Abstract
Awareness about the occurrence of viral infectious (or other) tail risks can influence their socioeconomic inter-temporal impacts. In this regard, a branch of the literature finds that personal experiences with significant shocks can have long-lasting effects on risk-taking attitudes and the perceived probability about the occurrence of extreme, negative shocks. In this paper, we proxy the level of societal experience (awareness) in the face of the COVID-19 outbreak by past exposure of a country to epidemics, and other catastrophic events. We show that in a large cross-section of more than 150 countries, more aware societies suffered a less intense impact of the COVID-19 disease, in terms of loss of lives and, to some extent, economic damage.
Keywords: Socioeconomic impact of pandemics, Global health crises
1. Introduction
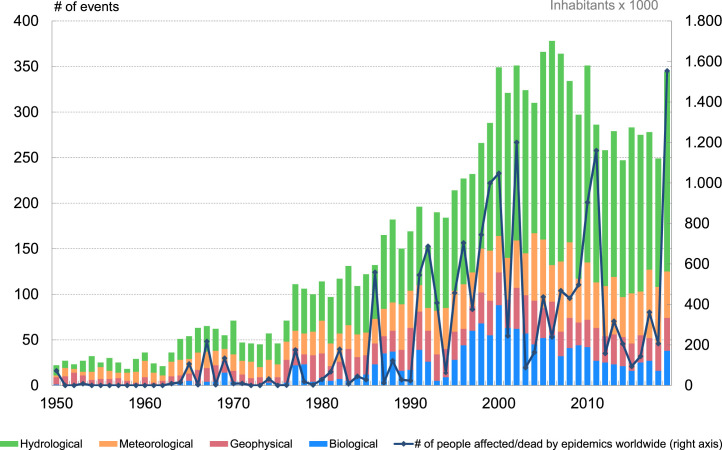
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2, the virus that causes COVID-19) came as a surprise for many individuals and nations, but not for others. Some governments and individuals were more aware of the possibility of a pandemic outburst of this sort than others, for at least two reasons: First, a big part of the scientific community had been warning for nearly one decade with increasing intensity about the likely appearance of “disease X” (see WHO, 2017, Daszah, 2020, de Bolle, 2021). On the other hand, some countries or regions may have more experience with this sort of events, insofar as they had been more affected than others in the past by infectious diseases (e.g. SARS in 2002, MERS in 2012, or Ebola in 2014) and/or other extreme natural events with very low frequency of impacting a given community. Such phenomena have become more frequent over the most recent decades (see Fig. 1). Societies that have experienced them in a not-so-distant past may be more prepared to identify a new episode – or a recurrent wave of an ongoing one (in case of biological events) – in an early fashion.
Fig. 1.
Worldwide biological and other natural, extreme, events per year, 1950-2020.
EM-DAT database: https://www.emdat.be/.
In this regard, a reference literature highlights the importance of individual experiences in shaping individuals’ behavior and beliefs. In economics, for example, Malmendier and Nagel (2011) show that personal experiences of economic fluctuations determine individuals’ willingness to take (financial) risk, while Giuliano and Spilimbergo (2014) find that the effect of recessions on beliefs is long-lasting. Kozlowski et al. (2020) show that agents’ experience with a pandemic could have enduring economic consequences as it may change their behavior in a persistent way, and Jordà et al. (2020) provide empirical evidence that pandemics do have long-run economic consequences.1 In turn, the epidemiological literature shows that individual awareness is a relevant factor to account for the spreading of an epidemic (see Granell et al., 2013, Wu et al., 2012, Samanta and Chattopadhyay, 2014, Wang et al., 2020).
We proxy the level of societal experience (awareness) in the face of the COVID-19 outbreak by past exposure of a country to viral outbreaks, and other catastrophic events, in order to test to what extent more aware societies suffered a less intense impact of the disease spread. To do so, we estimate spatial econometric models linking indicators of awareness and pandemic incidence (both human and economic) using a cross-section of some 150 countries across the world. We also include other geographical and socioeconomic controls, including lockdown and curfew-type measures adopted by governments, a key element identified in the literature (see e.g. Ferraresi et al., 2020).
The rest of this paper is organized as follows: In Section 2, we outline the econometric methodology and describe the data used. In Section 3 we discuss the main results of the paper and draw some policy implications.
2. Methodology and data
Methodology.
