Abstract
Comprehensive evaluation of photoselective vaporization of the prostate (PVP) versus plasmakinetic resection of the prostate (PKRP) in treating benign prostatic hyperplasia (BPH) is inadequate. This single-centre, retrospective observational study was designed to compare their efficacy, complications and sexual function. A total of 215 patients under PVP or PKRP were included in the study, propensity score matching (PSM) was performed to match the baseline characteristics of the two groups, and perioperative and three-year follow-up data were compared between them. Finally, 120 patients (60 for PVP and 60 for PKRP) were matched after PSM. Compared with the PKRP group, the intraoperative haemoglobin loss was lower (9.08 vs 13.75 g/L, P < 0.001) and the duration of catheterization and postoperative hospital stay were shorter (2.97 vs 4.10 day, P < 0.001; 3.95 vs 5.13 day, P < 0.001, respectively), but the operation time was longer (56.72 vs 49, 90 min, P < 0.001) in the PVP group. Urination measurements were improved for both groups after surgery, although no significant differences were found between them during follow-up. Sexual function after surgery was partly increased; however, frequent retrograde and discomfortable ejaculation occurred in both groups. In addition, dysuria incidence and retreatment were higher in the PVP group at 12 months. In conclusion, PVP is safe and effective in relieving BPH-related lower urinary tract symptoms with less perioperative blood loss and earlier recovery without inferior sexual function effects. However, the study is potentially affected by residual unmeasured confounding.
Subject terms: Health care, Signs and symptoms, Urology
Introduction
Current treatment options for benign prostatic hyperplasia (BPH)-related lower urinary tract symptoms (LUTSs) include observation, drug therapy and surgical intervention. At present, monopolar transurethral resection of the prostate (TURP) is still considered the "gold-standard" operation for treating BPH-related LUTS1, 2. In recent years, 160 W photoselective vaporization of the prostate (PVP) and bipolar plasmakinetic resection of the prostate (PKRP) have been widely used. The efficacy of PKRP is similar to that of TURP, while perioperative complications are greatly reduced3–5. The curative effect of PVP is similar to that of TURP, it has a good haemostasis effect, and its surgical-related complications are fewer than those of TURP6–8. Both PKRP and PVP may replace monopolar TURP as the gold standard of surgical treatment for BPH9–11.
However, the present studies comparing PVP and PKRP reported controversial results in some respects; moreover, few studies have investigated sexual function effects in the same cohort and with adequate follow-up. Therefore, we performed a retrospective, propensity score-matched (PSM) study with a 3-year follow-up to comprehensively compare the efficacy, complications, and sexual function outcomes between PVP and PKRP.
Methods
Patients
Patients who underwent surgical treatment for BPH between January 2014 and August 2016 at the Second Xiangya Hospital of Central South University were retrospectively analysed. This study was approved by the ethics committee of the Second Xiangya Hospital of Central South University, and informed consent was obtained from all included participants.
The inclusion criteria were as follows: (1) age > 50 years old; (2) moderate to severe LUTSs that seriously affect the quality of life of patients, an International Prostate Symptom Score (IPSS) > 7 points, and a maximal urinary flow rate (Qmax) < 15 ml/s; (3) drug treatment failure; (4) prostate volume < 100 g; and (5) an IPSS and quality of life (QoL) score that could be completed independently and effectively.
The exclusion criteria were as follows: (1) previous prostate or transurethral surgery; (2) total prostate specific antigen (tPSA) > 10 ng/ml or rectal finger examination showing prostate induration preoperatively and a diagnosis of prostate cancer on the basis of transrectal prostate biopsy; (3) the deterioration of comorbid medical diseases or a history of acute attack in the last 3 months; (4) urodynamic examination could not exclude neurogenic bladder or detrusor weakness; and (5) other suspected tumours or other diseases requiring surgical treatment, such as indirect inguinal hernia, bladder tumours and bladder stones.
Study design
The study was a single-centre, retrospective, PSM study comparing 160-week PVP and PKRP with a 3-year follow-up. The primary assessment included baseline characteristics, as shown in Table 1. The operation time, haemoglobin loss during operation, duration of catheterization and hospital stay after operation were counted.
Table 1.
