Abstract
Background:
Laparoscopic Adrenalectomy (LA) has rapidly become the gold standard in management of adrenal tumors as it has been found to be associated with better cosmoses, shorter hospital stay and rapid convalescence.
Objective:
The aim of this study was to compare laparoscopic and open approach to adrenal glands in terms of operative time, hospital stay, indications and blood loss at a tertiary medical center in Jordan.
Methods:
A retrospective comparative study which included all patients who underwent adrenalectomy (open or laparoscopic) from 2005 to 2015 at King Hussein Medical Center (KHMC). Patients’ demographics ,outcomes and essential study variables were extracted from patients’ files. Data analysis was performed using SPSS17 and Stata 10.
Results:
One hundred and three patients (mean age 44.9 years) were included, 90.2% of them underwent laparoscopic adrenalectomy. The size of the tumors ranged from 2 to 17 cm (mean 6.6 cm).The operative time, blood loss and hospital stay were significantly less in the laparoscopic group (P value <0.001). Patients in Open group had a significantly higher risk of incomplete excision of the tumors (P value=0.020).
Conclusion:
Laparoscopic adrenalectomy is associated with decreased operative time, blood loss and hospital stay compared to open approach. Tumor size and its malignant potential should be no more regarded as an absolute contraindication to laparoscopic adrenal surgery.
Keywords: Laparoscopic adrenalectomy, open adrenalectomy, adrenal tumors
1. BACKGROUND
The widespread use of non-invasive imaging methods (ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI)) has greatly improved the rate of early detection of adrenal masses. Adrenalectomy is indicated in most functional adrenal neoplasms and large incidentalomas. The traditional open surgical techniques require a large incision or even resection of 12th rib for the adequate exposure (1, 2).
Laparoscopic adrenalectomy (LA) was first described by Gagner et al in 1992 and has rapidly become the gold standard of treatment for benign adrenal tumors. It is associated with significantly decreased morbidity, shorter length of hospital stay, more rapid convalescence, and improved cosmoses compared with open resection (3, 4).
It was not until 2005 we began to perform LA at King Hussein Medical Center (KHMC).
2. OBJECTIVE
The aim of this study was to compare laparoscopic and open adrenalectomy in terms of length of hospital stay, blood loss, indications and adequacy of resection in patients who underwent the procedure at KHMC.
3. MATERIALS AND METHODS
This was a retrospective study in which all patients who underwent adrenalectomy (open or laparoscopic) from 2005 to 2015 at KHMC were included. The patient’s files were reviewed after the study had been approved by the institutional board review (IRB) at Royal Medical Services. The information collected from files included patient’s demographics, preoperative and histopathological diagnosis, adrenal size by computed tomography scan and histopathology, functionality of the tumor, the status of resection margins, operation time, intraoperative blood loss and length of hospital stay.
Data analyzed using SPSS 17 and Stata 10 for windows. Descriptive statistics and student t tests were used for means and frequency calculations. Chi square and logistic regressions were used for binary variables while linear regression was used for other variables. P value less than 0.05 is considered statistically significant.
4. RESULTS
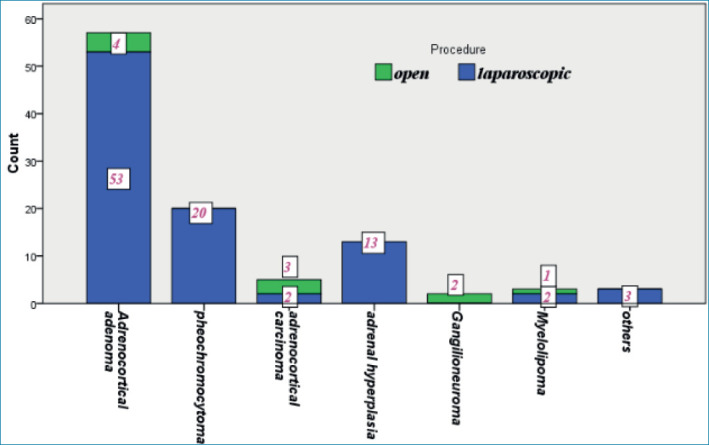
One hundred and three patients, with a mean age of 45 years (range 14-75), were included. Most of them (90.3%) underwent LA rather than open adrenalectomy. Table 1 shows comparison and the statistical significance of the parameters assessed. The patients in both groups were not different in terms of age, sex, side of surgery or functional status of the tumors. 77.5% of tumors were non-functional. All functional tumors were operated by laparoscopic approach. Male patients were found more likely to have functional tumors than females (odds ratio, 3.54; 95% CI, 1.33-9.4; P = 0.009). Also younger patients have been found more likely to have functional tumors even when corrected for sex and tumor size (P=0.014). The size of the tumor was significantly larger in open compared to LA group. All tumors of 9 centimeter (cm) or less were operated by laparoscopic approach, and all tumors of 10 cm or more were operated by open approach. A strong positive correlation was found between the preoperative size measured on CT scan and postoperatively on the histopathology report (r = 0.955, P<0.001). Figure 1 shows the final histopathological diagnosis for patients in open and laparoscopic groups.
