Abstract
While the influenza vaccine is recommended for all pregnant women, influenza vaccine coverage among this high-risk population remains inadequate. Factors associated with vaccine coverage among pregnant women, including insurance status, are poorly understood. In a cross-sectional study of the National Health Interview Survey (NHIS) data from 2012 to 2018, we evaluated predictors of self-reported influenza vaccine coverage in pregnant women. Among 1942 pregnant women surveyed, 39% reported receiving the influenza vaccine in accordance with national recommendations. Influenza vaccine coverage increased by 8 percentage points from 2012 to 2018. Only 15% of uninsured pregnant women received the influenza vaccine, compared to 41% of those with insurance (design-corrected F-test, p-value <0.001). In the multivariate Poisson regression analysis, significant predictors of influenza vaccine coverage were health insurance (prevalence ratio [PR] 1.90, 95% confidence interval [CI] 1.23–2.93), ratio of household income to federal poverty level (FPL) threshold >400% (PR 1.54, 95% CI 1.20–1.96), graduate school education (PR 1.52, 95% CI 1.04–2.23), and the 2015–2018 survey year period (PR 1.27, 95% CI 1.08–1.49). While previous literature focuses heavily on demographics, our research underscores the need to further explore modifiable factors that impact vaccine uptake during pregnancy, particularly the interplay between health insurance and access to care.
Keywords: maternal vaccination, influenza vaccine, influenza vaccine coverage, pregnant women, determinants
Introduction
The Advisory Committee on Immunization Practices (ACIP) lists pregnant women as a target group for annual influenza vaccine coverage [1]. Not only are pregnant women with influenza more likely to develop cardiopulmonary complications requiring inpatient admission compared to non-pregnant women [2, 3], but infection also confers an increased risk of fetal complications including miscarriage and preterm delivery [3, 4]. The safety and efficacy of the seasonal influenza vaccine during pregnancy is well-established [5, 6]. While the ACIP recommends the influenza vaccine for all women during each pregnancy, vaccine coverage among this high-risk population remains inadequate in the United States. A recent survey of 1,841 pregnant women conducted by the Immunization Services Division of the Centers for Disease Control (CDC) found that only 61.2% received the influenza vaccine during the 2019–2020 season, a 7.5% increase compared to the previous season [7].
While less is understood about routine vaccine coverage among adults as compared to children, previous studies have documented an association between lack of insurance and reduced uptake of immunizations among non-pregnant adults [8]. This is particularly relevant to pregnant women, as all individual, Veterans Affairs, Medicaid, and state Child’s Health Insurance Program insurance policies are now required to cover maternity care and influenza vaccines as of 2014, after the implementation of the Affordable Care Act (ACA) Essential Health Benefits (EHB) provisions [9]. Additionally, women who meet the state-specific federal poverty level (FPL) eligibility criteria can enroll in either full-scope Medicaid or pregnancy-related Medicaid at any point during pregnancy. If uninsured women are not eligible for Medicaid programs, several states offer maternity coverage through CHIP, including coverage for undocumented pregnant women. Estimates of lack of insurance at the time of delivery range from 1.5% to 12.5% [10–12].
Using the National Health Interview Survey (NHIS) data, we performed a cross-sectional study in a population of pregnant women to assess which factors were associated with self-reported influenza vaccine coverage from 2012–2013 (prior to the implementation of the ACA EHB provisions) compared to 2015–2018 (following the implementation of the ACA EHB provisions). We hypothesized that (1) having any type of health insurance was associated with higher influenza vaccine coverage among pregnant women, and (2) influenza vaccine coverage was higher among women in the post-EHB (2015–2018) survey years as compared to the pre-EHB (2012–2013) period. As most women in the United States are now eligible for insurance coverage during pregnancy, lack of insurance among pregnant women may serve as a proxy for difficulty navigating the medical system. Such difficulties may be related to a range of factors leading to inadequate prenatal care, which is a predictor of reduced vaccine uptake among pregnant women. In addition, the implementation of the ACA in 2010 and operationalization of the exchanges and EHB in 2014 led to rapid expansion of insurance coverage, which we hypothesized increased influenza vaccine coverage among pregnant women who were previously uninsured.
Materials and Methods
Data Source
We used the Integrated Public Use Microdata Series (IPUMS) NHIS data collected from 2012 to 2018 [13]. The NHIS is a cross-sectional, face-to-face interview conducted at the respondent’s home based on the non-institutionalized civilian population. The sampling process allows for base weight adjustments based on non-response rates [14]. In 2018, 29,839 households containing 72,831 persons were interviewed. The total household response rate was 64.2%, and the conditional response rate for the sample adult component was 83.9% [14]. The NHIS complex probability design and sampling process minimizes sampling bias, and when using its sampling weights provides estimates that are representative of the non-institutionalized civilian population in the United States. This study used publicly available de-identified data, and was therefore IRB exempt.
