Abstract
Background
Acceptance rates of COVID-19 vaccines have still not reached the required threshold to achieve herd immunity. Understanding why some people are willing to be vaccinated and others are not is a critical step to develop efficient implementation strategies to promote COVID-19 vaccines.
Objective
We conducted a theory-based content analysis based on the capability, opportunity, motivation–behavior (COM-B) model to characterize the factors influencing behavioral intentions toward COVID-19 vaccines mentioned on the Twitter platform.
Methods
We collected tweets posted in English from November 1-22, 2020, using a combination of relevant keywords and hashtags. After excluding retweets, we randomly selected 5000 tweets for manual coding and content analysis. We performed a content analysis informed by the adapted COM-B model.
Results
Of the 5000 COVID-19 vaccine–related tweets that were coded, 4796 (95.9%) were posted by unique users. A total of 97 tweets carried positive behavioral intent, while 182 tweets contained negative behavioral intent. Of these, 28 tweets were mapped to capability factors, 155 tweets were related to motivation, 23 tweets were related to opportunities, and 74 tweets did not contain any useful information about the reasons for their behavioral intentions (κ=0.73). Some tweets mentioned two or more constructs at the same time. Tweets that were mapped to capability (P<.001), motivation (P<.001), and opportunity (P=.03) factors were more likely to indicate negative behavioral intentions.
Conclusions
Most behavioral intentions regarding COVID-19 vaccines were related to the motivation construct. The themes identified in this study could be used to inform theory-based and evidence-based interventions to improve acceptance of COVID-19 vaccines.
Keywords: vaccine, COVID-19, behavior, tweet, intention, content analysis, Twitter, social media, acceptance, threshold, willing, theory, model, infodemiology, infoveillance
Introduction
The global COVID-19 pandemic is affecting 219 countries worldwide [1]. An important component of managing COVID-19 is preventing the infection [2,3]. Fortunately, development of vaccines against the disease is progressing well. In December 2020, the US Food and Drug Administration authorized COVID-19 vaccines for emergency use. Another currently pressing issue is how to increase vaccine acceptance rates [4]. In previously published survey studies, the acceptance rate of COVID-19 vaccines was a concern. Of 672 participants in the United States, approximately 67% said they would be willing to receive a vaccine [5]. It is necessary to vaccinate an estimated 55%-82% of the population to create herd immunity and slow the spread of a pandemic [6]. Therefore, it is critical to understand why some people are willing to be vaccinated and others are not.
Previous studies have described potential impediments to COVID-19 vaccines, including questioning the need for vaccines and preferring to benefit from the immunity conferred by surviving COVID-19 [7]; safety issues regarding the rapid development and testing process of vaccines [7]; issues related to mandatory vaccination [7]; and conspiracy beliefs [8]. Some researchers conducted surveys based on theoretical models to explore facilitators and barriers to COVID-19 vaccination. Williams et al [9] conducted a survey to examine factors that influenced respondents’ decisions to be vaccinated against COVID-19 and identified three facilitators (personal health, severity of COVID-19 disease, health consequences to others) and one barrier (concerns regarding vaccine safety). Lin et al [10] used the health belief model (HBM) to identify two facilitators (reduced likelihood of contracting COVID-10; others getting vaccinated) and one barrier (concerns about efficacy and side effects). Wong et al [11] also used the HBM to identify one facilitator of perceived benefits (the belief that the vaccination can reduce infection probability and alleviate concerns about COVID-19).
Compared with surveys, Twitter can gather timely information regarding behavioral intentions toward COVID-19 vaccines, especially to understand “anti-vaxxers” and those influenced by misinformation who are inclined not to get the vaccine. These types of users could be the most vulnerable population for COVID-19 vaccine outreach interventions. On the Twitter platform, there are more than 330 million users, and the median number of posts per person each month is 2 [12,13]. A recent survey of US Twitter users showed that they are younger and have a higher education level than the general population; however, their gender, race, and ethnicity distributions are similar to those of the general population [13]. The Twitter platform has been validated as a way to develop a public perception–tracking tool based on real-time content [14]. In addition, Twitter has been flooded with information about COVID-19, influenced by social isolation policies enacted during the epidemic [15]. The Twitter platform could be used to explore determinants of health-related behavior intentions [16]. Because the maximum length of each tweet is 280 characters, in addition to mentioning potential behavioral intentions, users can also briefly describe the reasons that led to their decision. In addition, using geotagged Twitter data, it is easier and faster to identify people's perceptions in different geographic locations. Therefore, we chose to use the Twitter platform to analyze behavioral intentions toward COVID-19 vaccines.
