Abstract
Objectives:
To compare the incidence of white spot lesions (WSLs) among patients treated with aligners and those treated with traditional braces.
Materials and Methods:
A group of 244 aligner patients (30.4 ± 14 years) was compared to a group of 206 patients (29.2 ± 11.5 years) treated with traditional fixed braces. Consecutive cases in the late mixed or permanent dentitions who had high-quality pre- and posttreatment digital photographs available were included in the study. Each set of photographs was independently evaluated by two investigators to determine pretreatment oral hygiene (OH), fluorosis, and WSLs, as well as changes in OH and WSLs during treatment.
Results:
Approximately 1.2% of the aligner patients developed WSLs, compared to 26% of the traditionally treated patients. The numbers of WSLs that developed were also significantly (P < .001) less among the aligner patients. The aligner patients developed three new WSLs, while the traditionally treated patients developed 174 WSLs. The incidence of WSLs was greater for the maxillary than for the mandibular teeth, and it was greater for the canines than for the incisors. For the patients treated with traditional braces, fair or poor pretreatment OH, worsening of OH during treatment, preexisting WSLs, and longer treatment duration significantly (P < .05) increased the risk of developing WSLs during treatment.
Conclusions:
Patients treated with aligners have less risk of developing WSLs than do patients treated with traditional braces, which could be partially due to shorter treatment duration, or better pretreatment OH.
Keywords: Aligners, Traditional braces, White spot lesions, Risk factors
INTRODUCTION
Approximately 23% of patients treated in university settings1 and 26% of patients treated in private practice settings2 develop white spot lesions (WSLs) during treatment that are visible on intraoral photographs. Some WSLs improve after treatment,3 and others can be improved with treatment.4,5 However, WSLs often leave permanent scars that can only be repaired by restoring the teeth. Treatment time in excess of 36 months, poor pretreatment hygiene, hygiene changes during treatment, and preexisting WSLs have all been shown to increase the risk of developing WSLs.1,2,6
Orthodontic treatment increases the risk of developing WSLs because fixed orthodontic appliances promote bacterial plaque accumulation and limit the patients' ability to clean their teeth. Following orthodontic bracket placement, oral bacterial counts increase; the more appliances that a patient has in his/her mouth, the greater the increase in bacterial counts.6 Since orthodontic treatment increases plaque buildup/adhesion and reduces the patient's ability to perform oral hygiene (OH), it is reasonable to ask whether “removable” braces would reduce WSL formation. More specifically, should patients treated with aligners be expected to exhibit fewer WSLs than patients treated with traditional braces?
Cross-sectional analyses7 have shown that aligner treatment results in better periodontal health than does fixed orthodontic treatment. Treatment duration is also shorter with aligners, which could limit the development of WSLs.8 The only study9 that evaluated WSLs among orthodontic patients treated with aligners reported an incidence of 2.9%, but the sample size for this study was small and there was no comparison group. Severe decalcification, decay, and even loss of teeth can occur as a consequence of poor OH during clear aligner therapy,10 but the true incidence of WSL among aligner patients remains unknown. To date, there have been no comparisons of patients treated with aligners and traditional braces.
The purpose of the present cohort study was to compare large samples of patients treated with either aligners or traditional braces. Large samples are necessary for accurate estimates of incidence and risk.
MATERIALS AND METHODS
The study was based on cases treated in one private practice and at the Department of Orthodontics, Texas A&M University College of Dentistry. The study was approved by the institution's ethical review committee. There were 244 aligner patients (30.4 ± 14 years) and 206 patients (29.2 ± 11.5 years) treated with traditional fixed appliances. Patients were chosen consecutively, starting with the most recently completed cases. All of the patients received hygiene instructions at the beginning of treatment; patients with poor OH during treatment received additional instructions, as did the parents of younger patients. Approximately 85% of the aligner cases and 48% of the traditional cases came from the private practice. Only patients for whom high-quality pre- and posttreatment digital photographs were available and who were in the late mixed or permanent dentitions were included in the study. No malocclusions were excluded, provided that the gingival thirds of the anterior teeth were visible on the photographs. Chart data collected included the patient's age at procurement of initial records, gender, age at start of treatment, banding age, and debanding age.