Measures
Female sample adults aged 18 to 49 who were pregnant at the time of the interview were asked if they received an influenza vaccine before or during their pregnancy in the past 12 months in accordance with the ACIP recommendations: pregnant women interviewed between January and March or August and December were asked if they received a flu shot before or during the current pregnancy, while women interviewed between April and July who had been pregnant since August 1st of the previous year were asked if they received the flu shot before or during the pregnancy. The structure of this survey question captured the seasonal influenza vaccine schedule, which is offered in the fall and winter in the United States. Influenza vaccine coverage was dichotomized based on an affirmative response to the question (Yes = 1, No = 0). Lack of insurance was based on an affirmative response to a re-coded variable in the NHIS dataset that aggregated responses to a list of health insurance coverage options (Insured = 1, Uninsured = 0).
Age was operationalized as a categorical variable: ages 18 to 30, 30 to 39, and 40 to 49. Race/ethnicity was defined as non-Hispanic White, non-Hispanic Black, Latina, and other, based on self-reported racial identity, using the 1997 revision of Statistical Policy Directive No.15, Race and Ethnic Standards for Federal Statistics and Administrative Reporting. Latina ethnicity was defined by self-reported Hispanic origin or ancestry, regardless of self-reported racial identity. Self-reported Native American, Asian, and multi-racial/other identities were collapsed into the “other” race category given the small sample size. While we acknowledge that race is a social construct, we chose to include race in the model to capture exposure to racism throughout the individual’s life. Although race is a proxy measure for systemic racism, given the extensive documentation of racial discrimination and impact of systemic racism on birth outcomes, particularly for Black women, its inclusion in the model is to remove potential confounding [15]. Educational attainment was defined as: less than high school (HS), HS degree or equivalent (including some college or technical school), college degree, and graduate school.
To account for the high prevalence of missing data with income only, we used the ratio of imputed household income to FPL thresholds, defined as three categories: less than or equal to 138% (level for Medicaid eligibility), 139% to 400% (level for eligibility for premium tax cuts that lower monthly premiums), and greater than 400%. Region of residence was defined as West, South, North Central/Midwest, and Northeast. Delayed care due to cost was defined as an affirmative response to the question “during the past 12 months, have you delayed seeking care because of worry about the cost?” Co-morbid conditions were defined as an asthma attack in the past 12 months, a diagnosis of hypertension (based on at least two provider visits), or diabetes requiring medications (either insulin or oral medications). Data on active immunosuppressive conditions were not available in the NHIS for all years. To evaluate the effects of operationalization of the exchanges and the EHB provisions in 2014, we collapsed the survey years into three categories: the 2012–2013 period (survey years 2012 and 2013), 2014 (treated as a wash-out period), and the 2015–2018 period (survey years 2015 to 2018).
Statistical Analysis
We conducted a cross-sectional analysis of the subpopulation of female adults who reported a current pregnancy at the time of the interview from 2012 to 2018. Descriptive analysis of the influenza vaccine coverage, demographics (age, race, education, ratio of income to FPL thresholds, and co-morbid conditions) and barriers to care (insurance status, and delayed care in the past 12 months due to cost) were performed. We compared the difference between pregnant women who received the influenza vaccine and those who did not receive the vaccine by estimating survey-weighted crude prevalence ratios (PR) and 95% confidence intervals (CI).
A design-corrected F-test was used to assess the association between insurance status and influenza vaccine coverage during pregnancy. We estimated survey-weighted crude PRs of women who received the influenza vaccine compared to those who did not in the 2012–2013 period, as well as the 2015–2018 period. We performed robust Poisson regression of influenza vaccine coverage on each of the independent variables. The final multivariate model consisted of the following variables based on previous literature: age, race/ethnicity, education, ratio of income to FPL thresholds, region, insurance status, delayed care due to cost, co-morbid conditions, and survey year time periods [16–20].
All variables that were unknown, not ascertained or to which the respondent did not know the answer were treated as missing (<1% of sample size). Since each year represented a different pregnancy for women with multiple pregnancies throughout the time period, we chose not to adjust the sample weights. A total of 1,947 women reported a current pregnancy at the time of the interview between 2012 and 2018. There were five unknown responses to the flu shot question: one refused, one was not ascertained, and three did not know. The subpopulation of 1,942 women were evaluated for the final analysis. Statistical analysis was performed using STATA version 16, with statistical significance defined using a two-sided α < 0.05.
Results
Using survey-weighted data, 38.73% of pregnant women reported receiving the influenza vaccine in accordance with ACIP recommendations (unweighted n=728). Table 1 shows the descriptive statistics of 1,942 pregnant women from 2012 to 2018, comparing those who did not receive the influenza vaccine to those who did receive the influenza vaccine. Women who received the influenza vaccine were more likely to have a college degree or graduate school education, more likely to have a ratio of income to FPL threshold greater than 138%, and more likely to have insurance. Women who received the influenza vaccine were less likely to identify as Latina or other, and less likely to report delayed care due to cost in the past 12 months.
Table 1.
