Thanks to advances in HIV prevention and treatment, such as pre-exposure prophylaxis (PrEP) and treatment as prevention, the overall number of new HIV infections in the United States decreased from 2005 to 2017 (Centers for Disease Control and Prevention, 2018). Despite the overall decrease in HIV cases, certain groups, such as young adults and racial/ethnic minorities remain disproportionately affected. In New York City (NYC), one of the epicenters of the U.S. HIV epidemic, disparities by gender and race/ethnicity persist; Black and Latina women contributed 90% of all new diagnoses among women in 2016 (New York City Department of Health and Mental Hygiene, 2017). Almost two-third (64.9%) of new HIV diagnoses in NYC were in Black and Latino men who have sex with men (MSM)(New York City Department of Health and Mental Hygiene, 2018). Factors contributing to high rates of HIV include poverty, stigma, substance use, and mental health issues (Pellowski, Kalichman, Matthews, & Adler, 2013). Successful sexual health programs must address these social and behavioral determinants of health.
The Ending the Epidemic Blueprint for New York State, established in 2014, recognized the urgent need to enhance low-threshold HIV prevention efforts and enhance multidimensional clinical services with the goal of decreasing HIV incidence, increasing access to prevention services, and driving down prevalence by the end of 2020 (New York State Department of Health, 2015a). Its innovative components include facilitating PrEP access and sustaining retention in prevention care by, among other things, implementing a PrEP assistance program (PrEP-AP) modeled after the AIDS Drug Assistance Program available in every state (New York State Dept of Health, 2015b).
Although overall uptake of PrEP among groups at risk for HIV has been increasing, disparities in access persist and data from the first 3 years of PrEP utilization in the United States reveal that only 10–12% of prescriptions were provided to Blacks and Latinos (Lelutiu-Weinberger, 2016). In New York, a survey conducted in 2015 of approximately 2,000 Black MSM and transgender women revealed low awareness of PrEP (18.2%) and that low awareness was associated with not identifying as gay, being from older age groups, hazardous/harmful alcohol use, greater feelings of stigma toward people living with HIV, and infrequent prior HIV testing (Garnett et al., 2018). Studies have also identified the following barriers experienced by Black MSM trying to access PrEP: medical mistrust, lower efficacy beliefs, not discussing sexual health with providers, stigma, and socioeconomic burdens (Philbin et al., 2016). Latinos expressed similar barriers to PrEP as Black MSM with the addition of language barriers, undocumented status, and lack of health insurance (Page et al., 2017). A study promoting PrEP uptake for Latinos suggested the use of promotores/promotoras, who are trusted community members who could communicate medical language and bridge PrEP services to high-risk Latino communities (Page et al., 2017). These data highlight the urgency for more comprehensive PrEP education and further development of community partnerships with agencies serving Black and Latino MSM.
Translating the success of PrEP from clinical research studies into the real world requires successful implementation of a number of key steps in the PrEP care continuum, starting with education and awareness about PrEP, awareness of risk, linkage to services, initiation of PrEP, adherence and persistence to PrEP, and PrEP retention. Various settings such as sexually transmitted infection (STI) clinics, primary care practices, and community based organizations (CBO) have explored various aspects of the continuum of care and how to best provide PrEP services (Myers, 2018). Although PrEP uptake in NYC increased 9-fold between 2014 and 2016, it is evident that highest risk groups such as (cis) women, people of color, and those not receiving care in community health centers are still under-prescribed PrEP (Salcuni, Smolen, Jain, Myers, & Edelstein, 2017). A review of provider care and interventions to promote PrEP implementation in primary care highlighted the importance of CBO partnership, proper training for providers, financial barriers placed on patients, and time constraints imposed by conducting baseline patient risk assessments and routine HIV/STI screening (Silapaswan, Krakower, & Mayer, 2017).
In this paper, we describe our experiences developing and implementing a multifaceted, community-focused HIV Prevention program in an urban academic medical center located in northern Manhattan. The medical center serves patients in high poverty neighborhoods (ZIP codes in which ≥ 20% of residents live below the federal poverty level) and predominantly Black and Latino communities with high rates of HIV and other STIs. We evaluated the demographics of our program to describe the groups reached. We discuss the key components of developing a successful program in a primarily minority community and lessons learned from the process to serve as a guide to other large hospital networks constructing HIV prevention and education programs.
