notified to take specific actions (e.g., self-isolate). The decentralized approach is a bottom-up architecture and was reported in six papers (Barrat et al., 2020; Currie et al., 2020; Ferretti et al., 2020; Hinch et al., 2020; Nakamoto et al., 2020; Plank et al., 2020). The user has control over the data and decides whether they will be uploaded to a central server. Although this approach is less privacy-invasive, it struggles to ensure that sufficient data will be collected for successful contact tracing (Gasser et al., 2020).
In both architectures, proximity and location awareness technologies offer a set of tools to survey an individual’s movement. Global Navigation Satellite Systems (GNSS), is a location awareness technology as it provides the geographic location of the user. WiFi, Bluetooth Low Energy (BLE), Beacons, or Quick Response (QR) codes collect proximity data. In other words, proximity-based approaches directly detect nearby smartphones (or other devices) and not the exact geographic location (Abueg et al., 2021). However, under specific system architectural settings and calculations, proximity awareness technologies can also provide the location of an individual (see Table 2 ). Data are then analyzed in anticipation of rapid tracing of secondary virus cases, thus enforcing specific health protocols to mitigate the spread of the virus (see Supplementary Table S4 for a description of proximity awareness technologies).
Table 2.
Proximity/Location awareness technologies for COVID-19 digital contact tracing
| Technology | Location/ Proximity Accuracy |
COVID-19 tracing |
Privacy Concerns | ||
|---|---|---|---|---|---|
| Outdoors | Indoors | Suitable for | Unsuitable for | ||
| GNSS | 10 m GPS only, 5 m GPS + WiFi |
Most likely not operating | Outdoors / Tracking overlapping routes / Detection of hotspots | Indoors | High |
| BLE | <2 m | <2 m | Tracing individuals within 2 meters | Spaces with airborne transmission of SARS-CoV-2 | Low |
| Beacons | Building level | Room/floor level | Same room/ floor/building | Assessing the distance between individuals | Low |
| QR | Building level | Room/floor level | Same room/ floor/building | Assessing the distance between individuals | Moderate to high |
| WiFi | Depending on Access Points | <1m | Indoors | Outdoors | Low |
| UWB | Depending on UWB transmitters | <0.5 m | Indoors | Currently, few smartphones have this technology | Low |
This review found that BLE is the most widely used technology matched to a decentralized architecture (Barrat et al., 2020; Currie et al., 2020; Ferretti et al., 2020; Hinch et al., 2020; Nakamoto et al., 2020; Plank et al., 2020; Pollmann et al., 2020; Xia & Lee, 2020). Wilmink et al. (2020) coupled beacons with wearables. Following a centralized architecture, real-time location data are uploaded to cloud-based software to visualize egocentric contact networks. This system is suitable for indoor environments, such as nursing homes. The results show that this technology could reduce infections by more than 12% compared to manual tracing. Another work emphasizes privacy issues, and therefore the proposed app does not use personal or location data (Yasaka et al., 2020). Users should create “checkpoints” by scanning QR codes whenever they meet other people, either in public or private. In the case of infection, users should anonymously self-report their health status to the network.
It is worth mentioning that only one paper modelled different combinations of alternative digital contact tracing system architectures with varying proximity awareness technologies (Plank et al., 2020). A centralized BLE approach was compared to a decentralized BLE approach, and a QR code exposure notification system. Only the effect of the combined use of manual and digital contact tracing at an 80% uptake was assessed. The centralized BLE approach reduced Reff to 1.1, nearly succeeding in containing the epidemic. The other two approaches (i.e., decentralized BLE approach, and a QR code exposure notification system) reduced Reff to 1.4, a significant difference when compared to the centralized BLE approach.
Privacy considerations were examined in four studies (Currie et al., 2020; Nakamoto et al., 2020; Xia & Lee, 2020; Yasaka et al., 2020). For the COVIDSafe app, the Australian government used a centralized architecture. However, it maximized data security with legislation restricting data transfer, storage, use, and disposal (Currie et al., 2020). Only one study prioritized the privacy protection of users (Nakamoto et al., 2020). In this study, a peer-to-peer framework was developed for the COCOA app to provide individuals with reliable updates of COVID-19 without exposing their private data. Xia and Lee (2020) proposed a stand-alone device, called “contact recorder”, specifically designed for contact tracing. A contact recorder, equipped with BLE technology, would be easier to preserve data privacy as it would store only data related to proximity and health status, minimizing thus privacy infringement. Lastly, Yasaka et al. (2020) used an anonymized graph of interpersonal interactions through a specifically designed privacy-preserving smartphone app that implements peer-to-peer contact tracing through the use of QR codes.