We regress, for a cross-section of around 150 countries, an indicator of the incidence of the pandemic () on an indicator of awareness (), and a number of control variables (), including a spatial lag. For country and time unit the model takes the form:
| (1) |
where captures the autocorrelation of the effects of the pandemic between close countries through the spatial weighting matrix . For countries, this object contains elements where the element captures the distance from country to country . The main diagonal is filled with zeros. Accounting for the proximity among countries is key, given that the health situations of closer geographies are likely to be more connected. While the concept of distance can refer to a variety of economic, social or geographical attributes, we adopt the latter in our analysis. In our benchmark estimations we use the contiguity approach, whereby only adjacent countries affect each other. Results using the alternative metric inverse distance between countries in the sample are similar, and are available upon request.
Indicators of awareness.
We proxy awareness with exposure in the past to epidemic outbreaks, and to natural disasters. To identify the events we resort to the Emergency Events Database (https://www.emdat.be/), constructed by the Center for Research on the Epidemiology of Disasters. Events cover natural disasters (geophysical, meteorological, hydrological, climatological, biological – of which epidemics – and extra-terrestrial) and technological disasters. We combine information in EM-DAT with population statistics from the World Bank and construct the following indicators by country: (i) number of epidemic episodes affecting more than 100 people; (ii) within the previous measure, focus on outbreaks linked to respiratory diseases (such as MERS and SARS, among others), and, more specifically, on SARS-CoV-1; (iii) number of natural disasters affecting more than 0.1% of the country’s population. We focus on events that occurred in the period 2000–2019. The results are robust to the selection of alternative thresholds for the affected population.
Indicators of incidence of the pandemic.
For human incidence of COVID-19, we use data from the Johns Hopkins Coronavirus Resource Center (https://coronavirus.jhu.edu/) to compute the accumulated number of deaths at a given reference date in a given country as a fraction of the number of inhabitants, for three reference dates: 1 month after the pandemic outbreak (date at which the 10th death was reported), 3 months after, and the total as of 31 December 2020. Looking at different reference dates allows us to account for the fact that, as the pandemic developed worldwide, individuals took social distancing measures and actions.
Regarding economic incidence, we focus on economic losses in 2020. The use of higher frequency data (either monthly or quarterly) would have severely reduced our sample of countries to between 40 and 70, with a marked bias towards advanced economies. Resorting to annual data allows us to keep some 150 countries (see Table A.1). More specifically, we construct the following measures: (i) annual growth rate of GDP in 2020; (ii) revisions to 2020 GDP growth forecasts by the International Monetary Fund (IMF) with respect to the pre-pandemic outlook (forecasts published in November 2019). We take the projections from the World Economic Outlook — the IMF’s flagship publication-: the April 2020 vintage, that can be seen as an initial estimate of the incidence of the pandemic (“IMF first revision” henceforth), and the November 2020 one (“IMF revision 1-year” henceforth). In all cases we trim the upper and lower 5% of the distribution of country forecasts.
Table A.1.
Countries included in the analysis.
| ABW | Aruba | CHN | China | GMB | Gambia, The | LBR | Liberia | NZL | New Zealand | THA | Thailand |
| AFG | Afghanistan | CIV | Cote d’Ivoire | GNB | Guinea-Bissau | LCA | St. Lucia | OMN | Oman | TJK | Tajikistan |
| AGO | Angola | CMR | Cameroon | GNQ | Eq. Guinea | LKA | Sri Lanka | PAK | Pakistan | TLS | Timor-Leste |
| ALB | Albania | COD | Congo, Dem. Rep. | GRC | Greece | LSO | Lesotho | PAN | Panama | TTO | Trinidad and Tobago |
| ARG | Argentina | COG | Congo, Rep. | GRD | Grenada | LTU | Lithuania | PER | Peru | TUN | Tunisia |
| ARM | Armenia | COL | Colombia | GTM | Guatemala | LUX | Luxembourg | PHL | Philippines | TUR | Turkey |
