Abstract
This case report describes orthodontic space closure for managing an avulsed maxillary central incisor and a lateral incisor in a growing girl with a Class I deep bite malocclusion with moderate lower and mild upper crowding. The treatment approach moved a central incisor across the midline and substituted a lateral incisor for a central incisor, in combination with canine substitution. Veneers on all maxillary anterior teeth attained acceptable esthetics. The right central incisor was moved to serve as the avulsed left central incisor. The right lateral incisor was moved to the position of the right central incisor and restored. The canines on both sides were substituted as lateral incisors; the posterior occlusion was left in Class II. Mesialization of central and lateral incisors with prosthetic rehabilitation is an acceptable treatment option.
Keywords: Mesialization of central incisors, Canine substitution
INTRODUCTION
Occasionally, orthodontists encounter traumatic loss of maxillary incisors in growing patients. Multiple factors are considered to obtain optimal results, including patient age, facial morphology, growth pattern, number of missing teeth, occlusion, remaining bone, and the need for orthodontic treatment.1 Several treatment options are available to manage missing incisors. Prognosis of replantation of avulsed permanent teeth is dependent upon the time of replantation, the storage condition, and the stage of root development.2 Transplantation can also be considered.3 Another option maintains the edentulous space and replaces missing teeth with implant or tooth supported restorations.4 An additional option is orthodontic space closure with subsequent prosthodontics.5
Orthodontic space closure with substitution of missing teeth should be considered when there is malocclusion.5–7 Zachrisson,7 Bosio et al.,8 and Pair et al.9 highlighted the importance of proper case selection for orthodontic substitution of missing central incisors.