Baseline patient characteristics.
| Characteristic | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
| PVP group (n = 109) | PKRP group (n = 106) | P Value | PVP group (n = 60) | PKRP group (n = 60) | P Value | |
| Age (year) | 72.68 ± 6.95 | 67.47 ± 7.39 | < 0.001 | 70.37 ± 6.09 | 71.12 ± 6.07 | 0.500 |
| BMI (kg/m2) | 21.93 ± 3.23 | 21.30 ± 3.16 | 0.146 | 21.68 ± 3.25 | 21.13 ± 3.12 | 0.341 |
| PV (g) | 63.19 ± 19.94 | 54.60 ± 21.00 | 0.002 | 59.40 ± 21.38 | 60.02 ± 20.33 | 0.872 |
| tPSA (ng/ml) | 5.18 ± 3.15 | 3.43 ± 2.48 | < 0.001 | 4.07 ± 2.56 | 4.15 ± 2.64 | 0.856 |
| IPSS | 23.13 ± 3.80 | 21.74 ± 3.69 | 0.007 | 21.98 ± 4.30 | 22.92 ± 2.98 | 0.169 |
| QoL | 4.93 ± 0.65 | 4.79 ± 0.67 | 0.138 | 4.77 ± 0.70 | 4.97 ± 0.52 | 0.078 |
| Qmax (ml/s) | 6.63 ± 2.27 | 7.31 ± 2.40 | 0.034 | 7.24 ± 2.43 | 6.70 ± 1.84 | 0.176 |
| PVR (ml) | 84.06 ± 60.80 | 72.18 ± 59.87 | 0.150 | 72.32 ± 62.27 | 80.40 ± 55.78 | 0.455 |
| IIEF-5 | 8.04 ± 1.67 | 8.96 ± 2.11 | < 0.001 | 8.37 ± 1.79 | 8.27 ± 2.11 | 0.780 |
| MSHQ | 41.61 ± 18.98 | 48.38 ± 15.91 | 0.005 | 46.07 ± 17.59 | 43.10 ± 16.90 | 0.348 |
| MSHQ-EjD | 12.08 ± 5.02 | 14.16 ± 5.48 | 0.004 | 12.87 ± 5.21 | 12.00 ± 5.18 | 0.362 |
| Charlson CI | 0.035 | 0.678 | ||||
| 0 | 42 | 49 | 27 | 22 | ||
| 1 | 37 | 42 | 18 | 26 | ||
| 2 | 21 | 14 | 9 | 12 | ||
| 3 | 9 | 1 | 6 | 0 | ||
BMI body mass index, PV prostate volume, tPSA total prostate-specific antigen, IPSS international prostate symptom score, QoL quality of life score, Qmax maximal urinary flow rate, PVR postvoid residual, IIEF-5 international index of erectile function-five term score, MSHQ male sexual health questionnaire score, MSHQ-EjD male sexual health questionnaire on ejaculatory dysfunction score, Charlson CI charlson comorbidity index.
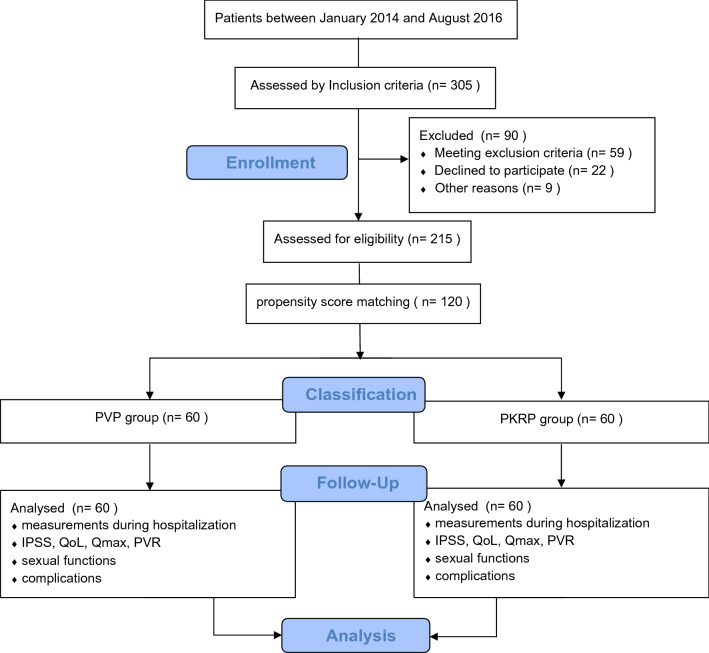
Postoperative follow-up data of 12 months, 24 months, and 36 months included three units: (1) efficacy measures: International Prostate Symptom Score (IPSS)12, maximal urinary flow rate (Qmax), quality of life (QoL) score12, and postvoid residual (PVR); (2) sexual function outcomes: International Index of Erectile Function-five term Score (IIEF-5)13, Male Sexual Health Questionnaire total Score (MSHQ) and Male Sexual Health Questionnaire-Ejaculatory Dysfunction Score (MSHQ-EjD)14, retrograde ejaculation and discomfort on ejaculation events; and (3) postoperative adverse events by Clavien-Dindo grading. This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for cohort studies15. The study is depicted by flow diagram as shown in Fig. 1.
