Abstract
Objectives
The objective of this study was to compare the association between mental well-being between obese (classes 1 and 2), over-weight and non-obese population-based individuals
Methods
A population-based cross-sectional study was conducted in Al-Kharj, Saudi Arabia. A total of 1019 Saudi nationals aged ≥ 18 years participated in the survey. BMI scores were used to categorize participants into three groups: Obese, overweighted and non-obese/non-overweight. Mental well-being was evaluated by using the validated Arabic version of the General Health Questionnaire version 12 (GHQ-12).
Results
We used total GHQ score (Mean=12; SD=5.23) to compare mental well-being between the four BMI class categories. The overall one-way ANOVA model was statistically significant (F = 7.018, d = 6, P < 0.001). In multivariate analysis, after adjusting for sociodemographic variables, diabetes and smoking statuses we found that higher psychological distress (as evident by a higher total GHQ score) was associated with higher BMI. The unstandardized Beta regression coefficient = 2.627; P = 0.034). Females were more likely to have higher psychological distress than males (unstandardized Beta = 1.466, P = 0.003). Job status whether being unemployed or ‘civilian’ (civil worker) was significantly associated with higher psychological distress (unstandardized Beta = 1.405, P = 0.041). Being diabetic has a 1.6 times higher risk of psychological distress (unstandardized Beta = 1.604, P = 0.027).
Conclusion
The study highlights the public health implications of psychological distress amongst individuals with overweight and obesity in Saudi Arabia. Future longitudinal studies should explore the temporality of this relationship.
Keywords: General Health Questionnaire-12, Obesity, Overweight, BMI, Psychological distress, Saudi Arabia
1. Introduction
Obesity is a term that generally refers to the accumulation of excessive body fat (Al-Ghamdi et al., 2018). The World Health Organization (WHO) has created its definition of being overweight and obese based on health, with the terms denoting abnormal or excessive fat accumulation that may impair health (Organization, 2013). The Center for Disease Control and Prevention (CDC) defines them as “labels for ranges of weight that are greater than what is generally considered healthy for a given height.” Primary obesity refers to when an individual consumes more energy than that which can be utilized (Mukherjee et al., 2017). This contributes to 95% of obesity globally. Secondary obesity is attributed to an underlying organic cause that leads to the accumulation of body fat (Mukherjee et al., 2017). Worldwide obesity has reached epidemic proportions over the years (Consultation, 2003, James et al., 2004), affecting both developed and developing countries. It is estimated that around a third of the world’s population is affected by obesity and 38.5 million DALYs (Disability-adjusted life years) are lost (Organization, 2016).
Body Mass Index (BMI) is calculated by dividing one’s weight in kilograms and the square of one’s height in meters2, and is considered a valid index to determine obesity (Després, 1991; Zhao et al., 2011). The prevalence of obesity and being overweight individuals varies from region to region (Shayan et al., 2016). In developing regions such as South Asia, the obese and overweight population ranges from 11 to 52.6% (Peltzer et al., 2014). In the Middle East and Central Europe, obesity and overweight is seen as high as 47.4% (Peltzer et al., 2014). Previously, WHO has reported the prevalence of obesity to be 44% of females and 28% of males in Saudi Arabia (Gollogly, 2009; Al-Ghamdi et al., 2018), while 71% of women and 66% of men were overweight (Gollogly, 2009, Al-Ghamdi et al., 2018). In our previous survey of the participants of Al-Kharj, Saudi Arabia, (n = 1019) 54.3% of our cohort was obese or overweight, compared to 45.7% non-obese (Al-Ghamdi et al., 2018).
