Abstract
Objective
SSc often leads to fibrotic cutaneous involvement of the face and reduced oral aperture, with impaired food intake and oral hygiene. Oral exercises can increase oral aperture but are often hampered by low adherence rates. The aim of this mixed method study was to explore the feasibility, patient satisfaction and effectiveness of two exercise programmes in SSc-associated microstomia.
Methods
Adult patients suffering from SSc and microstomia (maximal oral aperture <40 mm) were randomized to two groups. Group A exercised with a jaw motion device (Therabite), whereas group B performed mouth-stretching exercises. Patients were expected to exercise for 10 min, three times per day for 3 months. Patients were evaluated at baseline, 3 months (period without intervention), 6 months (after 3 months of intervention) and 9 months (post-intervention). At month 6, semi-structured one‐to‐one interviews were conducted.
Results
We included six women and three men, median age 60 years and median disease duration 8 years. At 6 months, all patients in group A (n = 4) and four in group B (n = 5) improved, with a median of 9 and 7 mm, respectively. The adherence ranged between 63.7 and 98.9% in group A and between 48.5 and 97.4% in group B. The interview revealed three themes: drivers, challenges and perceived improvement.
Conclusion
Both interventions improved maximal oral aperture. The adherence to therapy was high, but none of the patients considered it feasible to continue practising three times per day. Future studies are needed in order to define feasible long-term exercise programmes.
Keywords: systemic sclerosis, microstomia, occupational therapy, exercise therapy, Therabite
Key messages
Exercises can improve the maximal oral aperture if the frequency, duration and the number of repetitions is sufficiently intensive.
Continuing to exercise three times a day is not feasible for adults with SSc.
It is necessary to define feasible exercise programmes for professionally active patients that can be sustained in the long term.
Introduction
SSc is a severe autoimmune disease, and fibrotic cutaneous involvement of the hands and face is a typical disease feature [1]. Reduced oral aperture is frequent and associated with impaired food intake, reduced oral hygiene and secondary dental problems [2]. Microstomia is defined as an interincisal distance smaller than 40 mm [3]. Exercises [4–7] and injection therapy [8] have been suggested to restore or maintain mouth opening and freedom of lip movement to improve patients’ quality of life. Several studies have shown that stretching (placing the thumbs in opposite corners of the mouth and pulling outward) and oral augmentation exercises (training with tongue depressors) can increase oral aperture in patients with SSc [4–7]. In a study by Yuen et al. [9], the authors could not show a significant improvement and highlighted the low exercise adherence rate. The passive jaw motion therapeutic device Therabite is effective in increasing the range of motion in patients with TM joint and muscle disorders, but data in SSc-associated microstomia are lacking [2, 10]. Furthermore, there are no studies investigating the feasibility of these exercises.
In this pilot study, we aimed to explore feasibility, patient satisfaction and effectiveness of two different exercise programmes, Therabite and orofacial exercises, in SSc-associated microstomia.
Methods
Study design
A descriptive explorative convergent mixed method study was conducted from January 2017 to June 2018.
Patient selection and randomization
We addressed all adult SSc patients (>18 years) with microstomia (maximal oral aperture <40 mm), fulfilling the ACR/EULAR 2013 criteria [11] who presented during 1 year at an outpatient visit at the Division of Rheumatology of the University Hospitals Leuven. The subtype of SSc was classified according to criteria by LeRoy et al. [12]. Patients with a history of maxillary or mandibular fractures, infection, osteomalacia or osteoradionecrosis were excluded. Research ethics committee approval was obtained from our local Institutional Review Board. Patients provided written informed consent and were randomized to two groups in a 1:1 ratio by means of a randomization list.
Intervention
Group A exercised with a passive jaw motion device (Therabite), whereas group B performed manual mouth-stretching exercises. Both groups were asked to exercise for 10 min, three times per day for 3 months. Our department provided the device Therabite free of charge to the participants for the duration of the study, without sponsorship. At the start of the intervention, the participants practised their exercises together with the occupational therapist (E.S.), and written instructions (including photographs) were provided. A description of the exercises for both groups can be found in Supplementary Figs S1 and S2, available at Rheumatology Advances in Practice online.