To better characterize the factors that influence behavioral intentions on the COVID-19 vaccines mentioned in the tweets, we conducted a theory-based content analysis based on the capability, opportunity, motivation–behavior (COM-B) model. The COM-B model was proposed by Michie et al [17] in 2011, and it contains three basic constructs: capability (physical and psychological), motivation (automatic and reflective), and opportunity (social and physical). The COM-B model is a comprehensive theoretical model based on causal mechanisms to identify individual and context factors that influence behavioral change. It was developed by merging 19 behavior change frameworks through a systematic literature review and discussions with behavior change experts. It has been successfully applied to many health-related behaviors, such as smoking cessation [18-20] and obesity reduction [21,22]. In contrast to other health behavior theories (eg, HBM, theory of planned behavior), the COM-B model was developed based on the behavior change wheel, which not only provides a theoretical analysis of behavior but, more importantly, provides results that can be used to assist with intervention design [17,23]. In addition, the World Health Organization (WHO) Regional Office for Europe has adapted it to vaccination behaviors to design its Tailoring Immunization Programmes (TIP) approach [24,25]. They merged subconstructs in capability and motivation, respectively. Because of vaccination behavior, the physical capability is interlinked with the psychological capability. Likewise, automatic motivation (ie, emotions, impulses) interacts with reflective motivation (ie, intentions, beliefs). Another advantage of the adapted COM-B model is that it focuses on vaccination behavior and provides refined details for each construct in the vaccine context. Therefore, we used an adapted COM-B model (see Figure 1) as the theoretical model of this study. The objectives of this study are to (1) determine if the adapted COM-B model can explain behavioral intentions toward COVID-19 vaccines using tweets; (2) examine theory-informed factors that may affect behavioral intentions toward COVID-19 vaccines; and (3) extract themes to provide information for public health researchers to develop theory-based and evidence-based promotion interventions.
Figure 1.
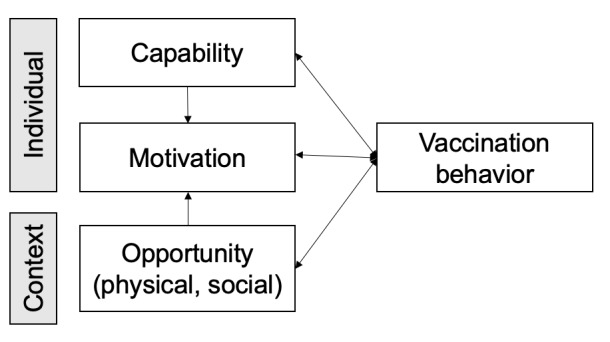
The theoretical model based on the capability, opportunity, motivation—behavior (COM-B) model adapted to vaccination behavior, developed by the World Health Organization Regional Office for Europe [24,25].
Methods
Adapted COM-B Model
The adapted COM-B model has three theoretical constructs: (1) capability, (2) motivation, and (3) opportunity. The WHO Regional Office for Europe also provided examples for each construct (see Table 1). Capability refers to the individual’s physical and psychological ability to perform the behavior, along with the knowledge and skills required to complete the activity [17]. In particular, psychological ability is the ability of an individual to have the necessary thought processes, such as being able to understand, reason, etc [17]. Motivation has a broad definition that includes goals and conscious decision-making as well as all other individual processes that motivate and lead to behavior, such as automatic processes (habitual processes, emotional responses) and reflective processes (analytical decision-making) [17]. Opportunity refers to the contextual factors that prompt the behavior to occur, including the physical opportunity and the environment and social opportunity [17]. The adapted COM-B model also provides a dynamic relationship between constructs. For example, both capability and opportunity can affect motivation. All three constructs of competence, motivation, and opportunity can generate behavior; on the other hand, behavior can influence these three constructs.
Table 1.
