Abstract
Objective:
To compare the dentoskeletal effects of rapid (RME) and slow (SME) maxillary expansion in patients with bilateral complete cleft lip and palate (BCLP).
Materials and Methods:
This was a secondary analysis of a previous randomized controlled trial (RCT). Forty-six patients (34 male, 12 female) with BCLP and posterior crossbite (mean age of 9.2 years) were randomly assigned to two study groups. Group RME comprised subjects treated with Haas/Hyrax expander. Group SME included patients treated with quad-helix appliance. Cone-beam computed tomography (CBCT) was performed before expansion (T1) and after appliance removal at the end of a 6-month retention period (T2) for a previous RCT that compared the transverse skeletal effects of RME and SME. CBCT-derived cephalometric images were generated and cephalometric analysis was performed using Dolphin Imaging Software (Chatsworth, Calif). Intergroup comparisons were performed using t tests (P < .05).
Results:
Baseline forms were similar between groups. No significant differences between RME and SME groups were found.
Conclusions:
Rapid and slow maxillary expansion produced similar sagittal and vertical changes in patients with BCLP. Both Haas/Hyrax and quad-helix appliances can be used in patients with vertical facial pattern. Clinical relevance: RME and SME can be equally indicated in the treatment of maxillary arch constriction in patients with BCLP.
Keywords: Palatal expansion technique, Cephalometry, Cleft lip and palate
INTRODUCTION
Rehabilitation of individuals with complete cleft lip and palate starts right after birth.1 Lip and palate repairs are performed in the first months and years of life, respectively.1–3 At the same time that the primary surgeries repair lip and palate morphology, a side effect of maxillary growth restriction is frequently observed.2–7 Individuals with complete bilateral cleft lip and palate (BCLP) show, at birth, enlarged anteroposterior and transverse maxillary dimensions.5,6 After primary lip and palate repairs, soft tissue traction and scar fibrosis produce medial displacement of the palatal segments, frequently causing maxillary transverse constriction and posterior crossbites.6,8–10 At the same time, significant reduction of the overjet occurs, due to retrusion of the premaxilla.11
In patients with BCLP, correction of maxillary constriction is usually performed before the secondary alveolar bone graft procedure.1 Expansion improves the maxillary arch morphology and causes the segmental alignment creating appropriate conditions for bone graft surgery.1,12 Maxillary expansion also corrects posterior crossbites.1,4,13,14 In general, two therapeutic options are available for maxillary expansion in patients with complete cleft lip and palate: rapid maxillary expansion (RME) with Hyrax or Haas-type appliances, and slow maxillary expansion (SME) with quad-helix appliance.1,4,13–16
Brunetto et al.17 compared the results of RME and SME in noncleft patients. The authors used Haas appliance for both modalities of expansion and used different expansion protocols of activation. RME showed more buccal tipping of the anchorage teeth than SME. Slow expansion caused significant buccal alveolar bone loss at the molar region. Medeiros Alves et al.18 compared rapid and slow maxillary expansion in patients with BCLP by means of digital dental models. Arch widths and perimeter were significantly increased with both expanders.18 No differences were observed between RME and SME except for the capability of the quad-helix in promoting differential expansion in the anterior and posterior regions, and a shorter treatment time for the RME therapy.18 Recently, Almeida et al.19 compared the skeletal effects of rapid and slow maxillary expansion in BCLP using pre-expansion and postretention cone-beam computed tomography (CBCT). Haas/Hyrax and Quad-helix type appliances similarly promoted significant increases in all the measured maxillary transverse dimensions at the premolar and molar regions.19 Similar orthopedic effects with decreasing transverse gains from the alveolar crest level to the nasal cavity were observed for both appliances.19 The authors also reported similar buccal bone inclination of the anchorage teeth for both appliances, without significant periodontal bone changes in the mixed dentition.19
Anteroposterior and vertical outcomes of maxillary expansion are also relevant for selecting the expander type. No previous study, however, compared the anteroposterior and vertical cephalometric effects of RME and SME in patients with complete cleft lip and palate. Considering that patients with BCLP show predominantly a hyperdivergent facial pattern, investigations of the vertical effects of maxillary expansion procedures become relevant.3 Previous randomized controlled trials18,19 have compared the transverse effects of RME and SME providing study material for the current cephalometric comparison. Therefore, the purpose of this study was to compare the sagittal and vertical dentoskeletal cephalometric effects of rapid and slow maxillary expansion in patients with complete bilateral cleft lip and palate. The null hypothesis was that there would be no difference in the sagittal and vertical dentoskeletal effects between Haas/Hyrax and quad-helix expanders.
