ABSTRACT
Objective
This review highlights the scope and significance of the coronavirus disease 2019 (COVID-19) pandemic with a focus on biobehavioral aspects and critical avenues for research.
Methods
A narrative review of the published research literature was undertaken, highlighting major empirical findings emerging during the first and second waves of the COVID-19 pandemic.
Results
Interactions among biological, behavioral, and societal processes were prominent across all regions of the globe during the first year of the COVID-19 emergency. Affective, cognitive, behavioral, socioeconomic, and technological factors all played a significant role in the spread of infection, response precautions, and outcomes of mitigation efforts. Affective symptoms, suicidality, and cognitive dysfunction have been widely described consequences of the infection, the economic fallout, and the necessary public health mitigation measures themselves. The impact of COVID-19 may be especially serious for those living with severe mental illness and/or chronic medical diseases, given the confluence of several adverse factors in a manner that appears to have syndemic potential.
Conclusions
The COVID-19 pandemic has made clear that biological and behavioral factors interact with societal processes in the infectious disease context. Empirical research examining mechanistic pathways from infection and recovery to immunological, behavioral, and emotional outcomes is critical. Examination of how emotional and behavioral factors relate to the pandemic—both as causes and as effects—can provide valuable insights that can improve management of the current pandemic and future pandemics to come.
Key words/Abbreviations: COVID-19, SARS-CoV-2, emotion, behavior, mental health, pandemic, COVID-19 = coronavirus disease 2019, MERS-CoV = Middle East respiratory syndrome coronavirus, SARS-CoV = severe acute respiratory syndrome coronavirus, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic emerged rapidly during the first 3 months of 2020 after the identification of a cluster of 44 cases (11 severe) of atypical viral pneumonia of unknown cause in Wuhan, China, on December 31, 2019. Some cases of the index cluster were vendors who had a common link to a large wet market selling live seafood and wildlife (1). Despite early and extensive actions within China to prevent spread, by January 8, 2020, the first case outside of China was reported in Thailand (2), followed closely by subsequent large-scale outbreaks in Europe (particularly Italy and Spain), North America, South America, and finally, Africa (Figures 1–3). The COVID-19 situation was declared a pandemic by the World Health Organization on March 11, 2020 (3). Lockdowns and other mitigation measures were implemented around the world in a staged manner during this time, with significant evidence of success during the first wave (4,5). In the closing months of 2020, several candidate vaccines concluded phase 3 clinical trials, several of which emerged with high levels of demonstrated efficacy (6–10) setting the stage for the largest coordinated vaccination effort in world history.
FIGURE 1.
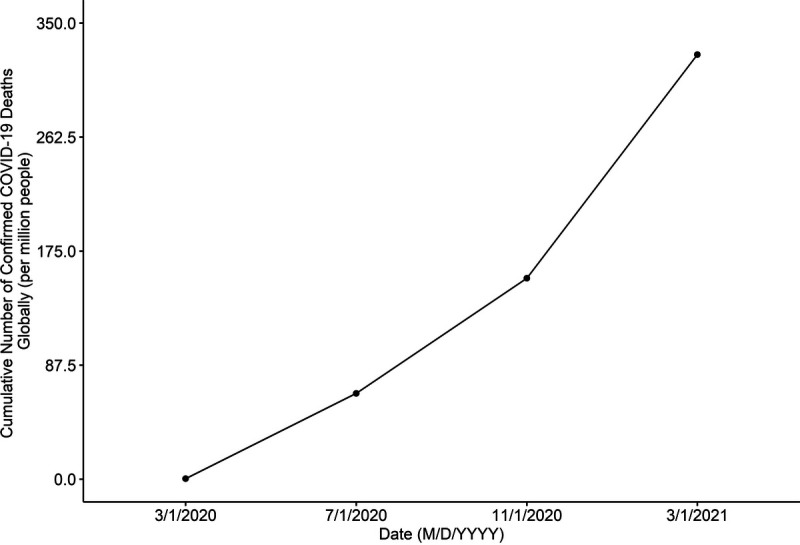
Cumulative deaths per million in the first year of the COVID-19 pandemic. Data are in the public domain. Source: https://ourworldindata.org/coronavirus.
FIGURE 3.
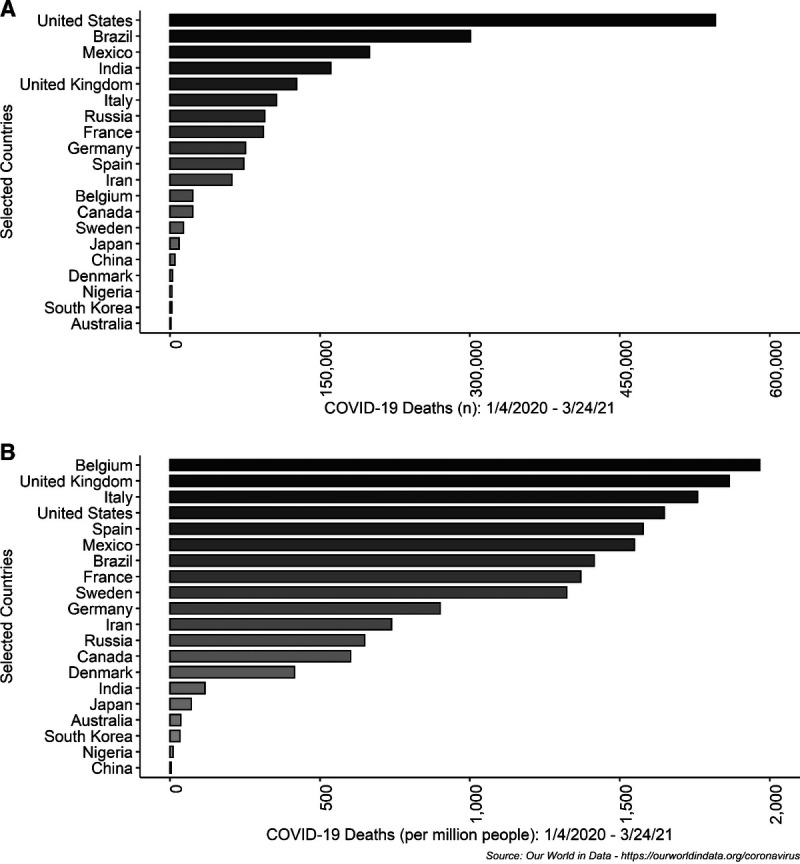
Deaths by selected country in the first year of the COVID-19 pandemic, expressed in absolute numbers (A) and per capita (B). Data are in the public domain. Source: https://ourworldindata.org/coronavirus.
FIGURE 2.
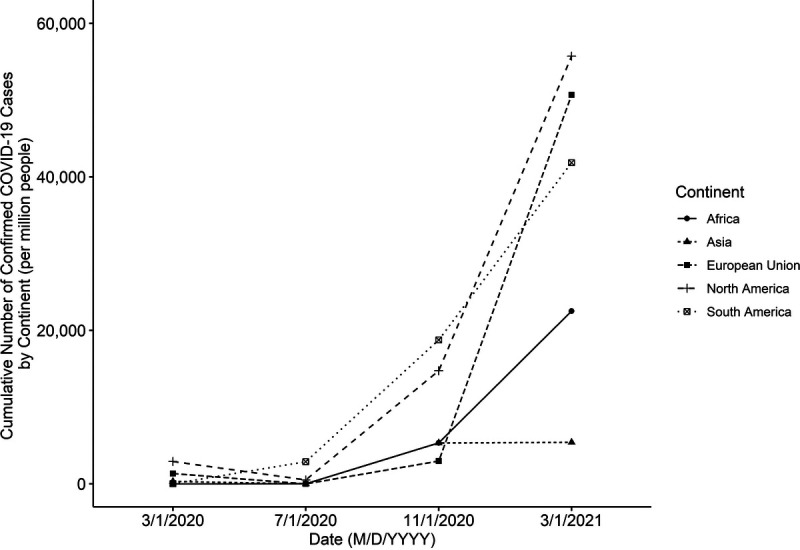
Cumulative cases by selected continent in the first year of the COVID-19 pandemic. Data are in the public domain. Source: https://ourworldindata.org/coronavirus.
A BRIEF OVERVIEW OF COVID-19
COVID-19 is a respiratory illness caused by a novel variant of coronavirus, previously unknown to medical science. The coronavirus family of viruses (formally known as Coronaviridae) is so named based on the spike proteins (s-protein) around the outer surface of the virus giving the protein a distinct crown or “corona”-like appearance (11,12). This family includes numerous viruses that naturally exist and reside within a variety of animal hosts (e.g., bats, pangolins, and camels). Fortunately, only a small handful (n = 7) of known coronaviruses have significant adverse effects on human beings. Of those known coronaviruses that infect humans, approximately half (NL63, 229E, OC43, and HKU1) cause a very mild or asymptomatic upper respiratory tract illness in otherwise healthy individuals. The other species known to interact with humans cause more serious infections: severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and now SARS coronavirus 2 (SARS-CoV-2). SARS-CoV and MERS-CoV have both caused epidemic outbreaks in recent decades and significant fatalities within the geographical regions where these viruses initially emerged (13–16). SARS-CoV-2 is the virus responsible for the current global pandemic as it causes COVID-19 (17–20). Despite being identified only in early 2020, SARS-CoV-2 may have been responsible for isolated cases of human infection within rural regions of China in the months or even years before the current outbreak (21), and converging evidence suggests the possibility of limited circulation of the virus in human populations outside of China in late 2019 (22).
