Abstract
As an ancient Gram-negative bacterium, Helicobacter pylori has settled in human stomach. Eradicating H. pylori increases the morbidities of asthma and other allergic diseases. Therefore, H. pylori might play a protective role against asthma. The “disappearing microbiota” hypothesis suggests that the absence of certain types of the ancestral microbiota could change the development of immunology, metabolism, and cognitive ability in our early life, contributing to the development of some diseases. And the Hygiene Hypothesis links early environmental and microbial exposure to the prevalence of atopic allergies and asthma. Exposure to the environment and microbes can influence the growing immune system and protect subsequent immune-mediated diseases. H. pylori can inhibit allergic asthma by regulating the ratio of helper T cells 1/2 (Th1/Th2), Th17/regulatory T cells (Tregs), etc. H. pylori can also target dendritic cells to promote immune tolerance and enhance the protective effect on allergic asthma, and this effect relies on highly suppressed Tregs. The remote regulation of lung immune function by H. pylori is consistent with the gut-lung axis theory. Perhaps, H. pylori also protects against asthma by altering levels of stomach hormones, affecting the autonomic nervous system and lowering the expression of heat shock protein 70. Therapeutic products from H. pylori may be used to prevent and treat asthma. This paper reviews the possible protective influence of H. pylori on allergic asthma and the possible application of H. pylori in treating asthma.
Keywords: Helicobacter pylori, Allergic asthma, Protective effect, Dendritic cells, Helper T cells, Regulatory T cells
Introduction
Since Gram-negative Helicobacter pylori was discovered, the relationship between H. pylori infection and asthma has gradually attracted people's eyes. Kalach et al. [1] analyzed the infection of H. pylori in adults and children from the perspective of host response, epidemiology, related diseases, clinical features, therapies, and diagnosis. The incidence of H. pylori infection is decreasing in both adults and children in developed countries and several developing areas, which is opposite from the increased incidence of asthma in children and other allergic disorders. Ness-Jensen et al. [2] found that H. pylori infection has been related to a 40% decrease of asthma in those who are below the age of 18 years with abdominal obesity. A recent study found that 16.4 percent of children who were negative for H. pylori at the age of 2 and 10 had asthma at the age of 16, but if they were positive for H. pylori at the age of 12, they did not have asthma at the age of 16. It is suggested that the early exposure to H. pylori can prevent asthma [3]. Fouda et al. [4] used ELISA for determination of H. pylori IgG in the serum of asthma and healthy children. The results showed that the titer of IgG was negatively correlated with the degree of asthma. Serum H. pylori could prevent asthma in children and was inversely correlated with the severity of asthma. Accumulating evidence suggested that the infection of H. pylori, particularly CagA-positive H. pylori, was negatively correlated with the development of asthma. A study of Greek children has also proved this viewpoint [5]. Recent and earlier cross-sectional studies also suggested that H. pylori infection had protective effects on asthma [6, 7, 8, 9]. However, not all studies supported this result, which still requires future research [10, 11, 12, 13, 14, 15, 16]. Although the effects of H. pylori in the pathophysiological mechanisms of asthma still remain controversial, the researchers detected H. pylori exotoxin VacA in human lung biopsies and directly stimulated pulmonary airway epithelial cells to secrete inflammatory cytokines in vitro [17]. Moreover, H. pylori has been discovered in the lung tissues of patients with COPD [18]. More studies confirmed that existence of H. pylori provided protective effects against asthma, and eradication of H. pylori may have a negative impact [19, 20, 21].
The immune system includes adaptive immunity (acquired immunity) and innate immunity (natural immunity) [22, 23, 24]. Adaptive immunity mainly recognizes “non-self” antigen and produces immune tolerance, and innate immunity is the first line of defense against pathogenic microorganism invasion, which can effectively distinguish self from pathogenic microorganism [25, 26]. The immune pathogenesis of allergic asthma is quite complex. The studies have focused on Toll-like receptors (TLRs), dendritic cells (DCs), helper T cells 1/2 (Th1/Th2), Th17, regulatory T cells (Tregs), etc. The formation of a complex interaction network between cells and receptors also provides a broad view for immunological research of asthma [27, 28, 29]. The followings are the possible protective mechanisms of H. pylori against allergic asthma reported in recent years and the possible associated treatment of asthma.
Possible Protective Mechanisms of H. pylori against Allergic Asthma
The Hygiene Hypothesis
The hygiene hypothesis [30, 31] links early environmental and microbial exposure to the prevalence of atopic allergies and asthma. The exposure to environment and microbes can help to form the growing immunity system and protect subsequent immune-mediated diseases [32]. “Unhygienic exposure” to microorganisms in an early age can prevent the development of allergic diseases in later years [33]. H. pylori infection usually occurs in children, and the way to be infected is related to unhygienic family environment or habits, and this association appears in mouse asthma models [34]. Early studies [35] have shown that the hygiene hypothesis may be related to Th1/Th2 imbalance. Synthetic adjuvants or microbial components can directly influence the cells in the innate immune system, including NK and DCs cells, and also stimulate the secretion of interferon-γ (IFN-γ), IL-12, and IFN-α, leading to the phenotypic transformation of allergen-specific Th2 to Th1 cells [7, 36]. The specific mechanisms still need to be further studied.
Adjusting Th1/Th2 Balance
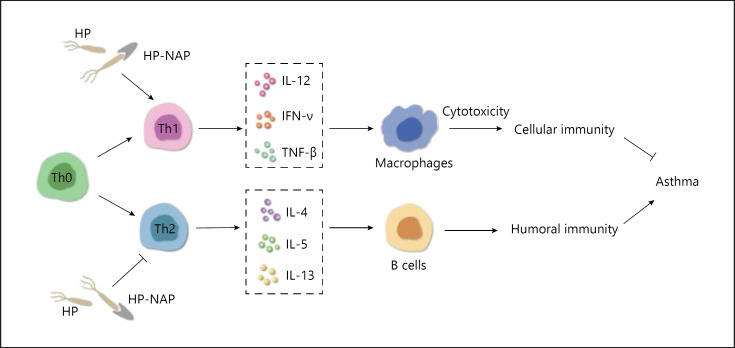
It has been proved that Th1/Th2 ratio imbalance is one of the essential immunological mechanisms of asthma. According to the responses to foreign antigens, T cells can be divided into 2 types of effector cells, Th1 and Th2, which have totally different functions [37, 38]. Th1 mainly secretes IL-12, IFN-γ, and transforming growth factor β (TNF-β), activates macrophages and causes cytotoxicity, and mediates cellular immunity. Th2 mainly secretes IL-4, IL-5, and IL-13, activates B cells to produce immunoglobulin, and mediates humoral immunity. Th1 and Th2 are restrictive to each other and reach a balance. Asthma is a disease characterized by the count of Th2 and the effects it exerts [39, 40, 41].
H. pylori neutrophil-activating protein (HP-NAP) is one of the main virulence factors of H. pylori, which is also applied as a possible biomarker in the diagnosis of H. pylori-related diseases [42]. Studies [43, 44, 45] have shown that HP-NAP plays a protective role in asthma, which could stimulate Th1 activation and attenuate Th2 response in allergy-related asthma both in vitro and in vivo (Fig. 1). In the research by Karakullukcu et al. [46], 18 cases (20.4%) of H. pylori DNA were discovered in 88 healthy stool samples but none in 92 asthmatic children (3–8 years). Multivariate Logistic regression analysis suggested that HP-NAP had a protective effect on asthma in male children. In order to verify HP-NAP as a regulatory factor against the Th2 inflammatory effect, Zhou et al. [47] exposed the mice to purified recombinant H. pylori NAP (rNAP) through intraperitoneal injection or inhalation. The increase and infiltration of the eosinophils were remarkably suppressed in the lungs of the asthma mice model induced by ovalbumin (OVA). Moreover, the count of eosinophils was decreased in the lavage fluid from bronchoalveolar (BALF) in the mice treated with rNAP. Additionally, the levels of IL-13 and IL-4 declined (p < 0.01), the levels of IFN-γ and IL-10 elevated (p < 0.01), and the serum level of IgE declined (p < 0.01) in experimental groups in comparison with the control group. It is suggested that mucosal and systemic pretreatment of rNAP might attenuate asthma in the mice induced by OVA. Furthermore, rNAP could be used as a new method in preventing or treating allergic disorders. In phase I/II clinical trials, it has been reported that the effect of soluble IL-4 receptor (sIL-4R) was satisfactory in treating asthma. To discover more effective antiasthma therapies, Liu et al. [48] attempted to test whether the HP-NAP could increase the therapeutic effect of sIL-4R on asthma. In their research, pcDNA3.1-sIL-4R-NAP plasmid (PSN) was constructed, which could encode a fusion protein of murine HP-NAP and sIL-4R. PSN could remarkably reduce inflammation in the airway, suppress the secretion of OVA-specific IgE in serum, and reestablish the balance of Th1 and Th2. Moreover, PSN has been more effective in the treatment for asthma in comparison with the plasmid only generating sIL-4R.
Fig. 1.
H. pylori promotes Th1 activation and inhibits Th2 response through HP-NAP in allergic asthma. HP, H. pylori; HP-NAP, H. pylori neutrophil-activating protein; Th0/Th1/Th2, helper T cells 0/1/2.