MATERIALS AND METHODS
Trial Design
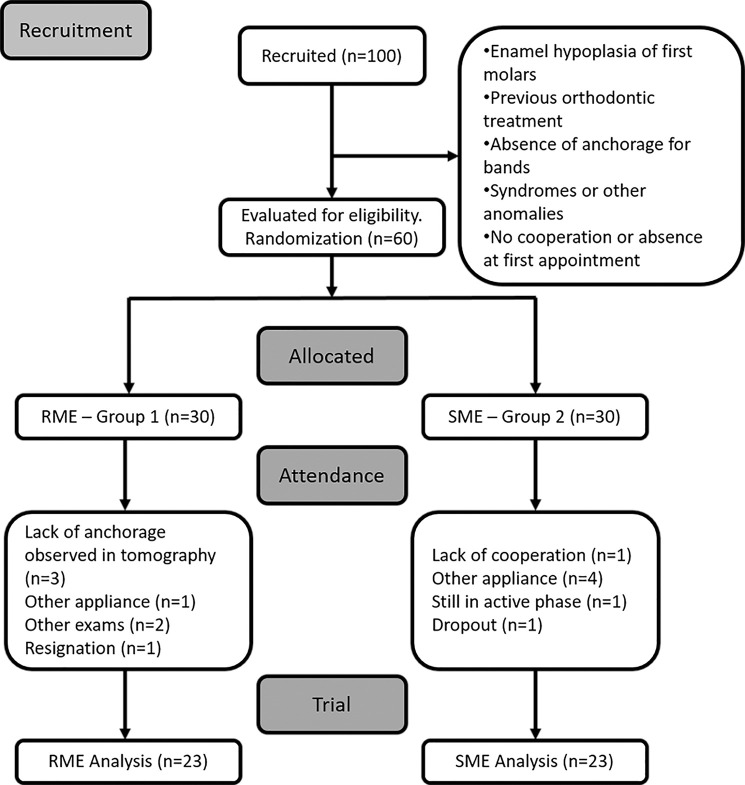
This paper was developed according to the CONSORT (Consolidated Standards of Reporting Trials) statements. It consists in a blind secondary data analysis from a previous randomized controlled trial (RCT) with a 1:1 allocation ratio design, explained in the flowchart (Figure 1).19 It was not necessary to make any changes after trial commencement.
Figure 1.
Flowchart steps of the sample distribution.
Participants, Eligibility Criteria, and Setting
The study was approved by the ethical committee of the Hospital for Rehabilitation of Craniofacial Anomalies (protocol number CAAE: 41327415.2.0000.5441).
One hundred patients with bilateral cleft lip and palate from 8 to 10 years of age were recruited from September 2011 to September 2013 for a previous study.18 Sixty patients attended the appointment. Written informed consent was obtained from participants' parents or legal guardians before their recruitment.
Eligibility criteria were: (1) middle or late mixed dentition; (2) both sexes; (3) lip repair performed between 3 and 6 months of age and palate repair performed between 12 and 24 months of age; (4) presence of maxillary constriction and need for maxillary expansion previous to the secondary bone graft; (5) permanent first molars without extensive restorations; (6) good periodontal health; (7) no previous orthodontic treatment; and (8) absence of syndromes or other craniofacial anomalies. Exclusion criteria were: (1) early loss of both first and second maxillary deciduous molars on the same side; and (2) previous secondary alveolar bone grafting. Forty-six patients (34 male; 12 female) were selected according to the inclusion and exclusion criteria (Figure 1).
Interventions
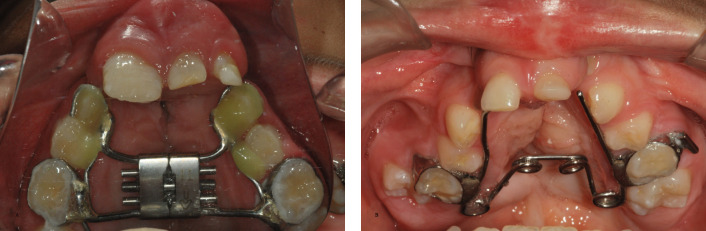
Clinical procedures/interventions were performed by two orthodontic residents under the supervision of two experienced orthodontists of the institution during the period from October of 2011 to February of 2014. The RME group included 23 patients (16 male; seven female) with a mean age of 9.25 years (SD = 1.35), who received maxillary expansion with the Haas-type or Hyrax appliance (Figure 2A). Bands were preferentially adapted on maxillary first permanent molars. When second deciduous molars were banded, a lingual extension wire was placed to the partially erupted maxillary first permanent molar. C-shape clasps were bonded on the deciduous canines. The 11-mm screw (Dentaurum, Ispringen, Germany) was activated two turns twice a day (1 mm/d) until overcorrection. The expansion active phase ranged from 7 to 14 days. The appliance was maintained as a retainer for 5 months. The mean amount of expansion was 5.11 mm (SD = 2.74) for the intercanine (3-3) and 3.53 mm (SD = 2.73) for the intermolar (6-6) regions.18
Figure 2.
