Abstract
Despite knowledge of subsequent melanoma risk and the benefit of sun protection in risk reduction, melanoma survivors often do not engage in adequate sun protection and continue to sunburn at rates similar to individuals without a history of skin cancer. This novel intensive intervention provided a wearable UV sensor delivering real-time UV exposure with a smartphone and daily text messages. On days 1-10 (period 1), behavioral facilitation and outcome expectancies messages were provided. On day 10, participants reviewed and reflected on their daily UV exposure on the previous 10 days and set goals for improving sun protection. Then on days 11-21 (period 2) self-efficacy and self-regulation messages were provided. Sixty melanoma survivors were randomized (1:1) to receive structured or unstructured goal setting queries on day 10. Controlling for cloudy/ rain conditions with less UV due to weather, there was a time effect with a significant decrease in UV exposure from periods 1-2 [period 1-2, F (59) = 22.60, p < 0.0001]. In this short-term study, melanoma survivors managed their daily UV exposure to stay below their maximum tolerated UV dose.
Keywords: melanoma, primary prevention, sun protection, mobile health, wearable sun sensor technology
INTRODUCTION
Despite community-wide mass media campaigns [1], sun protection remains inadequate in the general population [2,3]. The annual rate of sunburn has not changed in the last twenty years; thus, 50% of United States (US) adults with sun sensitive skin sunburn annually [4,5]. Sun protection can reduce the risk of developing melanoma [6–8]. Many decades of research showed that melanoma survivors failed to put knowledge into practice by engaging in adequate sun protection and continued to sunburn at rates similar to individuals with no history of skin cancer [9–11]. Following melanoma diagnosis, melanoma survivors reported improvements in sun protection, primarily sunscreen use [10,11]. However, survivors did not wear sunscreen as frequently as recommended [12,13] and did not practice sun avoidance during peak hours [12]. Furthermore, while melanoma survivors initially increased sun protection efforts following diagnosis, most melanoma survivors did not maintain the changes [13,14]. In one study, melanoma survivors received more exposure than control subjects at 3 years post-diagnosis [13]. In a mid-West US study, melanoma survivors and controls reported high sun exposure on weekends [15]. Twenty-seven percent of melanoma survivors reported sunburn in the past 12 months [2]. Since early stage melanoma survivors are typically otherwise healthy adults, who had an active outdoor lifestyle prior to developing melanoma, they wanted to continue to enjoy outdoor activities that were important to their quality of life; therefore, it was difficult for them to adhere to the universal sun protection recommendations, which included limiting outdoor activities from 10 AM to 4 PM [16,17].
A recent mHealth innovation, a wearable personal ultraviolet light (UV) sensor, instantaneously measures UV dose and reports it as well as the accumulated daily UV dose to the user’s smartphone [18]. Although UV sensors have been previously employed for research studies on sun exposure [13,19] such sensors have not entered widespread use as patient-facing educational tools. While the technology existed to deliver UV sensor data to connected smartphone applications, very little research has addressed change in sun protection behavior using this technology. The aim of this mixed methods study was to investigate short-term change in UV exposure among melanoma survivors receiving the intervention, which consisted of wearing the UV sensor, using the app providing daily UV exposure and receiving daily short message service (SMS-based) behavioral sun protection messages. The study did not address long-term maintenance after the intensive intervention ceased.
MATERIALS AND METHODS
Population
Patients with a history of melanoma were recruited using the Enterprise Data Warehouse (EDW) of Northwestern University, which is a repository of patients willing to participate in research obtained by searching the electronic medical records of Northwestern Medicine for eligible participants. Inclusion criteria consisted of: a) history of Stage 0 to IIB melanoma diagnosed within the prior two years, b) being age 18-80 years old, c) willing to use a smartphone to sync with the wearable device, d) having a reliable internet connection at home, e) familiarity with smartphones and mobile applications, f) willing to come to the Chicago campus of Northwestern University for two in-person appointments, and g) affirmation that they would be outdoors for at least 1 hour a day with at least 30 consecutive minutes throughout the 21 days of the research. First, letters were sent to potentially eligible patients identified by searching the electronic medical records of the Northwestern Medicine health care system with EDW. If there was no response to the letter, then a telephone call was made to explain the study to the potential participant. If there was no answer to the telephone call, a scripted voicemail provided a call back number. The institutional review board of Northwestern University approved the study. Participants provided written consent and were offered gift cards.
Equipment
The wrist worn UV sensor and Android phone (Samsung S9) with the application were provided to each participant. The UV dosimeter (sensor) was a battery-free, miniaturized, wireless, waterproof, 8 mm in diameter, 1.1 mm in thickness device weighing 51 mg that registered UVA (Wearifi, Chicago, IL) [18]. The UV dosimeter was worn with the face containing the UVA photodiode on the dorsal aspect of the wrist (Wearifi, Inc.). The photodiode generated a photocurrent with a magnitude that correlates with the instantaneous exposure intensity. Throughout a period of exposure, the resulting photocurrent continuously charged the supercapacitor. The accumulated charge on the supercapacitor was a function of exposure dose. Wireless readout involved the transmission of the voltage that develops on the supercapacitor via the digital output from the analog-to-digital converter. A calibration factor converted the raw voltage measurement to cumulative exposure dose. The mobile application syncs to the sensor via near-field communication (NFC) with the back of the provided Android phone, providing real-time UVA exposure and cumulative daily UVB. Participants viewed and assessed their exposure throughout the day whenever they sync the device. In addition, users received a cumulative summary of their daily UVB exposure for each of the preceding days during the 21 study days.
Intervention
This intervention paired a wearable UV sensor reporting real-time UV dose to the smartphone, with behavioral change strategies employing a series of daily text messages. On days 1-10 behavioral facilitation and outcome expectancies messages were provided. Then on day 10, participants were invited to review and reflect about their daily UV exposure on the prior 10 days and selected or created goals to improve their sun protection. On days 11-21, self-efficacy and self-regulation messages were provided. Messages developed in focus groups and structured interviews with melanoma survivors in the summer of 2018 were refined with four focus groups consisting of 8 melanoma survivors in each group. Focus group participants were excluded from participating in interventional research.