Methods
Study Population and Setting
Shortly after New York State unveiled its blueprint for ending the epidemic, New York Presbyterian Hospital-Columbia University Irving Medical Center received funding from the NYC Department of Health and Mental Hygiene (NYCDOHMH) and the New York State Department of Health/AIDS Institute to create an HIV Prevention Program. Six specific steps were identified by internal stakeholders as essential to the program’s success: (a) conducting outreach to local community partners and CBOs to bridge the first steps in the PrEP continuum: increasing awareness and facilitate linkages to care; (b) developing the PrEP Specialist role with the goal of training peer navigators representative of communities served by the PrEP program; (c) providing education sessions on PrEP post exposure prophylaxis (PEP) and cultural competency education to health care providers; (d) implementing extended clinic hours and walk-in capacity to increase access to PEP/PrEP- experienced health care providers and PrEP Specialists in clinic settings, (e) providing culturally responsive support and services to younger lesbian, gay, bisexual, transgender, and questioning (LGBTQ) patients; (f) providing patients with access to staff knowledgable about insurance eligibility and drug company medication payment assistance programs with the goal of facilitating PrEP same day access.
A retrospective review of medical records was conducted to find individuals screened for prevention services and to gather data, including descriptions of demographic and behavioral characteristics for those starting PrEP between January 2015 and December 2017. Data were extracted including self-identified race, self-identified ethnicity, age at first visit, risk factors for HIV acquisition, and whether or not they had started PrEP.
Our work was approved by the Columbia University Medical Center Institutional Review Board.
Key Elements of the Program
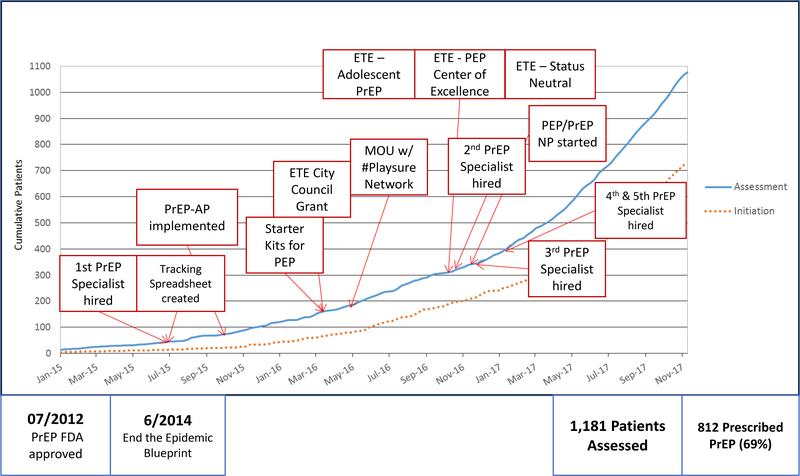
The New York Presbyterian Hospital HIV Prevention Team grew rapidly with regular expansion of staff through the assistance and increased availability of state and city Department of Health funding (Figure 1). The key elements of program implementation are described below.
Figure 1.
Timeline and growth of the New York Presbyterian Hospital HIV Prevention Program from January 2015 through December 2017.
Abbreviations: PrEP = Pre-exposure Prophylaxis; PrEP-AP = Pre-exposure Prophylaxis Assistance Program; PEP=Post Exposure Prophylaxis; ETE=Ending the Epidemic New York State Initiative; MOU = Memorandum of Understanding; NP = Nurse Practitioner
Partnership with local community stakeholders to increase awareness and linkage to PrEP.
