Abstract
Remember EPFI as a differential diagnosis in children with a rash on the scalp and no effect of antibiotic treatment.
Keywords: eosinophilic, folliculitis, inflammatory dermatosis
Remember EPFI as a differential diagnosis in children with a rash on the scalp and no effect of antibiotic treatment.

1. INTRODUCTION
Eosinophilic pustular folliculitis of infancy (EPFI) is a rare, very pruritic, benign skin disease that often presents before the age of 2 years. It is often misdiagnosed and treated extensively with antibiotics with no effect. Topical corticosteroids are sufficient in 90% of cases.
Eosinophilic pustular folliculitis of infancy is a pruritic cutaneous disease. It is a benign, self‐limiting condition with an unknown etiology. It is the least characterized subtype of the classic eosinophilic pustular folliculitis described by Ofuji. 1 We here report a pediatric case of EPFI treated with high‐potent topical steroid.
2. CASE PRESENTATION
A 10‐month‐old boy was referred to the pediatric department with pustules and crusts localized to the scalp (Figure 1). The skin rash was treated as impetigo with a combination of oral phenoxymethylpenicillin and dicloxacillin for 14 days. A swab for bacteria was negative. The rash reoccurred 1 week after the antibiotic treatment had ended, and the boy was readmitted to the pediatric department for further treatment. The patient was treated with oral flucloxacillin for another 10 days despite two negative swabs for bacteria. On day 10 of the antibiotic treatment, there was a flare‐up and the oral administered antibiotic was replaced to intravenous dicloxacillin in combination with high‐potent topical steroid. A peripheral blood sample showed eosinophilia of 4.2 × 109/L (<0.5 × 109/L). After 3 days of intravenous dicloxacillin, new pustules appeared and the patient was referred to the dermatology department for further examination. Skin examination showed only a few pustules and postinflammatory hyper‐pigmented areas of the scalp and a few papules on the right ankle. An examination for fungi and a punch biopsy was made. Histopathological examination showed a pustule‐forming eosinophilic folliculitis (Figure 2), and a diagnosis of EPFI was concluded. Topical treatment with betamethasone with clioquinol led to a resolution of the eruption, but with subsequent minor flare‐ups.
FIGURE 1.

The initial presentation of EPFI in our case. Papules, pustules and crust localized to the scalp on a 10‐month‐old boy before any treatment was initiated
FIGURE 2.
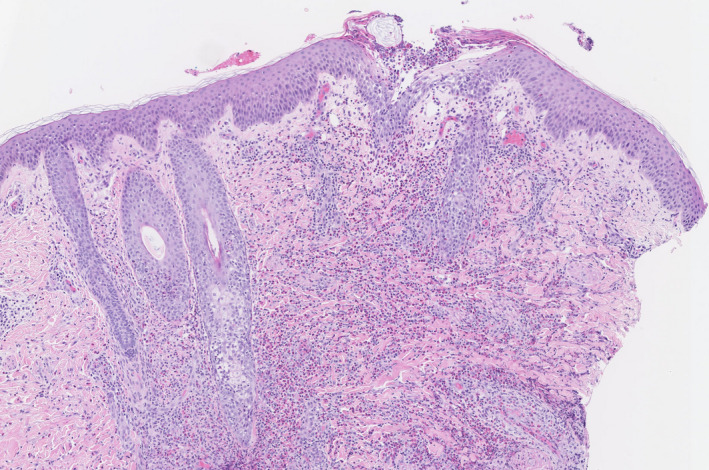
Punch biopsy showing heavy infiltration of eosinophilic granulocytes in and around the hair follicles and an eosinophilic‐rich pustule related to the follicular infundibulum. Hematoxylin and eosin (H&E) staining, original magnification ×70
3. DISCUSSION
Eosinophilic pustular folliculitis of infancy is a rare inflammatory disease characterized with sterile pustules and papules located on the scalp and in 65% of patients also on the trunk and extremities. 2 , 3 A retrospective review of 61 cases revealed that the disease is more common in boys (4:1), and 95% of the described cases presented before 14 months of age. 3
The common histological features are those of an eosinophilic‐rich “spongiotic” pustule related to ostium and infundibulum of the hair follicle with an adjacent heavy infiltrate of eosinophils, lymphocytes, and histiocytes. 4
The clinical differential diagnostic considerations in our case were kerion and langerhans cell histiocytosis, which is often reasoned in the clinical presentation of the EPFI cases.
