Abstract
Introduction
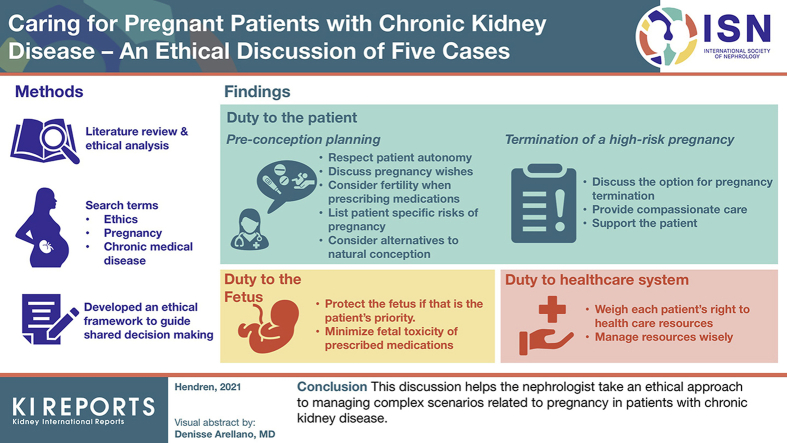
Pregnancy planning in patients with chronic kidney disease can result in ethical conflicts due to the potential for adverse outcomes. Traditionally, many nephrologists have advised their patients to avoid pregnancy altogether; however, this approach is paternalistic and not patient-centered. An ethical framework could guide joint decision-making between physicians and their patients, but this does not currently exist.
Methods
We performed a literature search to identify the ethical considerations associated with this patient population. We searched for articles published between 1975 and 2019 using the terms “ethics” and “high risk pregnancy,” along with 29 chronic disease-specific MeSH terms. Subsequently, we performed a critical evaluation using established ethical theories and adapted anonymized clinical cases from the Pregnancy in Kidney Disease Clinic (PreKid Clinic) at our institution to guide the discussion.
Results
We identified 968 articles and excluded 947 based on their title or abstract. Twelve full-text articles were included, representing discussions, case reports, and literature reviews on the ethics of pregnancy in 8 chronic diseases. The extracted data were applied to 5 clinical cases to guide the discussion.
Conclusions
This clinical review focuses on 3 main ethical themes: duty to patient, duty to the fetus, and duty to society, to help physicians explore common scenarios that may arise when counseling patients around pregnancy. Primarily, physicians have a duty to facilitate autonomous decision-making and informed consent. Secondarily, they have a duty to protect the fetus and use resources judiciously as long as it does not impact the care of their patients.
Keywords: bioethics, chronic kidney disease, pregnancy, women's health
Graphical abstract
Historically, the discussion of pregnancy in chronic kidney disease (CKD) has been linked with paternalism. In 1975, an article in The Lancet summarized the attitude of the time: “Children of women with chronic kidney disease used to be born dangerously or not at all. Not at all if doctors had their way.”1 The decision to pursue pregnancy is influenced by many personal and societal factors. People with CKD who wish to become pregnant are faced with an even more complex decision, as they can be at increased risk of adverse maternal and fetal outcomes, including hypertensive disorders of pregnancy, progression of renal impairment, and complications of prematurity and small-for-gestational-age infants.2, 3, 4 There is sufficient data on the risks and effects of pregnancy in CKD to warrant using it as a lens to discuss the ethics of caring for the medically complex patient who is or would like to become pregnant.
An ethical framework is a set of recommendations intended to guide clinical decision-making in the face of ethical dilemmas that may arise in the scope of clinical practice. A recent call to action to develop ethical frameworks in nephrology was released by a joint working group on ethical issues in nephrology consisting of representatives from the American Society of Nephrology and the European Renal Association.5 The priority ethical challenges suggested in that review included the development of an approach to guide shared decision-making.5 To date, no ethical framework has been published to assist the clinician in shared decision-making around pregnancy in CKDs.6 In this ethical discussion, we draw on the existing medical literature and ethical theories to delineate and analyze the ethical issues at play in 5 cases that the nephrologist may encounter when managing pregnant patients with CKD. We use this to develop an ethical framework to guide clinicians who provide care to this important patient population.