Targeted outreach to communities at highest risk of HIV transmission became essential in the structure of the program. This was accomplished through close collaboration with local community partners. The NYCDOHMH established the #Playsure Network early in their efforts for Ending the Epidemic. The aim of the network was to encourage agencies and hospitals to work together to link at-risk individuals to comprehensive sexual health care and, when appropriate, to PrEP. The guiding principle for the initiative was the recognition that individuals who were at risk for HIV but otherwise healthy, would not normally seek health care services and, therefore, might have difficulty locating a clinic to provide them with free access to PrEP. Through the #Playsure Network, NYCDOHMH selected CBOs that were experts in providing support to under-resourced, underinsured, and at-risk individuals. The CBOs were selected, via a competitive process, by the NYCDOHMH because of their longstanding ties in the communities they served. Clinics and hospital networks that provided free or low-cost access to PrEP in a culturally sensitive context were then identified. CBOs were encouraged and incentivized via grant dollars to create formal linkages with selected hospitals/clinics in which the CBOs would find clients in the community who would benefit from PrEP and bring them into the clinical sites.
New York Presbyterian Hospital created a linkage agreement with local CBOs, including the Latino Commission on AIDS (LCOA). LCOA works with uninsured and mostly undocumented Latino MSM and provides them with social support services. LCOA navigators directly escort their clients in need of sexual health services to New York Presbyterian Hospital where the Prevention Specialist team helps clients apply for insurance, if they qualify, or medication assistance programs. New York Presbyterian Hospital linkage with LCOA and other CBOs allowed the team to engage HIV-vulnerable individuals who would not have otherwise had access to our clinic.
Advertisement throughout NYC was funded by the NYCDOHMH and referrals were made to the #Playsure Network Sites so a client could get linked to PrEP care at CBOs listed throughout the city or directly with the funded hospital network. NYCDOHMH also provided grant dollars for funded programs to advertise services in whichever way the organization saw fit (e.g., online, banner ads on hook-up apps, signs at transit stations, outreach events).
Establishing PrEP specialists.
The role of the PrEP Specialist was initially created by the AIDS Institute’s Youth Access Program to train peers to help patients access PrEP. The PrEP Specialist served four key roles: (a) risk reduction counseling, (b) adherence counseling, (c) navigation to health care appointments, and (d) benefits navigation, all with the ultimate goal of the patient receiving health care and PrEP for little or no cost. Obtaining PrEP by applying for insurance or through medication assistance programs was a barrier for most patients and was a daunting undertaking. The PrEP Specialist was able to navigate the patient through the process of receiving free or low-cost medication so that they could access PrEP same day as their health care visit or as quickly as possible.
When recruiting for PrEP Specialists, experience in social work or case management was assessed. More crucial than prior work experience, however, was the importance of recruiting individuals who were able to provide culturally competent, non-judgmental, inclusive care, which was essential to engage and retain patients in sexual health care.
Provider education.
New York Presbyterian Hospital, like most urban hospital networks, has many satellite clinics and spans a large geographic area. During the initiation of the HIV Prevention Program, it was determined that the education of health care providers in the hospital network was as essential as engaging local CBOs. All departments in our hospital, from the Emergency Department to the Ambulatory Care Network satellite clinics, needed to be educated on the availability of PrEP within the hospital.
The New York Presbyterian Hospital HIV Prevention Team conducted presentations at many of the clinics within the hospital network. The talks ranged from an audience of just medical providers to the entire clinic staff based on the needs of the clinic. In the presentations, general PrEP and PEP education was conducted including appropriate sexual history taking techniques.
The goal of the education sessions was to empower providers to incorporate HIV prevention biomedical interventions into their clinical practices while also providing access to resources should issues arise. A key lesson learned from these efforts was the importance of refreshing the sessions frequently during the lifetime of the program. While in-person trainings were effective, as the program grew, web-based and online trainings became an important option that could be adapted to learner levels of training and specialty.
Developing culturally responsive services, expanding clinic access, and LGBTQ youth friendly services.
When an individual who is at high risk for HIV presents to the clinic and expresses interest in starting PrEP, there is an immediate opportunity to intervene and engage the individual. The majority of clinic structures have difficulty accommodating walk-in patients. The New York Presbyterian Hospital/Columbia program decided to accommodate PrEP and PEP walk-ins as much as possible. This initially started with having one clinic session per week designated to seeing walk-in patients only. When that clinic reached regular capacity and further funding was made available, a full time Nurse Practitioner was hired to see PEP and PrEP walk-ins exclusively. The New York Presbyterian Hospital HIV Prevention Team developed walk-in capacity for patients seeking prevention services Monday through Friday from 9 a.m. to 5p.m.