3.6. Quality assessment
The quality assessment of the 19 papers of this review varied considerably and is presented in Supplementary Table S2. All studies clearly defined their objectives, summarized the key findings, and discussed their limitations. Most of the studies sufficiently presented the applied models, and the related assumptions and parameters. However, some studies reported briefly or not at all the choice of the model (Nakamoto et al., 2020; Nuzzo et al., 2020), the model assumptions (Currie et al., 2020; Nakamoto et al., 2020; Nuzzo et al., 2020), the study parameters (Barrat et al., 2020; Currie et al., 2020; Kim & Paul, 2021; Nakamoto et al., 2020; Nuzzo et al., 2020; Yasaka et al., 2020). Some studies did not describe the characteristics of the base-case population (Bradshaw et al., 2021; Bulchandani et al., 2020; Currie et al., 2020; Ferretti et al., 2020; Kim & Paul, 2021; Kretzschmar & Rozhnova, 2020; Nakamoto et al., 2020; Nuzzo et al., 2020; Plank et al., 2020; Pollmann et al., 2020; Wilmink et al., 2020; Xia & Lee, 2020; Yasaka et al., 2020), while other studies described in a limited way the analytical methods that supported the evaluation of the results (Currie et al., 2020; Kim & Paul, 2021; Kretzschmar & Rozhnova, 2020; Nuzzo et al., 2020; Plank et al., 2020; Wilmink et al., 2020; Yasaka et al., 2020).
4. Discussion
Here we discuss the lessons learned from the 19 papers presented in the previous section. Identified gaps and related suggestions are highlighted to guide future contact tracing research and implementation.
4.1. Lesson 1. Digital contact tracing can mitigate COVID-19 if population uptake is substantial
All studies (19/19) in this review show that digital contact tracing reduces the Reff and the number of infected cases. However, its effectiveness exhibits a quadratic dependence from the uptake rate (Barrat et al., 2020; Kim & Paul, 2021). This implies that a considerable value in app adoption is needed for digital contact tracing to be effective on its own. Most studies of this review converged to the same uptake rate of at least 90% (in the absence of manual contact tracing) to control the epidemic (drop Reff below one). This finding is in agreement with other works that consider a broad uptake in the population as the key for digital contact tracing success (Munzert, Selb, Gohdes, Stoetzer, & Lowe, 2021).
In practice, it is tough to achieve such a high level of community uptake (Watts, 2020). However, a low adoption rate may still have a positive epidemiological impact. As shown in this review, even with low adoption rates the Reff and the number of infections decrease. Other empirical studies have confirmed this finding. For example, a study in Spain showed that a 33% app uptake, could significantly reduce infections (Rodríguez et al., 2021). The drawback is that individuals may gain a false sense of security at a low uptake level if they do not receive exposure notifications, which may encourage a more relaxed behaviour (i.e., not following social distancing measures) (Kim & Paul, 2021). However, the notifications’ absence could be attributed to the low uptake, not that individuals with COVID-19 have not crossed their pathways. For this reason, statistics should be summarized at small geographical units, creating GIS COVID-19 risk assessment maps that would be readily available to policymakers and users (Grekousis, 2020). This, underscores that accurate and updated content through the app and the subsequent spatial analysis of the identified patterns is crucial for people to align their behaviour (i.e., adhere to social distancing) with the actual epidemic severity.
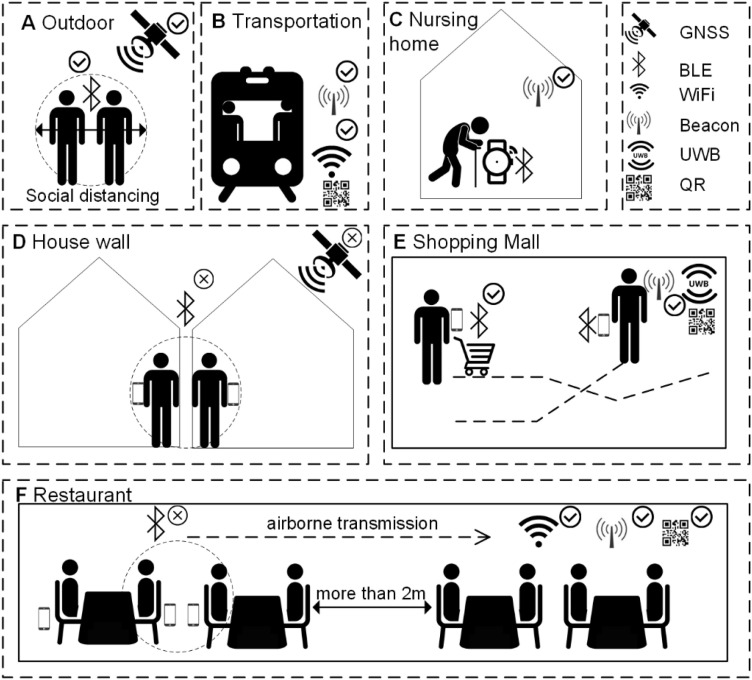
The benefits of digital contact tracing can be applied to subpopulations even if the uptake rate is low at the general population. For example, digital contact tracing apps would have greater epidemiological importance for older age groups. Yet, older people are less inclined to technology due to the phenomenon of technological exclusion (Watts, 2020). As such, they are less likely to download or systematically use a digital contact tracing app through their smartphone, something that has been already observed in many parts of the world, as for example, the UK and Singapore (Huang, Guo, Lim, & Chow, 2021; Watts, 2020). In this case, wearable devices could be used instead of smartphones to make digital contact tracing approachable to older persons. In nursing homes or long-term care facilities, with a COVID-19 mortality rate of nearly 25% among the elders, the need for specifically designed digital contact tracing systems is even higher (Wilmink et al., 2020). We argue that in closed structures with controlled access and high surveillance, such as nursery homes, or health care facilities digital contact tracing based on high location accuracy technologies (i.e.., beacons, UWB) integrated with wearable devices should be prioritized (Fig. 2 C).