Study time line and assessments
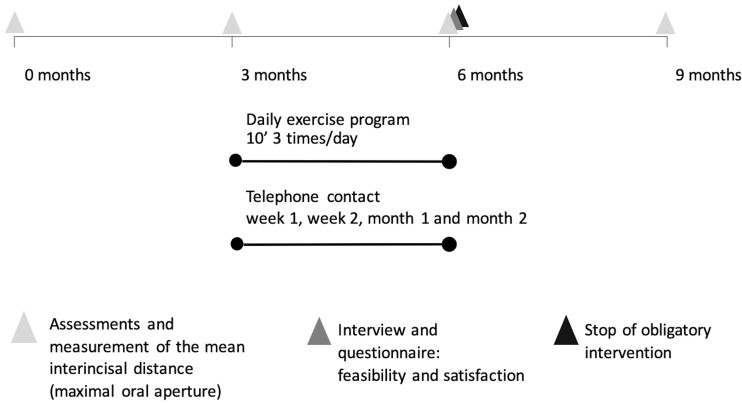
A detailed study time line is shown in Fig. 1. The baseline visit was followed by a 3 month non-interventional observation period. The interventional phase of the study lasted for 3 months (from 3 to 6 months), followed by a post-interventional observation period of 3 months (from 6 to 9 months). Patients were assessed at baseline, 3, 6 and 9 months, documenting oral aperture, skin thickness and patient-reported outcomes.
Fig. 1.
Study time line
The oral aperture was defined as the vertical distance from the bottom of the maxillary incisor to the top of the mandibular incisor with the mouth opened. All measurements were performed by the same assessor (E.S.) using digital callipers. Three consecutive measurements were performed, with a 5 s rest interval, and averages were calculated [13].
During the interventional period, patients were contacted four times by telephone to address problems encountered and provide guidance. These follow-up calls lasted 5–20 min. Interview guides can be found in Supplementary Tables S1 and S2, available at Rheumatology Advances in Practice online. The subjects completed an exercise diary to document adherence. Adherence was defined as the proportion of executed exercises to the planned number, expressed as a percentage.
The interventional period ended at time point 6 months. When completing the interventional phase, patients were at liberty to continue exercising at their own pace, continuing diary recording but without follow-up telephone calls. The end of the interventional period (6 months) included a one‐to‐one interview, performed by E.S., using a semi-structured interview guide. Interviews were recorded, transcribed verbatim, anonymized and systematically analysed using The Qualitative Analysis Guide of Leuven (QUAGOL) [14]. E.S. read and reread all transcripts and important units weregrouped into natural subthemes and then overarching themes. A subset was analysed independently by E.D.L., and this was followed by a team discussion of combined findings together with our rheumatologists. Based on these discussions, the final themes and subthemes were refined.
Ethics
All research subjects participating in this study provided written informed consent. Consent was obtained from all participants by the principal investigator. Documentation for the informed consent process and the signed consent forms are maintained in study binders at the Department of Rheumatology, University Hospital of Leuven in Belgium. All informed consent forms were reviewed and approved by the Ethical Committee of the University Hospital of Leuven (S59817, 23 December 2016). All subjects were also provided with copies of their signed informed consent forms to be kept in their own records. Copies of the informed consent forms are available for review if necessary.