| AUS | Australia | COM | Comoros | HKG | Hong Kong | LVA | Latvia | PNG | Papua New Guinea | TZA | Tanzania |
| AUT | Austria | CPV | Cabo Verde | HND | Honduras | MAR | Morocco | POL | Poland | UGA | Uganda |
| AZE | Azerbaijan | CRI | Costa Rica | HRV | Croatia | MDA | Moldova | PRI | Puerto Rico | UKR | Ukraine |
| BDI | Burundi | CYP | Cyprus | HTI | Haiti | MDG | Madagascar | PRT | Portugal | URY | Uruguay |
| BEL | Belgium | CZE | Czech Republic | HUN | Hungary | MDV | Maldives | PRY | Paraguay | USA | United States |
| BEN | Benin | DEU | Germany | IDN | Indonesia | MEX | Mexico | QAT | Qatar | UZB | Uzbekistan |
| BFA | Burkina Faso | DJI | Djibouti | IND | India | MKD | North Macedonia | ROU | Romania | VCT | St. Vincent & the Gr. |
| BGD | Bangladesh | DNK | Denmark | IRL | Ireland | MLI | Mali | RUS | Russian Federation | VEN | Venezuela, RB |
| BGR | Bulgaria | DOM | Dominican Rep. | IRN | Iran, Islamic Rep. | MLT | Malta | RWA | Rwanda | VNM | Vietnam |
| BHR | Bahrain | DZA | Algeria | IRQ | Iraq | MMR | Myanmar | SDN | Sudan | YEM | Yemen, Rep. |
| BHS | Bahamas, The | ECU | Ecuador | ISL | Iceland | MNE | Montenegro | SEN | Senegal | ZAF | South Africa |
| BIH | Bosnia & Herzegovina | EGY | Egypt, Arab Rep. | ISR | Israel | MNG | Mongolia | SGP | Singapore | ZMB | Zambia |
| BLR | Belarus | ERI | Eritrea | ITA | Italy | MOZ | Mozambique | SLE | Sierra Leone | ZWE | Zimbabwe |
| BLZ | Belize | ESP | Spain | JAM | Jamaica | MRT | Mauritania | SLV | El Salvador | ||
| BOL | Bolivia | EST | Estonia | JOR | Jordan | MUS | Mauritius | SOM | Somalia | ||
| BRA | Brazil | ETH | Ethiopia | JPN | Japan | MWI | Malawi | SRB | Serbia | ||
| BRB | Barbados | FIN | Finland | KAZ | Kazakhstan | MYS | Malaysia | STP | Sao Tome and Pr. | ||
| BRN | Brunei Darussalam | FJI | Fiji | KEN | Kenya | NAM | Namibia | SUR | Suriname | ||
| BTN | Bhutan | FRA | France | KGZ | Kyrgyz Republic | NER | Niger | SVK | Slovak Republic | ||
| BWA | Botswana | GAB | Gabon | KHM | Cambodia | NGA | Nigeria | SVN | Slovenia | ||
| CAF | Central African Rep. | GBR | United Kingdom | KOR | Korea, Rep. | NIC | Nicaragua | SWE | Sweden | ||
| CAN | Canada | GEO | Georgia | KWT | Kuwait | NLD | Netherlands | SWZ | Eswatini | ||
| CHE | Switzerland | GHA | Ghana | LAO | Lao PDR | NOR | Norway | TCD | Chad | ||
| CHL | Chile | GIN | Guinea | LBN | Lebanon | NPL | Nepal | TGO | Togo |
Notes: For countries in italics, either economic or human incidence data are unavailable.
Control variables.
We use the following variables: urban population as percent of total population in 2019; average temperature between 1991 and 2016; average household size in 2019; gross national income per capita (PPP); dummy variables to control for the geographical location of each country within a continental group (Africa, Oceania, North America, South-Central America, Asia, Europe); dummy for emerging market economies (“EME” henceforth); a dummy that takes value 1 if the population is above the median of all countries in the sample (“Large country”).
We control for the incidence of policy decisions using the Oxford COVID-19 Government Response Tracker of Hale et al. (2020) (“NPIs index”, Non Pharmaceutical Intervention indicator, henceforth). Ex ante, it is unclear whether more aware countries would be more prone to the implementation of policies in the spirit of those captured by the index, or they rather resorted to other alternatives — such as intensive testing and contact tracing. With the available data we cannot test either hypothesis. To account for potential endogeneity concerns with our empirical approach we explore the link between indicators of awareness and the stringency indicator in a very simple way by regressing one on the other. For that purpose, we calculate the average value of the stringency index one month and three months after the 10th death was notified in each country, as well as the average for the full year 2020. As shown in Table A.2 in the Appendix, the correlation between prior experience with epidemics (and other catastrophic events) and the stringency index is statistically not significantly different from zero in most cases. Anyhow, for the regression analysis, we extract the residuals of the previous regressions and include them as an additional control in the human incidence variables’ specifications.