Adjusting Thl7/Tregs Balance
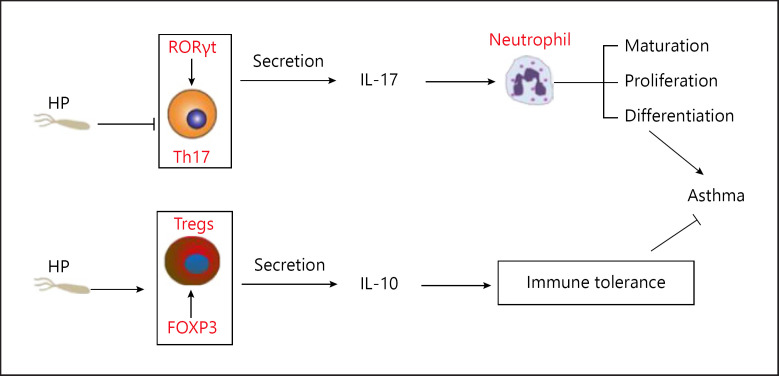
With the development of scientific research, Thl/Th2 imbalance cannot fully explain the mechanisms of asthma [49]. Although allergic asthma is often associated with abnormal TH2 cellular responses, a group of patients with severe disease showed a mixture of TH2 and TH17 cellular responses in the airways [50]. It was found that Thl7 and Tregs cells were also significantly related to the pathogenesis of asthma [51, 52, 53]. Synergy of multiple pathways, such as Th2, Th17, and even eosinophil/neutrophil infiltration, has been found in some asthma models [54, 55, 56]. The view that eosinophilic asthma is an exclusive TH2 disorder and neutrophil asthma is an exclusive TH17 disorder may be oversimplified [57]. It has been found that the TH2 and TH17 inflammatory pathways regulate each other in asthma [58]. Th1/Th2 and Thl7/Tregs and their various cytokines form an extremely complex interactive network [59, 60]. Thl7 cells are defined as “proinflammatory” immune cells, which mainly secrete IL-17, mediate inflammatory responses, and promote neutrophil maturation, proliferation, and chemotaxis. Retinoid-related orphan receptor (ROR) gamma t (RORγt) is a key transcriptional factor in the differentiation of Thl7 cells. The deletion of RORγt leads to the failure of Thl7 differentiation [61, 62]. Tregs secrete IL-10 and other inhibitory cytokines. Tregs play an important role in maintaining immune balance. Tregs specifically express forkhead transcription factor p3 (Foxp3), suppress immune response, and mediate immune tolerance [63, 64, 65].
The protective mechanisms of H. pylori in inflammatory diseases such as asthma may be associated with induction of Tregs, which could highly suppress the immune activity [66, 67, 68]. Published data strongly suggested that H. pylori caused an increase in the response levels of Tregs, Th1, and Th17 in mouse models and human, which could prevent asthma. According to the ontogeny of the immune system, H. pylori tends to infect in one's childhood and continues to stimulate immunity reaction throughout the life, including Th1, Th17, and Tregs responses. Additionally, children infected by H. pylori tend to have a stronger Tregs response than adults [69, 70, 71, 72]. Once human is infected by H. pylori, Tregs are found to be highly active in the gastric mucosa. The secretion of IL-10 by Tregs in peripheral blood was significantly higher than that in H pylori-specific Th1 cells. When there was a strong Tregs reaction, the concentration of total IgE and allergen-specific IgE was low. Suppressing IL-10 could significantly restore the IgE reaction in animal models. Therefore, systematic IL-10 and Tregs may play a role in preventing allergies mediated by H. pylori [72].
Kyburz et al. [73] established C57BL/6 mice experimental models of house dust mite- or ovalbumin-induced airway inflammation and influenza A virus or Citrobacter rodentium infection. It was found that the exposure to H. pylori extract or its immunomodulator vacuolating cytotoxin in the perinatal stage could exert robust protective functions against allergic inflammation in the airway not only in the offspring of the first generation but also the second generation, which did not increase the susceptibility to bacterial or viral infection. The immune responses correlated with prevention of allergy include inhibiting the activities of effectors or T cells, expanding the subsets of regulatory T cells expressing RORγt, and FOXP3 demethylation. The diversity and composition of the microbiota in the gastrointestinal system are notably influenced by the perinatal exposure of H. pylori. In conclusion, H. pylori exposure not only works on the carriers but also on the next generations. Maternal nutrient, the exposure to microorganisms, tobacco, and other environmental factors influence the formation of the immune system in a fetus via an epigenetic way (Fig. 2).
Fig. 2.
H. pylori has a protective effect on asthma by inducing highly immunosuppressive Tregs and inhibiting Th17. HP, H. pylori; Tregs, regulatory T cells; RORγt, retinoid-related orphan receptor (ROR) gamma t; Foxp3, forkhead transcription factor p3.
Inhibition of DCs
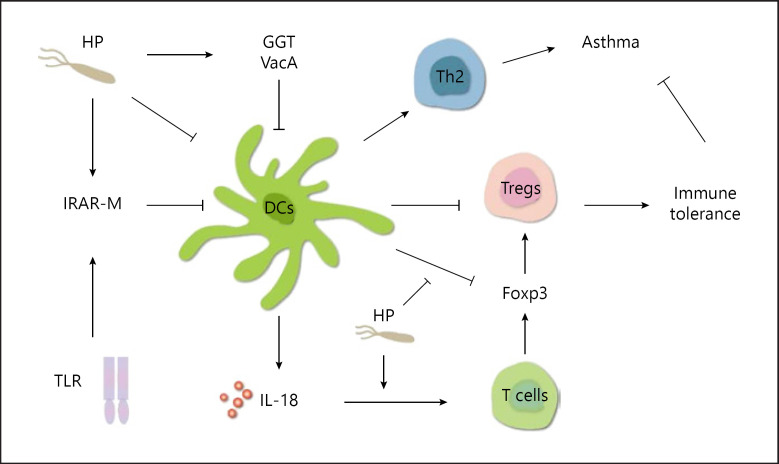
DCs can devour and kill invasive microorganisms and present microbial antigens to T cells, thus participating in the innate immunity [25, 74]. DCs help the initial T cells polarize into Th2 effector cells or differentiate into Tregs [75, 76]. It has been suggested that H. pylori targets DCs to promote immune tolerance and enhance the protective effect against allergic asthma, and this effect relies on highly suppressed Tregs [77, 78]. Oertli et al. [79, 80] found the level of Foxp3, the main regulatory factor expressed by Tregs, was increased in immature T cells when H. pylori was exposed to DCs in cells and animal experiments. Depleting the DCs in H. pylori-infected mice in the neonatal stage resulted in the improvement of infection control and the destruction of specific tolerance to H pylori. At the same time, it also aggravated the immune-pathological reactions driven by T cells. IL-18 secreted by DCs could directly act on T cells and promote transformation into Tregs. It promotes specific immune tolerance and asthma protection in mice. Vacuolating cytotoxin A (VacA) and γ-glutamyl transpeptidase (GGT), 2 virulence factors in H. pylori, independently interfere with the maturation of DCs, thus promoting the tolerance of DCs. Shiu et al. [81] found that the infection of H. pylori can upregulate the expression of anti-inflammation factors including IL-1 receptor-associated kinase M (IRAK-M). The expression of IRAK-M activated by TLRs in DCs directly inhibited the inherent function of DCs, such as the upregulation of cytokines and costimulatory molecules, rather than affecting the response of Th17 and Tregs (Fig. 3).
Fig. 3.
H. pylori targets DCs and relies on highly suppressed Tregs to promote immune tolerance and enhance the protective effect on allergic asthma. HP, H. pylori; Tregs, regulatory T cells; DCs, dendritic cells; TLR, Toll-like receptors; GGT, γ-glutamyl transpeptidase; VacA, vacuolating cytotoxin A.
Activation of TLRs
TLRs are a group of widely studied pattern recognition receptors, which are associated with the incidence and progression of asthma. At present, it is considered that TLRs are mainly expressed in the membrane or organelle capsule of antigen presenting cells (such as macrophages and DCs). TLRs participate in the early host defense and play an important role in the innate immune response. On the other hand, TLRs participate in the inflammatory response via secreting cytokines, chemokines, adhesion molecules, etc., and finally activate the acquired immune system. Different TLRs have different functions [82, 83, 84]. TLR2 is an important pattern recognition receptor in Tregs [85, 86] and TLR9 mainly plays a negative role in the regulation of allergic inflammation [87, 88, 89]. TLR4 not only relies on conserved sequences encoded by embryological genes to identify pathogenic microorganisms and activate innate immunity but also regulates adaptive immunity [90, 91]. In conclusion, TLRs are closely related to asthma [92].
In recent days, hypotheses were proposed that H. pylori could facilitate the activation of inflammasomes in mouse and human immune cells. The possible mechanisms and virulence factors stimulating the inflammasome have been discovered in animal and cell models. IL-1β could facilitate the responses of Th1 and Th17. IL-18 has been a hallmark in humans and mice infected by H. pylori, which plays an important role in H. pylori persistence, Tregs differentiation, and prevention of asthma. The secretion of IL-1β induced by H. pylori is regulated by the activation of NLRP3 (Nod-like receptor family member), caspase-1, and TLR2. The axis of TLR2/NLRP3/caspase-1/IL-18 was essential in the regulation of H. pylori-specific immune response which could prevent inflammatory bowel disease and asthma induced by allergens in mouse models [93, 94, 95].