The Origins of the Pandemic
The ultimate origins of the COVID-19 pandemic may never be conclusively known, but the available evidence is consistent with a “spillover” event. Spillover events take place when viruses residing within their natural reservoirs intermittently come into contact with humans through a variety of interactions (e.g., hunting, animal husbandry, or wet markets). Over time, with repeated contact and interactions, the virus evolves and adapts to gain the ability to infect human cells. Available evidence has linked SARS-CoV-2 to an initial bat host and a mammalian intermediary (possibly a pangolin or other mammalian species) (21,23). Although its infection fatality ratio is significantly lower than SARS and MERS, its transmissibility is high, and coupled with the lack of population immunity (innate or acquired), the risk to the human population is substantial.
In the 2020 waves of COVID-19, strict social distancing interventions are estimated to have had a strong beneficial impact on disease spread among the general population, offsetting tens of millions of cases and millions of deaths around the world, based on analyses of predictive models (24). The long-term success of more circumscribed and sustainable public health measures to contain the spread of infection in the coming months and years may partially depend on the identification of high-risk groups (25). It is worth noting that even with strict population-wide physical distancing, protection of the most vulnerable (i.e., people with significant comorbidities, those older than 70 years) has been inadequate. For example, in the United States and Canada, those residing in long-term care facilities have faced disproportionate infection and mortality risk (26). Other high-risk groups include middle-aged to older adults with chronic lung disease or moderate-to-severe asthma, serious heart disease, compromised immune systems, obesity, diabetes mellitus, or chronic renal disease; those undergoing dialysis; or those with liver disease (27). Recent work has also highlighted the excess risk of COVID-19 and a higher risk of experiencing more severe outcomes in ethnoculturally diverse, urban neighborhoods and among those generally subject to socioeconomic disadvantage (25,28).
Unique Features of COVID-19 Compared With Other Viral Epidemics
The novelty of SARS-CoV-2 to the human species is a critical factor in understanding both the pathogenic variability and the public health response to this pandemic. Because SARS-CoV-2 is a new virus, humans have no specific immunological protection from prior population-level exposure. With exposure and recovery, there is evidence that antibodies are produced readily in response to SARS-CoV-2 infection (21). There remains uncertainty about the specificity, strength, and longevity of immunological protection stemming from such exposure, although some parameters of immune response seem to last between 3 and 5 months after exposure (29,30).
In comparison to past pandemics, which includes the 2009 H1N1 pandemic (also known as “swine flu”), 1918 flu pandemic (also known as the “Spanish flu”), and the bubonic plague, COVID-19 differs along a number of dimensions. The mortality rate is lower than MERS (34%) (31), SARS (10%) (32), and the 1918 flu (1%–3%) (33). The most recent seropositivity studies suggest an overall COVID-19 infection fatality rate less than 1%, but highly age-stratified (34,35). Specifically, those older than 80 years of age and/or with medical comorbidities have a substantially greater likelihood of dying of infection (up to 20%) (34,35). Children, in comparison, are overwhelmingly likely to have no symptoms or very mild symptoms, even when using patient data from clinical settings (36,37); there is also evidence that children may indeed be less susceptible to infection overall than adults (38). Age-related risk stratification was also evident in the 1918 flu, where mortality rates were lower for older versus younger adults, possibly because of prior exposure to a similar pathogen in the decades before the vulnerable younger generation was born (possibly the 1889 Russian flu pandemic) (39).
AFFECTIVE DYNAMICS AND THE COVID-19 PANDEMIC
Fear has played a prominent role in responses to the COVID-19 pandemic in terms of political rhetoric and the experience of the individual member of the population. From the latter perspective, fear has an adaptive function because it serves to mobilize behavioral responses to immediately present threats of a physical nature (40,41), particularly those for threats that are evolutionarily significant (42). To the extent that humans are evolutionarily primed to fear unfamiliar infectious pathogens, such a system ensures a robust response to such threats.
Self-protective responses comprise two separable response systems within the human brain: a) a largely automated, subconscious system under the control of the amygdala and its subnuclei and b) a second conscious fear response of more neurophysiologically distributed origins within the neocortex, both of which are oriented to defensive threat preparedness in different ways (43,44). Under conditions of evolutionary preparedness, mobilized defensive responses—particularly the nonconscious variant linked to the amygdala—may be disproportionately stronger and/or more readily triggered by associated stimuli. This may be adaptive if it stimulates self-protective precautions on the individual and societal level, but may also misdirect responses in unproductive ways. The robust fear response to evolutionarily significant threats is in stark contrast to other threats that are very substantial, but either too familiar or of more recent evolutionary origins. For example, a robust and adaptive fear response is comparatively difficult to mobilize in response to the threat posed by familiar pathogens (e.g., mumps, rubella, and influenza), chronic illness (e.g., diabetes mellitus and heart disease), and climate change, despite their being very substantial threats to humans individually and collectively as a species.
Even robust fear of infection may not motivate adaptive behaviors that reduce the probability of getting the SARS-CoV-2 virus, however, for two reasons. First, SARS-CoV-2 not only poses a physical threat of infection but also presents financial (e.g., job loss) and abstract threats (e.g., diminished freedom). Whereas fear of infection can in principle drive appropriate precautionary behavior, the aforementioned symbolic threats may motivate less precautionary behavior in some circumstances (45). Second, decades of research indicate that fear can give rise to adaptive or maladaptive responses to threat depending on coping appraisals (46–48). Coping appraisals refer to judgments of response efficacy, self-efficacy, and response costs. When people believe that recommended behaviors will reduce the threat of infection, are confident they can undertake recommended actions, and see few costs in doing so, then fear promotes adaptive responses. However, when coping appraisal is low, fear engenders maladaptive responses, that is, responses that do not in fact protect against the threat, or unwittingly amplify harm (47,49). Maladaptive responses to the COVID-19 threat have included accidental self-poisonings (50–52), xenophobia (53–55), and fatalism in response to the threat (47,49,56–58). Of equal concern may be hesitation to seek and provide diagnosis/care for other life-threatening conditions (59,60), thereby creating other types of mortality risk.
It is clear that affective dynamics of COVID-19 are complex. Fear of infection energizes precautionary behavior, and this relationship is monotonic rather than curvilinear (41,57). However, according to prominent social psychological theories of precautionary behavior, arousing fear about infection by SARS-CoV-2 will not, on its own, promote physical distancing and other precautionary behaviors. Adaptive responses to fear rely on beliefs about the efficacy, and personal and social costs of precautionary behavior. Likewise, other motivating variables are important to consider beyond fear. For instance, geotracking data from 17 million US smartphone users indicate that sociocultural norms were much more powerful predictors of individual adherence to physical distancing than was the increase in rates of infection and death (as a proxy for life threat) from March 9 to May 8, 2020 (61). From this perspective, social norms—perceptions of others behavior and approval—might be a particularly important target for interventions and public communications in the specific case of COVID-19. A comprehensive review of normative influences and other social psychological factors can be found elsewhere (62).
MENTAL HEALTH
The degree of threat posed by COVID-19 and the heavy and prolonged public health actions undertaken to mitigate its spread both constitute significant stressors. Considerable disruption of worldview may occur for people previously viewing the world as a safe, predictable, and just place. Likewise, disruption of support networks, both personal and professional, has occurred for wide swaths of the population. These latter disruptions may be particularly serious for people who are most vulnerable to—or already suffering from—psychiatric illness before the onset of the pandemic, for example, those with a history of affective disorders, those with substance abuse issues, those with tenuous support networks, or those of lower socioeconomic status, particularly the homeless, those of African American and indigenous communities, and those affected by HIV/AIDS (63–65). Given the excess mortality from COVID-19 and other sources, more frequent instances of complicated bereavement may occur, particularly under circumstances where loved ones have not had an opportunity to adjust to the circumstance or say their goodbyes, and/or undertake their expected religious observances. Widespread unemployment may precipitate or exacerbate financial and other stressors, and in some cases, reduce access to quality mental health services. Any or all of these factors could contribute to a rise in psychiatric disorder within the world population in the wake of the COVID-19 pandemic.