Currently, obesity is not considered a psychological disorder (Cornette, 2011; Russell-Mayhew et al., 2012). Perhaps, because of this, underlying psychological causes of obesity have not yet been studied in detail (Russell-Mayhew et al., 2012). Obesity is known to contribute to many non-communicable diseases (Al-Ghamdi et al., 2018); For instance, type II diabetes,(Sobal et al., 2009) hypertension(Masaki et al., 1997) and ischemic stroke have all been linked to obesity (Al-Ghamdi et al., 2018). A linear relationship between obesity and obstructive sleep apnea has also been observed (Jehan et al., 2018). Previously, obesity and its related co-morbid conditions have been shown to significantly reduce health-related quality of life (Mar et al., 2013). Similarly, the overweight and obese participants has been observed at an increased risk of suffering from depression (Stunkard, 2003; Jarolimova et al., 2013) and mood disorders (Amianto et al., 2011). It is also thought that childhood obesity may lead to a higher risk of developing these conditions (Mustillo et al., 2003). A meta-analysis of 17 cross-sectional studies have reported a bidirectional relationship between obesity and depression (De Wit et al., 2010). This was more pronounced in women (De Wit et al., 2010). Another systematic review of 15 cross-sectional studies reported that there is a risk associated between the two variables. It also reported a 55% increased risk of developing depression amongst obese individuals as well as a 58% risk of developing obesity amongst depressed individuals (Luppino et al., 2010). This problem is further aggravated by stigma associated with obesity (Farhangi et al., 2017). Obese people are considered or thought to be indolent, weak and lacking self-confidence and the motivation to improve their health (Puhl and Suh, 2015).
There is a high prevalence of obesity and overweight in Saudi Arabia (Al-Ghamdi et al., 2018). In spite of this, there seems to be a lack of literature reporting the mental well-being of such individuals. The GHQ is a reliable tool that can been used to assess the psychological well-being of individuals (El-Metwally et al., 2018). It has many versions; however, owing to the ease of its use, GHQ-12 is the most commonly administered version (El-Metwally et al., 2018). The objective of this study was to assess the mental well-being of a cohort of the Saudi Arabian participants and correlate it with being obese, over-weight or non-obese.
2. Material and methods
2.1. Study design
A population-based cross-sectional study was conducted between January 2016 to June 2016 (for a duration of six months). Data were collected on the general population of Saudi Arabia.
2.2. Study setting
The study was conducted in one city of Saudi Arabia, Al Kharj, which is located in central Saudi Arabia. It hosts a population of approximately 376,000 and is located 77 km south of Riyadh. Connected to Riyadh and Dammam by rail, it has both an urban and rural population, while also being surrounded by adjacent nomadic communities.
2.3. Sampling technique
A total of 1019 participants (638 females and 381 males) were included in the study. From the previous published research we know that the prevalence of obesity in Saudi Arabia was 28.7 (Memish et al., 2014). A multistage sampling technique was used to recruit participants from both government and private institutions. This was carried out after obtaining verbal consent from the participants. Clusters were generated after acquiring a list of total participants from the respective institutions. Samples were further selected using simple random sampling from each of the clusters.
2.4. Eligibility criteria
Adult Saudi nationals (18 years and above) were selected for the study. It was based on their willingness to participate in the study. Non-Saudi, children and those who did not give informed consent were excluded from the study.
2.5. Material/instruments
A structured self-administrated questionnaire was used to collect data on each participant. The questionnaire consisted of a validated GHQ-12 for the Arab population (El-Rufaie and Daradkeh, 1996). Details of the data collection were mentioned in a previously published study (El-Metwally et al., 2018). Data were collected on various demographic and study related variables such as age, gender, marital status and level of education. Anthropometric measurements such as weight (kilograms), height (centimeters) and BMI were also included in the questionnaire. The GHQ-12 was filled out by the participants. It consists of 12-items assessing the severity of mental distress using a 4-point Likert scoring technique (ranging from 0-alwayes to 3-never). The total score was utilized to indicate the mental health of the individual.
2.6. Procedure
Based on the standards of anthropometric methods, the weight of every participant was noted with socks and lightweight clothing on. This was nearest to 0.1 kg using a digital medical scale. Height of participants was measured using a stadiometer closest to 0.1 cm with no shoes on. Prior to every measurement, the scale was recalibrated to zero and was repeatedly cross-checked during the course of measurements. BMI was calculated using the formula weight in kilograms and height in meter square (kg/m2). The WHO cutoff of 30 kg/m2 was used to identify obesity.
2.7. Operational definition
Overweight was defined as a BMI of 25 to 29.9 kg/m2 and obesity was a BMI of > 30 kg/m2 (Organization, 2017). GHQ-12 was used to assess the mental well-being of participants. The questionnaire was sent to participants and they returned it after responding to the questions.
2.8. Data analysis
Data analysis was performed on SPSS version 26.0 for Windows. Continuous data was reported in mean and in standard deviation when data was normally distributed. Categorical variables were reported as frequency and percentages. The Chi-squared test was used to assess the association between categorical variables. T-test, or ANOVA, was used to assess the association between continuous variables. P-value < 0.05 was considered significant.