Table I. Patients demographics, clinical and perioperative data.
| Laparoscopic Adrenalectomy n=93 | Open adrenalectomy n=10 | P value | |
|---|---|---|---|
| Age Mean Range |
44.6 14-75 |
48 21-73 |
0.5 |
| Gender Male Female |
28 65 |
5 5 |
0.2 |
| Side Right Left Bilateral |
30 62 1 |
4 6 0 |
0.847 |
| Functionality Functional Nonfunctional |
22 69 |
0 10 |
0.19 |
| Excision Complete Incomplete |
89 3 |
8 2 |
0.02 |
| Size on CT(cm) Mean Range |
4.4 2-8 |
9.7 7-14 |
<0.001 |
| Size on histopathology(cm) Mean Range |
5.9 2-9 |
12.2 10-17 |
<0.001 |
| Operative time(minutes) Mean Range |
71 40-100 |
115 100-140 |
<0.001 |
| Estimated blood loss(ml) Mean Range |
48 10-130 |
138 70-200 |
<0.001 |
| Hospital stay(days) Mean Range |
2 1-4 |
3.4 3-4 |
<0.001 |
Figure 1. Final histopathological diagnosis for both patients groups.
Estimated intraoperative blood loss, operative time and hospital stay were more in the patients who underwent open adrenalectomy than LA (P<0.001). Regression analysis showed that intraoperative blood loss was an independent factor that increased both operative time and hospital stay (P values were <0.001 and 0.006,respectively). In addition, there was a strong positive correlation between tumor size and blood loss, hospital stay and operative time (r = 0.744, 0.546 and 0.725, respectively, P<0.001).-However, there was no difference in respect to the side of surgery (P values were 0.992,0.227 and 0.566, respectively).
5. DISCUSSION
From the surgical point of view, the adrenal glands are considered relatively inaccessible due to their small size, fragility and their retroperitoneal location deep inside the fat. Propper exposure requires extensive incisions much larger than their size. Because of this, LA represented an attractive alternative to open approach since first report of LA in 1992 (3, 5, 6). Adrenal tumors which need surgical intervention are broadly classified into functional or nonfuctional. In our study, supported by other studies (1, 5, 7-9) , the majority of operated tumors were non-functional. Younger patients were found to be more likely to have functional tumors, but in contrary to what reported by Wooten and King (10), we found that males were more likely than females to have functional adrenal tumors. Two controversial issues are found in the selection of patients for either open or laparoscopic techniques: the size of the tumor and the presence of malignancy. Recently most author’s advice offering LA for tumors not exceeding 8 cm (11-13), although others reported successful LA for tumors up to 12 cm (14) and even Fiszer P et al (15) reported an 18 cm tumor removed successfully via laparoscopic approach. In the present study, all tumors of 9 cm or less in diameter were operated laparoscopically, whereas open surgery was offered to tumors of 10 cm or more. The other controversial area in LA is the suspicion or the presence of malignancy. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), in its 2013 published Guidelines for minimally invasive treatment for adrenal pathology, did not recommend laparoscopic surgery for tumors suspected to be malignant especially if more than 6 cm in diameter (16), on the other hand, the European Society of Endocrine Surgeons has suggested that LA can be considered for stage I and II adrenocortical carcinoma with tumors <10 cm in size(17). In their systematic review, Norman et al (3) concluded that open approach is recommended in patients with tumor invasion, vascular thrombi, and lesions larger than 10 cm, however, there is concern regarding the ability to achieve consistent oncological resection of lesions between 6 and 10 cm by LA and there is a need for further research in this area. The choice of LA over open approach is not related only to smaller incisions and better exposure. In the present study, we found that estimated intraoperative blood loss was significantly less with LA, which is consistent with other studies (2, 21, 24). Also, the postoperative hospital stay length was significantly less with the laparoscopic approach, a finding that has been proved by most other authors (2, 6, 21-26). The operation time was found in our study to be less with LA in keeping with other studies (21, 24, 25), although others found that this time was similar (2) to open approach or even longer (6). Of note, we found that operative time, estimated blood loss and hospital stay were significantly increased as the size of the tumor increased. This finding was reported by some authors (13, 14), although Serji B et al (20) showed that only operation time will increase as tumor size increases. We didn’t find in this study any significant difference in these parameters (blood loss, operation time, hospital stay) between left and right sided tumors. This was reported by other authors (18, 19) who concluded that the popular say that right sided surgery is more difficult than left sided is not justified. Other advantages for LA reported in the literature was the decrease in pain scale and analgesia demand (2), while overall complications rate was similar (2) or even less with LA (6).