Initial and final intraoral photographs were retrieved from the Dolphin Imaging System, placed side by side on a computer monitor, enlarged, and evaluated in a darkened room (Figure 1). Photographs have commonly been used to evaluate the incidence and prevalence of WSLs.1,6,11 OH was evaluated on both pre- and posttreatment photographs. Because the final photographs were taken immediately after debanding and composite removal, different criteria were applied for the pre- and posttreatment photographic evaluations (Table 1). Fluorosis of the anterior teeth was evaluated on the initial photographs only, as a result of composite removal and subsequent enamel desiccation on the posttreatment photographs. Fluorosis, which has been shown to decrease the risk of developing WSLs,1 was deemed significant if it appeared on more than one tooth and extended beyond the incisal edges.
Figure 1.
Examples of pre- and posttreatment photographs of two patients in the traditional braces group and two patients in the aligner group.
Table 1.
Criteria Used for Evaluating Pre- and Posttreatment Oral Hygiene Status (Adapted from Julien et al.1)
| Oral Hygiene |
Pretreatment |
Posttreatment |
| Good | No visible plaque, no gingivitis | No visible plaque, no hypertrophy, gingival bleeding only due to composite removal |
| Fair | Some visible plaque, isolated areas of gingivitis | Some visible plaque, isolated gingivitis or hypertrophy, gingival bleeding only due to composite removal |
| Poor | Thick and/or generalized plaque, with gingivitis | Multiple areas of visible plaque and/or generalized hypertrophy, gingivitis, and gingival bleeding |
Each tooth was evaluated for WSLs by two calibrated investigators who had to agree on the assessments. The two investigators evaluated each case independently. If the side-by-side comparison showed the same white spot on both the pre- and posttreatment photographs, it was considered to be developmental and was not counted as a WSL. White spots noted on the pretreatment photograph that worsened (enlarged or became more severe) over time were recorded as a WSL. New WSLs were also counted.
Chronological age, which was normally distributed based on the skewness and kurtosis statistics, was described with means and standard deviations; group differences were evaluated using an independent sample t-test. Treatment duration was categorized as either less than 2 years or greater than 2 years. Group differences in the number of WSLs, fluorosis, pretreatment hygiene, changes in OH, preexisting WSLs, and treatment duration were evaluated using the chi-square test. The risk ratio was calculated based on the absolute risks (ARs) of the groups being compared (eg, AR females/AR males).
RESULTS
There were no statistically significant between-group differences in pretreatment age (P = .306) or gender (P = .856). Females comprised approximately 64% of the aligner group and 63% of the traditional group. Treatment duration was significantly longer (0.9 years) in the traditional group than in the aligner group (Table 2). There also was a statistically significant (P = .001) between-group difference in pretreatment fluorosis, with 2.0% and 8.7% of the aligner and traditional group patients presenting with fluorosis, respectively. Approximately 9.0% of the aligner group and 10.1% of the traditional group had pretreatment WSLs, a difference that was not statistically significant (P = 0.395).
Table 2.
Pretreatment Ages (Years) and Treatment Durations (Years) of the Aligner and Traditional Groupsa
| Aligner Group |
Traditional Group |
Difference |
|||
| Mean |
SD |
Mean |
SD |
Probability |
|
| Pretreatment age | 29.2 | 11.5 | 30.4 | 14.4 | .306 |
| Treatment duration | 1.5 | 0.9 | 2.5 | 1.3 | <.001 |
SD indicates standard deviation.
