Abstract
Introduction:
Electronic medical records (EMRs) are computerized medical information systems that collect, store, and display patient information and essential for the achievement of primary health-care goals. This study explores the availability and utilization of EMR and analyzed the barriers inhibiting their implementation at primary health centers (PHCs) in Nalgonda district of Telangana, India.
Methods:
The research employed a sequential mixed-method design. Quantitative data were collected using a questionnaire by conducting facility surveys across 75 PHCs and in-depth interviews with district health authorities were conducted using a predesigned guide. Quantitative data were analyzed using descriptive statistics and thematic analysis of interviews resulted in four themes focusing on the factors inhibiting PHCs to use EMR.
Results:
The availability of EMR facility was low (19.14%) and they are routinely used for maintaining immunization data in 83% of the PHCs. In contrast, none of the PHCs used EMR for prescribing medications to patients. Budgetary constraints, unavailability of dedicated information technology staff, gaps in technical knowledge, and perceptions about EMR as a time-consuming system were the commonly reported barriers inhibiting PHCs to go digital.
Conclusion:
The availability and utilization of EMR keeping was low across PHCs of Nalgonda district. The study identified multiple barriers which hinder the implementation of EMR facilities at PHCs. Addressing these barriers is crucial for the successful implementation of EMR.
Keywords: Electronic health records, electronic medical records, electronic medical records adoption and digital health, primary health care
INTRODUCTION
Information technology (IT) in the health sector has revolutionized and improved the delivery of health-care services globally.[1] In India, health care accounts for approximately 8% of the country's GDP[2] with a scope to increase further. Despite this accessibility, affordability and availability of quality health services remains a challenge. The digital health technologies could potentially serve as a means to overcome these challenges and provide quality health care to many Indians.
Public health services in India are delivered in a three-tier system such as primary, secondary, and tertiary levels.[3] The state delivers a number of financial and nonfinancial health-care benefits to many Indians through its programs and schemes. EMR can enable accurate and easy tracking of these program beneficiaries and automate the process in respect of providers, government, and consumers. Similarly, the use of EMR, especially in primary health centers (PHCs) has the potential to significantly impact the practice of care by improving quality, better referral services, real-time data keeping, preventing duplication of services, and achieving primary health-care goals.[4]
Despite growing evidence of benefits and recognition, the adoption of EMR in public health facilities is arguably low.[5] However, some evidence exists concerning the digitalization of health records along the lines of AADHAAR, recording of health parameters by health workers in a web-based tracking system, use of e-HMS, e-Aushadhi, and the formulation of Integrated Health Dashboard in state health systems.[6,7]
Given the limited evidence of digitalization in public health facilities, especially at the primary level, this study examined the availability and utilization of EMRs and explored the barriers influencing its implementation at PHCs in one of the southern located districts of Telangana, “Nalgonda,” before its bifurcation in the year 2017. The undivided district has a population of 3.48 million and comprised of 59 mandals (subdistricts), 17 towns, 1135 villages, and 75 PHCs.[8,9] Nalgonda district is one of the fluoride affected districts with fluoride content in the groundwater above 1.5 ppm. It is one of the three districts in Telangana with endemic filariasis.[10] In the year 2016–2017, 96% of all the deliveries in the district were institutional, with over 40% of them taking place in government health facilities.[11] According to the NFHS-4, over 10% of women and 19% of men had high blood pressure, over 5% of men and 8.5% of women had high blood sugar levels.[12]
METHODS
We used a sequential mixed-method approach[13] to conduct this research. Both quantitative and qualitative data were collected in sequence for a period of 3 months (December 2018 to February 2019) upon receiving the ethics approval from the Institutional Human Ethics Committee, Central University of Kerala. Quantitative data were collected using an adapted tool, used by Powell et al. in their study in Chandigarh India.[14] The original tool was modified to current study objectives measure the availability and utilization of EMR in nine important domains at PHCs [Table 1]. The tool captured barriers in implementing EHR facilities at the primary health-care level. The analysis of barriers was conducted in respect of ten domains [Table 2]. A total of 75 PHCs were surveyed. The data obtained from facility surveys were analyzed using descriptive statistics in SPSS-20(IBM SPSS Version 20, developed by IBM Corporation, New York).[15] The analysis of “availability” and “utilization” of EMR was calculated overall and specifically for domains. In addition, barriers in implementing EMR were analyzed separately for the domains. Following the surveys, we also conducted 12 face-to-face interviews in Telugu with senior doctors and district health authorities using a semi-structured guide. They were purposively recruited based on convenience sampling technique.[16] Each interview lasted for about 40–45 min which was audio recorded, translated into English, transcribed verbatim in Microsoft Word, coded inductively, and analyzed thematically in ATLAS. Ti-7.57.[17]
Table 1.
