Abstract
Objectives:
We examined state variations in assisted living (AL) regulatory policies for admission/retention, staffing/training, medication management, and dementia care. Factors associated with domain-specific and overall regulatory stringency were identified.
Design:
This observational study employed the following data sources: 2019 review of state AL regulations; 2019 national inventory of AL communities; 2014 Government Accountability Office survey of Medicaid agencies; 2016 Genworth Cost of Care Survey; and the 2018 Nursing Home Compare.
Setting and Participants:
Final analyses included 46 states (excluding Alaska, Kentucky, Louisiana and West Virginia) and the District of Columbia.
Methods:
For each regulatory domain of interest (dependent variables) we generated policy scores by conducting content analysis of state regulatory databases. States were assigned points for presence of each policy (e.g. staff training). The number of points assigned to each policy was divided by the total possible number of policy-related points, producing state stringency scores (between 0% and 100%) for each policy domain. Independent variables included market-level characteristics (e.g. AL monthly cost), state generosity (e.g. proportion of Medicaid aged using AL services), quality of care (e.g. percent of nursing homes with few deficiencies), and others. Descriptive analyses and multivariable logistic regression models with stepwise selection were employed.
Results:
We found significant variations in all policy domains across states. No single policy appeared to clearly dominate a state’s rank. AL bed supply, monthly AL cost, proportion of Medicaid beneficiaries receiving AL services, and other variables were significantly associated with regulatory stringency of the domains examined.
Conclusions and Implications:
There were substantial variations in regulatory stringency across states. Several market and state generosity measures were identified as potential determinant of stringency, but the direction of these associations appeared to depend on what was being regulated. Future studies should examine how regulatory stringency affects access to and care quality in ALs.
Keywords: assisted living, regulation, stringency
Brief summary:
States vary significantly both with regard to assisted living policies that they regulate and with the stringency of these regulations. Several potential determinants of state regulatory stringency were identified.
INTRODUCTION
Over the past two decades, assisted living (AL) communities have become an important component of the US residential long-term care system. Today, there are about 29,000 AL communities with close to 1,000,000 beds/units,1 and this sector is expected to grow as the baby boomers age. There is, however, a great deal of variability across AL communities in size, services, population served, and cost.2–5 Because ALs are state (not federally) regulated, their oversight, and often the names used to describe them (e.g. residential care, adult care homes, personal care homes), vary widely. Historically, federal involvement in AL oversight has remained largely absent even as the number of residents has grown rapidly, and as state Medicaid programs began to reimburse AL for certain services provided to Medicaid enrolled residents.6,7
State AL regulations have both increased and become more variable over time. While 20 years ago only 28 states had any regulatory requirements for providing care to AL residents with Alzheimer’s disease and or related dementias (ADRD),8 by 2019 all except one had some dementia-specific regulations. In 2014, 19 states specified staffing requirements for ALs, with about 5 stipulating specific staff-to-resident ratios.9 By 2019, 39 states required staffing ratios, with 14 identifying specific staff-to-resident ratios. Such increases in regulatory stringency may have been motivated by greater acuity among AL residents. Today, more than 50% of residents require supportive care such as help with medications and assistance with activities of daily living,2 40% have moderate to severe dementia, and 90% have some degree of cognitive impairment.10–12 Nevertheless, substantial variations in AL regulations remain across states, and little is known about why states vary in extending these protections and the implications of such variations. A recent report by the Government Accountability Office (GAO) found that while most state Medicaid agencies cover AL services, they vary extensively in offering guidance and tracking deficiencies that impact beneficiary health and welfare, and in making such information publicly available.13 Another recent study compared AL staffing, training, inspection, and enforcement regulations to those required of nursing homes, and found the former to be highly variable and substantially less stringent than the latter, despite the increasing acuity levels among AL residents.14
Several studies have focused exclusively on dementia care regulations and examined state variation in the overall number of requirements, as well as in specific regulations pertaining to staffing, clinical care, and environmental safety.6,15 While prior research has been largely descriptive, a recent study examined the associations between several political, institutional and contextual factors and AL state dementia regulations, based on 2013 data.16 This study showed that after adopting AL regulations most states do not amend them. It also found that dementia policies were more stringent in states with a higher proportion of democratic legislators and where the long-term care ombudsman programs were more active. However, no study to date has examined the association of state AL regulations and contextual factors that may shape policy making for domains other than dementia.