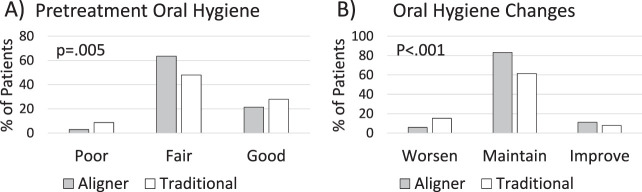
There was a statistically significant (P = .005) between-group difference in pretreatment OH (Figure 2). Slightly greater proportions of patients in the traditional group present with poor (5.7%) and good (6.6%) OH; fewer traditional patients presented with fair (12.3%) OH. There also was a significant between-group difference in OH changes during treatment, with the aligner group having 3.3% more patients who improved and 9.4% fewer patients who worsened. There was no relation between changes of OH during treatment and treatment duration (P = .778).
Figure 2.
Group differences in (A) the percentages of patients with poor, fair, or good pretreatment OH and (B) changes in OH during treatment.
The incidence of WSLs was slightly higher for the maxillary canines (7.3%) than for the maxillary laterals (6%) and was lowest for the maxillary central incisors (2.9%). In the mandible, the canines had the highest incidence of WSLs (7.1%), followed by the lateral incisors (2.6%) and the central incisors (2.2%) (Figure 3). Patients in both groups developed more WSLs on the maxillary than on the mandibular teeth (Table 3). Aligner patients developed WSLs on 0.8% and 0.4% of their maxillary and mandibular teeth, respectively, whereas the traditional group developed lesions on 18.9% of their maxillary and on 15.3% of their mandibular teeth.
Figure 3.
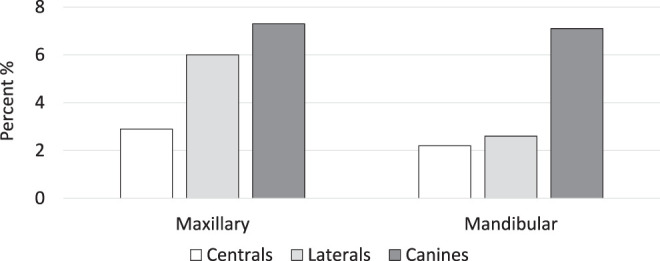
Percentage distributions of WSLs on the central incisors, lateral incisors, and canines (for traditionally treated subjects only).
Table 3.
Percent of Patients Who Developed White Spot Lesions (WSLs) on the Maxillary and Mandibular Teeth
| Aligner Group |
Traditional Group |
Probability |
|||
| Yes |
No |
Yes |
No |
||
| Maxillary WSL | 0.8 | 99.2 | 18.9 | 81.1 | <.001 |
| Mandibular WSL | 0.4 | 99.6 | 15.3 | 84.7 | <.001 |
| Total WSL | 1.2 | 99.8 | 25.7 | 74.3 | <.001 |
Overall, significantly (P < .001) fewer aligner than traditional patients developed WSLs. Only 1.2% of the aligner patients developed WSLs, compared to 25.7% of the traditionally treated patients. The total number of WSLs that developed also were significantly (P < .001) less among the aligner patients than the traditional patients. The three aligner patients who developed WSLs each developed only one WSL; two patients developed WSLs in the maxilla and one patient developed a WSL in the mandible. In contrast, the 52 affected traditional patients each developed between one and 12 WSLs (Figure 4); 86 and 88 new WSLs developed in the maxilla and mandible, respectively. Approximately 3.2% and 29.2% of the aligner and traditional patients, respectively, developed WSLs at the university setting, with a statistically significant between-group difference (P = .001). At the private practice setting, significantly (P < .001) fewer aligner than traditional patients developed WSLs (0.9% vs 22%).
Figure 4.