Characteristics of pregnant women from 2012 to 2018. by influenza vaccine coverage.
| N = 1942 | Did Not Receive Influenza Vaccine | Received Influenza Vaccine | Crude PR |
|---|---|---|---|
| Age | % [95% CI] | % [95% CI] | PR % [95% CI] |
| 18–29 | 58.23 [54.21, 62.15] | 55.39 [50.97, 59.73] | Reference |
| 30–39 | 37.54 [33.67, 41.58] | 41.74 [37.43, 46.19] | 1.10 [0.95, 1.28] |
| 40–49 | 4.23 [2.97, 5.98] | 2.86 [1.84, 4.43] | 0.80 [0.53, 1.21] |
| Race/Ethnicity | |||
| Non-Hispanic White | 54.06 [49.80, 58.26] | 65.07 [60.60, 69.30] | Reference |
| Non-Hispanic Black | 12.74 [10.51, 15.36] | 12.89 [9.71, 16.91] | 0.90 [0.71, 1.15] |
| Latina | 24.02 [20.83, 27.52] | 15.20 [12.38, 18.54] | 0.66 [0.53, 0.82]*** |
| Othera | 9.18 [7.36, 11.40] | 6.83 [5.02, 9.23] | 0.74 (0.56, 0.98)* |
| Education | |||
| Less than HS Degree | 16.36 [13.80, 19.29] | 8.47 [5.87, 12.06] | Reference |
| HS Degree of Equivalent | 56.53 [52.43, 60.55] | 45.11 [40.45, 49.86] | 1.36 [0.97, 1.90] |
| College Degree | 17.5 [14.91, 20.43] | 27.09 [23.19, 31.38] | 2.01 [1.43, 2.81]*** |
| Graduate School | 9.61 [7.63, 12.03] | 19.33 [15.83, 23.39] | 2.27 [1.61, 3.20)*** |
| Ratio of Income to FPL Thresholds | |||
| Less Than or Equal to 138% | 34.12 [30.65, 37.77] | 19.36 [15.65, 23.70] | Reference |
| 139% to 400% | 41.49 [37.36, 45.75] | 36.40 [31.93, 41.13] | 1.35 [1.07, 1.70]* |
| Greater Than 400% | 24.39 [21.35, 27.70] | 44.24 [39.58, 49.00] | 2.02 [1.64, 2.49]*** |
| Region | |||
| Northeast | 14.53 [12.00, 17.49] | 17.48 [14.39, 21.05] | Reference |
| North Central/Midwest | 23.18 [19.00, 27.96] | 25.34 [21.63, 29.46] | 0.95 [0.74, 1.21] |
| South | 39.42 [35.63, 43.35] | 34.48 [30.08, 39.17] | 0.82 [0.67, 1.02] |
| West | 22.87 [19.83, 26.21] | 22.7 [18.97, 26.90] | 0.89 [0.71, 1.12] |
| Insurance Status | |||
| Uninsured | 10.50 [8.26, 13.25] | 3.02 [1.95, 4.65] | Reference |
| Insured | 89.50 [86.75, 91.74] | 96.98 [95.35, 98.05] | 2.64 [1.71, 4.07]*** |
| Delayed Care Due to Cost in the Past 12 Months | |||
| No | 92.48 [90.41, 94.14] | 96.08 [93.89, 97.51] | Reference |
| Yes | 7.52 [5.86, 9.59] | 3.92 [2.49, 6.11] | 0.62 [0.42, 0.93]* |
| Co-Morbid Conditionsb | |||
| No | 88.63 [86.25, 90.64] | 90.71 [87.73, 93.03] | Reference |
| Yes | 11.37 [9.36, 13.75] | 9.29 [6.97, 12.27] | 0.87 [0.68, 1.11] |
| Unweighted N | 1214 | 728 | |
| Weighted Percentage | 61.27 | 38.73 | |
Crude prevalence ratios calculated with robust Poisson regression using survey-weighted data, Data Source: National Health Interview Survey. 2012 to 2018.
p < 0.001:
p < 0.01
p < 0.05.
Includes Native American. Asian. Multi-Racial, and Other.
Defined as an asthma attack in the past 12 months, a diagnosis of hypertension (based on at least two provider visits), or diabetes requinng medications (either insulin or oral medications).
Figure 1 shows the self-reported prevalence of influenza vaccine coverage among pregnant women by survey year. In 2012, 33.78% of women reported receiving the influenza vaccine, compared to 41.83% in 2018. After 2014, the self-reported prevalence appears to plateau between 40.71% and 44.45%. Table 2 shows the crude prevalence ratios of influenza vaccine coverage stratified by the 2012–2013 and 2015–2018 survey years. Some changes were observed between the two periods: from 2012–2013, women who received the influenza vaccine were more likely to have a graduate school education, while women in the 2015–2018 period were more likely to have a college degree or higher. In both time periods, women who received the influenza vaccine were more likely to report ratio of income to FPL thresholds greater than 400%, and insurance coverage. Women who received the vaccine in the 2012–2013 study period were less likely to report delayed care due to cost in the past 12 months, and less likely to identify as Latina in the 2015–2018 period.
Fig. 1.