Motivated by this gap in knowledge, we focused on several AL regulatory domains in addition to dementia care. Our objectives were to: 1) examine variations in regulatory stringency across states in relation to admission and retention criteria, staffing and training, medication management, and dementia care; and 2) identify factors that may be associated with the stringency of each domain as well as the overall state stringency.
CONCEPTUAL MODEL
We focused on these four areas of regulations because based on current literature they are likely to influence AL quality of care. 1) Admission and retention. Residents entering AL expect to age in place even as they develop conditions that would otherwise preclude AL entry in the first place (e.g. pressure ulcers).17 While states typically prohibit admission/retention when residents require “indefinite” or “ongoing” access to 24-hour nursing care, these criteria are not always well defined, have many exceptions, and vary across states.18,19 2) Staffing and training. A few nursing home studies have shown a positive effect of stricter state minimum staffing requirements on residents’ care and outcomes.20,21 In ALs, hospitalization rates were found to be lower in ALs with higher proportion of skilled staff hours.22 3) Medication management. ALs often need to provide health-related assistance, mainly support with taking of medications.23,24 More than 75% of the residents, including those with dementia, require such assistance.25 Medication administration error rates in AL have been reported to exceed 40%, with 7% of errors having a moderate-to-high potential for harm.26 The odds of such errors have been shown to be twofold when medication management is done by staff with training lower than that of a licensed practical nurse. State regulation of this domain may have further implications downstream on resident outcomes such as emergency room visits, hospital readmissions or fall-related injuries.27 4) Dementia care. Because of the high estimated proportion of ADRD among AL residents, many communities offer special care units and dementia-related services.28 Studies of dementia care in ALs show substantial variation in dementia-relevant regulations across states.
Following prior research examining both AL and nursing home state regulations, we focused on three categories of potential regulatory stringency predictors.16,29,30
Competition and Market.
While states do not regulate the supply of AL beds, it is possible that where AL is a more common long-term care alternative, state regulators are more inclined to implement more stringent regulations on some aspects of AL service delivery. Alternatively, where AL bed supply is low and less competition is occurring between these residential settings, states may be more concerned about quality and choose to issue more stringent regulations.31 In regard to market variables, AL costs are most frequently paid out-of-pocket and are not state regulated. However, in states with greater regulatory stringency, residents with higher acuity (e.g. requiring skilled care, being bed bound) may no longer be permitted to stay in AL, thus lowering the monthly cost. Furthermore, there is a substantial variation across states in AL community bed/unit size. In some states, small ALs with 25 or fewer beds are predominant, while in others, larger facilities are more common. Smaller settings have historically served more minority residents and those with more modest resources,32 and it is possible that in states in which small ALs predominate regulations are more lenient.14
State Generosity.
States vary widely in term of total Medicaid spending on AL services, as well as in the proportion of their Medicaid-eligible aged population receiving AL services.13 More generous states may be more likely to institute higher regulatory stringency.
Nursing Home Care Quality.
Most states paying for AL services for Medicaid beneficiaries provide some type of oversight, but these approaches are highly variable, have not been validated, and there has been no systematic data collection or research.13 Unlike AL, nursing homes are highly regulated. In states with stronger regulatory enforcement nursing homes have been shown to have fewer deficiencies.29 Such states may be more likely to extend their regulatory stringency to other residential care settings, including AL.
Other factors, which we evaluated but did not include in the final models were political party affiliation of state governors and control by legislature, state local tax revenues attributed to ALs, number of ALs in each state, and the state-level Centers for Medicare & Medicaid 5 star rating for nursing homes on staffing and overall quality.
METHODS
Data Sources
The data for this study were collected from five sources: 2019 review of state AL regulations; 33 2019 national inventory of AL communities; 2014 GAO survey of state Medicaid agencies;13 2016 Genworth Cost of Care Survey;34 and the 2018 Nursing Home Compare database. Below, we provide greater detail on these sources and their use in operationalizing the dependent and independent variables.