NOD1 is considered as a pattern recognition receptor in cells and specifically targets the Gram-negative peptidoglycan, which plays an important role in host defense against infections (e.g., H. pylori and Shigella flexneri) [96]. The variations in the NOD1 gene contribute to inflammatory bowel disease and asthma. NOD1 could be activated by a rather low concentration of M-Tri DAP, which is a specific muropeptide ligand. Moreover, NOD1 could induce minimal secretion of IL-10, TNF-α, and IL-1β from peripheral blood mononuclear cells in human and synergistically facilitated the responses induced by TLRs. Synergistic responses occurred across a variety of cytokine secretions (GM-CSF, IL-10, IL-4, IL-6, IL-1β, IL-1α, and TNF-α) and various ligands (to TLR5, 7/8, 2/6, 1/2, 4) [97].
TLR9 could partly contribute to the initiation of immunity responses induced by bacteria via binding to the unmethylated CpG-DNA rich in bacteria. A well-reported single nucleotide polymorphism (SNP) in the TLR9 promoter (TLR9-1237T/C) is related to multiple inflammatory diseases, such as atopy, allergic asthma, and inflammatory bowel disease. The sequence of the TLR9 promoter gene was analyzed, and the results demonstrated that carrying the variant “C” allele on position −1237 formed a possible site to bind NF-κB, which could theoretically stimulate the transcriptional process of the gene [98]. It has also been shown that the type IV secretion system of H. pylori facilitated the synthesis of IL-8 through the p38 protein kinase (p38MAPK) pathway in the primary tracheobronchial epithelial cells collected from young rhesus monkeys. It was suggested that the innate immune response in airway epithelial cells in infants infected by H. pylori was enhanced, but the TLR4 pathway was not essential in this process [99].
Reduction of Gastroesophageal Reflux
Gastroesophageal reflux can induce or aggravate asthma. Several possible mechanisms have been raised. The first is stimulation theory. The airway is stimulated by the aspiration resulting from the reflux, which increases airway responsiveness. The second is reflex theory. Since esophagus and bronchus are derived from the same embryonic organ, the autonomic innervation is similar. Reflux not only stimulates esophagus but also activates the vagus nerve, thus inducing bronchospasm and aggravating asthma [100, 101]. It has been shown that H. pylori inflammation changed gastric hormonal status and influenced the autonomic nervous system. H. pylori can also reduce gastroesophageal reflux [102].
The Gut-Lung Axis Theory
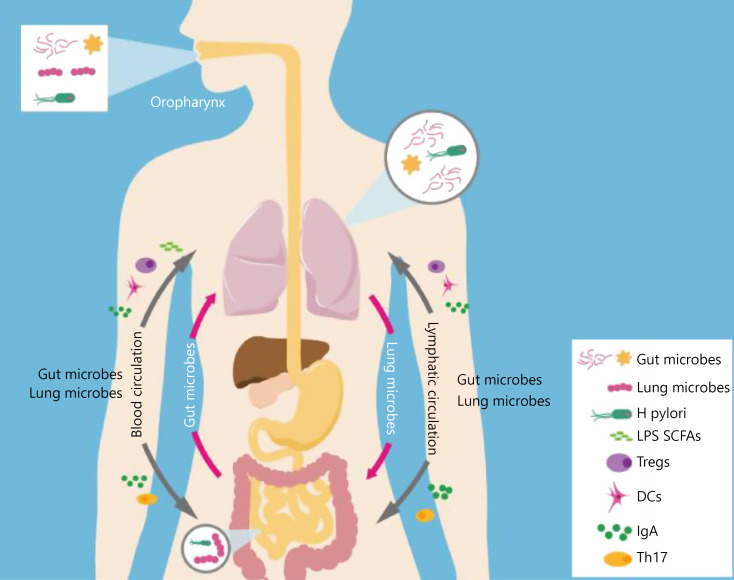
In recent decades, the role of gut flora in the pathogenesis of asthma has been extensively studied [103, 104, 105]. The gut and lungs interact with each other through microbes and immune functions, achieve bidirectional regulation, and amplify immune signals. It is known as the gut-lung axis [106]. Gut and lung microbes have certain homology at early colonization. They all first pass through the oropharynx and then enter the digestive tract or respiratory tract through swallowing or breathing [107]. Microorganisms in the gastrointestinal tract can reach the lower respiratory tract through gastroesophageal reflux [108]. Due to the increase of intestinal and alveolar capillary permeability in some patients, the bacteria from the intestinal mucosa can be transferred to the lungs through the blood circulation [109]. Changes in the pulmonary flora can also cause changes in the intestinal flora through the blood flow [110]. However, there is little evidence about direct shift of microorganisms between 2 sites [107].
Disorders of the gut can be observed in lung diseases [105, 111, 112, 113, 114]. Influenza virus can change the composition of intestinal flora and cause intestinal immune damage through Th17 cell mediation [115]. Locally induced pulmonary anaphylaxis may also affect the composition of intestinal flora [116]. Studies have shown that the severity of intestinal symptoms is highly consistent with the severity of pulmonary symptoms [117, 118].
Intestinal microbes promote development of the body's immune system early in life and affect the whole body and lungs through the blood and lymphatic system [104]. Both the gut and lungs have a strong mucosal defense system. For instance, intestinal and respiratory mucosal goblet cells can secrete IgA. The intestinal microflora can regulate pulmonary immune responses through bacterial lipopolysaccharide, short-chain fatty acids (SCFAs), and immune cells (e.g., Tregs and DCs), which can affect colonization of the lung microbiome [106, 119, 120]. The imbalance of intestinal flora is related to a variety of lung diseases such as asthma. The adjustment of intestinal flora can alleviate the symptoms and reduce the incidence of asthma. Probiotics supplementation has a certain preventive and therapeutic effect on asthma in mice. High-fiber diet can change the intestinal flora of mice and increase the content of SCFAs, thus inhibiting the activity of Th2 cells [121]. H. pylori can cause chronic immunopathologic changes in the stomach and dysbacteriosis and promote regulation of the immune function of the lung. H. pylori protects asthma by DCs, Tregs, etc., which is consistent with the gut-lung axis theory [106, 110, 122] (Fig. 4).
Fig. 4.
The gut-lung axis theory: Gut and lung interactions through microbiota and immune function. LPS, bacterial lipopolysaccharide; SCFAs, short-chain fatty acids; Tregs, regulatory T cells; DCs, dendritic cells; Th17, helper T cells 17.
Reducing the Expression of Heat Shock Protein 70
Heat shock protein 70 (HSP70), an ATP-dependent chaperone protein, is a known inhibitor of caspase activation, showing antiapoptotic activity in a variety of cells [123, 124]. It has been found that HSP70 might play a role in promoting asthma inflammation. HSP70 deficiency leads to significant reduction in airway inflammation, goblet cell proliferation, and Th2 cytokine production, including IL-4, IL-5, and IL-13, and targeting HSP70 can alleviate the potential utility of allergen-induced Th2 cytokines, goblet cell proliferation, and airway inflammation [125, 126, 127]. HSP70/CD80 DNA vaccine can inhibit airway remodeling by regulating the development of Th1/Th2 subsets in asthma mice, and HSP70 may be a potential target for inhaled glucocorticoids (ICS) in the treatment of asthma [128, 129]. Another study also found that HSP70 directly inhibited irritation-induced gastric ulcer formation and promoted gastric ulcer healing [130]. HSP70 can also protect the gastric mucosa through inhibition of apoptosis, proinflammatory cytokines, and cell adhesion molecules [131, 132]. H. pylori infection alters gastric epithelial cell proliferation and reduces or even abolishes HSP70 gene expression [133, 134]. The possible mechanisms included inducing the cellular protective effect of HSP70 against H. pylori infection via inhibiting the expression of inducible nitric oxide synthase (iNOS). However, the reliability and accuracy, as well as the underlying mechanisms, in this relationship remains poorly understood, and large-sample clinical research must be performed to verify this theory [135, 136]. The direct mechanism of HSP70 related H. pylori in protecting asthma remains to be further explored.
The “Disappearing Microbiota” Hypothesis
H. pylori is a kind of ancient, dominant bacteria that settle in the human stomach and closely attach to host cells. H. pylori might be a regular member in the gastric microflora in human. With the improvement of environment and lifestyle, and the eradication of H pylori, the prevalence of H. pylori infection in the developed countries has declined sharply, while the incidence of asthma, obesity, and allergic diseases has increased rapidly [137, 138, 139]. According to Blazer [140], the proponent of the “disappearing microbiota” hypothesis, the absence of certain bacterial species from the ancestral microbiota could change the environment where cognitive, metabolic, and immunological functions develop in our early life. This change could result in the increased susceptibility to some diseases. The disappearance of ancient microbiota may be a universal paradigm leading to modern diseases. This harmful trend implies that we need to put efforts in understanding and reversing the reasons contributing to the disappearing microbiota [5].
