Abstract
Introduction
Chronic venous leg ulcer (VLU) healing is a complex clinical problem. It requires intervention from skilled, costly, multidisciplinary wound-care teams, working with patients to manage their care. Compression therapy has been shown to help heal venous ulcers and to reduce recurrence, with some evidence suggesting the value of exercise as well. These activities require health education and health literacy (HL) as patients must process, understand and consistently apply health information for successful self-management. Research suggests that those most vulnerable to VLUs also tend to have limited HL, but there have been no reviews examining the state of HL in patients with previous or active VLUs. This scoping review aims to examine the level of HL in VLU patients and how HL may link to self-management behaviours (particularly exercise and compression adherence), and their VLU healing generally.
Methods and analysis
We will use Preferred Reporting Items for Systematic Reviews and Meta-Analyses Scoping Review guidelines and the Levac methodology framework to explore eligible papers that examine the effect of HL on their exercise and compression adherence. Electronic databases will be searched (MEDLINE, EMBASE, the Cochrane Library, PsycInfo and Health, OpenGray), examining for all papers on these subjects published between 2000 and 2020. All studies describing compression and or exercise during VLU management will be included. Study characteristics will be recorded; qualitative data will be extracted and evaluated. Quantitative data will be extracted and summarised.
Ethics and dissemination
We will disseminate results through peer-reviewed publications. We will use data (ie, journal articles) from publicly available platforms; so, this study does not require ethical review. The consultation step will be carried out with patients, carers and health professionals as part of an established wound consumer group.
Keywords: wound management, vascular medicine, vascular surgery, preventive medicine, public health
Strengths and limitations of this study.
This scoping review (ScR) protocol is the first to focus on the role of consumers’ health literacy in venous leg ulcer management.
In order to ensure a systematic approach to searching, screening and reporting, we use the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for ScRs tool, the most current guidance on conducting ScRs.
We have included a comprehensive search strategy and data extraction template.
The studies included in the review will be appraised for quality.
Studies published outside of the indicated databases may be missed.
Introduction
Venous leg ulcers (VLUs) are chronic skin ulcers mainly affecting the gaiter area, most often caused by continuous venous hypertension or chronic venous insufficiency.1 VLUs are a common health condition, affecting approximately 1%–3% of people globally.2–4 This is often due to persistent high blood pressure in varicose veins.5 6 The prevalence of VLU increases with age, doubling among those aged over 65 years.7 People with VLU often have various other comorbidities, including arterial hypertension, obesity, non-insulin-dependent diabetes and dyslipidaemia.8 VLU healing, defined as complete wound re-epithelisation,9 is often slow. The chance of recurrence of a healed VLU is high.10 11 The cycle of healing and frequent recurrent episodes has significant economic impact4 12–14 and severely affects VLU patients’ health and well-being, including that of their families.15–17 Despite advances in treatments, sustained healing of VLU continues to be an ongoing problem for patients, health services and health systems.18
Current best practice recommendation for people with active VLU is the use of compression therapy unless the patient has arterial insufficiency, where it is contraindicated.1 Compression therapy promotes VLU healing by reducing the hydrostatic pressure in lower limbs, enhancing venous return1 and preventing venous stasis. Research suggests that the use of below-knee multi-component compression is efficacious and effective.19–21 Consistent compression therapy is recommended to prevent VLU recurrence.1 21 Pharmaceutical, surgical, physiotherapy and other methods can be used as adjunctive to compression, although the evidence of their effectiveness is limited. 22 Other recommendations often include appropriate physical activity, adequate nutrition and leg elevation.1 Of these, physical activity has received mixed evidence on its efficacy when combined with compression.23 24 However, it is still recommended to patients with VLUs to improve VLU healing and reduce the risk of VLU recurrence.24 25
The best practice recommendations (exercise, compression) for treatment require significant patient involvement; however, patient adherence to the VLU management recommendations is often suboptimal.23 24 To optimise healing outcomes, VLU patients should follow the management plan and understand the importance of compression and other recommendations. The management plan should be developed in collaboration with patients in a standard consultation1 26 because shared decision making is paramount for a faster healing outcome.27 An informed patient can participate as an essential partner in the VLU management process.28 The patient’s role is complementary to their healthcare professional’s role, as they monitor symptoms, adhere to compression and adopt health behaviours, following the advice of health professionals.29 30 However, the extent to which patients can follow the advice varies, partially based on their HL.