Fig. 2.
Proximity/location awareness technologies for digital contact tracing in various environments. A) GNSS (belongs to location awareness technologies) tracks the location in outdoor environments (i.e. park). BLE can be used for proximity sensing but not for identifying the exact location. B) Beacons, WiFi, or QR code can be used on subway, buses, or other modes of transport. C) Wearables, coupled with beacons, are efficient for nursing homes and other closed structures. D) BLE may provide a false exposure notification for individuals separated by a wall. GNSS is hard to operate indoors. E) UWB can identify crossing pathways in indoor environments, while beacons and QR codes can provide proximity accuracy at the room level. F) Depending on smartphone’s placement and orientation, BLE can identify as close contacts those sitting back-to-back and miss those at the same table. For indoor airborne transmission of the virus, WiFi, beacons, and QR are sufficient.
4.2. Lesson 2. Digital contact tracing should be used in combination with manual contact tracing
This review examines another critical question: Is digital contact tracing more effective than manual contact tracing if used as the single tracing strategy? There is no consensus among this review’s studies on whether digital is more effective than manual contact tracing. Of the eight papers that compared manual to digital contact tracing, four reported that digital is better than manual, two reported only marginal gains of digital tracing, and two papers that manual is more effective than digital contact tracing. These contradictive conclusions suggest that more research is needed to establish the superiority, if any, of one tracing strategy over the other (Abueg et al., 2021; Ferretti et al., 2020). Given that digital contact tracing achieves a satisfactory reduction in Reff only at high uptake rates, we argue that excluding manual tracing is not rational for the time being. Other empirical studies also support this conclusion. For example, Lai, Tang, Kurup, and Thevendran (2021))_showed that although various digital contact tracing apps (i.e., SafeEntry and TraceTogether) helped in contact tracing in Singapore, they were not sufficient to replace manual contact tracing conducted by experienced personnel. Similar to others, we suggest the combined use of these strategies to maximize the benefits (Barrat et al., 2020; Kucharski et al., 2020). This is also highlighted in four studies of this review that assessed that the joint effect of these strategies could reduce infections by 50% and reduce Reff down to 1.1, very close to the critical value below which the epidemic enters a controlled phase.
4.3. Lesson 3. Proximity/location accuracy of digital contact tracing app varies across different built environments and facilities
Proximity/location awareness technologies are not suitable for every space or facility, something rarely mentioned in the modeling studies of this review. Almost half (9/19) of the studies did not report any technical characteristics, a severe shortcoming to their modeling outcomes. Moreover, no study reported how the proximity/location accuracy may affect the effectiveness of digital contact tracing, a significant literature gap. However, the digital contact tracing efficiency is directly linked to how the proximity is determined and how data are retrieved, processed, and stored (Silva et al., 2021). On this account, more focus should be placed on the joint analysis of the technological and epidemiological components of a digital contact tracing system. Here, we extend the discussion to describe how the proximity/location accuracy of proximity/location awareness technologies varies on different environments and facilities to guide the development of future digital contact tracing systems (Fig. 2 and Table 2).
BLE is the preferred proximity awareness technology applied in 80% (8/10) of the studies that reported information about the system architecture and the proximity awareness technology used. Nevertheless, it comes with accuracy problems when applied in different environments (Table 2) (Nguyen et al., 2020). BLE cannot identify physical barriers between two individuals (i.e., separated by a wall or anti-droplet plexiglass) (Fig. 2D). If one of these individuals is infected, then the second one is likely to be notified and isolated, even when he or she should not. BLE signal strength may vary not only with smartphone orientation but also with its placement (i.e., in the pocket or the hand if its owner) (Zastrow, 2020). Consequently, people sitting at the same table in a restaurant may seem to have less contact than those sitting back to back on a nearby table (Fig. 2F).