2.9. Ethical consideration
The study commenced after receiving ethical approval from the institutional review board (Committee of Scientific Research and Publication) of the College of Medicine, Prince Sattam bin Abdul-Aziz University. The approval number of the study is PSAU/COM/RC/IRB/P/49. Both written and verbal informed consent were obtained from all participants enrolled in the study. Participation in the study was voluntary and confidentiality was maintained at all times.
3. Results section
3.1. Demographic characteristics of study participants
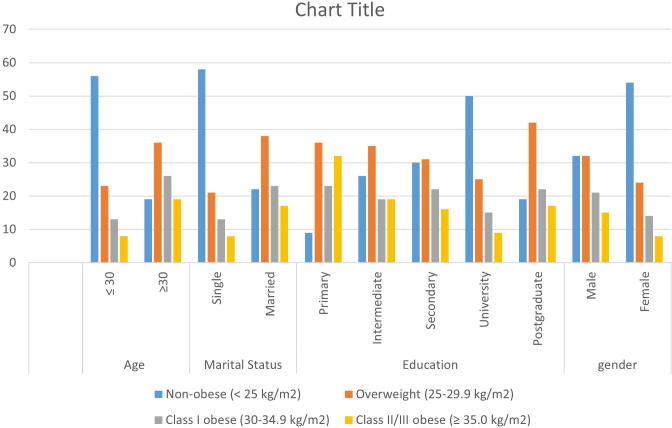
The detailed description of the study participants was reported in previous published studies (Al-Ghamdi et al., 2018). The summarized results were presented in Fig. 1.
Fig. 1.
3.2. GHQ-12 score and BMI class categorical variable (One-Way Anova)
We used a total GHQ score (Mean = 12; SD = 5.23); as previously reported (El-Metwally et al., 2018), to compare between four BMI class categories: non-obese (<25 kg/m2), overweight (25–29.9 kg/m2), class I obese (30–34.9 kg/m2), and class II/III obese (≥35.0 kg/m2). The overall one-way ANOVA model was statistically significant (F = 7.018, d = 6, P < 0.001).
Comparison of the mean total GHQ score across the four BMI categories is presented in Table 1.
Table 1.
Mean difference in total GHQ-12 Score across Body Mass Index (BMI) categories.
| N | Mean | Std. Deviation | Std. Error | ||
|---|---|---|---|---|---|
| 0 Non-obese (<25 kg/m2) | 459 | 10.96 | 5.067 | 0.237 | |
| 1 Overweight (25–29.9 kg/ m2) | 267 | 11.43 | 5.144 | 0.315 | |
| 2 Class1 obese (30–34.9 kg/ m2) | 165 | 12.28 | 5.768 | 0.449 | |
| 3 Class2&3 obese (>=35 kg/ m2) | 111 | 14.88 | 5.253 | 0.499 | |
| Total | 1002 | 12.39 | 5.229 | 0.165 | |
| Model | Fixed Effects | 5.229 | 0.165 | ||
| Random Effects | 0.167 |
3.3. Tukey’s Post-Hoc analysis
Within the One-Way ANOVA Model above, we performed several Tukey’s post-hoc multiple comparison tests (comparing the four BMI groups against each other). One post-hoc analysis illustrated that compared to the ‘non-obese’ group (as the reference category), the ‘class I obese’ was statistically significant (Mean difference 3.261, P = 0.028). The 95% confidence interval (CI) was from (2.659 to 7.024). A second post-hoc analysis showed the ‘class II/III obese’ was also statistically significant when compared to the ‘non-obese’ group as the reference category, with a Mean difference of 1.076 (P = 0.041). The 95% CI was from (0.87 to 1.35).
3.4. Multiple linear regression analysis
To examine the association between BMI as a continuous independent variable and the total GHQ score (outcome variable), a multiple linear regression model was carried out (Table 2). After adjusting for sociodemographic variables, diabetes and smoking statuses we found that higher psychological distress (as evident by a higher total GHQ score) was associated with higher BMI (i.e., in more overweight and obese people). The unstandardized Beta regression coefficient = 2.627; P = 0.034). Females were more likely to have higher psychological distress than males (unstandardized Beta = 1.466, P = 0.003). Job status whether being unemployed or ‘civilian’ (civil worker) was significantly associated with higher psychological distress (unstandardized Beta = 1.405, P = 0.041). Being diabetic has a 1.6 times higher risk of psychological distress (unstandardized Beta = 1.604, P = 0.027), as illustrated in Table 2.