Results
Patient recruitment
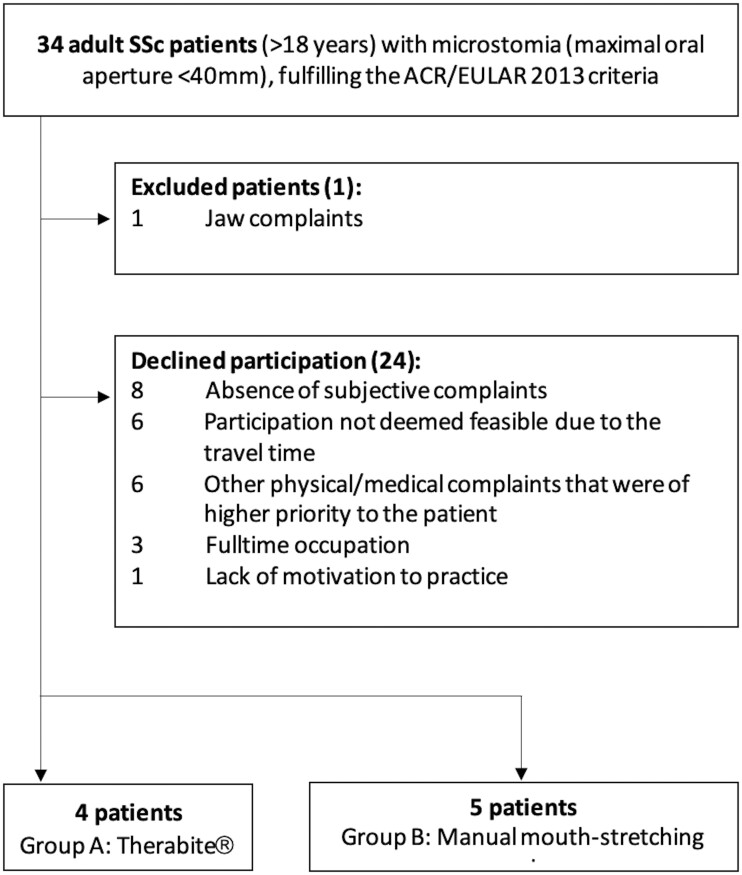
During the 1 year recruitment period, 34 patients were considered eligible for the study. Nine patients consented to participate. The recruitment process can be found in Fig. 2.
Fig. 2.
The recruitment process
Baseline patient data
Six women and three men were included, with a median age of 60 years (range 40–75 years) and median disease duration of 8 years (range 3–22 years) (Supplementary Table S3, available at Rheumatology Advances in Practice online.). Four patients were allocated to the Therabite group (group A) and five to the manual group (group B). No significant difference was found between the groups (P > 0.05 using the Mann–Whitney U test).
Efficacy and adherence
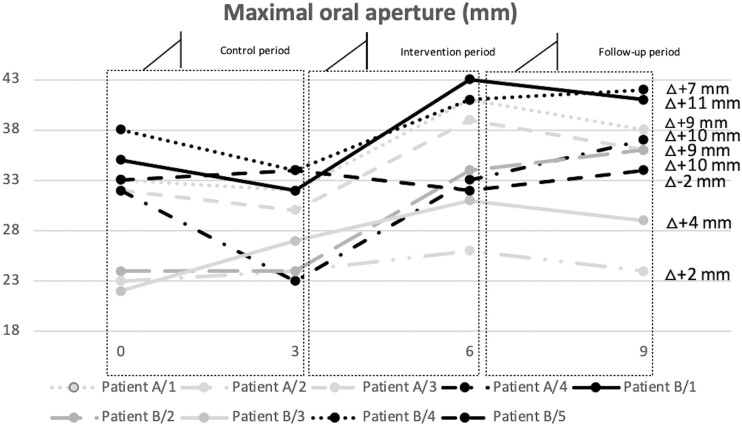
At time point 6 months, oral aperture improved in all patients in group A (n = 4) and four patients in group B (n = 5), with a median of 9 mm (range 2–10 mm) and 7 mm (range 4–11 mm), respectively (Fig. 3). In one patient of group B, maximal oral aperture decreased by 2 mm over time. Adherence ranged from 63.7 to 98.9% in group A and from 48.5 to 97.4% in group B. During the follow-up period there was always a decrease in oral aperture among the participants who stopped practising (Supplementary Table S4, available at Rheumatology Advances in Practice online). There was lasting improvement if they had continued exercising three times per week, once per day and maximal improvement at two times per day.