The theoretical constructs in the adapted capability, opportunity, motivation–behavior (COM-B) model and associated examples by the World Health Organization Regional Office for Europe.
| Theoretical construct | Examples |
| Capability |
|
| Motivation |
|
| Opportunity (physical) |
|
| Opportunity (social) |
|
Data Collection
We collected English tweets posted from November 1-22, 2020, using a combination of relevant keywords and hashtags: (#covid OR covid OR #covid19 OR covid19) AND (#vaccine OR vaccine OR #vacine OR vacine OR vaccinate OR immunization OR immune OR vax). After excluding retweets, we randomly selected 5000 tweets for manual coding and content analysis. The random numbers were generated through the NumPy package in Python. Then, we mapped the random numbers with the index of collected tweets.
Content Analysis
We performed a content analysis informed by the adapted COM-B model. The coding schema was developed iteratively. First, we developed the coding schema based on the definitions of constructs in the adapted COM-B model. Two reviewers (SL and JL) independently coded 1000 tweets in each round. After completing one round of coding, the two reviewers met with a third reviewer to discuss disagreements and update the coding schema until consensus was reached. We calculated the interrater reliability for the last round. If a tweet mentioned ≥2 constructs simultaneously, we coded it with multiple labels. We conducted chi-square tests to explore the relationship between theoretical constructs with the positive/negative behavioral intention. The statistical significance threshold was .05.
Results
Data Collection
We coded 5000 COVID-19 vaccine–related tweets, which were posted by 4796 unique users. We found 279 tweets that stated their behavioral intentions. The remaining tweets did not state any behavioral intentions toward COVID-19 vaccines. A total of 97 tweets were labeled with positive behavioral intentions, while 182 tweets contained negative behavioral intentions. Among them, 28 tweets were mapped with capability factors; 155 tweets were related to motivation; 23 tweets were related to opportunities; and 74 tweets did not contain any useful information about reasons for their behavioral intentions (see Figure 2). The κ value was 0.73. Of the tweets, 2 mentioned ≥2 constructs at the same time. Tweets that mentioned capability (χ21=17.286, P<.001), motivation (χ21=35.558, P<.001), and opportunity (χ21=4.545, P=.03) were more likely to have negative behavioral intentions (Table 2).
Figure 2.
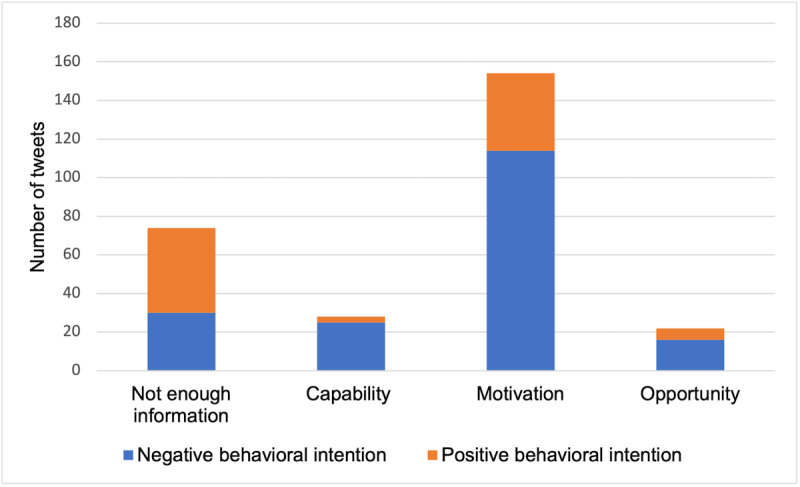
Numbers of tweets containing different theoretical constructs.
Table 2.
Themes and example tweets (n=204).
| Theme | Value, n (%) | Example tweets | |||
| Capability (n=28) | |||||
|
|
Knowledge | 24 (11.8) |
|
||
|
|
Physical condition | 4 (2) |
|
||
| Opportunity (n=22) | |||||
|
|
Rights, regulation and legislation (eg, charging for vaccination, mandatory vaccination, inadequate regulation of vaccines, poor availability of information) | 11 (5.4) |
|
||
|
|
Social and cultural demands and support | 9 (4.4) |
|
||
|
|
Social consequences and reactions to vaccination | 2 (1) |
|
||
| Motivation (n=154) | |||||
|
|
Attitudes and perceptions about the COVID-19 vaccine or the disease itself (eg, disease severity, vaccine effectiveness) | 68 (33.3) |
|
||
|
|
Strong emotions about COVID-19 vaccine (eg, fear of side effects, unfairness to COVID-19 survivors) | 5 (2.4) |
|
||
|
|
Values and beliefs (eg, natural immune system, alternative medicine, value of vaccination) | 37 (18) |
|
||
|
|
Confidence and trust (vaccine, health authorities, science, and government) | 13 (6.3) |
|
||
aTbh: to be honest.
bCDC: US Centers for Disease Control and Prevention.
cFDA: US Food and Drug Administration.