Hyrax expander (A) and quad-helix appliance (B).
The SME group included 23 patients (18 male; five female) with a mean age of 9.15 years (SD = 0.99) who received the Quad-helix appliance (Figure 2B). Bands were preferentially adapted on the first permanent molars, or on the second deciduous molars when the first permanent molars were partially erupted. The appliance was constructed using 0.036-inch round stainless steel wire. Activations were performed extraorally at installation and every 60 days until overcorrection. The amount of activation for each appointment was 6 mm in the anterior and posterior regions. The active expansion phase ranged from 4 to 21 months with a mean time of 11 months. For both groups, the overcorrection criterion was occlusion between the palatal cusps of the maxillary teeth and the buccal cusps of the mandibular teeth. The appliance remained in the mouth as a retainer during 5 months after the active phase. The mean amount of expansion was 6.58 mm (SD = 3.58) for the intercanine (3-3) and 3.98 mm (SD = 2.41) for the intermolar (6-6) regions.18
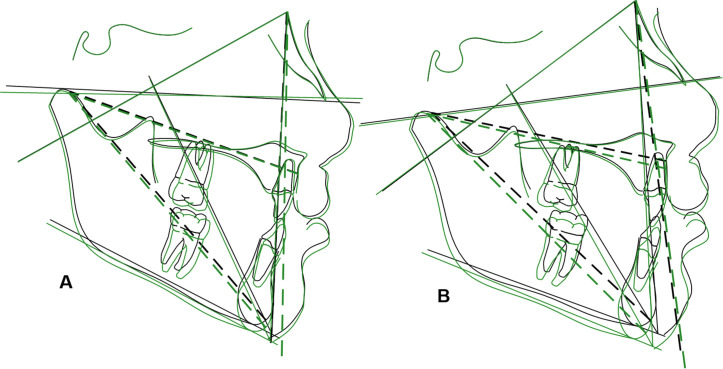
CBCT was performed using the i-CAT machine (Imaging Sciences International, Hartfield, Pa) immediately before expansion (T1) and after the retention period, when the expander was removed (T2). The CBCT exams were taken for a dentoskeletal evaluation previously published.19 All CBCT scans were taken with 120 kVp, 8 mA, 26.9 s of exposure time, FOV of 13 cm and a 0.25 mm voxel size. For this study, lateral cephalometric images were reformatted using Dolphin software (Chatsworth, Calif). The head position was standardized with the Frankfurt plane parallel to the horizontal plane in a lateral view. In a frontal view, the infraorbital plane was positioned parallel to the horizontal plane. In the axial plane, the ethmoidal septum was positioned parallel to the vertical plane. Cephalometric measurements are shown in Figures 3 and 4. During the analysis, the examiner was blinded.
Figure 3.
Cephalometric angular variables measured in the study: (1) SNA, (2) SNB, (3) ANB, (4) SNGoGn, (5) FMA, (6) IMPA, (7) U1.PP, (8) Nasolabial Angle, (9) NA.APog.
Figure 4.
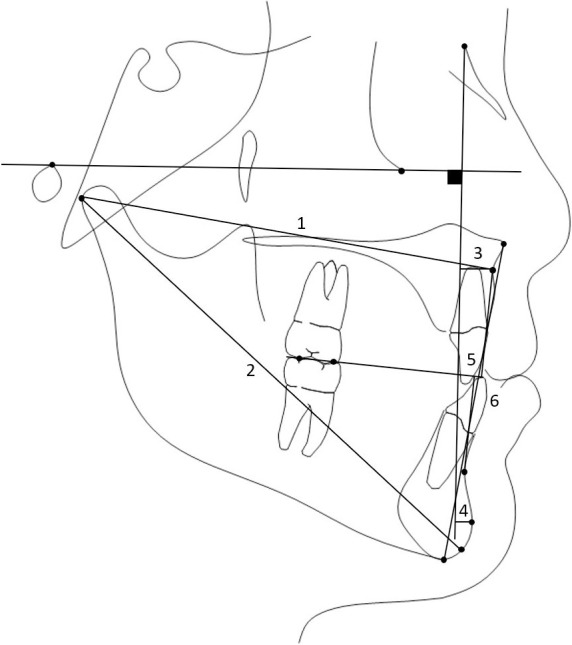
Cephalometric linear variables measured in the study: (1) Co - A, (2) Co-Gn, (3) A-Nperp, (4) Pog-Nperp, (5) Wits, (6) LAFH.