Digital contact tracing based on BLE traces contacts within 2 m (Table 2) (Rosenkrantz et al., 2020). However, SARS-CoV-2 also spreads through aerosols’ airborne transmission up to tens of meters (Morawska & Cao, 2020). Hence, contacts within the same room or space cannot be notified if the app is based only on BLE (Xia & Lee, 2020). A centralized architecture could probably handle tracing under such conditions and would easily learn from the collected data. In this manner, the system could modify the criteria to label a contact as exposed, reflecting the new findings of a novel virus and making alerts more precise.
Another approach could combine BLE with Beacons, WiFi access point, or UWB to offer higher proximity accuracy in indoor environments (Fig. 2E,F) (Wilmink et al., 2020). In addition, the use of specifically designed devices, instead of smartphones, may increase the usability and the accuracy of contact tracing. Studies have shown that smart watches with digital contact tracing apps increase the chances that the two devices are in line of sight, while a smartphone usually remains in a pocket or bag (Maccari & Cagno, 2021).
Finally, the GNSS of smartphone malfunctions in indoor environments with a location accuracy of approximately 10 m outdoors (Nguyen et al., 2020). Therefore, GNSS can assist in tracking rather than doing proximity evaluation in the digital contact tracing context (Fig. 2A).
In conclusion, the system architecture and proximity awareness technology are critical and should be considered in the modeling process to assess a digital contact tracing system's effectiveness.
4.4. Lesson 4. The decentralized architecture offers more privacy but it is not as efficient as the centralized architecture
The centralized app-based BLE architecture outperformed the decentralized app-based BLE system and the QR-notification system (Plank et al., 2020). Probably due to governmental advice/order (Fagherazzi et al., 2020), the app adoption rate is generally higher in the centralized architecture than in the decentralized one, but at a privacy cost (Nakamoto et al., 2020). On the other hand, a decentralized approach with voluntary app usage suffers from lower adoption rates potential due to fears of personal data privacy infringement (Ferretti et al., 2020). More similar studies are needed to help policymakers better decide on the most effective system architecture.
4.5. Lesson 5. Personal data privacy is the key for digital contact tracing success
With digital contact tracing critically depending on wide adoption for success, as shown in Lesson 1, governments opting for such a strategy should build a legal and technical framework, ensuring personal data privacy. The MIT Covid Tracing Tracker project reported that by July 30, 2020, 20 out of 31 countries that had officially adopted/supported the use of apps for digital contact tracing had an uptake of less than 8% (O’Neill, Ryan-Mosley, & Johnson, 2020). Surprisingly, an online survey of 5995 participants across five countries (i.e., France, Germany, Italy, the UK, and the US) found a high willingness to download a digital contact tracing app, with an overall acceptance rate of 74.8% (Altmann, Milsom, & Zillessen, 2020). The large gap between the intention to use such an app and the actual uptake is attributed to severe concerns about a) how governments will handle data after the end of the pandemic (42%), and b) cybersecurity (35%) (Altmann et al., 2020).
Balancing the need for epidemiological information with legitimate data privacy is critical (Altmann et al., 2020; Park, Choi, & Ko, 2020). As many concerns are raised regarding technology intervention for an individual’s privacy, a trade-off between protecting public health and retaining personal data control should be found. Most publications in this revew emphasized the importance of data privacy and suggested a decentralized architecture (Barrat et al., 2020; Ferretti et al., 2020; Hinch et al., 2020; Nakamoto et al., 2020; Xia & Lee, 2020). This architecture offers more tools to preserve anonymity and overall data privacy than the centralized approach (Rosenkrantz et al., 2020). However, studies have shown that, even with anonymized data, there are techniques to identify the actual individuals (Rocher, Hendrickx, & de Montjoye, 2019). Consequently, privacy standards should be the highest possible, while data should be kept only for a limited time and automatically deleted (Maccari & Cagno, 2021). Due to ethical and cybersecurity concerns, oversight from an inclusive advisory board is suggested (Ferretti et al., 2020). Studies show that the usefulness of digital tracing is leveraged only in combination with manual tracing, and other interventions such as testing, isolation, and social distancing (Rahmani and Mirmahaleh, 2020). On this account, a privacy infringement is not justified, as digital tracing can be observed only as supplementary to controlling an epidemic. However, as digital contact tracing is a strategy that can be highly effective under specific settings (i.e., closed structures), it involves technological, legal, and ethical issues that should be on top of their architectural designs. Key lessons, research gaps, and suggestions are summarized in Table 3 .
Table 3.