Table A.2.
Non-Pharmaceutical interventions and indicators of awareness.
| Dependent variable: Non Pharmaceutical Intervention indicator COVID-19 Government Response Tracker | ||||||||
|---|---|---|---|---|---|---|---|---|
| 1 month | 3 months | 3 months | end-2020 | end-2020 | end-2020 | end-2020 | end-2020 | |
| [1] | [2] | [3] | [4] | [5] | [6] | [7] | [8] | |
| # epidemics | 0.0577 | 0.0308 | 0.0589 | −0.146 | −0.0313 | |||
| (0.611) | (0.775) | (0.459) | (0.156) | (0.688) | ||||
| # SARS-CoV-1 | 0.0757 | |||||||
| (0.535) | ||||||||
| # respiratory ep. | −0.0629 | |||||||
| (0.494) | ||||||||
| # disasters | −0.200** | |||||||
| (0.0470) | ||||||||
| Spatial lag | −0.0149 | 0.0205 | 0.244* | 0.0534 | 0.338** | 0.0609 | 0.0597 | 0.0648 |
| (0.923) | (0.890) | (0.0901) | (0.709) | (0.0129) | (0.676) | (0.676) | (0.645) | |
| Additional controls | Yes | Yes | No | Yes | No | Yes | Yes | Yes |
| Observations | 143 | 143 | 143 | 143 | 143 | 143 | 143 | 143 |
| R-squared | 0.0607 | 0.154 | 0.00108 | 0.231 | 0.00324 | 0.222 | 0.222 | 0.240 |
Notes: () [] denotes statistical significance at 10% (5%) [1%]. Robust p-values in parentheses. Spatial regressions based on contiguity, assuming that adjacent counties affect each other. All non-dummy variables are in logs and standardized. Additional control variables included in all the regressions are: Continent; EME; “Large country”.
In addition, to further control for policy endogeneity we also used the Global Health Security Index (see https://www.ghsindex.org/about/), a quantitative indicator of health security and related capabilities. It contains several subindices, some of which might be more relevant for the issue at hand, in particular the “Early Detection and Reporting” and the “Rapid Response and Mitigation” components. The results (available upon request) indicate that there is no robust link between the GHS indices and pandemic incidence.
3. Results and policy implications
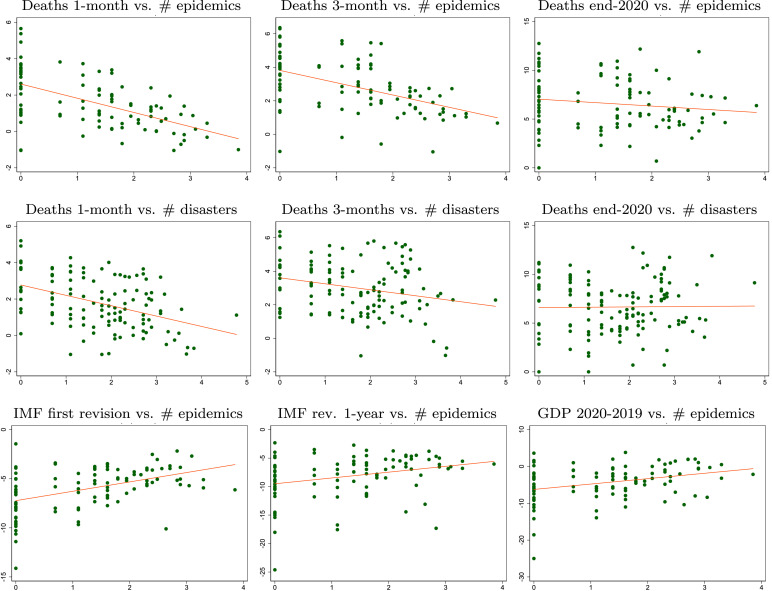
In Fig. 2, we display scatter plots relating our indicators of COVID-19 human and economic incidence against some measures of awareness. The simple (unconditional) correlations show the expected signs: First, more exposure in the past to epidemics/disasters is negatively related to human losses, i.e. countries more exposed in the past to such events tend to show a lower death toll from the current pandemic. Second, the revision to macroeconomic projections (IMF indicators) and the output loss are less pronounced for countries that experienced more epidemics/disasters in the past. In the scatters we do not control for potential confounding factors. We show our regression results in Table 1, Table 2 for social-human incidence, and in Table 3 as regards economic incidence. The columns in these Tables show estimated versions of model (1) for different sets of indicators of awareness, incidence, and control variables.