Treatment of Asthma Related to H. pylori Infection
Eradicating H. pylori could decrease the occurrence of dyspepsia, peptic ulcer, and gastric malignancy. However, concerns of extensive application of eradication treatment are also raised, such as the resistance to antimicrobial agents and an increase in the prevalence of disorders that are negatively correlated with the infection of H. pylori, including obesity, asthma, GERD, and Barrett esophagus [141, 142]. Eradicating the infection of H. pylori is considered as a double-edged sword. Thus, selective identification and elimination of only the virulent strains of H. pylori are of great importance in the eradication therapy [143]. Epidemiology studies and experiments have demonstrated that exposure to H. pylori could prevent asthma, especially in one's childhood. Recently, in vivo studies have shown that live bacteria are not involved in induction of this protective role. Administrating an extract of H. pylori in a newborn could prevent inflammation in the airway and metaplasia of the goblet cells. Injection of H. pylori extract could inhibit DCs in processing the allergen in the mediastinal lymph nodes and lungs. These results suggest that the extract of H. pylori following sensitization could effectively prevent allergic airway disorders [144]. H. pylori targets DCs and relies on highly suppressed Tregs. Since HP-NAP is considered as a possible regulator for Tregs and can inhibit allergic inflammation of asthma, it is possible to develop HP-NAP as an efficient H. pylori-specific vaccine to treat allergic asthma [78, 145, 146]. van Wijck et al. [147] have shown that H. pylori extract can effectively reduce the production of mucus and multiple characteristics of inflammation in the mice rechallenged by house dust mite. VacA and GGT, 2 persistence determinants in H. pylori, are sufficient in preventing asthma and could be given in their purified forms for treatment [148]. Transmaternal H. pylori exposure can reduce allergic airway inflammation in the offspring through Tregs and also provide new insights for interventional therapy of asthma [73]. High doses of vitamin D and fish oil supplements during pregnancy have been shown to help prevent and control disease in the offspring [149], and maternal treatment of Zika virus infection with the IL-1 receptor antagonist can directly reduce fetal neuroinflammatory response through placental immunity [150]. Immunological methods can be used to design vaccines against H. pylori infection, and it should also be used for the prevention of asthma across generations [64, 68, 70]. VacA, GGT, HP-NAP, Tregs, and even FOXP3 each play an important role in H. pylori-related asthma protection. It would be a very interesting topic if we could design an effective monoepitope or multiepitope vaccine that could be used by the mother before pregnancy, during pregnancy, or during breastfeeding to prevent asthma of the offspring through the placenta or breast milk.
Conclusion
H. pylori may protect allergic asthma by regulating Th1/Th2 and Thl7/Tregs balance, inhibiting DCs and HSP70, activating TLRs, and reducing gastroesophageal reflux. The hygiene hypothesis, the “disappearing microbiota” hypothesis, and the gut-lung axis theory all support this protective effect. Therapeutic products made by H. pylori may be used to prevent and treat asthma. In particular, perinatal exposure to H. pylori can reduce allergic airway inflammation in the offspring, which also provide a new insight for interventional treatment of asthma.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive any funding.
Author Contributions
Z.Z. and F.Y. conceived and designed this study and contributed equally to this work. Y.M., Y.S., C.B., and C.L. participated actively in the study and approved the submitted manuscript.
Acknowledgement
The authors acknowledge the editorial assistance of Shanghai Xu Mu Biotechnology Co., Ltd., and Miss. Xia Li for the illustrations.
Edited by: H.-U. Simon, Bern.
verified
References
- 1.Kalach N, Bontems P, Raymond J. Helicobacter pylori infection in children. Helicobacter. 2017;22((Suppl 1)):e12414. doi: 10.1111/hel.12414. [DOI] [PubMed] [Google Scholar]
- 2.Ness-Jensen E, Langhammer A, Hveem K, Lu Y. Helicobacter pylori in relation to asthma and allergy modified by abdominal obesity: the HUNT study in Norway. World Allergy Organ J. 2019;12((5)):100035. doi: 10.1016/j.waojou.2019.100035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melby KK, Carlsen KL, Håland G, Samdal HH, Carlsen KH. Helicobacter pylori in early childhood and asthma in adolescence. BMC Res Notes. 2020;13((1)):79. doi: 10.1186/s13104-020-04941-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fouda EM, Kamel TB, Nabih ES, Abdelazem AA. Helicobacter pylori seropositivity protects against childhood asthma and inversely correlates to its clinical and functional severity. Allergol Immunopathol. 2018;46((1)):76–81. doi: 10.1016/j.aller.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Tsigalou C, Konstantinidis TG, Cassimos D, Karvelas A, Grapsa A, Tsalkidis A, et al. Inverse association between Helicobacter pylori infection and childhood asthma in Greece: a case-control study. Germs. 2019;9((4)):182–7. doi: 10.18683/germs.2019.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kato H, Pattison R, Bhandari S. Inverse relationship between Helicobacter pylori infection and asthma in US adults with peptic ulcer disease. Indian J Gastroenterol. 2017;36((2)):158–9. doi: 10.1007/s12664-017-0736-6. [DOI] [PubMed] [Google Scholar]
- 7.Chen C, Xun P, Tsinovoi C, He K. Accumulated evidence on Helicobacter pylori infection and the risk of asthma: a meta-analysis. Ann Allergy Asthma Immunol. 2017;119((2)):137–45.e2. doi: 10.1016/j.anai.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Lim JH, Kim N, Lim SH, Kwon JW, Shin CM, Chang YS, et al. Inverse relationship between Helicobacter pylori infection and asthma among adults younger than 40 years: a cross-sectional study. Medicine. 2016;95((8)):e2609. doi: 10.1097/MD.0000000000002609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iizasa H, Ishihara S, Richardo T, Kanehiro Y, Yoshiyama H. Dysbiotic infection in the stomach. World J Gastroenterol. 2015;21((40)):11450–7. doi: 10.3748/wjg.v21.i40.11450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang YC, Lin TY, Shang ST, Chen HJ, Kao CH, Wu CC, et al. Helicobacter pylori infection increases the risk of adult-onset asthma: a nationwide cohort study. Eur J Clin Microbiol Infect Dis. 2017;36((9)):1587–94. doi: 10.1007/s10096-017-2972-1. [DOI] [PubMed] [Google Scholar]
- 11.Molina-Infante J, Gutierrez-Junquera C, Savarino E, Penagini R, Modolell I, Bartolo O, et al. Helicobacter pylori infection does not protect against eosinophilic esophagitis: results from a large multicenter case-control study. Am J Gastroenterol. 2018;113((7)):972–9. doi: 10.1038/s41395-018-0035-6. [DOI] [PubMed] [Google Scholar]
- 12.Holster IL, Vila AM, Caudri D, den Hoed CM, Perez-Perez GI, Blaser MJ, et al. The impact of Helicobacter pylori on atopic disorders in childhood. Helicobacter. 2012;17((3)):232–7. doi: 10.1111/j.1523-5378.2012.00934.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Q, Yu C, Sun Y. The association between asthma and Helicobacter pylori: a meta-analysis. Helicobacter. 2013;18((1)):41–53. doi: 10.1111/hel.12012. [DOI] [PubMed] [Google Scholar]
- 14.Wang Y, Bi Y, Zhang L, Wang C. Is Helicobacter pylori infection associated with asthma risk? A meta-analysis based on 770 cases and 785 controls. Int J Med Sci. 2012;9((7)):603–10. doi: 10.7150/ijms.4970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang SS, Hu HY. No inverse relationship between Helicobacter pylori infection and adult asthma with peptic ulcer disease. Hepatogastroenterology. 2014;61((130)):529–34. [PubMed] [Google Scholar]
- 16.Sabbagh P, Javanian M, Koppolu V, Vasigala VR, Ebrahimpour S. Helicobacter pylori infection in children: an overview of diagnostic methods. Eur J Clin Microbiol Infect Dis. 2019;38((6)):1035–45. doi: 10.1007/s10096-019-03502-5. [DOI] [PubMed] [Google Scholar]
- 17.Nakashima S, Kakugawa T, Yura H, Tomonaga M, Harada T, Hara A, et al. Identification of Helicobacter pylori VacA in human lung and its effects on lung cells. Biochem Biophys Res Commun. 2015;460((3)):721–6. doi: 10.1016/j.bbrc.2015.03.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang YJ, Kim E, Cox MJ, Brodie EL, Brown R, Wiener-Kronish JP, et al. A persistent and diverse airway microbiota present during chronic obstructive pulmonary disease exacerbations. OMICS. 2010;14((1)):9–59. doi: 10.1089/omi.2009.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karimi A, Fakhimi-Derakhshan K, Imanzadeh F, Rezaei M, Cavoshzadeh Z, Maham S. Helicobacter pylori infection and pediatric asthma. Iran J Microbiol. 2013;5((2)):132–5. [PMC free article] [PubMed] [Google Scholar]