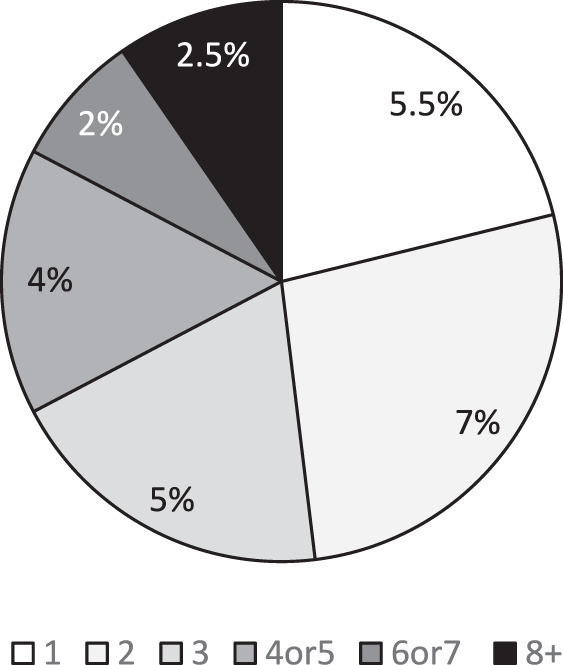
Percent of traditionally treated patients who developed one, two, three, four, or more WSLs.
Traditional Group Risk Factors
As a result of the low incidence of WSLs in the aligner group, only the traditional group was evaluated for risk factors. The sex distribution and pretreatment fluorosis were similar in the patients who did and did not develop WSLs. Pretreatment OH and changes in OH during treatment were significant (P < .001) risk factors (Table 4). Patients with poor and fair pretreatment OH were 6.5 and 3.4 times more likely, respectively, to develop WSLs than were patients with good OH. Patients whose OH worsened during treatment were 3.9 times more likely to develop lesions than were patients who maintained their OH; patients who improved their OH had no risk of developing WSLs during treatment. Patients with preexisting WSLs were also significantly (P < .001) more likely (8.5 times) to develop WSLs during treatment. Finally, patients who were in treatment for more than 2 years were 1.6 times more likely to develop WSLs than were patients treated for less than 2 years.
Table 4.
Risk Factors of Patients in the Traditionally Treated Group Who Did and Did Not Develop White Spot Lesions (WSLs; “Ref” indicates Reference or Comparison Group)
| Developed WSL |
Probability |
Risk Ratio |
||
| No |
Yes |
|||
| Sex | ||||
| Female | 74.6 | 25.4 | .835 | 1.0 |
| Male | 73.7 | 26.3 | Ref | |
| Pretreatment fluorosis | ||||
| Yes | 74.5 | 25.5 | .514 | 1.1 |
| No | 72.8 | 27.8 | Ref | |
| Pretreatment oral hygiene | ||||
| Poor | 42.9 | 57.1 | <.001 | 6.5 |
| Fair | 70.1 | 29.9 | 3.4 | |
| Good | 91.2 | 8.8 | Ref | |
| Change of oral hygiene | ||||
| Worsened | 29.8 | 70.2 | <.001 | 3.9 |
| Maintained | 82.0 | 18.0 | Ref | |
| Improved | 100.0 | 0.0 | 0.00 | |
| Preexiting WSL | ||||
| Yes | 15.9 | 84.1 | <.001 | 8.5 |
| No | 90.1 | 9.9 | Ref | |
| Treatment duration, y | ||||
| <2 | 81.7 | 19.3 | .037 | Ref |
| ≥2 | 69.5 | 30.5 | 1.6 | |
DISCUSSION
There is a substantial risk of developing WSLs among patients treated with traditional orthodontic braces. In the present study, the incidence of visible WSLs during treatment was approximately 26%, indicating that one of every four patients treated with traditional braces is at risk. This compares closely to incidences, ranging from 23% to 28%, reported in several large-scale studies1,2,10 using similar assessment methods. Others6,11,12 who used direct visualization or a combination of direct visualization and photographs to assess WSLs have reported higher incidences, ranging from 36% to 58%, but they had the ability to dry the teeth. The highest reported prevalence of WSLs after orthodontics (97%) was measured using quantitative light-induced fluorescence (QLF).13
Braces might be expected to increase the risk of developing WSLs as a result of increases in salivary bacterial counts,14,15 greater plaque accumulation,16 and difficulties cleaning teeth.