Many younger patients accessing HIV prevention and PrEP services with our program had primary care providers (PCP) at other institutions. A common reason for seeking prevention care outside the PCP included fear of stigma, difficulty discussing sex life with PCP, and PCP discomfort discussing PrEP: “they said I had to go to a specialist.”
Providing culturally competent care that is sensitive and non-stigmatizing to the sexual experiences of younger patients in need of HIV prevention services is essential to the development of any structured PrEP program. Additionally, the employment of diverse staff, with respect to sexual orientation, race, ethnicity, and age, can increase understanding of the needs and experiences of the population and help targeted outreach to high-risk individuals.
Results
Between January 2015 and December 2017, 1181 individuals were assessed for PEP/PrEP eligibility; 70% (832 of 1181) were assessed in 2017, highlighting the dramatic expansion of the program; 55% of those assessed were younger than 30 years of age and the mean age of patients was 30.6 years. African Americans (19.7%) and Hispanics (39%) made up the majority of patients evaluated for PrEP (Table 1). After initial assessment there was no significant difference in those starting or retained on PrEP by race or ethnicity (Zucker, 2018). The major risk factor for HIV acquisition among patients in our program was MSM (83.2%).
Table 1.
Individuals Assessed, Started, and Retained on PrEP by Ethnicity from January 2015 Through December 2017
| Assessed for PrEP N = 1181 | Started PrEP n = 855 | Retained on PrEP at 3 Months*** n = 365 | |
|---|---|---|---|
| Agea | |||
| < 24 years | 283 (24.0%) | 193 (22.6%) | 56 (15.3%) |
| 24 – 29 years | 369 (31.2%) | 327 (38.1%) | 140 (38.4%) |
| ≥ 30 years | 525 | 335 (39%) | 169 (46.3%) |
| Race/Ethnicityb | |||
| Black/African American (not Hispanic) | 233 (19.7%) | 151 (17.5%) | 76 (20.8%) |
| Latino/a | 471 (39.9%) | 354 (41.3%) | 177 (48.5%) |
| White | 343 (29%) | 261 (30.4%) | 115 (31.5%) |
| Asian/Other/Unknown | 128 (10.8%) | 89 (10.4%) | 46 (12.6%) |
| Risk Behaviorc | |||
| MSM | 983 (83.2%) | 766 (89.3%) | 329 (90.1%) |
| MSM having sex with male known to be living with HIV | 79 (6.7%) | 65 (7.6%) | 30 (8.2%) |
| Transgender female having sex with men | 20 (1.7%) | 11 (1.3%) | 4 (1.1%) |
| Cisgender female having sex with men | 92 (7.8%) | 36 (4.2%) | 15 (4.1%) |
| Cisgender female having sex with male known to be living with HIV | 30 (2.5%) | 19 (2.2%) | 10 (2.7%) |
Note. PrEP = pre-exposure prophylaxis, MSM = men who have sex with men.
Numbers do not add up to total N because of missing data
Participant could choose more than one response
Retention data from 1/1/2015–8/31/2017
Discussion
One key lesson learned from our program was that to successfully engage and retain high risk communities in HIV prevention and PrEP programs, collaboration with PCPs, community stakeholders, and networks of CBOs was necessary. The role of the PrEP Specialist was essential to an expanding PrEP program and will need to be replicated as the program expands.
Others have shown that using PrEP counselors and peer navigators contributed to the success of the prevention program and resulted in more PrEP referrals (Chan et al., 2016; Hojilla et al., 2017; Philbin et al., 2016; Silapaswan, et al., 2017). In an analysis from San Francisco, patient navigation support, of which peer navigation was a key component, was associated with a decrease in time between documented first PrEP discussion to actual start of PrEP (Marcus et al., 2016). Our data highlight that it is not only possible to engage, but also retain Black and Latino patients in PrEP services. It does require concerted effort and support from key stakeholders, as exemplified by the #Playsure Network model, to encourage agencies and hospitals to create a collaborative network for individuals at risk for HIV. Provider education was another key component and contributed to the success of the program.