The health behavior framework was Green and Kreuter’s Precede-Proceed Model, which categorizes the following three antecedents to behavioral change: 1) predisposing factors, 2) enabling factors, and 3) reinforcing factors [20]. Melanoma survivors had the predisposing factor of perception of their susceptibility to the dangers of sun exposure causing skin cancer. The easy to wear UV sensor that provided real-time personal UV exposure enabled change. Lastly, the text reminders and goal setting exercise were reinforcing factors.
During the baseline visit in the research office, participants were given the cumulative daily UVB dose their skin could tolerate without getting a sunburn (minimal erythema dose for skin type I 200 J/m−2, II 250, III 300, IV 400, V and VI> 600) [21]. Participants were shown how to sync the provided android phone with the UV sensor. The app demonstration included screens displaying the real-time UVA exposure. Participants were told that the UVB exposure could be obtained in real-time by dividing the UVA exposure displayed on the smartphone by 20 [22]. At the end of each day, the cumulative daily UVB exposure was provided on the screen of the phone. Participants compared daily UVB exposures received on the preceding days on the phone. Participants were asked to wear the UV sensor daily on their wrist for 21 days from 6 AM to 6 PM or until they remained inside for the evening. If they wore a long-sleeved shirt, they were asked to place the sensor outside the sleeve. This sensor placement was demonstrated by enlarging the band that circled the wrist and placing the sensor of the wrist with the face on the dorsal aspect of the wrist. Participants were informed that the sensor reported exposure of the wrist, which would be different for other locations on the body and did not consider the person’s use of sun protection. Participants received daily text messages to sync the device each morning, mid-day, afternoon and evening. They could sync the sensor as many times during the day as they wished to obtain the UV dose during an outdoor period.
Four thematic groups of text messages were provided daily in the following sequence: a) behavioral facilitation (Some shade structures provide low protection (SPF=2-5) due to reflection of sun. [23]), b) outcome expectancies (A “base tan” will only give you a SPF of 4 and does not prevent sunburn), c) self-efficacy (Keeping track of your UV exposure each day will get you a little closer to achieving your fullest potential), and d) self-regulation (Your health is important to you. Remember to use sun protection to prevent skin cancer.) Then, on the evening of day 10, all participants received a text message prompting them to review and reflect on their daily UV for the prior 10 days. Those randomized to the structured goal setting were provided with the following question: How will you meet your goal to engage in sun-protected outdoor activity? Choose a strategy to help you achieve your goal. Tomorrow, I will: a) apply sunscreen to all areas of my body that may be exposed to the sun. b) apply sunscreen before I go outdoors. c) wear a hat when I am outdoors. d) wear a shirt that covers my shoulders when I am outdoors. e) plan my outdoor activities to avoid being outside from 10AM to 2 PM. f) pay attention to the strength of the sun by checking the UV report 15 minutes after I go outside. g) be careful not to exceed the amount of UV my skin can tolerate. After selecting one item, participants were asked: Are you able to select more than one strategy to start doing? If yes, the same list was provided. Participants randomized to unstructured goal setting were asked: What will you do next week to reach your sun protected outdoor activity goal? A free text box provided the instruction: Tell us the specific action you will take tomorrow to achieve your sun-protected outdoor activity goal.
After the baseline in office visit, participants accessed the survey with a link to the electronic database REDCap [24] that randomized participants (1:1) to receive structured or unstructured goal setting queries in the evening of day 10. All research personnel were masked to the randomization.
Measures
Self-reported online surveys
Baseline self-reported responses included age, gender, race /ethnicity, household income, skin type, sunburn in the last 21 days, knowledge and attitudes about sun protection, and perception of their risk of getting skin cancer. (Table 1) The measures were used in prior sun exposure and protection studies [25, 26]. Daily sunburn was self-reported online each evening. The daily high temperature and sun/cloudy/rain conditions were obtained from the National Weather Service for the geographic location of the participant. Daily UV exposure for each participant was obtained from the wearable UV sensor.
Table 1.
Description of the population
|
| |||||
|---|---|---|---|---|---|
| Variable | level | Overall | Structured Goals | Unstructured Goals | P |
|
| |||||
| n | 60 | 31 | 29 | ||
| Age [mean (SD)] | 59.3 (12.5) | 59.9 ( 12.5) | 58.6 ( 12.7) | 0.687 | |
| Gender (%) | Female | 36 ( 60.0) | 18 ( 58.1) | 18 ( 62.1) | 0.958 |
| Male | 24 ( 40.0) | 13 (41.9) | 11 ( 37.9) | ||
| Education (%) | High school graduate | 1 ( 1.7) | 0 ( 0.0) | 1 ( 3.4) | 0.180 |
| Some post-high school education | 5 ( 8.3) | 3 ( 9.7) | 2 ( 6.9) | ||
| College graduate | 26 ( 43.3) | 17 ( 54.8) | 9 ( 31.0) | ||
| Graduate degree | 28 ( 46.7) | 11 ( 35.5) | 17 ( 58.6) | ||
| Income (%) | $10,000 to $19,999 | 1 ( 1.7) | 1 ( 3.2) | 0 ( 0.0) | 0.057 |
| $20,000 to $34,999 | 3 ( 5.0) | 3 ( 9.7) | 0 ( 0.0) | ||
| $35,000 to $50,999 | 3 ( 5.0) | 1 ( 3.2) | 2 ( 6.9) | ||
| $51,000 to $100,000 | 13 ( 21.7) | 4 ( 12.9) | 9 ( 31.0) | ||
| Over $100,000 | 34 ( 56.7) | 21 ( 67.7) | 13 ( 44.8) | ||
| Prefer not to answer | 6 ( 10.0) | 1 ( 3.2) | 5 ( 17.2) | ||
| Race (%) | White | 60 (100.0) | 31 (100.0) | 29 (100.0) | NA |
| Ethnicity (%) | Non-Hispanic | 59 ( 98.3) | 30 ( 96.8) | 29 (100.0) | 1.000 |
| Hispanic | 1 ( 1.7) | 1 ( 3.2) | 0 ( 0.0) | ||
| Skin Type (%) | 1 | 42 ( 70.0) | 25 ( 80.6) | 17 ( 58.6) 0.080 | |
| 2 | 15 ( 25.0) | 6 ( 19.4) | 9 ( 31.0) | ||
| 3 | 3 ( 5.0) | 0 ( 0.0) | 3 ( 10.3) | ||
NA= not applicable
Focus groups and in person exit interviews
Four focus groups of 8 melanoma survivors assessed each of the following items: a) the form of the UV sensor, b) presentation of UV exposure in the app, and c) the desirability, time, and type of daily text messages.