Capability
The first theme regarding capability was that some users lacked knowledge about the COVID-19 vaccines and were influenced by misinformation. mRNA vaccines are a new technology, and some believe that these vaccines can alter DNA. As for the vaccine itself, some users believe that it contains a microchip that can be tracked by the government. Some people expressed that they did not know the side effects of COVID-19 vaccines or even their long-term effects. Based on this concern, misinformation was generated that the vaccine could cause sterility, cancer, etc. Other reasons for not getting the vaccine included the belief that the vaccine could make people sick, the belief that there is no need for people who have been infected with COVID-19 to get the vaccine, and that the vaccine does not prevent infection but only alleviates symptoms. All these beliefs reflect a lack of understanding of the COVID-19 vaccines among users. Having more knowledge about vaccines could help people develop positive behavioral intentions; for example, some people mentioned that they could understand why the development process was fast because researchers only needed to isolate the correct strain rather than create one. Others mentioned understanding that vaccines do not contain live viruses, so they would be willing to get the vaccine.
Some users emphasized that their physical condition was not suitable for COVID-19 vaccination and that they were unsure how their body would react after vaccination (eg, recently had an influenza vaccine shot, had a suppressed immune system, had a severe adverse reaction to vaccination in the past, had a stroke).
Opportunity
In the physical opportunities category, some users said they would not accept the vaccine if they had to pay for it. Many users said vaccination should be a free choice and that they would refuse to receive the vaccine if it became mandatory. Some users wanted more regulation of the COVID-19 vaccine, and some were concerned about the availability of information.
Among the social opportunities, we found some factors influencing the COVID-19 vaccination related to social and cultural demands and support, such as going against religion, defying culture, health workers not recommending vaccination, and family members actively discouraging vaccination. Others intended to be vaccinated because of the fear of the social consequences and reactions to vaccination, such as fear of affecting their work and requiring proof of vaccination for many activities in the future.
Motivation
Most of the reasons for behavioral intentions were categorized into the motivation construct. Many users expressed attitudes and opinions about the COVID-19 vaccine or the disease itself, such as not considering the disease to be severe or life-threatening and not considering the vaccine to be effective (because of low efficiency and mutation of the virus). Others assessed the risks and considered the rushed vaccine to be more harmful than COVID-19. Some of those with positive behavioral intentions stated that they chose vaccination because they did not want to be infected with COVID-19.
Some users expressed strong emotions and feelings about COVID-19 vaccines, such as fear of the vaccine and concern about its side effects because it is new. Notably, others felt that vaccination was selfish or unfair, as they would not be exposing themselves to the same risk as others who survived COVID-19; thus, they were reluctant to be vaccinated.
Other themes were values and beliefs. Some users expressed a belief that the body’s natural immune system is better than any vaccine, or they believed more in alternative medicine. On the other hand, others who wanted to be vaccinated emphasized the positive values of vaccination, such as saving more lives, reopening the economy, and returning to normal life.
Confidence and trust were dominant themes. Users expressed distrust in many areas: the quality of the vaccines (hastily manufactured, untested), health authorities, science, companies, and government. For Twitter users in the United States, we found that unlike with other vaccines, part of the reason people do not trust the government is because of their past handling of the COVID-19 pandemic. In addition, the COVID-19 vaccine rollout came during a time when a new president was being elected in the United States, and some people lacked confidence in the newly elected president’s party.
Discussion
Principal Findings
In this study, we conducted a theory-based content analysis using a dataset of 5000 tweets posted from November 1-22, 2020. We identified 279 tweets that contained behavioral intentions regarding COVID-19 vaccines and mapped them to constructs in the adapted COM-B model. We generated nine themes that influence Twitter users’ intentions to receive COVID-19 vaccines. The constructs in the COM-B model could be applied systematically to characterize factors that influence behavioral intentions toward COVID-19 vaccines. In addition, we found that among tweets that simply stated behavioral intentions without including any reason, the number of positive intention tweets was higher than that of negative intention tweets. The results also implied that more than half of the tweets expressing the decision-making process were negative intention tweets. This finding aligns with our expectation of understanding the factors that contribute to vaccine hesitancy to better develop tailored vaccine promotion programs.
