Abstract
Background:
Cesarean section (CS) rates have been increasing worldwide with different effects on maternal and neonatal health. Factors responsible for the growing trend of CSs, include maternal characteristics, medical insurance and convenient scheduling or financial incentives. Effective interventions and guidelines are required to reduce CS rates.
Objective:
The aim of this research was to investigate the factors contributing to CS rate increase and their correlation with international guidelines.
Methods:
The performed analysis included the available socio-demographic and medical information retrieved from the medical records and a related questionnaire in both emergency and elective CSs.
Results:
Out of the included 633 births, the cesarean delivery rate was 58%. Women with a previous CS showed higher percentages for Elective CS (66.1%) compared to Emergency CSs for the same reasons (8.9%). Furthermore, 23% of the patients underwent an Emergency CS because of failure of labor to progress while 18% of CSs were due to maternal desire.
Conclusion:
The high rates of CS in Greece demonstrate the lack of use of international obstetric protocols, national strategies, Cesarean Section audits and a significant shortage of midwives. A decrease in iatrogenic and non-iatrogenic factors leading to the primary CS will decrease CS rates.
Keywords: Cesarean Section, elective cesarean section, emergency cesarean section, risk factors for cesarean sections, cesarean section and international guidelines
1. BACKGROUND
Cesarean Section (CS) rates have been increasing in recent decades worldwide with negative effects on maternal and neonatal health (1). CS is associated with an increased risk of intra- and postoperative complications (2), infant’s obesity, diabetes, respiratory morbidity, and atopic dermatitis in childhood (3, 4) and an increased risk of placenta previa in subsequent pregnancies (5, 6).
The World Health Organization (WHO) indicated that both very low and very high CS rates could be dangerous, that the ideal CS rate ranges from 10% to 15% (7) and emphasized that a CS rate >10% is not associated with a reduction in maternal-neonatal mortality. In northern Europe, most countries have maintained CS rates <20%, with very low perinatal mortality rates (8) while in Greece, over 50% of the deliveries are cesarean deliveries. The actions implemented to reduce CS were evaluated during the 54th session of the United Nations Committee for the Elimination of Discrimination against Women. The results announced in Greece, concerned recommendations for the reduction of unnecessary CS, by training medical personnel on natural birth and introduce strict medical indications for CSs (9). Therefore, the WHO/Europe organized a review to identify important factors leading to CS and develop policy recommendations to improve the situation in Greece (10). Apart from Greece, CS rates were very high in Cyprus, Romania, Bulgaria, Poland, Hungary (11) resulting in financial burden of health services (12).
Risk factors associated with CS deliveries include purported medical and non-medical indications, such as maternal characteristics (13, 14), medical insurance and convenient scheduling or financial incentives (13). In Greece, there has been a gradual commercialization of maternity services, as deliveries taking place in the private sector, and this increase may be due in part to the fact that private hospitals have been part of the stock market since the late 1990s (13). In addition, the Greek public health system itself is funded by a mix of public and private sources with much higher compensation for CS than for vaginal delivery. All over Europe, Greece has the largest percentage of private funding for health care (13-15) and a black economy in the field of public obstetric services. Another significant factor is a previous CS. Attempting a vaginal birth after Cesarean (VBAC) is an opportunity to stop this vicious cycle considering that after the introduction of the transverse lower incision, the risk of uterine rupture was decreased (16). Other factors include the medical technological advances improving safety in operations (17) and even financial incentives or the physicians’ convenient scheduling (13, 18), the relatively high number of gynecologists (19) and the low number of midwives resulting in predominantly medical-orientated health care (13, 20-22).
The estimated CS frequency in Greece has been increasing in the past 4 decades, recording a percentage of 13.8% (1977-1983), 17.3% (1984-1988), 22.7% (1989-1993), 29.9% (1994-2000) (23) and the continuing dramatic increase exceeded 50% of all deliveries in 2016 (10). After 2000, Greece does not give official birth rates by CS in international organizations (24). The aim of this research was the problem of CS in Greece, through the investigation of causes and factors depending on the type of CS and their correlation with clinical and non-clinical interventions.
Interventions to reduce CS rates
Clinical interventions target specific clinical practices on an individual woman which in addition to the economic benefits of a country’s health system, they significantly reduce the escalation of CS rates and maternal morbidity associated with multiple CS (25). The WHO in 2016 and 2018 has issued relevant guidelines (26, 27) including recommendations to reduce CS use, emphasizing that induction of labor should be done for women who are known with certainty to have reached 41 weeks of gestation (28). Programs of childbirth training workshops for mothers and couples and psychoeducation led by midwives, are recommended to reduce CS rates. It seems that CS audits and timely feedback to health-care professionals constitute an important factor to reduce CS rates. Furthermore, care provided primarily by midwives, with 24-hour back-up from an obstetrician is recommended to reduse CS rates. Finally, the equalization of physician fees for vaginal births and CS are considered necessary (29).
