Abstract
Objectives:
To explore the feasibility and outcomes of a resilience-based diabetes self-management education (RB-DSME) program to improve psychological and physiological health in African-American adults with type 2 diabetes.
Methods:
An experimental group (N = 32) received RB-DSME and a comparison group (N = 33) received standard DSME. Psychological and physiological measures were taken at baseline and 6 months. ANCOVAs assessed whether the experimental group improved its overall outcome relative to the comparison group, while controlling for baseline scores.
Results:
The experimental group’s outcomes were significantly improved vis-à-vis the comparison group for diabetes knowledge, positive meaning, HDL cholesterol, and fasting blood glucose.
Conclusions:
The RB-DSME shows feasibility and promise for enhancing health; a full-scale randomized trial is warranted.
Keywords: diabetes self-management, resilience, African Americans
Type 2 diabetes mellitus (T2DM) affects over 29 million Americans – 9.3% of the population – at an estimated cost of $245 billion annually. In 2012, 1.7 million new cases of T2DM were reported, and 86 million Americans had pre-diabetes. Minorities are disproportionately affected with 13.2% of African Americans and 12.8% Hispanics living with T2DM compared to 7.6% of non-Hispanic Whites. Complications from the disease (eg, heart disease and stroke, retinopathy, renal failure) are at an all-time high.1 African Americans are predisposed to higher rates of obesity (49%) and being overweight (27%), placing them at greater risk of T2DM.2 This common progression from obesity to T2DM3 to cardiovascular disease (CVD)4 is the greatest health threat facing African Americans. Moreover, the acceleration of T2DM, vascular disease and the resulting complications are largely preventable.5
Because T2DM is a demanding chronic disease, it affects patients both physiologically and psychologically. Individuals with T2DM worry about complications from the disease and experience greater stress than non-diseased individuals.6 African Americans also experience racial discrimination,7 and those of low socioeconomic status incur additional stressors (eg, financial insecurity, lack of quality healthcare and culturally relevant healthcare education), limiting their understanding of the disease and inhibiting their ability to make healthy lifestyle choices to control the disease. Further, African Americans report greater depressive symptoms than Caucasians,8 which constrains effective diabetes self-management9 and makes this population particularly vulnerable to complications from the synergistic effects of obesity, T2DM, and CVD. Given T2DM is a chronic condition, combined with the economic and personal costs associated with the disease progression, the potential impact of successful DSME interventions in the African-American community is substantial.
The RB-DSME intervention takes a new approach to DSME by infusing resilience into self-management education and promoting resilient resources based on the transactional model of stress and coping.10 This theory defines stress as a transaction between the person and the environment, whereby individuals appraise environmental demands as outweighing their abilities to cope with those demands. The concept of resilience has received increased attention over the years from researchers studying why some individuals in populations experiencing adversity do not succumb to those difficult circumstances. Resilience theory and research have the potential to enhance our understanding of individuals with T2DM by providing insight into possible interventions that enable enhanced diabetes self-management and subsequent diabetes control.
According to the protective factor model of resilience, a protective factor interacts with a stressor to reduce the likelihood of negative outcomes such as those described previously.10 Building on the work of O’Leary and Ickovics,11 Carver,12 and resilience interventions for heart health13 and breast cancer,14 we define the term resilience as the ability to recover quickly from disruptions in functioning that result from stress appraisals and return to the previous level of functioning. Resilient resources include: (1) positive adaptation to stress; (2) cognitive and behavioral abilities to cope effectively; (3) the ability to find positive meaning in the context of a stressor and to maintain patience and faith; and (4) tolerance of negative affect.10,12,15
Resilient resources have been shown to predict improved glycosylated hemoglobin (A1C) and to buffer worsening A1C in the face of increasing diabetes-related emotional distress.16 A link also has been found between low resilience and maladaptive coping in patients with diabetes longer than one year.17 However, only one study tested an intervention designed to enhance the resilient resources of individuals with T2DM, and in that study, although A1C improved, baseline A1C was already low (6.7%).18
Our previous pilot studies examined the beginning feasibility of offering a resilience-based diabetes self-management education (RB-DSME) intervention for African-American adults with T2DM. The resilience curriculum was originally developed and taught in corporate and military settings for over 10 years, and subsequently adapted for individuals with type 2 diabetes during our initial pilot work. We posited that resilience-based messages infused into current DSME training would help individuals think more realistically and flexibly about the stressful situations they encounter, and recognize that stressful situations provide opportunities for personal growth through taking greater responsibility, focusing on empowering interpretations, and creating meaningful connections. Further, individuals with greater resilient resources should be more likely to feel empowered to assess their blood glucose, and to take responsibility for eating a nutritious diet, being physically active, and creating an environment of support, rather than making excuses or blaming other people. In short, a strong foundation of resilience should enable enhanced self-management.
Using a one-group pretest-posttest design, a convenience sample of 16 African Americans ranging in age from 43 to 66 received a RB-DSME intervention. At the 6-month post-baseline data collection (N = 12), preliminary paired t-tests indicated significant improvements in diabetes empowerment, diabetes self-management behaviors, BMI, A1C, total cholesterol, LDL-cholesterol, and systolic and diastolic blood pressure, with medium to large effect sizes.19 We also found that a convenience sample of African-American adults (N = 93) who experienced a greater frequency of positive emotions to negative emotions reported greater health, as measured by higher resilience and lower depressive symptoms and A1C. Conversely, those who experienced one or more negative emotions for every positive emotion had lower resilience and higher depressive symptoms and A1C.20 Together, these pilot studies suggested that enhancing resilient resources might be a key factor enabling African Americans with T2DM to integrate self-management into their lives.