Table 2.
Multiple linear regression model regressing total GHQ score on body mass index (BMI) and other sociodemographic and lifestyle variables (n = 1,018).
| total GHQ score | Unstandardized Beta (B) | S.E. of B | Sig. | Standardized B | 95% C.I. for Odds ratio |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Body Mass Index (BMI) | 2.627 | 0.026 | 0.034 | 1.135 | 2.025 | 3.079 |
| Age | 0.032 | 0.028 | 0.252 | 0.054 | −0.023 | 0.088 |
| Gender (Female) | 1.466 | 0.492 | 0.003 | −0.052 | 0.500 | 2.432 |
| Marital status (single/not married) | −0.562 | 0.448 | 0.210 | −0.052 | −1.441 | 0.317 |
| Job (not working; or civilian) | 1.405 | 0.413 | 0.041 | 0.043 | 1.217 | 2.306 |
| Diabetes status (diabetic) | 1.604 | 0.862 | 0.027 | 1.120 | 1.327 | 2.768 |
| Smoking status | 0.141 | 0.297 | 0.633 | 0.017 | −0.441 | 0.723 |
4. Discussion
4.1. Summary of results
Research in Saudi Arabia that explores the association between overweight and obesity with mental health is scarce. Through our present study, we aimed to assess the mental well-being of Saudi citizens residing in Al-Kharj, Saudi Arabia. There was an overall significant difference in the mental health of individuals who were non-obese, overweight, obese class I and obese class II/III (p < 0.001) using One-Way ANOVA. Likewise, the majority of participants were either overweight or obese at 54.3%, compared to the non-obese participants at 45.7% (Al-Ghamdi et al., 2018) It was further seen that BMI increased linearly with increasing age (Al-Ghamdi et al., 2018).
4.2. Comparison of results
To the best of our knowledge, no previous study has been conducted in Saudi Arabia assessing the mental well-being of obese and overweight individuals. We used GHQ-12 to assess the psychological well-being of all groups of participants, both non-obese and obese. GHQ-12 is a frequently used and validated tool.
In one study, GHQ-28 was used to assess mental well-being in an Indian population of obese and non-obese individuals. It was seen that there was a significant difference in various subscales of GHQ between the two groups (p < 0.001) (Mukherjee et al., 2017) However, they had a relatively small sample size. This study’s findings concur with that study’s in that there was an overall significant difference between non-obese, overweight and both categories of obese (I and II/III) (F = 7.018, d = 6, P < 0.001) individuals. Another study from Iran which used GHQ-28 also reported a significant difference in mental health on all subscales between non-obese, overweight and obese participants (p < 0.001) (Shayan et al., 2016) The study was only conducted on women with a moderate sample size of 300 (Shayan et al., 2016) Another study reported overweight self-stigma using SF-12 and GHQ-12 It was seen that greater weight stigma was associated with higher mental distress (Farhangi et al., 2017). Another study assessing both overweight and underweight individuals reported that males aged 40 – 64 years had worse mental health in the Japanese population when gauged by GHQ-12 (Hori et al., 2016).
A meta-analysis also reported positive association between obesity and depression (O.R 1.34, 95% C.I 1.1–1.64, p-value 0.005) and obese female participants was more likely to have depression as compare to male (p < 0.05) (Quek et al., 2017). Our study results provide evidence that is similar to what has been previously reported—that the overweight and obese population has a greater tendency to be depressed or have a poor mental well-being. This was also supported by another study, which reported a higher association to be found in young and middle-aged women (Mannan et al., 2016). Another study conducted on 7108 women with age > 18 years and reported path analyses. In women with depression mediated the development of obesity through physical impairment, social dysfunction that is ow social support and high social strain and emotional eating that is they used food to deal with stress. Similarly, in obese women, physical impairment and emotional eating mediated the development of depression (Vittengl, 2018).
Although both conditions are commonly present in the general population and associated with many co-morbidities. Recent literature reported that both can overlap or combine and create a layered stigma which in turn associated with more health-related negative outcomes (Luck-Sikorski et al., 2018). It is also evident from the growing body of literature that both conditions shared some mechanisms that is epidemiological, clinical and biological pathways (Patist et al., 2018, Tyrrell et al., 2019, Milaneschi et al., 2019, Wurtman and Wurtman, 2018). It is, therefore, necessary to treat both conditions while treating in mental health clinics or in obesity clinics. A clinical trial showed that collaborative care integrated treatment including behavioral weight loss therapy and problem-solving therapy with or without using antidepressant medication. This integrated treatment showed helped in both weight loss and depressive symptoms in a year (Ma et al., 2019).