Methods
Data Sources and Searches
To develop this framework, we conducted a thorough search of the existing literature to summarize the breadth of the literature on this topic, clarify concepts, and identify themes, which were subsequently used to inform our ethical discussion. An experienced librarian worked with the authors to develop an Embase and Medline search using the keywords “ethics” and “pregnancy/high risk pregnancy” within a list of 29 diseases and their corresponding MeSH terms (see Supplementary Appendix S1). Further studies were hand-selected from the relevant articles’ reference lists during data extraction.
Study Selection
We selected articles about ethical issues that face patients diagnosed with complex, chronic medical conditions where there is potential maternal and fetal harm with a poorly timed pregnancy. We limited our search to articles published in English between June 1975 (when the aforementioned article in The Lancet was published, representing a shift in physicians’ viewpoints1) and June 2019 when the data analysis began. We excluded articles that were related to oncology and critical care (as patients with these conditions tend to either follow a curative or a palliative trajectory), mental health conditions (as we were focusing on complex medical conditions that compromise physical health), diseases limited to pregnancy (e.g., pre-eclampsia), infectious diseases, and genetic conditions (as the ethical issues tend to relate predominantly to vertical transmission from patient to child). Finally, we excluded articles where ethical questions were posed but no analysis was provided. Three independent assessors (EH, AL, MH) screened articles and analyzed those that met the inclusion criteria.
Data Extraction and Quality Assessment
EH and AL performed data charting in duplicate. Data extracted from the articles (including author, type of article, medical condition, and ethical dilemma raised) were recorded in a central database as per Arksey and O’Malley’s review framework.7 Disagreements were resolved through discussion to reach consensus. Ethical dilemmas from each article were catalogued, and the positions and ethical reasoning of the authors were analyzed.
Data Synthesis and Analysis
The final ethical framework started with a summary of the key ethical challenges and approaches identified in the literature review. Subsequently, we performed a critical evaluation of the previously identified challenges through the lens of ethical principles from biomedical ethics,8 utilitarianism,9 feminist ethics,10, 11, 12 and the deontological principle of respect for persons as outlined in Kantian ethics.13 The final framework offers recommendations for clinicians that are congruent with the philosophical literature. To guide discussion, prototypical case examples have been adapted from anonymized clinical cases from the Pregnancy in Kidney Disease Clinic (PreKid Clinic) at Sunnybrook Health Sciences Centre in Toronto, Ontario, Canada, with approval of the research ethics board to share such cases. Identifying information was omitted or altered.
Results
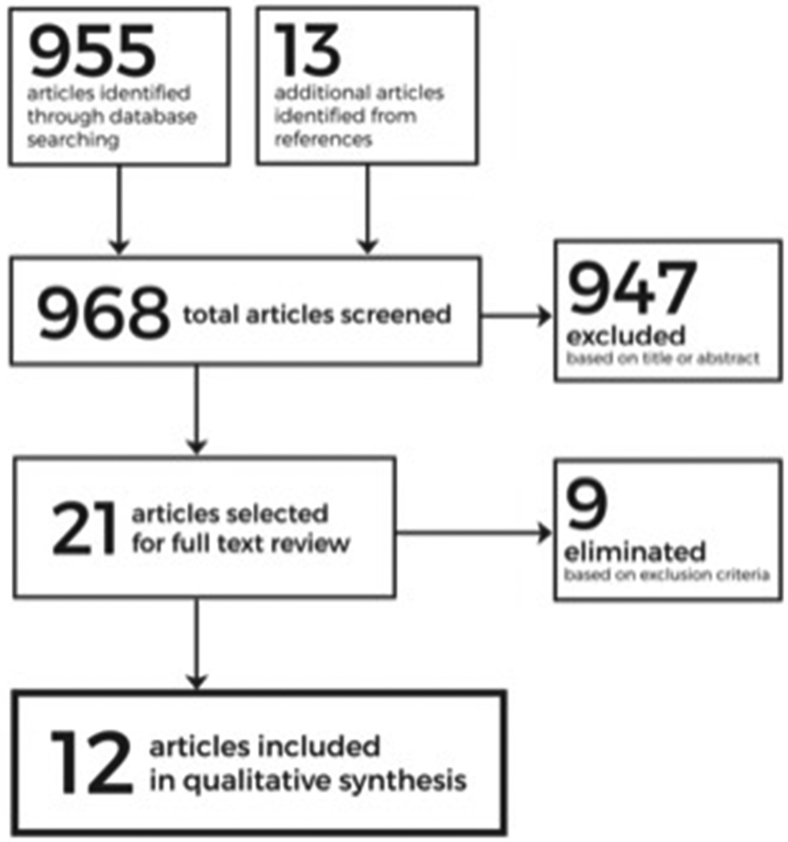
A total of 955 articles were identified in the initial search with a further 13 articles identified in the references of these articles, for a total of 968 articles screened. Of the 955 articles, 947 were excluded based on their title or abstract (Figure 1). The remaining 21 articles were selected for full-text review and a further 9 were eliminated based on the exclusion criteria. Consequently, 12 articles were included in final review (6 general discussion, 6 case report and discussion) and are summarized in Supplementary Table S1. The diseases discussed included: CKD (4 articles); multiple sclerosis (2 articles); and 1 article on each of diabetes, cystic fibrosis, congenital heart disease, solid-organ transplant, Marfan syndrome, and epilepsy. Three ethical themes were identified from our literature review: physician duty to the patient; duty to the fetus; and duty to the health-care system. They are described in detail in what follows and summarized in Table 1.
