Video
Video depicts EUS-guided choledochoduodenostomy creation using a biliary fully covered self-expanding metal stent after maldeployment of a lumen-apposing metal stent.
Abbreviations: CBD, common bile duct; LAMS, lumen-apposing metal stent
A 72-year-old man with stage IV renal cell carcinoma presented with obstructive jaundice secondary to a metastasis in the head of the pancreas. CT imaging demonstrated common bile duct dilation up to 15 mm secondary to a 6-cm pancreatic head mass (Fig. 1). ERCP was attempted but failed because of ampullary effacement from malignant invasion. Because the patient was not a surgical candidate, EUS-guided biliary drainage was attempted.
Figure 1.
CT imaging demonstrating common bile duct dilation to 15 mm secondary to a 6-cm pancreatic head mass.
A linear echoendoscope was advanced to the duodenal bulb. The common bile duct (CBD) was then punctured using a 19-gauge aspiration needle. An EUS-guided cholangiogram verified CBD dilation of 15 mm owing to a high-grade distal biliary stricture (Fig. 2). A 0.035-inch guidewire was passed into the CBD via the aspiration needle but was unable to traverse the biliary stricture. Owing to technical failure of EUS-guided rendezvous-assisted ERCP, the guidewire was withdrawn from the CBD. Freehand technique was used to perform EUS-guided choledochoduodenostomy using a 10-mm electrocautery-enhanced lumen-apposing metal stent (LAMS).
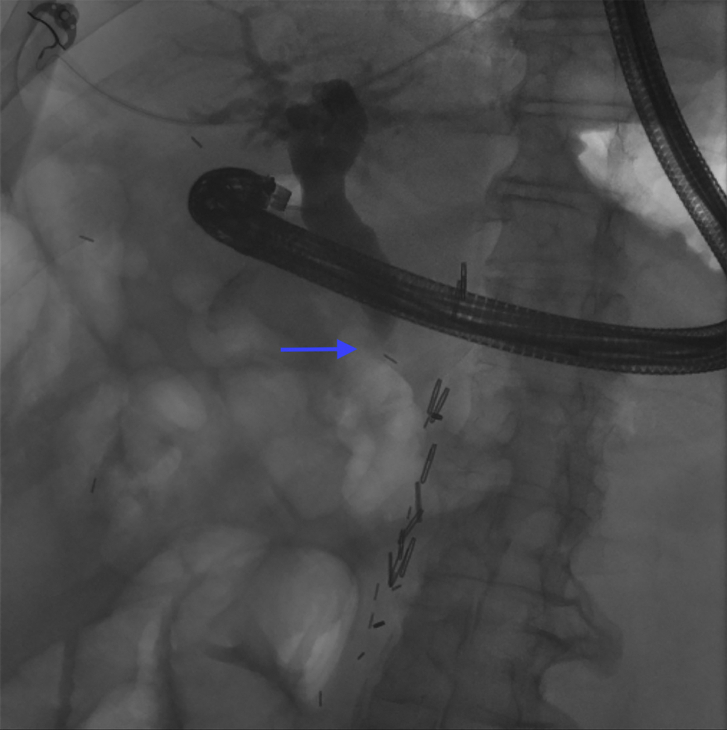
Figure 2.
EUS-guided cholangiogram verifying common bile duct dilation of 15 mm because of a high-grade distal biliary stricture.
The distal flange of the LAMS was dislodged from the CBD during deployment. The CBD perforation was endoscopically visualized through the indwelling duodenal LAMS (Fig. 3). Irritation of the retroperitoneum was appreciated and was likely secondary to the patient’s known malignancy or subclinical bile leakage across the gap that occurred during the time the stent was dislodged.
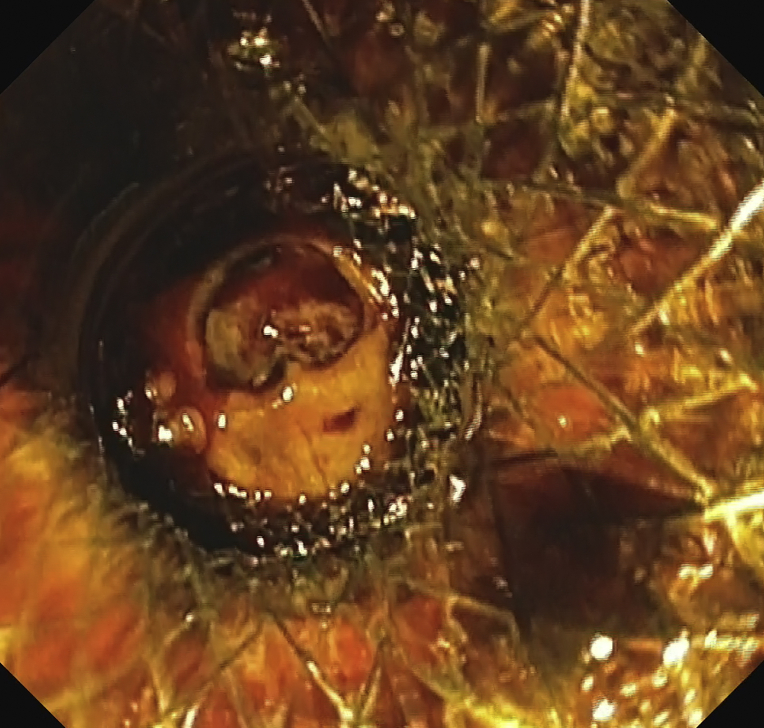
Figure 3.
