Dear Editor,
Coronary artery disease is a leading cause of mortality and morbidity worldwide. Blockade of effective blood flow to heart muscles results in cardiac ischemia and myocardial infarction (MI).1 Many angiogenic factors are known to be elicited during MI, indicating a natural response of the heart to induce the formation of new coronary vessels in an attempt to revascularize the ischemic myocardium.2,3 However, coronary vascular endothelial cells (VECs) do not have sufficient angiogenic potential to effectively repopulate all ischemic regions, and clinical trials aiming at inducing revascularization through the delivery of pro-angiogenic molecules after ischemia have invariably failed.4 During development, a significant portion of coronary VECs in ventricular free walls and septum are reported to arise from endocardium during fetal and neonatal stages.5–7 Nonetheless, adult endocardium barely contribute to coronary VECs in homeostasis or after injuries such as MI.8 Finding new ways to promote neovascularization of adult endocardium offers important clinical insights into developing potential new therapeutic approach for treating ischemic heart diseases.
Vascular endothelial growth factor (VEGF) and its receptors (VEGFRs) have been shown to play essential roles in angiogenesis.9 We therefore examined the expression of VEGFR2 (also named as KDR) in endocardium at different developmental stages. We found that KDR could be detected in the endocardium at embryonic day (E) 13.5, E16.5 and postnatal day (P) 1, and the endocardial expression of KDR gradually decreased from E13.5 to P1 (Supplementary information, Fig. S1a–c). However, we did not detect noticeable KDR expression in endocardium at P7 or adulthood (Supplementary information, Fig. S1d, e). Given the reduction of KDR expression in adult endocardium and considering that adult but not fetal endocardium loses the neovascularization capacity,5,8 we speculate that KDR supplement in the adult endocardium may reactivate its developmental program of blood vessel generation and promote neovascularization after MI.
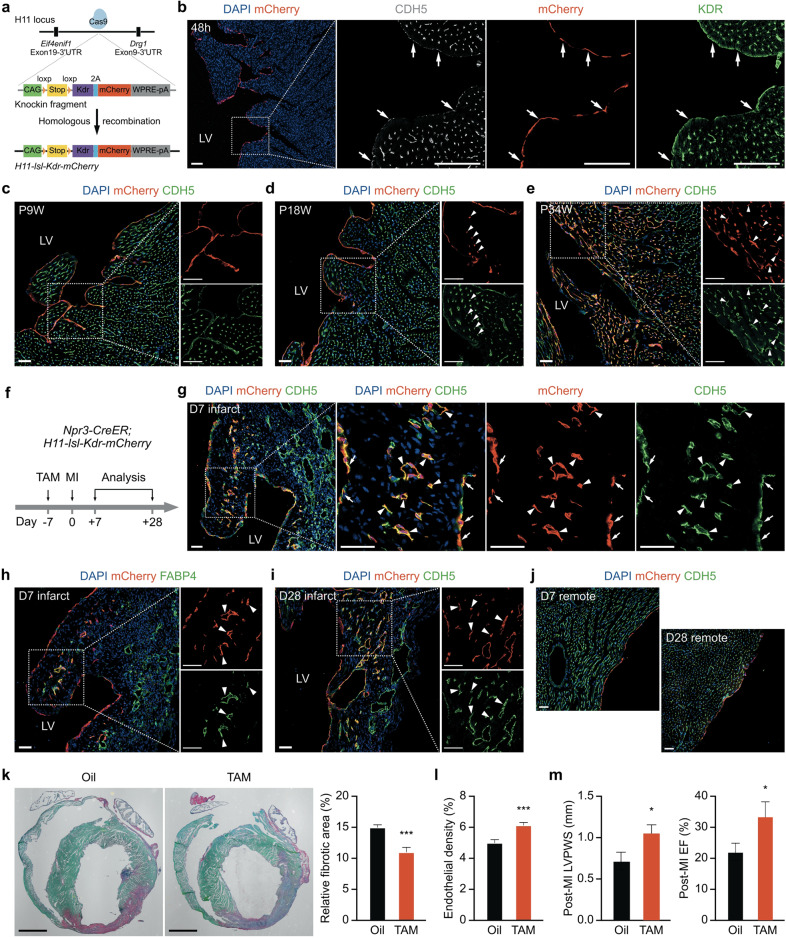
Therefore, to specifically express KDR in adult endocardium and simultaneously trace endocardial cells, we generated an inducible mouse line H11-loxp-stop-loxp-Kdr-2A-mCherry (H11-lsl-Kdr-mCherry) by inserting the CAG promoter driven cassette loxp-stop-loxp-Kdr-2A-mCherry into the Hipp11 (H11) locus located within an intergenic region between the Eif4enif1 and Drg1 genes (Fig. 1a).10 First, we crossed H11-lsl-Kdr-mCherry mice with endocardial specific Cre driver Npr3-CreER mice.7,8 We treated the Npr3-CreER;H11-lsl-Kdr-mCherry mice with tamoxifen at postnatal 8 weeks (P8W) and collected the hearts for analysis after 48 h. Immunostaining for KDR, mCherry, and pan endothelial marker Cadherin 5 (CDH5) showed that both KDR and mCherry were robustly detected in the endocardium (Fig. 1b), demonstrating successful overexpression of KDR in the endocardium of adult Npr3-CreER;H11-lsl-Kdr-mCherry mice.