4.3. Limitations of study design
We acknowledge that there are a few limitations to our study. These limitations are inherent to the study design. Firstly, being a cross sectional study, the direction of association between mental well-being and overweight/obesity cannot be deduced. A better study design would be a cohort study to assess that relationship. Secondly, the collected data was only on a subgroup of Saudi citizens: residents of Al-Kharj, Saudi Arabia. To further this, the participants consisted of active Saudi citizens. Individuals who were retired, jobless, and non-Saudi citizens were excluded. Those younger than 18 years of age were also excluded. Inclusion of these groups could have potentially altered the results and we could have better portrayed the true prevalence of mental disorder in Al-Kharj, Saudi Arabia. The results should also be interpreted in light of the fact that Al-Kharj, although composed of both an urban and a rural population, does not accurately depict the whole population of Saudi Arabia. However, it does resemble the wider population of Saudi Arabia, thus increasing the external validity of the study. Further, adding to the strength of this study is the utility of validated tools to evaluate mental well-being and its stringent eligibility criteria.
5. Conclusion
There was a significant association between the depression and obesity among the participants of Al Kharj, Saudi Arabia. Health practitioner also considered combined or overlapping effect of both conditions, when treating in depressed patient with obesity in mental health settings and vice versa. The study highlights the public health implications of psychological distress amongst the residents of Al- Kharj, Saudi Arabia. Future studies must explore this further.
5.1. Implementation and future prospects
To the best of our knowledge, this present study is the first to look into the mental well-being of overweight and obese residents of Saudi Arabia using a validated tool (GHQ-12). It can further be used as a steppingstone for research into a larger population of Saudi Arabia. This would also help sensitize the healthcare professionals of Saudi Arabia to the mental status of obese and overweight citizens. Likewise, it could help in assessing them and, if needed, referring them to specialized departments such as weight-loss programs and well-being clinics. Our study is significant in that it highlights an important and a neglected aspect of the overweight and obese population.
Source of funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable. This manuscript did not contain any individual personal data.
Authors' contributions
All authors contributed to the writing of the manuscript and had access to the data. KKA, MA, SG, BA, JA and AE were involved in the design of the study. SB contributed to the data collection for this study. MAA wrote the first draft. MA did the statistical analysis of the manuscript, after BK, SMA and KA read and contributed to the revision of the manuscript. All authors contributed to the final revisions of the manuscript. All authors have read and approved the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This study was supported by the Deanship of Scientific Research at the Prince Sattam Bin Abdulaziz University, Al-Kharj, Saudi Arabia. We are greatly thankful for this support.
Footnotes
Peer review under responsibility of King Saud University.
References
- Al-Ghamdi S., Shubair M.M., Aldiab A., Al-Zahrani J.M., Aldossari K.K., Househ M., Nooruddin S., Razzak H.A., El-Metwally A. Prevalence of overweight and obesity based on the body mass index; a cross-sectional study in Alkharj, Saudi Arabia. Lipids Health Dis. 2018;17:134. doi: 10.1186/s12944-018-0778-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amianto F., Lavagnino L., Leombruni P., Gastaldi F., Daga G.A., Fassino S. Hypomania across the binge eating spectrum. A study on hypomanic symptoms in full criteria and sub-threshold binge eating subjects. J. Affect. Disord. 2011;133:580–583. doi: 10.1016/j.jad.2011.04.049. [DOI] [PubMed] [Google Scholar]
- CONSULTATION, J. W. F. E. 2003. Diet, nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser, 916, i-viii, 1–149. [PubMed]
- Cornette, R. E. 2011. The emotional impact of obesity on children. Global Perspectives on Childhood Obesity. Elsevier.
