Approximately 20 million of the 333 million persons living in the United States are adolescent females.1 However, studies examining the reproductive care provided to adolescent females with kidney disease are scarce. Adolescents with chronic kidney disease (CKD) are at a critical transition phase, and many issues arising during adolescence can directly or indirectly affect renal and reproductive outcomes,2,3 including the effect of hormonal contraception on kidney physiology, a higher frequency of menstrual irregularities in patients with CKD, the potential for teratogenicity from kidney disease medications, and the need for preconception counseling about the risks of pregnancy.
Despite these needs, confidence levels related to women’s health topics among nephrologists with patients with CKD appear to be low. In a recent study, >65% of surveyed nephrologists treating adult women with CKD lacked confidence managing women’s health issues including menopause and pregnancy. Interestingly, 89% felt that opportunities for improving competency in these areas were needed.4
However, no similar study has been conducted among nephrologists managing adolescent females with CKD. Therefore, we sought to describe current practices among nephrologists in managing women’s health issues in adolescents with CKD, including confidence levels in providing this type of care.
Results
Provider Demographics and Practice Characteristics
We circulated 305 surveys and received 86 responses. Eleven incomplete responses were excluded, resulting in 75 complete responses available for analysis (Table 1). The most common age group of the providers was 41 to 50 years, and 65% of providers were women. Ninety-eight percent were practicing in the United States, and 88% practiced solely in an academic/university setting. Ninety-three percent reported spending at least 25% of their time in clinical care. Pediatric nephrologists comprised 94.9% of the providers, with the remaining 5% being adult nephrologists. Most (75%) reported that adolescents comprised >25% of their patient population, and 24% reported that they comprised >75% of their practice (Table 1).
Table 1.
Characteristics of survey respondents (N = 75)
| Demographic characteristics | Percentage of providers | |
|---|---|---|
| Sex | Male | 32 |
| Female | 65.3 | |
| Prefer not to answer | 2.7 | |
| Age (yr) | 30–40 | 30.6 |
| 41–50 | 36 | |
| 51–60 | 16.3 | |
| >60 | 10.6 | |
| Prefer not to answer | 6.5 | |
| Current location of practice | United States of America | 98.7 |
| Puerto Rico | 1.3 | |
| Current practice setting | Academic/university | 88 |
| Hybrid | 8 | |
| Other | 4 | |
| Scope of practice | Pediatric nephrology | 94.9 |
| Adult nephrology | 5.1 | |
| Percentage time dedicated to clinical care | 0%–24% | 6.7 |
| 25%–49% | 16.0 | |
| 50%–74% | 36.0 | |
| 75%–100% | 41.3 | |
| Percentage of patient population that is adolescent | 0%–24% | 12 |
| 25%–49% | 64 | |
| 50%–75% | 24 | |
| 75%–100% | 0 | |
| Received formal training in either of these areas? | Obstetric nephrology | 1.3 |
| Women’s health | 0 | |
| Neither | 98.7 | |
Nephrologists’ Formal Training in Women’s Health and Obstetric Nephrology
Only 1 provider received formal training in obstetric nephrology (with a focus on renal function during pregnancy) during their nephrology training (Table 1). When asked who cared for their adolescent patients if they became pregnant, 65% referred them to adult nephrologists. None of the providers reported training specific to women’s health.
Documentation of Menstrual Cycle, Sexual History, and Pregnancy
We noted that 16.6% of providers never/rarely documented age at menarche, and 34.7% never/rarely documented the date of the patient’s last menstrual period. An alarming 29.5% of providers never/rarely documented patient sexual activity, 74.7% never/rarely documented the number of sexual partners, and 38.1% never/rarely documented sexually transmitted infection history (Table 2). Furthermore, 33.8% never/rarely documented pregnancy history, and 45.8% never/rarely documented history of pregnancy loss/termination (Table 2).
Table 2.
Frequency of documentation (% of providers) in patient charts about sexual and menstrual health and fertility desire/risks
| How often do you document each of the following items for your adolescent patients? | Never | Rarely | Sometimes | Often | Always |
|---|---|---|---|---|---|
| Age at menarche | 4.2 | 12.5 | 33.3 | 37.5 | 12.5 |
| Pregnancy history | 9.6 | 24.2 | 14.5 | 14.5 | 37 |
| History of pregnancy termination/loss | 18.6 | 27.2 | 15.2 | 13.6 | 25.4 |
| Date of last menstrual period | 11.3 | 24.0 | 32.4 | 19.8 | 12.7 |
| Prior contraceptive use | 7.1 | 14.3 | 47.1 | 24.3 | 5.7 |
| Prior sexual activity | 7.0 | 22.5 | 43.7 | 21.1 | 5.6 |
| Sexual partner preference | 19.7 | 38 | 29.6 | 9.9 | 2.8 |
| Number of sexual partners | 26.8 | 47.9 | 18.3 | 2.8 | 4.2 |
| History of sexually transmitted infections | 9.9 | 28.2 | 36.6 | 17.0 | 8.5 |
Discussion of Teratogenicity and Fertility Impacts of Commonly Prescribed Renal Drugs
More than 92% of providers reported always/often discussing the teratogenic potential of certain medications used for the treatment of CKD (angiotensin II receptor blockers, angiotensin-converting enzyme inhibitors, and/or mycophenolate mofetil). However, 36.9% of providers never/rarely documented a negative pregnancy test before prescribing these medications (Table 3). Most (92.6%) of the providers discussed infertility risks with their patients before prescribing cyclophosphamide, and most discussed fertility-preserving options. However, only 41.3% always/often talked with patients about their desires for future pregnancy (Table 3).