This case report describes anterior orthodontic space closure and canine substitution as an option for managing an avulsed maxillary central incisor and a lateral incisor.
CASE REPORT
Diagnosis and Etiology
A healthy 11-year-old girl presented with a Class I deep bite malocclusion and moderate lower and mild upper crowding. Previously, a mandibular lingual arch space maintainer had been placed by her dentist.
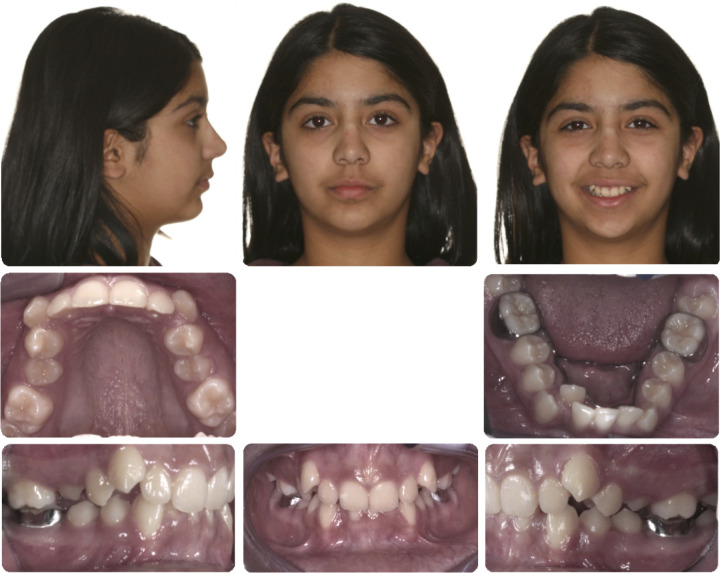
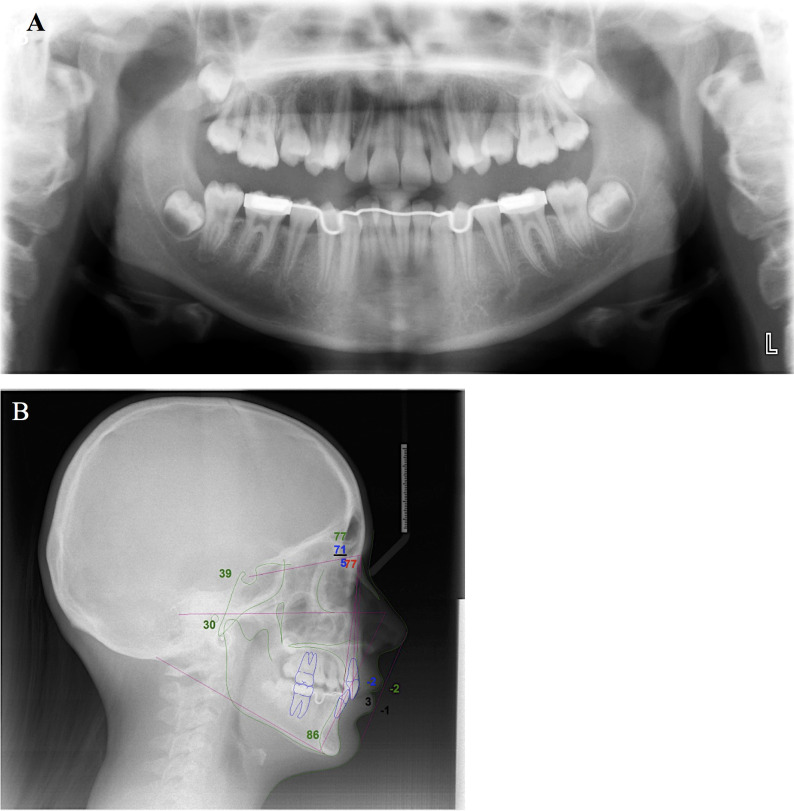
Facially, the nasolabial angle was satisfactory; there was mild mandibular retrusion with an acute labiomental fold. The maxillary midline was coincident with the facial midline. There was a Class I left molar and a right molar relationship slightly forward of Class I (Figures 1 and 2). The overjet was 2 mm and the overbite was 80% with retroclined maxillary incisors. The mandibular dental midline was to the patient's right. There was 6 mm of maxillary and 8 mm of mandibular crowding. Both maxillary and mandibular arch forms were square with second premolars in crossbite. The panoramic radiograph (Figure 3A) demonstrated absence of pathology with all developing third molars present. Cephalometrically, there was a mild skeletal Class II relationship with mild mandibular retrusion (Figure 3B and Table 1). Vertically, the mandibular plane angle was 39° to sella nasion (Table 1). The dental measurements showed a favorable anteroposterior positioning of the mandibular incisors with significant retroclination of maxillary incisors, consistent with a Class II division 2 type of malocclusion (Table 1). Between the time of initial records and starting treatment, the patient avulsed the maxillary left central and lateral incisors in a motor vehicle accident (Figure 4).
Figure 1.
Pretreatment facial and intraoral photographs.
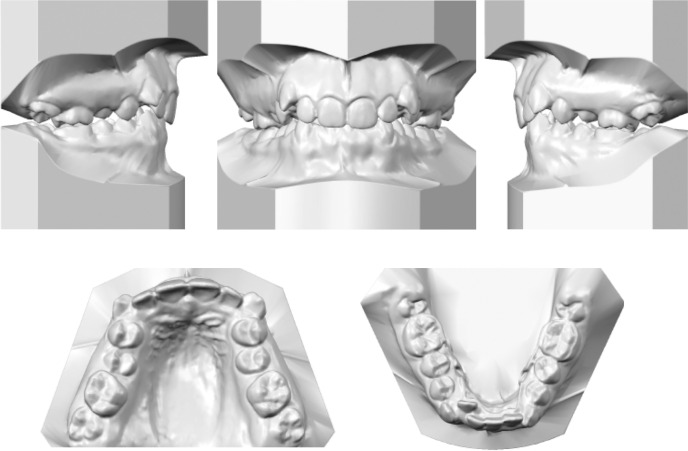
Figure 2.
Pretreatment dental models.