A limitation of our program evaluation and description was the lack of reproducibility in more health-care resource limited settings. Understanding retention in PrEP was challenging as no standard definition for retention in care exists. We recently evaluated our PrEP retention rates and found that,
… age < 30, more recent PrEP initiation, PrEP initiation in the sexual health clinic, and PrEP same-day start were associated with lower retention; while male gender at birth, transition from PEP to PrEP, feeling that they could benefit from, or participating in mental health services were associated with increased retention (Zucker et al., 2018, p. ).
Understanding how we can use this information to improve PrEP persistence in care is part of our continuing efforts to understand the unique set of needs of patients seeking HIV prevention services.
Hispanic/Latino and African American MSM in Upper Manhattan represent a high-risk population in the MSM community regarding new HIV infections. PrEP is an invaluable tool to reduce the rates of infection and help end the epidemic, however it is only useful if it can be delivered to high-risk individuals. We have observed that through a multi-tiered approach, African American and Hispanic/Latino MSM can not only be successfully assessed for PrEP, but can also be initiated and maintained on it. A multiprofessional and culturally competent PrEP program has the potential to remove barriers to PrEP and help make it more accessible to high-risk communities.
Conclusion
Pre-Exposure Prophylaxis is an important component in national efforts to End the HIV Epidemic but key populations are not accessing the HIV prevention services available. Novel and grassroots work is needed with young black and Latino MSM and cis/transwomen to determine how best to engage populations unlikely to access care. Collaboration between hospital networks and community based agencies that are embedded in the communities where engagement is needed is necessary to the success of any Ending the Epidemic Initiative. The addition of a PrEP Specialist to a developing HIV prevention program is a key element. The role provides specialized care in insurance/benefit navigation, risk reduction counseling, adherence support, and community engagement.
Acknowledgments:
This project was funded in part by the NYCDOHMH through a contract with Public Health Solutions. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the funders.
Disclosures: Caroline Carnevale is a recipient of an investigator-led research grant from Gilead Sciences. Dr. Jason Zucker is supported by the training grant, “Training in Pediatric Infectious Diseases” National Institute of Allergy and Infectious Diseases at the National Institutes of Health [T32AI007531 PI: Lisa Saiman].
Contributor Information
Caroline Carnevale, NewYork-Presbyterian Hospital/Columbia University Irving Medical Center.
Jason Zucker, Division of Infectious Diseases, Department of Internal Medicine Columbia University Irving Medical Center.
Alexander Borsa, NewYork-Presbyterian Hospital/Columbia University Irving Medical Center.
Bianka Northland, Division of Infectious Diseases, Department of Internal Medicine Columbia University Irving Medical Center.
Jonathan Castro, NewYork-Presbyterian Hospital/Columbia University Irving Medical Center.
Emma Molina, NewYork-Presbyterian Hospital/Columbia University Irving Medical Center.
Richards Paul, NewYork-Presbyterian Hospital/Columbia University Irving Medical Center.
Dominguez Jose, NewYork-Presbyterian Hospital/Columbia University Irving Medical Center.
George William, NewYork-Presbyterian Hospital/Columbia University Irving Medical Center.
Cohall Alwyn, Professor of Clinical Public Health & Clinical Pediatrics, Mailman School of Public Health & Columbia University Irving Medical Center.
Olender Susan, Division of Infectious Diseases, Department of Internal Medicine Columbia University Irving Medical Center.
Gordon Peter, Division of Infectious Diseases, Department of Internal Medicine Columbia University Irving Medical Center.
E. Sobieszczyk Magdalena, Division of Infectious Diseases, Department of Internal Medicine Columbia University Irving Medical Center.