- 20.Taye B, Enquselassie F, Tsegaye A, Amberbir A, Medhin G, Fogarty A, et al. Association between infection with Helicobacter pylori and atopy in young Ethiopian children: a longitudinal study. Clin Exp Allergy. 2017;47((10)):1299–308. doi: 10.1111/cea.12995. [DOI] [PubMed] [Google Scholar]
- 21.Popescu D, Andronescu D, Babes PA. The association between Helicobacter pylori infection and liver and biliary tract disorders. Curr Health Sci J. 2018;44((2)):186–91. doi: 10.12865/CHSJ.44.02.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hossain FMA, Choi JY, Uyangaa E, Park SO, Eo SK. The interplay between host immunity and respiratory viral infection in asthma exacerbation. Immune Netw. 2019;19((5)):e31. doi: 10.4110/in.2019.19.e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eisenbarth SC, Cassel S, Bottomly K. Understanding asthma pathogenesis: linking innate and adaptive immunity. Curr Opin Pediatr. 2004;16((6)):659–66. doi: 10.1097/01.mop.0000145920.00101.e4. [DOI] [PubMed] [Google Scholar]
- 24.Moui A, Klein M, Hassoun D, Dijoux E, Cheminant MA, Magnan A, et al. The IL-15/sIL-15Rα complex modulates immunity without effect on asthma features in mouse. Respir Res. 2020;21((1)):33. doi: 10.1186/s12931-020-1301-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shahir M, Mahmoud Hashemi S, Asadirad A, Varahram M, Kazempour-Dizaji M, Folkerts G, et al. Effect of mesenchymal stem cell-derived exosomes on the induction of mouse tolerogenic dendritic cells. J Cell Physiol. 2020;235:7043–55. doi: 10.1002/jcp.29601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arikoglu T, Akyilmaz E, Yildirim DD, Batmaz SB, Ulger ST, Aslan G, et al. The relation of innate and adaptive immunity with viral-induced acute asthma attacks: focusing on IP-10 and cathelicidin. Allergol Immunopathol. 2017;45((2)):160–8. doi: 10.1016/j.aller.2016.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin CL, Hsiao G, Wang CC, Lee YL. Imperatorin exerts antiallergic effects in Th2-mediated allergic asthma via induction of IL-10-producing regulatory T cells by modulating the function of dendritic cells. Pharmacol Res. 2016;110:111–21. doi: 10.1016/j.phrs.2016.04.030. [DOI] [PubMed] [Google Scholar]
- 28.Abdelaziz MH, Abdelwahab SF, Wan J, Cai W, Huixuan W, Jianjun C, et al. Alternatively activated macrophages; a double-edged sword in allergic asthma. J Transl Med. 2020;18((1)):58. doi: 10.1186/s12967-020-02251-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Puggioni F, Alves-Correia M, Mohamed MF, Stomeo N, Mager R, Marinoni M, et al. Immunostimulants in respiratory diseases: focus on Pidotimod. Multidiscip Respir Med. 2019;14:31. doi: 10.1186/s40248-019-0195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ege MJ. The hygiene hypothesis in the age of the microbiome. Ann Am Thorac Soc. 2017;14((Suppl 5)):S348–53. doi: 10.1513/AnnalsATS.201702-139AW. [DOI] [PubMed] [Google Scholar]
- 31.Miftahussurur M, Nusi IA, Graham DY, Yamaoka Y, Helicobacter Hygiene, atopy, and asthma. Front Microbiol. 2017;8:1034. doi: 10.3389/fmicb.2017.01034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones MG. Understanding of the molecular mechanisms of allergy. Methods Mol Biol. 2019;2020:1–15. doi: 10.1007/978-1-4939-9591-2_1. [DOI] [PubMed] [Google Scholar]
- 33.Leaker BR, Singh D, Lindgren S, Almqvist G, Eriksson L, Young B, et al. Effects of the Toll-like receptor 7 (TLR7) agonist, AZD8848, on allergen-induced responses in patients with mild asthma: a double-blind, randomised, parallel-group study. Respir Res. 2019;20((1)):288. doi: 10.1186/s12931-019-1252-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matsushima K, Nagai S. Unraveling the mystery of the hygiene hypothesis through Helicobacter pylori infection. J Clin Invest. 2012;122((3)):801–4. doi: 10.1172/JCI61466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palomares O, Yaman G, Azkur AK, Akkoc T, Akdis M, Akdis CA. Role of Treg in immune regulation of allergic diseases. Eur J Immunol. 2010;40((5)):1232–40. doi: 10.1002/eji.200940045. [DOI] [PubMed] [Google Scholar]
- 36.Daschner A, González Fernández J. Allergy in an evolutionary framework. J Mol Evol. 2020;88((1)):66–76. doi: 10.1007/s00239-019-09895-3. [DOI] [PubMed] [Google Scholar]
- 37.Asayama K, Kobayashi T, D'Alessandro-Gabazza CN, Toda M, Yasuma T, Fujimoto H, et al. Protein S protects against allergic bronchial asthma by modulating Th1/Th2 balance. Allergy. 2020;75((9)):2267–78. doi: 10.1111/all.14261. [DOI] [PubMed] [Google Scholar]
- 38.Hwang YH, Kim SJ, Yee ST. Physcion-matured dendritic cells induce the differentiation of Th1 cells. Int J Mol Sci. 2020;21((5)):1753. doi: 10.3390/ijms21051753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu C, Li Z, Feng J, Tang Y, Qin L, Hu X, et al. Glucocorticoids modulate Th1 and Th2 responses in asthmatic mouse models by inhibition of notch1 signaling. Int Arch Allergy Immunol. 2018;175((1–2)):44–52. doi: 10.1159/000485890. [DOI] [PubMed] [Google Scholar]
- 40.Chen Z, Liu N, Xiao J, Wang Y, Dong R. The amygdala via the paraventricular nucleus regulates asthma attack in rats. CNS Neurosci Ther. 2020;26((7)):730–40. doi: 10.1111/cns.13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hwang YH, Paik MJ, Yee ST. Diisononyl phthalate induces asthma via modulation of Th1/Th2 equilibrium. Toxicol Lett. 2017;272:49–59. doi: 10.1016/j.toxlet.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 42.Hong ZW, Yang YC, Pan T, Tzeng HF, Fu HW. Differential effects of DEAE negative mode chromatography and gel-filtration chromatography on the charge status of Helicobacter pylori neutrophil-activating protein. PLoS One. 2017;12((3)):e0173632. doi: 10.1371/journal.pone.0173632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Amedei A, Codolo G, Del Prete G, de Bernard M, D'Elios MM. The effect of Helicobacter pylori on asthma and allergy. J Asthma Allergy. 2010;3:139–47. doi: 10.2147/JAA.S8971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.D'Elios MM, Codolo G, Amedei A, Mazzi P, Berton G, Zanotti G, et al. Helicobacter pylori, asthma and allergy. FEMS Immunol Med Microbiol. 2009;56((1)):1–8. doi: 10.1111/j.1574-695X.2009.00537.x. [DOI] [PubMed] [Google Scholar]
- 45.Konturek PC, Rienecker H, Hahn EG, Raithel M. Helicobacter pylori as a protective factor against food allergy. Med Sci Monit. 2008;14((9)):CR452–8. [PubMed] [Google Scholar]
- 46.Karakullukcu A, Tokman HB, Nepesov S, Demirci M, Saribas S, Vehid S, et al. The protective role of Helicobacter pylori neutrophil-activating protein in childhood asthma. Allergol Immunopathol. 2017;45((6)):521–7. doi: 10.1016/j.aller.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 47.Zhou S, Huang Y, Liang B, Dong H, Yao S, Chen Y, et al. Systemic and mucosal pre-administration of recombinant Helicobacter pylori neutrophil-activating protein prevents ovalbumin-induced allergic asthma in mice. FEMS Microbiol Lett. 2017;364((2)):fnw288. doi: 10.1093/femsle/fnw288. [DOI] [PubMed] [Google Scholar]
- 48.Liu X, Fu G, Ji Z, Huang X, Ding C, Jiang H, et al. A recombinant DNA plasmid encoding the sIL-4R-NAP fusion protein suppress airway inflammation in an OVA-induced mouse model of asthma. Inflammation. 2016;39((4)):1434–40. doi: 10.1007/s10753-016-0375-6. [DOI] [PubMed] [Google Scholar]
- 49.Zhao Y, Yang J, Gao YD, Guo W. Th17 immunity in patients with allergic asthma. Int Arch Allergy Immunol. 2010;151((4)):297–307. doi: 10.1159/000250438. [DOI] [PubMed] [Google Scholar]
- 50.Massoud AH, Charbonnier LM, Lopez D, Pellegrini M, Phipatanakul W, Chatila TA. An asthma-associated IL4R variant exacerbates airway inflammation by promoting conversion of regulatory T cells to TH17-like cells. Nat Med. 2016;22((9)):1013–22. doi: 10.1038/nm.4147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang ZE, Zhou XN, Yang Y, Liu ZY. [Effect of Jian'erle granule on Thl7/Treg imbalance of asthma mice] Zhongguo Zhong Xi Yi Jie He Za Zhi. 2016;36((12)):1510–4. [PubMed] [Google Scholar]
- 52.Zhu J, Yamane H, Paul WE. Differentiation of effector CD4 T cell populations. Annu Rev Immunol. 2010;28:445–89. doi: 10.1146/annurev-immunol-030409-101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peng J, Li XM, Zhang GR, Cheng Y, Chen X, Gu W, et al. TNF-TNFR2 signaling inhibits Th2 and Th17 polarization and alleviates allergic airway inflammation. Int Arch Allergy Immunol. 2019;178((3)):281–90. doi: 10.1159/000493583. [DOI] [PubMed] [Google Scholar]