Our study has many limitations. First, information regarding postoperative complications and follow up could not be obtained. Second, details involving conversion rate could not be clearly extracted from patients’ files.
6. CONCLUSION
LA has become the gold standard in adrenal surgery. We found that it has the benefits of decreased operative time, decreased intraoperative blood loss and decreased hospital stay without jeopardizing the complete excision. The size of the tumor and its malignant potential should be no more regarded as an absolute contraindication for minimally invasive approach in adrenal surgery.
Patient Consent Form:
Appropriate patient consent forms were obtained.
Authors’ contributions:
All authors contributed equally to the manuscript and read and approved the final version of the manuscript.
Conflicts of interest:
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Financial support and sponsorship:
None.
REFERENCES
- 1.Filipponi S, Guerrieri M, Arnaldi G, Giovagnetti M, Masini AM, Lezoche E, et al. Laparoscopic adrenalectomy: a report on 50 operations. Eur J Endocrinol. 1998 May;138(5):548–553. doi: 10.1530/eje.0.1380548. [DOI] [PubMed] [Google Scholar]
- 2.Wu CT, Chiang YJ, Chou CC, Liu KL, Lee SH, Chang YH, et al. Comparative study of laparoscopic and open adrenalectomy. Chang Gung Med J. 2006 Sep-Oct;29(5):468–473. [PubMed] [Google Scholar]
- 3.Oneil Machado N, al Qadhi Hani, al Wahaibi Khalifa, Rizvi Syed G. Laparoscopic Adrenalectomy for Large Adrenocortical Carcinoma. JSLS. 2015 Jul-Sep;19(3):e2015.00036. doi: 10.4293/JSLS.2015.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teo XL, Lim SK. Robotic assisted adrenalectomy: Is it ready for prime time? Investig Clin Urol. 2016 Dec;57(Suppl 2):S130–S146. doi: 10.4111/icu.2016.57.S2.S130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marek-Safiejko M, Safiejko K, Łukaszewicz J, Dadan J, Ładny RJ, Kozłowski R, et al. A Comparison of Two Approaches to Laparoscopic Adrenalectomy: Lateral Transperitoneal Versus Posterior Retroperitoneal Approach. Adv Clin Exp Med. 2016;25(5):829–835. doi: 10.17219/acem/62347. [DOI] [PubMed] [Google Scholar]
- 6.Ramachandran MS, Reid JA, Dolan SJ, Farling PA, Russell CEY. Laparoscopic adrenalectomy versus open adrenalectomy: results from a retrospective comparative study. Ulster Med J. 2006 May;75(2):126–128. [PMC free article] [PubMed] [Google Scholar]
- 7.Ari A, Buyukasik K, Tatar C, Segmen O, Ersoz F, Arikan S, et al. Laparoscopic Treatment of Adrenal Tumors: A Single-Center Experience with 58 Patients. Surg Res Pract. 2016;2016:9574391. doi: 10.1155/2016/9574391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khanna S, Priya R, Bhartiya SK, Basu S, Shukla VK. Adrenal tumors: An experience of 10 years in a single surgical unit. Indian J Cancer. 2015 Jul-Sep;52(3):475–478. doi: 10.4103/0019-509X.176749. [DOI] [PubMed] [Google Scholar]
- 9.Kim J, Hyun Bae K, Choi Kyung Y, Jeong Ji Yun, Park Keun Gyu, Kim Jung Guk, et al. Clinical Characteristics for 348 Patients with Adrenal Incidentaloma. Endocrinol Metab (Seoul) 2013 Mar;28(1):20–25. doi: 10.3803/EnM.2013.28.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wooten MD, King DK. Adrenal cortical carcinoma. Epidemiology and treatment with mitotane and a review of the literature. Cancer. 1993 Dec 1;72(11):3145–3155. doi: 10.1002/1097-0142(19931201)72:11<3145::aid-cncr2820721105>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 11.Staren ED, Prinz RA. Adrenalectomy in the era of laparoscopy. Surgery. 1996;120:706–709. doi: 10.1016/s0039-6060(96)80020-1. [DOI] [PubMed] [Google Scholar]