Figure 1.
Flow diagram depicting cohort formation, treatment and follow-up of patients.
Surgical procedures
All included patients underwent surgery by one fully trained urologist. Exact procedures are described in the Supplementary Information.
Propensity score-matching and statistical analysis
To eliminate significant differences in comparison of baseline characteristics, we calculated a propensity score using multivariate logistic models on the basis of those clinical factors that were significantly different in the whole cohort. We performed one-to-one greedy nearest-neighbour matching within one-quarter of the standard deviation of the estimated propensity to create comparable cohorts (caliper 0.02). Patients receiving PVP were then matched with patients receiving PKRP.
The figures were made by prism (version 8.0.1). All data were analysed by SPSS software (IBM, New York, NY, USA). The continuous variables are described as the mean ± standard deviation (). The two-sample t test for continuous variables and Fisher’s exact test or chi-square test for categorical variables were used. Considering the matched nature of the dataset, paired t-test and McNemar test was also used for outcomes to check the consistency of test decisions (Supplementary Information). The difference was statistically significant when P < 0.05.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committees at the Second Xiangya Hospital of Central South University. Informed consent was taken from all individual participants.
Reporting guideline
This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for cohort studies.
Result
Baseline patient characteristics
The whole cohort consisted of 215 patients, with 109 patients receiving PVP and 106 patients receiving PKRP. As Table 1 shows, baseline patient characteristics for both arms were not comparable for the following clinical variables: age (72.68 vs 67.47 years, P < 0.001), prostate volume (63.19 vs 54.60 g, P = 0.002), tPSA (5.18 vs 3.43 ng/ml, P < 0.001), IPSS (23.13 vs 21.74, P = 0.007), Qmax (6.63 vs 7.31 ml/s, P = 0.03), IIEF-5 (8.04 vs 8.96, P < 0.001), MSHQ (41.16 vs 48.38, P = 0.005), MSHQ-EjD (12.08 vs 14.16, P = 0.004), and Charlson Comorbidity Index (42 vs 49, 37 vs 42, 21 vs 14, 9 vs 1, respectively, P = 0.04). After PSM on the basis of these variables, 60 patients for PVP and 60 patients for PKRP were matched for further investigation. There was no significant difference in baseline patient characteristics after PSM (Table 1).
Intraoperative indicators
A longer operation time was required in the PVP group than in the PKRP group (56.72 vs 49, 90 min, P < 0.001). However, the haemoglobin loss in the PVP group was lower than that in the PKRP group (9.08 vs 13.75 g/l, P < 0.001), the catheterization time in the PVP group was shorter (2.97 vs 4.10 days, P < 0.001), and the duration of hospital stay was shorter in the PVP group than in the PKRP group (3.95 vs 5.13 days, P < 0.001).