Importantly, we used an empowerment approach, incorporating a behavior-change protocol and creating a collaborative environment, thereby serving more as a partner than an expert.21 Based on cultural characteristics and preferences of African-American participants obtained from our pilot study19 and other research,22–24 the RB-DSME intervention was culturally responsive in many ways, including use of pastoral endorsement and support from key community leaders to establish trust in the community, participant involvement, and continued follow-up.25,26 It also was community based,27,28 encouraged participants to express their spiritual beliefs and cultural practices, used culturally competent learning methods such as story-telling,29–31 held participants accountable to the group, included peer mentors for support, and included family members as desired.27
The purpose of the study reported here was to examine the RB-DSME intervention’s potential feasibility and effectiveness at 6 months post-study entry with a larger sample and using a quasi-experimental design. Feasibility was assessed in terms of our ability to recruit and retain study participants in church and community settings, as well as program satisfaction. We also examined the intervention’s potential effectiveness via changes in diabetes knowledge, psychological well-being (including 4 resilient resources explained above), diabetes self-management behaviors and physiological markers of obesity, diabetes control and CVD indicators in an experimental group receiving the RB-DSME intervention, and a comparison group receiving standard DSME. It was hypothesized that both experimental and comparison group participants would show significant improvements in diabetes knowledge, but experimental group participants would show significantly greater improvements in psychological well-being, diabetes self-management behaviors, and physiological markers of obesity, diabetes control, and CVD indicators than the comparison group.
METHODS
Study Design
Intervention effectiveness was examined using a quasi-experimental design with the primary outcome variables measured at baseline and 6 months post-study entry. Participants (N = 33) were first recruited to a comparison condition receiving standard DSME. At the conclusion of these class sessions we recruited participants (N = 32) to an experimental condition receiving a RB-DSME intervention. In total, 65 participants comprising 6 small groups (3 comparison and 3 experimental) of approximately 10 people per group participated in the study. All participants completed the educational sessions; however 4 participants did not attend the 6-month post-intervention data collection (Figure 1).
Figure 1.
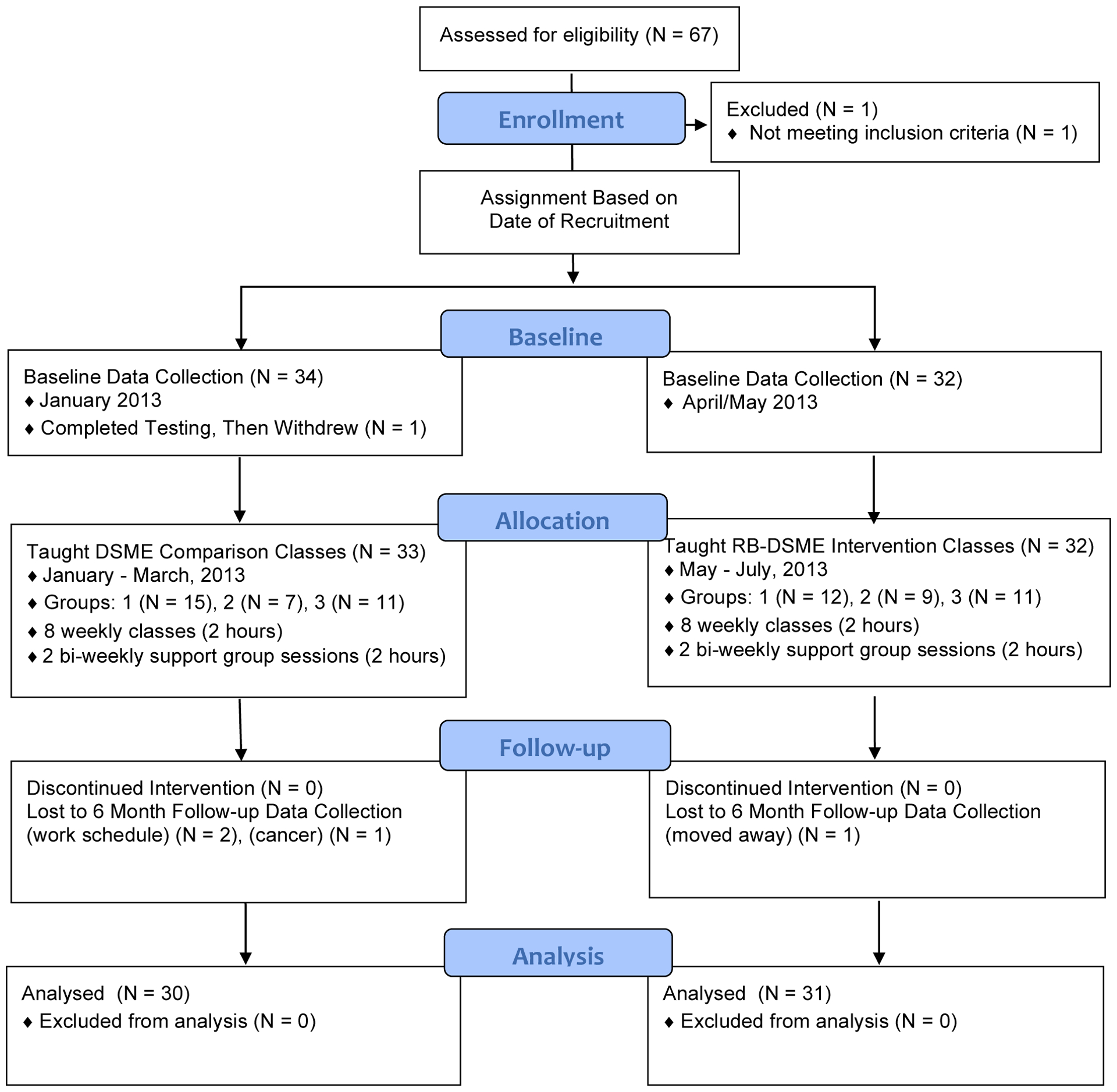
Flowchart of Study Design and Participants Retained at 6 Months Follow-Up
Participants and Procedures
Recruitment for the study sample was through radio and church announcements, flyers posted in the community, and fasting blood glucose screenings held at 2 participating churches on Sunday mornings. Study participants were required to meet the following inclusion criteria: (1) African-American race; (2) diagnosed with T2DM; (3) between 30 and 85 years old; and (4) not currently participating in another diabetes self-management program. Individuals were excluded if they were pregnant/lactating or had a medical condition for which changes in diet and physical activity would be contraindicated (eg, kidney failure requiring dialysis and peripheral vascular disease severe enough to preclude walking 3 times per week). We did not experience difficulty in enrolling individuals; over 85% of those who called and expressed a desire to participate attended baseline data collection and participated.