- 12.Gupta PK, Natarajan B, Pallati PK, Gupta H, Sainath J, Fitzgibbons RJ., Jr Outcomes after laparoscopic adrenalectomy. Surg Endosc. 2011;25:784–794. doi: 10.1007/s00464-010-1256-y. [DOI] [PubMed] [Google Scholar]
- 13.Ibragimovich KS, Bazarbaevich BU, Parpijalilovich SD. Our Experience Videoendoscopic Adrenalectomy in Patients with Benign Adrenal Tumors Large Sizes. American Journal of Medicine and Medical Sciences. 2017;7(1):11–13. [Google Scholar]
- 14.Boylu U, Oommen M, Lee BR, Thomas R. Laparoscopic adrenalectomy for large adrenal masses: pushing the envelope. J Endourol. 2009 Jun;23(6):971–975. doi: 10.1089/end.2008.0555. [DOI] [PubMed] [Google Scholar]
- 15.Fiszer P, Toutounchi S, Pogorzelski R, Krajewska E, Sutkowski B, Gierej P, et al. Is tumor size a contraindication to laparoscopic adrenalectomy? Case report. Videosurgery and other Miniinvasive Techniques. 2012;7(2):144–146. doi: 10.5114/wiitm.2011.25931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stefanidis D, Goldfarb M, Kercher K, Hope W, Richardson W, Fanelli R. Guidelines for the Minimally Invasive Treatment of Adrenal Pathology. Society of American Gastrointestinal and Endoscopic Surgeons. Surg Endosc. 2013;27(11):3960–3980. doi: 10.1007/s00464-013-3169-z. [DOI] [PubMed] [Google Scholar]
- 17.Henry JF, Peix JL, Kraimps JL. Positional statement of the European Society of Endocrine Surgeons (ESES) on malignant adrenal tumors. Langenbecks Arch Surg. 2012;397:145–146. doi: 10.1007/s00423-011-0893-5. [DOI] [PubMed] [Google Scholar]
- 18.Kokorak L, Soltes M, Vladovic P, Marko L. Laparoscopic left and right adrenalectomy from an anterior approach - is there any difference? Outcomes in 176 consecutive patients. Wideochir Inne Tech Maloinwazyjne. 2016;11(4):268–273. doi: 10.5114/wiitm.2016.64767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cianci P, Fersini A, Tartaglia N, Ambrosi A, Neri V. Are there differences between the right and left laparoscopic adrenalectomy? Our experience. Ann Ital Chir. 2016;87:242–246. [PubMed] [Google Scholar]
- 20.Serji B, Souadka A, Benkabbou A, Hachim H, Jaiteh L, Mohsine R, et al. Feasibility and safety of laparoscopic adrenalectomy for large tumors. Arab J Urol. 2016 May 19;14(2):143–146. doi: 10.1016/j.aju.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Popov Z, Jankulovski N, Stankov O, Stavridis S, Saidi S, Kuzmanoski M, et al. Laparoscopic Adrenalectomy: First Single-Center Experience in the Balkans. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2015;36(3):27–33. doi: 10.1515/prilozi-2015-0075. [DOI] [PubMed] [Google Scholar]
- 22.Wittayapairoch J, Jenwitheesuk K, Punchai S, Saeseow OT, Thanapaisal C, Paonariang K. Laparoscopic Adrenalectomy: 6 Years’ Experience in Srinagarind Hospital. J Med Assoc Thai. 2015 Aug;98(Suppl 7):S174–178. [PubMed] [Google Scholar]
- 23.Autorino R, Bove P, De Sio M, Miano R, Micali S, Cindolo L, et al. Open Versus Laparoscopic Adrenalectomy for Adrenocortical Carcinoma: A Meta-analysis of Surgical and Oncological Outcomes. Ann Surg Oncol. 2016 Apr;23(4):1195–1202. doi: 10.1245/s10434-015-4900-x. [DOI] [PubMed] [Google Scholar]
- 24.Yamashita S, Ito K, Furushima K, Fukushima J, Kameyama S, Harihara Y. Laparoscopic versus open adrenalectomy for adrenal myelolipoma. Annals of Medicine and Surgery. 2014;3(2):34–38. doi: 10.1016/j.amsu.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lyu X, Liu L, Yang L, Gao L, Wei Q. Surgical management of adrenal cysts: a single-institution experience. Int Braz J Urol. 2014 Sep-Oct;40(5):656–665. doi: 10.1590/S1677-5538.IBJU.2014.05.11. [DOI] [PubMed] [Google Scholar]
- 26.Zeh HJ, Udelsman R. One hundred laparoscopic adrenalectomies: a single surgeon’s experience. Ann Surg Oncol. 2003 Nov;10(9):1012–1017. doi: 10.1245/aso.2003.06.001. [DOI] [PubMed] [Google Scholar]