Semi-structured in person exit interviews were conducted by qualitatively trained research personnel. Interviews were 30-45 minutes long, and audio-recorded with consent. Interview questions assessed the acceptability of wearing the UV sensor, and using the app. Participants’ opinions about what was helpful and what could be changed in the following aspects of the program: information provided by the UV sensor exposure and app , the daily text messages and goal setting. The research staff’s field notes recorded non-verbal communications. Audio-recordings were transcribed for analysis (see qualitative data analysis).
Statistical analysis
Baseline characteristics of the sample, knowledge, and attitudes are given as counts and percentages. Age is presented as mean and standard deviation (SD). UV data was compared over time and between groups, while adjusting for daily weather conditions (sunny, raining or cloudy, high temperature), using mixed effects models with an unstructured covariance matrix, and accounting for repeated measures over time per participant. Estimates of daily UV exposure are presented as least square means (LSM) and standard errors (SE), and 95% confidence intervals. Models were fit using PROC MIXED in SAS v 9.4 (Cary, NC). All data was prepared and analyzed using R 3.6.0 or SAS 9.4.
Qualitative data analysis: identification of themes in structured interviews
The transcripts of focus groups and exit interviews and the research staff’s field notes of non-verbal communications were reviewed by two team members (DD, JKR), who had not performed the exit interview. They evaluated the audio transcripts for key patterns and themes using a combination of inductive and deductive thematic analysis [27, 28]. Each interview was coded independently, with team members remaining open to finding new patterns (inductive) [29] and guided by existing approaches to sun protection guidelines (deductive). Content was labeled according to the existing codes, and new codes were created to capture additional relevant themes. Initial themes were generated by interpretation and consensus discussions [30] between an experienced clinical researcher (JKR) and a research project manager (DD) based upon 25% of the transcribed interviews. After the primary codebook was developed, the remaining interviews were coded. The team met to discuss the interpretations, come to consensus, and identify data-driven approaches to summarize the findings from the interviews.
RESULTS
Focus groups
Four focus groups of eight melanoma survivors having a mean (standard deviation, SD) age of 52.1 (10.6) years with 44% (14 men of 32 participants) preferred a wrist worn device rather than one that attached to clothing. (n=32) Since our previous observational study explored sun exposure and protective behavior among melanoma survivor without immediate feedback from the sensor [31], focus groups for this study assessed the smartphone screen presentation of UV exposure. The presentation on the screen was adapted in subsequent focus groups until no further changes were needed. The first screen presented the UVA exposure at intervals created by syncing the phone, the second screen gave the cumulative daily UVB exposure, and the third presented a table of the daily UVB exposure, the date, and day of the week. Finally, focus group participants wanted to receive text messages daily at 10-11 AM that provided new ways to improve their sun protection. Melanoma survivors stated they did not want to receive text messages with the same four sun protection messages that they already knew. Participants in the first two focus groups noted a need to make a personal commitment to making improvements and setting a date to do it. This theme was refined in subsequent focus groups to review the individual’s performance and set goals for sun protection improvement at the mid-point of the program. A pledge of “I will…” was perceived as the best way to make the commitment.
Population receiving intervention
Sixty melanoma survivors with a mean (standard deviation, SD) age of 59.3 (12.5) years were randomized to receive structured or unstructured goal setting. There were no clinically relevant differences in gender, age, socioeconomic status or skin type between the two groups (Table 1). Similarly, there were no differences in baseline knowledge or attitudes about sun exposure or protection between the two groups. (Table 2). A pertinent lack of knowledge among most (83.3%) participants was the failure to state that “light-complexioned people will get a sunburn when the UVI is 3 or more” was true.
Table 2.