The novelty of COVID-19 vaccines and the current social context have created further difficulties in vaccine rollout. Identified barriers of influenza vaccination intention and behavior include lack of confidence (eg, negative attitudes, mistrust), inconvenience (eg, cost, access), calculation (eg, risk assessment), and complacency (eg, underestimating disease severity) [26]. Our results revealed the presence of several other factors that influence behavior toward COVID-19 vaccination. First, misinformation or conspiracy theories about COVID-19 and COVID-19 vaccines are much more prevalent on social media than those about other diseases or their related vaccines [27-29]. Some users were influenced by this misinformation, and this led to refusal of the vaccine. Second, Twitter users expressed concerns about mandatory vaccination. At the Emergency Use Authorization stage, mandatory vaccination is legally and ethically questionable [30]. However, with full Biologics License Application approval, policy makers may mandate vaccination for all populations. Given the existence of users who have strongly indicated that they would not accept mandatory vaccination against COVID-19, policy makers must be cautious in determining vaccination policies for the public. Some studies have suggested that vaccine mandates do not improve vaccine acceptance rates, and a proposed alternative approach is to apply informed risk communication and give people the freedom to choose without compromising personal autonomy [30]. Third, users with positive behavioral intentions emphasized that the positive value of vaccination to society, such as restoring economic and normal life from before the epidemic, motivated them to be vaccinated. This facilitator is uncommon in other vaccination behaviors. This facilitator could be matched with a strategy of converting personal decisions into public acts [31]. Fourth, we observed that some users were reluctant to be vaccinated because they felt that the COVID-19 vaccine was unfair to those who survived. Based on this concern, it may be helpful to select COVID-19 survivors as opinion leaders to promote COVID-19 vaccines, increasing public awareness of the severity and risk of the disease. Fifth, in addition to the mistrust of vaccines and science that also exists for other vaccines, for the COVID-19 vaccine, users in the United States expressed more mistrust of the government for two specific reasons: (1) the previous administration's inappropriate behavior in handling COVID-19 and (2) the lack of confidence in the newly inaugurated president’s political party. These findings were also aligned with previous studies that proposed a role of politics in COVID-19 vaccine hesitancy [8]. Sixth, it is worth noting that even though previous studies have identified that past vaccination behavior can be used to predict future vaccination behavior [32], we found that past experiences with other vaccines may not affect COVID-19 vaccination. For example, one user mentioned:
I'm not against every vaccine in history. Just this specific COVID-19 vaccine. There are many reasons why, for example the nonsensical social regulations.
The above differences contribute to the fact that the rollout of COVID-19 vaccines could be more complicated than that of other vaccines. Researchers need to develop interventions specific to the COVID-19 vaccine to improve acceptance rates. This also provides an opportunity for future studies to comprehensively analyze why behavioral intentions toward COVID-19 vaccines are different from those toward other vaccines.
In several studies, Twitter content analyses have been conducted of health care behaviors other than COVID-19 vaccination. For example, Chew and Eysenbach [14] collected 2009 H1N1-related tweets and identified the resource content posted most often, followed by personal experience, personal opinion, jokes, marketing, and spam. Li et al [33] extracted COVID-19 stigma–related tweets and found that group labeling, responsibility, and peril tweets disseminated the stigma. Furthermore, several studies have validated the usability of tweets through theory-based content analysis to promote breast cancer promotion programs [16,34]. Our study is the first study to analyze the behavior intention of COVID-19 vaccines through a theory-based content analysis using social media content.
Limitations
This study has several limitations. First, we only analyzed the behavioral intentions of users on Twitter. Previous studies have shown that health care providers are the primary advocates for vaccination and largely influence vaccination acceptance rates [35-38]. In this platform, we could not distinguish users’ occupations. However, the themes reported in this study could help researchers to develop evidence-based interventions for the general public. To examine the vaccine behavior of health care providers, we will conduct a questionnaire-based survey, and the results from that study could aid the development of clinical guidelines for health workers. This approach of considering the general public separately from health care providers is also recommended by the TIP approach developed by the WHO Regional Office for Europe [24]. Second, there are differences between behavioral intentions and actual vaccine behaviors. However, behavioral intentions have been shown to directly influence actual behaviors [39-41]. Third, Twitter users are considered to be younger and have a higher level of education than the general public [13]. Based on this concern, further qualitative research could be conducted on the older population, those with lower education levels, or those with limited access to the internet.