Endoscopic visualization of common bile duct defect through the indwelling duodenal lumen-apposing metal stent.
The linear echoendoscope was exchanged for a 16F gastroscope that was passed through the duodenal LAMS and into the retroperitoneum. The CBD was intubated, and a 0.025-inch guidewire was advanced into the CBD lumen. The biliary stricture was too tight to allow guidewire passage. The guidewire was then directed into the intrahepatic biliary ductal system.
A bridging 10-mm × 8-cm biliary fully covered self-expanding metal stent was deployed over the guidewire and through the indwelling LAMS (Fig. 4A and B). Contrast dye was injected through the biliary fully covered self-expanding metal stent using a sphincterotome, confirming a successful choledochoduodenostomy creation (Fig. 5). The gastroscope was withdrawn, and the procedure was terminated.
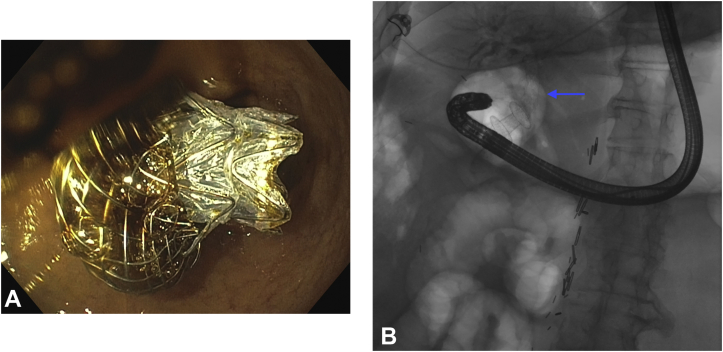
Figure 4.
Direct (A) and Fluoroscopic (B) visualization of the bridging 10-mm × 8-cm biliary fully covered self-expanding metal stent that was deployed over a guidewire and through the indwelling lumen apposing metal stent.
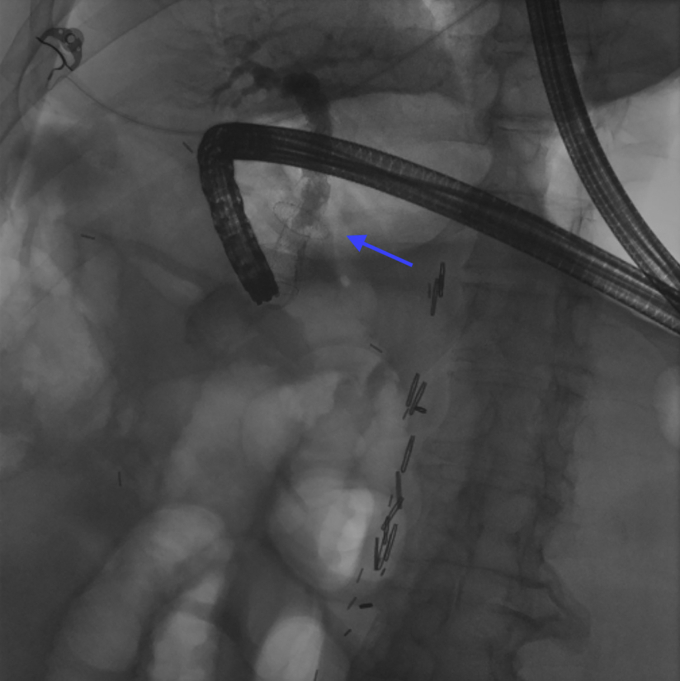
Figure 5.
Verification of choledochoduodenostomy creation via the injection of contrast dye through the biliary fully covered self-expanding metal stent using a sphincterotome.
Before the procedure, the patient’s total bilirubin peaked at 13.6; it improved after his procedure to 5.9 at the time of his discharge 5 days later. He was discharged with a plan to follow up with a repeat ERCP in 3 months (Video 1, available online at www.VideoGIE.org).
Disclosure
Dr Nasr is a consultant for Boston Scientific. All other authors disclosed no financial relationships.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Graves at Mgraves3@hsc.wvu.edu.
Supplementary data
Video depicts EUS-guided choledochoduodenostomy creation using a biliary fully covered self-expanding metal stent after maldeployment of a lumen-apposing metal stent.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video depicts EUS-guided choledochoduodenostomy creation using a biliary fully covered self-expanding metal stent after maldeployment of a lumen-apposing metal stent.
Video depicts EUS-guided choledochoduodenostomy creation using a biliary fully covered self-expanding metal stent after maldeployment of a lumen-apposing metal stent.