Postoperative comparison
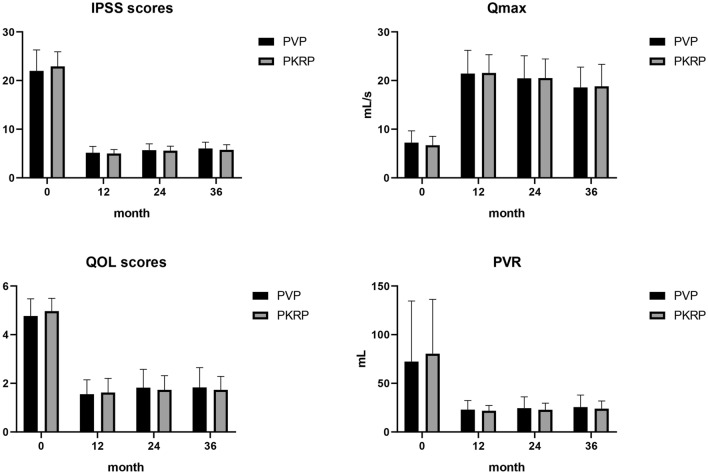
No patients were lost during the follow-up period. A total of 120 patients were followed up for 36 months, including 60 patients in the PVP group and 60 patients in the PKRP group. During the 36-month follow-up, the Qmax and QoL of both groups significantly increased, and the IPSS and PVR significantly decreased compared with the preoperative level (Fig. 2). However, there were no significant differences in Qmax (21.45 vs 21.57 ml/s, 20.47 vs 20.52 ml/s, 21.45 vs 21.57 ml/s, P = 0.89; P = 0.95; P = 0.77, respectively), PVR (22.88 vs 21.83 ml, 24.38 vs 22.78 ml, 25.57 vs 23.88 ml, P = 0.45; P = 0.36; P = 0.38, respectively), IPSS (5.27 vs 5.00, 5.68 vs 5.60, 6.05 vs 5.75, P = 0.40; P = 0.69; P = 0.17, respectively) or QoL (1.55 vs 1.62, 1.82 vs 1.73, 1.83 vs 1.73, P = 0.54; P = 0.50; P = 0.43, respectively) between the PVP group and PKRP group at the 12-, 24-, and the 36-month follow-ups (Table 2).
Figure 2.
IPSS, QoL score, Qmax, and PVR during the 12-month, 24-month, and 36-month follow-up. (P < 0.05) (‘0’ represents preoperative).
Table 2.
3-year follow-up results of PVP group and PKRP group.
| 12 months | 24 months | 36 months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PVP (n = 60) | PKRP (n = 60) | P value | PVP (n = 60) | PKRP (n = 60) | P value | PVP (n = 60) | PKRP (n = 60) | P value | |
| IPSS | 5.27 ± 1.28 | 5.00 ± 0.82 | 0.397 | 5.68 ± 1.31 | 5.60 ± 0.91 | 0.686 | 6.05 ± 1.29 | 5.75 ± 1.07 | 0.169 |
| QoL | 1.55 ± 0.59 | 1.62 ± 0.58 | 0.537 | 1.82 ± 0.75 | 1.73 ± 0.58 | 0.496 | 1.83 ± 0.81 | 1.73 ± 0.55 | 0.428 |
| Qmax (ml/s) | 21.45 ± 4.75 | 21.57 ± 3.74 | 0.881 | 20.47 ± 4.63 | 20.52 ± 3.91 | 0.949 | 18.58 ± 4.19 | 18.82 ± 4.52 | 0.770 |
| PVR (ml) | 22.88 ± 9.39 | 21.83 ± 5.30 | 0.452 | 24.38 ± 7.70 | 22.78 ± 6.80 | 0.362 | 25.57 ± 12.38 | 23.88 ± 7.92 | 0.377 |
IPSS International Prostate Symptom score, QoL Quality of Life score, Qmax maximal urinary flow rate, PVR postvoid residual.