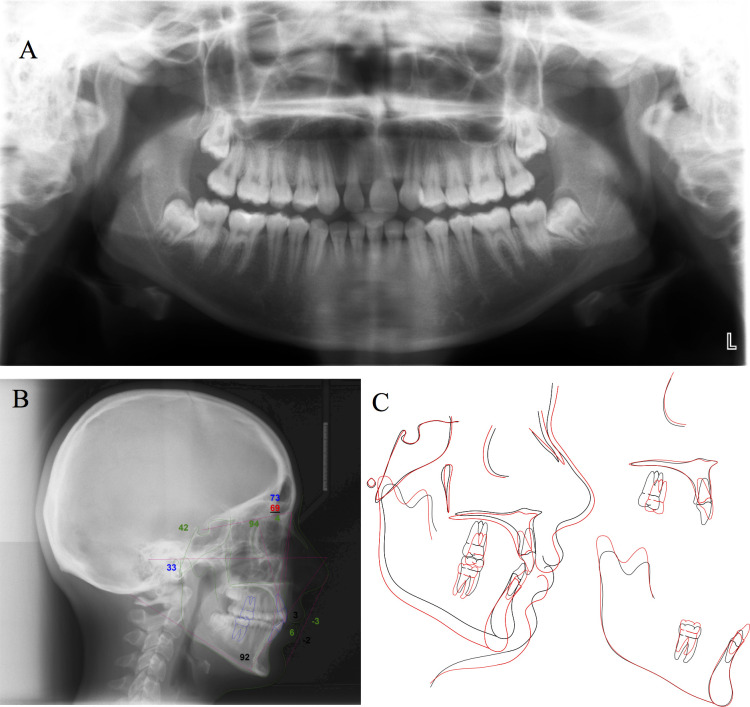
Figure 3.
Pretreatment panoramic radiograph (A), lateral cephalogram, and ABO tracing (B).
Table 1.
Pretreatment and Posttreatment Cephalometric Analysis
| Measurement |
Norm |
Pretreatment |
Posttreatment |
| Maxilla to cranial base | |||
| SNA (°) | 82.0 | 76.6 | 73.0 |
| Mandible to cranial base | |||
| SNB (°) | 80.9 | 71.3 | 69.3 |
| SN-MP (°) | 32.9 | 38.7 | 41.6 |
| FMA (MP-FH) (°) | 23.9 | 30.4 | 33.1 |
| Maxillomandibular | |||
| ANB (°) | 1.6 | 5.3 | 3.7 |
| Maxillary dentition | |||
| U1-NA (mm) | 4.3 | −1.7 | 3.0 |
| U1-SN (°) | 102.8 | 76.7 | 93.8 |
| Mandibular dentition | |||
| L1-NB (mm) | 4.0 | 3.3 | 6.4 |
| L1-MP (°) | 95.0 | 85.7 | 92.1 |
| Soft tissue | |||
| Lower lip to E-plane (mm) | –2.0 | –1.1 | –2.4 |
| Upper lip to E-Plane (mm) | –6.0 | –1.7 | –3.2 |
Figure 4.
Facial and intraoral photographs following traumatic avulsion of left maxillary central and lateral incisors (No. 21 and 22).
Treatment Objectives
Facial objectives included avoiding lip retraction, maintaining the smile width and arc, and avoiding an increase in the labiomental fold. Skeletal objectives involved reducing ANB. Dental objectives involved obtaining a normal overjet and overbite, centering midlines, and obtaining a posterior cusp fossa occlusal relationship. Further objectives were to open the bite and torque the maxillary incisor crowns forward. Another objective was to minimize future restorative care and lifetime maintenance.
Treatment Alternatives
Three treatment alternatives were considered. The first involved conventional orthodontics with extraction of upper first and lower second premolars, followed by anterior prosthetic management. This treatment plan would be associated with increased cost of both orthodontic and prosthetic treatments. The patient was not interested in having a removable partial dental prosthesis, and a long span fixed dental prosthesis was considered invasive as it required preparation of sound abutment teeth. Side by side implants have challenges, especially in managing the papilla.10
Resorption of alveolar bone follows traumatic loss of incisors and canines11 (Figure 4). Hard and soft tissue augmentation would be needed prior to implant placement to create bone volume and to improve esthetics. Implant-supported restorations would be the costliest treatment alternative. It was challenging to consider further extraction of two maxillary first premolars when there had been traumatic loss of two maxillary incisors.
The second option considered was transplantation of a maxillary right premolar to the avulsed central incisor region followed by canine substitution on the maxillary left side. It would create an asymmetric anterior arrangement, where the right side would be managed with no extraction and the left side treated with canine substitution. The overall esthetics might be compromised because the three anterior teeth would be a different size and shape on each side.