- de Wit L., Luppino F., van Straten A., Penninx B., Zitman F., Cuijpers P. Depression and obesity: a meta-analysis of community-based studies. Psychiatry Res. 2010;178:230–235. doi: 10.1016/j.psychres.2009.04.015. [DOI] [PubMed] [Google Scholar]
- Després J.-P. Obesity and lipid metabolism: relevance of body fat distribution. Curr. Opin. Lipidol. 1991;2:5–15. [Google Scholar]
- El-Metwally A., Javed S., Razzak H.A., Aldossari K.K., Aldiab A., Al-Ghamdi S.H., Househ M., Shubair M.M., Al-Zahrani J.M. The factor structure of the general health questionnaire (GHQ12) in Saudi Arabia. BMC health services research. 2018;18:595. doi: 10.1186/s12913-018-3381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Rufaie O.E.F., Daradkeh T.K. Validation of the Arabic versions of the thirty-and twelve-item General Health Questionnaires in primary care patients. The British Journal of Psychiatry. 1996;169:662–664. doi: 10.1192/bjp.169.5.662. [DOI] [PubMed] [Google Scholar]
- Farhangi M.A., Emam-Alizadeh M., Hamedi F., Jahangiry L. Weight self-stigma and its association with quality of life and psychological distress among overweight and obese women. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2017;22:451–456. doi: 10.1007/s40519-016-0288-2. [DOI] [PubMed] [Google Scholar]
- Gollogly L. World Health Organization; 2009. World health statistics 2009. [Google Scholar]
- Hori D., Tsujiguchi H., Kambayashi Y., Hamagishi T., Kitaoka M., Mitoma J., Asakura H., Suzuki F., Anyenda E.O., Nguyen T.T.T. The associations between lifestyles and mental health using the general health questionnaire 12-items are different dependently on age and sex: a population-based cross-sectional study in Kanazawa, Japan. Environ. Health Prev. Med. 2016;21:410–421. doi: 10.1007/s12199-016-0541-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James P.T., Rigby N., Leach R., Force I.O.T. The obesity epidemic, metabolic syndrome and future prevention strategies. European Journal of Cardiovascular Prevention & Rehabilitation. 2004;11:3–8. doi: 10.1097/01.hjr.0000114707.27531.48. [DOI] [PubMed] [Google Scholar]
- Jarolimova, J., Tagoni, J. & Stern, T. A. 2013. Obesity: its epidemiology, comorbidities, and management. The primary care companion for CNS disorders, 15. [DOI] [PMC free article] [PubMed]
- Jehan S., Myers A.K., Zizi F., Pandi-Perumal S.R., Jean-Louis G., McFarlane S.I. Obesity, obstructive sleep apnea and type 2 diabetes mellitus: Epidemiology and pathophysiologic insights. Sleep medicine and disorders: international journal. 2018;2:52. [PMC free article] [PubMed] [Google Scholar]
- Luck-Sikorski C., Schomerus G., Jochum T., Riedel-Heller S.G. Layered stigma? Co-occurring depression and obesity in the public eye. J. Psychosom. Res. 2018;106:29–33. doi: 10.1016/j.jpsychores.2018.01.003. [DOI] [PubMed] [Google Scholar]
- Luppino F.S., de Wit L.M., Bouvy P.F., Stijnen T., Cuijpers P., Penninx B.W., Zitman F.G. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch. Gen. Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Ma J., Rosas L.G., Lv N., Xiao L., Snowden M.B., Venditti E.M., Lewis M.A., Goldhaber-Fiebert J.D., Lavori P.W. Effect of integrated behavioral weight loss treatment and problem-solving therapy on body mass index and depressive symptoms among patients with obesity and depression: the RAINBOW randomized clinical trial. JAMA. 2019;321:869–879. doi: 10.1001/jama.2019.0557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannan M., Mamun A., Doi S., Clavarino A. Prospective associations between depression and obesity for adolescent males and females-a systematic review and meta-analysis of longitudinal studies. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0157240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mar J., Karlsson J., Arrospide A., Mar B., de Aragón G.M., Martinez-Blazquez C. Two-year changes in generic and obesity-specific quality of life after gastric bypass. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2013;18:305–310. doi: 10.1007/s40519-013-0039-6. [DOI] [PubMed] [Google Scholar]