Availability status of electronic medical record facilities in primary health centers (n=75)
| Domain | Available percentage |
|---|---|
| Patient’s demographics | 7% (5) |
| Clinical notes | 5% (4) |
| Complaints of patients’ | 5% (4) |
| Patient’s diagnosis | 37.3% (28) |
| Management of current medications | 3% (2) |
| Vital signs | 16% (12) |
| Allergies | 16% (12) |
| Immunization | 83% (62) |
| Prescribing medications | 0% (0) |
| Overall availability | 19.14% |
Table 2.
Barriers in the implementation of the electronic medical record in primary health centers (n=75)
| Domains | Barrier (%) |
|---|---|
| Lack of seed capital to start EMR facility | 97.4 |
| Uncertainty about the RoI | 96.0 |
| Recurring cost associated with EMR implementation | 97.3 |
| Resistance of physicians | 2.6 |
| Lack of capacity and competencies among the existing PHC staff | 16.0 |
| Disruption of clinical care due to implementation of EMR facility | 40.0 |
| Lack of dedicated IT staff | 94.6 |
| Illegal records tampering or hacking | 6.6 |
| Interoperable IT systems | 73.3 |
| Lack of future support | 74.6 |
EMR: Electronic medical record, RoI: Return on investment, PHC: Primary health center
RESULTS
The analyses were separately conducted for quantitative and qualitative data. The survey results are presented with respect to (a.) availability and utilization of electronic medical record (EMR) and (b.) barriers to utilization of EMR, in the PHCs surveyed.
Availability of electronic medical record facility in primary health centers
Overall availability
Facility-based surveys were conducted in 75 PHCs to assess the availability of EMR facilities in nine domains. The average of each domain was calculated to obtain information on the “overall availability.” The “overall availability” of EMR in PHCs was found to be considerably low (19.14%).
Domain-specific availability
While the overall availability was low (19.14%), it was observed that this figure was majorly influenced by two domains, i.e., immunization (83%) and patient diagnosis (37.3%). Furthermore, a very limited electronic record keeping facility was available for taking clinical notes 5% (4) and capturing patient demographics 7% (5). Additional details about domain-specific EMR availability are given in Table 1.
Utilization of electronic medical record facilities in primary health centers
The “overall utilization” of EMR in PHCs was 15.72%. However, this percentage was primarily influenced due to the availability of EMR. Utilization was high (82.75%) among those PHCs where EMR keeping facilities were available. For example, higher utilization was observed in the areas of “immunization 100% (62)” and “patient diagnosis 100% (28)” which were also the domains with high availability. A similar observation was also noted in other domains [Table 3].
Table 3.
Utilization and nonutilization of the electronic medical record in primary health centers where electronic medical record facility is available
| Domains | Utilization |
|---|---|
| Patient’s demographics (n=5) | 80% (4) |
| Clinical notes (n=4) | 75% (3) |
| Complaints of patients (n=4) | 75% (3) |
| Patient’s diagnosis (n=28) | 100% (28) |
| Management of current medications (n=2) | 50% (1) |
| Vital signs (n=12) | 91% (11) |
| Allergies (n=12) | 91% (11) |
| Immunization (n=62) | 100% (62) |
| Prescribing medications (n=0) | Not available |
| Average utilization in PHCs where EMR is available | 82.75% |
| Overall utilization | 15.72% |
PHCs: Primary health centers, EMR: Electronic medical record
Barriers in implementation of electronic medical record
The survey also examined the barriers inhibiting the implementation of EMR in the PHCs across ten domains [Table 2]. “Lack of seed capital to start EMR facility (97.4%),” “uncertainty about RoI (96%),” “higher recurring costs (97.3%),” and “Lack of dedicated IT staff” (94.6%) were noted as key barriers in EMR implementation at PHCs. Domains which were least considered as barriers included “resistance of physicians (2.6%)” and “illegal record tampering or hacking (6.6%)”. The detailed outline of barriers across the domains is given in Table 2.