2. OBJECTIVE
The aim of this research was to investigate the factors contributing to the increase in the Cesarean Section rate and their correlation with international guidelines.
3. PATIENTS AND METHODS
Procedure and ethical considerations
The research was approved by: Ethics Committee of the University Hospital of Larisa, approval: 18838/08-05-2019. All women gave their written consent for their participation.
Methods and Study Design
This cross-sectional study took place from August 2019 to February 2020 at the maternity unit of the University Hospital of Larisa in Greece which is considered representative of Greek hospitals. The total sample size was 633 women who gave birth during the research period, out of whom 365 had undergone a CS delivery (EMCS and ELCS).
The data were collected from the women’s medical records and from a researcher’s questionnaire, following an interview on the 3rd postpartum day. Socio-demographic and financial data of women and information about the health of the mothers before, during, and after the surgery were collected. The causes that led to EMCS or ELCS were also recorded.
Statistical analysis
Quantitative variables were presented as mean values (SD) or as median values (interquartile range=IQR). Qualitative variables are expressed as absolute and relative frequency. For the comparisons of proportions, chi-square and Fisher’s exact tests were used. Logistic regression analyses were applied to explore the factors likely to be related to the type of c-section. Unadjusted and adjusted odds ratios with 95% confidence intervals were computed from the results of the logistic regression analyses. All statistic tests were two-tailed, with a significant set at p<0.05. All statistical analyses were performed with SPSS 22.0 for Windows (SPSS; Chicago, IL, USA).
4. RESULTS
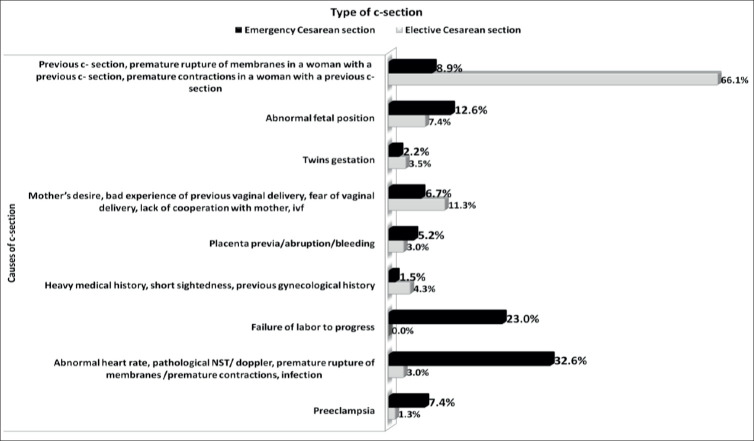
Of the 633 women who gave birth during the study period, 42% (n=268) had a vaginal delivery, 36% (n= 230) had an ELCS and 22% (n= 135) had an EMCS) (Figure 1).
Figure 1. Kind of delivery.
Demographic Characteristics of Participants
Total number of 365 women who had a CS were recruited and evaluated. Large areas of Greece with a general or university hospital providing obstetric services were designated as a “city”. Areas of Greece providing only primary health services and not a natural birth or a CS services were designated as a “village”. Both study groups showed a similarity in the family status, financial status, educational level, occupation, religion and minority groups showed similarity in the results in both study groups. Women with ELCS were more likely to live in rural areas or had a previous delivery and less likely to be of another nationality than Greek.
Causes of cesarean sections
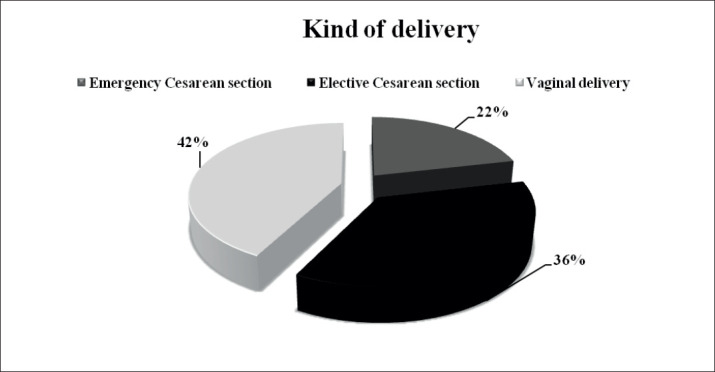
Figure 2 shows the rates of EMCS and elective CS as per the causes that provoked a CS. Women with a previous c-section, premature rupture of membranes and a previous CS, premature contractions and a previous CS had opted for ELCS at a higher rate (66.1%) compared to women who were forced to have an EMCS section with the same symptoms (8.9%).
Figure 2. Proportion of causes of Cesarean section according to the type of Cesarean section.