Key lessons learned from this review along with suggestions
| Lessons learned | Suggestions/research gaps | |
|---|---|---|
| Effectiveness | Digital contact tracing can control COVID-19 if the population uptake surpasses 90%. | As a 90% uptake is difficult to be achieved, digital contact tracing should be combined to manual contact tracing. |
| Digital vs. manual | There is no clear evidence that digital contact tracing can substitute manual. | Further research is needed with empirical data. |
| Proximity/location accuracy | Proximity/location accuracy highly varies on the technology used and the indoor or outdoor setting | To avoid false alerts or exposure notifications, the choice of proximity awareness technology should be central when designing a digital contact tracing system. |
| Proximity awareness technology | BLE is preferred. | As proximity accuracy is low with BLE, alternative technologies such as UWB should be promoted. |
| Architecture | Decentralized architecture allows for higher personal data privacy | Architecture should ensure the highest data privacy standards. |
| Privacy | Most studies raise privacy and ethical concerns related to personal data. | The need for epidemiological information should not lead to personal data privacy infringement. Governments should build a legal framework ensuring personal data privacy to gain people’s trust. |
This review has certain limitations. Due to the limited number of available papers that report comparable numerical outputs in the effective reproductive number Reff, or the reduction in infections, no meta-analysis has been conducted although initially planned. No empirical studies are included as none exists. Finally, we limited our search to English literature only.
5. Conclusions
Learning lessons from the current pandemic will be an essential step towards a stronger and more resilient society. This paper contributes towards informing policymakers on some lessons learned regarding digital contact tracing, community uptake, and proximity awareness technology to fight COVID-19 on the following topics/debates:
-
•
the effectiveness (and thus its potential necessity as a policy against COVID-19) of digital contact tracing in reducing Reff,
-
•
the necessary adoption rate (if any) by the public to ensure that digital contact tracing can assist in controlling the pandemic
-
•
the superiority (if any) of the digital contact tracing over the manual contact tracing
-
•
the proximity/location accuracy and privacy concerns raised with digital contact tracing
Policy-wise, the take-home message of this review is that, the success of digital contact tracing depends on a complex interplay of app uptake in the community, proximity awareness technologies, and public’s trust (see also Table 3). If governments consider the barriers that keep away people from adopting tracing apps, and scientists address technical limitations, digital contact tracing could be a successful strategy (Ferretti et al., 2020; Nguyen et al., 2020). It would offer a powerful toolkit for decision makers and the public that could be an essential part of long-term response not only to COVID-19 but also to future epidemics. Even when the COVID-19 pandemic is over, other epidemics will strike (Xia & Lee, 2020). In the wake of a novel pathogen, effective treatments and vaccines will lag behind the virus spread, and other means should be readily available to contain the new disease. Although digital contact tracing does not guarantee epidemic control, it provides technologies that respond quickly, have high location and proximity accuracy, and preserve anonymity.
Digital contact tracing should not only be linked to smartphones as their penetration varies significantly across countries and age groups, with a remarkably low usage among the elderly, the most susceptible to COVID-19 (López et al., 2021). Wearables or other stand-alone devices would ensure high uptake from elders and groups in need (Wilmink et al., 2020; Xia & Lee, 2020). For example, over a billion of the world’s population (15% of the total) lives with some form of disability (World Health Organization, 2018). This number is expected to double by 2050, and the WHO calls for the development of assistive technologies disability (World Health Organization, 2018). For this reason, future innovation should focus on creating stand-alone, smaller, and cheaper wearable devices with low energy consumption. In the case of new outbreaks, wearable devices such as watches or pins could be freely distributed among populations, especially in low-income countries. Along with mass testing, isolation, social distancing, and personal hygiene, a new virus is likely to be contained quickly, minimizing loss of lives, economic and societal costs that threaten sustainability, and allowing for faster and safer return to normality.
Funding