Fig. 3.
Maximal oral aperture (in millimetres)
Semi-structured interviews
All nine participants in the exercise programme participated in the interview, which lasted 30–60 min. Three main themes emerged from the data: drivers (Table 1), challenges (Table 2) and perceived improvement (Table 3).
Table 1.
Theme of drivers, subthemes and some of the participants’ narratives
| Main themes | Subthemes | Participants’ narratives |
|---|---|---|
| Drivers | Motivated by the study | I made a promise; if I make a promise to someone, I will keep it. (Male, 60, Therabite) |
| If it doesn’t help me, maybe it will help somebody else. For the future, that others are getting better of it. (Female, 61, manual) | ||
| Motivated by functional disability | Well, I don’t have lips any more. When I drink a cup of coffee … I always need to clean up with a napkin, otherwise there’s always droplets and you do feel like that’s a handicap. (Male, 56, Therabite) | |
| Supportive factors | It was motivating that you called me. It was a good motivation. It was a short conversation but still.… (Female, 55, manual) |
Table 2.
Theme of challenges, subthemes and some of the participants’ narratives
| Main themes | Subthemes | Participant’s narratives |
|---|---|---|
| Challenges | Time investment | The duration, it’s no time at all, it doesn’t take long, but still, it needs a while. (Male, 56, Therabite) |
| Three times a day is REALLY … yes, it is really tough that way. (Female, 40, Therabite) | ||
| Certainly not three times a day. Two times a day but reluctantly, I’d rather not really. Keeping it up is difficult. But I do want to keep doing it in the mornings. (Male, 60, manual exercises) | ||
| Mental struggle | It’s not something you do for fun, I’m telling you, the amount of effort is underestimated. (Female, 61, manual exercises) | |
| Need of routines | In the mornings, first a drink, something to eat and then practice. (Female, 47, Therabite) | |
| For my daily routine, I scheduled everything around the oral exercises. Well, not always, but you do need to take it into account all the time. (Female, 40, Therabite) | ||
| Physical consequences | Yes, at the start, during the first week I was thinking, ‘Do not do that, do not do that’; if I have to be honest, I did not feel good, I had pain there, pain here. The first week was a real challenge. (Female, 47, Therabite) | |
| Technical limitations of the Therabite | …at a certain point when I put the Therabite into my mouth, then my teeth could actually come off of those pads. (Male, 56, Therabite) | |
| Less enjoyable exercises | The third exercise, laughing with a closed mouth, that was hard, I wanted to perform perfectly but I didn’t feel if I did it well. (Male, 61, Therabite) |
Table 3.
Theme of perceived improvement, subthemes and some of the participants’ narratives
| Main themes | Subthemes | Participants’ narratives |
|---|---|---|
| Perceived improvement | Experiencing progress | Yes, with eating and articulating. Eating is easier. (Female, 55, manual exercises) |
| I have not felt much difference myself. That is why I am pleasantly surprised. I had not noticed it myself. (Female, 71, manual exercises) | ||
| If there was anyone else who was required to do it, I would immediately tell them, ‘You should try it, you won’t have any disadvantages’. (Male, 60, Therabite) | ||
| Hope to retain progress | I do hope, though, that the 3 months I’ve done, that that wasn’t wasted effort; imagine that. (Female, 61, manual exercises) | |
| Necessity for continued training | I think there will be a limit to how far you can get, but I suspect that you have to keep it up regularly, otherwise it may worsen again. (Female, 71, manual exercises) |
Theme 1: drivers
Participants highlighted several drivers that motivated them to perform the exercises at home.
Motivated by participating in a study
In both exercise groups, several participants were additionally motivated because of their participation in a study.
Motivated by functional disability
All participants experienced functional disabilities owing to microstomia and were concerned that their microstomia would worsen.