All survey and physiological data were collected at baseline and 6-months post-intervention. Questionnaires were self-administered, with assistance provided to those with literacy limitations, and took approximately 30–45 minutes to complete. All instruments were previously used with African-American adults. Demographic characteristics including sex, age, year of T2DM diagnosis, marital status, education level, employment status, and current household yearly income. In addition, any previous diabetes instruction also was noted.
Participants for the study were a convenience sample (N = 65) of African Americans (47 women, 18 men) ranging in age from 31 to 85 years (mean age: 62 ± 10.3 years). They had been diagnosed with T2DM an average of 9.9 ± 8.7 years. All study participants received up to $40 cash to compensate their time and any costs associated with transportation to sessions. Laboratory results were shared with participants and their healthcare provider (HCP). Participants who did not have a HCP were referred to the endocrinologist at a university-affiliated community clinic. All participants reported having a healthcare provider at study entry; however, several participants chose to make an appointment with the endocrinologist at the university-affiliated community clinic (5 comparison and 4 experimental) prior to 6-month data collection. Reasons given for wanting to see the endocrinologist included loss of healthcare, desire to change providers, and complications.
Measures
Program feasibility was assessed through program attendance and retention for both the RB-DSME and DSME programs. Program satisfaction also was assessed at the end of the intervention using the following item: Taking everything into consideration, how satisfied were you with the diabetes program? Possible response options ranged from 1 (extremely dissatisfied) to 7 (extremely satisfied). The primary outcome variables assessed at baseline and 6-month follow-up included: diabetes knowledge, psychological well-being (indicators of resilience, quality of life, perceived stress, depressive symptoms), diabetes self-management (physical activity, survey of additional behaviors), and physiological markers of obesity (body fat, body mass index [BMI], waist circumference), diabetes control (fasting blood glucose [FBG], A1C), and CVD indicators (blood pressure [BP], total cholesterol, low-density lipoprotein [LDL] cholesterol, high-density lipoprotein [HDL] cholesterol, triglycerides).
Diabetes knowledge.
Diabetes knowledge was measured using the Diabetes Knowledge Test.32 The general test includes 14 multiple-choice items and is scored from 0% to 100%. Baseline internal consistency (α = .39) was weak compared to the original study (α = .71).32
Positive adaptation to stress.
Resilience was measured using 4 indicators: (1) positive adaptation to stress; (2) cognitive and behavioral abilities to cope effectively; (3) the ability to find positive meaning in the context of a stressor and to maintain patience and faith; and (4) tolerance of negative affect. Positive adaptation to stress was measured using the Connor-Davidson Resilience Scale (CD-RISC).33 The CD-RISC identifies characteristics that enable individuals to adapt to stress successfully, such as faith, goal setting, and patience, as well as the tendency to perceive change as a challenge, maintain a commitment to the people and activities in which one is involved, and have a sense of personal control in handling life events. Following the approach used by Connor and Davidson,33 a resilience score was calculated as the sum of all items measured on a scale from 0 (not true at all) to 4 (always true), with higher scores indicating greater resilience. The CD-RISC internal consistency was strong (α = .88).
Coping.
Cognitive and behavioral abilities to cope effectively were measured using the brief version of the Coping Orientations to Problems Experienced Scale (Brief COPE).34 The Brief COPE measures a broad range of cognitive and behavioral coping strategies used during stressful experiences on a scale from 1 (not at all) to 4 (a lot). Items were grouped together into the most commonly used supersets: problem-focused and emotion-focused coping strategies. Problem-focused coping (PFC) strategies are those that directly address the stressful situation or whose value exceeds merely reducing distress (ie, active coping, planning, positive reframing, acceptance, emotional support, instrumental support, and religion). Emotion-focused coping (EFC) strategies are used to reduce or manage emotional reactions and feelings of distress (ie, self-distraction, denial, venting, substance use, behavioral disengagement, self-blame, and humor). The brief COPE instrument alpha coefficients were .86 and .72 for the PFC and EFC subscales, respectively. The study focused on the percentage of PFC, computed by dividing PFC by the sum of PFC and EFC.35
Positive meaning.
The ability to find positive meaning in the context of a stressor and to maintain patience and faith was measured using the Positive Meaning Scale (PMS).36 The PMS includes 5 items and measures the extent to which participants find positive meaning (eg, trying to learn from the experience, changing one’s life in a positive way, trying to see the good side of the situation) in the context of T2DM. Individuals’ scale scores were calculated as the mean across all items on a scale ranging from 0 (definitely no) to 3 (definitely yes). The PMS had an internal consistency of α = .79.
Negative affect.
Tolerance of negative affect was measured using the 20-item Positive and Negative Affect Schedule (PANAS).37 The PANAS measures the extent that individuals generally experienced various positive (eg, excited, inspired, interested) and negative (eg, irritable, upset, afraid) emotions. Participants’ responded on a scale from 1 (not at all) to 5 (very much so), and scale scores were calculated as the mean across all items, with alpha coefficients of .83 and .84 for positive and negative emotions, respectively.
Quality of life.
Quality of life concerns regarding diabetes were measured using the 13-item Social and Personal Factors Scale of the Diabetes Care Profile.38 This scale assessed how often diabetes made life difficult or kept participants from doing normal daily activities on a scale ranging from 1 (strongly disagree) to 5 (strongly agree). Individuals’ scale scores were calculated as the mean across all items. The quality of life measure was reliable, with a strong internal consistency (α = .86).
Perceived stress.
Perceived stress was assessed using the 10-item Perceived Stress Scale (PSS),39 which measured the degree that situations in one’s life are perceived as stressful. Participants rated how often stressful events occurred during the past month on a scale from 0 (never) to 4 (very often). Following the approach used by Cohen,39 a stress score was calculated as the sum of the 10 items. The PSS measure was reliable, with a strong internal consistency (α = .82).
Depressive symptoms.
Depressive symptoms were assessed with the 20-item Center for Epidemiologic Studies Depression Scale (CES-D), which measured depressive symptoms experienced, such as depressed mood, worthlessness, helplessness, and restless sleep.40 Responses ranged from 0 (rarely or none of the time; less than one day) to 3 (most or all of the time, 5–7 days). A CES-D score of 16 or greater is considered a moderately severe level of depressive symptoms.40 The CES-D measure had a strong internal consistency (α = .84).