Indeed, US population-level data from the Household Pulse Survey documented high levels of significant (i.e., present nearly every day or at least half the days in a week, and of a severity that would warrant clinical follow-up) depression and anxiety symptoms from April 23, 2020, to early 2021 (66); Figure 4 presents cumulative averages by age group. The mental health of young adults in the 18- to 29-year age range seems to be worst affected, with 51.5% reporting significant symptoms of depression or anxiety compared with the population-wide benchmark value of 11% from the 2019 National Health Interview Survey conducted a year earlier. Those in the highest age ranges (>70 years) reported significant symptoms at less than half the prevalence of younger adults (approximately 25%), but rates were still more than double the 2019 population benchmark value. Czeisler (67) reported the findings from a representative panel survey conducted between June 24 and 30, 2020. In this survey, 40.9% of respondents reported at least one adverse emotional or behavioral symptom related to the COVID-19 public health emergency (i.e., anxiety, depression, stress/trauma, substance use for coping, or suicidal ideation). The same age gradient was evident, but even more striking in that 74.9% of young adults (18–24 years) showed at least one mental or behavioral health symptom compared with 15.1% of those older than 65 years. This was also reflected in comparisons between those retired and those of working age (both employed and unemployed). Rates of reported symptoms of a depressive or anxiety disorder (30.9%), trauma/stress-related disorder (26.3%), and substance use for coping with emotions (13.3%) were more than double the normative levels. Approximately one-quarter of young adults (18–24 years; 25.5%) and unpaid caregivers for older adults (30.7%) reported having seriously considered suicide 30 days before the survey. Similarly, members of visible minorities (Hispanic [18.6%] and Black [15.1%]) had significantly higher levels of such thoughts than the general population value of 10.7%.
FIGURE 4.
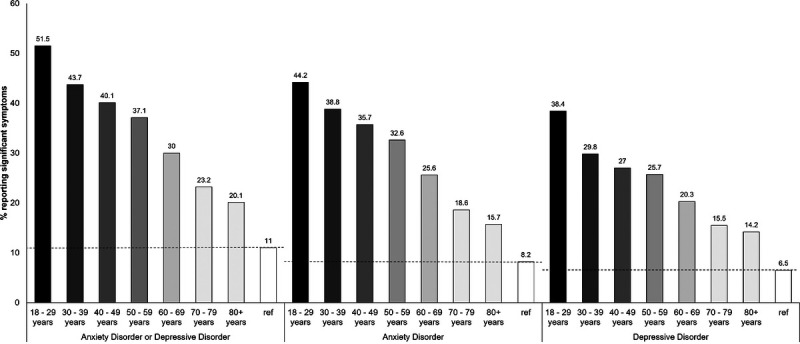
Mental health impacts of the COVID-19 pandemic as a function of age group. Data are from the Household Pulse Survey, Centers for Disease Control and Prevention. Bars represent average values collapsed across all panels of data collection between April 23, 2020, and February 1, 2021. For interpretive purposes, an all-ages reference value of 11% (anxiety or depressive symptoms; 6.5% for depression symptoms only; 8.2% for anxiety symptoms only) was found in the National Health Interview Survey conducted in the year before the pandemic. In the Household PULSE Survey, measurements were taken using a two-item version of the Patient Health Questionnaire and a two-item version of the Generalized Anxiety Disorder scale, both adapted to a 7-day recall time frame. Data are public domain. Source: Centers for Disease Control and Prevention, https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm.
A recent systematic review on the mental health impact of COVID-19 internationally has confirmed the aforementioned trends internationally, with a high risk of mental disorder among young adults (<40 years of age), students, women, and those with high levels of exposure to COVID-19 media communications (68). With respect to the latter, in a Chinese sample, the mental health impact on children was particularly prominent among those with a high level of media exposure, via Internet addiction or smartphone addiction (69). Further elucidation of social media as an amplifying and mitigating factor for psychological distress and disorder is an important avenue for research in the biobehavioral sphere.
The temporal patterning of psychological distress will be important to track in longitudinal studies. One such early study involving repeated longitudinal assessments in the United Kingdom showed increases followed by relative declines that nonetheless remained above expected levels (70).
A Syndemic Framework
The syndemic framework may be an appropriate lens through which to understand the interaction between psychiatric disorders, stress, and behavioral factors in the COVID-19 context. A syndemic is a disproportionately increased disease burden resulting from a clustering of adverse factors; the interaction between the two or more factors is synergistic rather than additive (71). For example, severe psychiatric disorders interact directly with physiological vulnerability to COVID-19 and potentiate severe outcomes from it, and this may be further amplified by behavioral and emotional factors that each also confer their own vulnerability (e.g., smoking and stress) (72–77). The prevalence of smoking is much higher among those with severe mental illness (particularly schizophrenia) than in the general population (53–56), and smoking also introduces physiological vulnerability to respiratory infection via structural and immunological mechanisms (57,58), making it likely that those with severe mental illness will experience more severe outcomes from COVID-19 than other people. The public health measures themselves may burden already taxed coping mechanisms and increased stress in this population, via behavioral and immunological mechanisms (78).
In support of the syndemic hypothesis, early data from a large retrospective cohort study (n = 7348 consecutive adult patients, with laboratory-confirmed COVID-19) in the United States found that a diagnosis of a schizophrenia spectrum disorder was associated with 2.67 odds of mortality relative to patients without a psychiatric disorder (79). This finding is remarkable in part because a schizophrenia diagnosis adds an increment in mortality risk second only to age in magnitude, which is otherwise the strongest known risk factor for death after SARS-CoV-2 infection. In the aforementioned study, those diagnosed with an anxiety or depressive disorder were not at enhanced mortality risk compared with patients without a psychiatric diagnosis, after adjustment for confounders (79).
In summary, the syndemic framework is a potentially useful framework with which to understand the multiple interacting vulnerabilities that are introduced by COVID-19 for psychiatric populations (71). At least one early study suggests that those living with schizophrenia spectrum disorder are one candidate group that warrants special attention in this respect (79).
Suicide
Although statistically rare, suicide is an important mental health outcome to monitor in the wake of COVID-19, equally as a function of psychiatric morbidities, economic situations, personal loss, stress, loneliness, and social isolation (58,80–84). Prior pandemics have been associated with reliable increases in suicide rates, although the absolute number of suicides in such cases is a small fraction of those killed by the pandemic itself (85–87), highlighting the importance of interpreting both relative risk and absolute numbers (88). Early signs suggest the potential for increased suicide rates during the COVID-19 pandemic, though such effects may be time-lagged. In a large-scale study in Japan, an initial 14% drop in suicide rates was observed in the first 5 months of the pandemic, followed by a rise of 16% relative to baseline in Wave 2 (89). The effect in this case was particularly pronounced among women (37% increase) and children/adolescents (49% increase). The increase in women was noteworthy because of their higher level of domestic and parenting responsibilities, potential for role conflict and exposure to domestic abuse. The increase in suicide risk among younger age groups tracks the disproportionately amplified anxiety and depressive symptoms observed in such age groups in North America (see “Mental Health and Addictions” section of this article above). In one major Canadian city, the number of deaths by suicide on the main subway system—a relatively unambiguous instance intentional self-harm—was nearly double that of the running 10-year average and the highest absolute level since such data were collected systematically (90). Likewise, significant increases in the prevalence of suicidal ideation have been documented in self-report surveys, particularly among young adults (67). Large-scale longitudinal analyses will assist in providing a clearer picture of the full range of impact of the pandemic in terms of ideation and self-harm and should likely include consideration of passive forms of self-harm and so-called “deaths of despair” via substance abuse (91). The use of technology to reach and mitigate risk among those with psychiatric and substance abuse disorders will be critical for several years after the abatement of the pandemic itself (see the “Technology and Behavior in the Pandemic Response” section of this article hereinafter).
NEUROLOGICAL IMPACTS
Viral infections can affect the central nervous system directly or via inflammatory processes arising from the activation of the body’s defensive immune response. The latter inflammatory responses may affect membranes surrounding the brain (meningitis) or brain tissue itself (encephalitis). These inflammatory processes can trigger a number of cognitive symptoms and impairments, ranging from headache and pain, to difficulty concentrating and confusion, and even more severe clinical outcomes such as seizures, edema, or death in extreme cases. A viral infection also contributes to one’s infectious burden, which is associated with cognitive decline (92,93).
One of the many unknowns about COVID-19 is the extent to which it impacts the brain (94,95). Other viral infections that can produce neurological or neuropsychiatric symptoms include influenza (96), MERS (97), Zika (98), herpes (99), and chickenpox (100). SARS-CoV-2 has a similar receptor binding domain structure to SARS-CoV and likely shares its neurotropism and neurotoxicity (101), and so we may expect COVID-19 to impact the brain similarly at least among those with severe infections. Current evidence suggests that SARS-CoV-2 can induce endotheliitis (102). Thus, coagulopathy and vascular endothelial dysfunction are proposed as COVID-19 complications (103). Endothelial dysfunction plays a critical role in the mechanisms leading to cerebral small vessel disease and related brain changes, such as white matter lesions and lacunar infarcts (104).
The high occurrence of cerebrovascular incidents among those hospitalized with COVID-19 suggests at least an indirect effect on the brain when the infection is severe; many other symptoms such as agnosia/ageusia, dizziness, and confusion (widely reported among those who were or were not hospitalized) also suggest brain impacts of infection. Animal and human tissue research suggests that adverse consequences also exist from a mechanistic perspective (105). A recent surveillance study in the United Kingdom showed significant neurological manifestations of COVID-19 infection (106), as did a large retrospective cohort study in the United States involving 62,354 patients (107). The latter study found reciprocal relationships between COVID-19 risk and neuropsychiatric disorder, such that a preexisting neuropsychiatric disorder amplified COVID-19 infection risk, and likewise, COVID-19 infection increased the risk of new-onset psychiatric disorder or dementia (107).