Fig. 2.
COVID-19 incidence (Y-axis) and awareness (X-axis). Notes: Human incidence indicators in logs. See main text of the paper for the definition of the variables.
Table 1.
Social-human incidence of COVID-19 and number of epidemics in the past.
| Dependent variable: COVID-19 deaths per million, period after death 10 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 month | 1 month | 1 month | 3 month | 3 month | 3 month | end-2020 | end-2020 | end-2020 | |
| [1] | [2] | [3] | [4] | [5] | [6] | [7] | [8] | [9] | |
| # epidemics | −0.305*** | −0.285*** | −0.249*** | −0.235*** | −0.167* | −0.169* | −0.257*** | −0.195** | −0.180*** |
| (0.000) | (0.000) | (0.008) | (0.004) | (0.097) | (0.081) | (0.000) | (0.014) | (0.008) | |
| Spatial lag | 0.195* | 0.199* | 0.173 | 0.265** | 0.356*** | 0.306*** | 0.306*** | 0.372*** | 0.312*** |
| (0.083) | (0.067) | (0.134) | (0.019) | (0.002) | (0.007) | (0.000) | (0.000) | (0.000) | |
| NPIs index | −0.024 | 0.189*** | 0.177*** | 0.283*** | 0.311*** | ||||
| (0.661) | (0.002) | (0.006) | (0.000) | (0.000) | |||||
| Urban | −0.020 | 0.033 | 0.067 | 0.082 | 0.135* | ||||
| (0.835) | (0.748) | (0.518) | (0.282) | (0.061) | |||||
| Temperature | 0.098 | −0.063 | −0.112 | 0.103 | −0.092 | ||||
| (0.298) | (0.535) | (0.252) | (0.129) | (0.183) | |||||
| Household size | 0.129 | 0.213* | 0.163 | 0.119 | 0.133* | ||||
| (0.227) | (0.062) | (0.148) | (0.184) | (0.086) | |||||
| GNI per capita | 0.252* | 0.209 | 0.135 | 0.129 | 0.013 | ||||
| (0.074) | (0.166) | (0.373) | (0.278) | (0.905) | |||||
| Africa | 0.704*** | 0.676*** | 0.476* | 0.096 | −0.112 | 0.001 | −0.125 | −0.325 | −0.099 |
| (0.003) | (0.007) | (0.072) | (0.725) | (0.695) | (0.996) | (0.526) | (0.140) | (0.628) | |
| Oceania | −0.616 | −0.637 | −0.762 | −1.076** | −1.338*** | −1.202** | −0.831** | −1.422*** | −0.811** |
| (0.183) | (0.164) | (0.102) | (0.031) | (0.007) | (0.012) | (0.017) | (0.000) | (0.016) | |
| North America | 1.096*** | 1.035*** | 0.700 | 1.389*** | 1.139** | 1.177** | 0.845*** | 0.909** | 0.923** |
| (0.006) | (0.009) | (0.164) | (0.001) | (0.035) | (0.023) | (0.005) | (0.036) | (0.011) | |
| Central-South | 0.851*** | 0.897*** | 0.643** | 0.655** | 0.532* | 0.575* | 0.456** | 0.501** | 0.557** |
| America | (0.001) | (0.001) | (0.031) | (0.020) | (0.097) | (0.066) | (0.021) | (0.046) | (0.011) |
| Asia | 0.254 | 0.236 | −0.063 | −0.121 | −0.413 | −0.379 | −0.066 | −0.146 | −0.058 |
| (0.293) | (0.341) | (0.823) | (0.652) | (0.170) | (0.201) | (0.727) | (0.535) | (0.781) | |
| Europe | 0.979*** | 0.945*** | 0.952*** | 0.582*** | 0.460* | 0.424* | 0.688*** | 0.649*** | 0.751*** |
| (0.000) | (0.000) | (0.000) | (0.001) | (0.052) | (0.061) | (0.000) | (0.001) | (0.000) | |
| EME | −0.618*** | −0.690*** | −0.506** | −0.342 | −0.191 | −0.323 | −0.135 | −0.191 | −0.263 |
| (0.002) | (0.001) | (0.037) | (0.137) | (0.463) | (0.213) | (0.403) | (0.343) | (0.149) | |
| Large country | −0.322*** | −0.254** | −0.178 | −0.052 | 0.090 | 0.114 | −0.013 | 0.168 | 0.029 |
| (0.008) | (0.041) | (0.175) | (0.697) | (0.524) | (0.409) | (0.893) | (0.131) | (0.765) | |
| Observations | 150 | 143 | 126 | 143 | 126 | 123 | 143 | 132 | 123 |
| R-squared | 0.573 | 0.584 | 0.607 | 0.509 | 0.506 | 0.558 | 0.723 | 0.700 | 0.773 |
Notes: () [] denotes statistical significance at 10% (5%) [1%]. Robust p-values in parentheses. Spatial regressions based on contiguity. All non-dummy variables are in logs and standardized. See main text of the paper for the definition of the variables.