Baseline Sun exposure and sun protection knowledge and attitudes
| Variable | level | Overall | Structured Goals | Unstructured Goals | p |
|---|---|---|---|---|---|
| n | 60 | 31 | 29 | ||
| Knowledge | |||||
| Select the lowest number of the UV Index when light-complexioned people will get a sunburn. (%) | 1 | 32 ( 53.3) | 17 ( 54.8) | 15 ( 51.7) | - |
| 2 | 17 ( 28.3) | 8 ( 25.8) | 9 ( 31.0) | ||
| 3 | 10 ( 16.7) | 6 ( 19.4) | 4 ( 13.8) | ||
| 4 | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| 5 | 1 ( 1.7) | 0 ( 0.0) | 1 ( 3.4) | ||
| The strength of the sun depends on (% correct) | All the above | 57 ( 95.0) | 30 ( 96.8) | 27 ( 93.1) | 0.953 |
| In the greater Chicago area, the strength of the sun starts to increase in: (%) | March | 15 ( 25.0) | 6 ( 19.4) | 9 ( 31.0) | 0.201 |
| April | 1 ( 1.7) | 1 ( 3.2) | 0 ( 0.0) | ||
| May | 4 ( 6.7) | 4 ( 12.9) | 0 ( 0.0) | ||
| June | 26 ( 43.3) | 14 ( 45.2) | 12 ( 41.4) | ||
| July | 14 ( 23.3) | 6 ( 19.4) | 8 ( 27.6) | ||
| Standing at the edge of the shadow cast by the beach umbrella will give me enough sun protection. (%) | True | 3 ( 5.0) | 1 ( 3.2) | 2 ( 6.9) | 0.953 |
| False | 57 ( 95.0) | 30 ( 96.8) | 27 ( 93.1) | ||
| People can get a sunburn on a cloudy day. (%) | True | 60 (100.0) | 31 (100.0) | 29 (100.0) | - |
| False | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| When you are fishing, a baseball cap will provide sufficient sun protection. (%) | True | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | - |
| False | 60 (100.0) | 31 (100.0) | 29 (100.0) | ||
| A good way to figure out if a tree gives enough shade for complete sun protection is to look at the ground and see if there are spots of sun. (%) | True | 30 ( 50.0) | 14 ( 45.2) | 16 ( 55.2) | 0.605 |
| False | 30 ( 50.0) | 17 ( 54.8) | 13 ( 44.8) | ||
| If a person is running fast, they will not get a sunburn. (%) | True | 1 ( 1.7) | 0 ( 0.0) | 1 ( 3.4) | 0.973 |
| False | 59 ( 98.3) | 31 (100.0) | 28 ( 96.6) | ||
| Walking outside at noon for about 1 hour is not enough exposure to need sun protection (%) | True | 1 ( 1.7) | 1 ( 3.2) | 0 ( 0.0) | 1.000 |
| False | 59 ( 98.3) | 30 ( 96.8) | 29 (100.0) | ||
| Attitudes | |||||
| I am at risk of getting skin cancer. (%) | Strongly agree | 54 ( 90.0) | 28 ( 90.3) | 26 ( 89.7) | - |
| Agree | 6 ( 10.0) | 3 ( 9.7) | 3 ( 10.3) | ||
| Undecided | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Strongly disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| It is important to protect my skin from the sun. (%) | Strongly agree | 58 ( 96.7) | 29 ( 93.5) | 29 (100.0) | - |
| Agree | 2 ( 3.3) | 2 ( 6.5) | 0 ( 0.0) | ||
| Undecided | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Strongly disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Skin cancer is an important disease. (%) | Strongly agree | 58 ( 96.7) | 29 ( 93.5) | 29 (100.0) | - |
| Agree | 2 ( 3.3) | 2 ( 6.5) | 0 ( 0.0) | ||
| Undecided | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Strongly disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Regular use of sun protection helps to prevent skin cancer. (%) | Strongly agree | 52 ( 86.7) | 27 ( 87.1) | 25 ( 86.2) | - |
| Agree | 7 ( 11.7) | 3 ( 9.7) | 4 ( 13.8) | ||
| Undecided | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Disagree | 1 ( 1.7) | 1 ( 3.2) | 0 ( 0.0) | ||
| Strongly disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| I am very confident that I know how strong the sun is. (%) | Strongly agree | 11 ( 18.3) | 4 ( 12.9) | 7 ( 24.1) | 0.523 |
| Agree | 34 ( 56.7) | 20 ( 64.5) | 14 ( 48.3) | ||
| Undecided | 10 ( 16.7) | 4 ( 12.9) | 6 ( 20.7) | ||
| Disagree | 4 ( 6.7) | 2 ( 6.5) | 2 ( 6.9) | ||
| Strongly disagree | 1 ( 1.7) | 1 ( 3.2) | 0 ( 0.0) | ||
| I am very confident that I can protect myself from getting a sunburn. (%) | Strongly agree | 20 ( 33.3) | 12 ( 38.7) | 8 ( 27.6) | - |
| Agree | 33 ( 55.0) | 17 ( 54.8) | 16 ( 55.2) | ||
| Undecided | 4 ( 6.7) | 0 ( 0.0) | 4 ( 13.8) | ||
| Disagree | 3 ( 5.0) | 2 ( 6.5) | 1 ( 3.4) | ||
| Strongly disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| How concerned are you about developing skin cancer? (%) | Extremely | 43 ( 71.7) | 20 ( 64.5) | 23 ( 79.3) | - |
| Moderatel | 15 ( 25.0) | 10 ( 32.3) | 5 ( 17.2) | ||
| Somewhat | 1 ( 1.7) | 0 ( 0.0) | 1 ( 3.4) | ||
| Slightly | 1 ( 1.7) | 1 ( 3.2) | 0 ( 0.0) | ||
| Not at all | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| If I don’t protect my skin from the sun, I will feel very vulnerable to getting skin cancer in my lifetime. (%) | Strongly agree | 49 ( 81.7) | 25 ( 80.6) | 24 ( 82.8) | - |
| Agree | 9 ( 15.0) | 6 ( 19.4) | 3 ( 10.3) | ||
| Undecided | 1 ( 1.7) | 0 ( 0.0) | 1 ( 3.4) | ||
| Disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Strongly disagree | 1 ( 1.7) | 0 ( 0.0) | 1 ( 3.4) | ||
| If I don’t protect my skin from the sun, I feel that my chances of getting skin cancer in my lifetime are high. (%) | Strongly agree | 52 ( 86.7) | 26 ( 83.9) | 26 ( 89.7) | - |
| Agree | 8 ( 13.3) | 5 ( 16.1) | 3 ( 10.3) | ||
| Undecided | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) | ||
| Strongly disagree | 0 ( 0.0) | 0 ( 0.0) | 0 ( 0.0) |
Completion of measures
All 60 participants completed the study, which required participation for 21 days. In 1260 study days, 3% of days (37 days) had missing self-reported surveys. There were 35 days with missing UV exposure, including days when rain precluded going outside and the UV sensor was not worn nor was the survey completed. Thus, feasibility of wearing the UV sensor daily and completing the daily self-report online survey was achieved by 97.8% of participants when the weather permitted going outside. Since the temperature range was from 18°- 31° C (65°-88° F), temperature did not preclude being outside. No melanoma survivors developed a sunburn.
Daily UV exposure
Two time periods were compared for UV exposure. Period 1, days 1-10, was prior to the review and reflection on UV exposure and goal setting. Period 2, days 11-21, was after goal setting. Controlling for cloudy/ rain conditions with less available UV, there was a time effect with a significant decrease in UV exposure from periods 1-2 [period 1-2, least square mean difference, (LSMd), J/m2 (standard error, SE) 344.2 (72.3), F (59) = 22.60, p < 0.0001]. (Table 3, Fig 1)
Table 3.