Factors associated with the type of CS
Univariate logistic regression analysis (ULRA) was initially conducted in order to define possible factors which were associated with the type of CS (Table 1). In turn, a multivariate logistic regression analysis (MLRA) was applied in order to clarify whether women undergo EMCS vs ELCS by including variable that were statistically significant (p<0.05). According to ULRA, the factors that were associated with the type of CS were address, age, nationality, parity, psychiatric history, pathology of gestation, gestational week, full-term labor, causes of CS and complications in early postpartum period. The MLRA (Table 1), showed that women residing in cities, with normal conception, diagnosed with stress disorders or depression, late preterm delivery and early postpartum complications after CS were more likely to undergo an EMCS. On the contrary, women with one previous birth or more than 2 births, diagnosed with oligohydramnios/polyhydramnios or placenta previa/abruption/bleeding during pregnancy and who had a previous CS with possible complications or past severe medical/gynecological history or vision problems (short sightedness) were less likely to undergo an EMCS.
Table 1. Results of logistic regression model for the factors associated with the type of CS +indicates reference category , ++could not be computed due to no distribution, OR=Odds Ratio, CI=Confidence Interval, *p<0.05.
| n=365 | Unadjusted OR | p-value | Adjusted OR | p-value |
|---|---|---|---|---|
| (95% CI) | (95% CI) | |||
| Address | ||||
| City | 2.525(1.340-4.758) | 0.004 | 5.532(1.681-18.203) | 0.005 |
| Village | 1.00+ | 1.00 | ||
| Age | 0.959(0.926-0.993) | 0.019 | 0.991(0.927-1.060) | 0.797 |
| Family status | ||||
| Single | 0.000000001526(0.000000001526-0.000000001526) | - | - | - |
| In relationship | 0.867(0.049-15.279) | 0.922 | - | - |
| Married | 0.577(0.036-9.308) | 0.698 | - | - |
| Divorced | 0.333(0.009-11.939) | 0.547 | - | - |
| Engaged | 1.00 | |||
| Educational level | ||||
| Primary school | 4(0.396-40.424) | 0.240 | - | - |
| Junior high school | 3.077(0.296-31.982) | 0.347 | - | - |
| High school | 1.885(0.205-17.308) | 0.575 | - | - |
| University | 2.381(0.259-21.902) | 0.444 | - | - |
| Msc | 4(0.383-41.744) | 0.247 | - | - |
| PhD | 1.00 | - | - | |
| Occupation | ||||
| Public/privatesector | 1.075(0.522-2.213) | 0.844 | - | - |
| Freelance | 1.220(0.541-2.750) | 0.632 | - | - |
| Health careprofessional | 0.824(0.291-2.332) | 0.715 | - | - |
| Educators | 1.361(0.537-3.450) | 0.516 | - | - |
| Household | 0.848(0.401-1.793) | 0.665 | - | - |
| Unemployed | 1.00 | - | - | |
| Financial status | ||||
| Low | 2.441(0.491-12.137) | 0.276 | - | - |
| Middle | 2.380(0.495-11.439) | 0.279 | - | - |
| High | 1.00 | - | - | |
| Religion | ||||
| OrthodoxChristians | 0.406(0.159-1.037) | 0.059 | - | - |
| Other | 1.00 | - | - | |
| Nationality | ||||
| Greek | 0.434(0.191-0.986) | 0.046 | 0.364(0.082-1.613) | 0.184 |
| Other | 1.00 | 1.00 | ||
| Minority | ||||
| Yes | 1.335(0.569-3.135) | 0.506 | - | - |
| No | 1.00 | - | - | |
| Parity | ||||
| 2 and morebirth | 0.153(0.075-0.309) | <0.001 | 0.252(0.067-0.943) | 0.041 |
| 1 birth | 0.131(0.076-0.224) | <0.001 | 0.274(0.075-1.003) | 0.050 |
| None | 1.00 | 1.00 | ||
| Type ofpreviouslabor | ||||
| Vaginal | 3.667(0.374-35.979) | 0.265 | - | - |
| C- section | 0.748(0.083-6.708) | 0.796 | - | - |
| Vaginal and c- section | 1.00 | - | - | |
| Kind of conception | ||||
| Normal | 1.389(0.640-3.014) | 0.406 | 20.679(3.863-110.698) | <0.001 |
| IVF | 1.00 | 1.00 | ||
| Psychiatric history | ||||
| Stress disorders | 3.649(1.432-9.301) | 0.007 | 12.940(2.643-63.350) | 0.002 |
| Postpartum mental disorders | 0.365(0.079-1.694) | 0.198 | 3.163(0.457-21.898) | 0.243 |
| Depression | 1.368(0.301-6.221) | 0.685 | 10.259(1.12-93.998) | 0.039 |
| Psychotic syndromes | 3.649(0.327-40.682) | 0.293 | 1.315(0.001-2841.057) | 0.944 |
| No | 1.00 | 1.00 | ||
| Atomichistory | ||||
| Low-risk | 0.816(0.441-1.510) | 0.517 | - | - |
| High-risk | 0.855(0.396-1.844) | 0.689 | - | - |
| No | 1.00 | - | - | |
| Gynecologicalhistory | ||||
| Intrauterine fetal demise/miscarriages/ recurrent miscarriages/ ectopic pregnancy | 1.57(0.672-3.667) | 0.297 | - | - |
| Surgeries | 0.571(0.059-5.550) | 0.629 | - | - |
| Uterine&Ovarian pathology | ++ | - | - | |