Table 2.
Social-human incidence of COVID-19: other indicators of awareness.
| Dependent variable: COVID-19 deaths per million, period after death 10 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 month | 1 month | 1 month | 1 month | 3 months | end-2020 | end-2020 | end-2020 | end-2020 | |
| [1] | [2] | [3] | [4] | [5] | [6] | [7] | [8] | [9] | |
| # epidemics | −0.252*** | −0.158* | −0.179** | ||||||
| (0.003) | (0.087) | (0.016) | |||||||
| # SARS-COV-1 | 0.081 | 0.013 | −0.065 | −0.194*** | −0.245*** | ||||
| (0.362) | (0.887) | (0.507) | (0.002) | (0.000) | |||||
| # respiratory ep. | −0.016 | −0.121** | |||||||
| (0.812) | (0.021) | ||||||||
| # disasters | −0.139* | −0.226*** | −0.192** | −0.020 | −0.088 | ||||
| (0.085) | (0.003) | (0.031) | (0.784) | (0.140) | |||||
| Spatial lag | 0.170 | 0.274** | 0.277** | 0.242** | 0.303*** | 0.374*** | 0.379*** | 0.371*** | 0.370*** |
| (0.137) | (0.012) | (0.011) | (0.027) | (0.010) | (0.000) | (0.000) | (0.000) | (0.000) | |
| NPIs index | −0.037 | −0.037 | −0.041 | 0.311*** | 0.296*** | 0.288*** | |||
| (0.514) | (0.515) | (0.457) | (0.000) | (0.000) | (0.000) | ||||
| Additional controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 150 | 143 | 143 | 143 | 150 | 160 | 143 | 143 | 143 |
| R-squared | 0.586 | 0.535 | 0.534 | 0.564 | 0.477 | 0.631 | 0.713 | 0.692 | 0.686 |
Notes: () [] denotes statistical significance at 10% (5%) [1%]. Robust p-values in parentheses. Spatial regressions based on contiguity. All non-dummy variables are in logs and standardized. “# SARS-CoV-1” number of people affected by the disease in each country; “# respiratory ep.” number of respiratory epidemic episodes suffered by a country between 2000 and 2019; “# disasters” number of biological and other natural disasters suffered by a country between 2000 and 2019 that affected more that 0.1% of its population. Additional control variables: Continent; EME; “Large country”.
Table 3.
Economic incidence of COVID-19 and number of epidemics in the past.