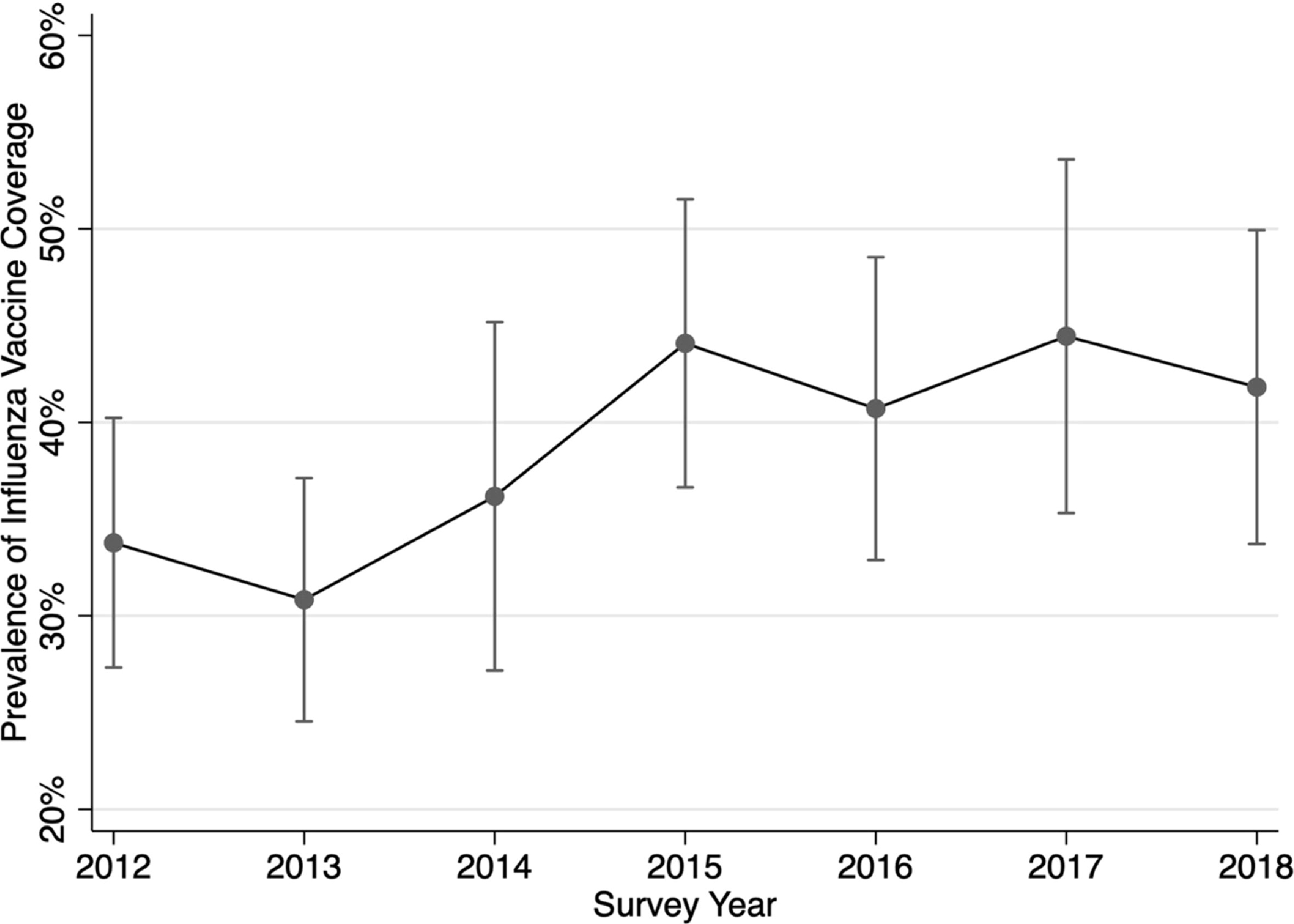
Influenza vaccine coverage by survey year, with 95% confidence intervals.
Table 2.
Crude prevalence ratios of influeiua vaccine coverage among pregnant women, stratified by pre-EHB survey- years 2012–2013 and post-EHB survey years 2015– 2015.
| Years 2012 – 2013 PR [95% CI] |
Years 2015 – 2018 PR [95% CI] |
|
|---|---|---|
| Age | ||
| 18–29 | Reference | Reference |
| 30–39 | 1.25 [0.97, 1.61] | 0.96 [0.80, 1.15] |
| 40–49 | 0.99 [0.44, 2.23] | 0.65 [0.34, 1.27] |
| Race | ||
| Non-Hispamc White | Reference | Reference |
| Non-Hispanic Black | 0.74 [0.46, 1.17] | 0.96 [0.72, 1.27] |
| Latina | 0.80 [0.56, 1.16] | 0.57 [0.43, 0.76]*** |
| Othera | 0.95 [0.59, 1.53] | 0.71 [0.48, 1.06] |
| Education | ||
| Less than HS Degree | Reference | Reference |
| HS Degree of Equivalent | 0.89 [0.57, 1.39] | 1.57 [0.87, 2.84] |
| College Degree | 1.54 [0.97, 2.43] | 2.18 [1.21, 3.93]* |
| Graduate School | 1.68 [1.01, 2.80]* | 2.38 [1.31, 4.34]*** |
| Ratio of Income to FPL Thresholds | ||
| Less Than or Equal to 138% | Reference | Reference |
| 139% to 400% | 1.21 [0.81, 1.81) | 1.35 [1.0, 1.82] |
| Greater Than 400% | 2.31 [1.61, 3.30]*** | 1.84 [1.28, 2.45]*** |
| Region | ||
| Northeast | Reference | Reference |
| North Central/Midwest | 1.13 [0.71, 1.79] | 0.92 [0.70, 1.21] |
| South | 0.94 [0.60, 1.46] | 0.82 [0.63, 1.07] |
| West | 1.14 [0.73, 1.77] | 0.81 [0.61, 1.07] |
| Insurance Status | ||
| Uninsured | Reference | Reference |
| Insured | 2.05 [1.01, 4.19]* | 3.23 [1.83, 5.70]*** |
| Delayed Care Due to Cost in the Past 12 Months | ||
| No | Reference | Reference |
| Yes | 0.50 [0.26, 0.96]* | 0.73 [0.45, 1.20] |
| Co-Morbid Conditionsb | ||
| No | Reference | Reference |
| Yes | 0.78 [0.50, 1.21] | 0.94 [0.68, 1.30] |
| Unweighted N | 214 | 383 |
| Weighted Percentage | 32.36 | 42.78 |
Crude prevalence ratios calculated with robust Poisson regression using survey-weighted data. Data Source: National Health Interview Survey. 2012 to 2018. stratified by pre-2014 and post-2014 periods.