Patient HL is defined as ‘the ability to obtain, process and understand basic health information and services needed to make appropriate health decisions and follow instructions for treatment.’17 18 There is a distinction between general health literacy (HL) often assessed through population-level surveys,31 and specific HL which deals with health skill and knowledge specific to the condition or disease.29 General HL scales are often used to assess a patient’s general capabilities in navigating their health environment (eg, where do you go for medical advice), often for the purpose of directing health policy at a population scale. Meanwhile, specific HL scales assess individual capabilities in dealing with a specific condition, like heart disease or diabetes. Both general and VLU-specific HL may affect VLU outcomes through affecting patient’s adoption of health behaviours. Improvements in general and specific HL may improve patient knowledge and understanding of the benefits of adhering to VLU self-management recommendations25–27 and support patients to adopt healthy behaviours in line with the agreed plan. For example, when choosing compression hosiery, patients may rely on HL to critique the options based on their analysis of comfort28 which may be opposed to achieving maximum therapeutic benefit.30 Furthermore, HL may enhance their compression application skills due to improved understanding of the manufacturer’s instructions.21 32 Finally, improved HL may influence patient understanding that lifelong compression hosiery is recommended to prevent VLU recurrence.23
Study rationale
Recent research has indicated that people vulnerable to VLUs, those with VLUs and those with other comorbidities tend to have concurrent deficits in HL.33 VLU incidence increases with age13 and older people have been shown to have limited general HL.34 For example, although the 2015 European health literacy survey showed that respondents received an average score of 33.8/50 (demonstrating ‘sufficient’ HL), the majority (58%) of people aged over 66 years had limited HL, compared with less than half of the general population.31 A possible reason is internet usage. Though internet use is proportional to increased HL,35 current research consistently reports that older adults prefer to learn from their healthcare professionals,36 as opposed to independent learning through the use of the internet.37 Qualitative research has shown that VLU patients often discuss the volume of information and skills that are needed for self-management on VLU development as a significant burden, as VLU self-management can be complex.38 The education needs of VLU patients are not well understood39 resulting in unmet HL needs. In general, limited HL in adults is associated with reduced adherence to treatment and health recommendations, poorer health outcomes and increased cost of medical treatment,40 especially among older adults.41 Furthermore, checking on patient understanding is not a routine practice for healthcare professionals,42 although this was recommended in at least one set of international guidelines on VLU care.26 27
Limited qualitative studies published in the past indicate that HL may affect VLU patients’ self-management capabilities,43–45 yet there have been no recent reviews published examining the level of HL of patients with VLUs, and the effect it has on patient’s adoption of health behaviours. These studies suggest that inadequate HL reduces the likelihood of engaging in VLU compression, but there is also the possibility that those with lower HL may not increase their physical activity in response to a VLU (despite also being in the recommendations). One educational intervention study (N=20) indicated that specific HL in VLU is poor, but also demonstrated that there is utility in improving HL in VLU patients. The authors reported that patients felt more confident in VLU management after the educational intervention.46 However, this study did not examine physical activity rates, and was hampered by a small sample size. Therefore, most research in this field requires further refinement.
Furthermore, whether or not HL relates to VLU healing outcomes is not currently known. In some studies, examining other illnesses including type 2 diabetes, HL has a marginal effect on health outcomes. For example, two studies on diabetic foot ulcers have found that lower levels of HL were linked to inappropriate self-care and delayed wound healing.47 48 Furthermore, the potentially mediating or moderating effects of IT skills49 and other psychological concepts, such as self-efficacy50 should be considered, as these factors have been suggested to play a role in HL’s link to healing outcomes.
Given that HL in VLU patients appears less extensively researched than other factors in VLU healing, we opted to conduct a scoping review (ScR). The proposed ScR is a flexible method for identifying and discussing information useful for answering our research questions, and allowing a holistic presentation of the available literature on this topic.51
Study objective
The aim of this review is to scope the research examining the level of HL in VLU patients, and how this level may link to self-management behaviours (particularly exercise and compression adherence), and their VLU healing generally. Findings of this ScR will guide the development of clinical practice guidelines on instructing VLU patients according to their level of HL, as well as an assessment instrument for clinicians caring for VLU patients. We anticipate that the findings of this review will aid practitioners and public health officials in developing HL intervention programmes. These programmes may improve VLU care and facilitate evidence-based practise through improved knowledge translation.