Supportive factors
All participants of the Therabite group and one patient of the manual exercise group described extrinsic motivational factors. They were motivated primarily by individuals in their environment or from the follow-up calls by the occupational therapist. Most of the participants placed their device or their instruction papers in a visible location, functioning as a memory aid.
Theme 2: challenges
Participants mentioned several challenges related to the feasibility of the home-based exercises.
Time investment
In both groups, participants experienced a substantial time investment to complete the exercises on a daily base. Before initiating the exercise programme, they expected that performing the exercises for 10 min three times during the day would be easy to complete. All participants experienced that exercising three times a day was not feasible to implement into their daily routine.
Mental struggle
All participants mentioned that it was hard to maintain their motivation to keep doing the exercises.
Need for routines
Participants highlighted how important it was to develop a routine. To support the daily routine, most of them combined their exercises with another activity that they were doing on a daily basis. The mid-day period was challenging, because many participants were not at home at this time of the day, and mid-day planning was less structured compared with mornings or evenings.
Physical consequences
Most of the participants experienced physical consequences, especially in the first week. For some participants the physical consequences persisted after the first week, but the type and seriousness varied. Two participants adjusted the frequency of the exercises because of pain at the corners of the mouth or pain at the neck.
Technical limitations of the Therabite
The participants of the Therabite group indicated limitations related to the device. For half of them the possibilities were not challenging enough, and they also missed horizontal exercises. Two participants found that the device was too large, meaning that they did not like to take the device with them when leaving the house.
Less enjoyable exercises
Everyone in the manual exercise group had an exercise they did with less pleasure. In the Therabite group, the participants had no comments about the exercises.
Theme 3: perceived improvement
Participants also had several different perceptions about their improvement.
Experiencing progress
Several participants experienced functional improvement in their daily living. Other participants did not experience subjective improvement but were surprised by the objective measurements. The participants had an overall positive experience.
Hope to retain progress
Most of the participants were hoping that they could maintain their improvement.
Necessity for continued training
Everyone indicated that it would probably be necessary to continue practising, but they all hoped that it could be less intensive.
Discussion
The present study is the first to explore the feasibility and satisfaction of mouth exercises and the use of the Therabite device for microstomia in patients suffering from SSc. Previous studies have shown that oral augmentation exercises increase oral aperture [4–7], but did not include the experience of the participants. The results of the present study suggest that both interventions can improve the maximum oral aperture. The improvement in the observed maximum oral aperture (11 ± 2 mm) is comparable to previously published work by Pizzo et al. [7] (10.7 ± 2.06 mm). In that study, participants were monitored every 2 weeks, whereas in the present study more self-discipline was expected from the participants. Other studies reported smaller improvements [4,15–16].
The observed improvement in the maximum oral aperture suggests that the applied regimen (frequency, duration and number of repetitions) is effective. The 30 s stretch duration and the 10 min duration three times a day was based on the comments in the study by Maddali-Bongi et al. [4]. Concerning the type of exercise, we opted to use only exercises without involvement of fingers in the mouth, because of sensitivity and wounds on the fingers, and this contrasts with other studies. The improvement gives an indication that manual exercises without using the fingers in the mouth can be efficient. Previous studies investigating the effects of the Therabite device on other conditions have shown that the Therabite device offers more comfort for the patient than using tongue depressors [10].
In our study, the frequency (three times per day) was a stumbling block for our professionally active patients. Also, only patients who experienced functional disability as a consequence of microstomia consented to participate. In clinical practice, this will be a very important aspect to consider. This can be seen as selection bias and could have influenced the high adherence rate that was shown in the present study. In previous studies it is clear that few participants persist in practising [15]. It is conceivable that a 3 month exercise period could increase patient adherence compared with a 6 month period.
During the follow-up period there was always a decrease in oral aperture in the participants who stopped practising. There was improvement if they had continued exercising three times per week, once a day, and the most improvement at two times per day. Further research for long-term follow-up is necessary.
