Abstract
Baek et al.1 investigated the duration of COVID-19 virus shedding in infected patients and demonstrated that even in patients demonstrating prolonged viral clearance, the virus was no longer viable after 15 days post onset of symptoms. Our study aimed to measure whether nitric oxide nasal spray (NONS) further accelerates this reduction in SARS-CoV-2 RNA load versus a control arm with saline spray. Our study recruited 80 participants who were divided into a NONS treatment arm or a placebo arm to test the efficacy of NONS as a treatment for mild COVID-19 infection.
Keywords: SARS-CoV-2, Prevention, Antiviral, Antimicrobial, COVID-19, Nitric oxide, Coronavirus, Treatment, Nasal Spray
Summary
Baek et al.1 investigated the duration of COVID-19 virus shedding in infected patients and demonstrated that even in patients demonstrating prolonged viral clearance, the virus was no longer viable after 15 days post onset of symptoms. Our study aimed to measure whether nitric oxide nasal spray (NONS) could accelerate the reduction in SARS-CoV-2 RNA load versus control with a saline spray. Our study recruited 80 participants who were divided into a NONS treatment or a placebo arm to test the efficacy of NONS as a treatment for mild COVID-19 infection.
Introduction
The coronavirus (COVID-19) pandemic has had a profound impact on the world, resulting in a worldwide death toll of over 2.6 million and global cases in excess of 119 million as at March 2021.2 These figures demonstrate the necessity of rapidly developing new and effective ways in which to control and treat the virus in support of the emergency use of already-available COVID-19 vaccines.3
There are currently no evidence-based treatments for mild COVID-19 infection. This double-blind phase IIb clinical trial used a placebo control to evaluate the efficacy of nitric oxide in the treatment of mild, symptomatic COVID-19 infection in the form of a self-administered nasal spray. Nitric oxide (NO) is a free radical gas molecule involved in innate immunity, as well as wound healing, vasodilation, neurotransmission, and angiogenesis.4 Although produced physiologically, NO has been shown to exhibit a number of antimicrobial actions at therapeutic dosage regimens both in vitro and in vivo.[5], [6], [7]
Materials and methods
This trial was carried out at Ashford and St. Peter's Hospitals NHS Foundation Trust (ASPHFT). 80 adults (18–70 years) who were isolated with mild COVID-19 infection confirmed by laboratory SARS-CoV-2 RT-PCR nasal and throat swab within the 48 h of randomisation were eligible for recruitment. Participants were randomised 1:1 to receive NONS (n = 40) placebo (n = 40). The nasal sprays were self-administered 5–6 times daily (two sprays per nostril/dose, 120–140 μL of solution/spray) for 9 days.
Treatment with NONS or placebo commenced on day 1. Participants took self-sampled nasal and throat swabs on days 1 (at baseline, before initiating treatments), 2, 4, and 6 in the mornings, prior to treatment. Quantitative RT-PCR was carried out at Berkshire Surrey Pathology Services Virology laboratory to determine SARS-CoV-2 RNA levels. SARS-CoV-2 sequencing for variants was performed at Public Health England Colindale. Daily self-reporting questionnaires on symptoms, compliance, and treatment tolerance were completed by patients and follow-up continues for a total of 18 days.
Results
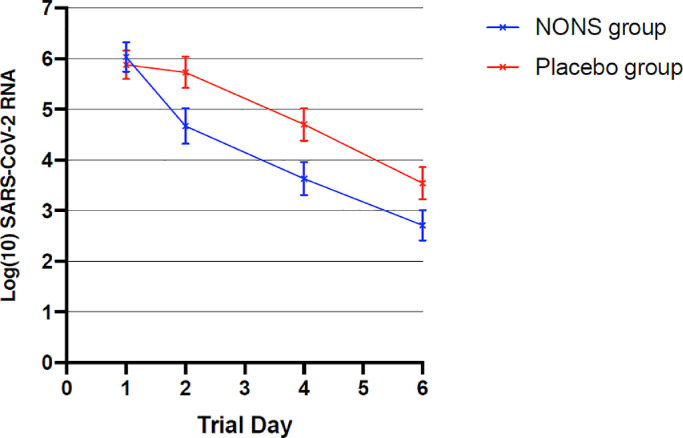
Patients in both trial groups started on NONS or placebo at least 4 days after the onset of symptoms and were well balanced in terms of risk factors (Table 1 ). 34 (85%) of the NONS group and the placebo group were determined to be lineage B.1.1.7 (VOC202012/01) and the remainder were not determined to be a variant of concern. There were no serious adverse events in patients within either trial group. NONS versus placebo started on at least day 4 of symptom onset was independently associated with an accelerated decrease in log(10) SARS-CoV-2 RNA concentration of −1.21 (95% CI, −2.07 to −0.35; P = 0.01) and −1.21 (95% CI, −2.19 to −0.24; P = 0.02) on days 2 and 4 respectively (Fig. 1 ). Mean SARS-CoV-2 RNA concentration was lower on NONS by a factor of 16.2 at days 2 and 4. A rapid reduction (95%) in the SARS-CoV-2 viral load was observed within 24 hours, with a 99% reduction observed within 72 hours with NONS treatments.