Dependent Variables
We employed the CY2019 regulatory review conducted by the National Center for Assisted Living (NCAL) as the primary data source for categorizing state regulatory rigor.33 For each regulatory item of interest – admission and retention, medication management, dementia care, and staffing and training – we started with a set of policies based on prior research.6,15 During the coding process new codes were inductively developed.35 Each domain was coded by two experienced researchers and coding disagreements were reviewed and discussed, reaching consensus; if consensus could not be reached, the principal investigator made the final decision. When the NCAL information was unavailable or ambiguous, we used LexisNexis’ and Westlaw’s legal research databases.
Similar to prior work by Nettinger and Kaskie,16 each policy domain was assigned a numeric code depending on the number of policies evaluated and their stringency (see Appendix Table A). For example, for the domain of staffing and training, we coded for 4 policies with a maximum number of points being 16. New York scored 6 on the 4 policies and was assigned a stringency score of 0.375 (6/16; with higher score=greater stringency). We also created an overall stringency score for each state as an average of the four policy domains.
Independent Variables
Competition and Market.
Using the 2019 data obtained from individual states’ licensing agencies, we created an inventory of AL communities in each state. Most state directories listed the number of beds/units available in each AL. When such data were not available, we followed up with each state licensing agency and also searched the web. Using bed capacity of each AL and the US Census’ annual population estimates, we calculated AL bed supply per 1000 population age 75+ in each state. For each state we also calculated the proportion of small (≤25 beds) ALs.
Average state monthly AL costs were obtained from the annual Genworth Cost of Care Survey; we used the 2016 data to allow for time it may take the state to promulgate regulation in response to such contextual factors. Cost data were not adjusted for cost of living in the state or differences in per capital income.
State Generosity.
We employed two variables of state interest/generosity with regard to AL communities, measuring the percent of Medicaid aged and disabled beneficiaries who received AL services, and total state Medicaid spending on AL services, using the most current GAO survey data.13
Nursing Home Care Quality.
The proportion of each state’s nursing homes rating 4–5 stars36,37 on deficiency citations was obtained from the Nursing Home compare website.
Analysis
Descriptive analyses were performed to examine the overall regulatory score for each state and to explore the distribution of state stringency vis-à-vis each policy domain of interest. Pearson correlation coefficients among policy domain scores were not highly correlated suggesting that these measures are independent of each other. However, each of the four policy domains was highly correlated with the overall stringency metric (see Appendix Figure A).
Multivariable logistic regression models were constructed to estimate the association between state-level factors and each stringency domain, and with the overall score. Given the small number of observations, we employed a stepwise selection and retained only significant (p<0.2) variables in the final models. All statistical analyses were performed in SAS (Version 9.4; SAS Institute Inc., Cary, NC).
This study was reviewed and approved by the University of Rochester institutional review board.
RESULTS
By 2019, all states had promulgated some regulations for AL admission/retention, staffing/training, medication management, and dementia care (except Hawaii with regard to the latter). Although we assessed the regulatory rigor for all 50 states and the District of Columbia (DC), some key covariates were not available for all states and our final analyses included 46 states (excluding Alaska, Kentucky, Louisiana and West Virginia) and DC.
There were substantial variations in the number of policies promulgated across different regulatory domains (Table 1). For example, on average 45.7% of the 7 dementia care policies examined were included in the regulations across states, ranging from 0% in Hawaii to 90% in Arkansas and Illinois. Of the four staffing/training policies we identified, 60.8% on average were promulgated, ranging from 32% in New Hampshire to 87% in Pennsylvania and Virginia. With regard to admission/retention policies, state regulatory stringency ranged from 11% in Connecticut, Hawaii and North Dakota, to 77% in Montana, with an overall mean of 49.2%. Medication management appeared least stringent in 12 states and most stringent in 17, with an average stringency score of 52.1%.