p < 0.001
p < 0.01
p < 0.05.
Includes Native American. Asian. Multi-Racial and Other.
Defined as an asthma attack in the past 12 months, a diagnoses of hypertension (based on at least two provider visits), or diabetes requiring medications (either insulin or oral medications).
From 2012 to 2018, 8.87% of women did not have insurance. Only 15.47% of uninsured women received the influenza vaccine, compared to 40.78% of those with insurance (design-corrected F test, p-value <0.001). Table 3 shows the adjusted prevalence ratios for characteristics associated with influenza vaccine coverage among pregnant women from 2012 to 2018, using the multivariate Poisson regression model. Controlling for other factors, women with insurance had a significantly higher prevalence of influenza vaccine coverage (PR 1.90, 95% CI 1.23 – 2.93). A graduate school education (PR 1.52, 95% CI 1.04 – 2.23), a household income ratio to FPL threshold >400% (PR 1.54, 95% CI 1.20 – 1.96), and inclusion in the 2015 – 2018 survey years (PR 1.27, 95% CI 1.08 – 1.49) were also positively associated with influenza vaccine coverage. The only statistically significant negative predictor in the final model was the other race category (PR 0.69, 95% CI 0.53 – 0.90).
Table 3.
Adjusted prevalence ratios for characteristics associated with influenza vaccine coverage.
| Age | Adjusted PR (95% CI) |
|---|---|
| 18 – 29 | Reference |
| 30 – 39 | 0.90 [0.78, 1.03] |
| 40 – 49 | 0.68 [0.45, 1.03] |
| Race/Ethnicity | |
| Non-Hispanic White | Reference |
| Non-Hispamc Black | 1.10 [0.87, 1.39] |
| Latina | 0.88 [0.71, 1.10] |
| Other | 0.69 [10.53, 0.90]** |
| Education | |
| Less than HS Degree | Reference |
| HS Degree of Equivalent | 1.10 [0.79, 1.54] |
| College Degree | 1.41 [0.99, 2.01] |
| Graduate School | 1.52 [1.04, 2.23]* |
| Ratio of Income to FPL Thresholds | |
| Less Than or Equal to 138% | Reference |
| 139% to 400% | l.20 [0.95, 1.52] |
| Greater Than 400% | l.54 [1.20, 1.96]** |
| Region | |
| Northeast | Reference |
| North Central/Midwest | 0.99 [0.79, 1.24] |
| South | 0.92 [0.75, 1.12] |
| West | 1.05 [0.84 1.31] |
| Insurance Status | |
| Uninsured | Reference |
| Insured | 1.90 [l.23, 2.93]** |
| Delayed Care Due to Cost | |
| No | Reference |
| Yes | 0.79 [0.53, 1.18] |
| Co-Morbid Conditionsb | |
| No | Reference |
| Yes | 0.93 [0.73. 1.18] |
| Survey Years | |
| 2012 – 2013 | Reference |
| 2014 | 1.13 [0.86, 1.49] |
| 2015 – 2018 | 1.27 [1.08, 1.49]** |
Data ate presented as adjusted prevalence ratios with 95% CI calculated with robust Poisson regression using survey weighted data. Data Source: National Health Interview Survey, 2012 to 2018.
p < 0.001
p < 0.01
p < 0.05.
Includes Native Amencaa Asian. Multi Racial aisd Other.
Defined as an asthma attack in the past 12 months, a diagnosis of hypertension (based on at least two provider visits), or diabetes requiring medications 'either insulin or oral medications).
Discussion
Among 1,942 women who reported a pregnancy at the time of the NHIS interview between 2012 and 2018, over one-third reported receiving the influenza vaccine in accordance with ACIP guidelines. Influenza vaccine coverage increased by approximately 10 percentage points in the 2015 – 2018 period compared to the preceding period. The strongest predictor of influenza vaccine coverage in the study population was health insurance: pregnant women with any form of health insurance had significantly higher influenza vaccine coverage. Women who received the influenza vaccine were also more likely to have a graduate school education, and a household income ratio to FPL threshold above 400%.