Eosinophilic pustular folliculitis of infancy belongs to the group of eosinophilic skin diseases. Other differential diagnostic considerations may include erythema toxicum neonatorum, eosinophilic cellulitis, and granuloma faciale. They share the characteristic of eosinophilia in the skin, however, the latter two do not display eosinophilic folliculitis. Like EPFI neither the etiology nor the pathogenesis for these diseases are well understood. 5
There are no treatment guidelines for EPFI, but treatment with mild to moderate topical steroids is effective in 90% of cases. 3 Other treatments are topical tacrolimus and oral antihistamine. 2 , 6 , 7 In refractory cases, treatment with dapsone, erythromycin, and indomethacin has been proposed. 7 , 8
Eosinophilic pustular folliculitis of infancy is a rare skin condition in children and important to be aware of, since it can be challenging to distinguish from our mentioned differential diagnoses, thus often treated unnecessarily extensive with systemic medications as shown in our case.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
ASF, ABO, KAUP: contributed equally in writing the case report. RR‐H: contributed with expert knowledge in pathology and made Figure 2 including the figure legend.
CONSENT STATEMENT
All the mentioned authors consent for publication.
ETHICAL APPROVAL
Written consent was obtained from the patient's mother ahead of submission.
Frølunde AS, Olesen AB, Riber‐Hansen R, Pallesen KAU. Eosinophilic pustular folliculitis of infancy: A rare diagnosis in children. Clin Case Rep. 2021;9:e04167. 10.1002/ccr3.4167
DATA AVAILABILITY STATEMENT
No data were obtained for this case report.
REFERENCES
- 1. Nomura T, Katoh M, Yamamoto Y, Miyachi Y, Kabashima K. Eosinophilic pustular folliculitis: a proposal of diagnostic and therapeutic algorithms. J Dermatol. 2016;43(11):1301‐1306. [DOI] [PubMed] [Google Scholar]
- 2. Demirsoy EO, Demirsoy U, Ozon U, Kiran R. Eosinophilic pustular folliculitis of infancy suppressed with cetirizine. Pediatr Dermatol. 2019;36(3):395‐396. [DOI] [PubMed] [Google Scholar]
- 3. Hernández‐Martín Á, Nuño‐González A, Colmenero I, Torrelo A. Eosinophilic pustular folliculitis of infancy: a series of 15 cases and a review of the literature. J Am Acad Dermatol. 2013;68(1):150‐155. [DOI] [PubMed] [Google Scholar]
- 4. McKee's Pathology of the Skin, Vol 1, 5th edn, Amsterdam, Netherlands: Elsevier; 2020:240. [Google Scholar]
- 5. Peckruhn M, Elsner P, Tittelbach J. Eosinophilic dermatoses. J Dtsch Dermatol Ges. 2019;17(10):1039‐1051. [DOI] [PubMed] [Google Scholar]
- 6. Lee JH, Kang JH, Cho BK, Park HJ. Generalized eosinophilic pustular folliculitis of infancy responding to hydroxyzine. Ann Dermatol. 2015;27(4):458‐460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Patel NP, Laguda B, Roberts NM, Francis ND, Agnew K. Treatment of eosinophilic pustulosis of infancy with topical tacrolimus. Br J Dermatol. 2012;167(5):1189‐1191. [DOI] [PubMed] [Google Scholar]
- 8. Katoh M, Nomura T, Miyachi Y, Kabashima K. Eosinophilic pustular folliculitis: a review of the Japanese published works. J Dermatol. 2013;40(1):15‐20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data were obtained for this case report.