Finally, a newly published study using a large electronic health records of 236,379 patients diagnosed with COVID-19, showed a 33.6% chance of neurological or psychiatric diagnosis in the 6 months following infection, 12.8% of which were first lifetime diagnoses; these values rose to 46.4% and 25.8% for those patients with the most severe infections, requiring ICU treatment (108). By far, the most prominent incident diagnosis was anxiety disorder at 17.4%, followed by ischemic stroke (2.4%) and psychotic disorder (1.4%).
LIFESTYLE BEHAVIORS, COMORBIDITIES, AND SOCIAL DETERMINANTS
Primary demographic and disease-related risk factors for COVID-19 mortality are male sex, older age (>65 years; Figure 5), and the presence of underlying chronic medical conditions, such as hypertension, diabetes mellitus, chronic respiratory diseases (e.g., asthma), and cardiovascular and cerebrovascular diseases. Behavioral risk factors are equally important and could include exercise as a protective factor vis-à-vis aerobic fitness and smoking as a risk factor. Indeed, a systematic review of data from China suggests that smokers were more likely to suffer from severe outcomes and hospitalizations. Early data from the US Centers for Disease Control and Prevention subsequently confirmed the same pattern among North American infections (27,109), and a more recent meta-analysis confirmed that smoking nearly doubles the chance of severe COVID-19 infection (77). A study at a major health system in New York revealed that among 5700 patients presenting for hospital treatment as a result of COVID-19 infection, the average age was 65 years, 60% were male, and most had comorbidities, the most common being hypertension (56.6%), obesity (41.7%), and diabetes mellitus (33.8%) (110). In China, among 191 COVID-19 admissions to two major hospitals in Wuhan, 48% had comorbidities, of which hypertension was the most common (30%), followed by diabetes mellitus (19%) and heart disease (8%) (111). At least four studies have confirmed that those with evidence of cardiovascular disease are at an increased risk of mortality with COVID-19 infection (112–114). Although data are not yet available for vaping as a risk factor for severe outcomes, the potential exists (115) and could explain some occurrence of severe outcomes in younger age groups. Indeed, COVID-19–related risks may be a compelling addition to antismoking and vaping communications (116). Other early life exposures that may confer risk include substance use (cocaine), anabolic steroid use, and some antidepressant medications (117–120). Careful research will be required to distinguish premorbid diatheses from the effects of the virus itself.
FIGURE 5.
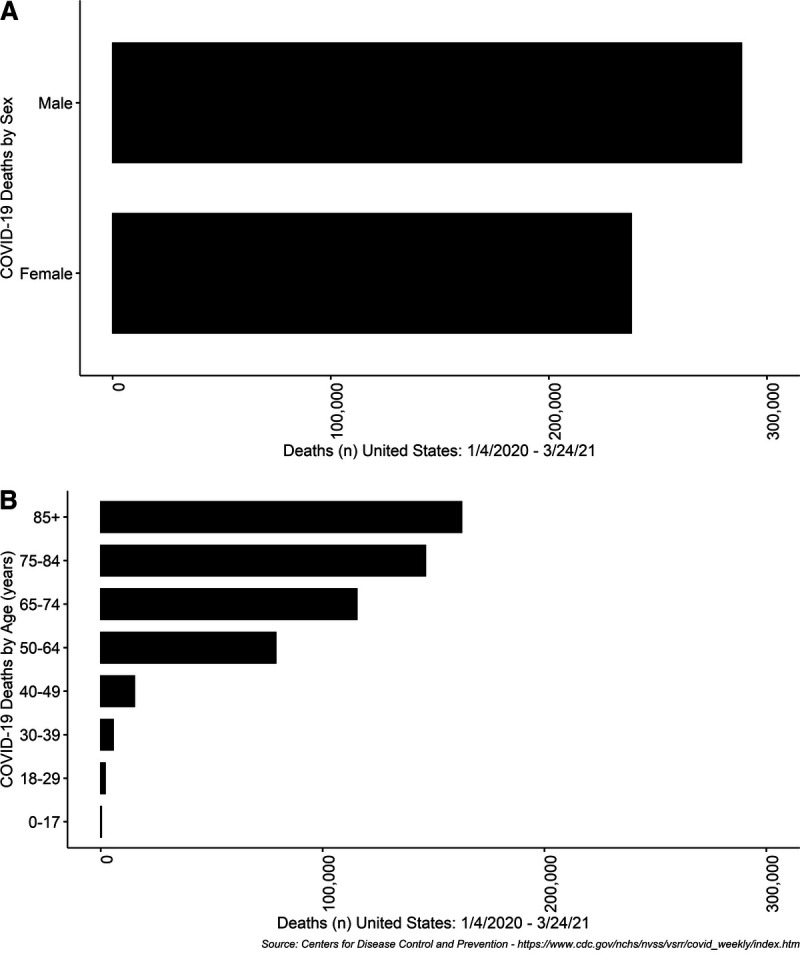
Age and sex distribution of COVID-19 deaths in the first year of the COVID-19 pandemic. Data are in public domain. Source: Centers for Disease Control and Prevention, https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm.
Social determinants of health, such as poverty, race, physical environment, and homelessness seem to have a substantial impact on outcomes related to COVID-19 (25). Critical public health measures such as physical distancing are also more difficult for people/populations experiencing adverse social circumstances. Homelessness can contribute to overcrowding especially during lockdowns when public spaces are closed, which may increase the risk of infection (65). Similarly, food insecurity for children living in poverty who rely on school lunch programs may be increased during school closures. The resultant undernutrition or malnutrition contributes to lowered immunity, thereby increasing the risk of viral transmission (25). Social determinants can also interact with medical conditions in insidious ways. For example, asthma morbidity is associated with poverty, exposure to smoke, and non-Hispanic Black race (121), whereas asthma itself is a risk factor for COVID-19 morbidity (122). In the United States, several studies have found that those of African American descent are more likely to experience greater rates of infection and mortality from COVID-19 (123,124), an effect that could be attributable to a higher likelihood of holding jobs that involve higher exposure to COVID-19, such as service positions and other frontline positions, and less likely to be able to work from home.
Spatiotemporal analysis can play an essential role in the assessment of the associations between race or ethnicity, geographic and neighborhood inequities, and morbidity or mortality related to diseases (125,126). In this context, this analysis can be used to identify clusters or “hot spots” of COVID-19 cases and detect spatial and temporal variations in racial and neighborhood disparities related to COVID-19, for targeted public health interventions (127). In effect, understanding where, when, and which group is disproportionately affected by COVID-19 can significantly enhance the public health response toward the disease.
RACISM AND SOCIAL UNREST
The COVID-19 pandemic has coincided with and contributed to various expressions of racism and social unrest. For example, for Chinese Americans, racist tropes veiled under health-related fears (128,129), perceptions as “perpetual foreigners,” (130) have been used to support the belief that they are threatening physical and cultural health of a White, Anglo-dominant US society. Nearly half of both Chinese American parents and youth in one study reported being directly targeted by COVID-19 racial discrimination online and/or in person (131). Up to 91% of parents and youth reported witnessing at least one incident of COVID-19 racial discrimination online and/or in person. In addition, the majority of parents and youth in the sample perceived collective racism in the forms of health-related Sinophobia, where the Chinese are considered a health threat to American society, and the media’s role in perpetuating Sinophobia. These experiences of racism and racial discrimination were positively associated with poorer mental health and reduced psychological well-being in both parents and youth (131). Similar experiences have been reported by other Asian American communities during COVID-19 as spillover effects of anti-Chinese racism (132). Americans who were more fearful of COVID-19, had less accurate knowledge of the virus, and had more negative attitudes toward Asians, as well as those who had less trust in science and more trust in far-right political leadership, reported being more likely to engage in discriminatory behavior toward people of Asian descent (133). The COVID-19 pandemic also coincides with a heightened awareness of the adverse consequences of discrimination, such as anti-black racism, and the systemic barriers in the care and safety that members of various minority groups experience. Likewise, an increased focus on the relationship between humans and our habitat has encouraged re-engagement with indigenous peoples, whom have retained more accurate understanding of the necessary reciprocity between humans and nature. Reconciling social and ecological imbalances may prove critical for preventing, mitigating and recovering from future pandemics.
TECHNOLOGY AND BEHAVIOR IN THE PANDEMIC RESPONSE
The role of technology during the COVID-19 epidemic has been prominent in a number of ways, both positive and negative. With respect to the former, technology continues to play a crucial role in efficiently and effectively conveying COVID-19 risk information and instructions for population-level response. Some countries are reliant on conventional text messaging (e.g., Vietnam), whereas others developed COVID-19–specific mobile phone applications (e.g., Canada, the United States, and the United Kingdom) to provide up-to-date information to the public (134). However, despite the added features of apps, their passive nature makes them less preferable to active push notification systems, given the greater potential for information penetration and uniformity of messaging in the latter (135).