For option 3, an alternative transplantation approach was considered with both right and left maxillary premolars transplanted to the region of the avulsed incisors. This treatment plan would resolve the symmetry but would require restorative management for the transplanted premolars. Premolar autotransplantation to the maxillary anterior region is more predictable when two-thirds to three-fourths of the root is developed.12 Since premolar root development was almost complete, this treatment option was considered less favorable due to the increased risk of pulp necrosis and replacement root resorption (Figure 3).3,12 Should either transplant fail, this would compromise this maxillary anterior ridge for prosthetic management.
Option 4 consisted of moving the maxillary right central incisor across the midline to serve as the avulsed maxillary left central incisor. The maxillary right lateral incisor would be moved to the position of the right central and restored. The canines on both sides would be left adjacent to central incisors and substituted as lateral incisors. Mandibular interproximal reduction might minimize lower incisor proclination in a nonextraction lower arch treatment. Given the patient's age, the advantages associated with this less invasive approach included a better periodontal condition, maintenance of alveolar bone, and patient satisfaction. Another modification involved lower premolar extraction.
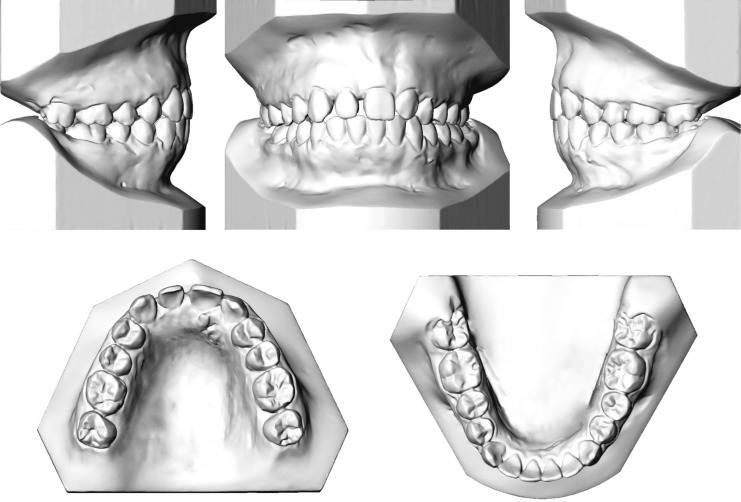
Option 3 was the most acceptable to the patient as this approach kept all of the patient's natural dentition. The patient wanted to avoid lower premolar extraction and elected nonextraction lower arch treatment with interproximal reduction. A diagnostic setup was done prior to initiating orthodontic treatment (Figure 5).
Figure 5.
Diagnostic setup with upper right incisor moved across the midline and upper right lateral incisor moved to the upper right central incisor position. Both canines were left adjacent to the central inciors with molars left in Class II occlusion.
Treatment Progress
After obtaining parental consent, .018” Ormco Orthos appliances (Ormco, California, USA) were bonded on second premolars forward and lower second molars. Bands were placed on all maxillary first and second molars. After initial alignment with round 0.016” Nitinol wires (Memry, Connecticut, USA), leveling took place with rectangular 0.016” × 0.022” heat-activated nickel titanium wires (Dentsply GAC International, New York, USA). Light Class III elastics (Ormco, California, USA) were placed on both sides for molar protraction and to minimize lower incisor proclination associated with alignment and leveling. After alignment and leveling, a progress panoramic radiograph was taken; selected brackets were repositioned to improve marginal ridge heights, rotations, and root parallelism. Then 0.016” × 0.022” stainless steel wires were placed for space closure and finishing.
During space closure, the maxillary right central incisor was moved to the left side by chaining from the maxillary left posterior region to the maxillary right central incisor. As the right central incisor moved to the left, the maxillary anterior frenum was deflected, which required frenectomy (Figures 6 and 7). Once the right central incisor had been moved to the left and midlines were coincident, passive coils were placed to hold the space. Then, the maxillary right lateral incisor was moved from the patient's right toward the right central incisor region. Coils were placed to control the mesial and distal width of the lateral incisor to match that of the other central incisor (Figure 7). Class III elastics were used to protract the maxillary posterior segment and reduce unwanted forward movement of the mandibular incisor. Treatment progress was disrupted by missed appointments and by some compliance issues with elastics. Prior to debanding, prosthodontic consultation was done to approve final tooth position. During finishing, elastics were used to improve interdigitation. Treatment time was 48 months due to issues with elastic compliance and keeping appointments.