In future research, a literature review could be conducted to summarize current implementation strategies for COVID-19 vaccine promotion and map them to the themes identified in this study to determine gaps in recent research. The inner mechanism of the adapted COM-B model—the behavior change wheel—could inform evidence-based and theoretical implementation strategies to improve the effectiveness of COVID-19 vaccine promotion programs.
Conclusion
The study demonstrates the capability of applying the COM-B model to characterize behavioral intentions toward COVID-19 vaccines on the Twitter platform. We successfully generated nine themes of factors that affect behavioral intentions. Positive behavioral intentions were affected by the positive values of vaccination (eg, reduced risk of infection, socioeconomic recovery, return to normal life). In contrast, negative behavioral intentions were associated with attitudes and perceptions about COVID-19 vaccines or the disease itself (eg, underestimation of disease severity, low vaccine effectiveness), values and beliefs (eg, greater belief in the natural immune system), confidence and trust (eg, distrust of government or vaccines), and lack of knowledge. The generated themes could be used to create theory-based and evidence-based implementation strategies to promote COVID-19 vaccines.
Abbreviations
- COM-B
capability, opportunity, motivation–behavior
- HBM
health belief model
- TIP
Tailoring Immunization Programmes
- WHO
World Health Organization
Footnotes
Authors' Contributions: JL and SL conceived the study. SL and JL performed the analysis, interpreted the results and drafted the manuscript. All authors revised the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest: None declared.
References
- 1.WHO coronavirus disease (COVID-19) dashboard. World Health Organization. [2021-01-31]. https://covid19.who.int/
- 2.Liu J, Liu S. The management of coronavirus disease 2019 (COVID-19) J Med Virol. 2020 Sep;92(9):1484–1490. doi: 10.1002/jmv.25965. http://europepmc.org/abstract/MED/32369222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu J, Liu S, Wei H, Yang X. Epidemiology, clinical characteristics of the first cases of COVID-19. Eur J Clin Invest. 2020 Oct 11;50(10):e13364. doi: 10.1111/eci.13364. [DOI] [PubMed] [Google Scholar]
- 4.Pogue K, Jensen J, Stancil C, Ferguson Daniel G, Hughes Savannah J, Mello Emily J, Burgess Ryan, Berges Bradford K, Quaye Abraham, Poole Brian D. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines (Basel) 2020 Oct 03;8(4):582. doi: 10.3390/vaccines8040582. https://www.mdpi.com/resolver?pii=vaccines8040582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020 Sep;26:100495. doi: 10.1016/j.eclinm.2020.100495. https://linkinghub.elsevier.com/retrieve/pii/100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020 Jul;26(7):1470–1477. doi: 10.3201/eid2607.200282. doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schaffer DeRoo S, Pudalov NJ, Fu LY. Planning for a COVID-19 vaccination program. JAMA. 2020 Jun 23;323(24):2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 8.Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020 Oct;263:113356. doi: 10.1016/j.socscimed.2020.113356. https://linkinghub.elsevier.com/retrieve/pii/S0277-9536(20)30575-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams L, Gallant AJ, Rasmussen S, Brown Nicholls LA, Cogan N, Deakin K, Young D, Flowers P. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020 Nov 05;25(4):1039–1054. doi: 10.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 10.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl Trop Dis. 2020 Dec 17;14(12):e0008961. doi: 10.1371/journal.pntd.0008961. https://dx.plos.org/10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong LP, Alias H, Wong P, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020 Sep 01;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Number of monthly active Twitter users worldwide from 1st quarter 2010 to 1st quarter 2019. Statista. 2021. Jan 27, [2021-04-03]. https://www.statista.com/statistics/282087/number-of-monthly-active-twitter-users/
- 13.Wojcik S, Hughes A. Sizing Up Twitter Users. Pew Research Center. 2019. Apr 24, [2021-05-06]. https://www.pewinternet.org/wp-content/uploads/sites/9/2019/04/twitter_opinions_4_18_final_clean.pdf.