Fig. 1. Adult endocardium with Kdr-overexpression generates coronary VECs in homeostasis and post-MI.
a The strategy for generating H11-lsl-Kdr-mCherry mice. b mCherry, CDH5 and KDR staining on heart sections from Npr3-CreER;H11-lsl-Kdr-mCherry mice that were harvested at 48 h after tamoxifen treatment at P8W. The arrows indicate KDR+ endocardium. c–e mCherry and CDH5 staining on heart sections from Npr3-CreER;H11-lsl-Kdr-mCherry mice at the indicated time points after tamoxifen administration at P8W. The triangles indicate mCherry+ coronary VECs. f Experimental strategy for tracing Kdr-overexpressed adult endocardium during MI using Npr3-CreER;H11-lsl-Kdr-mCherry mice. g, h mCherry and CDH5 or FABP4 staining on heart sections from Npr3-CreER;H11-lsl-Kdr-mCherry mice at day-7 post-MI. The arrows indicate mCherry+ endocardium. The triangles indicate mCherry+ coronary VECs. i mCherry and CDH5 staining on heart sections from Npr3-CreER;H11-lsl-Kdr-mCherry mice at day-28 post-MI. The triangles indicate mCherry+ VECs. j Few endocardial-derived coronary VECs were identified in the remote regions at day-7 or day-28 post-MI. k Sirius red staining showing that the relative fibrotic area (fibrotic area/ventricular area) was reduced in the Kdr-overexpressed group at day-7 post-MI. n = 7 mice for each group. l The endothelial density (endothelial area/infarct area) in the infarct regions was increased in the Kdr-overexpressed group at day-7 post-MI. n = 3 mice for each group. m Left ventricular posterior wall thickness at end systole (LVPWS) and ejection fraction (EF) were improved at day-7 post-MI in the Kdr-overexpressed group. n = 9 for the oil group; n = 6 for the TAM group. *P < 0.05. LV, left ventricle; RV, right ventricle. White scale bars, 50 µm; Black scale bars, 2 mm. Boxed regions are magnified on the right.
We next examined the cell fate of Kdr-expressing endocardium during cardiac homeostasis. Tamoxifen administration was performed at P8W and the hearts were harvested for analyses at 1-, 10- or 26-week later. No mCherry-labeled coronary VECs were identified in the P9W Npr3-CreER;H11-lsl-Kdr-mCherry mice (Fig. 1c). Only sparse mCherry+ coronary VECs were detected in the myocardium at 10 weeks after tamoxifen treatment (Fig. 1d). Nevertheless, we still followed the fates of Kdr-overexpressed endocardium for half a year post tamoxifen treatment, and intriguingly found a massive coronary VECs labeled with mCherry in the inner layer of the myocardial free walls (Fig. 1e and Supplementary information, Fig. S2a). Intravenous injection of fluorescein-conjugated isolectin B4 (FITC-IB4) showed that these endocardial-derived coronary endothelial cells were functional (Supplementary information, Fig. S2b). We next examined whether endocardial-derived coronary vessels were directly connected to the endocardial layer, which would be deleterious and permit retrograde blood flow from vessels into the ventricular chamber during diastole. Co-staining for mCherry, CDH5, and Endomucin (EMCN), a protein highly detected in endocardial endothelial cells, showed no direct connections between the endocardial-derived VECs and the endocardium (Supplementary information, Fig. S2c). Collectively, adult endocardium with prolonged Kdr-overexpression contribute to coronary VECs during cardiac homeostasis.