| IMF first revision |
IMF first revision |
IMF first revision |
IMF 1-year revision |
IMF 1-year revision |
IMF 1-year revision |
GDP 2020 vs. 2019 |
GDP 2020 vs. 2019 |
GDP 2020 vs. 2019 |
|
|---|---|---|---|---|---|---|---|---|---|
| [1] | [2] | [3] | [4] | [5] | [6] | [7] | [8] | [9] | |
| # epidemics | 0.173** | 0.159** | 0.007 | 0.113 | 0.096 | −0.057 | 0.174** | 0.130* | −0.020 |
| (0.019) | (0.028) | (0.945) | (0.171) | (0.245) | (0.575) | (0.015) | (0.058) | (0.813) | |
| Spatial lag | 0.060 | 0.002 | −0.062 | 0.058 | 0.059 | −0.099 | 0.060 | 0.106 | −0.012 |
| (0.666) | (0.986) | (0.666) | (0.700) | (0.683) | (0.533) | (0.683) | (0.453) | (0.937) | |
| NPIs index | −0.100* | −0.112* | −0.257*** | −0.259*** | −0.179*** | −0.186*** | |||
| (0.084) | (0.080) | (0.000) | (0.000) | (0.001) | (0.001) | ||||
| Urban | −0.078 | −0.119 | −0.054 | ||||||
| (0.457) | (0.266) | (0.557) | |||||||
| Temperature | 0.039 | −0.067 | −0.056 | ||||||
| (0.688) | (0.514) | (0.550) | |||||||
| Household size | 0.026 | −0.215* | 0.060 | ||||||
| (0.808) | (0.066) | (0.546) | |||||||
| GNI per capita | −0.151 | −0.241 | −0.211 | ||||||
| (0.312) | (0.127) | (0.111) | |||||||
| Tourism share | −0.159** | −0.275*** | −0.231*** | ||||||
| (0.031) | (0.000) | (0.000) | |||||||
| Additional controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 161 | 138 | 118 | 162 | 140 | 119 | 161 | 137 | 117 |
| R-squared | 0.432 | 0.502 | 0.550 | 0.183 | 0.235 | 0.359 | 0.293 | 0.307 | 0.425 |
Notes: () [] denotes statistical significance at 10% (5%) [1%]. Robust p-values in parentheses. Spatial regressions based on contiguity. Regressands standardized; regressors in logs and standardized. Additional control variables: Continent; EME; “Large country”. For details on controls and other variables see footnote to Table 1.
Turning to Table 1, some results are worth highlighting. First and foremost, we find a strong and robust negative association between the number of past epidemics and human incidence. The result holds for all the empirical specifications shown, and is robust to the inclusion of a number of control variables. In particular, to the introduction of the stringency index, NPI. Second, the statistical significance of the spatial lag indicates that proximity to countries affected by the pandemic has some bearing on cases, as expected. Third, countries more affected by COVID-19 put in place more stringent containment measures, as of the 3rd month after the 10th case, and overall when looking at the whole 2020 period. The results in Table 2 show that the key findings are robust to the use of alternative measures of awareness.
In Table 3 we provide results on economic incidence. This is a more demanding exercise, as several confounding factors may be at work, most notably economic and containment policies adopted since the outburst of the pandemic, and the heterogeneous economic structure of countries. We try to proxy some of these factors with a number of control variables. Results in the most basic regressions for the initial impact and the overall output loss in 2020 display a positive and statistically significant coefficient, that is, robust to the inclusion of the NPI stringency index. Nevertheless, the inclusion of additional, plausible, control variables dissipates this finding, which is evidence of lack of robustness. In addition, when looking at alternative awareness indicators (see Table A.3 in the Appendix) we do not find significant correlations.
Table A.3.
Economic incidence of COVID-19: other indicators of awareness.
| IMF first revision |
IMF 1-year revision |
GDP 2020 vs. 2019 |
IMF first revision |
IMF 1-year revision |
GDP 2020 vs. 2019 |
IMF first revision |
IMF 1-year revision |
GDP 2020 vs. 2019 |
|
|---|---|---|---|---|---|---|---|---|---|
| [1] | [2] | [3] | [4] | [5] | [6] | [7] | [8] | [9] | |
| # SARS-CoV-1 | 0.104 | −0.067 | −0.075 | ||||||
| (0.217) | (0.488) | (0.355) | |||||||
| # respiratory ep. | 0.023 | −0.008 | 0.012 | ||||||
| (0.718) | (0.915) | (0.849) | |||||||
| # disasters | 0.054 | −0.048 | −0.045 | ||||||
| (0.456) | (0.568) | (0.529) | |||||||
| Spatial lag | 0.085 | 0.090 | 0.151 | 0.069 | 0.092 | 0.156 | 0.051 | 0.092 | 0.159 |
| (0.501) | (0.527) | (0.278) | (0.590) | (0.517) | (0.263) | (0.692) | (0.520) | (0.253) | |
| NPIs index | −0.115** | −0.263*** | −0.188*** | −0.109* | −0.264*** | −0.189*** | −0.103* | −0.268*** | −0.194*** |
| (0.048) | (0.000) | (0.001) | (0.060) | (0.000) | (0.001) | (0.079) | (0.000) | (0.001) | |
| Additional controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 138 | 140 | 138 | 138 | 140 | 138 | 138 | 140 | 138 |
| R-squared | 0.498 | 0.233 | 0.307 | 0.493 | 0.233 | 0.307 | 0.495 | 0.233 | 0.308 |
Notes: () [] denotes statistical significance at 10% (5%) [1%]. Robust p-values in parentheses. Spatial regressions based on contiguity, assuming that adjacent counties affect each other. Regressands standardized; regressors in logs and standardized. Additional control variables included in all the regressions are: Continent; EME; “Large country”.