Outcomes
The outcomes evaluated in this study were sagittal and vertical cephalometric changes of RME and SME in children with BCLP.
Sample Size Calculation
To detect a minimum intergroup difference in vertical growth (SN.GoGn) of 2°, with a standard deviation of 1.7°,20 with an alpha error of 5% and a test power of 80%, a sample of 22 patients was required for each group.
Randomization, Allocation Concealment, and Implementation
Computer-generated randomization based on random permute blocks of 20 patients was accomplished using Stata Software (StataCorp, College Station, Tex) to ensure equal distribution of participants in the groups. Allocation concealment was achieved with sequentially sealed, numbered, opaque envelopes containing the expansion modality allocation cards, which were prepared before the trial. One operator was responsible for opening the next envelope in sequence and implementing the randomization process.18
Blinding
Blinding of patients and operator was not possible regarding the modality of expansion; however, the outcome assessment was blinded because CBCT-derived cephalometric images were unidentified during analysis.
Error Study
The same examiner repeated the measurements in 50% of the sample after a 30-day interval. The examiner did not participate in any of the clinical activities nor in the randomization process. Reliability was calculated using Intraclass Correlation Coefficient (ICC).21
Statistical Analyses
Normal distribution of variables was verified using Kolmogorov-Smirnov tests. Intergroup comparison was performed with t tests. The level of significance used for all the tests of the study was 5%, with an associated 95% confidence interval. Statistical analyses were performed with Statistica software, version 11.9 (StatSoft Inc., Tulsa, Okla).
RESULTS
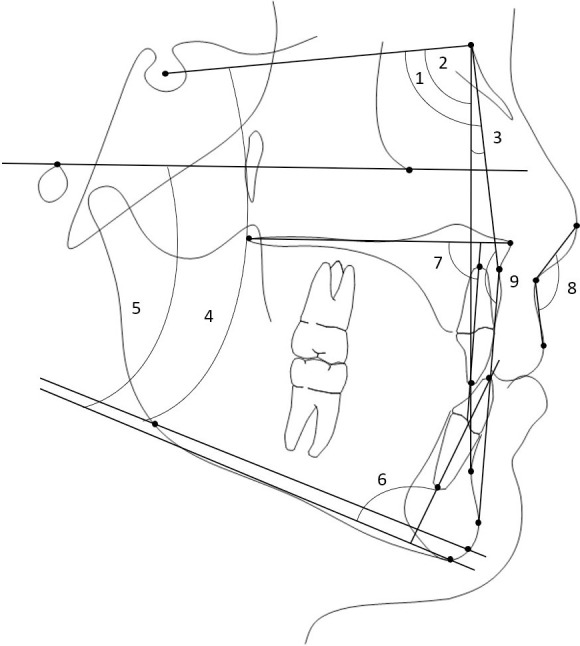
Participant flow, baseline data, numbers analyzed for each outcome and harms were previously reported.18,19 Intraexaminer agreement was considered excellent (ICC > 0.75), varying from 0.88 to 1.00. There were no intergroup differences in the starting forms (Table 1). There were no significant intergroup treatment changes (Table 2). Figure 5 illustrates superimpositions of the average cephalometric tracings before (T1) and after (T2) expansion, for the RME and the SME groups. No cases of damage were observed.
Table 1.