Table 1:
Descriptive Statistics for State Assisted Living Regulatory Stringency
| Variables | Mean | Std. Dev. | Minimum | Maximum | Median |
|---|---|---|---|---|---|
| Dependent | |||||
| Admission & retention policy score | 49.17 | 16.18 | 11.11 | 77.78 | 55.56 |
| Medication management policy score | 52.13 | 19.39 | 25.00 | 75.00 | 50.00 |
| Dementia care policy score | 45.74 | 22.34 | 0.00 | 90.00 | 40.00 |
| Staffing & training policy score | 60.77 | 13.08 | 31.25 | 87.50 | 62.50 |
| Summary policy score | 53.36 | 10.40 | 23.08 | 71.79 | 53.85 |
| Independent | |||||
| Average monthly AL cost (divided by 500)1 | 7.66 | 1.67 | 5.07 | 13.40 | 7.20 |
| AL beds per 1000 population age >75 | 70.72 | 31.63 | 11.00 | 174.00 | 71.00 |
| Pct. aged/disabled Medicaid AL users (divided by 5)1 | 0.73 | 1.26 | 0.00 | 8.18 | 0.35 |
| Pct. of NHs with 4–5 star deficiencies | 34.55 | 2.02 | 30.50 | 40.18 | 34.51 |
| Total Medicaid spending on AL (divided by 100M)1 | 2.10 | 2.96 | 0.01 | 12.92 | 0.57 |
| Pct. of ALs with =<25 beds | 42.28 | 27.34 | 2.07 | 94.47 | 40.44 |
Note:
These variables were standardized to make interpretation of the estimates easier
In Figure 1 we ranked each state by its overall regulatory stringency, ordered from most to least stringent, and depicted the scores for each regulatory domain in that state. Among the most stringent states were Arkansas, Virginia, Pennsylvania, North Carolina and Rhode Island (the latter being on par with New Mexico and Alabama), but they differed in terms of which regulatory domain most contributed to that stringency. For example, in Arkansas and North Carolina, dementia care was the key contributor, while in Virginia and Pennsylvania staffing/training was predominant. Among the least regulated states were Hawaii and New Hampshire. While in Hawaii staffing/training appeared to have been the principal stringency contributor, in New Hampshire both staffing/training and admission/retention drove the stringency score.
Figure 1:
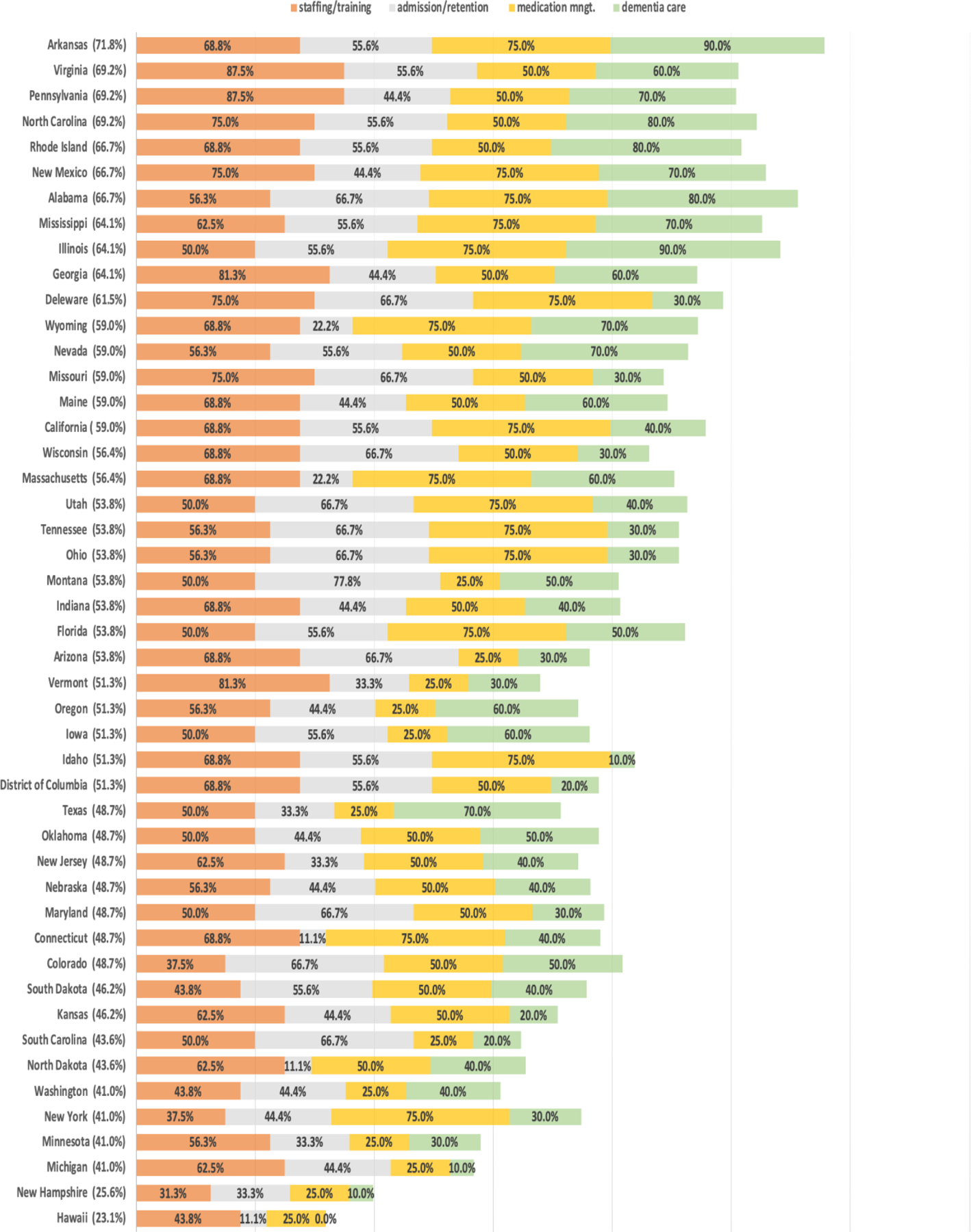
Assisted Living State Regulatory Stringency: By State (Overall Stringency Score) & Domain-Specific Stringency Scores
Note: Higher score denotes greater regulatory stringency