The development of WSLs was closely linked to OH. The traditionally treated patients in the present study who had poor pretreatment OH were 6.5 times more likely to develop WSLs than were those with good OH. Patients whose OH worsened during treatment were 3.9 times more likely to develop WSLs than were those who maintained or improved their OH. Julien et al.1 showed that poor pretreatment hygiene more than doubled the risk, whereas worsening of OH during treatment tripled the risk of developing WSL. The association between poor OH and the risk of developing WSLs has been previously established.6,10
In contrast to patients treated with traditional braces, those treated with removable aligners had a very low incidence of WSLs. Only 1.2% of the aligner patients in the present study developed WSLs. This is even lower than the 2.85% incidence reported9 for a younger and smaller sample treated with clear aligners and evaluated with QLF. It remains unclear whether the low incidences observed with aligners were due to treatment or should be expected for untreated subjects. Approximately 9%–10% of the patients in the present study had pretreatment WSLs, which compares well with the pretreatment prevalence previously reported.1 WSLs form regardless of whether or not individuals undergo orthodontic treatment.
While the present study was the first to compare the incidence of WSLs among aligner and traditional patients, a reduction in WSLs might have been expected. The low incidence of WSLs in patients with removable aligners can be attributed to the shorter treatment durations8 and better hygiene. As a result of the ability to remove the aligners, there are lower levels of plaque and improved OH in aligner patients than in patients treated with traditional braces.7
OH was better maintained in patients with removable aligners than in those with traditionally bonded braces. The present study showed that 94.3% of the aligner patients were able to maintain or even improve their OH during treatment, compared to 84.8% of the traditional patients. This supports the notion that teenagers treated with removable aligners have better OH compliance and better scores on various measures of OH than do patients in traditional braces.17 Aligners allowed the patients to more effectively remove plaque and comply with OH instructions.
There were differences in WSL formation within and between jaws. The present study showed that WSLs were more likely to develop on maxillary than on mandibular teeth, as previously demonstrated.10,11 In patients treated with traditional braces or aligners, the number of WSLs was significantly greater in the maxillary arch. The canines and maxillary lateral incisors appear to be the teeth most susceptible to WSLs. Gorelick et al.11 found the maxillary lateral incisor to be the most frequently affected tooth. The results of Ogaard18 and Mizrahi19 showed that the maxillary laterals and mandibular canines were most affected.
The present study was not without limitations. The sensitivity of diagnosing WSLs could have been increased using QLF or other more sensitive assessment methods that can identify lesions before they become visible. The fact that 85% of the aligner cases and 48% of the fixed cases were drawn from the private practice setting could have biased the results, even though the OH instructions and management of patients with poor OH were similar in both settings. While the incidence of WSLs was slightly higher in the school setting, the relative differences between treatment modalities were similar, with very low incidences of WSLs among aligner patients in both settings. Since the incidence of WSLs among the traditional patients in the present study was similar to rates previously reported,1,2,10 the pretreatment differences in OH could have been counteracted by the pretreatment differences in fluorosis. There also could have been group differences in pretreatment complexity and treatment results, which were not controlled for in the present study. Finally, the longer treatment duration of the traditional group could also explain some of the differences, but aligner treatments are often shorter,8 and very few of the traditional patients were treated beyond the 36 months shown to increase the risk of developing WSLs.1 Randomized trials that control for pretreatment complexity and treatment results are needed to eliminate the pretreatment between-group differences and to minimize differences in treatment duration.
CONCLUSION
Patients treated with aligners have less risk of developing WSLs than do patients treated with traditional braces.