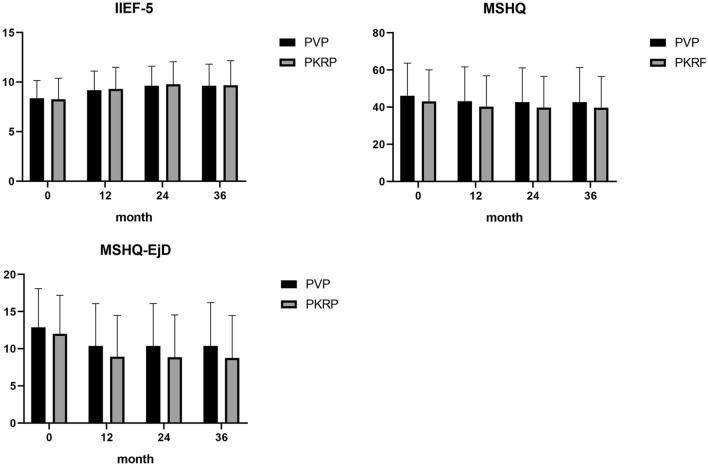
For sexual function outcomes, there was an increase in the IIEF-5 score of both groups, which suggested an erectile function improvement after surgery (Fig. 3). However, the postoperative MSHQ total score and MSHQ-EjD score were significantly decreased in both groups (Fig. 3). In addition, there were no significant differences in IIEF-5 (9.18 vs 9.30, 9.63 vs 9.78, 9.63 vs 9.68, P = 0.76; P = 0.70; P = 0.91, respectively), MSHQ (43.15 vs 40.20, 42.70 vs 39.78, 42.70 vs 39.68, P = 0.36; P = 0.37; P = 0.35, respectively), MSHQ-EjD (10.38 vs 8.93, 10.38 vs 8.85, 10.38 vs 8.75, P = 0.16; P = 0.14; P = 0.12, respectively), retrograde ejaculation (43 vs 44%, 40 vs 39%, 37 vs 37%, P = 0.84; P = 0.85; P = 1.00, respectively) or discomfortable ejaculation incidence (43 vs 47%, 38 vs 42%, 35 vs 35%, P = 0.52; P = 0.44; P = 1.00, respectively) between the PVP group and the PKRP group at the 12-, 24, and 36-month follow-ups (Table 3).
Figure 3.
IIEF-5, MSHQ score, MSHQ-EjD score during the 12-month, 24-month, and 36-month follow-up. (P < 0.05) (‘0’ represents preoperative).
Table 3.
3-year follow-up results of sexual function in two groups.
| 12 months | 24 months | 36 months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PVP (n = 60) | PKRP (n = 60) | P value | PVP (n = 60) | PKRP (n = 60) | P value | PVP (n = 60) | PKRP (n = 60) | P value | |
| IIEF-5 | 9.18 ± 1.93 | 9.30 ± 2.18 | 0.757 | 9.63 ± 1.96 | 9.78 ± 2.26 | 0.698 | 9.63 ± 2.18 | 9.68 ± 2.47 | 0.907 |
| DOE (%) | 44 (73.33) | 47 (78.33) | 0.522 | 38 (63.33) | 42 (70.00) | 0.439 | 35 (58.33) | 35 (58.33) | 1.000 |
| RE (%) | 43 (71.67) | 44 (73.33) | 0.838 | 40 (66.67) | 39 (65.00) | 0.847 | 37 (61.67) | 37 (61.67) | 1.000 |
| MSHQ-EjD | 10.38 ± 5.67 | 8.93 ± 5.54 | 0.159 | 10.38 ± 5.69 | 8.85 ± 5.69 | 0.142 | 10.38 ± 5.81 | 8.75 ± 5.71 | 0.123 |
| MSHQ | 43.15 ± 18.47 | 40.20 ± 16.66 | 0.360 | 42.70 ± 18.42 | 39.78 ± 16.74 | 0.366 | 42.70 ± 18.61 | 39.68 ± 16.75 | 0.352 |
DOE discomfort on ejaculation, RE retrograde ejaculation, IIEF-5 international index of erectile function-five term score, MSHQ male sexual health questionnaire score, MSHQ-EjD male sexual health questionnaire on ejaculatory dysfunction score.
All the patients in the two groups underwent surgery successfully. The complication data classified using the Clavien-Dindo scale are shown in Table 4. At the 12-month follow-up, dysuria incidence was higher in the PVP group (8 vs 2% of Grade II, P < 0.05; 10 vs 1% of Grade III, P = 0.001). There were no differences in other complications between the two groups. Furthermore, retreatment at 12 months (regardless of the cause) occurred more frequently in the PVP patients (12 vs 3%, P = 0.01).
Table 4.