Factors associated with the regulatory rigor of each policy domain, and with the overall state score, are presented in Table 2. Admission/retention stringency was lower (OR=0.92; p<0.10) in states with higher AL costs and a greater proportion of Medicaid beneficiaries receiving AL services (OR=0.69; p<0.01), but higher where AL bed supply was greater (OR=1.01; p<0.10). State stringency of medication management was negatively associated with AL bed supply (OR=0.99; p<0.05), as was dementia care stringency (OR=0.99; p<0.01). Three other variables were significantly associated with dementia care stringency; greater regulatory rigor in this domain was associated with lower monthly AL costs (OR=0.83; p<0.05) and lower preponderance of small (≤25 beds) ALs in the state (OR=0.99; p<0.10), but with higher total Medicaid spending on AL services (OR=1.05; p<0.10). Higher Medicaid spending was also predictive of greater stringency in staffing and training (OR=1.05; p<0.10), as was greater proportion of nursing homes with fewer deficiency citations (OR=1.09; p<0.05).
Table 2:
Assisted Living Regulatory Stringency By Policy Domain: Multivariable Logistic Regression Odds Rations (95% CIs)
| Admission & Retention | Medication Management | Dementia Care | Staffing & Training | Overall Summary | |
|---|---|---|---|---|---|
| Average monthly AL cost | 0.92* (0.81–1.04) |
0.83** (0.73–0.94) |
0.92*** (0.86–0.97) |
||
| AL beds per 1000 population age >75 | 1.01* (0.99–1.01) |
0.99 ** (0.98–0.99) |
0.99*** (0.98–0.99) |
0.99** (0.99–1.00) |
|
| Pct. aged/disabled Medicaid AL users | 0.69 *** (0.54–0.91) |
0.94* (0.86–1.10) |
|||
| Pct. of NHs with 4–5 star deficiencies | 1.09** (1.01–1.17) |
1.06*** (1.03–1.12) |
|||
| Total Medicaid spending on AL | 1.05* (0.98–1.12) |
1.05* (0.99–1.11) |
1.04** (1.00–1.07) |
||
| Pct. of ALs with =<25 beds | 0.99* (0.99–1.00) |
0.99* (0.99–1.00) |
Note: 95% Wald Confidence Limits in parentheses
significant at 0.1 level
significant at 0.05 level
significant at <=0.01 level
While all independent variables had some association with overall stringency, their effect differed in size and direction. In states with higher monthly AL costs and a greater proportion of Medicaid beneficiaries using AL, overall stringency was 8% (OR=0.92; p<0.01) and 6% (OR=0.94; p<0.10) lower, respectively. Higher overall stringency was also negatively associated with higher AL supply (OR=0.99; p<0.05) and the proportion of small ALs (OR=0.99; p<0.10). However, in states with more high quality nursing homes (i.e. fewer deficiencies) and higher Medicaid spending on AL services, the odds of overall stringency were higher (OR=1.06; p<0.01 and OR=1.04; p<0.05), respectively.