Diabetes self-management.
Diabetes self-management was assessed using a survey of diabetes self-management behaviors, and downloaded information from participants’ pedometers and glucometers. The 13-item Self-Care Inventory-Revised (SCI-R)41 assessed perceived self-management adherence such as checking blood glucose levels, eating correct food portions, reading food labels, and keeping clinic appointments. The SCI-R has demonstrated sensitivity to change among adults with T2DM following a 2-month intervention.41 The SCI-R at baseline had an adequate internal consistency (α = .74).
Physical activity.
All physical activity was assessed with wrist-worn MOVABLE pedometers (Brecksville, OH). Pedometers were computer-synced at the beginning of each diabetes class and average steps per day were assessed over a 2-week period at baseline and at 6 months follow-up.
Self-monitoring of blood glucose.
Self-monitoring blood of glucose (SMBG) was assessed by participants using an Ascencia Contour glucometer (Whippany, NJ). Glucometers were distributed to participants during the second week of class and instruction provided on how to test blood glucose. Subsequently, downloaded data were printed in the form of graphs each week and used to enhance participant understanding of blood glucose and the relationship between blood glucose values and food logs, and individual trends in blood glucose throughout the intervention.
Obesity.
Obesity was assessed via BMI, percent body fat, and waist circumference. BMI was calculated using the formula: BMI = (weight [kg])/(height [m]2). Body weight and percent body fat were measured using bio-electrical impedance analysis (Tanita Professional Digital Scale, Model BF350), a valid measure of percent body fat.42 Participants wore street clothes and no shoes; coats and belts were removed. Height was determined using a portable stadiometer (Seca 214). Waist circumference was measured to the nearest .1 cm using a non-stretchable standard tape measure attached to a spring balance, .1 cm above the iliac crest on the horizontal plane.
Diabetes control.
This variable was determined through FBG and A1C concentration, using an aliquot of whole blood from a fasting blood sample measured on a DCA Vantage™ analyzer (Siemens Medical Solutions Diagnostics, Tarrytown, NY). Results are based on a latex agglutination inhibition methodology. The DCA Vantage™ meets the National Glycohemoglobin Standardization Program certification criteria of having a total coefficient of variation < 3% in the clinically relevant range.43
CVD indicators.
These indicators included BPs, cholesterol, and triglycerides. An Omincron model HEM-712C Automatic Inflation BP Monitor (Omincron, Philadelphia, PA) assessed systolic and diastolic BPs. Following a 5-minute rest period, 3 measurements were taken using the participant’s right arm and averaged. Fasting plasma concentrations of total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides were determined by enzymatic methods with a semi-automated chemistry analyzer (Vitros DT60 II; Johnson & Johnson, Rochester, NY).
Intervention
Groups were taught by a team of 2 nurses including an Advanced Clinical Nurse Specialist with Prescriptive Authority (ACNS-BC) and a Public Health Registered Nurse (RN), both members of the African-American community. The ACNS-BC taught 2 small groups in the comparison and experimental conditions. The RN taught the remaining group in each condition; prior to each class the RN observed the ACNS-BC teach the same class to ensure consistency in presentation of class materials. Further, all classes used the same educational materials. Each small group also included one or 2 mentors, individuals from the community with T2DM who had previously participated in our pilot study,19 and whose role was to attend class sessions, provide social support, and occasionally contact participants by phone offering support.
DSME comparison groups.
The comparison groups received a standard diabetes curriculum, outlined in national standards of the American Diabetes Association.44 The scope and sequence of the DSME curriculum is summarized in Table 1.
Table 1.
Overview of DSME Comparison Group
Week 1: Diabetes 101
|
Week 2: Self-Monitoring Blood Glucose
|
Week 3: Healthy Eating
|
Week 4: Healthy Eating
|
Week 5: Medications
|
Week 6: Being Active
|
Week 7: Complications of Diabetes
|
Week 8: Diabetes Self Management
|
Post Intervention: 2 Bi-Weekly Support Groups
|
RB-DSME experimental groups.
The experimental groups received a RB-DSME curriculum integrating resilience and coping strategies with current DSME standards to provide participants the skills to effectively manage their diabetes, both physiologically and psychologically. The scope and sequence of the RB-DSME intervention is summarized in Table 2.
Table 2.
Overview of RB-DSME Experimental Group
Week 1: What is Diabetes?
|
Week 2: Getting Your Glucometer to Work for You
|
Week 3: Carbs Count!
|
Week 4: Eating Made Easy: The Healthy Plate
|
Week 5: A Step Towards Success
|
Week 6: Understanding Medications
|
Week 7: Your Stories of Resilience-based Diabetes Self Care
|
Week 8: Diabetes Self Management: Stay in Charge
|
Post Intervention: 2 Bi-Weekly Support Groups
|
Data Analysis
Baseline demographic characteristics were compared between groups using Pearson’s chi-square analyses; Cramer’s V was calculated as a measure of effect size. For outcome variables, means and standard errors were calculated by group and time. ANCOVAs assessed whether the experimental group improved its outcomes over the 6-month period relative to the comparison group; each ANCOVA included the 6-month follow-up as the outcome, comparison versus experimental status as a categorical factor, and the outcome’s baseline score as a covariate. In this analysis, the F-test captures the extent to which the change in the experimental group’s outcome from baseline to follow-up differed from the change in the comparison group’s outcome at the .05 level of significance. To capture an effect size for the difference, we calculated Cohen’s d based on the model-adjusted follow-up scores for each group (interpreted as .20 = small, .50 = moderate, .80 = large).45
RESULTS
As shown in Table 3, the groups did not significantly differ at baseline (p < .05) in demographic characteristics, and according to conventions for Cramer’s V (.10 = small, .30 = moderate, .50 = large),45 observed group differences were typically small. During the 3-month intervention period, the RB-DSME group tested blood glucose an average of 1.6 times/day, and the DSME group tested blood glucose an average of 1.4 times/day. Regarding feasibility, both the RB-DSME and DSME groups experienced exceptionally high attendance and retention rates, and overall satisfaction with their respective program. Class attendance averaged 95% across both groups, with no participants dropping out during the 3-month intervention period. Program satisfaction on a scale ranging from 1 (extremely dissatisfied) to 7 (extremely satisfied) was high for both the RB-DSME (6.9) and DSME (6.7) groups.