Adverse events in each study period.
| 0–12 months | 12–24 months | 24–36 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PVP (n = 60) | PKRP (n = 60) | P value | PVP (n = 60) | PKRP (n = 60) | P value | PVP (n = 60) | PKRP (n = 60) | P value | ||
| Clavien-Dindo Grade I | IS (%) | 16 | 16 | 5 | 5 | 0 | 0 | |||
| UTI (%) | 3 | 6 | 0 | 0 | 0 | 0 | ||||
| UI (%) | 3 | 3 | 0 | 0 | 0 | 0 | ||||
| UR (%) | 4 | 3 | 0 | 0 | 0 | 0 | ||||
| Clavien-Dindo Grade II | DU (%) | 8 | 2 | 0.048 | 0 | 0 | 0 | 0 | ||
| IS (%) | 6 | 4 | 0 | 0 | 0 | 0 | ||||
| UI (%) | 2 | 3 | 0 | 0 | 0 | 0 | ||||
| US (%) | 1 | 2 | 0 | 0 | 0 | 0 | ||||
| Clavien-Dindo Grade III | US (%) | 2 | 4 | 0 | 0 | 0 | 0 | |||
| UI (%) | 1 | 0 | 0 | 0 | 0 | 0 | ||||
| DU (%) | 10 | 1 | 0.004 | 0 | 0 | 0 | 0 | |||
| UR (%) | 4 | 4 | 2 | 0 | 0 | 0 | ||||
| All cause retreatment (%) | 12 | 3 | 0.013 | 14 | 6 | 0.050 | 13 | 9 | 0.345 | |
Clavien-Dindo Grade the Clavien-Dindo classification of surgical complications into 5 grades (I, II, III, IV and V), IS irritative symptoms, US Urethral stricture, UI urinary incontinence, UTI urinary tract infection, UR urinary retention, DU Dysuria.
Discussion
BPH-related LUTS is one of the most common conditions in elderly men and seriously affects their health and quality of life. Surgical intervention is the most effective treatment for BPH. Monopolar TURP has been regarded as the "gold standard" of BPH surgery for nearly half a century. With the development of medical equipment, PKRP and PVP are becoming alternatives to monopolar TURP. Some studies have shown that the efficacy of PKRP or PVP is similar to that of TURP, but the incidence of related complications is much lower than that of TURP6, 16–18. Liu reported that PKRP was superior to TURP in terms of serum sodium reduction, hospital stay, blood transfusion rate, TURS and urethral stricture incidence, while there was no significant difference in IIEF-5 or retrograde ejaculation19. Many studies have compared PVP with PKRP, indicating their efficacy and safety in the treatment of BPH20–25. However, studies comprehensively comparing their effects with adequate follow-up are lacking.
In the present study, we found that the intraoperative blood loss in the PVP group was significantly less than that in the PKRP group, which may be due to the good haemostasis performance of green light. The average operation time in the PVP group was clearly longer, but when using a 160 W high-power laser, this small difference is not clinically relevant. During the whole follow-up, we found no significant differences in IPSS, QoL, Qmax, PVR or sexual function outcomes between the two groups, which is consistent with most published studies2, 26, 27. Patients in the two groups had improved postoperative erectile function as a result of LUTS relief and a better QoL. However, the discomfort and retrograde ejaculation incidence at 12 months was high for both PVP and PKRP, which is comparable to that previously reported for monopolar TURP27. The exact mechanism of ejaculation has not been well defined, and the structure of the bladder neck and ejaculatory hood are necessary for antegrade ejaculation28, 29; thus, surgical strategies preserving these structures are worth exploring.
On the other hand, this study suggested that perioperative complications are comparable between PVP and PKRP, but we did find that early dysuria incidence was higher in the PVP group. In this study, we defined dysuria as pain and/or burning, stinging, or itching of the urethra or urethral meatus with urination. There are many causes of dysuria. Here, we focus on surgical-procedure-related, noninfectious inflammatory causes, such as urethral anatomic abnormalities and local trauma. The higher dysuria rate in PVP may be because of thermal damage and oedema in urethral tissue in the early stage. In addition, the all-cause-retreatment rate is slightly higher in PVP patients, and the reason can be dysuria-related or inadequate laser energy delivery, leading to incomplete tissue removal; the latter would be markedly solved with 180 W laser systems.
This study still has shortcomings: it is a single-centre retrospective observational cohort study analysed by PSM, and is potentially affected by residual unmeasured confounding. Even so, we can also conclude that compared with PKRP, PVP is a safe and effective choice to relieve BPH-related lower urinary tract symptoms without inferior sexual function effects, and PVP is better in perioperative blood loss and early recovery after surgery. However, surgical strategies preserving more functions, including ejaculation, are still worth exploring.