DISCUSSION
This study is the first to examine variations in multiple domains of state AL regulatory policies and to identify factors associated with their stringency. Several prior studies focusing on state policies regulating AL dementia care,6,15 and staffing14 have shown substantial state-to-state variations. Our findings support and extend these studies, demonstrating variations in other policy domains such as admission/retention and medication management. Combining these policy domains in a single score, we were also able to categorize states by regulatory stringency and identify which policies dominate state ranking. No single policy appeared to clearly dominate a state’s rank. For example, while Georgia ranked within top 10 most overall stringent states, its admission and retention as well as medication management scores were below the US average. On the other hand, Michigan, which ranked low on the overall stringency, had staffing and training score on par with the US median.
Some have suggested that state AL regulatory policy, in absence of a clearly defined constituency, may be shaped by advocacy from entities with financial or other interest in providing AL services.15 Our findings may provide some support for this supposition. For example, in states with lower monthly AL costs, overall regulatory stringency as well as the admission/retention and dementia care scores were higher. While our findings cannot determine the direction of this association (or causality), it is possible that in states that more stringently regulate resident case-mix AL providers may be able to offer lower base monthly costs. Similarly, AL bed supply was significantly associated with admission and retention, medication management, and dementia care stringency. But the direction of this association was not consistent across these domains, suggesting that the relationship between regulatory stringency and market-level variables may depend on what is being regulated. For example, in markets with more AL beds states, may be more inclined (or pressured) to less stringently regulate services most needed by residents (i.e. assistance with medications and dementia care). Higher regulation in these domains may require AL providers to hire staff with additional credentials/licensure and provide more training. For larger ALs this may be costlier but doable, while for small ALs this may be largely impossible, perhaps threatening closure of communities or significantly lowering their occupancy. On the other hand, in states with stricter admission and retention regulations, one may expect lower acuity among residents perhaps allowing AL providers to operate at lower cost.
Unlike AL providers who largely depend on private-pay residents and may therefore have varied interests in states’ regulatory stringency, state Medicaid agencies are likely to advocate for greater regulatory rigor as they become more financially invested in the care that AL communities provide to Medicaid beneficiaries. Indeed, we found that states with higher Medicaid spending had greater stringency with regard to dementia care, staffing and training, and the overall score. States may also have interest in controlling Medicaid beneficiaries access to AL services. Typically, states provide AL services under home and community-based service (HCBS) waivers, allowing them to target services to specific groups and to limit enrollment.13 More stringent admission and retention policies, which appeared to be associated with a lower proportion of Medicaid beneficiaries receiving AL services, are consistent with greater state controls. Furthermore, states in which greater regulatory oversight of nursing homes has been associated with higher quality (i.e. fewer deficiency citations) may be more likely to implement stronger AL staffing and training regulations to achieve higher quality in this care setting as well.
In states with greater preponderance of small ALs, regulatory stringency was lower, albeit marginally, for dementia care (and for overall stringency). Perhaps state regulators recognize that small ALs could not possibly abide by the same level of stringency as larger communities are able to do, and therefore where small ALs predominated, regulatory demands were lower.
Limitations
We acknowledge some limitations. Because our analysis was conducted at the state-level, we were limited by the number of covariates that could be simultaneously included in the model. However, this was an exploratory model and as such it identified a number of significant predictors of state stringency. While this study was national, four states were not included because of missing covariates. The impact of these exclusions on our findings is likely negligible as the number of communities in these excluded states accounts for <2% of all ALs. Our study was cross-sectional and only identified associations rather than causal inferences. State regulations are subject to continuous revisions and thus our findings with regard to regulatory stringency in 2019 may not be generalizable a few years from now.
CONCLUSIONS AND IMPLICATIONS
Our findings show that states vary significantly both with regard to AL policies that they choose to regulate and the stringency of these regulations. We identified several state-level factors significantly associated with regulatory stringency but the direction of these associations may depend on the particular policy domain being regulated. These associations are complex and more pointed insights, which are beyond the scope of this study, will require additional research.