The vaccine coverage estimates were lower than other studies based on self-reported data collected via internal panel surveys [21, 22], as well as estimates generated with maternal vaccination records [16, 19]. While self-reported vaccine coverage collected via the NHIS face-to-face interview may be more susceptible to social desirability bias, the reported coverage in the 2015 – 2018 survey years was lower than the 49.1% vaccine coverage reported among 1,771 respondents via an internet panel survey during the 2017 – 2018 season [21]. In addition, the internet panel survey may be weighted toward women with access to a smartphone and reliable internet access. This may explain the higher reported vaccine coverage compared to our study, as we found that higher education and income were associated with increased likelihood of vaccination. Vaccine coverage estimates in the 2012 – 2013 period were comparable to those generated from an all-payer claims database in Wisconsin, but lower than estimates generated from matched maternal vaccine records from state records [16]. Regardless, all studies highlight the need to increase influenza vaccine coverage among pregnant women.
Consistent with previous literature in non-pregnant populations, health insurance was associated with increased influenza vaccine coverage in our study. Not only does insurance increase access to care, but we suspect that contact with healthcare personnel functions as a mediator between insurance and increased vaccine coverage, since influenza vaccine recommendation by a healthcare personnel in pregnancy is strongly associated with higher uptake [23, 24]. While inadequate prenatal care is often cited as a predictor of reduced vaccine uptake in pregnancy [16, 25, 26], this may be in fact a direct consequence of lack of insurance, and thus challenging to interpret in isolation. This is particularly important because several prior studies rely primarily on claims data, which is only available for insured populations. Therefore, lack of insurance among pregnant women may represent the primary driver behind reduced vaccine uptake in pregnancy, as opposed to the demographics linked to health insurance which are typically cited.
Higher educational attainment and higher income ratio to FPL thresholds are related, which may explain the positive association with influenza vaccine coverage among pregnant women. Women of lower educational attainment, and income ratio to FPL thresholds below 400% may benefit from targeted public health campaigns on the safety and efficacy of the influenza vaccine during pregnancy. While previous literature documents decreased influenza vaccine uptake among non-Hispanic Black women in pregnancy [16, 18, 25–27], our study did not find a significant association with race, except for the other race category. While health inequities and mistrust among Black women is well-documented as a result of systemic racism, our findings highlight that the mechanism by which race impacts vaccine coverage in pregnancy remains unclear. Race in relation to vaccine coverage among pregnant women may in fact be a confounder when controlling for other variables relating to insurance and access to care. Surprisingly, a co-morbid medical condition was not found to be significantly associated with influenza vaccine coverage in our multivariate analysis, although previous studies have found a higher percentage of pregnant women with chronic conditions received the flu vaccine in bivariate analyses [28].
The cause of increased influenza vaccine coverage among pregnant women during our study period is likely multi-factorial. First, the Healthy People 2020 campaign launched by the Department of Health and Human Services set a goal in 2010 of 80% influenza vaccine coverage for pregnant women after the 2009 H1N1 influenza pandemic disproportionately impacted pregnant women [29]. Second, preventive measures with A and B grades according to the United States Preventive Services Task Force (USPSTF), including annual influenza vaccines, are now covered free of cost under the ACA [30]. Third, the rise in influenza vaccine coverage over the years mirrors the rise in insurance coverage. Influenza vaccine coverage in our population appears to plateau between 2015 and 2018, although further surveillance is warranted to evaluate whether there is in fact a secular trend as documented by previous studies in both pregnant and non-pregnant populations [7, 17, 18, 22, 26, 31].
Our study design has several strengths. First, few studies have examined the direct association between insurance status and influenza vaccine coverage among pregnant women [16]. Second, our study population is relatively large, representing a sample of 1,942 pregnant female respondents from 2012 to 2018. Third, the probability design of the NHIS survey allows for representative sampling of households, and thus minimizes sampling bias [14]. While the significance of associations in an observational study should be interpreted with caution, as confounding and reverse causality cannot be excluded, this analysis helps describe vaccine behavior among a vulnerable population over time. Additionally, the survey question structure was tailored to the month of the survey, which captured the seasonality of the influenza vaccine schedule in the United States.
There are several limitations to our study. First, as noted above, observational studies cannot demonstrate causality. Second, the reason for not receiving an influenza vaccine is not listed as an NHIS variable, which could provide valuable insight into low vaccine uptake, including previously documented concerns among pregnant women about effectiveness [32], side effects [21, 24, 33], and harm to the fetus [21, 33]. It is unclear to what extent the anti-vaccine movement impacts vaccine behavior and hesitancy, which may be better elucidated using a qualitative study. Third, while our statistical model is based on primary literature, the dataset lacked important variables such as receipt of prenatal care, therefore omitted variable bias may threaten the internal validity of our study. Lastly, our findings may be limited by recall bias, as we were unable confirm receipt of the influenza vaccine in this study population. While several vaccination coverage studies in pregnancy rely on self-reported status [7, 21, 22, 34], the reliability of self-report compared to health records is unknown. However, a large telephone survey of 11,760 adults found relatively high agreement between self-reported influenza vaccine coverage and electronic medical records, with a kappa of 0.56 and sensitivity of 93% [35], slightly improved compared to earlier studies [36]. As noted above, while self-reported vaccine coverage estimates may be more prone to social desirability bias, these estimates were in fact lower than data collected via internet panel surveys and matched maternal vaccine receipts from state records.