Thematic analysis of key informants' interviews
The analysis of key informants' interviews provided a greater insight resulting in four themes and subthemes. The detailed outlay of the themes and subthemes is given in Figure 1.
Figure 1.
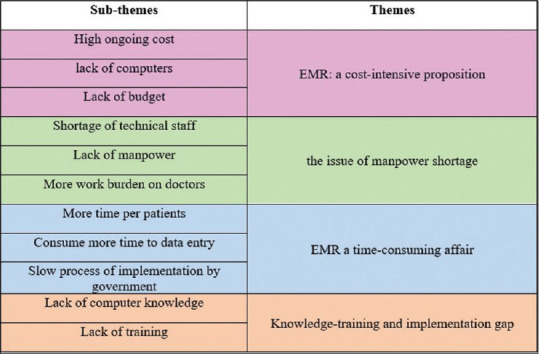
Themes and subthemes emerging from the analyses of key informants' interviews explaining the barriers to the implementation of electronic medical records in primary health centers
“The issue of manpower shortage”
Challenges of manpower shortages, specifically those trained in IT systems were profound within the health system at the grassroot level. The need for dedicated staff to implement and maintain EMR systems was an idea reverberated in the key informant interviews.
”I personally feel that Government should better have the provision of keeping computer operators or dedicated personnel who is technically trained and qualified and can help or assist our doctors and paramedics in streamlining the digital process …………… (KI 05).”
These findings were consistent with the survey results [Table 2], where over 90% of the PHCs reported a lack of dedicated IT staff, a significant barrier in the implementation of the EMR system.
“Electronic medical record a cost-intensive proposition”
Health authorities viewed EMR implementation as a “cost intensive” proposition requiring substantial capital investment. Accordingly, the analyses of interviews reported specific barriers namely, lack of basic infrastructures, less budgetary allocation, and high recurring expenditure. These factors are found to discourage health authorities from implementing EMR facilities.
”We are getting limited funds from the Government to run our existing projects and health programs. The Government has to provide sufficient funds to buy computer systems, software, and hardware and then only we can think of having EMR enabled PHCs in our district” (KI 06).
Implementing EMR is a long-term proposition as the higher cost is involved in terms of modifying, upgrading, and maintaining EMR adding up both capital and recurring expenditure. These results are also consistent with the survey findings where economic aspects were reported as major barriers for implementation EMR.
“Knowledge-training and implementation gap”
Limited understanding of computers and IT systems was observed as an important barrier in the implementation of EMR. The lack of digital literacy among health workers compromising the implementation of EMR in the PHCs, despite EMR systems, is physically present in some PHCs of the district.
”Lack of training is also one of the major issues in implementing electronic medical records. Because We are not experts to use the computers for electronic medical records keeping and all.” (KI 08).
It was observed that majority of the health workers in the PHCs received their qualifications before the introduction of IT systems resulting in limited knowledge on part of implementers. Moreover, limited in-service training with respect to the use of EMR compounded with inherently limited hands on experience is one of the primary hindrances limiting usage of EMR technologies.
“A time-consuming affair”
EMR is widely considered as an important tool in saving physician time and improving the quality of care. However, in this study, the analysis of interviews noted concerns of spending more time per patient due to the use of computers in clinical practice. Specifically, it was found that physicians and allied staff are spending more time on data entry rather than actual care provision.
”If we need to enter the data in computers it will take more time because we do not know the shortcut in computer and even don't have proper typing skills to enter the data fast” (KI 02).
The lack of experience in operating computers by the PHC staff compromises their ability to use EMR, with simple tasks such as data entry taking more time. In addition, the analysis also sheds light on other barriers perceived to be faced by the health authorities in the implementation of EMR. This includes the resistance of the health providers to go digital, fear of being caught due to misutilization of health services (including pilferage and biometric attendance), poor acceptability by health-care providers, privacy and security issues associated with patient's information, high-speed Internet issues, load shedding and absence of uninterrupted power supply, and concern over the sustainability of maintenance of EMR system.