Intergroup Comparison at T1 (t Tests)
| Variables |
RME Group |
SME Group |
|||
| Mean |
SD |
Mean |
SD |
P Value |
|
| Maxillary skeletal components | |||||
| SNA | 81.68 | 3.89 | 81.81 | 3.80 | .913 |
| A-Nperp | 4.11 | 4.01 | 2.83 | 4.47 | .322 |
| Co-A | 84.21 | 5.08 | 84.52 | 3.73 | .816 |
| Mandibular skeletal components | |||||
| SNB | 74.79 | 4.42 | 74.77 | 4.23 | .990 |
| Pog-Nperp | −4.04 | 7.07 | −7.54 | 8.58 | .150 |
| Co-Gn | 105.68 | 5.43 | 105.73 | 6.01 | .977 |
| Maxillomandibular relationship | |||||
| ANB | 6.89 | 2.72 | 7.04 | 2.81 | .860 |
| Wits | 3.73 | 4.41 | 1.04 | 4.46 | .051 |
| Max/Mand Diff. | 21.17 | 4.76 | 21.01 | 4.42 | .907 |
| NAPog | 14.73 | 6.07 | 14.16 | 6.79 | .774 |
| Vertical component | |||||
| SNGoGn | 36.84 | 5.35 | 38.2 | 5.29 | .403 |
| FMA | 27.22 | 5.28 | 29.96 | 4.88 | .081 |
| LAFH | 64.11 | 5.38 | 67.06 | 6.28 | .104 |
| Maxillary dentoalveolar components | |||||
| U1.PP | 79.90 | 19.26 | 82.81 | 10.29 | .530 |
| Mandibular dentoalveolar components | |||||
| IMPA | 86.91 | 8.21 | 85.54 | 7.07 | .557 |
| Soft tissue profile | |||||
| Nasolabial angle | 117.39 | 13.00 | 120.12 | 12.88 | .492 |
Table 2.
Intergroup Comparisons for Expansion Changes (t Tests)
| Variables |
Hyrax (T2-T1) |
Quad-helix (T2-T1) |
Diff. |
P Value |
||
| Mean |
SD |
Mean |
SD |
|||
| Maxillary skeletal components | ||||||
| SNA | −0.09 | 1.76 | −0.74 | 1.88 | 0.66 | .238 |
| A-Nperp | −0.19 | 2.95 | −0.67 | 1.93 | 0.49 | .516 |
| Co-A | 0.19 | 2.90 | 0.10 | 3.48 | 0.09 | .930 |
| Mandibular skeletal components | ||||||
| SNB | −0.07 | 1.84 | −0.09 | 2.10 | 0.02 | .974 |
| Pog-Nperp | −1.00 | 5.51 | −0.58 | 4.34 | 0.41 | .783 |
| Co-Gn | 1.91 | 2.55 | 2.82 | 2.74 | 0.92 | .258 |
| Maxillomandibular relationship | ||||||
| ANB | −0.02 | 2.11 | −0.64 | 1.36 | 0.62 | .245 |
| Wits | −0.87 | 2.56 | −0.17 | 2.24 | 0.70 | .340 |
| Max/Mand Diff. | 1.77 | 2.66 | 2.91 | 3.03 | 1.15 | .191 |
| NAPog | −0.84 | 4.33 | −0.33 | 3.72 | 0.51 | .680 |
| Vertical component | ||||||
| SNGoGn | 0.74 | 3.49 | 1.03 | 2.84 | 0.29 | .765 |
| FMA | 1.09 | 4.12 | 0.72 | 3.34 | 0.37 | .742 |
| LAFH | 2.77 | 5.83 | 1.56 | 5.75 | 1.21 | .492 |
| Maxillary dentoalveolar components | ||||||
| U1.PP | −0.89 | 6.66 | 1.71 | 5.75 | 2.60 | .179 |
| Mandibular dentoalveolar components | ||||||
| IMPA | −0.09 | 4.01 | −0.21 | 4.57 | 0.12 | .928 |
| Soft tissue profile | ||||||
| Nasolabial angle | 1.42 | 7.48 | 0.8 | 8.11 | 0.63 | .793 |
Figure 5.
Superimposition (S-N on S) of the average cephalometric tracings of each group, at each stage of the study. (A) Superimposition of T1 (black) and T2 (green) for RME group. (B) Superimposition of T1 and T2 for SME group.
DISCUSSION
Main Findings in the Context of the Existing Evidence
CBCT-derived cephalograms have been widely studied and used in orthodontics.22–26 The method using cephalometric reconstruction from CBCT images showed overall landmark identification errors comparable with conventional digital cephalograms and improvement in the accuracy of cephalometric measurements.22,27 Patients from this study had pre-existing CBCTs taken for a previous RCT, so CBCT-derived cephalograms were used to eliminate the radiation exposure associated with additional conventional radiographs.