Supplementary Information
Author contributions
(I) Conception and design: Y.H.W., X.C.; (II) Administrative support: Y.H.W., Y.J.L., D.R., S.Q.W.; (III) Provision of study materials or patients: X.C., C.Y.Q., P.X., L.Z.Z.; (IV) Collection and assembly of data: X.C., C.Y.Q., P.X., Y.J.L., M.P., S.Q.W., D.R., L.Z.Z.; (V) Data analysis and interpretation: X.C., C.Y.Q.; (VI) Manuscript writing: all authors; (VII) Final approval of manuscript: all authors.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Xu Cheng and Chuying Qin.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-89623-4.
References
- 1.Lee SW, et al. Transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement: A quality and meta-analysis. Int. Neurourol. J. 2013;17(2):59–66. doi: 10.5213/inj.2013.17.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar N, Vasudeva P, Kumar A, Singh H. Prospective randomized comparison of monopolar TURP, bipolar TURP and photoselective vaporization of the prostate in patients with benign prostatic obstruction: 36 months outcome. Lower Urin. Tract Symptoms. 2018;10(1):17–20. doi: 10.1111/luts.12135. [DOI] [PubMed] [Google Scholar]
- 3.Cornu JN, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: An update. Eur. Urol. 2015;67(6):1066–1096. doi: 10.1016/j.eururo.2014.06.017. [DOI] [PubMed] [Google Scholar]
- 4.Stucki P, et al. Bipolar versus monopolar transurethral resection of the prostate: A prospective randomized trial focusing on bleeding complications. J. Urol. 2015;193(4):1371–1375. doi: 10.1016/j.juro.2014.08.137. [DOI] [PubMed] [Google Scholar]
- 5.Sandhu JS, Leong JY, Das AK. Photoselective vaporization of the prostate: Application, outcomes and safety. Can. J. Urol. 2019;26(4S1):8–12. [PubMed] [Google Scholar]
- 6.Cimino S, et al. Transurethral resection of the prostate (TURP) vs GreenLight photoselective vaporization of benign prostatic hyperplasia: Analysis of BPH6 outcomes after 1 year of follow-up. Int. J. Impot. Res. 2017;29(6):240–243. doi: 10.1038/ijir.2017.30. [DOI] [PubMed] [Google Scholar]
- 7.Bausch K, et al. High incidence of urinary tract infections after photoselective laser vaporisation of the prostate: A risk factor analysis of 665 patients. World J. Urol. 2020;38(7):1787–1794. doi: 10.1007/s00345-019-02969-3. [DOI] [PubMed] [Google Scholar]
- 8.Kang DH, Cho KS, Ham WS, Choi YD, Lee JY. A systematic review and meta-analysis of functional outcomes and complications following the photoselective vaporization of the prostate and monopolar transurethral resection of the prostate. World J. Mens. Health. 2016;34(2):110–122. doi: 10.5534/wjmh.2016.34.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nettleton J, et al. The industrial revolution for the management of benign prostate obstruction: Worldwide publication trends for surgical and medical therapies over the past two decades. Cent. Eur. J. Urol. 2019;72(2):149–155. doi: 10.5173/ceju.2019.1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang ZY, et al. Transurethral bipolar plasmakinetic prostatectomy for benign prostatic hyperplasia in high-risk and senior patients in China: A systematic review and meta-analysis. Zhonghua Yi Xue Za Zhi. 2019;99(10):778–782. doi: 10.3760/cma.j.issn.0376-2491.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 11.Falahatkar S, et al. Bipolar transurethral vaporization: A superior procedure in benign prostatic hyperplasia: A prospective randomized comparison with bipolar TURP. Int. Braz. J. Urol. 2014;40(3):346–355. doi: 10.1590/S1677-5538.IBJU.2014.03.08. [DOI] [PubMed] [Google Scholar]
- 12.Barry MJ, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J. Urol. 1992;148:1549. doi: 10.1016/S0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 13.Rosen RC, et al. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822. doi: 10.1016/S0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 14.Rosen RC, et al. Development and validation of four-item version of Male Sexual Health Questionnaire to assess ejaculatory dysfunction. Urology. 2007;69:805–809. doi: 10.1016/j.urology.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 15.Vandenbroucke JP, STROBE initiative et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Ann. Intern. Med. 2007;4(10):e297. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abdelwahab O, et al. Bipolar vaporization of the prostate may cause higher complication rates compared to bipolar loop resection: A randomized prospective trial. Int. Urol. Nephrol. 2019;51(12):2143–2148. doi: 10.1007/s11255-019-02280-5. [DOI] [PubMed] [Google Scholar]