Table 3.
Socio-demographic Characteristics at Baseline by Group
| Comparison (N = 33) | Intervention (N = 32) | |||
|---|---|---|---|---|
| Column % | Column % | χ2 p-value | Cramer’s V | |
| Age | .141 | .290 | ||
| 30 – 44 | 0 | 6.3 | ||
| 45 – 59 | 36.4 | 53.1 | ||
| 60 – 74 | 45.5 | 34.4 | ||
| 75 or above | 18.2 | 6.3 | ||
| Years with Diabetes | .825 | .118 | ||
| 4 or less | 39.4 | 31.3 | ||
| 5 – 9 | 24.2 | 21.9 | ||
| 10 – 14 | 12.1 | 18.8 | ||
| 15 or above | 24.2 | 28.1 | ||
| Sex | .113 | .197 | ||
| Women | 63.6 | 81.3 | ||
| Men | 36.4 | 18.8 | ||
| Marital Status | .358 | .178 | ||
| Married | 36.4 | 37.5 | ||
| Never married | 15.2 | 28.1 | ||
| Sep/Div/Widowed | 48.5 | 34.4 | ||
| Education | .809 | .081 | ||
| High school or less | 27.3 | 31.3 | ||
| Some college | 45.5 | 37.5 | ||
| Bachelors or higher | 27.3 | 31.3 | ||
| Employment Status | .845 | .072 | ||
| Full-time | 21.2 | 25.0 | ||
| Part-time or unemployed | 24.2 | 18.8 | ||
| Retired or disabled | 54.5 | 56.3 | ||
| Household Income | .288 | .241 | ||
| 19,999 or less | 42.4 | 46.9 | ||
| 20,000 – 39,000 | 30.3 | 15.6 | ||
| 40,000 – 59,000 | 21.2 | 18.8 | ||
| 60,000 or above | 6.1 | 18.8 | ||
| Previous DSME | .265 | .138 | ||
| No | 33.3 | 46.9 | ||
| Yes | 66.7 | 53.1 |
Overall, Table 4 shows that the change in the experimental group’s outcomes differed from the change in the comparison group’s outcomes in the hypothesized direction. Differences between groups in changes from baseline to 6 months were statistically significant (p < .05) for diabetes knowledge, positive meaning, FBG, and HDL cholesterol.
Table 4.
Outcome Variables, Descriptives by Group and Time, and ANCOVA Tests
| Comparison (DSME) | Experimental (RB-DSME) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (N = 33) |
Follow-Up (N = 30) |
Baseline (N = 32) |
Follow-Up (N = 31) |
|||||||
| M | SE | M | SE | M | SE | M | SE | F | d | |
| Diabetes Knowledge | 52.42 | 2.29 | 72.92 | 1.94 | 60.16 | 2.51 | 81.05 | 1.43 | 7.80** | .75 |
| Psychological Well-Being | ||||||||||
| Indicators of Resiliene | ||||||||||
| Adaptation to stress | 80.15 | 1.91 | 80.03 | 1.53 | 80.69 | 1.89 | 82.19 | 2.06 | .87 | .24 |
| Coping (%PFC) | .67 | .01 | .67 | .01 | .65 | .01 | .67 | .01 | .70 | .21 |
| Positive meaning | 1.81 | .13 | 1.94 | .11 | 1.66 | .11 | 2.21 | .10 | 5.50* | .61 |
| Positive emotion | 3.63 | .10 | 3.69 | .11 | 3.87 | .12 | 4.06 | .13 | 2.62 | .42 |
| Negative emotion | 1.84 | .09 | 1.72 | .10 | 1.84 | .10 | 1.85 | .12 | 1.25 | .29 |
| Quality of Life | 2.64 | .14 | 2.51 | .10 | 2.28 | .11 | 2.13 | .13 | 1.22 | −.30 |
| Perceived Stress | 15.93 | .98 | 16.40 | 1.02 | 15.56 | 1.33 | 14.10 | 1.14 | 3.05 | −.45 |
| Depressive Symptoms | 15.22 | 1.55 | 13.97 | 1.43 | 14.25 | 1.37 | 12.61 | 1.33 | .19 | −.11 |
| Diabetes Management | ||||||||||
| Steps Per Day | 4482 | 516 | 4943 | 657 | 5189 | 411 | 6331 | 599 | 2.15 | .40 |
| Self-Management | 3.33 | .14 | 3.82 | .11 | 3.25 | .12 | 3.98 | .08 | 3.63 | .50 |
| Obesity | ||||||||||
| BMI | 34.27 | 1.22 | 34.28 | 1.21 | 39.65 | 1.67 | 38.92 | 1.73 | .33 | −.15 |
| % Body Fat | 41.08 | 1.52 | 39.23 | 1.60 | 45.46 | 1.46 | 43.94 | 1.44 | 1.51 | .32 |
| Waist Circumference | 103.59 | 2.30 | 105.01 | 2.02 | 116.84 | 2.81 | 114.47 | 2.92 | 3.06 | −.48 |
| Diabetes Control | ||||||||||
| FBG | 135.06 | 8.23 | 131.73 | 9.86 | 140.25 | 9.53 | 113.06 | 5.62 | 5.19* | −.59 |
| A1C | 7.12 | .24 | 7.23 | .34 | 7.29 | .31 | 6.95 | .22 | 1.04 | −.27 |
| CVD-Indicators | ||||||||||
| Systolic BP | 143.09 | 3.12 | 138.50 | 3.78 | 134.69 | 3.66 | 127.74 | 3.41 | 1.80 | −.35 |
| Diastolic BP | 83.88 | 2.28 | 79.87 | 2.82 | 79.56 | 2.13 | 75.35 | 1.87 | .45 | −.18 |
| LDL Cholesterol | 104.47 | 6.69 | 95.43 | 6.66 | 93.27 | 6.83 | 81.04 | 4.95 | 2.97 | −.47 |
| HDL Cholesterol | 48.59 | 2.72 | 44.07 | 2.89 | 49.72 | 3.50 | 56.73 | 3.03 | 9.96** | .84 |
| Triglycerides | 102.88 | 8.51 | 102.83 | 7.91 | 112.06 | 7.65 | 127.53 | 12.73 | 2.83 | .45 |
| Total Cholesterol | 175.19 | 7.00 | 157.57 | 6.92 | 169.84 | 6.22 | 160.81 | 5.69 | .69 | .22 |
Note.