Figure 1.
Selection process for articles included in literature review.
Table 1.
Ethical framework for pregnancy in chronic kidney disease
Physician duty to the patient:
|
Physician duty to the fetus:
|
Physician duty to the health-care system:
|
Physician Duty to the Patient
Preconception planning
Clinical case: A 36-year-old patient with CKD due to hereditary nephritis has a strong desire to have children, but she admits her disease is poorly controlled due to difficulty attending follow-up appointments, poor medication adherence, and multiple psychosocial stressors. She has been told by another nephrologist that pregnancy is dangerous in patients with kidney disease and instructs her to avoid becoming pregnant, but no individualized risk assessment is provided. She comes to you for a second opinion.
Several ethical challenges arise in preconception counseling for patients who are living with chronic or end-stage kidney disease. The physician whose priority is aggressive care for a serious renal threat may not elicit the patient’s reproductive desires, and so, may not align their proposed treatments with their patient’s values and wishes. In caring for patients for whom pregnancy would be very likely to result in poor clinical outcomes, the physician may be inclined to dissuade their patients from becoming pregnant, but this approach does not respect patient autonomy, is overly paternalistic, and may harm the physician/patient therapeutic alliance, especially if the patient “disobeys” their doctor.
Patient autonomy and informed consent are fundamental considerations for preconception planning and will ultimately guide a shared decision-making process. Drawing on Beauchamp and Childress’s principles of biomedical ethics8 and supported by our literature review, several authors (Morgan-Followell et al.,14 Davison,15 and Nelson16) argued that the physician has an obligation to respect the patient’s autonomy to make their own decisions regarding their reproductive potential. Discussing a patient’s wishes for pregnancy also gives the opportunity to opt for disease-modifying medications or interventions that do not impact fertility or refer for fertility preservation therapy before initiating treatment that may impact fertility (i.e., choosing mycophenolate mofetil instead of cyclophosphamide to treat lupus nephritis). For example, for a woman on dialysis, this could include intensification of her dialysis regimen or switching from peritoneal dialysis to intensive in-center or nocturnal hemodialysis.6
There may be instances in which physicians judge that the risk of becoming pregnant far outweighs the benefit of pregnancy. For example, active nephritis poses a risk of maternal morbidity and mortality, progression to end-stage renal disease, and fetal morbidity.17 However, although the physician can (and indeed, should) recommend against becoming pregnant when there is an inordinate risk to the patient, forbidding a woman to become pregnant constitutes a breach of her right to make autonomous decisions.16
Not all patients of childbearing age wish to pursue pregnancy and parenthood. Anticipatory motherhood, the assumption that every woman will or should want to become a mother, fails to recognize women’s prerogative to decide not to have children.18 Overall, although a physician should sensitively address the topic of pregnancy at least once while providing longitudinal care to women of reproductive age, they should not express a recommendation that the patient should have children, nor a moral predilection that the patient would be better off doing so.18
Preconception counseling also involves respecting the ethical principle of informed consent, as discussed by Davison,15 Riviello et al.,19 Bogardus et al.,20 and Piccoli et al.6 Informed consent requires individualized counseling about the patient’s risk of adverse events, including identity and probability of the risk (e.g., progression of underlying disease, potential risks to the fetus), the permanence of the risk, the timing of when it is likely to occur, and steps that can be taken to minimize this risk.21 As noted by Piccoli et al., the nephrologist is uniquely suited to provide information regarding the risks of pregnancy and ways to mitigate the risks in the face of chronic and end-stage kidney disease (ESRD).6 Because the potential for risk reduction with appropriate planning is so great, we support the recommendation that nephrologists should engage all patients of childbearing potential in shared decision-making around contraception and pregnancy.15,22 The physician should also discuss alternatives to natural conception, including assisted reproductive technologies, fertility preservation, adoption, and surrogacy.15,21 While counseling, the physician must provide advice based only on knowledge and experience, and should not raise fears of becoming pregnant based on personal prejudices.16