References
- Centers for Disease Control and Prevention. (2018). HIV surveillance report, 2017. Retrieved from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- Chan PA, Mena L, Patel R, Oldenburg CE, Beauchamps L, Perez‐Brumer AG, … Nunn A (2016). Retention in care outcomes for HIV pre‐exposure prophylaxis implementation programmes among men who have sex with men in three US cities. Journal of the International AIDS Society, 19(1), 20903. doi: 10.7448/IAS.19.1.20903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett M, Hirsch-Moverman Y, Franks J, Hayes-Larson E, El-Sadr WM, & Mannheimer S (2018). Limited awareness of pre-exposure prophylaxis among Black men who have sex with men and transgender women in New York City. AIDS Care, 30(1), 9–17. doi: 10.1080/09540121.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hojilla JC, Vlahov D, Crouch PC, Dawson-Rose C, Freeborn K, & Carrico A (2018). HIV pre-exposure prophylaxis (PrEP) uptake and retention among men who have sex with men in a community-based sexual health clinic. AIDS and Behavior, 22: 1096. 10.1007/s10461-017-2009-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelutiu-Weinberger C, & Golub SA (2016). Enhancing PrEP access for Black and Latino men who have sex with men. Journal of acquired immune deficiency syndromes (1999), 73(5), 547. doi: 10.1097/QAI.0000000000001140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus JL, Volk JE, Pinder J, Liu AY, Bacon O, Hare CB, & Cohen SE (2016). Successful implementation of HIV preexposure prophylaxis: Lessons learned from three clinical settings. Current HIV/AIDS Reports, 13(2), 116–124. 10.1007/s11904-016-0308-x [DOI] [PubMed] [Google Scholar]
- Myers JE, Edelstein ZR, Daskalakis DC, Gandhi AD, Misra K, Rivera AV, … & Braunstein SL (2018). Preexposure Prophylaxis Monitoring in New York City: A Public Health Approach. American journal of public health, 108(S4), S251–S257. doi; 10.2105/AJPH.2018.304729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York City Department of Health and Mental Hygiene. (2017). HIV surveillance annual report, 2016. Retrieved from https://www1.nyc.gov/assets/doh/downloads/pdf/dires/hiv-surveillance-annualreport-2016.pdf
- New York City Department of Health and Mental Hygiene. (2018). HIV surveillance annual report, 2017. Retrieved from https://www1.nyc.gov/assets/doh/downloads/pdf/dires/hiv-surveillance-annualreport-2017.pdf
- New York State Department of Health. (2015a). New York State’s Blueprint to End the AIDS Epidemic. Retrieved from www.health.ny.gov/diseases/aids/ending_the_epidemic/index.htm
- New York State Department of Health. (2015b). Pre-Exposure Prophylaxis Assistance Program (PrEP-AP). Retrieved from https://www.health.ny.gov/diseases/aids/general/resources/adap/prep.htm
- Page KR, Martinez O, Nieves-Lugo K, Zea MC, Grieb SD, Yamanis TJ, … & Davis WW (2017). Promoting pre-exposure prophylaxis to prevent HIV infections among sexual and gender minority Hispanics/Latinxs. AIDS Education and Prevention, 29(5), 389–400. doi: 10.1521/aeap.2017.29.5.389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellowski JA, Kalichman SC, Matthews KA, & Adler N (2013). A pandemic of the poor: Social disadvantage and the US HIV epidemic. American Psychologist, 68(4), 197. doi: 10.1037/a0032694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philbin MM, Parker CM, Parker RG, Wilson PA, Garcia J, & Hirsch JS (2016). The promise of pre-exposure prophylaxis for Black men who have sex with men: An ecological approach to attitudes, beliefs, and barriers. AIDS Patient Care and STDs, 30(6), 282–290. doi: 10.1089/apc.2016.0037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salcuni P, Smolen J, Jain S, Myers J, & Edelstein Z (2017). Trends and associations with PrEP prescription among 602 New York City (NYC) ambulatory care practices, 2014–2016. Open Forum Infectious Diseases, 4(Suppl.1), pp. S21–S21. doi: 10.1093/ofid/ofx162.053 [DOI] [Google Scholar]
- Silapaswan A, Krakower D, & Mayer KH (2017). Pre-exposure prophylaxis: A narrative review of provider behavior and interventions to increase PrEP implementation in primary care. Journal of General Internal Medicine, 32(2), 192–198. doi: 10.1007/s11606-016-3899-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker J, Carnevale C, Richards P, Slowikowski J, Borsa A, Gottlieb F, … Gordon P (2019). Predictors of disengagement in care for individuals receiving pre-exposure prophylaxis (PrEP). Journal of Acquired Immune Deficiency Syndromes. April 11, 2019 - Volume Publish Ahead of Print - Issue – p. doi: 10.1097/QAI.0000000000002054 [DOI] [PMC free article] [PubMed] [Google Scholar]