- 54.Park SC, Kim H, Bak Y, Shim D, Kwon KW, Kim CH, et al. An alternative dendritic cell-induced murine model of asthma exhibiting a robust Th2/Th17-skewed response. Allergy Asthma Immunol Res. 2020;12((3)):537–55. doi: 10.4168/aair.2020.12.3.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Go HN, Lee SH, Cho HJ, Ahn JR, Kang MJ, Lee SY, et al. Effects of chloromethylisothiazolinone/methylisothiazolinone (CMIT/MIT) on Th2/Th17-related immune modulation in an atopic dermatitis mouse model. Sci Rep. 2020;10((1)):4099. doi: 10.1038/s41598-020-60966-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lin CC, Wang YY, Chen SM, Liu YT, Li JQ, Li F, et al. Shegan-Mahuang decoction ameliorates asthmatic airway hyperresponsiveness by downregulating Th2/Th17 cells but upregulating CD4+FoxP3+ Tregs. J Ethnopharmacol. 2020;253:112656. doi: 10.1016/j.jep.2020.112656. [DOI] [PubMed] [Google Scholar]
- 57.Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16((1)):45–56. doi: 10.1038/ni.3049. [DOI] [PubMed] [Google Scholar]
- 58.Choy DF, Hart KM, Borthwick LA, Shikotra A, Nagarkar DR, Siddiqui S, et al. TH2 and TH17 inflammatory pathways are reciprocally regulated in asthma. Sci Transl Med. 2015;7((301)):301ra129. doi: 10.1126/scitranslmed.aab3142. [DOI] [PubMed] [Google Scholar]
- 59.Li HT, Lin YS, Ye QM, Yang XN, Zou XL, Yang HL, et al. Airway inflammation and remodeling of cigarette smoking exposure ovalbumin-induced asthma is alleviated by CpG oligodeoxynucleotides via affecting dendritic cell-mediated Th17 polarization. Int Immunopharmacol. 2020;82:106361. doi: 10.1016/j.intimp.2020.106361. [DOI] [PubMed] [Google Scholar]
- 60.Nadeem A, Ahmad SF, Al-Harbi NO, Ibrahim KE, Siddiqui N, Al-Harbi MM, et al. Inhibition of Bruton's tyrosine kinase and IL-2 inducible T-cell kinase suppresses both neutrophilic and eosinophilic airway inflammation in a cockroach allergen extract-induced mixed granulocytic mouse model of asthma using preventative and therapeutic strategy. Pharmacol Res. 2019;148:104441. doi: 10.1016/j.phrs.2019.104441. [DOI] [PubMed] [Google Scholar]
- 61.Santana FPR, da Silva RC, Grecco SDS, Pinheiro AJMCR, Caperuto LC, Arantes-Costa FM, et al. Inhibition of MAPK and STAT3-SOCS3 by sakuranetin attenuated chronic allergic airway inflammation in mice. Mediators Inflamm. 2019;2019:1356356. doi: 10.1155/2019/1356356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cui H, Huang J, Lu M, Zhang Q, Qin W, Zhao Y, et al. Antagonistic effect of vitamin E on nAl2O3-induced exacerbation of Th2 and Th17-mediated allergic asthma via oxidative stress. Environ Pollut. 2019;252((Pt B)):1519–31. doi: 10.1016/j.envpol.2019.06.092. [DOI] [PubMed] [Google Scholar]
- 63.Kardan M, Rafiei A, Ghaffari J, Valadan R, Morsaljahan Z, Haj-Ghorbani ST. Effect of ginger extract on expression of GATA3, T-bet and ROR-γt in peripheral blood mononuclear cells of patients with allergic asthma. Allergol Immunopathol. 2019;47((4)):378–85. doi: 10.1016/j.aller.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 64.Nemattalab M, Shenagari M, Taheri M, Mahjoob M, Nazari Chamaki F, Mojtahedi A, et al. Co-expression of Interleukin-17A molecular adjuvant and prophylactic Helicobacter pylori genetic vaccine could cause sterile immunity in Treg suppressed mice. Cytokine. 2020;126:154866. doi: 10.1016/j.cyto.2019.154866. [DOI] [PubMed] [Google Scholar]
- 65.Lina T, Gonzalez J, Pinchuk I, Beswick E, Reyes V. Helicobacter pylori elicits B7H3 expression on gastric epithelial cells: implications in local T cell regulation and subset development during infection. Clin Oncol Res. 2019;2((5)):2–12. doi: 10.31487/j.cor.2019.05.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kyburz A, Müller A. Helicobacter pylori and extragastric diseases. Curr Top Microbiol Immunol. 2017;400:325–47. doi: 10.1007/978-3-319-50520-6_14. [DOI] [PubMed] [Google Scholar]
- 67.Jafarzadeh A, Larussa T, Nemati M, Jalapour S. T cell subsets play an important role in the determination of the clinical outcome of Helicobacter pylori infection. Microb Pathog. 2018;116:227–36. doi: 10.1016/j.micpath.2018.01.040. [DOI] [PubMed] [Google Scholar]
- 68.Lehours P, Ferrero RL. Review: helicobacter: inflammation, immunology, and vaccines. Helicobacter. 2019;24((Suppl 1)):e12644. doi: 10.1111/hel.12644. [DOI] [PubMed] [Google Scholar]
- 69.Gong Y, Tao L, Jing L, Liu D, Hu S, Liu W, et al. Association of TLR4 and Treg in Helicobacter pylori colonization and inflammation in mice. PLoS One. 2016;11((2)):e0149629. doi: 10.1371/journal.pone.0149629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nezafat N, Eslami M, Negahdaripour M, Rahbar MR, Ghasemi Y. Designing an efficient multi-epitope oral vaccine against Helicobacter pylori using immunoinformatics and structural vaccinology approaches. Mol Biosyst. 2017;13((4)):699–713. doi: 10.1039/c6mb00772d. [DOI] [PubMed] [Google Scholar]
- 71.Arnold IC, Dehzad N, Reuter S, Martin H, Becher B, Taube C, et al. Helicobacter pylori infection prevents allergic asthma in mouse models through the induction of regulatory T cells. J Clin Invest. 2011;121((8)):3088–93. doi: 10.1172/JCI45041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hussain K, Letley DP, Greenaway AB, Kenefeck R, Winter JA, Tomlinson W, et al. Helicobacter pylori-mediated protection from allergy is associated with IL-10-secreting peripheral blood regulatory T cells. Front Immunol. 2016;7:71. doi: 10.3389/fimmu.2016.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kyburz A, Fallegger A, Zhang X, Altobelli A, Artola-Boran M, Borbet T, et al. Transmaternal Helicobacter pylori exposure reduces allergic airway inflammation in offspring through regulatory T cells. J Allergy Clin Immunol. 2019;143((4)):1496–e11. doi: 10.1016/j.jaci.2018.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lambrecht BN, Hammad H. Biology of lung dendritic cells at the origin of asthma. Immunity. 2009;31((3)):412–24. doi: 10.1016/j.immuni.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 75.Lee DCP, Tay NQ, Thian M, Prabhu N, Furuhashi K, Kemeny DM. Prior exposure to inhaled allergen enhances anti-viral immunity and T cell priming by dendritic cells. PLoS One. 2018;13((1)):e0190063. doi: 10.1371/journal.pone.0190063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Amon L, Lehmann CHK, Baranska A, Schoen J, Heger L, Dudziak D. Transcriptional control of dendritic cell development and functions. Int Rev Cell Mol Biol. 2019;349:55–151. doi: 10.1016/bs.ircmb.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 77.Oertli M, Müller A. Helicobacter pylori targets dendritic cells to induce immune tolerance, promote persistence and confer protection against allergic asthma. Gut Microbes. 2012;3((6)):566–71. doi: 10.4161/gmic.21750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Arnold IC, Hitzler I, Müller A. The immunomodulatory properties of Helicobacter pylori confer protection against allergic and chronic inflammatory disorders. Front Cell Infect Microbiol. 2012;2:10. doi: 10.3389/fcimb.2012.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Oertli M, Sundquist M, Hitzler I, Engler DB, Arnold IC, Reuter S, et al. DC-derived IL-18 drives Treg differentiation, murine Helicobacter pylori-specific immune tolerance, and asthma protection. J Clin Invest. 2012;122((3)):1082–96. doi: 10.1172/JCI61029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Oertli M, Noben M, Engler DB, Semper RP, Reuter S, Maxeiner J, et al. Helicobacter pylori γ-glutamyl transpeptidase and vacuolating cytotoxin promote gastric persistence and immune tolerance. Proc Natl Acad Sci USA. 2013;110((8)):3047–52. doi: 10.1073/pnas.1211248110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shiu J, Czinn SJ, Kobayashi KS, Sun Y, Blanchard TG. IRAK-M expression limits dendritic cell activation and proinflammatory cytokine production in response to Helicobacter pylori. PLoS One. 2013;8((6)):e66914. doi: 10.1371/journal.pone.0066914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Farrokhi S, Abbasirad N, Movahed A, Khazaei HA, Pishjoo M, Rezaei N. TLR9-based immunotherapy for the treatment of allergic diseases. Immunotherapy. 2017;9((4)):339–46. doi: 10.2217/imt-2016-0104. [DOI] [PubMed] [Google Scholar]
- 83.Månsson Kvarnhammar A, Tengroth L, Adner M, Cardell LO. Innate immune receptors in human airway smooth muscle cells: activation by TLR1/2, TLR3, TLR4, TLR7 and NOD1 agonists. PLoS One. 2013;8((7)):e68701. doi: 10.1371/journal.pone.0068701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lucas K, Maes M. Role of the Toll like receptor (TLR) radical cycle in chronic inflammation: possible treatments targeting the TLR4 pathway. Mol Neurobiol. 2013;48((1)):190–204. doi: 10.1007/s12035-013-8425-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.George JA, Park SO, Choi JY, Uyangaa E, Eo SK. Double-faced implication of CD4(+) Foxp3(+) regulatory T cells expanded by acute dengue infection via TLR2/MyD88 pathway. Eur J Immunol. 2020;50((7)):1000–18. doi: 10.1002/eji.201948420. [DOI] [PubMed] [Google Scholar]