Table 1.
Characteristics of the patients at baseline.
| NONS group (n = 40) | Placebo group (n = 40) | p-value | |
|---|---|---|---|
| Age (mean, sd) | 44 (12.1) | 43.9 (12.6) | 0.966 |
| Sex | |||
| Male | 16 (40.0%) | 13 (32.5%) | 0.488 |
| Female | 24 (60.0%) | 27 (67.5%) | |
| Ethnicity | 0.692 | ||
| White | 34 (85.0%) | 37 (92.5%) | |
| Black African + Caribbean | 1 (2.5%) | 0 (0%) | |
| South Asian | 2 (5.0%) | 3 (7.5%) | |
| Mixed | 2 (5.0%) | 0 (0%) | |
| Other | 1 (2.5%) | 0(0%) | |
| BMI | 0.034* | ||
| BMI ≥ 30 | 12 (30.0%) | 7 (17.5%) | |
| BMI < 30 | 19 (47.5%) | 30 (75.0%) | |
| No data | 9 (22.5%) | 3 (7.5%) | |
| Comorbidities | |||
| Any comorbidity | 6 (15.0%) | 4 (10.0%) | 0.502 |
| Chronic lung disease | 2 (5.0%) | 0 (0%) | 0.155 |
| Chronic liver disease | 0 (0%) | 0 (0%) | |
| Chronic heart disease | 0 (0%) | 0 (0%) | |
| Diabetes | 3 (7.5%) | 2 (5.0%) | 0.646 |
| Hypertension | 2 (5.0%) | 3 (7.5%) | 0.646 |
| Presenting symptoms | |||
| Dry cough | 22 (55.0%) | 27 (67.5%) | 0.496 |
| Fever | 7 (17.5%) | 16 (40.0%) | 0.081 |
| Loss of sense of smell | 9 (22.5%) | 5 (12.5%) | 0.323 |
| None of the above | 6 (15.0%) | 8 (17.5%) | 0.743 |
| No data | 5 (12.5%) | 3 (7.5%) | |
| SARS-CoV-2 variant | |||
| B.1.1.7 | 34 (85.0%) | 34 (85.0%) | |
| Not known variant | 6 (15.0%) | 6 (15.0%) |
Fig. 1.
Mean Log(10) SARS-CoV-2 RNA at days 1 to 6
Shown is the difference in the change from baseline in SARS-CoV-2 RNA between the active (NONS) group and the placebo (saline) group from day 1 to day 6. The I bars represent standard error.
The mean SARS-CoV-2 RNA concentration at day 6 was lowered to −3.32 on NONS, with a treatment difference of −0.98 (95% CI, −2.04 to 0.08; P = 0.069). The mean treatment difference using an area under curve estimate from baseline through day 6 was −5.22 with a 95% CI, −9.14 to −1.31; P = 0.001), where the mean change was −10.17 for the NONS group and −4.95 for the placebo group.
40 subjects (15 NONS and 25 placebo subjects) completed and returned the trial assessment questionnaire. A total of 46.7% (7 of 15) of NONS respondents reported feeling better versus 8% (2 of 25) of placebo respondents on treatment. NONS subjects typically reported being better by day 2-4 on treatment, whereas the placebo subjects typically did not report feeling better until after day 5.