| Birth of a dead infant | 0.571(0.059-5.550) | 0.629 | - | - |
| No | 1.00 | - | - | |
| Pathology of gestation | ||||
| Oligohydramnios/ polyhydramnios | 0.467(0.054-4.069) | 0.490 | 0.020(0.001-0.750) | 0.034 |
| Preeclampsia/Increased impedanceto flow in the uterine arteries, thrombophilia, HELLP syndrome, hyperemesis | 2.852(1.439-5.651) | 0.003 | 0.322(0.078-1.322) | 0.116 |
| Placenta previa (type 4)/ abruption/ bleeding | 0.583(0.188-1.808) | 0.350 | 0.068(0.005-0.902) | 0.042 |
| Diabetes | 1.909(0.964-3.783) | 0.064 | 2.206(0.630-7.731) | 0.216 |
| Cervical insufficiency | 16.333(1.972-135.286) | 0.010 | 7.004(0.003-16488.187) | 0.623 |
| Premature contractions & Infection | 8.167(1.654-40.311) | 0.010 | 4.322(0.377-49.511) | 0.239 |
| Uteroplacental/ vascular/ insufficiency, single umbilical artery | 3.267(1.002-10.650) | 0.050 | 0.346(0.041-2.914) | 0.329 |
| No | 1.00 | 1.00 | ||
| Gestationalweek | 0.841(0.752-0.941) | 0.003 | 0.883(0.652-1.195) | 0.419 |
| Fulltermlaborornot | ||||
| 22- 27,6 (extremepreterm) | ++ | ++ | ++ | |
| 28-31+6 (verypreterm) | ++ | ++ | ++ | |
| 32-36+6(latepreterm) | 3.365(1.806-6.270) | <0.001 | 6.957(0.999-48.423) | 0.050 |
| 37-40+4(Fullterm) | 1.00 | 1.00 | ||
| Causes of CS | ||||
| Previous CS, premature rupture of membranes in a woman with a previous CS, premature contractions and a previous CS | 0.024(0.006-0.098) | <0.001 | 0.024(0.002-0.282) | 0.003 |
| Abnormal fetal position | 0.3(0.07-1.285) | 0.105 | 0.224(0.021-2.412) | 0.217 |
| Twins gestation | 0.113(0.018-0.716) | 0.021 | 0.179(0.011-2.806) | 0.221 |
| Mother’s desire, Bad experience of previous vaginal delivery, fear of vaginal delivery, lack of cooperation with mother, IVF | 0.104(0.023-0.464) | 0.003 | 0.134(0.011-1.566) | 0.109 |
| Placenta previa/abruption/bleeding | 0.3(0.057-1.581) | 0.156 | 0.737(0.035-15.293) | 0.843 |
| Heavy medical history, short sightedness, previous gynaecological history | 0.06(0.008-0.44) | 0.006 | 0.031(0.002-0.555) | 0.018 |
| Failure of labor to progress | ++ | 580797441.649(0-0) | 0.998 | |
| Abnormal heart rate, Pathological NST/ Doppler, premature rupture of membranes /premature contractions, infection | 1.886(0.414-8.594) | 0.412 | 3.062(0.313-29.919) | 0.336 |
| Preeclampsia | 1.00 | 1.00 | ||
| Early Postpartum Complications | ||||
| (bleeding, preeclampsia, infection, early postpartum mental disorders) | 4.022(1.764-9.172) | 0.001 | 13.430(2.834-63.646) | 0.001 |
| No | 1.00 | 1.00 |
5. DISCUSSION
This is the first research to have used data from a group of postpartum women to identify and explore factors associated with emergency or elective Cesarean deliveries in Greece. It was revealed an increasing rate in both EMCS and ELCS. The results show that the CS rate was 36% for ELCS and 22% for EMCS (Figure 1). Although several studies which investigated the CS socio-demographic factors have shown maternal age, educational and financial levels as key factors (30), in this research living in rural areas seems to be a determining factor for ELCS due to possible insecurity for both women and physicians in those areas.
Although a previous CS does not necessarily mean a scheduled CS in next pregnancy (31, 32), the ELCS rates of our findings were 66.1% for women with a previous CS, while in Germany it is just under 24% (14). This phenomenon may be explained by the obstetrician’s fear of uterine rupture although the estimated prevalence of this complication is very low (33). VBAC rates in Germany, Italy and Ireland are significantly lower (29-36%) than they are in Finland, Netherland and Sweden (45-55%) and about 160.000 unnecessary CSs are performed every year (34). In Greece, there is no officially recorded percentage of VBAC.
Previous abdominal surgeries seem to have influenced the obstetricians’ decision for a scheduled CS, without documented literature to support this approach (35). Uterine rupture occurs at a frequency of <1% in women with a previous uterine scar. In theory, an increased number of CSs is associated with an increased risk of uterine rupture (36). In addition, the literature shows that women with a several medical history (37) are also more likely to have an ELCS and this is also supported by the findings of our study. Furthermore, there is no sufficient evidence for ELCS in the relevant literature pertaining to short-sightedness, which was a risk factor for ELCS in this research (38).