- 14.Chew C, Eysenbach G. Pandemics in the age of Twitter: content analysis of Tweets during the 2009 H1N1 outbreak. PLoS One. 2010 Nov 29;5(11):e14118. doi: 10.1371/journal.pone.0014118. https://dx.plos.org/10.1371/journal.pone.0014118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yin H, Yang S, Li J. Detecting topic and sentiment dynamics due to COVID-19 pandemic using social media. ArXiv. Preprint posted online on July 5, 2020 https://arxiv.org/abs/2007.02304. [Google Scholar]
- 16.Diddi P, Lundy LK. Organizational Twitter use: content analysis of tweets during Breast Cancer Awareness Month. J Health Commun. 2017 Mar 19;22(3):243–253. doi: 10.1080/10810730.2016.1266716. [DOI] [PubMed] [Google Scholar]
- 17.Michie S, van Stralen Maartje M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011 Apr 23;6:42. doi: 10.1186/1748-5908-6-42. https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gould GS, Bar-Zeev Y, Bovill M, Atkins L, Gruppetta M, Clarke MJ, Bonevski B. Designing an implementation intervention with the Behaviour Change Wheel for health provider smoking cessation care for Australian Indigenous pregnant women. Implement Sci. 2017 Sep 15;12(1):114. doi: 10.1186/s13012-017-0645-1. https://implementationscience.biomedcentral.com/articles/10.1186/s13012-017-0645-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raupach T, Falk J, Vangeli E, Schiekirka S, Rustler C, Grassi MC, Pipe A, West R. Structured smoking cessation training for health professionals on cardiology wards: a prospective study. Eur J Prev Cardiol. 2014 Jul 24;21(7):915–22. doi: 10.1177/2047487312462803. [DOI] [PubMed] [Google Scholar]
- 20.Fulton E, Brown K, Kwah K, Wild S. StopApp: using the behaviour change wheel to develop an app to increase uptake and attendance at NHS Stop Smoking Services. Healthcare (Basel) 2016 Jun 08;4(2):31. doi: 10.3390/healthcare4020031. https://www.mdpi.com/resolver?pii=healthcare4020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Croker H, Russell SJ, Gireesh A, Bonham A, Hawkes C, Bedford H, Michie S, Viner RM. Obesity prevention in the early years: a mapping study of national policies in England from a behavioural science perspective. PLoS One. 2020 Sep 30;15(9):e0239402. doi: 10.1371/journal.pone.0239402. https://dx.plos.org/10.1371/journal.pone.0239402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flannery C, McHugh S, Anaba AE, Clifford E, O'Riordan M, Kenny LC, McAuliffe FM, Kearney PM, Byrne M. Enablers and barriers to physical activity in overweight and obese pregnant women: an analysis informed by the theoretical domains framework and COM-B model. BMC Pregnancy Childbirth. 2018 May 21;18(1):178. doi: 10.1186/s12884-018-1816-z. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-018-1816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gould GS, Bar-Zeev Y, Bovill M, Atkins L, Gruppetta M, Clarke MJ, Bonevski B. Designing an implementation intervention with the Behaviour Change Wheel for health provider smoking cessation care for Australian Indigenous pregnant women. Implement Sci. 2017 Sep 15;12(1):114. doi: 10.1186/s13012-017-0645-1. https://implementationscience.biomedcentral.com/articles/10.1186/s13012-017-0645-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tailoring Immunization Programmes: TIP. World Health Organization. 2019. [2021-05-06]. https://www.euro.who.int/en/health-topics/disease-prevention/vaccines-and-immunization/publications/2019/tip-tailoring-immunization-programmes-2019.