Several countries close to China were able to keep the COVID-19 cases and deaths very low because of their efficient use of technology, particularly South Korea and Vietnam. The extensive use of contact tracing apps (e.g., NCOVI and SmartCity in Vietnam) was a notable feature in their pandemic response (136). The use of such technology raises concerns over data privacy and the ethics of mass surveillance, likely contributing to their limited use in North America, the United Kingdom, and the European Union. A Bluetooth-based contact tracing app, developed by a joint initiative of Google and Apple, offers more data security for contact tracing and may deliver the desired security and information protection preferred by many Western countries. However, more psychologically meaningful apps that engage self-regulatory mechanisms to promote active disease avoidance are important to explore.
Beyond loss of privacy, an additional dark role for technology is the viral spread of misinformation and rumors, particularly in social media (e.g., Facebook and Twitter) (137,138). Because of the ubiquitous nature of smartphones, people now have unrestricted access to this misinformation. Some rumors are potentially dangerous (e.g., consumption of methanol or disinfectant as a remedy of COVID-19) and can threaten human life (135). Furthermore, the use of social media and mobile apps (e.g., WhatsApp) to spread hatred and xenophobia was also widespread in the early days of the pandemic (139). Technology has also accelerated acceptance and integration of new routes to accessing health care, including mental health service provision, with social distancing intact (e.g., telemedicine, for both physical and mental health contacts). Further technological progress—specifically in consumer-focused sphere—could bring a plethora of brain and body sensors to out-of-clinic and home settings, benefiting telemedicine, and urgent care and facilitating research in these contexts. There are already new dedicated biomedical technologies announced that are intended for consumers to fight COVID-19, such as smart masks, disposable biosensors for continuous temperature, and cardiac function monitoring. Using such biomedical sensing and new mobile approaches stemming from uniquely capable and tightly integrated artificial intelligence could provide an in-depth and extensive health care, remotely.
CURRENT UNKNOWNS AND FUTURE DIRECTIONS
Although scientific understanding of SARS-CoV-2 is growing steadily, there are still a number of unknowns about the virus itself, the illness that it causes in humans (COVID-19), and its biobehavioral impact on the population. Hereinafter are some of the critical questions for future biobehavioral research:
What are the psychological (e.g., stress, mood, and social-cognition) and psychiatric (e.g., new occurrence of affective disorders, stress-related disorders, and/or exacerbation of existing conditions) impacts of COVID-19? How do these differ with respect to those who directly experienced infection, health care workers, and people in their wider social networks (family, friends)? What are the mechanisms by which such adverse impacts are generated (e.g., immunological, endocrinological, neurobiological, and cognitive)? What factors predict resilience to adverse psychological and psychiatric effects of COVID-19?
What are the best ways to promote vaccine uptake and fidelity to precautionary behaviors as the pandemic persists? Perhaps more importantly, can biobehavioral research help to inform the communications strategies that might overcome vaccine hesitancy?
What are the effects of SARS-CoV-2 on the central nervous system, in an acute sense (immediately after infection), in the short-term after recovery, and in the long-term? Are there lasting impacts in some of those infected, and if so, what predicts these impacts? Does degree of impact of COVID-19 on the brain depend on exposure level or type of exposure?
Positive growth experiences have been reported anecdotally among some population members in industrialized nations during stay-at-home orders; plausible mechanisms might include reduced work stress, increased time with family, reduced exposure to advertising, reduced consumerism, and reevaluation of life situation. How common are such effects? What are the factors that predict personal growth during the pandemic? How lasting are such effects? What are the relevant mechanisms?
What are the psychological (cognitive, affective, and attitudinal) predictors of receptivity to the uptake of vaccines? Several studies have characterized those with low levels of trust in conventional authorities (e.g., physicians and public health officials) and associated communication sources as more likely to be hesitant about vaccination (140). In a large sample of 13,426 respondents from 19 countries in June 2020, approximately 2 of 3 respondents intended to take a vaccine if available, and those who were older, had higher income, and had higher levels of trust were more likely to indicate strong intentions (141). Troublingly, vaccine hesitancy in the United States seems to have increased from earlier to late in the pandemic (142). In a study involving Turkey and the United Kingdom, beliefs that COVID-19 was of natural origin were associated with less vaccine hesitancy (143). A recent meta-analysis of large sample studies revealed consistent effects of demographic variables as predictors of hesitancy, with female sex, lower income, and ethnic minority status as predictors of higher hesitancy (144). Other individual differences are largely unexplored; it is possible, for instance, that some cognitive styles and personality types might be more or less likely to endorse vaccination. Identification and tailoring of communications may be helpful in this respect.
What types of individual differences (i.e., cognitive, personality, attitudinal) predict adherence to social distancing and other COVID-19 mitigation measures? (145). Do these factors differ among the general population and health professionals in clinical settings?
What are the origins of the large age-related differences in psychiatric symptomology? What cohort-appropriate interventions might best be mobilized to assist those suffering from adverse mental health outcomes? Likewise, what psychological factors account for the relative resilience of older adults to such outcomes?
CONCLUSIONS
The COVID-19 pandemic has made clear that infectious disease continues to pose a major global threat, with virtually every country in the world profoundly affected by the virus itself and/or extreme mitigation measures intended to contain its spread. Throughout this historic event, interactions between biology and behavior have been prominent in the context of the substantial social and economic consequences of the COVID-19 pandemic. Important areas for continued investigation include affective responses to COVID-19, the neurobiological sequelae of the disease (both acute and long-term), and syndemic potentials involving psychopathology, substance use, and stress in the context of socioeconomic disadvantage. Interdisciplinary cooperation will enable the highest-quality research to be conducted, ideally involving behavioral scientists, social scientists, epidemiologists, neuroscientists, technologists, biochemists, and medical scientists working together to examine biobehavioral facets of the COVID-19 pandemic and its lasting effects on the world population. Many accounts suggest that the frequency of such spillover events is on the rise because of a number of facets of globalization and human interference with wildlife; if true, it will mean that the templates that we establish for tracking and responding to these facets will be important to maintain and reflect upon long after the COVID-19 pandemic has fully abated.
Acknowledgments
Source of Funding and Conflicts of Interest: The lead author is supported by funding from the Social Sciences and Humanities Research Council of Canada and the Natural Sciences and Engineering Research Council of Canada. The authors declare no conflicts of interest
Contributor Information
Paschal Sheeran, Email: psheeran@unc.edu.
Geoffrey T. Fong, Email: gfong@uwaterloo.ca.
Charissa S. L. Cheah, Email: ccheah@umbc.edu.
Mark Oremus, Email: moremus@uwaterloo.ca.
Teresa Liu-Ambrose, Email: teresa.ambrose@ubc.ca.
Mohammad N. Sakib, Email: mn2sakib@uwaterloo.ca.
Zahid A. Butt, Email: zahid.butt@uwaterloo.ca.
Hasan Ayaz, Email: hasan.ayaz@drexel.edu.
Narveen Jandu, Email: narveen.jandu@uwaterloo.ca.
Plinio P. Morita, Email: plinio.morita@uwaterloo.ca.