In our research, the ELCS rates appear to be affected by the type of conception and other factors. Precious pregnancies of women with IVF conception, a high risk of placenta accreta (39) and, in some cases, the maternal age (40) constitute factors for ELCS. In our study, women with anxiety disorder or depression were more likely to have an EMCS, a comparable finding of similar studies (41, 42) revealing a deficit in perinatal mental health services in Greece (43, 44) as opposite to other European countries with low CS rates (45, 46).
Women with pathology of gestation are more likely to have a scheduled CS, in relation to women without such problems (47). For these reasons, such pregnancies are considered high risk and are usually scheduled for ELCS in Greece. On the other hand, placenta previa rates have increased and are likely to continue to increase as a result of CS deliveries. The aim of ELCS is to secure the safest route of delivery, to avoid the anticipated risks of bleeding during vaginal delivery due to the position of the placenta. These complications resulting from the above pregnancy conditions would pose a greater risk compared to a routine ELCS (48).
Another important factor associated with EMCS in this research is low preterm delivery (32-36, 6 weeks). Women who gave birth during these weeks were more likely to undergo an EMCS, especially when there was an underlying pregnancy pathology (49). In Greece, the meaning of emergency does not really apply because the term EMCS includes cases of relevant medical indications, i.e. a previous CS is a relevant and not an absolute indication such as hemorrhage, preeclampsia, pathological Doppler, leading in most cases again to a CS. In general, an individual approach to assessing the urgency for surgery must be implemented (50). In addition to prematurity, EMCS is also associated with a greater likelihood of postpartum complications. CS is a major surgery with high morbidity rates; however, the urgent nature of surgery after obstetric complications (eg, bleeding, preeclampsia, sepsis) seems to be related to postpartum complications. In Greece, another very important factor associated with CS, mainly EMCS, is the termination of pregnancy, which is usually done between 39-40 weeks, in addition to WHO recommendations (28) and other European countries which accept as a limit 42 weeks (24). In 2015, according to European Perinatal Health report, maternal and infant perinatal mortality rates in Greece, were similar to other European countries which have lower rates of CS, than Greece (24). This observation indicates the existence of unnecessary CS as well as the lack of national strategies.
6. CONCLUSION
In Greece of financial crisis, women continue to give birth by CS, with adverse consequences on the insurance funds, on their (mental and physical) and their child health, and on their decision for future pregnancies. The high CS rates must be confronted with less interventionist obstetricians practice when not needed and a focus on midwifery-obstetrician model of staffing, based on primarily by midwives. To reduce CS rates, financial strategies (insurance reforms which will compensate more in vaginal births and less for CSs) must also be implemented. In addition, there is a great need to establish psychoeducation centers for mothers and couples, and especially program for women with fear of pain, anxiety or other mental disorders. Finally, the uses of evidence-based clinical guidelines are recommended to reduce CS rates. In our results, both EMCS and ELCS factors are not in all cases related to absolute medical indications. The total CS rates are a combination of increased primary CS rates, as well as women with previous CS who had no choice of VBAC. Therefore, the 2 major goals of reducing CSs are the prevention of primary Cesarean deliveries and the management of women with previous CSs. In Greece, the increasing CS rates are major Public Health problem extending in the national economy and the human rights in childbirth.
Patient Consent Form:
All women were informed about the subject of the study and confirm their participation.
Author’s contribution:
E.A.: conceptualization, formal analysis, investigation, supervision, validation, visualization, writing original draft and editing. E.O: visualization, project administration and methodology. M.I. and A.S: investigation and methodology. E.P: validation. A.S: methodology, review and editing. G.I: methodology, review and editing, software analysis. M.D: review and editing, EA, AO, GI equally contributed to the study and made final proofreading.
Conflicts of interest:
There are no conflicts of interest.
Financial support and sponsorship:
None.