Figure 6.
Progress intraoral photographs showing central incisor crossing midline and deflection of the maxillary frenum.
Figure 7.

Progress intraoral photographs showing the use of a passive coil to control the mesiodistal width of the maxillary lateral incisor to match that of the other central incisor.
Treatment Results
Facially there was lip competence, and the mild mandibular retrusion remained. The labiomental fold was slightly improved. Smile width and arc were maintained. There was reduction in maxillary incisor display and an increase in mandibular incisor display (Figure 8).
Figure 8.
Final (before restorations) facial and intraoral photographs.
The final occlusion demonstrated coincident midlines with the maxillary right lateral incisor placed in the region of the maxillary right central incisor (Figures 8 and 9). The posterior occlusion was Class II, with the upper first premolars articulating between the mandibular canines and the first premolars. The overjet and overbite were significantly reduced. The tips of the maxillary canines were selectively reduced; this was limited by patient sensitivity.
Figure 9.
Final (before restorations) dental models.
The final panoramic radiograph (Figure 10A) revealed reasonable root parallelism with impacted mandibular third molars. The maxillary third molars were close to the second molar root. The final cephalometric film (Figure 10B,C) revealed improvement in maxillary incisor angulation and a reduction in ANB that was related to changes in maxillary incisor inclination. There was proclination of the mandibular incisor, which remained within 3 mm of the A-pogonion line and within 6 mm of the N-B line (Table 1). The mandibular plane angle was increased by posterior bite opening secondary to Class III elastics. Because of upper molar extrusion, mandibular growth was expressed in clockwise rotation of the mandible. In retrospect, lower extraction should have been used to reduce Class III elastic wear and prevent the unfavorable bite opening and lower incisor proclination.
Figure 10.
Final (before restorations) panoramic radiograph (A), lateral cephalogram taken at the end of orthodontic treatment with ABO tracing (B), and superimposed cephalometric tracing of pretreatment (black line) and posttreatment (red line) (C) appearance.
The patient was referred for prosthodontic treatment at age 17 years. Overall, four veneers on the maxillary anterior teeth were needed to make the maxillary right lateral incisor appear as a central incisor and to make both maxillary canines resemble lateral incisors. Modification of the maxillary central incisor that crossed the midline was indicated to obtain symmetry between teeth.
Both direct composite and indirect porcelain veneers were considered; the patient and her parent chose ceramic veneers to maximize esthetics. Prosthodontic treatment started with a diagnostic wax-up and intraoral mockups to evaluate esthetics (Figure 11). Incisal overlap preparations were done for all four anterior teeth. Pressed lithium disilicate veneers were fabricated based on the diagnostic wax-up and tried intraorally to evaluate color, shape, emergence profile, and occlusion. Veneers were bonded starting from the midline and working distally using light cure resin cement according to manufacturer's recommendations (Figure 12). Follow-up photos (Figure 13) show the patient 18 months following orthodontic deband and veneer placement. Figure 14 shows the immediate, 1 month, and 6 month post-veneer placement appearance.
Figure 11.
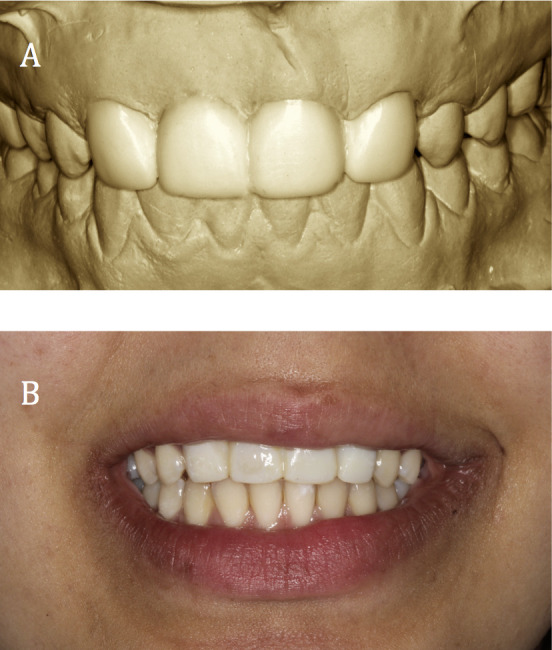
Image before prosthetic diagnostic wax-up (A) and intraoral mockup (B).