Changes in the anteroposterior position of the maxilla may occur after expansion in noncleft patients.25,28 In patients with UCLP, no anterior maxillary displacement was found when the Hyrax appliance was used.23 In patients with BCLP, arch length showed a slight decrease after expansion due to premaxillary retrusion.18,19 In the current study, no differences were observed in the sagittal outcome of the maxilla between RME and SME. Both Haas/Hyrax and quad-helix appliances produced slight retrusion of the maxilla (Table 2).
In this study, the mandible showed slight and similar retrusion in both groups (Table 2). In noncleft patients, similar behavior has been reported after RME and SME.29
There was similar improvement in the skeletal Class II relationship for both groups (Table 2). This behavior was different from noncleft patients, who usually demonstrate a significant increase in skeletal Class II relationship, with a significantly greater increase after RME.29 This was probably caused by a lack of maxillary growth in patients with BCLP.2–6 The continuous mandibular growth, characteristic of patients in this age range, may have contributed to the increase of the maxillomandibular difference.30
Although RME causes temporary mandibular clockwise rotation and anterior face height increase,20,28,31,32 no differences in the vertical outcomes were observed between RME and SME (Table 2). In both groups, slight increases in SN-GoGn, FMA, and LAFH were noticed. The similarity between RME and SME can be explained by the expansion overcorrection of 2 to 3 mm that produced a cusp to cusp occlusion in both groups, increasing the mandibular plane angulation and anterior face height.
The maxillary incisors underwent slight palatal tipping in the RME group and slight labial tipping in the SME, however, without significant intergroup differences (Table 2). In noncleft patients, there is no unanimity regarding maxillary incisor response after RME or SME.28,29,31–34 The mandibular incisors remained practically unchanged after expansion in both groups. These findings were in agreement with other studies in noncleft patients.32,34,35 This is probably because the forces of these expander devices were applied only to the maxillary teeth.
Changes in the soft tissue were similar in both groups (Table 2). The nasolabial angle slightly increased, probably due to the slight maxillary retrusion produced by the appliances, associated with the progressive retrusion of the maxilla during growth caused by the primary plastic surgeries performed in the first months of life.3–7
The quad-helix had similar cephalometric changes compared to the Hyrax appliance. The inconveniences of slow expansion include the greater expansion time and a less practical clinical procedure due to the constant need for appliance removal/rebonding for activations.18 These aspects are very relevant when selecting the appliances in clinical practice.
Limitations
The greater treatment time with the quad-helix compared to the Hyrax expander was a limitation of the study concerning growth comparison. However, the difference in treatment time was only 3.8 months and should not have compromised the results.19 Further studies with longer follow-up times to evaluate the stability and relapse tendency of the cephalometric results after rapid and slow maxillary expansions are necessary.
CONCLUSIONS
The null hypothesis could not be rejected. No anteroposterior and vertical differences were observed between the effects of RME and SME in patients with bilateral cleft lip and palate.
ACKNOWLEDGMENT
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Brazil (CAPES), Finance Code 001.
REFERENCES
- 1.Freitas JA, Garib DG, Oliveira M, et al. Rehabilitative treatment of cleft lip and palate: experience of the Hospital for Rehabilitation of Craniofacial Anomalies-USP (HRAC-USP)–part 2: pediatric dentistry and orthodontics. J Appl Oral Sci. 2012;20:268–281. doi: 10.1590/S1678-77572012000200024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Semb G. A study of facial growth in patients with unilateral cleft lip and palate treated by the Oslo CLP Team. Cleft Palate Craniofac J. 1991;28:1–21. doi: 10.1597/1545-1569_1991_028_0001_asofgi_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 3.Semb G. A study of facial growth in patients with bilateral cleft lip and palate treated by the Oslo CLP Team. Cleft Palate Craniofac J. 1991;28:22–39. doi: 10.1597/1545-1569_1991_028_0022_asofgi_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 4.Capelozza Filho L, De Almeida AM, Ursi WJ. Rapid maxillary expansion in cleft lip and palate patients. J Clin Orthod. 1994;28:34–39. [PubMed] [Google Scholar]