Table 3.
Frequency of discussion and/or documentation of fertility-preserving options and fetotoxicity of commonly prescribed renal drugs (% of providers)
| How often do you document each of the following items for your adolescent patients? | Never | Rarely | Sometimes | Often | Always |
|---|---|---|---|---|---|
| Documentation of a discussion on the risk of fetotoxicity with ACEis/ARBs or mycophenolate use | 0.0 | 0.0 | 6.9 | 16.7 | 76.3 |
| Document a negative pregnancy test before starting a fetotoxic medication | 9.9 | 27.0 | 16.9 | 18.3 | 28.2 |
| Discuss the risk of infertility with cyclophosphamide | 0 | 0 | 1.5 | 5.9 | 92.6 |
| Discuss the fertility-preserving options (hormonal ovarian suppression and oocyte cryopreservation) with exposure to cyclophosphamide | 4.5 | 7.6 | 13.6 | 28.8 | 45.5 |
| Discussion on patient’s desire for future pregnancy | 1.4 | 20.0 | 37.1 | 27.1 | 14.2 |
ACEis, angiotensin-converting enzyme inhibitors; ARBs, angiotensin II receptor blockers.
Confidence in Discussing Women’s Health Topics
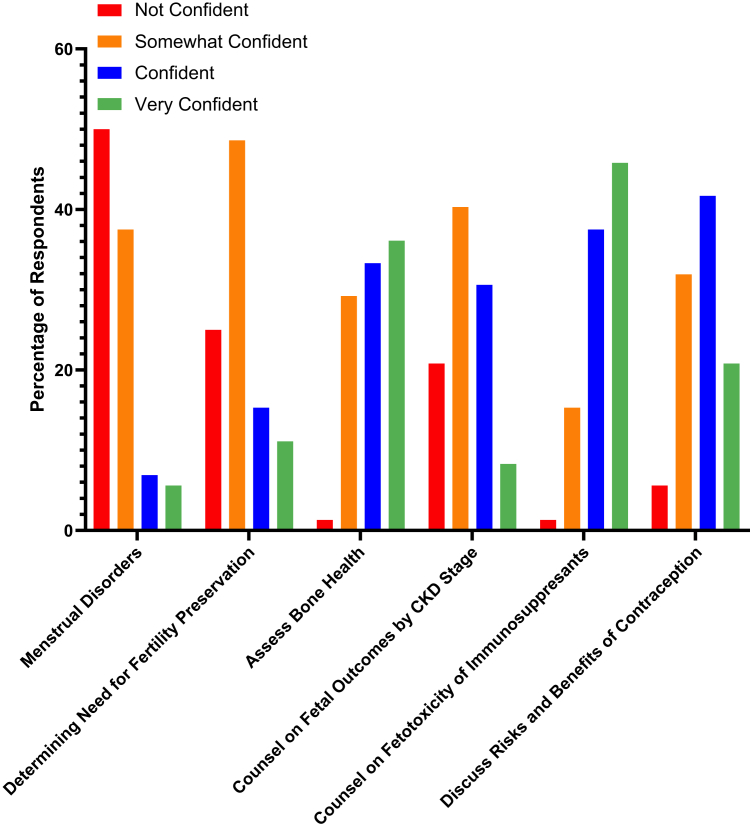
A majority of providers were not at all confident/somewhat confident in managing menstrual disorders (87.5%). Only 26.4% were very confident/confident discussing fertility preservation. Only 38.9% were very confident/confident discussing fetal outcomes with pregnancy in CKD. However, 83.3% were very confident/confident discussing the fetotoxicity of immunosuppressants (Figure 1).
Figure 1.
Confidence level of providers on the ability to discuss contraceptive measures, menstrual disorders, fetotoxicity/fetal outcomes, and fertility preservation with adolescents. We noted that a majority of providers were not confident or only somewhat confident on discussing menstrual disorders (87.5%), fertility preservation (73.6%), and fetal outcomes (59.7%) in adolescents with chronic kidney disease (CKD). However, 83.3% of providers were confident or very confident discussing the fetotoxicity of immunosuppressants used for the treatment of CKD and risks/benefits of contraceptives (62.5%).