It is worthwhile noting some conflicting views have been published in the area of informed consent. For example, Wexler et al. mentioned that a physician should discuss the burden and responsibilities of motherhood along with the reduced lifespan of the mother when counseling patients with chronic lung disease about pregnancy.21 However, perseverating on the risk of pregnancy, discussing risk outside of the parameters of maternal or fetal health, or implying that the woman is making a “bad choice” will compromise the woman’s right to make a decision free of coercion and contravenes biomedical and feminist ethical principles.12,16 This approach may hurt the doctor/patient relationship, which could have been harnessed to improve preconception planning and harm reduction. Regardless of the decision, physicians must continue to provide excellent care to patients who do not follow their recommendations.15
Termination of a high-risk pregnancy
Clinical case: A 25-year-old woman diagnosed with lupus nephritis is treated with prednisone and mycophenolate mofetil (MMF). She is told by her nephrologist that she is at risk of renal failure if she discontinues her MMF and that pregnancy is contraindicated. However, she self-discontinues the medication and proceeds with pregnancy. Her pregnancy is subsequently complicated by a significant flare of her lupus nephritis and loss of kidney function. At 16 weeks, termination is offered, but she refuses. She subsequently develops pre-eclampsia and her baby is born prematurely at 27 weeks.
On rare occasions, an unplanned or poorly timed pregnancy in a patient with CKD can be associated with a high risk of severe maternal and fetal morbidity, including loss of residual renal function, progression to ESRD, and severe prematurity with high risk of neonatal complications and need for neonatal intensive care monitoring.3 In some pregnancies, the physician may come to realize that continuing the pregnancy may pose an unreasonable amount of risk to the patient’s health or that the pregnancy is unlikely to result in a good outcome.21 For example, in some low-income countries where public funding for dialysis is limited, a pregnancy that results in renal failure may mean death for the patient.23 Therefore, the physicians involved in the patient’s care (including nephrologists, neonatologists, and obstetricians) must decide whether they should recommend or mention the possibility of termination of the pregnancy and, if so, how they will communicate this to their patient, the ultimate arbiter of the decision.
There are cultural, religious, and legal factors that may make some physicians hesitant to recommend termination.24 If therapeutic abortion is legal in the jurisdiction in which the physician is practicing, they are obligated to indicate that it is an option to avoid a poor outcome for the patient or the potential child.15 To fail to describe the risk of continuing the pregnancy or to fail to indicate that termination is one option to mitigate the risk (as proposed by Baggot et al.) would be to contravene the physician’s obligation to uphold the principle of non-maleficence, as the patient would be put at risk without recourse to potentially avoid this risk.18,24
From a patient perspective, the value placed on parenthood may be so high that it outweighs the value placed on their own personal health.25 As in pre-pregnancy counseling, a physician must not recommend terminating a pregnancy too vociferously, so as to prevent the patient from choosing autonomously.26 In the end, regardless of whether the patient’s choice is congruent with their recommendation, the physician has an ethical duty to provide compassionate care and support the patient.8 If resources allow, a high-risk pregnancy should be supported by close surveillance from a multidisciplinary team to minimize risk to the mother.26
Physician Duty to the Fetus
Balancing risk to the patient with risk to the fetus
Clinical case: A 30-year-old woman with a kidney transplant and previous severe allograft rejection episode is on MMF, tacrolimus, prednisone, and trimethoprim‒sulfamethoxazole. Despite being advised to avoid pregnancy while on these medications, she becomes pregnant. Even though she is aware of the risk to her fetus, she refuses to modify her medications, as she does not want to risk transplant rejection.