Figure 12.
Prosthetic rehabilitation and tooth substitution. Before prosthetic frontal and occlusal views (A and B) demonstrating right central incisor substituting for left central incisor, right lateral incisor for right central incisor, and the canines for lateral incisors. Minimal tooth preparations (C and D) using silicon guide made from diagnostic wax-up. Facial and palatal views of lithium disilicate veneers (E and F). Frontal and occlusal postoperative photographs (G and H) showing lateral incisor and canine substitution with four bonded e-max veneers (Ivoclar Vivadent AG, Schaan, Principality of Liechtenstein) with good esthetics and soft tissue health. Smile photos taken before and after prosthodontics treatment (I and J).
Figure 13.
Facial and intraoral photographs taken 18 months after orthodontic treatment.
Figure 14.
Post-restoration facial view demonstrating stability of the gingival tissues immediately after cementation (A), 4 weeks after cementation (B), and 6 month after cementation (C).
Retention
A mandibular removable Hawley/acrylic rotational control appliance was used full-time for 6 months, followed by nighttime and then alternate nights on a long-term basis. A maxillary Hawley appliance was used with the labial bow soldered to the Adams clasps on maxillary first molars. Wire spurs were placed mesial and distal to the maxillary right lateral incisor, mesial to the right canine and mesial to the right central incisor (now on the left) to control the position of the maxillary right lateral incisor prior to restoration. Full-time wear was requested until the prosthodontic management was completed. After restorative care, a clear vacuum retainer was made for night wear. This served as a retainer and for protection against the mandibular arch of porcelain veneers placed in the maxillary anterior region, since the veneers overlapped the incisal edges.
Final Evaluation of Treatment
Few studies have reported acceptable esthetic results with moving central incisors across the midlines.8,9,13 This case study is the first presenting orthodontic space closure and canine substitution as an option for managing avulsed maxillary central and lateral incisors in a growing patient with a Class I malocclusion. This treatment included moving a central incisor across the midline and substituting a lateral incisor for a central incisor, in combination with canine substitution. The occlusal result was satisfactory, and the esthetics of the maxillary anterior region significantly improved prosthetically. The overjet, overbite, and midline were satisfactory. Posteriorly, there was a cusp fossa occlusal relationship with a Class II premolar and molar. The patient did not incur the significant anticipated costs of implant-supported crowns associated with conventional nonextraction treatment preceded by anticipated hard and soft tissue bone grafting. The restorative costs were reduced with the four veneers. Third molars were recommended to be extracted in the lower arch and observed in the upper arch.
However, there were limitations to this treatment. The maxillary midpalatal suture deflected to the left as a result of moving the central incisor across the midline; root positioning was also compromised (Figure 15). Other studies reported that the suture bends to accommodate the tooth crossing the midline.8,13 The maxillary midline was deviated from the facial midline during treatment. Another flaw was the proclination of the mandibular incisors necessitating long-term mandibular retainer wear. Another complication was the maxillary molar and mandibular incisor extrusion from the Class III elastics. This counterclockwise rotation of the occlusal plane increased mandibular incisor tooth display and resulted in steepening of the mandibular plane, an increase in lower face height, clockwise rotation of the growth pattern, and convex facial profile.
Figure 15.

Maxillary anterior periapical radiograph showing displacement of the midline suture.