Daily UVA dose by Time Period (Least Squares Means)
|
| |||
|---|---|---|---|
| Time Period (Days) | Estimated UVA dose (J/m2) | Lower | Upper |
|
| |||
| 1 (1-10) | 1062.80 | 864.8 | 1260.8 |
| 2 (11-21) | 718.64 | 519.1 | 918.2 |
Figure 1.
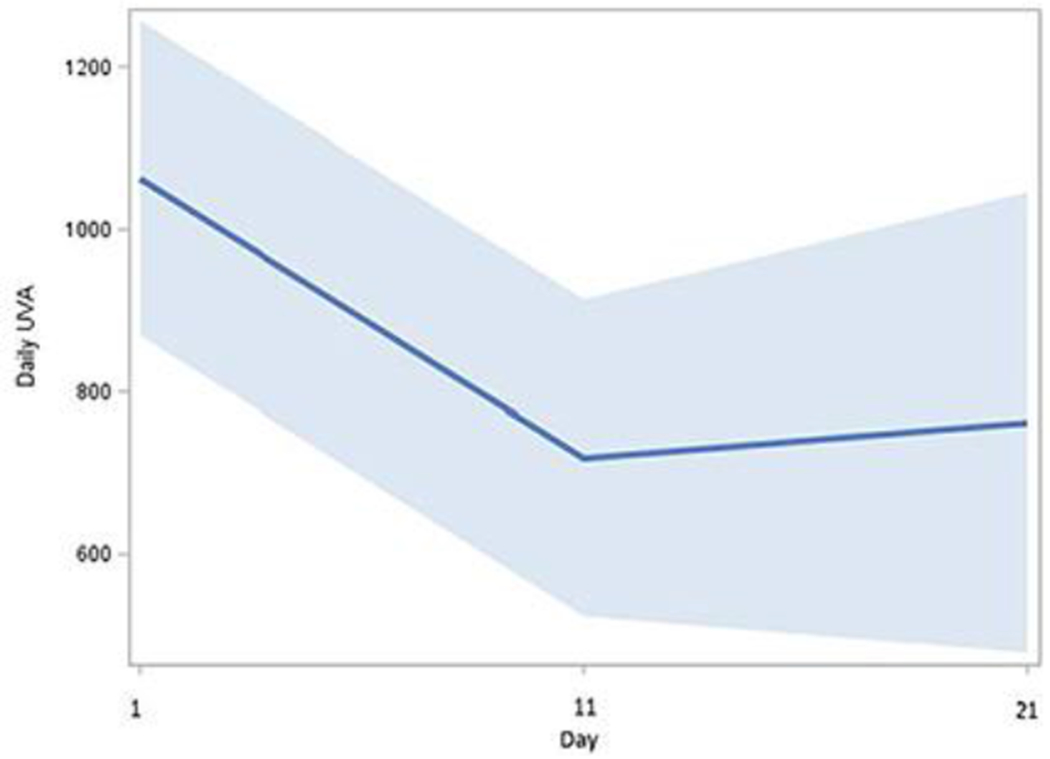
Mean daily UVA exposure over time
Daily UVA exposure (J/m2) decreased significantly from period 1 (day 1-10) to period 2 (day 11-21). Review of daily UVA exposure on days 1-10 and goal setting was performed by melanoma survivors on the evening of day 10.
Comparing Structured and Unstructured Goal Setting Groups
Modeling the differences for the two groups over periods 1-2 did not show a statistically significant interaction between melanoma survivors randomized to structured or unstructured goal setting and time period [F (58) = 2.05, p =0.1385]. (Table 4) However, as shown in Figure 2, while the LSM daily UVA exposure decreased in both groups during period 1-2, LSM exposure differed by group in period 2. Participants in the unstructured goal setting reduced exposure in period 2 by a LSMd (SE) of 196.8 (129.1) J/m2; whereas participants randomized to structured goal setting decreased exposure by a LSMd (SE) of 399.0 (120.6) J/m2. While mean UVA exposure decreased in both groups immediately after goal setting (day 11), melanoma survivors in the unstructured group did not maintain the reduction in UVA exposure from days 11-21. (Fig 2).
Table 4.
Daily UVA Exposure by Time Period and Goal Setting (Least Squares Means)
|
| ||||
|---|---|---|---|---|
| Goal Setting | Time Period (Days) | Estimated UVA dose (J/m2) | Lower | Upper |
|
| ||||
| Structured | 1 (1-10 ) | 1008.82 | 734.12 | 1283.52 |
| Structured | 2 (11-21) | 609.78 | 210.93 | 1008.63 |
| Unstructured | 1 (1-10) | 1108.40 | 826.90 | 1389.90 |
| Unstructured | 2 (11-21) | 911.58 | 495.91 | 1327.25 |
Figure 2.