This work was supported the National Natural Science Foundation of China, grant number [41871140]. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.scs.2021.102995.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Abueg M., Hinch R., Wu N., Liu L., Probert W., Wu A., et al. Modeling the effect of exposure notification and non-pharmaceutical interventions on COVID-19 transmission in Washington state. npj Digital Medicine. 2021;4(1):1–10. doi: 10.1038/s41746-021-00422-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleta A., Martín-Corral D., Piontti A.P., et al. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nature Human Behaviour. 2020;4(9):964–971. doi: 10.1038/s41562-020-0931-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almagor J., Picascia S. Exploring the effectiveness of a COVID-19 contact tracing app using an agent-based model. Scientific reports. 2020;10(1) doi: 10.1038/s41598-020-79000-y. Dec 17, 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altmann S., Milsom L., Zillessen H., et al. Acceptability of App-Based Contact Tracing for COVID-19: Cross-Country Survey Study. JMIR mHealth and uHealth. 2020;8(8) doi: 10.2196/19857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglemyer A., Moore T., Parker L., et al. Digital contact tracing technologies in epidemics: a rapid review. Cochrane Database of Systematic Reviews. 2020:8. doi: 10.1002/14651858.CD013699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrat A., Cattuto C., Kivelä M., Lehmann S., Saramäki J. Effect of manual and digital contact tracing on COVID-19 outbreaks: a study on empirical contact data. medRxiv. 2020 doi: 10.1098/rsif.2020.1000. Published on line July 25. https://www.medrxiv.org/content/10.1101/2020.07.24.20159947v1 (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batty M. The Coronavirus crisis: What will the post-pandemic city look like? Environment and Planning B: Urban Analytics and City Science. 2020;47(4):547–552. doi: 10.1177/2399808320926912. [DOI] [Google Scholar]
- Booth A., Mitchell A.S., Mott A., James S., Cockayne S., Gascoyne S., et al. An assessment of the extent to which the contents of PROSPERO records meet the systematic review protocol reporting items in PRISMA-P. F1000Research. 2020;9 doi: 10.12688/f1000research.25181.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradshaw W.J., Alley E.C., Huggins J.H., Lloyd A.L., Esvelt K.M. Bidirectional contact tracing could dramatically improve COVID-19 control. Nature communications. 2021;12(1):1–9. doi: 10.1038/s41467-020-20325-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite I., Callender T., Bullock M., Aldridge R.W. Automated and partly automated contact tracing: a systematic review to inform the control of COVID-19. The Lancet Digital Health. 2020;2(11):e607–e621. doi: 10.1016/S2589-7500(20)30184-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulchandani V.B., Shivam S., Moudgalya S., Sondhi S. Digital herd immunity and COVID-19. ArXiv. 2020 doi: 10.1088/1478-3975/abf5b4. published online April 15. https://arxiv.org/abs/2004.07237 (preprint) [DOI] [PubMed] [Google Scholar]
- Calvo R.A., Deterding S., Ryan R.M. Health surveillance during covid-19 pandemic. BMJ. 2020:369. doi: 10.1136/bmj.m1373. [DOI] [PubMed] [Google Scholar]
- Cohen I.G., Gostin L.O., Weitzner D.J. Digital Smartphone Tracking for COVID-19: Public Health and Civil Liberties in Tension. JAMA. 2020;323(23):2371–2372. doi: 10.1001/jama.2020.8570. [DOI] [PubMed] [Google Scholar]
- Currie D.J., Peng C.Q., Jameson B.A., Frommer M.S., Lyle D.M. Stemming the flow: How much can the Australian smartphone app help to control COVID-19? Public Health Research and Practice. 2020;30(2) doi: 10.17061/phrp3022009. [DOI] [PubMed] [Google Scholar]
- DeLuca, Papageorge N., Mitchel B., Kalish E. 2020. The unequal cost of social distancing.https://coronavirus.jhu.edu/from-our-experts/the-unequal-cost-of-social-distancing Accessed in March 25, 2021, from. [Google Scholar]
- Elavarasan R.M., Pugazhendhi R., Shafiullah G.M., Irfan M., Anvari-Moghaddam A. A hover view over effectual approaches on pandemic management for sustainable cities–The endowment of prospective technologies with revitalization strategies. Sustainable Cities and Society. 2021;68 doi: 10.1016/j.scs.2021.102789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagherazzi G., Goetzinger C., Rashid M.A., Aguayo G.A., Huiart L. Digital health strategies to fight COVID-19 worldwide: challenges, recommendations, and a call for papers. Journal of Medical Internet Research. 2020;22(6) doi: 10.2196/19284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferretti L., Wymant C., Kendall M., et al. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020;368 doi: 10.1126/science.abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaxman S., Mishra S., Gandy A., Unwin H.J.T., Mellan T.A., Coupland H., et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- Fokas A.S., Cuevas-Maraver J., Kevrekidis P.G. A quantitative framework for exploring exit strategies from the COVID-19 lockdown. Chaos, solitons, and fractals. 2020;140 doi: 10.1016/j.chaos.2020.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasser U., Ienca M., Scheibner J., Sleigh J., Vayena E. Digital tools against COVID-19: taxonomy, ethical challenges, and navigation aid. The Lancet Digital Health. 2020;2(8):e425–e434. doi: 10.1016/S2589-7500(20)30137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge X.Y., Pu Y., Liao C.H., Huang W.F., Zeng Q., Zhou H., et al. Evaluation of the exposure risk of SARS-CoV-2 in different hospital environment. Sustainable cities and society. 2020;61 doi: 10.1016/j.scs.2020.102413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grekousis G. Cambridge University Press; Cambridge, UK: 2020. Spatial analysis methods and practice: Describe, Explore Explain, through GIS. [Google Scholar]