REFERENCES
- 1.Ayres-De-Campos D, Cruz J, Medeiros-Borges C, Costa-Santos C, Vicente L. Lowered national cesarean section rates after a concerted action. [2020 Apr 6];Acta Obstet Gynecol Scand (Internet) 2015 94(4):391–398. doi: 10.1111/aogs.12582. Available from: https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/aogs.12582. [DOI] [PubMed] [Google Scholar]
- 2.Field A, Haloob R. Complications of caesarean section. [2020 Apr 7];Obstet Gynaecol (Internet) 2016 18(4):265–272. Available from: https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/tog.12280. [Google Scholar]
- 3.Cardwell CR, Stene LC, Joner G, Cinek O, Svensson J, Goldacre MJ, et al. Caesarean section is associated with an increased risk of childhood-onset type 1 diabetes mellitus: a meta-analysis of observational studies. Diabetologia. 2008 May;51(5):726–735. doi: 10.1007/s00125-008-0941-z. [DOI] [PubMed] [Google Scholar]
- 4.Magnus MC, Håberg SE, Stigum H, Nafstad P, London SJ, Vangen S, et al. Delivery by Cesarean section and early childhood respiratory symptoms and disorders: the Norwegian mother and child cohort study. Am J Epidemiol. 2011 Dec 1;174(11):1275–1285. doi: 10.1093/aje/kwr242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Getahun D, Oyelese Y, Salihu HM, Ananth CV. Previous cesarean delivery and risks of placenta previa and placental abruption. Obstet Gynecol. 2006 Apr;107(4):771–778. doi: 10.1097/01.AOG.0000206182.63788.80. [DOI] [PubMed] [Google Scholar]
- 6.Betran A, Torloni M, Zhang J, Gülmezoglu A, Aleem H, Althabe F, et al. WHO Statement on Caesarean Section Rates. [2020 Mar 23];Bjog (Internet) 2016 Apr;123(5):667–670. doi: 10.1111/1471-0528.13526. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5034743/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bailey P, Lobis S, Fortney J, Maine D, et al., editors. Family Health International (Organization), Joseph L. Mailman School of Public Health. Monitoring emergency obstetric care: a handbook. Geneva, Switzerland: World Health Organization; 2009. p. 152. [Google Scholar]
- 8.Health at a Glance 2011: OECD Indicators (Internet) [2020 Sep 12]. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2011_health_glance-2011-en.
- 9.OHCHR | Committee on the Elimination of Discrimination against Women (Internet) [2020 Sep 15]. Available from: https://www.ohchr.org/en/hrbodies/cedaw/pages/cedawindex.aspx.
- 10.Greece commits to addressing excessive reliance on caesarean sections (Internet) World Health Organization. 2016. [2020 Apr 8]. Available from: http://www.euro.who.int/en/countries/greece/news/news/2016/11/greece-commits-to-addressing-excessive-reliance-on-caesarean-sections.
- 11.Large differences in share of caesarean births (Internet) [2020 Apr 8]. Available from: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/DDN-20191217-1.
- 12.Yu Y, Lin F, Dong W, Li H, Zhang X, Chen C. The effectiveness of financial intervention strategies for reducing caesarean section rates: a systematic review. [2020 Jun 20];BMC Public Health (Internet) 2019 19(1):1080. doi: 10.1186/s12889-019-7265-4. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mossialos E, Allin S, Karras K, Davaki K. An Investigation of Caesarean Sections in Three Greek Hospitals: The Impact of Financial Incentives and Convenience. Eur J Public Health. 2005 Jul 1;15:288–295. doi: 10.1093/eurpub/cki002. [DOI] [PubMed] [Google Scholar]
- 14.Mylonas I, Friese K. Indications for and Risks of Elective Cesarean Section. Dtsch Arzteblatt Int. 2015 Jul 20;112(29-30):48995. doi: 10.3238/arztebl.2015.0489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaitelidou DCh, Tsirona CS, Galanis PA, Siskou OCh, Mladovsky P, Kouli EG, et al. Informal payments for maternity health services in public hospitals in Greece. [2020 Aug 20];Health Policy (Internet) 2013 Jan;109(1):23–30. doi: 10.1016/j.healthpol.2012.10.012. Available from: https://linkinghub.elsevier.com/retrieve/pii/S016885101200293X. [DOI] [PubMed] [Google Scholar]
- 16.Cegolon L, Mastrangelo G, Maso G, Dal Pozzo G, Ronfani L, Cegolon A, et al. Understanding Factors Leading to Primary Cesarean Section and Vaginal Birth After Cesarean Delivery in the Friuli-Venezia Giulia Region (North-Eastern Italy), 2005–2015. [2020 Apr 11];Sci Rep (Internet) 2020 Jan 15;10(1):1–18. doi: 10.1038/s41598-019-57037-y. Available from: https://www.nature.com/articles/s41598-019-57037-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bragg F, Cromwell DA, Edozien LC, Gurol-Urganci I, Mahmood TA, Templeton A, et al. Variation in rates of caesarean section among English NHS trusts after accounting for maternal and clinical risk: cross sectional study. The BMJ (Internet) 2010. Oct 6, [2020 Apr 11]. p. 341. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2950923/ [DOI] [PMC free article] [PubMed]