State regulations provide a base requirement for all AL. However, AL communities within a state may set their own internal policies that may be more stringent.19,28 State and community-level regulations are typically imposed to control access to services and to improve care quality. Currently, however, very little is known about care quality in AL and the extent to which stricter regulations may actually improve quality and/or hinder access. Studies to understand the relationship between regulatory stringency and care quality are needed to identify areas that may need greater policy stringency, and where higher rigor may result in adverse access consequences.
Supplementary Material
Funding source:
This work was supported by the Agency for Healthcare Research and Quality grant number R01HS026893
Footnotes
Conflicts of Interest
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Harris-Kojetin L, Sengupta M, Lendon J, Rome V, Valverde R, Caffrey C. Long-Term Care Providers and services users in the United States: data from the National Study of Long-Term Care Providers, 2015–2016. Vital & health statistics Series 3 (43), Analytical and epidemiological studies / [US Dept of Health and Human Services, Public Health Service, National Center for Health Statistics]; 2019. p. x–xii; 1–105. [PubMed] [Google Scholar]
- 2.Caffrey C, Harris-Kojetin L, Sengupta M. Variation in Residential Care Community Resident Characteristics, by Size of Community: United States, 2014. NCHS brief 2015:1–8. [PubMed]
- 3.Caffrey C, Harris-Kojetin L. Variation in Operating Characteristics of Residential Care Communities, by Size of Community: United States, 2014. NCHS data brief 2015:1–8. [PubMed]
- 4.Rome V, Harris-Kojetin LD. Variation in Residential Care Community Nurse and Aide Staffing Levels: United States, 2014. National health statistics reports; 2016. p. 1–11. [PubMed]
- 5.Kisling-Rundgren A, Paul DP III, Coustasse A. Costs, Staffing, and Services of Assisted Living in the United States: A Literature Review. The Health Care Manager 2016;35:156–63. [DOI] [PubMed] [Google Scholar]
- 6.Carder PC. State Regulatory Approaches for Dementia Care in Residential Care and Assisted Living. Gerontologist 2017:776–86. [DOI] [PubMed]
- 7.Levinson D. Home and community based services in assisted living facilities. 2012.
- 8.Mollica RL. State Medicaid Reimbursement Policies and Practices in Assisted Living. Public Policy; 2009. p. 170.
- 9.Carder P, O’Keeffe J, O’Keeffe C. Compendium of Residential Care and Assisted Living Regulations and Policy: 2015 Edition. Rockville: 2015. [Google Scholar]
- 10.Caffrey C, Harris-Kojetin L, Rome V, Sengupta M. Operating characteristics of residential care communities, by community bed size: United States, 2012. NCHS data brief 2014:1–8. [PubMed]
- 11.Rome V, Harris-Kojetin LD. Variation in Residential Care Community Nurse and Aide Staffing Levels: United States, 2014. National health statistics reports 2016:1–11. [PubMed]
- 12.Thomas KS, Zhang W, Cornell PY, Smith L, Kaskie B, Carder PC. State Variability in the Prevalence and Healthcare Utilization of Assisted Living Residents with Dementia. J Am Geriatr Soc 2020. [DOI] [PMC free article] [PubMed]
- 13.GAO. Medicaid Assisted Living Services. Improved Federal Oversight of Beneficiary Health and Welfare is Needed. . Washington, DC: United States Government Accountability Office; 2018. [Google Scholar]
- 14.Trinkoff AM, Yoon JM, Storr CL, Lerner NB, Yang BK, Han K. Comparing residential long-term care regulations between nursing homes and assisted living facilities. Nurs Outlook 2019;68:114–22. [DOI] [PubMed] [Google Scholar]
- 15.Kaskie BP, Nattinger M, Potter A. Policies to protect persons with dementia in assisted living: Déjà vu all over again? Gerontologist 2015;55:199–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nattinger MC, Kaskie B. Determinants of the Rigor of State Protection Policies for Persons With Dementia in Assisted Living. J Aging Soc Policy 2017;29:123–42. [DOI] [PubMed] [Google Scholar]
- 17.Mead LC, Eckert JK, Zimmerman S, Schumacher JG. Sociocultural Aspects of Transitions From Assisted Living for Residents With Dementia. The Gerontologist 2005;45:115–23. [DOI] [PubMed] [Google Scholar]