- 86.Nawijn MC, Motta AC, Gras R, Shirinbak S, Maazi H, van Oosterhout AJ. TLR-2 activation induces regulatory T cells and long-term suppression of asthma manifestations in mice. PLoS One. 2013;8((2)):e55307. doi: 10.1371/journal.pone.0055307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sanchez-Zauco N, Del Rio-Navarro B, Gallardo-Casas C, Del Rio-Chivardi J, Muriel-Vizcaino R, Rivera-Pazos C, et al. High expression of Toll-like receptors 2 and 9 and Th1/Th2 cytokines profile in obese asthmatic children. Allergy Asthma Proc. 2014;35((3)):34–41. doi: 10.2500/aap.2014.35.3749. [DOI] [PubMed] [Google Scholar]
- 88.Piao W, Xiong Y, Li L, Saxena V, Smith KD, Hippen KL, et al. Regulatory T cells condition lymphatic endothelia for enhanced transendothelial migration. Cell Rep. 2020;30((4)):1052–62.e5. doi: 10.1016/j.celrep.2019.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Thio CL, Lai AC, Chi PY, Webster G, Chang YJ. Toll-like receptor 9-dependent interferon production prevents group 2 innate lymphoid cell-driven airway hyperreactivity. J Allergy Clin Immunol. 2019;144((3)):682–97.e9. doi: 10.1016/j.jaci.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 90.Shalaby KH, Al Heialy S, Tsuchiya K, Farahnak S, McGovern TK, Risse PA, et al. The TLR4-TRIF pathway can protect against the development of experimental allergic asthma. Immunology. 2017;152((1)):138–49. doi: 10.1111/imm.12755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dong M, Yu H, Wang Y, Sun C, Chang Y, Yin Q, et al. Critical role of toll-like receptor 4 (TLR4) in ricin toxin-induced inflammatory responses in macrophages. Toxicol Lett. 2020;321:54–60. doi: 10.1016/j.toxlet.2019.12.021. [DOI] [PubMed] [Google Scholar]
- 92.Borbet TC, Zhang X, Muller A, Blaser MJ. The role of the changing human microbiome in the asthma pandemic. J Allergy Clin Immunol. 2019;144((6)):1457–66. doi: 10.1016/j.jaci.2019.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pachathundikandi SK, Muller A, Backert S. Inflammasome activation by Helicobacter pylori and its implications for persistence and immunity. Curr Top Microbiol Immunol. 2016;397:117–31. doi: 10.1007/978-3-319-41171-2_6. [DOI] [PubMed] [Google Scholar]
- 94.Koch KN, Hartung ML, Urban S, Kyburz A, Bahlmann AS, Lind J, et al. Helicobacter urease-induced activation of the TLR2/NLRP3/IL-18 axis protects against asthma. J Clin Invest. 2015;125((8)):3297–302. doi: 10.1172/JCI79337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pachathundikandi SK, Blaser N, Backert S. Mechanisms of inflammasome signaling, microRNA induction and resolution of inflammation by Helicobacter pylori. Curr Top Microbiol Immunol. 2019;421:267–302. doi: 10.1007/978-3-030-15138-6_11. [DOI] [PubMed] [Google Scholar]
- 96.Ying L, Ferrero RL. Role of NOD1 and ALPK1/TIFA signalling in innate immunity against Helicobacter pylori infection. Curr Top Microbiol Immunol. 2019;421:159–77. doi: 10.1007/978-3-030-15138-6_7. [DOI] [PubMed] [Google Scholar]
- 97.van Heel DA, Ghosh S, Butler M, Hunt K, Foxwell BM, Mengin-Lecreulx D, et al. Synergistic enhancement of Toll-like receptor responses by NOD1 activation. Eur J Immunol. 2005;35((8)):2471–6. doi: 10.1002/eji.200526296. [DOI] [PubMed] [Google Scholar]
- 98.Ng MT, Van't Hof R, Crockett JC, Hope ME, Berry S, Thomson J, et al. Increase in NF-kappaB binding affinity of the variant C allele of the toll-like receptor 9-1237T/C polymorphism is associated with Helicobacter pylori-induced gastric disease. Infect Immun. 2010;78((3)):1345–52. doi: 10.1128/IAI.01226-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dela Pena-Ponce MG, Jimenez MT, Hansen LM, Solnick JV, Miller LA. The Helicobacter pylori type IV secretion system promotes IL-8 synthesis in a model of pediatric airway epithelium via p38 MAP kinase. PLoS One. 2017;12((8)):e0183324. doi: 10.1371/journal.pone.0183324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kumar P, Singh G, Goyal JP, Khera D, Singh K. Association of common comorbidities with asthma in children: a cross-sectional study. Sudan J Paediatr. 2019;19((2)):88–92. doi: 10.24911/SJP.106-1544873451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rogliani P, Sforza M, Calzetta L. The impact of comorbidities on severe asthma. Curr Opin Pulm Med. 2020;26((1)):47–55. doi: 10.1097/MCP.0000000000000640. [DOI] [PubMed] [Google Scholar]
- 102.Lankarani KB, Honarvar B, Athari SS. The mechanisms underlying Helicobacter pylori-mediated protection against allergic asthma. Tanaffos. 2017;16((4)):251–9. [PMC free article] [PubMed] [Google Scholar]
- 103.Hufnagl K, Pali-Scholl I, Roth-Walter F, Jensen-Jarolim E. Dysbiosis of the gut and lung microbiome has a role in asthma. Semin Immunopathol. 2020;42((1)):75–93. doi: 10.1007/s00281-019-00775-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ver Heul A, Planer J, Kau AL. The human microbiota and asthma. Clin Rev Allergy Immunol. 2019;57((3)):350–63. doi: 10.1007/s12016-018-8719-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lerias JR, Paraschoudi G, de Sousa E, Martins J, Condeco C, Figueiredo N, et al. Microbes as master immunomodulators: immunopathology, cancer and personalized immunotherapies. Front Cell Dev Biol. 2019;7:362. doi: 10.3389/fcell.2019.00362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.McAleer JP, Kolls JK. Contributions of the intestinal microbiome in lung immunity. Eur J Immunol. 2018;48((1)):39–49. doi: 10.1002/eji.201646721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Budden KF, Gellatly SL, Wood DL, Cooper MA, Morrison M, Hugenholtz P, et al. Emerging pathogenic links between microbiota and the gut-lung axis. Nat Rev Microbiol. 2017;15((1)):55–63. doi: 10.1038/nrmicro.2016.142. [DOI] [PubMed] [Google Scholar]
- 108.Bassis CM, Erb-Downward JR, Dickson RP, Freeman CM, Schmidt TM, Young VB, et al Analysis of the upper respiratory tract microbiotas as the source of the lung and gastric microbiotas in healthy individuals. mBio. 2015;6((2)):e00037. doi: 10.1128/mBio.00037-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mukherjee S, Hanidziar D. More of the gut in the lung: how two microbiomes meet in ARDS. Yale J Biol Med. 2018;91((2)):143–9. [PMC free article] [PubMed] [Google Scholar]
- 110.He Y, Wen Q, Yao F, Xu D, Huang Y, Wang J. Gut-lung axis: the microbial contributions and clinical implications. Crit Rev Microbiol. 2017;43((1)):81–95. doi: 10.1080/1040841X.2016.1176988. [DOI] [PubMed] [Google Scholar]
- 111.Anand S, Mande SS. Diet, microbiota and gut-lung connection. Front Microbiol. 2018;9:2147. doi: 10.3389/fmicb.2018.02147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Frati F, Salvatori C, Incorvaia C, Bellucci A, Di Cara G, Marcucci F, et al. The role of the microbiome in asthma: the gut(−)lung axis. Int J Mol Sci. 2018;20((1)):123. doi: 10.3390/ijms20010123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Samuelson DR, Welsh DA, Shellito JE. Regulation of lung immunity and host defense by the intestinal microbiota. Front Microbiol. 2015;6:1085. doi: 10.3389/fmicb.2015.01085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gupta N, Kumar R, Agrawal B. New players in immunity to tuberculosis: the host microbiome, lung epithelium, and innate immune cells. Front Immunol. 2018;9:709. doi: 10.3389/fimmu.2018.00709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wang J, Li F, Wei H, Lian ZX, Sun R, Tian Z. Respiratory influenza virus infection induces intestinal immune injury via microbiota-mediated Th17 cell-dependent inflammation. J Exp Med. 2014;211((12)):2397–410. doi: 10.1084/jem.20140625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Vital M, Harkema JR, Rizzo M, Tiedje J, Brandenberger C. Alterations of the murine gut microbiome with age and allergic airway disease. J Immunol Res. 2015;2015:892568. doi: 10.1155/2015/892568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ojha UC, Singh DP, Choudhari OK, Gothi D, Singh S. Correlation of severity of functional gastrointestinal disease symptoms with that of asthma and chronic obstructive pulmonary disease: a multicenter study. Int J Appl Basic Med Res. 2018;8((2)):83–8. doi: 10.4103/ijabmr.IJABMR_258_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hauptmann M, Schaible UE. Linking microbiota and respiratory disease. FEBS Lett. 2016;590((21)):3721–38. doi: 10.1002/1873-3468.12421. [DOI] [PubMed] [Google Scholar]