Because the health of the mother and the fetus are linked, the physician’s responsibility to respect the autonomy of the patient can occasionally come into conflict with the duty to non-maleficence toward the fetus.14 A pregnant patient may opt for an effective medication that is not safe during pregnancy and, in doing so, prioritize their own health over that of the fetus, such as in the case report that Dresner et al. described of a young woman with congenital heart disease taking digoxin.27 However, the right to personal autonomy determines that the physician only has a duty to protect the fetus if prioritized by the patient.16,22 The patient does have a moral duty to protect their fetus if possible, but they cannot be compelled to do so.15,28 This may make the prescribing physician uncomfortable, as they are implicated in the potential harm to the fetus. Faced with the decision whether or not to continue prescribing a medication that may be teratogenic, the physician may prefer to prescribe a safer, but less effective option instead. In transplantation, for example, the physician will typically prescribe azathioprine instead of MMF.
For each clinical decision, a physician has a responsibility to ensure the patient has provided informed consent, following the same principles as in preconception counseling. However, the ultimate choice depends on the patient’s values and whether they would opt for a potentially inferior medication for their own health in order to protect the fetus.28 In cases where there is a conflict between the autonomy of the patient and the recommendation of the physician, Riviello et al. and Farrell-Carnahan et al. proposed the technique of motivational interviewing, which, by reducing the impact of the power differential in the relationship, has been helpful for counseling pregnant patients with substance use disorder.19,29
Pregnancy in the face of a shortened lifespan
Clinical case: A 32-year-old woman with ESRD on nocturnal hemodialysis wishes to have a family. She is highly sensitized from a prior kidney transplant (calculated panel-reactive antibodies 100%), and therefore, has a low likelihood of retransplantation. After adequate counseling and optimization, she becomes pregnant while under your care and with your support. She has 2 uncomplicated pregnancies while on hemodialysis However, 6 years later, she dies due to a complication from her underlying chronic diseases. You are left to wonder if you have contributed to a negative outcome, leaving her children without a mother.
Several authors (including Wexler et al., Davison, and Ross) acknowledge that some physicians believe that women with a chronic medical illness should not have children due to the mother’s shortened expected lifespan.15,21,28 Does a physician facilitate a negative outcome for the fetus simply by aiding such a pregnancy that could lead to an eventually motherless child? The folly in this perspective is highlighted by the fact that, although this argument has been made for women with chronic illness, the literature is silent on recommending against pursuing fatherhood for men with a limited lifespan.15 Indeed, Held has argued that motherhood is defined not by a contract or a decision to become pregnant, but by a linked relationship between person and child.11 It is not just the mother who can fulfill the duty of parenthood for the child; rather, children are born to families and communities of support. Furthermore, Kant’s deontological respect for persons counsels against inadvertently considering persons as a means to an end, and considering a woman as primarily a mother to her children rather than as an autonomous decision-making individual contravenes our duty to respect her full personhood.13
We argue that no child is guaranteed to have a parent healthy enough to raise them into adulthood, and it would certainly not be justifiable to posit that a child who loses a parent would be better off not ever having been born. This accounts for the right of older women to pursue treatment for infertility and, by extension, given the mortality of all people, the right of all people to pursue their reproductive potential (as protected by the United Nations Declaration on Social Progress and Development).30,31 We contend that physicians should engage each of their patients in advanced care planning, which includes discussing the patient’s values and preferences in the event of a catastrophic illness, but it may also include the consideration of appointing a substitute decision-maker or an alternative guardian for one’s children depending on the patient’s circumstances.32
Physician Duty to the Health-care System
Clinical case: A 40-year-old woman with a failing renal allograft becomes pregnant and develops progressive allograft dysfunction over the course of pregnancy. She delivers a full-term infant, but thereafter she develops allograft failure and requires hemodialysis by 6 weeks postpartum. She comes to you 12 months later asking if she is can be listed for a repeat transplant.