Conclusions
While influenza vaccine coverage among pregnant women has increased over the years, further work is required to meet the Healthy People 2020 goal of 80% influenza vaccine coverage for pregnant women. This population may benefit from targeted public health campaigns, provider incentives to increase uptake, or further research to understand vaccine decision-making. While previous literature focuses heavily on demographics, our research underscores the need to further explore modifiable factors that impact vaccine uptake in pregnancy, including the interplay between health insurance, household income, and access to care. Uninsured women who unexpectedly become pregnant and do not meet the state-specific criteria for Medicaid or CHIP will remain uninsured. This represents a particularly vulnerable population that may require enhanced focus in future research, and would greatly benefit from the development of creative alternatives for receipt of much needed vaccines.
Funding Sources:
Mary Catherine Cambou was supported by the UCLA Postdoctoral Fellowship Training Program in Global HIV Prevention Research (Currier and Gorbach, PIs); T32MH080634.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Grohskopf LA, Alyanak E, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices - United States, 2019–20 Influenza Season. MMWR Recomm Rep. 2019;68(3):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mertz D, Geraci J, Winkup J, Gessner BD, Ortiz JR, Loeb M. Pregnancy as a risk factor for severe outcomes from influenza virus infection: A systematic review and meta-analysis of observational studies. Vaccine. 2017;35(4):521–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mosby LG, Rasmussen SA, Jamieson DJ. 2009 pandemic influenza A (H1N1) in pregnancy: a systematic review of the literature. Am J Obstet Gynecol. 2011;205(1):10–8. [DOI] [PubMed] [Google Scholar]
- 4.Haberg SE, Trogstad L, Gunnes N, Wilcox AJ, Gjessing HK, Samuelsen SO, et al. Risk of fetal death after pandemic influenza virus infection or vaccination. N Engl J Med. 2013;368(4):333–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madhi SA, Cutland CL, Kuwanda L, Weinberg A, Hugo A, Jones S, et al. Influenza vaccination of pregnant women and protection of their infants. N Engl J Med. 2014;371(10):918–31. [DOI] [PubMed] [Google Scholar]
- 6.Thompson MG, Kwong JC, Regan AK, Katz MA, Drews SJ, Azziz-Baumgartner E, et al. Influenza Vaccine Effectiveness in Preventing Influenza-associated Hospitalizations During Pregnancy: A Multi-country Retrospective Test Negative Design Study, 2010–2016. Clin Infect Dis. 2019;68(9):1444–53. [DOI] [PubMed] [Google Scholar]
- 7.Razzaghi H, Kahn KE, Black CL, Lindley MC, Jatlaoui TC, Fiebelkorn AP, et al. Influenza and Tdap Vaccination Coverage Among Pregnant Women - United States, April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(39):1391–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu PJ, O'Halloran A, Williams WW. Impact of health insurance status on vaccination coverage among adult populations. Am J Prev Med. 2015;48(6):647–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bagley N, Levy H. Essential health benefits and the Affordable Care Act: law and process. J Health Polit Policy Law. 2014;39(2):441–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curtin SC, Osterman M, Uddin S, Sutton S, Reed P. Source of payment for the delivery: births in a 33-state and District of Columbia reporting area, 2010. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2013;62(5):1–20. [PubMed] [Google Scholar]
- 11.D’Angelo DV, Le B, O’Neil ME, Williams L, Ahluwalia IB, Harrison LL, et al. Patterns of health insurance coverage around the time of pregnancy among women with live-born infants—Pregnancy Risk Assessment Monitoring System, 29 states, 2009. Morbidity and Mortality Weekly Report: Surveillance Summaries. 2015;64(4):1–19. [PMC free article] [PubMed] [Google Scholar]
- 12.Daw JR, Hatfield LA, Swartz K, Sommers BD. Women In The United States Experience High Rates Of Coverage 'Churn' In Months Before And After Childbirth. Health Aff (Millwood). 2017;36(4):598–606. [DOI] [PubMed] [Google Scholar]
- 13.Lynn A. Blewett JARD, King Miriam L.and Williams. Kari CW IPUMS Health Surveys: National Health Interview Survey. 6.4 ed. Minneapolis, MN; 2019. [Google Scholar]
- 14.National Center for Health Statistics. National Health Interview Survey, 2018. Public-use data file and documentation 2019 [Available from: https://www.cdc.gov/nchs/nhis/data-questionnairesdocumentation.htm.