To address whether Kdr-overexpressing endocardium contributes to new coronary VECs during MI, we performed tamoxifen administration 7 days before ligation of left anterior descending coronary artery in P8W hearts, and harvested the hearts 7 days post-surgery (Fig. 1f). Noticeably, a significant number of mCherry-labeled coronary VECs were identified in inner myocardial wall abutting the infarct regions (Fig. 1g). Immunostaining for mCherry and FABP4, which is a coronary VEC marker,7 confirmed endocardial-derived coronary VECs in the infarct areas at day-7 post-MI (Fig. 1h). Kdr-expressing endocardium contributed to both venous endothelia identified by EPH receptor B4 (EphB4) staining (Supplementary information, Fig. S3a) and arteries surrounded by aSMA+ smooth muscle cells (Supplementary information, Fig. S3b). Analysis of the injured hearts at day-28 post-MI revealed that endocardial-derived coronary VECs persisted in the injured regions (Fig. 1f, i). These endocardial-derived VECs in the injured hearts were not directly connected to the endocardial layer either (Supplementary information, Fig. S3c, d). Intravenous injection of FITC-IB4 demonstrated that these endocardial-derived coronary VECs were also functional (Supplementary information, Fig. S4). However, few mCherry+ coronary VECs were detected in the remote regions of injured hearts at both day-7 and day-28 post-MI (Fig. 1j). No mCherry signal was detected in the hearts from Npr3-CreER;H11-lsl-Kdr-mCherry mice without tamoxifen treatment at day-28 post-MI (Supplementary information, Fig. S5), suggesting no MI-induced CreER leakiness in the hearts. To address why Kdr-overexpressed endocardium contributed to coronary VECs largely in the injured sites rather than the remote regions, we assessed the expression of VEGFa and found intense expression of VEGFa in the infarct regions, while only sparse signals in the remote regions and sham-operated hearts (Supplementary information, Fig. S6a). As positive controls, we also detected VEGFa expression in fetal and neonatal myocardial walls (Supplementary information, Fig. S6b). Western blotting confirmed the increased VEGFa expression in the injured regions (Supplementary information, Fig. S6c). Much less VEGFa expression in the sham-operated hearts also explains why Kdr-overexpressed endocardium contributes to VECs in a much slower and reduced manner in homeostasis compared with that in MI. Taken together, MI-induced VEGFa may trigger Kdr-overexpressed endocardium to transform into coronary VECs in the injured hearts.
We next performed sirius red staining to examine cardiac fibrosis after MI, and found that endocardial-overexpression of Kdr significantly reduced fibrotic area compared with the control group (Fig. 1k). Meanwhile, the endothelial density was increased and cardiomyocyte apoptosis was decreased in the infarct regions of Kdr-overexpressed hearts (Fig. 1l and Supplementary information, Figs. S7 and S8). We also assessed cardiac function using echocardiography (Supplementary information, Fig. S9a). One day before the surgery, there was no significant difference in heart function between the Kdr-overexpressed and the control groups (Supplementary information, Fig. S9b). However, at day-7 post-MI, the heart functions, including ejection fraction, fraction shortening, and left ventricular posterior wall thickness at end systole, were significantly improved in the Kdr-overexpressed mice (Fig. 1m and Supplementary information, Fig. S9c). Hence, overexpression of Kdr in adult endocardium reduced cardiac fibrosis, increased vascular density, decreased cardiomyocyte apoptosis, and improved heart function after MI.