In caring for pregnant patients, the physician’s duty to their patient may come into conflict with their duty to the health-care system as a steward of its resources. The ethical allocation of limited resources like kidney transplantation and access to assisted reproductive technology (ART) is governed by the principle of justice and the responsibility to ensure fair access to resources.8,28 The ethical dilemmas raised in this section weigh each patient’s right to health-care resources with the physician’s responsibility to other patients in society to wisely manage these resources.
Davison and Ross have both written about the ethical issues of patient autonomy and resource allocation in the context of kidney transplantation and allograft failure.15,28 Furthermore, this topic is discussed in the guidelines of the kidney transplant and pregnancy working group of the Italian Society of Nephrology.33 Pregnancy in kidney transplant patients is complicated by the ethical imperative to justly distribute society’s limited resources in this regard. For example, should a woman who pursues a higher risk pregnancy with a failing allograft be given a lower priority (or excluded altogether) from receiving another transplant? Both Ross and Davison make the argument that, because the relationship between pregnancy and allograft function is complex, pregnancy is rarely the sole reason that a patient requires a second renal transplant and should therefore not be disqualifying for further transplantation. In addition, from a utilitarian perspective for that patient, repeat transplantation is associated with improved quality and quantity of life compared with dialysis.34 The discussion of bioethics in the Italian guidelines suggests there may be a geographic influence on the hierarchy of ethical principles in play and that principles are shifting over time, away from more paternalistic approaches.33 In most cases, the physician’s top priority is to their own patient, and they must advocate first for their patient’s right to access health-care resources rather than prioritizing the management of those resources on a societal level.
Regarding the provision of ART, Davison explores the concept of reproductive freedom as a negative rather than a positive right---although physicians cannot prevent a person from becoming pregnant naturally, they do not necessarily have to aid them to become pregnant if it will put a burden on the health-care system.15 Patients with advanced CKD have low rates of spontaneous pregnancy and may require ART to become pregnant.35 Providing publicly funded ART is expensive, and even privately funded ART may result in an increased cost to the health-care system that must manage a complicated pregnancy. However, unless there is a compelling medical reason that pregnancy is likely to place the mother at risk, the decision to provide or deny ART should ultimately be made by a fertility specialist, and a referral should be made upon request.
Discussion
This ethical discussion summarizes many challenges that physicians face when managing pregnancy in the context of a chronic disease that may have significant impact on maternal and fetal health. Using anonymized cases from our PreKid Clinic and placing this in the context of the ethical literature, we have built a practical ethical framework to guide nephrologists toward a model of shared decision-making. When managing pregnancy in CKD, the nephrologist must consider their duty to their patient, to the fetus, and to society. Before conception, initiating discussions with all patients of childbearing potential can help elucidate individual goals, clarify expectations for the physician and patient, and avoid the presumption of anticipatory motherhood. Ideally, informed consent starts before conception, and the risks and expected outcomes should be discussed throughout the pregnancy, whenever new information becomes available. The physician can also mitigate harm to the patient and the fetus by optimizing medications while ensuring that the patient’s priorities are respected. Finally, advanced care planning should be discussed with all patients and can include contingency planning for children in the face of a potentially shortened lifespan.
The limitations of this framework include an inability to incorporate local regulations regarding the rights and abilities of pregnant patients to access termination and other resources into general clinical decision-making recommendations. In certain jurisdictions, legal precedence may infringe upon the patient’s right to bodily autonomy. In such cases, there may be conflict between the ethical and legal responsibilities of the physician. In addition, we have limited our discussion to incurable, chronic, noninfectious, nonmalignant diseases, potentially narrowing the scope of our recommendations.
Considering the principles of biomedical ethics, utilitarianism, Kantian ethics, and feminist ethics, the physician can balance their duty to provide compassionate, patient-centered care with their duty to uphold non-maleficence and consider issues of systemic justice. These issues are not limited to patients with kidney disease and can be applied to many chronic medical conditions. Overall, the patient is best served when their physician engages in a shared decision-making model, which combines the patient’s values and social context with medical considerations. Development of a strong patient/physician bond based on mutual respect, open-mindedness, and empathy over time can also be helpful in maintaining a strong therapeutic relationship that allows for ongoing medical care in the face of complex conversations and circumstances.
Disclosure
All the authors declared no competing interests.
Footnotes
MAH and AL contributed equally to the supervision of this research project.