Confidence in Discussing Contraceptives With Adolescents
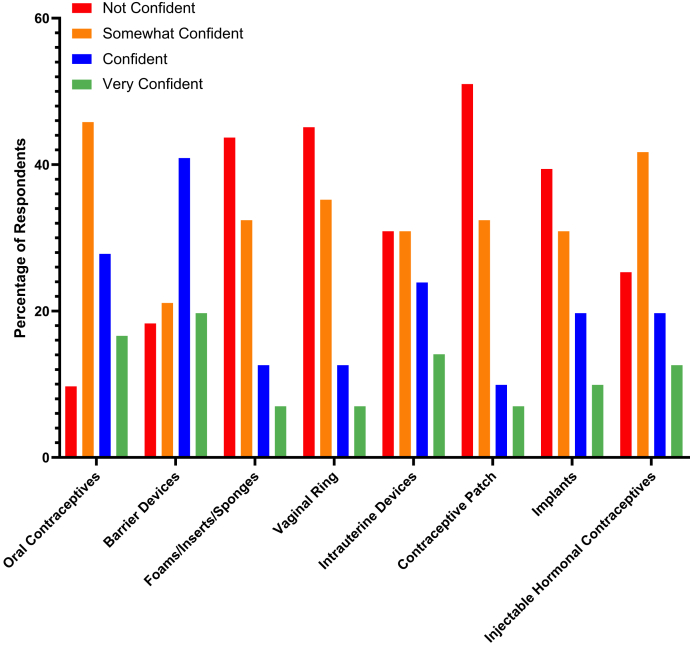
Overall, 62.5% of providers were very confident/confident discussing the risks and benefits of contraceptives. However, only 44.4% were confident in discussing oral contraceptives, whereas 60.6% were comfortable discussing barrier methods (60.6%). Furthermore, 30.9% of providers were uncomfortable with discussing long-acting reversible contraceptives, including intrauterine devices, implants, and injectables (Figure 2).
Figure 2.
The confidence level of providers on discussing different types of contraceptives. Although we noted that most providers were confident with discussing the risks and benefits of contraceptives, we found that a majority of providers were not confident or only somewhat confident (55.6%) in discussing oral contraceptives and intrauterine devices (60.8%). However, most were confident or very confident counseling patients about barrier methods (60.6%).
Discussion
This survey provides insights into the confidence levels of nephrologists in managing women’s health issues in adolescent female patients with CKD. Although most providers cared for female adolescents, an overwhelming majority denied having received any formal training in topics pertaining to women’s health. Together, our findings support those from prior studies among adult patients showing low physician confidence and insufficient training on topics concerning women’s health5, 6, 7, 8, 9,S1,S2 and highlight the need for enhanced training for nephrologists regarding women’s health issues.
We observed that within the last year, all providers had counseled adolescents of childbearing age with CKD about contraception, although only 10% were prescribing contraceptives. Furthermore, many providers lacked confidence in discussing individual contraceptive options with adolescents. One US study found that 50% of pediatricians advised abstinence as the primary form of birth control in their adolescent patients.S3–S5 Another study found that only two-thirds of adolescent girls received contraceptive education in schools, indicating an educational void that could be filled by physicians.S4,S6,S21 In other studies, physicians reported receiving most of their information on contraception from colleagues and conferences (56%), medical journals (40%), and websites (33%), rather than through formal training. Moreover, those that lacked knowledge about different forms of contraception were less likely to prescribe them to adolescents.S4,S6
We also noted that an average of 31.9% of providers were not comfortable talking with adolescents about long-acting reversible contraceptives. However, the American Academy of Pediatrics and the American College of Obstetrics and Gynecology both recommend long-acting reversible contraceptives as first-line contraception for adolescent females because these have been deemed safe for their use for pregnancy prevention and dysmenorrhea.S7,S8 Targeted education for nephrologists about the benefits and practicalities of long-acting reversible contraceptives might help to address this knowledge gap, thus minimizing the risk for unplanned pregnancy while avoiding potential side effects from estrogen-based oral contraceptives.9,S9–S13
We found that nephrology providers also infrequently documented the details of adolescent menstrual cycles. This agrees with prior studies, which showed that there are inconsistencies in menstrual cycle documentation in pediatric clinics across the United States.S14–S16 Because the American Academy of Pediatrics classifies the menstrual cycle as a vital sign,S14 documentation of the last menstrual period in adolescents should be a standard clinical practice and should be included in all templates developed for electronic medical records. Documentation of the menstrual cycle can provide knowledge of overall health and can also allow physicians to introduce contraceptives. Irregular menstrual cycles affect approximately 25% of adolescent females and can impact quality of life and, therefore, can be addressed by physicians by prescribing contraceptives for menstrual irregularity.S17,S18 Discussing contraceptive use is especially important in nephrology clinics because pregnancy in patients with CKD can be risky and requires close observation throughout the pregnancy.S19,S20 It is important for nephrologists not to assume that another provider has addressed menstrual issues in their CKD.