DISCUSSION
We noted only 19.4% availability of EMR in the PHCs surveyed. Lower digitalization of medical records in public health facilities is reported in earlier studies in countries of similar economies.[4] Similarly, the difference in electronic record keeping across functional domains was also reported in the PHCs surveyed. This difference is possibly attributed to priority accorded to certain functional domains in respect of state or centrally funded health programs. For example, under the flagship of the Reproductive, Maternal Newborn, Child and Adolescent Health program, an electronic data management system called “RCH portal” was specifically designed to store Maternal and Child Health data including immunization data.[7] This resulted in the digitalization of immunization records in primary health-care settings across the country. Moreover, immunization coverage monitored through the “RCH portal” is one of the key health system performance indicators promulgated by NITI Aayog.[18]
In India, EMR facilities are mainly concentrated in top tier private hospitals, whereas in the public health settings, they are functional only in a handful number of tertiary care centers.[19] The lower adoption of EMR in the public health facilities including PHCs is attributed to the budgetary constraint. The public health spending in India is traditionally low, and deployment of EMR within all levels of the public health system is cost intensive[19,20] as huge expenditures are involved in the purchase of hardware, software, installation, and maintenance of EMR in public health facilities.[21] Likewise, the private primary care providers in India also lack financial backing from the government which inhibits EMR adoption in their standalone and polyclinics.[20] Therefore, there is an urgent need to bring down the cost of EMR technologies or shift toward acquiring an open medical record system.[22]
We also found lower (15.4%) utilization of EMR in the PHCs surveyed. The lower usage was seen in those PHCs where EMR did not exist. Within the PHCs, the usage of EMR was primarily concentrated around keeping immunization records. While availability was considered as a deterministic parameter in EMR usage, interestingly nonusage was also observed in the areas where EMR was available [Table 3]. Specifically, unavailability of EMR infrastructure, shortage of dedicated human resource, issues of interoperability, and disruption of normal clinical care were found to be adding to the nonusage of EMR and these findings were consistently noted in other studies.[23,24]
As India is aiming toward achieving universal health coverage through its prestigious Ayushman Bharat Yojana, strengthening the PHCs, and/or health and wellness centers, implementing EMR systems is need of the hour. Roping in private players for the development and deployment of EMR systems through public–private partnerships and corporate social responsibility initiatives could lessen the economic costs of EMR implementation. Building on the existing IT technologies and databases (such as ANMOL, RCH Portal, and Aadhaar) could enhance interoperability and interconnectedness. Training and capacity building in IT for health workers is needed to reap the benefits of the progress made in EMR availability. While the implementation of these systems is resource intensive, in long run, the benefits of EMR implementation would outweigh the costs.
Limitations of the study
The study limitations include a unilateral focus on PHCs and self-reported data obtained from PHC medical officers during the surveys. The readers are advised to consider the limitations before extrapolating the study results.
CONCLUSION
The availability of electronic record keeping of patient's data was low in PHCs in Nalgonda district of Telangana. Most of the PHCs in the district were primarily using EMR for immunization record keeping. Multiple barriers were found to be inhibiting the implementation of EMR facilities at PHCs. These barriers are related to the nonavailability of technical human resources at the grassroot level of the health system, budgetary constraints, knowledge training and implementation gap, and the perceptions of PHC staff about EMR as a time-consuming process resulting in treatment delays. Addressing these barriers is crucial for the successful implementation of EMR.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mkalira Msiska KE, Kumitawa A, Kumwenda B. Factors affecting the utilisation of electronic medical records system in Malawian central hospitals. Malawi Med J. 2017;29:247–53. doi: 10.4314/mmj.v29i3.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NHP. e-Health India. 2017. [Last accessed on 2019 Feb 10]. Available from: https://www.nhp.gov.in/e-health-india_mty .