Table S1. Articles discussing ethics of pregnancy in chronic medical conditions (excluding cancer, mental health and infectious diseases)
Appendix S1. Embase and Medline search keywords and MeSH terms
Supplementary Material
Table S1. Articles discussing ethics of pregnancy in chronic medical conditions (excluding cancer, mental health and infectious diseases)
Appendix S1. Embase and Medline search keywords and MeSH terms
References
- 1.Pregnancy and renal disease. Lancet. 1975;306:801–802. [PubMed] [Google Scholar]
- 2.Jones D.C., Hayslett J.P. Outcome of pregnancy in women with moderate or severe renal insufficiency. N Engl J Med. 1996;335:226–232. doi: 10.1056/NEJM199607253350402. [DOI] [PubMed] [Google Scholar]
- 3.Piccoli G.B., Cabiddu G., Attini R. Risk of adverse pregnancy outcomes in women with CKD. J Am Soc Nephrol. 2015;26:2011–2022. doi: 10.1681/ASN.2014050459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fitzpatrick A., Mohammadi F., Jesudason S. Managing pregnancy in chronic kidney disease: improving outcomes for mother and baby. Int J Womens Health. 2016;8:273–285. doi: 10.2147/IJWH.S76819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin D.E., Harris D.C.H., Jha V. Ethical challenges in nephrology: a call for action. Nat Rev Nephrol. 2020:1–11. doi: 10.1038/s41581-020-0295-4. [DOI] [PubMed] [Google Scholar]
- 6.Piccoli G., Attini R., Cabiddu G. Kidney diseases and pregnancy: a multidisciplinary approach for improving care by involving nephrology, obstetrics, neonatology, urology, diabetology, bioethics, and internal medicine. J Clin Med. 2018;7:135–136. doi: 10.3390/jcm7060135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Social Res Method. 2005;8:19–32. [Google Scholar]
- 8.Beauchamp T.L., Childress J.F. Oxford University Press; New York: 2013. PrincipIes of Bioethics, 7th ed. [Google Scholar]
- 9.Shaw W.H. Blackwell Publishing; Hoboken, NJ: 1999. Contemporary Ethics. [Google Scholar]
- 10.Haraway D. Situated knowlege: the science question in feminism and the privilege of partial perspective. Feminist Studies. 1988;14:575–599. [Google Scholar]
- 11.Held V. Non-contractual society: a feminist view. Can J Philosophy. 1987;17(suppl 1):111–137. [Google Scholar]
- 12.Sherwin S. Feminist and medical ethics: two different approaches to contextual ethics. Hypatia. 1989;4:57–72. doi: 10.1111/j.1527-2001.1989.tb00573.x. [DOI] [PubMed] [Google Scholar]
- 13.O'Neill O. 2nd ed. Cambridge University Press; Cambridge, UK: 2013. Acting on Principle: an Essay on Kantian Ethics. [Google Scholar]
- 14.Morgan-Followell B.N., Nicholas J.A., Weisleder P. Reproductive issues in women with multiple sclerosis: ethical considerations. Continuum (Minneap Minn) 2014;20:177–180. doi: 10.1212/01.CON.0000443845.63804.9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davison S.N. Ethical considerations regarding pregnancy in chronic kidney disease. Adv Chronic Kidney Dis. 2007;14:206–211. doi: 10.1053/j.ackd.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 16.Nelson R.F. Ethical issues in multiple sclerosis. Semin Neurol. 1997;17:227–234. doi: 10.1055/s-2008-1040933. [DOI] [PubMed] [Google Scholar]
- 17.Smyth A., Oliveira G.H.M., Lahr B.D., Bailey K.R., Norby S.M., Garovic V.D. A systematic review and meta-analysis of pregnancy outcomes in patients with systemic lupus erythematosus and lupus nephritis. Clin J Am Soc Nephrol. 2010;5:2060–2068. doi: 10.2215/CJN.00240110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waggoner M.R. Motherhood pre-conceived. J Health Polit Policy Law. 2013;38:345–371. doi: 10.1215/03616878-1966333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Riviello C., Ottanelli S., Di Tommaso M.R., Mello G. Ethical issue and consent form in the management of high-risk pregnancy. J Matern Fetal Neonatal Med. 2009;23:179–183. doi: 10.3109/14767050903165206. [DOI] [PubMed] [Google Scholar]