REFERENCES
- 1.World Health Organization . Coronavirus disease (COVID-19)—World Health Organization. WHO; 2020. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed August 3, 2020. [Google Scholar]
- 2.World Health Organization . Novel Coronavirus (2019-nCoV): Situation Report, 1. Geneva, Switzerland: World Health Organization; 2020. Available at: https://apps.who.int/iris/handle/10665/330760. Accessed January 19, 2021. [Google Scholar]
- 3.World Health Organization . Coronavirus Disease 2019 (COVID-19): Situation Report, 72. Geneva, Switzerland: World Health Organization; 2020. Available at: https://apps.who.int/iris/handle/10665/331685. Accessed January 19, 2021. [Google Scholar]
- 4.Koo JR, Cook AR, Park M, Sun Y, Sun H, Lim JT, Tam C, Dickens BL. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infect Dis 2020;20:678–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis 2020;20:631–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Le TT, Andreadakis Z, Kumar A, Román RG, Tollefsen S, Saville M, Mayhew S. The COVID-19 vaccine development landscape. Nat Rev Drug Discov 2020;19:305–6. [DOI] [PubMed] [Google Scholar]
- 7.Mahase E. COVID-19: UK approves Pfizer and BioNTech vaccine with rollout due to start next week. BMJ 2020;371:m4714. [DOI] [PubMed] [Google Scholar]
- 8.Oliver SE. The Advisory Committee on Immunization Practices’ Interim Recommendation for Use of Moderna COVID-19 Vaccine—United States, December 2020. MMWR Morb Mortal Wkly Rep [Internet] 2021;69:1653–3. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm695152e1.htm. Accessed January 19, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tanne JH. COVID-19: Pfizer-BioNTech vaccine is rolled out in US. BMJ 2020;371:m4836. [DOI] [PubMed] [Google Scholar]
- 10.Voysey M Clemens SAC Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021;397:99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crawford DH. Viruses: A Very Short Introduction. 2nd ed. Oxford, UK: Oxford University Press; 2018. [Google Scholar]
- 12.Li F. Structure, function, and evolution of coronavirus spike proteins. Annu Rev Virol 2016;3:237–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peiris JSM, Yuen KY, Osterhaus ADME, Stöhr K. The severe acute respiratory syndrome. N Engl J Med 2003;349:2431–41. [DOI] [PubMed] [Google Scholar]
- 14.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, Tong S, Urbani C, Comer JA, Lim W, Rollin PE, Dowell SF, Ling A-E, Humphrey CD, Shieh W-J, Guarner J, Paddock CD, Rota P, Fields B, DeRisi J, Yang J-Y, Cox N, Hughes JM, LeDuc JW, Bellini WJ, Anderson LJ. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 2003;348:1953–66. [DOI] [PubMed] [Google Scholar]
- 15.Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet 2015;386:995–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DAT, Alabdullatif ZN, Assad M, Almulhim A, Makhdoom H, Madani H, Alhakeem R, Al-Tawfiq JA, Cotten M, Watson SJ, Kellam P, Zumla AI, Memish ZA. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med 2013;369:407–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020;109:102433–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Du Toit A. Outbreak of a novel coronavirus. Nat Rev Microbiol 2020;18:123–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–42. [DOI] [PubMed] [Google Scholar]
- 20.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daszak P, Olival KJ, Li H. A strategy to prevent future epidemics similar to the 2019-nCoV outbreak. Biosaf Health 2020;2:6–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.La Rosa G, Mancini P, Bonanno Ferraro G, Veneri C, Iaconelli M, Bonadonna L, Lucentini L, Suffredini E. SARS-CoV-2 has been circulating in northern Italy since December 2019: evidence from environmental monitoring. Sci Total Environ 2021;750:141711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morens DM, Daszak P, Taubenberger JK. Escaping Pandora’s box—another novel coronavirus. N Engl J Med 2020;382:1293–5. [DOI] [PubMed] [Google Scholar]
- 24.Hsiang S, Allen D, Annan-Phan S, Bell K, Bolliger I, Chong T, Druckenmiller H, Huang LY, Hultgren A, Krasovich E, Lau P, Lee J, Rolf E, Tseng J, Wu T. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020;84:262–7. Available at: 10.1038/s41586-020-2404-8. [DOI] [PubMed] [Google Scholar]
- 25.Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med 2020;8:659–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McIntosh K. Coronavirus disease 2019 (COVID-19): epidemiology, virology, and prevention. In Hirsch MS, editor. UpToDate; : 2020. Available at: https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-epidemiology-virology-and-prevention. Accessed August 3, 2020. [Google Scholar]
- 27.Centers for Disease Control and Prevention . Coronavirus Disease 2019 (COVID-19). Atlanta, GA: Centers for Disease Control and Prevention; 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed August 3, 2020. [Google Scholar]
- 28.Public Health Ontario . COVID-19 in Ontario—a focus on diversity. Public Health Ontario. 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/epi/2020/06/covid-19-epi-diversity.pdf?la=en. Accessed August 3, 2020.
- 29.Dan JM, Mateus J, Kato Y, Hastie KM, Faliti CE, Ramirez SI, Frazier A, Yu ED, Grifoni A, Rawlings SA, Peters B, Krammer F, Simon V, Saphire EO, Smith DM, Weiskopf D, Sette A, Crotty S. Immunological memory to SARS-CoV-2 assessed for greater than six months after infection. bioRxiv 2020. doi: 10.1101/2020.11.15.383323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Isho B, Abe KT, Zuo M, Jamal AJ, Rathod B, Wang JH, Li Z, Chao G, Rojas OL, Bang YM, Pu A, Christie-Holmes N, Gervais C, Ceccarelli D, Samavarchi-Tehrani P, Guvenc F, Budylowski P, Li A, Paterson A, Yue FY, Marin LM, Caldwell L, Wrana JL, Colwill K, Sicheri F, Mubareka S, Gray-Owen SD, Drews SJ, Siqueira WL, Barrios-Rodiles M, Ostrowski M, Rini JM, Durocher Y, McGeer AJ, Gommerman JL, Gingras A-C. Persistence of serum and saliva antibody responses to SARS-CoV-2 spike antigens in COVID-19 patients. Sci Immunol 2020;5:eabe5511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization . Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Geneva, Switzerland: World Health Organization; 2019. Available at: http://www.who.int/emergencies/mers-cov/en/. Accessed August 3, 2020. [Google Scholar]
- 32.World Health Organization . Summary of Probable SARS Cases With Onset of Illness From 1 November 2002 to 31 July 2003. Geneva, Switzerland: World Health Organization; 2003. Available at: https://www.who.int/csr/sars/country/table2004_04_21/en/. Accessed August 3, 2020. [Google Scholar]
- 33.Taubenberger JK, Morens DM. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis 2006;12:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. medRxiv 2020. doi: 10.1101/2020.07.23.20160895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Driscoll M, Ribeiro Dos Santos G, Wang L, Cummings DAT, Azman AS, Paireau J, Fontanet A, Cauchemez S, Salje H. Age-specific mortality and immunity patterns of SARS-CoV-2. In: Nature [Internet] vol. 590. 2021:140–5. Available at: 10.1038/s41586-020-2918-0. [DOI] [PubMed] [Google Scholar]
- 36.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S. Epidemiology of COVID-19 among children in China. Pediatrics 2020;145:e20200702. [DOI] [PubMed] [Google Scholar]
- 37.Parri N, Lenge M, Buonsenso D. Children with COVID-19 in pediatric emergency departments in Italy. N Engl J Med 2020;383:187–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR. Are children less susceptible to COVID-19? J Microbiol Immunol Infect 2020;53:371–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Short KR, Kedzierska K, E van de Sandt C. Back to the future: lessons learned from the 1918 influenza pandemic. Front Cell Infect Microbiol 2018;8:343–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ferrer RA, Klein WMP, Persoskie A, Avishai-Yitshak A, Sheeran P. The tripartite model of risk perception (tririsk): distinguishing deliberative, affective, and experiential components of perceived risk. Ann Behav Med 2016;50:653–63. [DOI] [PubMed] [Google Scholar]
- 41.Tannenbaum MB, Hepler J, Zimmerman RS, Saul L, Jacobs S, Wilson K, Albarracín D. Appealing to fear: a meta-analysis of fear appeal effectiveness and theories. Psychol Bull 2015;141:1178–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mineka S, Öhman A. Phobias and preparedness: the selective, automatic, and encapsulated nature of fear. Biol Psychiatry 2002;52:927–37. [DOI] [PubMed] [Google Scholar]
- 43.LeDoux J, Daw ND. Surviving threats: neural circuit and computational implications of a new taxonomy of defensive behaviour. Nat Rev Neurosci 2018;19:269–82. [DOI] [PubMed] [Google Scholar]
- 44.LeDoux JE. Evolution of human emotion: a view through fear. Prog Brain Res 2012;195:431–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kachanoff FJ, Bigman YE, Kapsaskis K, Gray K. Measuring realistic and symbolic threats of COVID-19 and their unique impacts on well-being and adherence to public health behaviors. Soc Psychol Pers Sci 2020. doi: 10.1177/1948550620931634. [DOI] [Google Scholar]
- 46.Peters G-JY, Ruiter RAC, Kok G. Threatening communication: a critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychol Rev 2013;7:S8–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rippetoe PA, Rogers RW. Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. J Pers Soc Psychol 1987;52:596–604. [DOI] [PubMed] [Google Scholar]
- 48.Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull 2014;140:511–43. [DOI] [PubMed] [Google Scholar]
- 49.Abraham CS, Sheeran P, Abrams D, Spears R. Exploring teenagers’ adaptive and maladaptive thinking in relation to the threat of HIV infection. Psychol Health 1994;9:253–72. [DOI] [PubMed] [Google Scholar]
- 50.Delirrad M, Mohammadi AB. New methanol poisoning outbreaks in Iran following COVID-19 pandemic. Alcohol Alcohol 2020;55:347–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Soltaninejad K. Methanol mass poisoning outbreak: a consequence of COVID-19 pandemic and misleading messages on social media. J Occup Environ Med 2020;11:148–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chang A. Cleaning and disinfectant chemical exposures and temporal associations with COVID-19—National Poison Data System, United States, January 1, 2020–March 31, 2020. MMWR; 2020. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6916e1.htm. Accessed August 3, 2020. [DOI] [PMC free article] [PubMed]
- 53.Reny TT, Barreto MA. Xenophobia in the time of pandemic: othering, anti-Asian attitudes, and COVID-19. Politics Groups Identities 2020;1–24. [Google Scholar]
- 54.Yamagata M, Teraguchi T, Miura A. The relationship between infection-avoidance tendency and exclusionary attitudes towards foreigners: a case study of the COVID-19 outbreak in Japan. PsyArXiv 2020. doi: 10.31234/osf.io/vhrqn. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.White AIR. Historical linkages: epidemic threat, economic risk, and xenophobia. Lancet 2020;395:1250–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav 2000;27:591–615. [DOI] [PubMed] [Google Scholar]
- 58.Dsouza DD, Quadros S, Hyderabadwala ZJ, Mamun MA. Aggregated COVID-19 suicide incidences in India: fear of COVID-19 infection is the prominent causative factor. Psychiatry Res 2020;290:113145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of us patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA 2020;3:e2017267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lai AG, Pasea L, Banerjee A, Hall G, Denaxas S, Chang WH, Katsoulis M, Williams B, Pillay D, Noursadeghi M, Linch D, Hughes D, Forster MD, Turnbull C, Fitzpatrick NK, Boyd K, Foster GR, Enver T, Nafilyan V, Humberstone B, Neal RD, Cooper M, Jones M, Pritchard-Jones K, Sullivan R, Davie C, Lawler M, Hemingway H. Estimated impact of the COVID-19 pandemic on cancer services and excess 1-year mortality in people with cancer and multimorbidity: near real-time data on cancer care, cancer deaths and a population-based cohort study. BMJ Open 2020;10:e043828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gollwitzer A, Martel C, Brady W, Knowles E, Bavel J. Partisan differences in physical distancing predict infections and mortality during the coronavirus pandemic. SSSR; 2020. Available at: https://ssrn.com/abstract=3609392 or http://dx.doi.org/10.2139/ssrn.3609392. Accessed August 3, 2020.