- 5.da Silva Filho OG, de Castro Machado FM, de Andrade AC, de Souza Freitas JA, Bishara SE. Upper dental arch morphology of adult unoperated complete bilateral cleft lip and palate. Am J Orthod Dentofacial Orthop. 1998;114:154–161. doi: 10.1053/od.1998.v114.a86380. [DOI] [PubMed] [Google Scholar]
- 6.da Silva Filho OG, Ramos AL, Abdo RC. The influence of unilateral cleft lip and palate on maxillary dental arch morphology. Angle Orthod. 1992;62:283–290. doi: 10.1043/0003-3219(1992)062<0283:TIOUCL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Heidbuchel KL, Kuijpers-Jagtman AM, Van't Hof MA, Kramer GJ, Prahl-Andersen B. Effects of early treatment on maxillary arch development in BCLP. A study on dental casts between 0 and 4 years of age. J Craniomaxillofac Surg. 1998;26:140–147. doi: 10.1016/s1010-5182(98)80003-6. [DOI] [PubMed] [Google Scholar]
- 8.Bishara SE, de Arrendondo RS, Vales HP, Jakobsen JR. Dentofacial relationships in persons with unoperated clefts: comparisons between three cleft types. Am J Orthod. 1985;87:481–507. doi: 10.1016/0002-9416(85)90086-7. [DOI] [PubMed] [Google Scholar]
- 9.Heidbuchel KL, Kuijpers-Jagtman AM. Maxillary and mandibular dental-arch dimensions and occlusion in bilateral cleft lip and palate patients form 3 to 17 years of age. Cleft Palate Craniofac J. 1997;34:21–26. doi: 10.1597/1545-1569_1997_034_0021_mamdad_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 10.Larson O, Ideberg M, Nordin KE. Early bone grafting in complete cleft lip and palate cases following maxillofacial orthopedics. IV. A radiographic study of the incorporation of the bone grafts. Scand J Plast Reconstr Surg. 1983;17:93–98. doi: 10.3109/02844318309013103. [DOI] [PubMed] [Google Scholar]
- 11.Hotz M, Perko M, Gnoinski W. Early orthopaedic stabilization of the praemaxilla in complete bilateral cleft lip and palate in combination with the Celesnik lip repair. Scand J Plast Reconstr Surg Hand Surg. 1987;21:45–51. doi: 10.3109/02844318709083579. [DOI] [PubMed] [Google Scholar]
- 12.Cavassan Ade O, de Albuquerque MD, Filho LC. Rapid maxillary expansion after secondary alveolar bone graft in a patient with bilateral cleft lip and palate. Cleft Palate Craniofac J. 2004;41:332–339. doi: 10.1597/02-099.1. [DOI] [PubMed] [Google Scholar]
- 13.Aizenbud D, Ciceu C, Rachmiel A, Hazan-Molina H. Reverse quad helix appliance: differential anterior maxillary expansion of the cleft area before bone grafting. J Craniofac Surg. 2012;23:e440–443. doi: 10.1097/SCS.0b013e318264681a. [DOI] [PubMed] [Google Scholar]
- 14.Huang L, Huang N, Deng X, Chen X. [Semi-attached quad-helix appliance can expand the maxillary arches in patients with cleft lip and palate before alveolar bone grafting] Hua Xi Kou Qiang Yi Xue Za Zhi. 2012;30:393–395. 398. [PubMed] [Google Scholar]
- 15.Aizenbud D, Hazan-Molina H, Peled M, Rachmiel A. The reverse quad helix expander: easy access for bone graft manipulation in the cleft maxilla. Pediatr Dent. 2013;35:120–123. [PubMed] [Google Scholar]
- 16.Dholakia KD, Bhat SR. KD loop for increasing arch perimeter in cleft and noncleft cases. Orthodontics (Chic.) 2012;13:e140–152. [PubMed] [Google Scholar]
- 17.Brunetto M, Andriani Jda S, Ribeiro GL, Locks A, Correa M, Correa LR. Three-dimensional assessment of buccal alveolar bone after rapid and slow maxillary expansion: a clinical trial study. Am J Orthod Dentofacial Orthop. 2013;143:633–644. doi: 10.1016/j.ajodo.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 18.de Medeiros Alves AC, Garib DG, Janson G, de Almeida AM, Calil LR. Analysis of the dentoalveolar effects of slow and rapid maxillary expansion in complete bilateral cleft lip and palate patients: a randomized clinical trial. Clin Oral Investig. 2016;20:1837–1847. doi: 10.1007/s00784-015-1675-1. [DOI] [PubMed] [Google Scholar]