- 119.Stiemsma LT, Turvey SE. Asthma and the microbiome: defining the critical window in early life. Allergy Asthma Clin Immunol. 2017;13:3. doi: 10.1186/s13223-016-0173-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mendez R, Banerjee S, Bhattacharya SK, Banerjee S. Lung inflammation and disease: a perspective on microbial homeostasis and metabolism. IUBMB Life. 2019;71((2)):152–65. doi: 10.1002/iub.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cheng M, Cao L, Ning K. Microbiome big-data mining and applications using single-cell technologies and metagenomics approaches toward precision medicine. Front Genet. 2019;10:972. doi: 10.3389/fgene.2019.00972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chiu L, Bazin T, Truchetet ME, Schaeverbeke T, Delhaes L, Pradeu T. Protective microbiota: from localized to long-reaching co-immunity. Front Immunol. 2017;8:1678. doi: 10.3389/fimmu.2017.01678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Baturcam E, Snape N, Yeo TH, Schagen J, Thomas E, Logan J, et al. Human metapneumovirus impairs apoptosis of nasal epithelial cells in asthma via HSP70. J Innate Immun. 2017;9((1)):52–64. doi: 10.1159/000449101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Liu L, Huang Y, Feng X, Chen J, Duan Y. Overexpressed Hsp70 alleviated formaldehyde-induced apoptosis partly via PI3K/Akt signaling pathway in human bronchial epithelial cells. Environ Toxicol. 2019;34((4)):495–504. doi: 10.1002/tox.22703. [DOI] [PubMed] [Google Scholar]
- 125.Harkins MS, Moseley PL, Iwamoto GK. Regulation of CD23 in the chronic inflammatory response in asthma: a role for interferon-gamma and heat shock protein 70 in the TH2 environment. Ann Allergy Asthma Immunol. 2003;91((6)):567–74. doi: 10.1016/S1081-1206(10)61536-0. [DOI] [PubMed] [Google Scholar]
- 126.Yombo DJK, Mentink-Kane MM, Wilson MS, Wynn TA, Madala SK. Heat shock protein 70 is a positive regulator of airway inflammation and goblet cell hyperplasia in a mouse model of allergic airway inflammation. J Biol Chem. 2019;294((41)):15082–94. doi: 10.1074/jbc.RA119.009145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Huang X, Tan X, Liang Y, Hou C, Qu D, Li M, et al. Differential DAMP release was observed in the sputum of COPD, asthma and asthma-COPD overlap (ACO) patients. Sci Rep. 2019;9((1)):19241. doi: 10.1038/s41598-019-55502-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yan L, Xiao-Ling S, Zheng-Yan C, Guo-Ping L, Sen Z, Zhuang C. HSP70/CD80 DNA vaccine inhibits airway remodeling by regulating the transcription factors T-bet and GATA-3 in a murine model of chronic asthma. Arch Med Sci. 2013;9((5)):906–15. doi: 10.5114/aoms.2013.33180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Jiang H, Zhang X, Chi X, Wang J, Wang J, Dou J. [The effect of inhaled glucocorticoid therapy on serum proteomics of asthmatic patients] Zhonghua Jie He He Hu Xi Za Zhi. 2014;37((4)):274–8. [PubMed] [Google Scholar]
- 130.Saremi K, Rad SK, Khalilzadeh M, Hussaini J, Majid NA. In vivo acute toxicity and anti-gastric evaluation of a novel dichloro Schiff base: Bax and HSP70 alteration. Acta Biochim Biophys Sin. 2020;52((1)):26–37. doi: 10.1093/abbs/gmz140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.deFoneska A, Kaunitz JD. Gastroduodenal mucosal defense. Curr Opin Gastroenterol. 2010;26((6)):604–10. doi: 10.1097/MOG.0b013e32833f1222. [DOI] [PubMed] [Google Scholar]
- 132.Sidahmed HM, Azizan AH, Mohan S, Abdulla MA, Abdelwahab SI, Taha MM, et al. Gastroprotective effect of desmosdumotin C isolated from Mitrella kentii against ethanol-induced gastric mucosal hemorrhage in rats: possible involvement of glutathione, heat-shock protein-70, sulfhydryl compounds, nitric oxide, and anti-Helicobacter pylori activity. BMC Complement Altern Med. 2013;13:183. doi: 10.1186/1472-6882-13-183. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 133.Tao L, Zou H, Huang Z. Effects of Helicobacter pylori and heat shock protein 70 on the proliferation of human gastric epithelial cells. Gastroenterol Res Pract. 2014;2014:794342. doi: 10.1155/2014/794342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pierzchalski P, Krawiec A, Ptak-Belowska A, Baranska A, Konturek SJ, Pawlik WW. The mechanism of heat-shock protein 70 gene expression abolition in gastric epithelium caused by Helicobacter pylori infection. Helicobacter. 2006;11((2)):96–104. doi: 10.1111/j.1523-5378.2006.00383.x. [DOI] [PubMed] [Google Scholar]
- 135.Qu B, Jia Y, Liu Y, Wang H, Ren G, Wang H. The detection and role of heat shock protein 70 in various nondisease conditions and disease conditions: a literature review. Cell Stress Chaperones. 2015;20((6)):885–92. doi: 10.1007/s12192-015-0618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Targosz A, Pierzchalski P, Krawiec A, Szczyrk U, Brzozowski T, Konturek SJ, et al. Helicobacter pylori inhibits expression of heat shock protein 70 (HSP70) in human epithelial cell line. Importance of Cag A protein. J Physiol Pharmacol. 2006;57((2)):265–78. [PubMed] [Google Scholar]
- 137.Taube C, Muller A. The role of Helicobacter pylori infection in the development of allergic asthma. Expert Rev Respir Med. 2012;6((4)):441–9. doi: 10.1586/ers.12.40. [DOI] [PubMed] [Google Scholar]
- 138.Otero LL, Ruiz VE, Perez Perez GI. Helicobacter pylori: the balance between a role as colonizer and pathogen. Best Pract Res Clin Gastroenterol. 2014;28((6)):1017–29. doi: 10.1016/j.bpg.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 139.Blaser MJ. The Jeremiah Metzger Lecture: global warming redux: the disappearing microbiota and epidemic obesity. Trans Am Clin Climatol Assoc. 2012;123:230–8. [PMC free article] [PubMed] [Google Scholar]
- 140.Blaser MJ. The theory of disappearing microbiota and the epidemics of chronic diseases. Nat Rev Immunol. 2017;17((8)):461–3. doi: 10.1038/nri.2017.77. [DOI] [PubMed] [Google Scholar]
- 141.O'Connor A, O'Morain CA, Ford AC. Population screening and treatment of Helicobacter pylori infection. Nat Rev Gastroenterol Hepatol. 2017;14((4)):230–40. doi: 10.1038/nrgastro.2016.195. [DOI] [PubMed] [Google Scholar]
- 142.Yap TW, Leow AH, Azmi AN, Callahan DL, Perez-Perez GI, Loke MF, et al. Global fecal and plasma metabolic dynamics related to Helicobacter pylori eradication. Front Microbiol. 2017;8:536. doi: 10.3389/fmicb.2017.00536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Abadi AT, Kusters JG. Management of Helicobacter pylori infections. BMC Gastroenterol. 2016;16((1)):94. doi: 10.1186/s12876-016-0496-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.van Wijck Y, de Kleijn S, John-Schuster G, Mertens TCJ, Hiemstra PS, Muller A, et al. Therapeutic application of an extract of Helicobacter pylori ameliorates the development of allergic airway disease. J Immunol. 2018;200((5)):1570–9. doi: 10.4049/jimmunol.1700987. [DOI] [PubMed] [Google Scholar]
- 145.Sehrawat A, Sinha S, Saxena A. Helicobacter pylori neutrophil-activating protein: a potential Treg modulator suppressing allergic asthma? Front Microbiol. 2015;6:493. doi: 10.3389/fmicb.2015.00493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.D'Elios MM, Andersen LP. Inflammation, immunity, and vaccines for Helicobacter pylori. Helicobacter. 2009;14((Suppl 1)):21–8. doi: 10.1111/j.1523-5378.2009.00698.x. [DOI] [PubMed] [Google Scholar]
- 147.van Wijck Y, John-Schuster G, van Schadewijk A, van den Oever RL, Obieglo K, Hiemstra PS, et al. Extract of Helicobacter pylori ameliorates parameters of airway inflammation and goblet cell hyperplasia following repeated allergen exposure. Int Arch Allergy Immunol. 2019;180((1)):1–9. doi: 10.1159/000500598. [DOI] [PubMed] [Google Scholar]
- 148.Engler DB, Reuter S, van Wijck Y, Urban S, Kyburz A, Maxeiner J, et al. Effective treatment of allergic airway inflammation with Helicobacter pylori immunomodulators requires BATF3-dependent dendritic cells and IL-10. Proc Natl Acad Sci U S A. 2014;111((32)):11810–5. doi: 10.1073/pnas.1410579111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Bisgaard H, Vissing NH, Carson CG, Bischoff AL, Folsgaard NV, Kreiner-Moller E, et al. Deep phenotyping of the unselected COPSAC2010 birth cohort study. Clin Exp Allergy. 2013;43((12)):1384–94. doi: 10.1111/cea.12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lei J, Vermillion MS, Jia B, Xie H, Xie L, McLane MW, et al. IL-1 receptor antagonist therapy mitigates placental dysfunction and perinatal injury following Zika virus infection. JCI Insight. 2019;4((7)):e122678. doi: 10.1172/jci.insight.122678. [DOI] [PMC free article] [PubMed] [Google Scholar]