Discussion
Treatment with NONS in this trial was found to be effective and safe in reducing the viral load in patients with mild, symptomatic COVID-19 infection. Patients with recent disease onset were enrolled in the trial to evaluate the effect of early intervention with NONS on SARS-CoV-2 RNA load. Patients in the NONS treatment arm demonstrated viral loads, as determined from PCR testing of nose and throat swab sampling, that were lower at days 2 and 4 by a factor of 16.2 than those on placebo, and symptom resolution was also found to be faster on NONS treatment than on placebo in this study.
Lower SARS-CoV-2 RNA loads in patients with NONS may be beneficial in the prevention of SARS-CoV-2 transmission. It has been described that higher viral loads in patients with SARS-CoV-2 earlier than SARS-CoV may have contributed to greater difficulties in reducing the onward transmission.8 Furthermore, it has been observed that the risk of symptomatic COVID-19 was associated with the SARS-CoV-2 RNA levels of contacts and incubation time was shortened in a dose-dependent manner.9
Accelerated SARS-CoV-2 clearance with NONS may reduce symptom duration, decrease infectivity period, reduce hospital admissions, and lower disease severity. Consequently, this study could be used as supporting evidence for emergency use of NONS for patients with mild COVID-19 infection.
Acknowledgements
We would like to thank Dr Chris Miller and Dr Gilly Regev (SaNOtize Research & Development Corporation) for their contribution to the study protocol and content. We would like to thank the study participants, site research staff, site scientific staff and statistician Dr Jonathan Belsey (JB Medical Ltd.). We would also like to thank Dr Kevin Brown (Public Health England) for Virology and Public Health discussion.
Funding
This trial was investigator-led. Funding was provided to Ashford and St Peter's Hospitals NHS Foundation Trust by SaNOtize Research & Development Corporation, Canada, through Metanoic Health Ltd., UK.
The funder of the study conducted the randomisation of the anonymised participant data and provided the study supply materials. They otherwise had no role in study design, data collection, data analysis, data interpretation, or the writing of the report. The researchers are not employed by SaNOtize Research & Development Corporation, Canada, and are independent of the funder.
References
- 1.Baek Y.J., Lee Y.J., Yoon J.S. Duration of culturable SARS-CoV-2 within different specimens among mild and severe COVID-19 patients: a longitudinal study. J Infect. 2021 doi: 10.1016/j.jinf.2021.04.025. doi:https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johns Hopkins University and Medicine . Johns Hopkins University; 2021. COVID-19 map - Johns Hopkins Coronavirus Resource Center.https://coronavirus.jhu.edu/map.html Accessed 14 March. [Google Scholar]
- 3.World Health Organization. Coronavirus disease (COVID-19): herd immunity, lockdowns and COVID-19.https://www.who.int/news-room/q-a-detail/herd-immunity-lockdowns-and-covid-19. December 31, 2020. Accessed February 27, 2021.
- 4.Moncada S., Higgs E. Endogenous nitric oxide: physiology, pathology and clinical relevance. Eu Jof Clin Invest. 1991;21(4):361–374. doi: 10.1111/j.1365-2362.1991.tb01383.x. [DOI] [PubMed] [Google Scholar]
- 5.Fang F. 1997. Perspectives series: host/pathogen interactions. mechanisms of nitric oxide-related antimicrobial activity. J Clin Invest. 1997;99(12):2818–2825. doi: 10.1172/JCI119473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Regev-Shoshani G., Vimalanathan S., McMullin B., Road J., Av-Gay Y., Miller C. Gaseous nitric oxide reduces influenza infectivity in vitro. Nitric Oxide. 2013;31:48–53. doi: 10.1016/j.niox.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Regev-Shoshani G., Vimalanathan S., Prema D. 2014. Safety, bioavailability and mechanism of action of nitric oxide to control bovine respiratory disease complex in calves entering a feedlot. Res Vet Sci. 2014;96(2):328–337. doi: 10.1016/j.rvsc.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Walsh K., Jordan K., Clyne B. SARS-CoV-2 detection, viral load and infectivity over the course of an infection. J Inf. 2020;81:357–371. doi: 10.1016/j.jinf.2020.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marks M, Millat-Martinez P, Ouchi D, et al. Transmission of COVID-19 in 282 clusters in Catalonia, Spain: A cohort study. Lancet Infect Dis. 2021;Feb 2:S1473-3099(20)30985-3. doi: 10.1016/S1473-3099(20)30985-3. Epub ahead of print. [DOI] [PMC free article] [PubMed]