- 19.de Almeida AM, Ozawa TO, Alves ACM, et al. Slow versus rapid maxillary expansion in bilateral cleft lip and palate: a CBCT randomized clinical trial. Clin Oral Investig. 2017;21:1789–1799. doi: 10.1007/s00784-016-1943-8. [DOI] [PubMed] [Google Scholar]
- 20.Garib DG, Henriques JF, Carvalho PE, Gomes SC. Longitudinal effects of rapid maxillary expansion. Angle Orthod. 2007;77:442–448. doi: 10.2319/0003-3219(2007)077[0442:LEORME]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Fleiss JL. Analysis of data from multiclinic trials. Control Clin Trials. 1986;7:267–275. doi: 10.1016/0197-2456(86)90034-6. [DOI] [PubMed] [Google Scholar]
- 22.Chang ZC, Hu FC, Lai E, Yao CC, Chen MH, Chen YJ. Landmark identification errors on cone-beam computed tomography-derived cephalograms and conventional digital cephalograms. Am J Orthod Dentofacial Orthop. 2011;140:e289–297. doi: 10.1016/j.ajodo.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 23.Figueiredo DS, Bartolomeo FU, Romualdo CR, et al. Dentoskeletal effects of 3 maxillary expanders in patients with clefts: A cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2014;146:73–81. doi: 10.1016/j.ajodo.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 24.Gnoinski WM, Rutz G. A longitudinal cephalometric study from age 5 to 18 years on individuals with complete bilateral cleft lip and palate. J Craniofac Surg. 2009;20(Suppl 2):1672–1682. doi: 10.1097/SCS.0b013e3181b2d8dd. [DOI] [PubMed] [Google Scholar]
- 25.Habeeb M, Boucher N, Chung CH. Effects of rapid palatal expansion on the sagittal and vertical dimensions of the maxilla: a study on cephalograms derived from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2013;144:398–403. doi: 10.1016/j.ajodo.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 26.Cevidanes LH, Styner MA, Proffit WR. Image analysis and superimposition of 3-dimensional cone-beam computed tomography models. Am J Orthod Dentofacial Orthop. 2006;129:611–618. doi: 10.1016/j.ajodo.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moshiri M, Scarfe WC, Hilgers ML, Scheetz JP, Silveira AM, Farman AG. Accuracy of linear measurements from imaging plate and lateral cephalometric images derived from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2007;132:550–560. doi: 10.1016/j.ajodo.2006.09.046. [DOI] [PubMed] [Google Scholar]
- 28.Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961;31:73–90. [Google Scholar]
- 29.Akkaya S, Lorenzon S, Ucem TT. A comparison of sagittal and vertical effects between bonded rapid and slow maxillary expansion procedures. Eur J Orthod. 1999;21:175–180. doi: 10.1093/ejo/21.2.175. [DOI] [PubMed] [Google Scholar]
- 30.Stahl de Castrillon F, Baccetti T, Franchi L, Grabowski R, Klink-Heckmann U, McNamara JA. Lateral cephalometric standards of Germans with normal occlusion from 6 to 17 years of age. J Orofac Orthop. 2013;74:236–256. doi: 10.1007/s00056-013-0140-5. [DOI] [PubMed] [Google Scholar]
- 31.Chung CH, Font B. Skeletal and dental changes in the sagittal, vertical, and transverse dimensions after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2004;126:569–575. doi: 10.1016/j.ajodo.2003.10.035. [DOI] [PubMed] [Google Scholar]
- 32.Aras I, Olmez S, Akay MC, Gunbay T, Aras A. The effects of maxillary expansion on the soft tissue facial profile. J Istanb Univ Fac Dent. 2017;51:1–10. doi: 10.17096/jiufd.85884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cerruto C, Ugolini A, Di Vece L, Doldo T, Caprioglio A, Silvestrini-Biavati A. Cephalometric and dental arch changes to Haas-type rapid maxillary expander anchored to deciduous vs permanent molars: a multicenter, randomized controlled trial. J Orofac Orthop. 2017;78:385–393. doi: 10.1007/s00056-017-0092-2. [DOI] [PubMed] [Google Scholar]
- 34.Farronato G, Maspero C, Esposito L, Briguglio E, Farronato D, Giannini L. Rapid maxillary expansion in growing patients. Hyrax versus transverse sagittal maxillary expander: a cephalometric investigation. Eur J Orthod. 2011;33:185–189. doi: 10.1093/ejo/cjq051. [DOI] [PubMed] [Google Scholar]
- 35.Corekci B, Goyenc YB. Dentofacial changes from fan-type rapid maxillary expansion vs traditional rapid maxillary expansion in early mixed dentition. Angle Orthod. 2013;83:842–850. doi: 10.2319/103112-837.1. [DOI] [PMC free article] [PubMed] [Google Scholar]