Vertical gingival heights of the six maxillary anterior teeth were not ideal. The recommended approach of obtaining gingival margins that are higher on the central incisor, lower on the lateral incisor, and higher on the canine were not followed.14,15 While an attempt was made to extrude the canines and reduce the cusp tip to correct gingival margin heights, sensitivity was encountered. This resulted in positioning the gingival margins of the canines at the same level as the central incisors. The first premolars were not intruded or restored, as recommended by Rosa et al.,14 to avoid additional restorative care with associated financial burden for the patient. Furthermore, there were concerns regarding the potential for vertical bone heights to be compromised in the area of first premolar intrusion in canine substitution cases.14,16 Rosa et al.17 showed long-term follow-up and confirmed previous concern about interproximal bone heights of intruded premolars. Additionally, a long upper lip helped to conceal the gingival esthetics in this patient.
Follow-up photographs taken 18 months after orthodontic treatment (Figure 13) demonstrated good stability and esthetics. It was difficult to create ideal crown form and emergence profile on the lateral incisor substituting for the missing central incisor due to the need to overcontour the restoration mesiodistally due to its smaller root diameter and mesiodistal tooth position. Placing the proximal finish line slightly subgingival on the lateral incisor provided a smooth transition from the cervical margin to the incisal edge. Symmetry between the maxillary lateral incisors and the right maxillary central incisor that was moved to the opposite side was achieved.13 Porcelain veneers were selected as the most conservative predictable treatment rehabilitation option because of the reported estimated survival rate of 94.4% after 5 years, 93.5% at 10 years, and 82.9% at 20 years.18 Gingival tissue contours around the restored four maxillary anterior teeth demonstrated central papilla fill 6 months after cementation with slight variation in the gingival margin of the two central incisors (Figure 14). This was consistent with Czochrowska et al.,19 who reported that width at the gingival margin of the recontoured lateral incisor did not match the appearance of the controls in 25% of the patients.
The patient and her parent were satisfied with the final results of this treatment. This is consistent with other studies that evaluated patient satisfaction with esthetics following orthodontic space opening and prosthetic replacement vs space closure in patients with missing lateral incisors; patients reported higher satisfaction with orthodontic space closure.20–22
CONCLUSIONS
This article presented orthodontic space closure and substitution as an option for managing avulsed maxillary central and lateral incisors in a growing patient with a Class I malocclusion. This treatment included moving a central incisor across the midline, substituting a lateral incisor for a central incisor in combination with canine substitution.
Ceramic veneers could be used successfully in patients with missing lateral incisors and canine substitution.
REFERENCES
- 1.Stenvik A, Zachrisson BU. Orthodontic closure and transplantation in the treatment of missing anterior teeth. An overview. Endod Dent Traumatol. 1993;9:45–52. doi: 10.1111/j.1600-9657.1993.tb00658.x. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM. Replantation of 400 avulsed permanent incisors. 4. Factors related to periodontal ligament healing. Endod Dent Traumatol. 1995;11:76–89. doi: 10.1111/j.1600-9657.1995.tb00464.x. [DOI] [PubMed] [Google Scholar]
- 3.Czochrowska EM, Stenvik A, Bjercke B, Zachrisson BU. Outcome of tooth transplantation: survival and success rates 17-41 years posttreatment. Am J Orthod Dentofacial Orthop. 2002;121:110–119. doi: 10.1067/mod.2002.119979. quiz 193. [DOI] [PubMed] [Google Scholar]