- 17.Ruszat R, et al. Comparison of potassium-titanyl-phosphate laser vaporization of the prostate and transurethral resection of the prostate: Update of a prospective non-randomized two-centre study. BJU Int. 2008;102(10):1432–1438. doi: 10.1111/j.1464-410X.2008.07905.x. [DOI] [PubMed] [Google Scholar]
- 18.Bouchier-Hayes DM, et al. A randomized trial of photoselective vaporization of the prostate using the 80-W potassium-titanyl-phosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int. 2010;105(7):964–969. doi: 10.1111/j.1464-410X.2009.08961.x. [DOI] [PubMed] [Google Scholar]
- 19.Liu Z, Li YW, Wu WR, Lu Q. Long-term clinical efficacy and safety profile of transurethral resection of prostate versus plasmakinetic resection of the prostate for benign prostatic hyperplasia. Urology. 2017;103:198–203. doi: 10.1016/j.urology.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 20.Mordasini L, et al. 80-W GreenLight laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic obstruction: 5-Year outcomes of a single-center prospective randomized trial. Urology. 2018;116:144–149. doi: 10.1016/j.urology.2018.01.037. [DOI] [PubMed] [Google Scholar]
- 21.Kumar A, et al. A prospective randomized comparative study of monopolar and bipolar transurethral resection of the prostate and photoselective vaporization of the prostate in patients who present with benign prostatic obstruction: A single center experience. J. Endourol. 2013;27(10):1245–1253. doi: 10.1089/end.2013.0216. [DOI] [PubMed] [Google Scholar]
- 22.Peng M, Yi L, Wang Y. Photoselective vaporization of the prostate vs plasmakinetic resection of the prostate: A randomized prospective trial with 12-month follow-up in mainland China. Urology. 2016;87:161–165. doi: 10.1016/j.urology.2014.08.038. [DOI] [PubMed] [Google Scholar]
- 23.Bachmann A, et al. A European multicenter randomized noninferiority trial comparing 180 W GreenLight XPS laser vaporization and transurethral resection of the prostate for the treatment of benign prostatic obstruction: 12-month results of the GOLIATH study. J. Urol. 2015;193(2):570–578. doi: 10.1016/j.juro.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Leonardo C, et al. What is the standard surgical approach to large volume BPE? Systematic review of existing randomized clinical trials. Minerva Urol. Nefrol. 2020;72(1):22–29. doi: 10.23736/S0393-2249.19.03589-6. [DOI] [PubMed] [Google Scholar]
- 25.Zhang X, et al. Photoselective vaporization versus transurethral resection of the prostate for benign prostatic hyperplasia: A meta-analysis. J. Endourol. 2012;26(9):1109–1117. doi: 10.1089/end.2012.0136. [DOI] [PubMed] [Google Scholar]
- 26.Vasudeva P, et al. Impact of monopolar TURP, bipolar TURP and photoselective vaporization of prostate for enlarged prostate on erectile function. Lower Urin. Tract Symptoms. 2019;11(1):24–29. doi: 10.1111/luts.12189. [DOI] [PubMed] [Google Scholar]
- 27.Kini M, Te A, Kashanian J, Kaplan S, Chughtai B. Ejaculatory hood-sparing photoselective vaporization of the prostate bipolar button plasma vaporization of the prostate in the surgical management of benign prostatic hyperplasia. J. Endourol. 2020;34(3):322–329. doi: 10.1089/end.2019.0558. [DOI] [PubMed] [Google Scholar]
- 28.Hashmat A, Hakim L. Antegrade ejaculation following transurethral laser ablation of the prostate. J. Androl. 1994;15:28S–30S. [PubMed] [Google Scholar]
- 29.Hermabessiere J, Guy L, Boiteux J. Human ejaculation: Physiology, surgical conservation of ejaculation. Progres en urologie: journal de l'Association francaise d'urologie et de la Societe francaise d'urologie. 1999;9(2):305–309. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.