- 25.Dubé Eve, Leask J, Wolff B, Hickler B, Balaban V, Hosein E, Habersaat K. The WHO Tailoring Immunization Programmes (TIP) approach: review of implementation to date. Vaccine. 2018 Mar 07;36(11):1509–1515. doi: 10.1016/j.vaccine.2017.12.012. https://linkinghub.elsevier.com/retrieve/pii/S0264-410X(17)31752-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schmid P, Rauber D, Betsch C, Lidolt G, Denker M. Barriers of influenza vaccination intention and behavior - A systematic review of influenza vaccine hesitancy, 2005 - 2016. PLoS One. 2017 Jan 26;12(1):e0170550. doi: 10.1371/journal.pone.0170550. https://dx.plos.org/10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kouzy R, Abi Jaoude Joseph, Kraitem A, El Alam Molly B, Karam Basil, Adib Elio, Zarka Jabra, Traboulsi Cindy, Akl Elie W, Baddour Khalil. Coronavirus goes viral: quantifying the COVID-19 misinformation epidemic on Twitter. Cureus. 2020 Mar 13;12(3):e7255. doi: 10.7759/cureus.7255. http://europepmc.org/abstract/MED/32292669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evanega S, Lynas M, Adams J, Smolenyak K. Coronavirus misinformation: quantifying sources and themes in the COVID-19 'infodemic'. JMIR Preprints. doi: 10.2196/preprints.25143. Preprint posted online on October 19, 2020. [DOI] [Google Scholar]
- 29.Al-Rakhami MS, Al-Amri AM. Lies kill, facts save: detecting COVID-19 misinformation in Twitter. IEEE Access. 2020;8:155961–155970. doi: 10.1109/access.2020.3019600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gostin LO, Salmon DA, Larson HJ. Mandating COVID-19 vaccines. JAMA. 2021 Feb 09;325(6):532–533. doi: 10.1001/jama.2020.26553. [DOI] [PubMed] [Google Scholar]
- 31.Volpp KG, Loewenstein G, Buttenheim AM. Behaviorally informed strategies for a national COVID-19 vaccine promotion program. JAMA. 2021 Jan 12;325(2):125–126. doi: 10.1001/jama.2020.24036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin CJ, Nowalk MP, Toback SL, Rousculp MD, Raymund M, Ambrose CS, Zimmerman RK. Importance of vaccination habit and vaccine choice on influenza vaccination among healthy working adults. Vaccine. 2010 Nov 10;28(48):7706–12. doi: 10.1016/j.vaccine.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 33.Li Y, Twersky S, Ignace K, Zhao M, Purandare R, Bennett-Jones B, Weaver SR. Constructing and communicating COVID-19 stigma on Twitter: a content analysis of tweets during the early stage of the COVID-19 outbreak. Int J Environ Res Public Health. 2020 Sep 19;17(18) doi: 10.3390/ijerph17186847. https://www.mdpi.com/resolver?pii=ijerph17186847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lyles CR, López Andrea, Pasick R, Sarkar U. "5 mins of uncomfyness is better than dealing with cancer 4 a lifetime": an exploratory qualitative analysis of cervical and breast cancer screening dialogue on Twitter. J Cancer Educ. 2013 Mar;28(1):127–33. doi: 10.1007/s13187-012-0432-2. [DOI] [PubMed] [Google Scholar]
- 35.Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatr. 2012 Sep 21;12:154. doi: 10.1186/1471-2431-12-154. https://bmcpediatr.biomedcentral.com/articles/10.1186/1471-2431-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cooper LZ, Larson HJ, Katz SL. Protecting public trust in immunization. Pediatrics. 2008 Jul 01;122(1):149–53. doi: 10.1542/peds.2008-0987. [DOI] [PubMed] [Google Scholar]
- 37.Schmitt H, Booy R, Aston R, Van Damme P, Schumacher RF, Campins M, Rodrigo C, Heikkinen T, Weil-Olivier C, Finn A, Olcén Per, Fedson D, Peltola H. How to optimise the coverage rate of infant and adult immunisations in Europe. BMC Med. 2007 May 29;5(1):11. doi: 10.1186/1741-7015-5-11. https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Habersaat KB, Jackson C. Understanding vaccine acceptance and demand-and ways to increase them. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2020 Jan 04;63(1):32–39. doi: 10.1007/s00103-019-03063-0. http://europepmc.org/abstract/MED/31802154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams MD, Rana NP, Dwivedi YK. The unified theory of acceptance and use of technology (UTAUT): a literature review. J Enterp Inf Manag. 2015 Apr 13;28(3):443–488. doi: 10.1108/JEIM-09-2014-0088. [DOI] [Google Scholar]
- 40.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action Control. SSSP Springer Series in Social Psychology. Berlin, Germany: Springer; 1985. [Google Scholar]
- 41.Hale J, Householder B, Greene K. The Persuasion Handbook: Developments in Theory and Practice. Thousand Oaks, CA: SAGE Publications; 2002. The theory of reasoned action; pp. 259–286. [Google Scholar]