- 62.Bavel JJV, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ, Crum AJ, Douglas KM, Druckman JN, Drury J, Dube O, Ellemers N, Finkel EJ, Fowler JH, Gelfand M, Han S, Haslam SA, Jetten J, Kitayama S, Mobbs D, Napper LE, Packer DJ, Pennycook G, Peters E, Petty RE, Rand DG, Reicher SD, Schnall S, Shariff A, Skitka LJ, Smith SS, Sunstein CR, Tabri N, Tucker JA, van der Linden S, van Lange P, Weeden KA, Wohl MJA, Zaki J, Zion SR, Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 2020;4:460–71. [DOI] [PubMed] [Google Scholar]
- 63.Poteat T, Millett G, Nelson LE, Beyrer C. Understanding COVID-19 risks and vulnerabilities among Black communities in america: the lethal force of syndemics. Ann Epidemiol 2020;47:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shiau S, Krause KD, Valera P, Swaminathan S, Halkitis PN. The burden of COVID-19 in people living with hiv: a syndemic perspective. AIDS Behav 2020;24:2244–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health 2020;5:e186–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Centers for Disease Control and Prevention . Mental Health—Household Pulse Survey—COVID-19. Atlanta, GA: Centers for Disease Control and Prevention; 2021. Available at: https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm. Accessed January 19, 2021. [Google Scholar]
- 67.Czeisler MÉ. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep [Internet] 2020;69:1049–57. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6932a1.htm. Accessed January 19, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 2020;277:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Duan L, Shao X, Wang Y, Huang Y, Miao J, Yang X, Zhu G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord 2020;275:112–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Daly M, Sutin AR, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med 2020;1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet 2017;389:941–50. [DOI] [PubMed] [Google Scholar]
- 72.Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. In: Tob Induc Dis [Internet] vol. 18. 2020:20. Available at: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, Li Q, Jiang C, Zhou Y, Liu S, Ye C, Zhang P, Xing Y, Guo H, Tang W. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect 2020;81:e16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yu T, Cai S, Zheng Z, Cai X, Liu Y, Yin S, Peng J, Xu X. Association between clinical manifestations and prognosis in patients with COVID-19. Clin Ther 2020;42:964–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Guo FR. Smoking links to the severity of COVID-19: an update of a meta-analysis. J Med Virol 2020;92:2304–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Berlin I, Thomas D, Le Faou A-L, Cornuz J. COVID-19 and smoking. Nicotine Tob Res 2020;22:1650–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Patanavanich R, Glantz SA. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob Res 2020;22:1653–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiat 2020;77:891–2. [DOI] [PubMed] [Google Scholar]
- 79.Nemani K, Li C, Olfson M, Blessing EM, Razavian N, Chen J, Petkova E, Goff DC. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry 2021;e204442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Thakur V, Jain A. COVID 2019-suicides: a global psychological pandemic. Brain Behav Immun 2020;88:952–3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 81.Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav Immun 2020;87:23–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Griffiths MD, Mamun MA. COVID-19 suicidal behavior among couples and suicide pacts: case study evidence from press reports. Psychiatry Res 2020;289:113105–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res 2020;290:113104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Samson K, Sherry SB. Projected increases in suicide in Canada as a consequence of COVID-19 revisited. Psychiatry Res 2020;294:113492–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chang Y-H, Chang S-S, Hsu C-Y, Gunnell D. Impact of pandemic on suicide: excess suicides in Taiwan during the 1918–1920 influenza pandemic. J Clin Psychol 2020;81:13454–4. [DOI] [PubMed] [Google Scholar]
- 86.Cheung YT, Chau PH, Yip PSF. A revisit on older adults suicides and severe acute respiratory syndrome (SARS) epidemic in Hong Kong. Int J Geriatr Psychiatry 2008;23:1231–8. [DOI] [PubMed] [Google Scholar]
- 87.Wasserman IM. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life Threat Behav 1992;22:240–54. [PubMed] [Google Scholar]
- 88.Leaune E, Samuel M, Oh H, Poulet E, Brunelin J. Suicidal behaviors and ideation during emerging viral disease outbreaks before the COVID-19 pandemic: a systematic rapid review. Prev Med 2020;141:106264–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. 2021;5:229–38. [DOI] [PubMed] [Google Scholar]
- 90.Moore O. Suicides up sharply on Toronto subway during pandemic. Available at: https://www.theglobeandmail.com/canada/toronto/article-suicides-on-the-ttc-have-risen-sharply-over-the-last-eight-months/. Accessed January 19, 2021.
- 91.Wu P, Liu X, Fang Y, Fan B, Fuller CJ, Guan Z, Yao Z, Kong J, Lu J, Litvak IJ. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol 2008;43:706–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Katan M, Moon YP, Paik MC, Sacco RL, Wright CB, Elkind MSV. Infectious burden and cognitive function: the Northern Manhattan Study. Neurology 2013;80:1209–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, Worthman CM, Yardley L, Cowan K, Cope C, Hotopf M, Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020;7:547–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 2020;87:18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun 2020;87:34–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Goenka A, Michael BD, Ledger E, Hart IJ, Absoud M, Chow G, Lilleker J, Lunn M, McKee D, Peake D, Pysden K, Roberts M, Carrol ED, Lim M, Avula S, Solomon T, Kneen R. Neurological manifestations of influenza infection in children and adults: results of a national british surveillance study. Clin Infect Dis 2014;58:775–84. [DOI] [PubMed] [Google Scholar]
- 97.Kim JE, Heo JH, Kim HO, Song SH, Park SS, Park TH, Ahn JY, Kim MK, Choi JP. Neurological complications during treatment of Middle East respiratory syndrome. J Clin Neurol 2017;13:227–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Barreto de Araújo TV, Rodrigues LC, de Alencar Ximenes RA, de Barros Miranda-Filho D, Montarroyos UR, Lopes de Melo AP, Valongueiro S, de Fátima Pessoa Militão de Albuquerque M, Souza WV, Braga C, Filho SPB, Cordeiro MT, Vazquez E, Di Cavalcanti Souza Cruz D, Henriques CMP, Bezerra LCA, da Silva Castanha PM, Dhalia R, Marques-Júnior ETA, Martelli CMT. Association between Zika virus infection and microcephaly in Brazil, January to May, 2016: preliminary report of a case-control study. Lancet Infect Dis 2016;16:1356–63. [DOI] [PubMed] [Google Scholar]
- 99.Berger JR, Houff S. Neurological complications of herpes simplex virus type 2 infection. Arch Neurol 2008;65:596–600. [DOI] [PubMed] [Google Scholar]
- 100.Gilden DH, Kleinschmidt-DeMasters BK, LaGuardia JJ, Mahalingam R, Cohrs RJ. Neurologic complications of the reactivation of varicella-zoster virus. N Engl J Med 2000;342:635–45. [DOI] [PubMed] [Google Scholar]