- Masaki K.H., Curb J.D., Chiu D., Petrovitch H., Rodriguez B.L. Association of body mass index with blood pressure in elderly Japanese American men: the Honolulu Heart Program. Hypertension. 1997;29:673–677. doi: 10.1161/01.hyp.29.2.673. [DOI] [PubMed] [Google Scholar]
- Memish Z.A., el Bcheraoui C., Tuffaha M., Robinson M., Daoud F., Jaber S., Mikhitarian S., Al Saeedi M., Almazroa M.A., Mokdad A.H., Al Rabeeah A.A. Obesity and associated factors–Kingdom of Saudi Arabia, 2013. Preventing chronic disease. 2014;11:E174. doi: 10.5888/pcd11.140236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milaneschi Y., Simmons W.K., van Rossum E.F.C., Penninx B.W.J.H. Depression and obesity: evidence of shared biological mechanisms. Mol. Psychiatry. 2019;24:18–33. doi: 10.1038/s41380-018-0017-5. [DOI] [PubMed] [Google Scholar]
- Mukherjee U., Bhattacharya B., Mukhopadhyay S., Poddar S. A comparative study of psychosocial factors of obesity. International Journal of Educational and Psychological Researches. 2017;3:87. [Google Scholar]
- Mustillo S., Worthman C., Erkanli A., Keeler G., Angold A., Costello E.J. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111:851–859. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- Organization W.H. World Health Organization; 2013. Global tuberculosis report 2013. [Google Scholar]
- ORGANIZATION W.H. World Health Organization; 2016. World health statistics 2016: monitoring health for the SDGs sustainable development goals. [Google Scholar]
- Organization W.H. Prevalence Obesity and Overweight. Diakses pada. 2017;20 [Google Scholar]
- Patist C.M., Stapelberg N.J.C., du Toit E.F., Headrick J.P. The brain-adipocyte-gut network: Linking obesity and depression subtypes. Cognitive, Affective, & Behavioral Neuroscience. 2018;18:1121–1144. doi: 10.3758/s13415-018-0626-0. [DOI] [PubMed] [Google Scholar]
- Peltzer K., Pengpid S., Samuels T., Özcan N.K., Mantilla C., Rahamefy O.H., Wong M.L., Gasparishvili A. Prevalence of overweight/obesity and its associated factors among university students from 22 countries. Int. J. Environ. Res. Public Health. 2014;11:7425–7441. doi: 10.3390/ijerph110707425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl R., Suh Y. Stigma and eating and weight disorders. Current psychiatry reports. 2015;17:10. doi: 10.1007/s11920-015-0552-6. [DOI] [PubMed] [Google Scholar]
- Quek Y.H., Tam W.W.S., Zhang M.W.B., Ho R.C.M. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes. Rev. 2017;18:742–754. doi: 10.1111/obr.12535. [DOI] [PubMed] [Google Scholar]
- Russell-Mayhew, S., Mcvey, G., Bardick, A. & Ireland, A., 2012. Mental health, wellness, and childhood overweight/obesity. Journal of obesity. [DOI] [PMC free article] [PubMed]
- Shayan A., Masumi Z., Ataollahi M., Tohodi S., Forouhari S., Khani S. Investigation relationship between body mass index and general health of patient in Hamadan Fatemieh Hospital. Iran. Der Pharma Chemica. 2016;8:554–558. [Google Scholar]
- Sobal J., Hanson K.L., Frongillo E.A. Gender, ethnicity, marital status, and body weight in the United States. Obesity. 2009;17:2223–2231. doi: 10.1038/oby.2009.64. [DOI] [PubMed] [Google Scholar]
- Stunkard A. Faith MS. Allison KC. Depression and obesity. Biol Psychiatry. 2003;54:330–337. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- Tyrrell J., Mulugeta A., Wood A.R., Zhou A., Beaumont R.N., Tuke M.A., Jones S.E., Ruth K.S., Yaghootkar H., Sharp S. Using genetics to understand the causal influence of higher BMI on depression. Int. J. Epidemiol. 2019;48:834–848. doi: 10.1093/ije/dyy223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittengl J.R. Mediation of the bidirectional relations between obesity and depression among women. Psychiatry Res. 2018;264:254–259. doi: 10.1016/j.psychres.2018.03.023. [DOI] [PubMed] [Google Scholar]
- Wurtman J., Wurtman R. The trajectory from mood to obesity. Current obesity reports. 2018;7:1–5. doi: 10.1007/s13679-017-0291-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao G., Ford E.S., Li C., Tsai J., Dhingra S., Balluz L.S. Waist circumference, abdominal obesity, and depression among overweight and obese US adults: National Health and Nutrition Examination Survey 2005–2006. BMC psychiatry. 2011;11:130. doi: 10.1186/1471-244X-11-130. [DOI] [PMC free article] [PubMed] [Google Scholar]