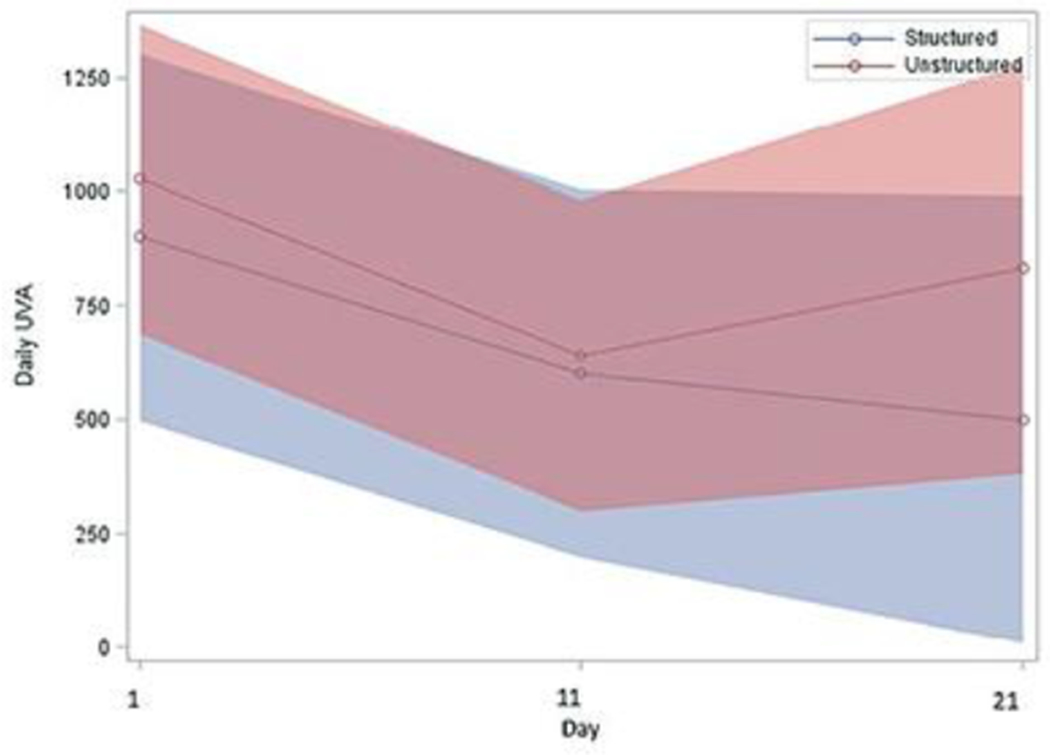
Mean daily UVA exposure over time by structured or unstructured group
After performing goal setting in the evening of day 10, participants randomized to the structured goal (blue) setting demonstrate sustained reduction in daily UVA dose.
All participants randomized to the structured goals selected one strategy (n=31) and 14 selected a second strategy. In descending order of frequency, the responses were “ tomorrow, I will”: a) apply sunscreen to all areas of my body that may be exposed to the sun (n=12), b) apply sunscreen before I go outdoors (n=7), c) plan my outdoor activities to avoid being outside from 10 AM to 2 PM (n=7), d) pay attention to the strength of the sun by checking the UV sensor report 15 minutes after I go outside (n=5), e) be careful not to exceed the amount of UV my skin can tolerate (n=5), f) wear a hat when I am outdoors (n=5), and g) wear a shirt that covers my shoulders when I am outdoors (n=4).
No free text responses were obtained from 13 of the 29 participants randomized to the unstructured goal setting and none used the word “I” in the responses or set a time to start. The following themes were identified in the free text responses: a) apply sunscreen before going outside (n=8), b) do outside activities before 10 AM (n=4), c) avoid being outside (n=3), d) reapply sunscreen (n =3), e) wear protective clothing (n=2).
Themes Identified with Exit Interviews
Melanoma survivors related that they preferred using the UV sensor to determine their UVA exposure during commonly performed outdoor activities, e.g. gardening. These survivors preferred the UVA exposure recorded by the sensor in real-time rather than the cumulative daily UVB exposure provided at the end of the day. Knowing the amount of real-time UV exposure helped participants to change their habitual outdoor activities and stay below their maximum tolerated dose, e.g. shifted gardening before 10 AM, reduced the time walking the dog at noon. Melanoma survivors appreciated knowing their activity-related UV exposure, and felt this knowledge gave them the freedom to do outdoor activities that they enjoy with friends and family without restricting all outdoor activities from 10 AM to 4 PM. In exit interviews, 8 of the 15 participants who selected apply sunscreen before I go outdoors noted the surprising amount of UVA exposure received while driving to work in the morning and said it was a “wake up call”.
Participants expressed a desire to retain all three aspects of the intervention (UV sensor and app, daily text messages, and goal setting). Those receiving the structured goal setting felt the different aspects of the program helped to hold their attention; however, participants in the unstructured goal setting arm stated they wanted to be given a choice of goals. Some participants would have preferred tailored messages that evaluated their current sun protection and offered specific suggestions for improvements.
DISCUSSION
This novel intensive intervention pairing technology, a wearable UV sensor with real-time UV exposure provided on a smartphone, with behavioral change supported by a series of daily text messages, review and reflection on daily UV exposure during the prior 10 days, and structured and unstructured goal setting resulted in short-term reduction in daily UV exposure. The UVA exposure was a larger number than the UVB exposure because a) summer sunlight was comprised of about 95% UVA and 5% UVB [22], and b) UVA penetrated the side, rear and sun roof windows of cars of melanoma survivors, who spent about 1.5 hours a day commuting to work. This large UVA number served as a “wake up call” to improve sun protection. Melanoma survivors used the UVA exposure reported by the sensor after 15 minutes outside to adjust the time spent outdoors doing commonly performed activities and stayed below their maximum tolerated daily UVB exposure.
Text message-based programs used by others have summarized the local weather forecast for the hours around noon which have the most intense UV radiation and made predictions based on the UV Intensity in the participant’s geographic location [32]. This approach lacks the personal relevance provided by the wearable UV sensor and app used in this study. Behavioral messages provided in other programs were general prompts to wear sun-safe clothing and sunscreen. The daily behavioral messages provided in this study were evaluated and refined by melanoma survivors, who advised on the sequence of messages and the need to make a commitment to improve sun protection.
Reducing the proportion of adults who report sunburn was objective C-20.2 of Healthy People 2020 [33]. Sunburn is a biologic measure of UVB over exposure in the at-risk population. The sun sensitive population was expected to be receptive to warnings about approaching the “sunburn danger zone” communicated to users’ smartphones [34]. Our research suggested that reporting real-time UVA exposure recorded by the UV sensor in combination with daily text messages received by melanoma survivors, who were sun sensitive people, motivated reduction in sun exposure. In the last decade DNA damage from UVA exposure was identified [35, 36] and UVA was recognized as a causative factor in the development of human melanoma [37, 38] Recognition that excessive UVA exposure from indoor tanning caused melanoma formed the basis for our study design that monitored real-world UVA exposure and provided UVA exposure to melanoma survivors [39–42].