- 18.Goyert GL, Bottoms SF, Treadwell MC, Nehra PC. The physician factor in cesarean birth rates. N Engl J Med. 1989 Mar 16;320(11):706–709. doi: 10.1056/NEJM198903163201106. [DOI] [PubMed] [Google Scholar]
- 19.Alran S, Sibony O, Oury J-F, Luton D, Blot P. Differences in management and results in term-delivery in nine European referral hospitals: descriptive study. Eur J Obstet Gynecol Reprod Biol. 2002 Jun 10;103(1):4–13. doi: 10.1016/s0301-2115(02)00028-3. [DOI] [PubMed] [Google Scholar]
- 20.Wang Z, Sun W, Zhou H. Midwife-led care model for reducing caesarean rate: A novel concept for worldwide birth units where standard obstetric care still dominates. [2020 Apr 12];J Med Hypotheses Ideas (Internet) 2012 Jan 1;6(1):28–31. Available from: http://www.sciencedirect.com/science/article/pii/S2251729412000146. [Google Scholar]
- 21.Pratilas GC, Sotiriadis A, Dinas K. Is high use of caesarean section sometimes justified? [2020 Apr 2];The Lancet (Internet) 2019 Jul 6;394(10192):25–26. doi: 10.1016/S0140-6736(19)30221-1. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)30221-1/abstract. [DOI] [PubMed] [Google Scholar]
- 22.Betrán AP, Temmerman M, Kingdon C, Mohiddin A, Opiyo N, Torloni MR, et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. [2020 Sep 14];The Lancet (Internet) 2018 Oct 13;392(10155):1358–1368. doi: 10.1016/S0140-6736(18)31927-5. Available from: http://www.sciencedirect.com/science/article/pii/S0140673618319275. [DOI] [PubMed] [Google Scholar]
- 23.Hesham H, Hesham M, Goodman A. Obstetric Care among Refugees: The Complex Interplay of Barriers to Care, Culture, Health Resources and the Healthcare Infrastructure of Host Countries. [2020 Jun 21];Open J Obstet Gynecol (Internet) 2019 Feb 1;9(2):170–185. Available from: http://www.scirp.org/Journal/Paperabs.aspx?paperid=90448. [Google Scholar]
- 24.European Perinatal Health Report 2015 - Euro-Peristat (Internet) [2020 Sep 18]. Available from: https://www.europeristat.com/index.php/reports/european-perinatal-health-report-2015.html.
- 25.Birth after Previous Caesarean Birth (Green-top Guideline No. 45) (Internet) Royal College of Obstetricians & Gynaecologists. [2020 Sep 15]. Available from: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg45/
- 26.WHO recommendations on antenatal care for a positive pregnancy experience (Internet) World Health Organization. [2020 Sep 14]. Available from: http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/ [PubMed]
- 27.WHO | WHO recommendations: intrapartum care for a positive childbirth experience (Internet) WHO. World Health Organization. [2020 Sep 14]. Available from: http://www.who.int/reproductivehealth/publications/intrapartum-care-guidelines/en/ [PubMed]
- 28.WHO | WHO recommendations for induction of labour (Internet) WHO. World Health Organization. [2020 Sep 14]. Available from: http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/9789241501156/en/
- 29.WHO | New WHO guidance on non-clinical interventions specifically designed to reduce unnecessary caesarean sections (Internet) WHO. World Health Organization. [2020 Sep 13]. Available from: http://www.who.int/reproductivehealth/guidance-to-reduce-unnecessary-caesarean-sections/en/
- 30.Manyeh AK, Amu A, Akpakli DE, Williams J, Gyapong M. Socioeconomic and demographic factors associated with caesarean section delivery in Southern Ghana: evidence from INDEPTH Network member site. [2020 Apr 15];BMC Pregnancy Childbirth (Internet) 2018 Oct 16;18 doi: 10.1186/s12884-018-2039-z. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6191905/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.ACOG Practice Bulletin No. 205: Vaginal Birth After Cesarean Delivery. [2020 Apr 11];Obstet Gynecol (Internet) 2019 Feb;133(2):e110. doi: 10.1097/AOG.0000000000003078. Available from: https://journals.lww.com/greenjournal/Abstract/2019/02000/ACOG_Practice_Bulletin_No__205__Vaginal_Birth.40.aspx. [DOI] [PubMed] [Google Scholar]
- 32.Bangal VB, Giri PA, Shinde KK, Gavhane SP. Vaginal Birth after Cesarean Section. [2020 Apr 14];North Am J Med Sci (Internet) 2013 Feb;5(2):140–144. doi: 10.4103/1947-2714.107537. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3624716/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vandenberghe G, Blaere MD, Leeuw VV, Roelens K, Englert Y, Hanssens M, et al. Nationwide population-based cohort study of uterine rupture in Belgium: results from the Belgian Obstetric Surveillance System. [2020 Apr 19];BMJ Open (Internet) 2016 May 1;6(5):e010415. doi: 10.1136/bmjopen-2015-010415. Available from: https://bmjopen.bmj.com/content/6/5/e010415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Optimisation of childbirth in Europe | Result In Brief | CORDIS | European Commission. [2020 Sep 17]. Available from: https://cordis.europa.eu/article/id/157755-optimisation-of-childbirth-in-europe.