- Hellewell J., Abbott S., Gimma A., et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8:e488–96. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinch R., Probert W., Nurtay A., et al. 2020. Effective configurations of a digital contact tracing app: a report to NHSX.https://github.com/BDI-pathogens/covid-19_instant_tracing (Accessed April 15, 2020) [Google Scholar]
- Huang Z., Guo H., Lim H.Y., Chow A. Awareness, acceptance, and adoption of the national digital contact tracing tool post COVID-19 lockdown among visitors to a public hospital in Singapore. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2021 doi: 10.1016/j.cmi.2021.01.007. S1198-743X(21)00033-1. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husereau D., Drummond M., Petrou S., Carswell C., Moher D., Greenberg D., et al. 2020. CHEERS Task Force. Consolidated health economic evaluation reporting standards (CHEERS) [DOI] [PubMed] [Google Scholar]
- International Monetary Fund . 2020. A year like no other. IMF Annual report 2020.https://www.imf.org/external/pubs/ft/ar/2020/eng/downloads/imf-annual-report-2020.pdf (Accessed at March 29, 2021) from. [Google Scholar]
- Jadidi M., Jamshidiha S., Masroori I., Moslemi, Mohammadi A., Pourahmadi V. A two-step vaccination technique to limit COVID-19 spread using mobile data. Sustainable Cities and Society. 2021;70 doi: 10.1016/j.scs.2021.102886. 2021, ISSN 2210-6707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H., Paul A. Automated contact tracing: a game of big numbers in the time of COVID-19. Journal of the Royal Society Interface. 2021;18(175) doi: 10.1098/rsif.2020.0954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kretzschmar M.E., Rozhnova G. Bootsma MCJ, van Boven M, van de Wijgert JHHM, Bonten MJM. Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. The Lancet Public Health. 2020;5(8):e452–e459. doi: 10.1016/S2468-2667(20)30157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucharski A.J., Klepac P., Edmunds W.J., et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. The Lancet Infectious Diseases. 2020;20(10):1151–1160. doi: 10.1016/S1473-3099(20)30457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai S.H.S., Tang C.Q.Y., Kurup A., Thevendran G. The experience of contact tracing in Singapore in the control of COVID-19: highlighting the use of digital technology. International orthopaedics. 2021;45(1):65–69. doi: 10.1007/s00264-020-04646-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López J.A.M., García B.A., Bentkowski P., Bioglio L., Pinotti F., Boëlle P.Y., et al. Anatomy of digital contact tracing: role of age, transmission setting, adoption and case detection. Science advances. 2021 doi: 10.1126/sciadv.abd8750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maccari L., Cagno V. Do we need a contact tracing app? Computer Communications. 2021;166:9–18. doi: 10.1016/j.comcom.2020.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiti A., Zhang Q., Sannigrahi S., Pramanik S., Chakraborti S., Cerda A., et al. Exploring spatiotemporal effects of the driving factors on COVID-19 incidences in the contiguous United States. Sustainable cities and society. 2021;68 doi: 10.1016/j.scs.2021.102784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizumoto K., Kagaya K., Zarebski A., Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance. 2020;25(10) doi: 10.2807/1560-7917.ES.2020.25.10.2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environment International. 2020;139 doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munzert S., Selb P., Gohdes A., Stoetzer L.F., Lowe W. Tracking and promoting the usage of a COVID-19 contact tracing app. Nature Human Behaviour. 2021;5(2):247–255. doi: 10.1038/s41562-020-01044-x. [DOI] [PubMed] [Google Scholar]
- Nakamoto I., Jiang M., Zhang J., et al. A Peer-To-Peer COVID-19 Contact Tracing Mobile App in Japan: Design and Implementation Evaluation. JMIR mHealth and uHealth. 2020 doi: 10.2196/22098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen C.T., Saputra Y.M., Van Huynh N., Nguyen N.T., Khoa T.V., Tuan B.M., et al. Enabling and emerging technologies for social distancing: A comprehensive survey. arXiv preprint arXiv:2005.02816. 2020 doi: 10.1109/ACCESS.2020.3018140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuzzo A., Tan C.O., Raskar R., DeSimone D.C., Kapa S., Gupta R. Universal Shelter-in-Place Versus Advanced Automated Contact Tracing and Targeted Isolation: A Case for 21st-Century Technologies for SARS-CoV-2 and Future Pandemics. Mayo Clinic Proceedings. 2020;95(9):1898–1905. doi: 10.1016/j.mayocp.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill P.H., Ryan-Mosley T., Johnson B. 2020. A flood of coronavirus apps are tracking us. Now it’s time to keep track of them. MIT Technology Review, May 7 2020.https://www.technologyreview.com/2020/05/07/1000961/launching-mittr-covid-tracing-tracker/ (Accessed November 13, 2020) [Google Scholar]
- Park S., Choi G.J., Ko H. Information Technology-Based Tracing Strategy in Response to COVID-19 in South Korea - Privacy Controversies. JAMA. 2020;323(21):2129–2130. doi: 10.1001/jama.2020.6602. [DOI] [PubMed] [Google Scholar]