- 15.Burris HH, Passarella M, Handley SC, Srinivas SK, Lorch SA. Black-White disparities in maternal in-hospital mortality according to teaching and Black-serving hospital status. Am J Obstet Gynecol. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koepke R, Schauer SL, Davis JP. Measuring maternal Tdap and influenza vaccination rates: Comparison of two population-based methods. Vaccine. 2017;35(18):2298–302. [DOI] [PubMed] [Google Scholar]
- 17.Groom HC, Henninger ML, Smith N, Koppolu P, Cheetham TC, Glanz JM, et al. Influenza Vaccination During Pregnancy: Influenza Seasons 2002–2012, Vaccine Safety Datalink. Am J Prev Med. 2016;50(4):480–8. [DOI] [PubMed] [Google Scholar]
- 18.Henninger M, Crane B, Naleway A. Trends in influenza vaccine coverage in pregnant women, 2008 to 2012. Perm J. 2013;17(2):31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barber A, Muscoplat MH, Fedorowicz A. Coverage with Tetanus, Diphtheria, and Acellular Pertussis Vaccine and Influenza Vaccine Among Pregnant Women - Minnesota, March 2013-December 2014. MMWR Morb Mortal Wkly Rep. 2017;66(2):56–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu E. Influenza vaccination among pregnant women--Massachusetts, 2009–2010. MMWR Morb Mortal Wkly Rep. 2013;62(43):854–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Kahn KE, Black CL, Ding H, Williams WW, Lu PJ, Fiebelkorn AP, et al. Influenza and Tdap Vaccination Coverage Among Pregnant Women - United States, April 2018. MMWR Morb Mortal Wkly Rep. 2018;67(38):1055–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lindley MC, Kahn KE, Bardenheier BH, D'Angelo DV, Dawood FS, Fink RV, et al. Vital Signs: Burden and Prevention of Influenza and Pertussis Among Pregnant Women and Infants - United States. MMWR Morb Mortal Wkly Rep. 2019;68(40):885–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chamberlain AT, Seib K, Ault KA, Rosenberg ES, Frew PM, Cortes M, et al. Improving influenza and Tdap vaccination during pregnancy: A cluster-randomized trial of a multi-component antenatal vaccine promotion package in late influenza season. Vaccine. 2015;33(30):3571–9. [DOI] [PubMed] [Google Scholar]
- 24.Strassberg ER, Power M, Schulkin J, Stark LM, Mackeen AD, Murtough KL, et al. Patient attitudes toward influenza and tetanus, diphtheria and acellular pertussis vaccination in pregnancy. Vaccine. 2018;36(30):4548–54. [DOI] [PubMed] [Google Scholar]
- 25.Doraivelu K, Boulet SL, Biswas HH, Adams JC, Haddad LB, Jamieson DJ. Predictors of tetanus, diphtheria, acellular pertussis and influenza vaccination during pregnancy among full-term deliveries in a medically underserved population. Vaccine. 2019;37(41):6054–9. [DOI] [PubMed] [Google Scholar]
- 26.Ghaswalla P, Poirrier JE, Packnett ER, Irwin DE, Gray SR, Buck PO. Maternal Immunization in the U.S.: A Nationwide Retrospective Cohort Study. Am J Prev Med. 2019;57(3):e87–e93. [DOI] [PubMed] [Google Scholar]
- 27.Influenza vaccination among pregnant women--Massachusetts, 2009–2010. MMWR Morb Mortal Wkly Rep. 2013;62(43):854–7. [PMC free article] [PubMed] [Google Scholar]
- 28.Pregnant Women and Flu Vaccination, Internet Panel Survey, United States, November 2017. [Available from: https://www.cdc.gov/flu/fluvaxview/pregnant-women-nov2017.htm#high-risk. [Google Scholar]
- 29.Office of Disease Prevention and Health Promotion. Increase the percentage of pregnant women who are vaccinated against seasonal influenza [Available from: https://www.healthypeople.gov/node/4660/data_details.
- 30.Seiler N, Malcarney M-B, Horton K, Dafflitto S. Coverage of clinical preventive services under the Affordable Care Act: from law to access. Public Health Rep. 2014;129(6):526–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aris E, Montourcy M, Esterberg E, Kurosky SK, Poston S, Hogea C. The adult vaccination landscape in the United States during the Affordable Care Act era: Results from a large retrospective database analysis. Vaccine. 2020;38(14):2984–94. [DOI] [PubMed] [Google Scholar]
- 32.Gorman JR, Brewer NT, Wang JB, Chambers CD. Theory-based predictors of influenza vaccination among pregnant women. Vaccine. 2012;31(1):213–8. [DOI] [PubMed] [Google Scholar]
- 33.Ahluwalia IB, Jamieson DJ, Rasmussen SA, D'Angelo D, Goodman D, Kim H. Correlates of seasonal influenza vaccine coverage among pregnant women in Georgia and Rhode Island. Obstet Gynecol. 2010;116(4):949–55. [DOI] [PubMed] [Google Scholar]
- 34.Kriss JL, Albert AP, Carter VM, Jiles AJ, Liang JL, Mullen J, et al. Disparities in Tdap Vaccination and Vaccine Information Needs Among Pregnant Women in the United States. Matern Child Health J. 2019;23(2):201–11. [DOI] [PubMed] [Google Scholar]
- 35.Rolnick SJ, Parker ED, Nordin JD, Hedblom BD, Wei F, Kerby T, et al. Self-report compared to electronic medical record across eight adult vaccines: do results vary by demographic factors? Vaccine. 2013;31(37):3928–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Greene SK, Shi P, Dutta-Linn MM, Shoup JA, Hinrichsen VL, Ray P, et al. Accuracy of data on influenza vaccination status at four Vaccine Safety Datalink sites. Am J Prev Med. 2009;37(6):552–5. [DOI] [PubMed] [Google Scholar]