F, p, and d results from ANCOVA.
p < .05,
p < .01
Positive entries for Cohen’s d denote the RB-DSME group scores increased more strongly than did the DSME group, while negative entries denote the RB-DSME group scores declined more strongly than did the DSME group.
DISCUSSION
This study examined the potential feasibility and effectiveness of an experimental group receiving a RB-DSME intervention and a comparison group receiving standard DSME at 6 months post-study entry. With regard to feasibility, both the RB-DSME and DSME groups experienced high attendance and retention rates and overall satisfaction with the program. We attribute the high attendance rates to the investigators’ cultural competency, 5-year involvement in the community, and use of key community leaders and mentors to establish trust, participant involvement, and continued follow-up. In particular, support from church pastors and community leaders enhanced participation. The convenient location of classes in church and neighborhood community centers where participants regularly spent time enhanced comfort and ease of attendance. Further, both groups used culturally appropriate learning methods such as story-telling, peer mentors for support, and including family members as desired.25–31 Taken together, the overall program satisfaction and high attendance and retention rates emphasize the critical importance of the investigators’ engagement in the community, and provides evidence for the feasibility of the RB-DSME intervention.
With regard to the potential effectiveness of the RB-DSME intervention, it is noteworthy that we found statistically significant improvements in diabetes knowledge, positive meaning, HDL cholesterol, and FBG compared to the DSME group. Broadly, this highlights the RB-DSME’s potential to have a favorable impact on the psychological and physiological health in patients with T2DM. Although diabetes knowledge increased for both groups, the change was significantly greater in the RB-DSME group. A possible explanation is that participants in the RB-DSME intervention group took greater responsibility for their education, a central component of resilience that was emphasized throughout the course. However, given the low internal consistency of the diabetes knowledge measure in the current study, this finding should be interpreted with caution, and future research should explore more culturally appropriate and reliable knowledge measures for African-American adults with T2DM. An alternative explanation, given that the reliability (α = .71) was sufficient in the original study32 is that participant fatigue played a factor in the current study.
In terms of psychological health, the findings from the RB-DSME intervention suggest that the ability to find positive meaning in the context of the disease improves self-management behaviors and prevents or delays the progression of the disease. Those in the RB-DSME group significantly enhanced their ability to find positive meaning and learned from their experiences with T2DM compared to the DSME group. Importantly, in addition to addressing diabetes risks and vulnerabilities, the RB-DSME curriculum focused on identifying and fostering strengths that support healthy behaviors. Participants were taught how to reframe stressful situations as opportunities for personal growth and for taking positive behavioral steps. Group members reflected on difficult situations, shared their struggles openly with other group members, and took the time to reframe their thinking and recommit to their T2DM health-related goals. We speculate that frequently reframing difficult situations into opportunities for growth, and noticing small positive behavioral steps enhanced a belief in their ability to take greater responsibility and positively affect their life circumstances and the progression of the disease. Limited support for this speculation is the increase in diabetes self-management for the RB-DSME group compared to the DSME group.
In terms of physiological health, we observed significant improvements in 2 markers reflecting T2DM disease progression: FBG and HDL cholesterol. FBG, a key physiological marker of T2DM, decreased significantly in the group receiving the RB-DSME compared to the DSME group. The RB-DSME group began with an average FBG of 140 mg/dl and decreased to 113 mg/dl, thus potentially helping to halt the persistent buildup of damage and the resulting complications from the disease. In contrast, the DSME group decreased only marginally, from 135 to 131 mg/dl. Given that the cutoff between pre-diabetes and diabetes is 125 mg/dl,46 this change represents a meaningful clinical difference. HDL cholesterol also increased significantly in the intervention group vis-à-vis the comparison group, demonstrating an additional physiological protective effect. HDL catabolism is related to insulin resistance even in non-diabetic individuals,47 so increasing HDL cholesterol – in concert with lowering blood glucose – helps triangulate the physiological improvements seen in the RB-DSME group.
With respect to a major marker for diabetes control, A1C, the difference between the groups was not statistically significant. However, when evaluating interventions in diseased samples, it can be important to look beyond statistically significant results, and consider clinically relevant outcomes. At 6 months follow-up 71% of the RB-DSME participants met the American Diabetes Association goal of A1C less than 7%,48 compared to 60% in the comparison group. Given that the intervention group’s A1C was higher at baseline and lower at 6 months’ post-program, this finding suggests that the RB-DSME may be useful in reducing the number of patients with clinically significant elevations in A1C. From a practical standpoint, this clinical relevance provides further support of the RB-DSME and suggests a full-scale randomized trial is warranted.
With respect to indicators of resilience, given that finding positive meaning was the only statistically significant resilience indicator, our finding suggests that future research should focus primarily on helping participants find positive meaning within the context of living with T2DM. Although the resilience indicator, adaptation to stress (ie, CD-RISC), increased in the expected direction for the RB-DSME group, it was not a statistically significant change compared to the DSME group. One explanation for this finding is that similar to our previous pilot study,19 the resilience mean scores in the current study were uniformly high at baseline and 6 months (81 and 82, respectively). Several resilience scholars have noted an urgent need to better understand resilience experiences among African Americans, as they are an understudied group relative to Whites. Teti et al49 describe 5 categories of resilience as expressed by low-income African-American men including: (1) perseverance and refusing to quit despite tremendous challenges; (2) a commitment to learning and growing from hardships; (3) using reflection and refocusing their planning and efforts to address life difficulties; (4) creating a positive and supportive environment that includes community, family and self; and (5) drawing on one’s religion and/or spirituality to gather the necessary strength to overcome adversities. Unlike the commonly accepted definition that resilience involves a good outcome despite an acute threat to adaptation or development,33,50 resilience in the African-American community has been described more akin to a coping strategy used to combat daily chronic stressors, such as poverty or racism. Too often, despite an impressive resolve to succeed, good outcomes are not achieved.49 As such, Ungar51 describes a model of resilience as one’s capacity to seek health-sustaining resources, while simultaneously living in an environment where resources are available and easily accessed in culturally meaningful ways.