- 18.Carder P, O’Keeffe J, O’Keeffe C. Compendium of Residential Care and Assisted Living Regulations and Policy: 2015 Edition. 2015; Rockville, MD. [Google Scholar]
- 19.Han K, Trinkoff AM, Storr CL, Lerner N, Yang BK. Variation Across U.S. Assisted Living Facilities: Admissions, Resident Care Needs, and Staffing. Journal of Nursing Scholarship 2017;49:24–32. [DOI] [PubMed] [Google Scholar]
- 20.Konetzka RT, Stearns SC, Park J. The staffing-outcomes relationship in nursing homes. Health Services Research 2008;43:1025–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schnelle JF, Simmons SF, Harrington C, Cadogan M, Garcia E, Bates-Jensen BM. Relationship of Nursing Home Staffing to Quality of Care. Health Services Research 2004;39:225–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stearns SC, Park J, Zimmerman S, Gruber-Baldini AL, Konrad TR, Sloane PD. Determinants and effects of nurse staffing intensity and skill mix in residential care/assisted living settings. The Gerontologist 2007;47:662–71. [DOI] [PubMed] [Google Scholar]
- 23.Harris-Wallace B, Schumacher JG, Perez R, et al. The Emerging Role of Health Care Supervisors in Assisted Living. Seniors housing & care journal 2011;19:97–108. [PMC free article] [PubMed] [Google Scholar]
- 24.Young HM, Sikma SK, Reinhard SC, McCormick WC, Cartwright JC. Strategies to Promote Safe Medication Administration in Assisted Living Settings. Research in Gerontological Nursing 2013;6:161–70. [DOI] [PubMed] [Google Scholar]
- 25.Hawes C, Phillips C, Rosełdots M. High service or high privacy assisted living facilities, their residents and staff: Results from a national survey. InfoassistPanphaOrg 2000:1–69.
- 26.Zimmerman S, Love K, Sloane PD, Cohen LW, Reed D, Carder PC. Medication administration errors in assisted living: Scope, characteristics, and the importance of staff training. Journal of the American Geriatrics Society 2011:1060–8. [DOI] [PubMed]
- 27.Young HM, Gray SL, McCormick WC, et al. Types, prevalence, and potential clinical significance of medication administration errors in assisted living. Journal of the American Geriatrics Society 2008;56:1199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zimmerman S, Sloane PD, Reed D. Dementia prevalence and care in assisted living. Health Affairs 2014;33:658–66. [DOI] [PubMed] [Google Scholar]
- 29.Harrington C, Mullan JT, Carrillo H. State nursing home enforcement systems. J Health Polit Policy Law 2004;29:43–73. [DOI] [PubMed] [Google Scholar]
- 30.Mukamel DB, Weimer DL, Harrington C, Spector WD, Ladd H, Li Y. The effect of state regulatory stringency on nursing home quality. Health Services Research 2012;47:1791–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nyman JA. Improving the quality of nursing home outcomes. Are adequacy- or incentive-oriented policies more effective? Med Care 1988;26:1158–71. [DOI] [PubMed] [Google Scholar]
- 32.Howard DL, Sloane PD, Zimmerman S, et al. Distribution of African Americans in residential care/assisted living and nursing homes: more evidence of racial disparity? Am J Public Health 2002;92:1272–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.NCAL. 2019 Assisted Living State Regulatory Review. 2019. https://www.ahcancal.org/ncal/advocacy/regs/Pages/AssistedLivingRegulations.aspx
- 34.Genworth I Cost of Care Survey 2016: Methodology. https://www.genworth.com/dam/Americas/US/PDFs/Consumer/corporate/48590_050516.pdf
- 35.Charmaz K Constructing grounded theory. 2014. Second edition. Sage Publishing, Los Angeles, CA. [Google Scholar]
- 36.Li Y, Cen X, Cai X, Temkin-Greener H. Perceived Patient Safety Culture in Nursing Homes Associated with “Nursing Home Compare” Performance Indicators. Medical Care 2019; 57(8):641–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yan D, Wang S, Temkin-Greener H, Cai S. Quality of Nursing Homes and Admission of Residents with Alzheimer’s Disease and Related Dementias: The Potential Influence of Market Factors and State Policies. Journal of the American Medical Directors Association 2020;In press. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