- 4.Kokich VG, Crabill KE. Managing the patient with missing or malformed maxillary central incisors. Am J Orthod Dentofacial Orthop. 2006;129(4 suppl):S55–S63. doi: 10.1016/j.ajodo.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Rayner WJ, Barber SK, Spencer RJ. The effect of canine characteristics and symmetry on perceived smile attractiveness when canine teeth are substituted for lateral incisors. J Orthod. 2015;42:22–32. doi: 10.1179/1465313314Y.0000000118. [DOI] [PubMed] [Google Scholar]
- 6.Kokich VO, Jr, Kinzer GA. Managing congenitally missing lateral incisors. Part I: canine substitution. J Esthet Restor Dent. 2005;17:5–10. doi: 10.1111/j.1708-8240.2005.tb00076.x. [DOI] [PubMed] [Google Scholar]
- 7.Zachrisson BU. Improving orthodontic results in cases with maxillary incisors missing. Am J Orthod. 1978;73:274–289. doi: 10.1016/0002-9416(78)90134-3. [DOI] [PubMed] [Google Scholar]
- 8.Bosio JA, Bradley TG, Hefti AF. Moving an incisor across the midline: a treatment alternative in an adolescent patient. Am J Orthod Dentofacial Orthop. 2011;139:533–543. doi: 10.1016/j.ajodo.2009.10.041. [DOI] [PubMed] [Google Scholar]
- 9.Pair J. Movement of a maxillary central incisor across the midline. Angle Orthod. 2011;81:341–349. doi: 10.2319/051910-270.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71:546–549. doi: 10.1902/jop.2000.71.4.546. [DOI] [PubMed] [Google Scholar]
- 11.Oikarinen KS, Sandor GK, Kainulainen VT, Salonen-Kemppi M. Augmentation of the narrow traumatized anterior alveolar ridge to facilitate dental implant placement. Dent Traumatol. 2003;19:19–29. doi: 10.1034/j.1600-9657.2003.00125.x. [DOI] [PubMed] [Google Scholar]
- 12.Zachrisson BU, Stenvik A, Haanaes HR. Management of missing maxillary anterior teeth with emphasis on autotransplantation. Am J Orthod Dentofacial Orthop. 2004;126:284–288. doi: 10.1016/S0889540604005244. [DOI] [PubMed] [Google Scholar]
- 13.Garib DG, Janson G, dos Santos PB, de Oliveira Baldo T, de Oliveira GU, Ishikiriama SK. Orthodontic movement of a maxillary incisor through the midpalatal suture: a case report. Angle Orthod. 2012;82:370–379. doi: 10.2319/022111-125.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosa M, Zachrisson BU. Integrating space closure and esthetic dentistry in patients with missing maxillary lateral incisors. J Clin Orthod. 2007;41:563–573. quiz 424. [PubMed] [Google Scholar]
- 15.Rosa M, Zachrisson BU. The space-closure alternative for missing maxillary lateral incisors: an update. J Clin Orthod. 2010;44:540–549. [PubMed] [Google Scholar]
- 16.Rosa M, Zachrisson BU. Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors. J Clin Orthod. 2001;35:221–234. [PubMed] [Google Scholar]
- 17.Rosa M, Lucchi P, Ferrari S, Zachrisson BU, Caprioglio A. Congenitally missing maxillary lateral incisors: long-term periodontal and functional evaluation after orthodontic space closure with first premolar intrusion and canine extrusion. Am J Orthod Dentofacial Orthop. 2016;149:339–348. doi: 10.1016/j.ajodo.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 18.Beier US, Kapferer I, Burtscher D, Dumfahrt H. Clinical performance of porcelain laminate veneers for up to 20 years. Int J Prosthodont. 2012;25:79–85. [PubMed] [Google Scholar]
- 19.Czochrowska EM, Skaare AB, Stenvik A, Zachrisson BU. Outcome of orthodontic space closure with a missing maxillary central incisor. Am J Orthod Dentofacial Orthop. 2003;123:597–603. doi: 10.1016/s0889-5406(03)00054-4. [DOI] [PubMed] [Google Scholar]
- 20.Schneider U, Moser L, Fornasetti M, Piattella M, Siciliani G. Esthetic evaluation of implants vs canine substitution in patients with congenitally missing maxillary lateral incisors: are there any new insights? Am J Orthod Dentofacial Orthop. 2016;150:416–424. doi: 10.1016/j.ajodo.2016.02.025. [DOI] [PubMed] [Google Scholar]
- 21.De-Marchi LM, Pini NI, Ramos AL, Pascotto RC. Smile attractiveness of patients treated for congenitally missing maxillary lateral incisors as rated by dentists, laypersons, and the patients themselves. J Prosthet Dent. 2014;112:540–546. doi: 10.1016/j.prosdent.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 22.Armbruster PC, Gardiner DM, Whitley JB, Jr, Flerra J. The congenitally missing maxillary lateral incisor. Part 1: esthetic judgment of treatment options. World J Orthod. 2005;6:369–375. [PubMed] [Google Scholar]