This broader perspective of resilience was reflected by participants in our program who described resilience similarly to that of Ungar’s51 and Teti et al’s49 “I’m a keep rising. I’m a keep going forward, regardless.” Perhaps participants’ high attendance and satisfaction with the RB-DSME intervention reflected the program’s success in creating a resilience-promoting environment that matched participants’ individual efforts to combat daily chronic stressors, and improve their lives and their health. We suspect that this resilience-promoting environment helped account for the significant finding for the resilience indicator ‘positive meaning’ within the context of living with T2DM. Nonetheless, future work is needed to address the broader social-structural inequities that make it harder for African Americans to achieve desirable outcomes.49,51
Limitations
Our findings should be considered in light of several limitations. First, we used a quasi-experimental design; thus, participants were not randomly selected from the population, a process that is often not feasible in social science research. Therefore, the sample may not be representative of the population from which it was drawn, which has implications for generalizability of the results. Second, the use of self-report survey data has inherent limitations, like the potential for untruthful or inaccurate responses due to lack of self-awareness or fatigue. To enhance the validity of survey responses, survey items were read to participants needing assistance, reading glasses were provided as needed, and water and healthy snacks were available. Third, whereas comparable to some intervention studies, the sample size was relatively small and may have contributed in some instances to the lack of significant findings due to lack of power. Nevertheless, the study documented the potential feasibility and effectiveness of the RB-DSME to enhance diabetes knowledge, positive meaning, and HDL cholesterol, and decrease FBG. Furthermore, participant satisfaction was greater for the RB-DSME compared with the DSME group, although it was high for both groups, perhaps due to the cultural responsiveness of both conditions. Fourth, this study involved only African Americans with T2DM; therefore, the results may not generalize to other ethnicities or health statuses. However, examining the health in African-American adults with T2DM is valuable, as this population is an underserved population, yet one that bears a disproportionate T2DM burden.1,2
Conclusions
If recent trends continue, over 25% of Americans will have diabetes by 2050, with higher rates expected for racial minority adults.52 The current study demonstrated the potential feasibility and effectiveness of the RB-DSME intervention to enhance the health of African-American adults with T2DM. We did not experience difficulty in recruiting participants to be in the study, and adherence and satisfaction with the program were exceptionally high. Infusing the resilience strategy of finding positive meaning within the context of living with T2DM into standard DSME in church and community settings may enhance the ability of African Americans to manage T2DM more effectively, and thus, avoid its serious consequences. Given that diabetes is one of the most psychologically and behaviorally demanding chronic diseases,7 adults with T2DM are more likely to benefit from resilience-based interventions that help them gain the necessary skills and mindset to effectively manage the disease.
Acknowledgments
The project described was supported by Award Number R34DK085218 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDDK or the National Institutes of Health.
Footnotes
Conflict of Interest Statement
The authors declare no conflict of interest.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Washington, DC: US Department of Health and Human Services; 2014. [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit B, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. [DOI] [PubMed] [Google Scholar]
- 3.Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444(7121):840–846. [DOI] [PubMed] [Google Scholar]
- 4.Buse JB, CORD Study Group. Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: design and methods. Am J Cardiol. 2007;99(12):S21–S33. [DOI] [PubMed] [Google Scholar]
- 5.Poirier P, Giles TD, Bray GA. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss an update of the 1997 American Heart Association scientific statement on obesity and heart disease from the obesity committee of the council on nutrition, physical activity, and metabolism. Circulation. 2006;113(6):898–918. [DOI] [PubMed] [Google Scholar]
- 6.Boyle SH, Helms MJ, Surwitt RS, et al. Depressive symptoms, race, and glucose concentrations. Diabetes Care. 2007;30(10):2484–2488. [DOI] [PubMed] [Google Scholar]
- 7.Schnittker J, McLeod JD. The social psychology of health disparities. Annu Rev Sociol. 2005;31(1):75–103. [Google Scholar]
- 8.Reeves WC, Strine TW, Pratt LA, et al. Mental illness surveillance among adults in the United States. MMWR Surveill Summ. 2011;60(Suppl 3):1–29. [PubMed] [Google Scholar]
- 9.Katon W, Russo J, Lin EH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medication adherence or lack of treatment intensification? Psychosom Med. 2009;71(9):965–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer; 1984. [Google Scholar]
- 11.O’Leary VE, Ickovics JR. Resilience and thriving in response to challenge: An opportunity for a paradigm shift in women’s health. Womens Health. 1995;1(2):121–142. [PubMed] [Google Scholar]
- 12.Carver CS. Resilience and thriving: Issues, models, and linkages. J Soc Issues. 1998;54(2):245–266. [Google Scholar]
- 13.Burton NW, Pakenham KI, Brown WJ. Evaluating the effectiveness of psychosocial resilience training for heart health, and the added value of promoting physical activity: a cluster randomized trial of the READY program. BMC Public Health. 2009;9(1):427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friborg O, Sorlie T, Rosenvinge JH. Breast cancer: a manual for a proposed group treatment integrating evidence based resilience factors. Psychol Rep. 2005;97(1):77–97. [DOI] [PubMed] [Google Scholar]
- 15.Ong AD, Bergeman CS, Bisconti TL, et al. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J Pers Soc Psychol. 2006;91(4):730–739. [DOI] [PubMed] [Google Scholar]