- 35.Aduloju O, Akintayo A, Aduloju T. Uterine rupture in Ekiti State University Teaching Hospital, Ado-Ekiti: a review of presentation and outcome of management. [2020 Aug 19];Int Med (Internet) 2020 2(1):28. Available from: https://www.ejmanager.com/fulltextpdf.php?mno=66216. [Google Scholar]
- 36.Manoharan M, Wuntakal R, Erskine K. Uterine rupture: a revisit. [2020 Aug 18];Obstet Gynaecol (Internet) 2010 12(4):223–30. Available from: https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1576/toag.12.4.223.27613. [Google Scholar]
- 37.Amjad A, Amjad U, Zakar R, Usman A, Zakar MZ, Fischer F. Factors associated with caesarean deliveries among child-bearing women in Pakistan: secondary analysis of data from the Demographic and Health Survey, 2012–13. [2020 Apr 21];BMC Pregnancy Childbirth (Internet) 2018 Apr 23;18(1):113. doi: 10.1186/s12884-018-1743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sapuła-Grabowska M, Ciszewska J, Brydak-Godowska J, Sawa A, Laszewicz P, Bartha E, et al. Delivery in Myopic Women: A Comparison of Mode of Delivery in Years 1990, 2000, and 2010. [2020 Jun 21];Med Sci Monit Int Med J Exp Clin Res (Internet) 2019 Oct 14;25:7715–9. doi: 10.12659/MSM.916479. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6812470/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Esh-Broder E, Ariel I, Abas-Bashir N, Bdolah Y, Celnikier DH. Placenta accreta is associated with IVF pregnancies: a retrospective chart review. BJOG Int J Obstet Gynaecol. 2011 Aug;118(9):1084–9. doi: 10.1111/j.1471-0528.2011.02976.x. [DOI] [PubMed] [Google Scholar]
- 40.Egbe TO, Sandjon G, Ourtchingh C, Simo A, Priso EB, Benifla J-L. In-vitro fertilization and spontaneous pregnancies: matching outcomes in Douala, Cameroon. [2020 Apr 19];Fertil Res Pract (Internet) 2016 Jan 19;2(1):1. doi: 10.1186/s40738-015-0013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holka-Pokorska J, Jarema M, Stefanowicz A, Piróg-Balcerzak A, Wichniak A. Elective cesarean section on psychiatric indications – the phenomenon analysis, report of two cases and psychiatric clinical recommendations. [2020 Apr 21];Psychiatr Pol (Internet) 2016 50(2):357–73. doi: 10.12740/PP/43486. Available from: http://www.psychiatriapolska.pl/357_373. [DOI] [PubMed] [Google Scholar]
- 42.Orovou E, Dagla M, Iatrakis G, Lykeridou A, Tzavara C, Antoniou E. Correlation between Kind of Cesarean Section and Posttraumatic Stress Disorder in Greek Women. [2020 Mar 6];Int J Environ Res Public Health (Internet) 2020 Jan;17(5):1592. doi: 10.3390/ijerph17051592. Available from: https://www.mdpi.com/1660-4601/17/5/1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tzouvara V, Papadopoulos C. Public stigma towards mental illness in the Greek culture. J Psychiatr Ment Health Nurs. 2014 Dec;21(10):931–8. doi: 10.1111/jpm.12146. [DOI] [PubMed] [Google Scholar]
- 44.Johnson T. The Perinatal Mental Health Care Pathways: Full Implementation Guidance. 45 [Google Scholar]
- 45.Blomdahl Wetterholm M, Bendix M, Pettersson K, Lindefors N. (A Swedish example of integrated perinatal mental health care) Lakartidningen. 2018;17:115. [PubMed] [Google Scholar]
- 46.Yokoyama Y, Hakulinen T, Sugimoto M, Silventoinen K, Kalland M. Maternal subjective well-being and preventive health care system in Japan and Finland. [2020 Sep 18];Eur J Public Health (Internet) 2018 Aug 1;28(4):652–657. doi: 10.1093/eurpub/ckx211. Available from: https://academic.oup.com/eurpub/article/28/4/652/4764008. [DOI] [PubMed] [Google Scholar]
- 47.Hamza A, Herr D, Solomayer EF, Meyberg-Solomayer G. Polyhydramnios: Causes, Diagnosis and Therapy. [2020 Apr 23];Geburtshilfe Frauenheilkd (Internet) 2013 Dec;73(12):1241–1246. doi: 10.1055/s-0033-1360163. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3964358/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Palacios-Jaraquemada JM. Caesarean section in cases of placenta praevia and accreta. [2020 Jun 21];Best Pract Res Clin Obstet Gynaecol (Internet) 2013 Apr 1;27(2):221–232. doi: 10.1016/j.bpobgyn.2012.10.003. Available from: http://www.sciencedirect.com/science/article/pii/S1521693412001642. [DOI] [PubMed] [Google Scholar]
- 49.Romero R, Dey SK, Fisher SJ. Preterm labor: one syndrome, many causes. Science. 2014 Aug 15;345(6198):760–765. doi: 10.1126/science.1251816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schauberger CW, Chauhan SP. Emergency cesarean section and the 30-minute rule: definitions. Am J Perinatol. 2009 Mar;26(3):221–226. doi: 10.1055/s-0028-1103033. [DOI] [PubMed] [Google Scholar]