Knowledge of patients’ goals in relation to pregnancy and fertility is an integral part of discussions with adolescent CKD patients, especially given their impending transition to adulthood. We observed that 92.6% of providers discussed potential infertility with the use of cyclophosphamide,76% discussed fetotoxicity of angiotensin II receptor blockers and angiotensin-converting enzyme inhibitors, and 50% were confident discussing fertility preservation in patients with CKD. However, pregnancy history and desires for future pregnancy were infrequently documented, which is worrying because multiple studies have identified prepregnancy planning as a key to optimizing maternal and fetal outcomes.4,S19,S20 These findings are similar to a survey of adult nephrologists in which only half of the providers documented pregnancy history.4 Given that the vast majority of nephrologists surveyed in our study transferred the care of their adolescent CKD patients to an adult nephrologist once they became pregnant, we wonder whether this lack of clinical exposure (in addition to the lack of formal training) compounds the poor confidence of nephrologists in counseling adolescents with CKD about pregnancy risks. This observation is concerning because the transition of care in such pregnant patients is often very abrupt at a time when they are dealing with the significant stress of an adolescent pregnancy.
Conclusions
In summary, nephrologists who care for female adolescent patients are very well positioned to address these patients’ emerging fertility and reproductive needs and/or problems. However, we identified key elements of adolescents’ menstrual, sexual, and reproductive histories that were only infrequently documented by nephrologists and that the providers lack confidence prescribing contraception, counseling about pregnancy risks, and managing pregnancy in adolescent patients with CKD. More formal training in women’s health and obstetric nephrology during fellowships and greater clinical exposure to pregnant adolescents and women would likely improve provider competence and confidence in the future, thus enabling nephrologists to better care for female adolescents with CKD and to more safely transition them into adulthood.
Disclosures
SA consults with Aurinia Pharmaceuticals outside the submitted work. All other authors declared no competing interests.
Acknowledgments
The authors would like to thank The Laura W. Bush Institute for Women’s Health for supporting publication fees for this study.
Footnotes
Supplementary Methods.
Supplementary References.
Supplementary Study Limitations.
Supplementary Material
Supplementary Methods.
Supplementary References.
Supplementary Study Limitations.
References
- 1.Projected 5-year age groups and sex composition: Main projections series for the United States, 2017-2060. US Census Bureau; Washington, DC: 2017. [Google Scholar]
- 2.Gerson A.C., Riley A., Fivush B.A. Assessing health status and health care utilization in adolescents with chronic kidney disease. J Am Soc Nephrol. 2005;16:1427–1432. doi: 10.1681/ASN.2004040258. [DOI] [PubMed] [Google Scholar]
- 3.Xiao N., Stolfia A., Malatesta-Muncher R. Risk behaviors in teens with chronic kidney disease: a study from the Midwest Pediatric Nephrology Consortium. Int J Nephrol. 2019;2019:7828406. doi: 10.1155/2019/7828406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hendren E.M., Reynolds M.L., Mariani L.H. Confidence in women’s health: a cross border survey of adult nephrologists. J Clin Med. 2019;8:176. doi: 10.3390/jcm8020176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berns J.S. A survey-based evaluation of self-perceived competency after nephrology fellowship training. Clin J Am Soc Nephrol. 2010;5:490–496. doi: 10.2215/CJN.08461109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fox H.B., McManus M.A., Klein J.D. Adolescent medicine training in pediatric residency programs. Pediatrics. 2010;125:165–172. doi: 10.1542/peds.2008-3740. [DOI] [PubMed] [Google Scholar]
- 7.Hellerstedt W.L., Smith A.E., Shew M.L., Resnick M.D. Perceived knowledge and training needs in adolescent pregnancy prevention: results from a multidisciplinary survey. Arch Pediatr Adolesc Med. 2000;154:679–684. doi: 10.1001/archpedi.154.7.679. [DOI] [PubMed] [Google Scholar]
- 8.Spencer A.L., Kern L.M. Primary care program director’s perceptions of women’s health education: a gap in graduate medical education persists. J Womens Health (Larchmt) 2008;17:549–556. doi: 10.1089/jwh.2007.0473. [DOI] [PubMed] [Google Scholar]
- 9.Dehlendorf C., Levy K., Ruskin R., Steinauer J. Health care providers’ knowledge about contraceptive evidence: a barrier to quality family planning care? Contraception. 2010;81:292–298. doi: 10.1016/j.contraception.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.