Protocol development
We will conduct the review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extended for scoping review (PRISMA-ScR) outlined in Tricco et al52 (table 1). Methods for this ScR were developed based on guidelines developed by Levac et al53 using the six framework stages as outlined below.
Table 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extended for scoping review (PRISMA-ScR) checklist adapted from PRISMA-ScR (2018)
| Section | Item | PRISMA-ScR checklist | Check | |
| Title | 1 | Identify the report as a scoping review (ScR) | ||
| Abstract | Structured summary | 2 | Provide a structured summary that includes (as applicable) background, objectives, eligibility criteria, sources of evidence, charting methods, results and conclusions that relate to the review questions and objectives | |
| Introduction | Rationale | 3 | Describe the rationale for the review in the context of what is already known. Explain why the review questions/objectives lend themselves to a ScR approach | |
| Objectives | 4 | Provide an explicit statement of the questions and objectives being addressed with reference to their key elements (eg, population or participants, concepts and context) or other relevant key elements used to conceptualise the review questions and/or objectives | ||
| Methods | Protocols and registration | 5 | Indicate whether a review protocol exists; state if and where it can be accessed (eg, a web address); and if available, provide registration information, including the registration number | |
| Eligibility criteria | 6 | Specify characteristics of the sources of evidence used as eligibility criteria (eg, years considered, language and publication status), and provide a rationale | ||
| Information sources | 7 | Describe all information sources in the search (eg, databases with dates of coverage and contact with authors to identify additional sources), as well as the date the most recent search was executed | ||
| Search | 8 | Present the full electronic search strategy for at least one database, including any limits used, such that it could be repeated | ||
| Selection of evidence | 9 | State the process for selecting sources of evidence (ie, screening and eligibility) included in the ScR | ||
| Data charting process | 10 | Describe the methods of charting data from the included sources of evidence (eg, calibrated forms or forms that have been tested by the team before their use, and whether data charting was done independently or in duplicate) and any processes for obtaining and confirming data from investigators | ||
| Data items | 11 | List and define all variables for which data were sought and any assumptions and simplifications made | ||
| Critical appraisal of individual sources of evidence | 12 | If done, provide a rationale for conducting a critical appraisal of included sources of evidence; describe the methods used and how this information was used in any data synthesis (if appropriate) | ||
| Summary measures | 13 | Not applicable for ScRs | ||
| Synthesis of results | 14 | Describe the methods of handling and summarising the data that were charted | ||
| Risk of bias across studies | 15 | Not applicable for ScRs | ||
| Additional analyses | 16 | Not applicable for ScRs | ||
| Results | Selection of sources of evidence | 17 | Give numbers of sources of evidence screened, assessed for eligibility and included in the review, with reasons for exclusions at each stage, ideally using a flow diagram | |
| Characteristics of sources of evidence | 18 | For each source of evidence, present characteristics for which data were charted and provide the citations | ||
| Critical appraisal within sources of evidence | 19 | If done, present data on critical appraisal of included sources of evidence (see item 12) | ||
| Results of individual sources of evidence | 20 | For each included source of evidence, present the relevant data that were charted that relate to the review questions and objectives | ||
| Synthesis of results | 21 | Summarise and/or present the charting results as they relate to the review questions and objectives | ||
| Risk of bias across studies | 22 | Not applicable for ScRs | ||
| Additional analyses | 23 | Not applicable for ScRs | ||
| Discussion | Summary of evidence | 24 | Summarise the main results (including an overview of concepts, themes and types of evidence available), link to the review questions and objectives, and consider the relevance to key groups | |
| Limitations | 25 | Discuss the limitations of the ScR process | ||
| Conclusions | 26 | Provide a general interpretation of the results with respect to the review questions and objectives, as well as potential implications and/or next steps | ||
| Funding | 27 | Describe sources of funding for the included sources of evidence, as well as sources of funding for the ScR. Describe the role of the funders of the ScR |
Stage 1: identifying the research question
Based on the preliminary research, we have developed the following research questions. Our primary research question is:
What levels of HL (both general and specific) have been reported in adults with active or past VLUs across outpatient, home care, community and inpatient care?
Our secondary research questions are as follows:
Is there any relationship between HL and VLU patient adherence to compression and/or exercise?
Is there any relationship between HL and VLU patient healing outcomes?