- 3.Chokshi M, Patil B, Khanna R, Neogi SB, Sharma J, Paul VK, et al. Health systems in India. J Perinatol. 2016;36:S9–12. doi: 10.1038/jp.2016.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jawhari B, Ludwick D, Keenan L, Zakus D, Hayward R. Benefits and challenges of EMR implementations in low resource settings: A state-of-the-art review. BMC Med Inform Decis Mak. 2016;16:116. doi: 10.1186/s12911-016-0354-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daga M. Digitising Health Records in India. 2016. [Last accessed on 2020 Apr 12]. Available from: https://www.dailypioneer.com/2016/columnists/digitising-health-records-in-india.html .
- 6.Goel H, Srivastava PK, Gupta A, Garg C E-Aushadhi'A Drug Warehouse Management System. A Drug Warehouse Management System. 2013 [Google Scholar]
- 7.Faujdar DS, Sahay S, Singh T, Jindal H, Kumar R. Public health information systems for primary health care in India: A situational analysis study. J Family Med Prim Care. 2019;8:3640–6. doi: 10.4103/jfmpc.jfmpc_808_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jeyaranjan J. Public Distribution System in Telangana. Social Development Report. 2017:151. [Google Scholar]
- 9.GoT. Nalgonda District. Government of Telangana. 2018. [Last accessed on 2019 Feb 12]. Available from: https://nalgonda.telangana.gov.in/
- 10.GoT. Nalgonda District. Government of Telangana. 2018. [Last accessed on 2019 Feb 12]. Available from: https://nalgonda.telangana.gov.in/
- 11.Gov.Telangana. Health–Office of District Medical and Health officer Telangana. 2019. [Last accessed on 2020 Jan 20]. Available from: https://nalgonda.telangana.gov.in/health/
- 12.IIPS. National Family Health Survey-4 2015-16: District Factsheet-Nalgonda, Telangana. International Institute of Population Sciences. 2017 [Google Scholar]
- 13.Creswell JW, Klassen AC, Plano Clark VL, Smith KC. Best Practices for Mixed Methods Research in the Health Sciences. Bethesda (Maryland): National Institutes of Health 2011; 2013. pp. 541–5. [Google Scholar]
- 14.Powell AC, Ludhar JK, Ostrovsky Y. Electronic health record use in an affluent region in India: Findings from a survey of Chandigarh hospitals. Int J Med Inform. 2017;103:78–82. doi: 10.1016/j.ijmedinf.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Spss I. IBM SPSS Statistics for Windows. Version 20.0. New York: IBM Corporation; 2011. [Google Scholar]
- 16.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Sage; 1994. [Google Scholar]
- 17.Archer E, Herman H, van Vuuren J, Hugo D. Introduction to Atlas. Ti: Basic Operations, Tips and Tricks for Coding: Research Rescue. 2017 [Google Scholar]
- 18.NITIAayog. Performance on Health Outcomes. In: India NIfT. 2016. [Google Scholar]
- 19.Singh B, Muthuswamy P. Factors affecting the adoption of electronic health records by nurses. World Applied Sci J. 2013;28:1531–5. [Google Scholar]
- 20.Mehta N, Pandit A. Perceptions of EMR system by doctors in Pune (India) Indian J Public Health Res Develop. 2017;8:540–6. [Google Scholar]
- 21.Randeree E. Exploring physician adoption of EMRs: A multi-case analysis. J Med Syst. 2007;31:489–96. doi: 10.1007/s10916-007-9089-5. [DOI] [PubMed] [Google Scholar]
- 22.Crichton R, Moodley D, Pillay A, Gakuba R, Seebregts CJ, editors. Springer: International Symposium on Foundations of Health Informatics Engineering and Systems; 2012. An Architecture and Reference Implementation of an Open Health Information Mediator: Enabling Interoperability in the Rwandan Health Information Exchange. [Google Scholar]
- 23.Al-Rawajfah O, Tubaishat A. Barriers and facilitators to using electronic healthcare records in Jordanian hospitals from the nurses' perspective: A national survey. Inform Health Soc Care. 2019;44:1–1. doi: 10.1080/17538157.2017.1353998. [DOI] [PubMed] [Google Scholar]
- 24.Belletti D, Zacker C, Mullins CD. Perspectives on electronic medical records adoption: Electronic medical records (EMR) in outcomes research. Patient Relat Outcome Meas. 2010;1:29–37. doi: 10.2147/prom.s8896. [DOI] [PMC free article] [PubMed] [Google Scholar]