- 16.Yi JP, Vitaliano PP, Smith RE, et al. The role of resilience on psychological adjustment and physical health in patients with diabetes. Brit J Health Psych. 2008;13(2):311–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yi-Frazier JP, Smith RE, Vitaliano PP, et al. A person-focused analysis of resilience resources and coping in patients with diabetes. Stress Health. 2009;26(1):51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bradshaw BG, Richardson GE, Kumpfer K, et al. Determining the efficacy of a resiliency training approach in adults with type 2 diabetes. Diabetes Educ. 2007;33(4):650–659. [DOI] [PubMed] [Google Scholar]
- 19.Steinhardt MA, Mamerow MM, Brown SA, Jolly CA. A resilience intervention in African American adults with type 2 diabetes: a pilot study of efficacy. Diabetes Educ. 2009;35(2):274–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Steinhardt MA, Dubois SK, Brown SA, et al. Positivity and indicators of health among African Americans with diabetes. Am J Health Behav. 2015;39(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clinical Diabetes. 2004;22(3):123–127. [Google Scholar]
- 22.Ammerman A, Washington C, Jackson B, et al. The PRAISE! Project: a church-based nutrition intervention designed for cultural appropriateness, sustainability, and diffusion. Health Promot Pract. 2002;3(2):286–301. [Google Scholar]
- 23.Samuel-Hodge CD, Keyserling TC, France R, et al. A church-based diabetes self-management education program for African Americans with type 2 diabetes. Prev Chronic Dis. 2006;3(3):1–16. [PMC free article] [PubMed] [Google Scholar]
- 24.Samuel-Hodge CD, Keyserling TC, Park S, et al. A randomized trial of a church-based diabetes self-management program for African Americans with type 2 diabetes. Diabetes Educ. 2009;35(3):439–454. [DOI] [PubMed] [Google Scholar]
- 25.Ard JD, Durant RW, Edwards LC, Svetkey LP. Perceptions of African-American culture and implications for clinical trial design. Ethnic Dis. 2005;15(2):292–299. [PubMed] [Google Scholar]
- 26.Corbie-Smith G, Thomas SB, St. George DM. Distrust, race, and research. Arch Intern Med. 2002;162(21):2458–2463. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy BM, Ard JD, Harrison L, et al. Cultural characteristics of African Americans: implications for the design of trials that target behavior and health promotion programs. Ethnic Dis. 2007;17(3):548–554. [PubMed] [Google Scholar]
- 28.Campbell MK, Hudson MA, Resnicow K, et al. Church-based health promotion interventions: evidence and lessons learned. Annul Rev Public Health. 2007;28:213–234. [DOI] [PubMed] [Google Scholar]
- 29.Brody GH, Kogan SM, Murry VM, et al. Psychological functioning, support for self-management, and glycemic control among rural African American adults with diabetes mellitus type 2. Health Psychol. 2008;27(1):S83–S90. [DOI] [PubMed] [Google Scholar]
- 30.Samuel-Hodge CD, Headen SW, Skelly AH, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: spirituality, the multi-caregiver role, and other social context factors. Diabetes Care. 2000;23(7):928–933. [DOI] [PubMed] [Google Scholar]
- 31.Boltri HM, Davis-Smith YM, Zayas LE, et al. Developing a church-based diabetes prevention program with African Americans. Diabetes Educ. 2006;32(6):901–909. [DOI] [PubMed] [Google Scholar]
- 32.Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21(5):706–710. [DOI] [PubMed] [Google Scholar]
- 33.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. [DOI] [PubMed] [Google Scholar]
- 34.Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. [DOI] [PubMed] [Google Scholar]
- 35.Vitaliano PP, Maiuro RD, Russo J. Raw versus relative scores in the assessment of coping strategies. J Behav Med. 1987;10(1):1–18. [DOI] [PubMed] [Google Scholar]
- 36.Frederickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol. 2003;84(2):365–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. [DOI] [PubMed] [Google Scholar]
- 38.Fitzgerald JT, Davis WK, Connell CM, et al. Development and validation of the diabetes care profile. Eval Health Prof. 1996;19(2):209–231. [DOI] [PubMed] [Google Scholar]
- 39.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 40.Radloff LS. The Center for Epidemiologic Studies Depression Index. Appl Psych Meas. 1977;1(3):385–401. [Google Scholar]
- 41.Weinger K, Butler HA, Welch GW, La Greca AM. Measuring diabetes self-care: a psychometric analysis of the self-care inventory-revised with adults. Diabetes Care. 2005;28(6):1346–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baumgartner RN. Electrical impedance and total body electrical impedance for the measurements of percent body fat. In Roche AF, Heymsfield SB, Lohman TG, eds. Human Body Composition. Champaign, IL: Human Kinetics; 1996:79–107. [Google Scholar]
- 43.Lenters-Westra E, Slingerland RJ. Six of eight hemoglobin A1c point-of-care instruments do not meet the general accepted analytical performance criteria. Clin Chem. 2010;56(1):44–52. [DOI] [PubMed] [Google Scholar]
- 44.Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Care. 2014;37(Suppl 1):S144–S153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cohen J Statistical Power Analyses for the Behavioral Sciences. New York, NY: Erlbaum; 1988. [Google Scholar]
- 46.American Diabetes Association. Diagnosing diabetes and learning about prediabetes (on-line). Available at: http://www.diabetes.org/diabetes-basics/diagnosis/. Accessed October 20, 2014.
- 47.Pont F, Duvillard L, Florentin E, et al. High-density lipoprotein apolipoprotein AI kinetics in obese insulin resistant patients. an in vivo stable isotope study. Int J Obes Relat Metab Disord. 2002;26(9):1151–1158. [DOI] [PubMed] [Google Scholar]
- 48.American Diabetes Association. Standards for medical care in diabetes. Diabetes Care. 2014;37(Suppl 1):S14–S80. [DOI] [PubMed] [Google Scholar]
- 49.Teti M, Martin AE, Ranade R, et al. “I’m a keep rising. I’m a keep going forward, regardless”: exploring black men’s resilience amid sociostructural challenges and stressors. Qual Health Res. 2012;22(4):524–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Masten A Ordinary magic, resilience process in development. Am Psychol. 2001;56(3):227–238. [DOI] [PubMed] [Google Scholar]
- 51.Ungar M Resilience across cultures. Brit J Soc Work. 2008;38(2):218–235. [Google Scholar]
- 52.Boyle JP, Thompson TJ, Gregg EW, et al. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]