Despite the limitations of a 21-day study, this study contributed to the field as the first to document behavioral change attributable to an intervention incorporating real-time UVA exposure obtained from a wearable UV sensor with sequential daily text messages including goal setting. Self-management of UV exposure was maintained better among those randomized to receive structured goal setting than those who created their own free text responses (unstructured). The structured goal responses defined the time to initiate the behavior (tomorrow) and the pledge: “I will do…”. Establishing personal goals was an important part of the self-management process in this study [43]. In the future, reinforcement of personal goals with personalized text messages that integrate participant characteristics, moods and the environmental context may improve maintenance of reduced UV exposure [44].
In this study, participants determined in-the-moment their own UVA exposure recorded by the wearable UV sensor. Then, participants adapted their sun exposure to their needs and preferences for outdoor activities during the hours of peak sun intensity. Results from studies to date on sun protection behaviors among melanoma survivors have been mixed, though most suggested that if an improvement in sun behaviors among melanoma survivors was present, it was moderate and not maintained [45,46]. Self-management by the participants in this study preserved their quality of life with enjoyment of outdoor activities. This approach may allow others who are at-risk to develop melanoma to improve and maintain sun protection.
Acknowledgments
Funding
Research reported in this publication was supported by the National Cancer Institute (R44 CA224658). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
ClinicalTrials.gov Protocol Record NCT0334796, date of registration Nov 15, 2017
Conflicts of interest
There are no conflicts of or competing interests for the following authors (JKR, EG, MK, SYH, MWK) Mr. Banks and Dr. Rogers declare a relationship with Wearifi, Inc. and a patent on the device (U.S. Patent Application: 15/578,602 and U.S. Patent Application No.: 15/578,617).
Ethics approval
All procedures performed in these studies involving human participants were in accordance with the ethical standards of the institution established by the Institutional Review Board of Northwestern University. This article does not contain any studies with animals performed by any of the authors.
Consent to participate.
Written consent to participate in the study was obtained from all participants.
Data Availability The data are not publicly available due to their containing information that could compromise the privacy of research participants. Deidentified data are available upon request from the corresponding author, [JKR].
References
- 1.Wu YP, Aspinwall LG, Conn BM, Stump T, Grahmann B, Leachman SA. A systematic review of interventions to improve adherence to melanoma preventive behaviors for individuals at elevated risk. Prev Med. 2016;88:153–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bränström R, Kasparian NA, Chang YM, Affleck P, Tibben A, Aspinwall LG, et al. Predictors of sun protection behaviors and severe sunburn in an international online study. Cancer Epidemiol Biomarkers Prev. 2010; 19(9):2199–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holman DM, Berkowitz Z, Guy GP Jr., Hartman AM, Perna FM. The association between demographic and behavioral characteristics and sunburn among U.S. adults - National Health Interview Survey, 2014. Prev Med. 2014;63:6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buller DB, Cokkinides V, Hall HI, et al. Prevalence of sunburn, sun protection, and indoor tanning behaviors among Americans: review from national surveys and case studies of 3 states. J Am Acad Dermatol. 2011;65:S114–23. [DOI] [PubMed] [Google Scholar]
- 5.Holman DM, Ding H, Guy GP, et al. Prevalence of sun protection use and sunburn and association of demographic and behavioral characteristics with sunburn among US adults. JAMA Dermatol. 2018;154 (5):51–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Erdmann F, Lortet-Tieulent J, Schuz J, et al. International trends in the incidence of malignant melanoma 1953-2008--are recent generations at higher or lower risk? Internat J Cancer. 2013;132(2):385–400. [DOI] [PubMed] [Google Scholar]
- 7.Whiteman DC, Green AC, Olsen CM. The Growing Burden of Invasive Melanoma: Projections of Incidence Rates and Numbers of New Cases in Six Susceptible Populations through 2031. J Invest Dermatol. 2016;136(6):1161–1171. [DOI] [PubMed] [Google Scholar]
- 8.Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol. 2010;29:257–63. [DOI] [PubMed] [Google Scholar]
- 9.Diao DY, Lee TK. Sun-protective behaviors in populations at high risk for skin cancer. Psychol Res Behav Manag. 2013;20:9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freiman A, Yu J, Loutfi A, Wang B. Impact of melanoma diagnosis on sun-awareness and protection: efficacy of education campaigns in a high-risk population. J Cutan Med Surg. 2004; 8:303–9. [DOI] [PubMed] [Google Scholar]
- 11.Soto E, Lee H, Saladi RN, Gerson Y, Manginani S, Lam K, Persaud AN, Wong R, Alexandrescu DT, Fox JL. Behavioral factors of patients before and after diagnosis with melanoma: a cohort study–are sun-protection measures being implemented? Melanoma Res. 2010; 20:147–52. [DOI] [PubMed] [Google Scholar]
- 12.Idorn LW, Datta P, Heydenreich J, Philipsen PA, Wulf HC. Sun behaviour after cutaneous malignant melanoma: a study based on ultraviolet radiation measurements and sun diary data. Br J Dermatol. 2013;168(2):367–73. [DOI] [PubMed] [Google Scholar]
- 13.Idorn LW, Datta P, Heydenreich J, Philipsen PA, Wulf HC. A 3-year follow-up of sun behavior in patients with cutaneous malignant melanoma. JAMA Dermatol. 2014;150:163–8 [DOI] [PubMed] [Google Scholar]