- Peak Corey M., Childs Lauren M., Grad Yonatan H., Buckee Caroline O. Comparing nonpharmaceutical interventions for containing emerging epidemics. Proceedings of the National Academy of Sciences. 2017;114(15):4023–4028. doi: 10.1073/pnas.1616438114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plank M., James A., Lustig A., Steyn N., Binny R., Hendy S. Potential reduction in transmission of COVID-19 by digital contact tracing systems. medRxiv. 2020 doi: 10.1093/imammb/dqac002. Published online September 1. https://www.medrxiv.org/content/10.1101/2020.08.27.20068346v1 (preprint) [DOI] [PubMed] [Google Scholar]
- Pollmann T., Pollmann J., Wiesinger C., et al. The impact of digital contact tracing on the SARS-CoV-2 pandemic - a comprehensive modelling study. medRxiv. 2020 doi: 10.1140/epjds/s13688-021-00290-x. Published on line September 14. https://www.medrxiv.org/content/10.1101/2020.09.13.20192682v1 (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahmani A.M., Mirmahaleh S.Y.H. Coronavirus disease (COVID-19) prevention and treatment methods and effective parameters: A systematic literature review. Sustainable cities and society. 2020 doi: 10.1016/j.scs.2020.102568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocher L., Hendrickx J.M., de Montjoye Y.A. Estimating the success of re-identifications in incomplete datasets using generative models. Nature Communications. 2019;10(1):1–9. doi: 10.1038/s41467-019-10933-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez P., Graña S., Alvarez-León E.E., Battaglini M., Darias F.J., Hernán M.A., et al. A population-based controlled experiment assessing the epidemiological impact of digital contact tracing. Nature communications. 2021;12(1):1–6. doi: 10.1038/s41467-020-20817-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenkrantz L., Schuurman N., Bell N., Amram O. The need for GIScience in mapping COVID-19. Health and Place. 2020 doi: 10.1016/j.healthplace.2020.102389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salehinejad S., Niakan Kalhori S.R., Hajesmaeel Gohari S., Bahaadinbeigy K., Fatehi F. A review and content analysis of national apps for COVID-19 management using Mobile Application Rating Scale (MARS) Informatics for Health and Social Care. 2021;46(1):42–55. doi: 10.1080/17538157.2020.1837838. [DOI] [PubMed] [Google Scholar]
- Silva J.C.S., de Lima Silva D.F., Neto A.D.S.D., Ferraz A., Melo J.L., Júnior N.R.F., et al. A city cluster risk-based approach for Sars-CoV-2 and isolation barriers based on anonymized mobile phone users’ location data. Sustainable cities and society. 2021;65 doi: 10.1016/j.scs.2020.102574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoll D., Miller J.C., Saxon L.A. COVID-19 testing and infection surveillance: Is a combined digital contact-tracing and mass-testing solution feasible in the United States? Cardiovascular Digital Health Journal. 2020 doi: 10.1016/j.cvdhj.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Development Programme . 2015. What are the Sustainable Development Goals.https://www.undp.org/content/undp/en/home/sustainable-development-goals.html/ Accessed January 26, 2020 from. [Google Scholar]
- United Nations . 2020. Liquidity and Debt Solutions to Invest in the SDGs: The Time to Act is Now.https://www.un.org/sites/un2.un.org/files/sg_policy_brief_on_liquidity_and_debt_solutions_march_2021.pdf Accessed March 29, 2021 from. [Google Scholar]
- Velraj R., Haghighat F. The contribution of dry indoor built environment on the spread of Coronavirus: Data from various Indian states. Sustainable cities and society. 2020;62 doi: 10.1016/j.scs.2020.102371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts G. COVID-19 and the digital divide in the UK. The Lancet. Digital health. 2020;2(8):e395–e396. doi: 10.1016/S2589-7500(20)30169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmink G., Summer I., Marsyla D., et al. Real-Time Digital Contact Tracing: Development of a System to Control COVID-19 Outbreaks in Nursing Homes and Long-Term Care Facilities. JMIR public health and surveillance. 2020;6(3) doi: 10.2196/20828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2018. Disability and health.https://www.who.int/news-room/fact-sheets/detail/disability-and-health (Accessed November 13, 2020) [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2020. COVID-19 strategy update–14 april 2020.https://www.who.int/publications/i/item/covid-19-strategy-update---14-april-2020 (Accessed March 20, 2021) [Google Scholar]
- Xia Y., Lee G. How to return to normalcy: fast and comprehensive contact tracing of COVID-19 through proximity sensing using mobile devices. ArXiv. 2020 published online April 27. https://arxiv.org/abs/2004.12576 (preprint) [Google Scholar]
- Yasaka T.M., Lehrich B.M., Sahyouni R. Peer-to-peer contact tracing: development of a privacy-preserving smartphone app. JMIR mHealth and uHealth. 2020;8(4) doi: 10.2196/18936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zastrow M. Coronavirus contact-tracing apps: can they slow the spread of COVID-19? Nature. 2020 doi: 10.1038/d41586-020-01514-2. [DOI] [PubMed] [Google Scholar]
- Zhou C., Su F., Pei T., Zhang A., Du Y., Luo B., et al. COVID-19: challenges to GIS with big data. Geography and sustainability. 2020;1(1):77–87. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.