REFERENCES
- 1.Julien KC, Buschang PH, Campbell PM. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013;83:641–647. doi: 10.2319/071712-584.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown MD, Campbell PM, Buschang PH, Schneiderman ED. A practice-based evaluation of the prevalence and predisposing etiology of white spot lesions. Angle Orthod. 2016;86:181–186. doi: 10.2319/041515-249.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shungin D, Olsson AL, Persson M. Orthodontic treatment-related white spot lesions: a 14-year prospecitive quantitative follow-up, including bonding material assessment. Am J Orthod Dentofacial Orthop. 2010;138:136.e1–136.e18. doi: 10.1016/j.ajodo.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 4.Bailey DL, Adams GG, Tsao CE, et al. Regression of post-orthodontic lesions by a remineralizing cream. J Dent Res. 2009;88:1148–1153. doi: 10.1177/0022034509347168. [DOI] [PubMed] [Google Scholar]
- 5.Akin M, Basciftci FA. Can white spot lesions be treated effectively? Angle Orthod. 2012;82:770–775. doi: 10.2319/090711.578.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chapman JA, Roberts WE, Eckert GJ, Kula KS, González-Cabezas C. Risk factors for incidence and severity of white spot lesions during treatment with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010;138:188–194. doi: 10.1016/j.ajodo.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 7.Azaripour A, Weusmann J, Mahmoodi B, et al. Braces versus Invisalign: gingival parameters and patients' satisfaction during treatment: a cross-sectional study. BMC Oral Health. 2015;15:69–74. doi: 10.1186/s12903-015-0060-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buschang PH, Shaw SG, Ross M, Crosby D, Campbell PM. Comparative time efficiency of aligner therapy and conventional edgewise braces. Angle Orthod. 2014;84:391–396. doi: 10.2319/062113-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azeem M, Hamid WU. Incidence of white spot lesions during orthodontic clear aligner therapy. J World Fed Orthod. 2017;6:127–130. [Google Scholar]
- 10.Moshiri M, Eckhart JE, McShane P, German DS. Consequence of poor oral hygiene during aligner therapy. J Clin Orthod. 2013;47:494–498. [PubMed] [Google Scholar]
- 11.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 12.Strateman MW, Shannon IL. Control of decalcification on orthodontic patients by daily self-administered application of water free 0.4% stannous fluoride gel. Am J Orthod Dentofacial Orthop. 1974;66:273–279. doi: 10.1016/0002-9416(74)90291-7. [DOI] [PubMed] [Google Scholar]
- 13.Boersma JG, van der Veen MH, Lagerweij MD, Bokhout B, Prahl-Andersen B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors. Caries Res. 2005;39:41–47. doi: 10.1159/000081655. [DOI] [PubMed] [Google Scholar]
- 14.Bloom RH, Brown LR., Jr A study of the effects of orthodontic appliances on the oral microbial flora. Oral Surg Oral Med Oral Pathol. 1964;17:658–667. doi: 10.1016/0030-4220(64)90373-1. [DOI] [PubMed] [Google Scholar]
- 15.Rosenbloom RG, Tinanoff N. Salivary Streptococcus mutans levels in patients before, during, and after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991;100:35–37. doi: 10.1016/0889-5406(91)70046-Y. [DOI] [PubMed] [Google Scholar]
- 16.Naranjo AA, Trivino ML, Jaramillo A, Betancourth M, Botero JE. Changes in the subgingival microbiota and periodontal parameters before and 3 months after bracket placement. Am J Orthod Dentofacial Orthop. 2006;130:275.e17–275.e22. doi: 10.1016/j.ajodo.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 17.Abbate GM, Caria MP, Montanari P, et al. Periodontal health in teenagers treated with removable aligners and fixed orthodontic appliances. J Orofac Orthop. 2015;76:240–250. doi: 10.1007/s00056-015-0285-5. [DOI] [PubMed] [Google Scholar]
- 18.Ogaard B. Prevalence of white spot lesions in 19-year-olds: a study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989;96:423–427. doi: 10.1016/0889-5406(89)90327-2. [DOI] [PubMed] [Google Scholar]
- 19.Mizrahi E. Surface distribution of enamel opacities following orthodontic treatment. Am J Orthod. 1983;84:323–331. doi: 10.1016/s0002-9416(83)90348-2. [DOI] [PubMed] [Google Scholar]