From the interviews, facilitating factors have been identified that motivate patients and increase the feasibility of the exercises. It is important to take into account that different participants maintained a high adherence rate solely because of their participation in a trial. Supportive factors are also an attentive partner and/or involved health professionals. In the future it would also be possible to work with a mobile application that provides a notification. If there are few supporting factors in patients, it might be important to provide more support via telephone monitoring.
Various challenges also emerged from this study. The time investment and the mental struggle to keep up exercising threatened the feasibility of continuing to practise three times per day in the long term. All participants considered once a day to be feasible. In clinical practice, health professionals could recommend adults with microstomia to exercise intensively (three times per day) for 3 months to obtain an improvement and to maintain this improvement by exercising once a day. It is also important to try to do the exercises together with a routine daily activity, and all participants preferred to exercise in the morning or the evening. The follow-up telephone call after 1 week is crucial to be able to offer support and to prevent physical complaints, such as pain. It is crucial to downsize the instructions ‘keep the mouth as large as possible’; it has to be as large as possible without obtaining pain during or after the exercise. Patients underestimated that they had to keep the same position for 30 s.
Furthermore, when deciding which intervention to use, it is important to consider the various advantages and disadvantages. Six of the nine participants reported side effects. Two participants from the Therabite group and one from the manual group did not experience any side effects. The side effects varied in nature and severity. Two participants exercising with manual exercises had pain at the corners of the mouth, meaning that they had to adjust the frequency of the exercise. One participant from the Therabite group had cramps under the chin, and three participants suffered from neck cramps (two from the Therabite group and one from the manual group). In one of these participants, exercising with Therabite, these pains were so intense that the participant had to adjust the frequency to two times per day. Yawning was provoked in one participant during the manual exercises.
The Therabite has a purchase price of €412.80 (exclusive of VAT) and is not reimbursed in Belgium, whereas there are no costs associated with the manual exercises. With the Therabite, the exercises are only vertical, whereas the manual exercises include both vertical and horizontal exercises. Participants also experienced that the Therabite exercises were not challenging enough and that they could open the mouth further than the device itself. Everyone in the manual group had an exercise they did with less pleasure; for therapists, it will be important to coach the patients and to adapt the exercises according to the needs of the individual patient.
The participants all believe that practising should be part of their lives, but they hope it can be less intensive. Further research is needed into feasible exercise programmes with a lower frequency.
A recent study [8] suggests that a treatment with injections (hyaluronic acid and platelet-rich plasma) also improves both maximal oral aperture and quality of life. It is noteworthy that these injections require general anaesthesia and are invasive procedures. Exercises are accessible for everyone and can be done without substantial costs.
The strengths of this study are the availability of qualitative interview results for all patients, providing insight into the psychosocial aspects associated with the feasibility of the proposed exercise programmes. Limitations are the low number of participants, precluding statements on the effectiveness of either of the interventions, and the lack of blinding of the health professional; there was nothing added to aim to reduce this bias.
This study shows that exercises can improve the maximal oral aperture if the frequency, duration and the number of repetitions is sufficiently intensive. In conclusion, patients with SSc need to be aware of the benefit of physical exercises to improve microstomia. As a therapist, it is crucial to educate patients on this topic, and our study can serve as guidance for attention points to take in account.
Further studies are needed in order to define exercise programmes that are feasible for professionally active patients and can be sustained in the long term. It should therefore be considered whether the same exercises with the same duration and number of repetitions would also have an effect with a lower frequency. To increase sample size, a multicentre study might be necessary for this rare disease.
Supplementary Material
Acknowledgements
The authors are thankful to all participants. We also thank Sabien Severi for providing patients and Johan Joly, Delphine Bertrand, Evelien Truyersand Inne Van Gastel for giving advice and support.
E.S., E.D.L. and R.W. designed the study. E.S. was responsible for patient recruitment, performed the intervention and wrote the manuscript. All authors critically revised the manuscript for content and approved the final version for submission.