- 14.Nahar VK, Allison Lord M, Brodell RT, et al. Skin cancer prevention practices among malignant melanoma survivors: a systematic review. J Cancer Res Clin Oncol. 2016;142: 1273–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vogel RI, Strayer LG, Engelman L, Nelson HH, Blaes AH, Anderson KE, Lazovitch D. Sun Exposure and Protection Behaviors among Long-term Melanoma Survivors and Population Controls. Cancer Epidemiol Biomarkers Prev. 2017April;26(4):607–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore SC, Lee IM, Weiderpass E, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Int Med. 2016; 176(6): 8160825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coups EJ, Ostroff JA. A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Prev Med. 2005;40;702–711. [DOI] [PubMed] [Google Scholar]
- 18.Heo SY, Kim J, Gutruf P, Banks A, Wei P, Pielak R, Balooch G, Araki H, Rollo D, Gaede C, Patel M, Yun y, Robinson JK, Xu S, Rogers JA. Wireless, battery-free, miniaturized dosimeters for monitoring exposure to solar radiation. Sci Transl Med. 2018December5;10(470). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thieden E, Philipsen PA, Sandby-Moller J, Wulf HC. Sunscreen use related to UV exposure, age, sex, and occupation based on personal dosimeter readings and sun-exposure behavior diaries. Arch Dermatol 2005;141(8):967–73. [DOI] [PubMed] [Google Scholar]
- 20.Green LW, Kreuter MW. Health Program Planning: An Educational and Ecological Approach. 4th ed. McGraw-Hill; 2005. [Google Scholar]
- 21.Diffey B Sun Protection: a Risk Management, Bristol, IOP Publishing Lts, UK, 2017. [Google Scholar]
- 22.Kollias N, Ruvolor E, Sayre RM. The value of the ratio of UVA to UVB in sunlight. Photochem and Photobio 2011; 87:1474–5. [DOI] [PubMed] [Google Scholar]
- 23.Parisi AV, Kimlin MG, Wong JC, Wilson M. Personal exposure distribution of solar erythemal ultraviolet radiation in tree shade over summer. Phys Med Biol. 2000February; 45(2):349–56. [DOI] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N , Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robinson JK, Guevara Y, Gaber R, Clayman ML, Kwasny MJ, Friedewald JJ, Gordon EJ. Efficacy of a sun protection workbook for kidney transplant recipients: a randomized controlled trial of a culturally sensitive educational intervention. Am J Transpl 2014;14:2821–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robinson JK, Friedewald JJ, Desai A, Gordon EJ. A randomized controlled trial of a mobile medical app for kidney transplant recipients: effect on use of sun protection. Transplant Direct 2016Jan;2(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nursing. 2008;62(1):107–115. [DOI] [PubMed] [Google Scholar]
- 28.Hsieh H-F, Shannon SE. Three Approaches to Qualitative Content Analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 29.Charmaz K Constructing grounded theory: a practical guide through qualitative analysis. London; Thousand Oaks, Calif.: Sage Publications; 2006. [Google Scholar]
- 30.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- 31.Robinson JK, Durst DA, Gray E, Kwasny M. Protection-adjusted UV dose estimated for body areas: daily self-reported sun protection modification of wearable UV sensor dose. Photoderm Photoimm & Photomed. 2020;00:1–8 [DOI] [PubMed] [Google Scholar]
- 32.Sache MM, Böttcher S, Pape L, Wagner G, Mehls O, Klaus G, et al. Face-to-face sun protection training and text messages improve sun protection behavior in adolescent organ transplant recipients: HIPPOline Feasibility study. Acta Derm Venereol 2016;96:341–345. [DOI] [PubMed] [Google Scholar]
- 33.US Department of Health and Human Services. Healthy People 2020 topics & objectives: cancer.http://www.healthypeople.gov/2020/topics-objectives/topic/cancer.Published 2015. Accessed May 3, 2020.
- 34.Cheuk M, Xu D, McLean R. Delivery of personal ultraviolet radiation information to smartphones. NIWA UV Workshop, Auckland, NZ April2014. www.niwa.co.nz/atmosphere/uv-ozone/uv-science-workshops/2014-uv-workshop.Accessed May 3, 2020. [Google Scholar]
- 35.Khan AQ, Travers JB, Kemp MG. Roles of UVA radiation and DNA damage responses in melanoma pathogenesis. Environ Mol Mutagen. 2018;59(5):438–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kamenisch Y, Baban TSA, Schuller W, et al. UVA-Irradiation Induces Melanoma [DOI] [PubMed] [Google Scholar]
- 37.Young AR. Does UVA exposure cause human malingnant melanoma? In Protections of the Skin against Ultraviolet Radiations,ed. Rougier A and Schaefer H, John Libbey Eurotext, Paris, 1998, pp. 25–28. [Google Scholar]
- 38.Miller SA, Hamilton SL, Wester UG, Cyr WH. An analysis of UVA emissions from sunlamps and the potential importance for melanoma. Photochem Photobiol. 1998;68:63–70. [PubMed] [Google Scholar]; Invasion via the Enhanced Warburg Effect. J Invest Dermatol. 2016;136 (9):1866–1875. [DOI] [PubMed] [Google Scholar]
- 39.Coelho SG, Hearing VJ. UVA tanning is involved in the increased incidence of skin cancers in fair-skinned young women. Pigment Cell Melanoma Res. 2010;23:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Noonan FP, Zaidi MR, Wolnicka-Glubisz A, et al. Melanoma induction by ultraviolet A but not ultraviolet B radiation requires melanin pigment. Nat Commun. 2012;3:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hodis E, Watson I, Kryukov G, et al. A landscape of driver mutations in melanoma. Cell. 2012;150:251–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tewari A, Grage MM, Harrison GI, Sarkany R, Young AR. UVA1 is skin deep: molecular and clinical implications. Photochem Photobiol Sci. 2013;12:95–103. [DOI] [PubMed] [Google Scholar]
- 43.Deci EL, Ryan RM. The ‘what’ and ‘why’ of goal pursuits: human needs and the self-determination of behavior. Psycholog Inquiry 2000; 11, 227–268. [Google Scholar]
- 44.Stump TK, Spring B, Marchese SH, Alshurafa N, Robinson JK. Toward a precision behavioral medicine approach to addressing high-risk sun exposure: a qualitative analysis. JAMIA Open. 2019September16:2(4):547–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mujumdar UJ, Hay JL, Monroe-Hinds YC, Hummer AJ, Begg CB, Wilcox HB, Oliveria SA, Berwick M. Sun protection and skin self-examination in melanoma survivors. Psychooncology. 2009; 18:1106–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bowen D, Jabson J, Haddock N, Hay J, Edwards K. Skin care behaviors among melanoma survivors. Psycho-Oncology. 2012; 21:1285–1291. [DOI] [PubMed] [Google Scholar]