Administration of recombinant VEGFa proteins or virus-mediated VEGFa overexpression has been reported to promote cardiac vessel formation or improve heart function in preclinical studies. However, to date, clinical trials of VEGFa have not yet shown any clinical benefits, possibly because of the side effects of VEGFa treatment, short life of VEGFa proteins, inadequate transfection, or other reasons.11,12 In our study, we found that overexpression of KDR in adult endocardium promoted endocardial transformation into VECs after MI, suggesting that endogenous KDR ligands in the infarct region are sufficient to induce endocardial neovascularization without extra supply of VEGF proteins. As previously reported, endocardial cells and coronary VECs are two different populations with distinct expression profiles.7 Coronary VECs possess poor angiogenic potential and the delivery of AAV-VEGF promoted arteriogenesis but not endothelial cell proliferation.4 Why Kdr-overexpressed endocardium is able to participate into vessel formation while the pre-existing coronary VECs lack angiogenic potential is still unknown.
In summary, our work shows that endocardial overexpression of Kdr converts adult endocardium into coronary vessels during cardiac homeostasis and after MI, improving post-ischemic heart function. Development of clinically relevant applicable strategies to promote endocardial neovascularization merits further investigation.
Supplementary information
Supplementary information (Materials and Methods, Figures S1-9)
Acknowledgements
This work was sponsored by grants from the National key R&D Program of China (2018YFA0108100), National Science Foundation of China (31871474, 31822034, 81861128023), the “Shuguang Program” supported by Shanghai Education Development Foundation and Shanghai Municipal Commission (17SG54), and the ShanghaiTech University start-up fund. We thank research platforms at the School of Life Science and Technology, ShanghaiTech University. We thank Haojie Chen, Chaohua Zheng, Hao Feng, and Jianjie Gu for the animal husbandry. We also thank Zhonghui Weng and Cheng Wang at Shanghai Institute of Nutrition and Health, Chinese Academy of Sciences for the help in echocardiographic assessment.
Author contributions
Z.J. and H.Z. conceived and designed the experiments. Z.J., Z.L., S.K., T.F., Y.W., Z.G., D.D., and J.M. participated in multiple experiments. Z.J., Z.L., S.K., and T.F. analyzed the data. C.L. and B.Z. edited the manuscript and gave valuable suggestions. H.Z. supervised the study and wrote the manuscript.
Competing interests
The authors declare no competing interests.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41422-020-00436-y.
References
- 1.Go AS, et al. Circulation. 2014;129:e28–e292. doi: 10.1161/CIRCULATIONAHA.113.003961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rivard A, et al. Circulation. 1999;99:111–120. doi: 10.1161/01.CIR.99.1.111. [DOI] [PubMed] [Google Scholar]
- 3.Thiagarajan H, Thiyagamoorthy U, Shanmugham I, Dharmalingam Nandagopal G, Kaliyaperumal A. Heart Fail. Rev. 2017;22:665–683. doi: 10.1007/s10741-017-9630-7. [DOI] [PubMed] [Google Scholar]
- 4.Kocijan, T. et al. Cardiovasc Res.10.1093/cvr/cvaa012 (2020).
- 5.Tian XY, et al. Science. 2014;345:90–94. doi: 10.1126/science.1251487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu B, et al. Cell. 2012;151:1083–1096. doi: 10.1016/j.cell.2012.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang H, et al. Circ Res. 2016;118:1880–1893. doi: 10.1161/CIRCRESAHA.116.308749. [DOI] [PubMed] [Google Scholar]
- 8.Tang J, et al. Circ Res. 2018;122:984–993. doi: 10.1161/CIRCRESAHA.117.312354. [DOI] [PubMed] [Google Scholar]
- 9.Apte RS, Chen DS, Ferrara N. Cell. 2019;176:1248–1264. doi: 10.1016/j.cell.2019.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hippenmeyer S, et al. Neuron. 2010;68:695–709. doi: 10.1016/j.neuron.2010.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taimeh Z, Loughran J, Birks EJ, Bolli R. Nat. Rev. Cardiol. 2013;10:519–530. doi: 10.1038/nrcardio.2013.94. [DOI] [PubMed] [Google Scholar]
- 12.Yla-Herttuala S, Rissanen TT, Vajanto I, Hartikainen J. J. Am. Coll. Cardiol. 2007;49:1015–1026. doi: 10.1016/j.jacc.2006.09.053. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information (Materials and Methods, Figures S1-9)