Funding: No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Disclosure statement: The authors have declared no conflicts of interest.
Data availability statement
All the data are maintained in the Department of Rheumatology, University Hospital of Leuven, Belgium.
Supplementary data
Supplementary data are available at Rheumatology Advances in Practice online.
References
- 1. Agarwal SK, Reveille JD.. The genetics of scleroderma (systemic sclerosis). Curr Opin Rheumatol 2010;22:133–8. [DOI] [PubMed] [Google Scholar]
- 2. Alantar A, Cabane J, Hachulla E. et al. Recommendations for the care of oral involvement in patients with systemic sclerosis. Arthritis Care Res 2011;63:1126–33. [DOI] [PubMed] [Google Scholar]
- 3. Naylor WP. Oral management of the scleroderma patient. J Am Dent Assoc 1982;105:814–7. [DOI] [PubMed] [Google Scholar]
- 4. Maddali-Bongi S, Landi G, Galluccio F. et al. The rehabilitation of facial involvement in systemic sclerosis: efficacy of the combination of connective tissue massage, Kabat’s technique and kinesitherapy: a randomized controlled trial. Rheumatol Int 2011;31:895–901. [DOI] [PubMed] [Google Scholar]
- 5. Albilia JB, Lam DK.. Small mouths … big problems? A review of scleroderma and its oral health implications. J Can Dent Assoc 2007;73:831–6. [PubMed] [Google Scholar]
- 6. Naylor WP, Douglass CW, Mix E.. The nonsurgical treatment of microstomia in sclerodermia: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol 1984;57:508–11. [DOI] [PubMed] [Google Scholar]
- 7. Pizzo G, Scardina GA, Messina P.. Effects of a nonsurgical exercise program on the decreased mouth opening in patients with systemic scleroderma. Clin Oral Investig 2003;7:175–8. [DOI] [PubMed] [Google Scholar]
- 8. Pirrello R, Verro B, Grasso G. et al. Hyaluronic acid and platelet-rich plasma, a new therapeutic alternative for scleroderma patients: a prospective open-label study. Arthritis Res Ther 2019;21:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yuen HK, Weng Y, Bandyopadhyay D, Reed SG.. Effect of a multi-faceted intervention on gingival health among adults with systemic sclerosis. Clin Exp Rheumatol 2011;29(2 Suppl 65):S26–32. [PMC free article] [PubMed] [Google Scholar]
- 10. Pauli N, Andréll P, Johansson M, Fagerberg-Mohlin B, Finizia C.. Treating trismus: a prospective study on effect and compliance to jaw exercise therapy in head and neck cancer. Head Neck 2015;37:1738–44. Dec 1 [DOI] [PubMed] [Google Scholar]
- 11. Van Den Hoogen F, Khanna D, Fransen J. et al. 2013 classification criteria for systemic sclerosis: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 2013;65:2737–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. LeRoy EC, Medsger J.. Criteria for the classification of early systemic sclerosis. J Rheumatol 2001;28:1573–6. [PubMed] [Google Scholar]
- 13. Wood GD, Branco JA.. A comparison of three methods of measuring maximal opening of the mouth. J Oral Maxillofac Surg 1979;37:175–7. [PubMed] [Google Scholar]
- 14. Dierckx de Casterle B, Gastmans C, Bryon E, Denier Y.. QUAGOL: a guide for qualitative data analysis. Int J Nurs Stud 2012;49:360–71. [DOI] [PubMed] [Google Scholar]
- 15. Yuen HK, Marlow NM, Reed SG. et al. Effect of orofacial exercises on oral aperture in adults with systemic sclerosis. Disabil Rehabil 2012;34:84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Poole J, Conte C, Brewer C. et al. Oral hygiene in scleroderma: the effectiveness of a multi-disciplinary intervention program. Disabil Rehabil 2010;32:379–84. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data are maintained in the Department of Rheumatology, University Hospital of Leuven, Belgium.