- 20.Bogardus S.T., Holmboe E., Jekel J.F. Perils, pitfalls, and possibilities in talking about medical risk. JAMA. 1999;281:1037–1041. doi: 10.1001/jama.281.11.1037. [DOI] [PubMed] [Google Scholar]
- 21.Wexler I.D., Johannesson M., Edenborough F.P., Sufian B.S., Kerem E. Pregnancy and chronic progressive pulmonary disease. Am J Respir Crit Care Med. 2007;175:300–305. doi: 10.1164/rccm.200605-598OE. [DOI] [PubMed] [Google Scholar]
- 22.Levy D.P., Giatras I., Jungers P. Pregnancy and end-stage renal disease---past experience and new insights. Nephrol Dial Transplant. 1998;13:3005–3007. doi: 10.1093/ndt/13.12.3005. [DOI] [PubMed] [Google Scholar]
- 23.Htay H., Alrukhaimi M., Ashuntantang G.E. Global access of patients with kidney disease to health technologies and medications: findings from the Global Kidney Health Atlas project. Kidney Int Suppl. 2018;8:64–73. doi: 10.1016/j.kisu.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baggot P.J., Baggot M.G. Patients with grave maternal disorders. Ethics Medics. 2004;29:1–2. [PubMed] [Google Scholar]
- 25.Ralph C. Pregnancy in a hemodialysis patient with an ethical/cultural challenge. CANNT J. 2000;10:35–38. [PubMed] [Google Scholar]
- 26.Piccoli G.B. Vasculitis and kidney involvement in pregnancy: evidence-based medicine and ethics bear upon clinical choices. Nephrol Dial Transplant. 2004;19:2909–2913. doi: 10.1093/ndt/gfh353. [DOI] [PubMed] [Google Scholar]
- 27.Dresner N., Raskin V., Goldman L.S. Medical psychiatric grand rounds on an obstetrics---gynecology service: refusing to terminate a life-threatening pregnancy. Gen Hosp Psychiatry. 1990;12:335–340. doi: 10.1016/0163-8343(90)90053-f. [DOI] [PubMed] [Google Scholar]
- 28.Ross L.F. Ethical considerations related to pregnancy in transplant recipients. N Engl J Med. 2006;354:1313–1316. doi: 10.1056/NEJMsb041648. [DOI] [PubMed] [Google Scholar]
- 29.Farrell-Carnahan L., Hettema J., Jackson J., Kamalanathan S., Ritterband L.M., Ingersoll K.S. Feasibility and promise of a remote-delivered preconception motivational interviewing intervention to reduce risk for alcohol-exposed pregnancy. Telemed e-Health. 2013;19:597–604. doi: 10.1089/tmj.2012.0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hope T., Lockwood G., Lockwood M., Bewley S., Jackson J., Craft I. Should older women be offered in vitro fertilisation? BMJ. 1995;310:1455–1458. doi: 10.1136/bmj.310.6992.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.UN General Assembly, Declaration on Social Progress and Development, 11 December 1969, A/RES/2542(XXIV) https://www.refworld.org/docid/528c97704.html Available at:
- 32.Lefkowitz A., Henry B., Bottoms J., Myers J., Naimark D.M.J. Comparison of goals of care between hemodialysis patients and their health care providers. Can J Kidney Health Dis. 2016;3 doi: 10.1177/2054358116678207. 205435811667820-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cabiddu G. A best-practice position statement on pregnancy after kidney transplantation: focusing on the unsolved questions. The Kidney and Pregnancy Study Group of the Italian Society of Nephrology. J Nephrol. 2018;31:665–681. doi: 10.1007/s40620-018-0499-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clark S., Kadatz M., Gill J., Gill J.S. Access to kidney transplantation after a failed first kidney transplant and associations with patient and allograft survival: an analysis of national data to inform allocation policy. Clin J Am Soc Nephrol. 2019;14:1228–1237. doi: 10.2215/CJN.01530219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Webster P., Lightstone L., McKay D.B., Josephson M.A. Pregnancy in chronic kidney disease and kidney transplantation. Kidney Int. 2017:1–10. doi: 10.1016/j.kint.2016.10.045. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.