Turning to policy implications, the evidence on a less intense human impact of the COVID-19 disease spread (and less so economic impact) in more aware societies may provide lessons for policy-makers beyond the current pandemic. If past experience is of value, the current pandemic should make societies more resilient against upcoming viral shocks in the future, calling for greater preparedness of health systems. In addition, with extensive international travel and trade, prevention exceeds the national frontiers, thus highlighting the key role of multilateral coordination on disease prevention, including through international bodies such as the WHO.
Footnotes
This research did not receive any specific grant from the public, commercial, or non-profit sectors.
On related grounds, Lin and Meissner (2020), when studying the link between public health performance in the early days of the COVID-19 pandemic and those during the Spanish Influenza pandemic of 1918–20, find that experience with SARS is associated with lower mortality today, in a sample of 33 countries worldwide.
Appendix. Additional tables
References
- de Bolle M. RealTime Economic Issues Watch. Peterson Institute for International Economics; 2021. Novel viral variants: Why the world should prepare for chronic pandemics. [Google Scholar]
- Daszah P. We knew disease X was coming. It’s here now. N.Y. Times. 2020 [Google Scholar]
- Ferraresi M., Kotsogiannis C., Rizzo L., Secomandi R. The Great Lockdown and its determinants. Econom. Lett. 2020;197 doi: 10.1016/j.econlet.2020.109628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliano P., Spilimbergo A. Growing up in a recession. Rev. Econom. Stud. 2014;81:787–817. [Google Scholar]
- Granell C., Gómez S., Arenas A. Dynamical interplay between awareness and epidemic spreading in multiplex networks. Phys. Rev. Lett. 2013;111 doi: 10.1103/PhysRevLett.111.128701. [DOI] [PubMed] [Google Scholar]
- Hale, T., Angrist, N., Cameron-Blake, E., Hallas, L., Kira, B., Majumdar, S., Petherick, A., Phillips, T., Tatlow, H., Webster, S., (2020). Oxford COVID-19 Government Response Tracker. Blavatnik School of Government, University of Oxford. [DOI] [PubMed]
- Jordà, O., Singh, S.R., Taylor, A.M., 2020. Longer-Run Economic Consequences of Pandemics. Federal Reserve Bank of San Francisco Working Paper Series, 2020, 2020-09.
- Kozlowski Julian, Veldkamp Laura, Venkateswaran Venky. National Bureau of Economic Research, Inc; 2020. Scarring body and mind: The long-term belief-scarring effects of COVID-19, NBER Working Papers 27439. [Google Scholar]
- Lin Peter Z., Meissner C.M. 2020. A note on long-run persistence of public health outcomes in pandemics, NBER Working Paper 27119. [Google Scholar]
- Malmendier U., Nagel S. Depression babies: Do macroeconomic experiences affect risk taking? Q. J. Econ. 2011;126:373–416. [Google Scholar]
- Samanta S., Chattopadhyay J. Effect of awareness program in disease outbreak – a slow–fast dynamics. Appl. Math. Comput. 2014;237:98–109. [Google Scholar]
- Wang R., Chen X., Qing L., Wang W., Liu Q. Self-awareness-based resource allocation strategy for containment of epidemic spreading. Complexity. 2020 [Google Scholar]
- WHO . World Health Organization; 2017. Creating a Global Strategy for an R and D Blueprint for Action To Prevent Epidemics. Update 2017. [Google Scholar]
- Wu Q., Fu X., Small M., Xu X.-J. The impact of awareness on epidemic spreading in networks. Chaos. 2012;22 doi: 10.1063/1.3673573. [DOI] [PMC free article] [PubMed] [Google Scholar]