- 101.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020;395:1417–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, De Leacy RA, Shigematsu T, Ladner TR, Yaeger KA, Skliut M, Weinberger J, Dangayach NS, Bederson JB, Tuhrim S, Fifi JT. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med 2020;382:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Poggesi A, Pasi M, Pescini F, Pantoni L, Inzitari D. Circulating biologic markers of endothelial dysfunction in cerebral small vessel disease: a review. J Cereb Blood Flow Metab 2016;36:72–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Song E, Zhang C, Israelow B, Lu-Culligan A, Prado AV, Skriabine S, Lu P, Weizman O-E, Liu F, Dai Y, Szigeti-Buck K, Yasumoto Y, Wang G, Castaldi C, Heltke J, Ng E, Wheeler J, Alfajaro MM, Levavasseur E, Fontes B, Ravindra NG, Van Dijk D, Mane S, Gunel M, Ring A, Jaffar Kazmi SA, Zhang K, Wilen CB, Horvath TL, Plu I, Haik S, Thomas J-L, Louvi A, Farhadian SF, Huttner A, Seilhean D, Renier N, Bilguvar K, Iwasaki A. Neuroinvasion of SARS-CoV-2 in human and mouse brain. bioRxiv 2020;doi: 10.1101/2020.06.25.169946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, Sultan M, Easton A, Breen G, Zandi M, Coles JP, Manji H, Al-Shahi Salman R, Menon DK, Nicholson TR, Benjamin LA, Carson A, Smith C, Turner MR, Solomon T, Kneen R, Pett SL, Galea I, Thomas RH, Michael BD, Allen C, Archibald N, Arkell J, Arthur-Farraj P, Baker M, Ball H, Bradley-Barker V, Brown Z, Bruno S, Carey L, Carswell C, Chakrabarti A, Choulerton J, Daher M, Davies R, Di Marco Barros R, Dima S, Dunley R, Dutta D, Ellis R, Everitt A, Fady J, Fearon P, Fisniku L, Gbinigie I, Gemski A, Gillies E, Gkrania-Klotsas E, Grigg J, Hamdalla H, Hubbett J, Hunter N, Huys A-C, Ihmoda I, Ispoglou S, Jha A, Joussi R, Kalladka D, Khalifeh H, Kooij S, Kumar G, Kyaw S, Li L, Littleton E, Macleod M, Macleod MJ, Madigan B, Mahadasa V, Manoharan M, Marigold R, Marks I, Matthews P, Mccormick M, Mcinnes C, Metastasio A, Milburn-McNulty P, Mitchell C, Mitchell D, Morgans C, Morris H, Morrow J, Mubarak Mohamed A, Mulvenna P, Murphy L, Namushi R, Newman E, Phillips W, Pinto A, Price DA, Proschel H, Quinn T, Ramsey D, Roffe C, Ross Russell A, Samarasekera N, Sawcer S, Sayed W, Sekaran L, Serra-Mestres J, Snowdon V, Strike G, Sun J, Tang C, Vrana M, Wade R, Wharton C, Wiblin L, Boubriak I, Herman K, Plant G. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry 2020;7:875–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2021;8:130–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 2021;8:416–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Centers for Disease Control and Prevention . Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep 2020;69:382–6. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6913e2.htm. Accessed August 3, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Richardson S Hirsch JS Narasimhan M Crawford JM McGinn T Davidson KW, the Northwell COVID-19 Research Consortium . Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 2020;323:2052–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:811–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;5:802–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;46:846–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gotts JE, Jordt S-E, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? BMJ 2019;366:l5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Grummon AH, Hall MG, Mitchell CG, Pulido M, Mendel Sheldon J, Noar SM, Ribisl KM, Brewer NT. Reactions to messages about smoking, vaping and COVID-19: two national experiments. Tob Control 2020. doi: 10.1136/tobaccocontrol-2020-055956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Baggish AL, Weiner RB, Kanayama G, Hudson JI, Lu MT, Hoffmann U, Pope HG, Jr. Cardiovascular toxicity of illicit anabolic-androgenic steroid use. Circulation 2017;135:1991–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Pope HG, Jr., Wood RI, Rogol A, Nyberg F, Bowers L, Bhasin S. Adverse health consequences of performance-enhancing drugs: an Endocrine Society scientific statement. Endocr Rev 2014;35:341–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lichtenfeld J, Deal BJ, Crawford S. Sudden cardiac arrest following ventricular fibrillation attributed to anabolic steroid use in an adolescent. Cardiol Young 2016;26:996–8. [DOI] [PubMed] [Google Scholar]
- 120.Grace SL, Medina-Inojosa JR, Thomas RJ, Krause H, Vickers-Douglas KS, Palmer BA, Lopez-Jimenez F. Antidepressant use by class: association with major adverse cardiac events in patients with coronary artery disease. Psychother Psychosom 2018;87:85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Federico MJ, McFarlane AE, Szefler SJ, Abrams EM. The impact of social determinants of health on children with asthma. J Allergy Clin Immunol 2020;8:1808–14. [DOI] [PubMed] [Google Scholar]
- 122.Abrams EM, Szefler SJ. Managing asthma during coronavirus disease-2019: an example for other chronic conditions in children and adolescents. J Pediatr 2020;222:221–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Raisi-Estabragh Z, McCracken C, Bethell MS, Cooper J, Cooper C, Caulfield MJ, Munroe PB, Harvey NC, Petersen SE. Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank. J Public Health (Oxf) [Internet] 2020;42:451–460. Available at: 10.1093/pubmed/fdaa095. Accessed August 10, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA 2020;323:2466–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hu H, Xiao H, Zheng Y, Yu BB. A Bayesian spatio-temporal analysis on racial disparities in hypertensive disorders of pregnancy in Florida, 2005–2014. Spat Spatiotemporal Epidemiol 2019;29:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gracia E, López-Quílez A, Marco M, Lila M. Mapping child maltreatment risk: a 12-year spatio-temporal analysis of neighborhood influences. Int J Health Geogr 2017;16:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mo C, Tan D, Mai T, Bei C, Qin J, Pang W, Zhang Z. An analysis of spatiotemporal pattern for COIVD-19 in China based on space-time cube. J Med Virol 2020;92:1587–95. [DOI] [PubMed] [Google Scholar]
- 128.Gee GC, Ro MJ, Rimoin AW. Seven reasons to care about racism and COVID-19 and seven things to do to stop it. Am J Public Health 2020;110:954–5. [Google Scholar]
- 129.Earnshaw VA, Katz IT. Educate, amplify, and focus to address COVID-19 misinformation. JAMA Health Forum 2020;1:e200460–0. [DOI] [PubMed] [Google Scholar]
- 130.Huynh QL, Devos T, Smalarz L. Perpetual foreigner in one’s own land: potential implications for identity and psychological adjustment. J Soc Clin Psychol 2011;30:133–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cheah C, Wang C, Ren H, Zong X, Cho HS, Xue X. COVID-19 racism and mental health in Chinese American families. Pediatrics 2020;146:e2020021816. [DOI] [PubMed] [Google Scholar]
- 132.Borja M, Jeung R, Horse AY, Gibson J, Gowing S, Lin N, Navins A, Power E. Anti-Chinese rhetoric tied to racism against Asian Americans Stop AAPI Hate Report; CAA; 2020. Available at: https://caasf.org/2020/06/anti-chinese-rhetoric-tied-to-racism-against-asian-americans-stop-aapi-hate-report/. Accessed January 19, 2021.
- 133.Dhanani LY, Franz B. Unexpected public health consequences of the COVID-19 pandemic: a national survey examining anti-Asian attitudes in the USA. Int J Public Health 2020;65:747–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Thrive Health . Canada COVID-19 App. Thrive Health; 2020. Available at: https://www.thrive.health/canada-covid19-app. Accessed August 3, 2020.
- 135.Sakib MN, Butt ZA, Morita PP, Oremus M, Fong GT, Hall PA. Considerations for an individual-level population notification system for pandemic response: a review and prototype. J Med Internet Res 2020;22:e19930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ly TTH. How Vietnam is winning its war against COVID-19. Asia Pacific Foundation of Canada; 2020. Available at: https://www.asiapacific.ca/publication/how-vietnam-winning-its-war-against-covid-19. Accessed August 3, 2020.
- 137.Cuan-Baltazar JY, Muñoz-Perez MJ, Robledo-Vega C, Pérez-Zepeda MF, Soto-Vega E. Misinformation of COVID-19 on the Internet: infodemiology study. JMIR Public Health Surveill 2020;6:e18444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Mian A, Khan S. Coronavirus: the spread of misinformation. BMC Med 2020;18:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Budhwani H, Sun R. Creating COVID-19 stigma by referencing the novel coronavirus as the “Chinese virus” on twitter: quantitative analysis of social media data. J Med Internet Res 2020;22:e19301–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, McKay R, Bennett K, Mason L, Gibson-Miller J, Levita L, Martinez AP, Stocks TVA, Karatzias T, Hyland P. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun 2021;12:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. In: Nat Med [Internet] vol. 20. 2020:1–4; Available at: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Daly M, Robinson E. Willingness to vaccinate against COVID-19 in the US: longitudinal evidence from a nationally representative sample of adults from April–October 2020. medRxiv 2020. doi: 10.1101/2020.11.27.20239970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Salali GD, Uysal MS. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol Med 2020;1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. medRxiv 2020. doi: 10.1101/2020.12.01.20241729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Xie W, Campbell S, Zhang W. Working memory capacity predicts individual differences in social-distancing compliance during the COVID-19 pandemic in the United States. Proc Natl Acad Sci U S A 2020;117:17667–74. [DOI] [PMC free article] [PubMed] [Google Scholar]