Stage 2: identifying relevant studies
This search strategy was developed by the research team with guidance from a medical librarian (CF). Eligible studies will be identified from eight databases: The Cochrane Database of Systematic Reviews; The Cochrane Wounds Specialised Register; The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library); OvidMEDLINE; OvidMEDLINE (in-process and other non-indexed citations); Ovid EMBASE; EBSCO CINAHL, Embase and Google Scholar. We will also search trial registries, and reference lists of relevant publications for published and ongoing trials. The search will be limited from January 2000 to December 2020. The literature search will be developed using a combination of medical search headings and free text words. Keywords will be identified and selected from similar articles relevant to the population, concept and context of the study. The keywords and search string relevant to Medline via Ovid can be found in online supplemental appendix 1. The full search will be conducted using Boolean operators and proximity operators, including wildcards, AND, OR, parentheses, quotations and more as per the database used (table 2).
Table 2.
Ovid Medline search strategy. Identified search terms with truncated keywords and MeSH (Medical Subject Headings) terms for the MEDLINE search via Ovid
| Condition: active or past venous leg ulcers | Context: reported levels of health literacy (HL) | Concept: the effect of deficits in HL on patient’s adherence to compression and effect on healing outcomes | |
| Text words | Venous leg Ulcer* Venous ulcer* VLU Venous insufficiency Leg ulcer* Varicose ulcer* |
Health Literacy Educat* Health promotion Health Information Health education Nurse-led education |
Adher* Concord* Compl* Impact Effect Outcome |
| Medline | MeSH: Exp Leg Ulcer/ |
MeSH: Program Evaluation Exp Nursing Research Health education/ or consumer health information/ or health literacy/ or health promotion/ or healthy people programs/ or patient education as topic/ or teach-back communication/ Health facilities/ or hospital units/ or hospitals/ or hospitals, community/ or hospitals, general/ or hospitals, high-volume/ or hospitals, low-volume/ or exp hospitals, private/ or exp hospitals, public/ or exp hospitals, rural/ or exp residential facilities/ or health services/ or exp community health services/ or health services for the aged/ or exp nursing care/ or exp nursing services/ or preventive health services/ or exp rural health services/ |
MeSH: Attitude to health/ or health knowledge, attitudes, practice/ or “treatment adherence and compliance”/ or “patient acceptance of health care”/ or patient compliance/Recurrence treatment outcome/ or treatment failure/ Wound Healing Secondary Prevention Self Care Stockings, Compression |
bmjopen-2020-044604supp001.pdf (21.1KB, pdf)
Stage 3: study selection
We will limit our search to papers published in English from January 2000 to December 2020. Other languages will be excluded because the concept of health, and thus, the concept of HL, varies across languages.54 55 HL studies will be broadly defined to include studies that sought to assess specific (ie, VLU-related) or general health knowledge (ie, where to find general health information). This criterion is deliberately broad, as preliminary searches suggest there is scant literature on this topic. Our study selection will be guided by the following inclusion criteria:
Patients—patients with a current or previous VLU.
Settings—outpatient, community, home care and inpatient care settings where VLU is managed.
Studies—peer-reviewed reviews and studies (qualitative and quantitative) including randomised controlled trials, cohort, case–control, quasi-experimental, cross-sectional, qualitative studies, literature reviews, ScR guidelines, policies and protocols.
Studies that describe knowledge or education or general HL OR an intervention on this with measures at baseline/control group OR a domain relevant to VLU knowledge change will be included. Dependent variables include pre–post knowledge change OR pre–post change in general HL, OR description of HL at that state. For our secondary questions, dependent variables examined will be adherence to exercise recommendations OR adherence to compression in response to a VLU, or the healing rates of those with VLUs.
The following exclusion criteria will apply:
Patients—no diagnosis of VLU. Exclusion of diabetic foot ulcers, pressure ulcers, pressure injuries, vascular insufficiency.
Settings—no non-health care settings (eg, mail out surveys at home).
Studies—narrative reviews, opinions, commentary, conference proceedings. Studies that did not examine knowledge, education or general HL and its relationship with compression adherence will be excluded.
Selection of sources and evidence will take place in four stages.
Step A—initial retrieval, which will be performed by one researcher.
Step B—title screen. Titles that closely meet research aims will be retained. This step will be performed by one researcher.
Step C—abstract screen. Abstracts will be retained if applicable to research aims. This step will be performed by two researchers.
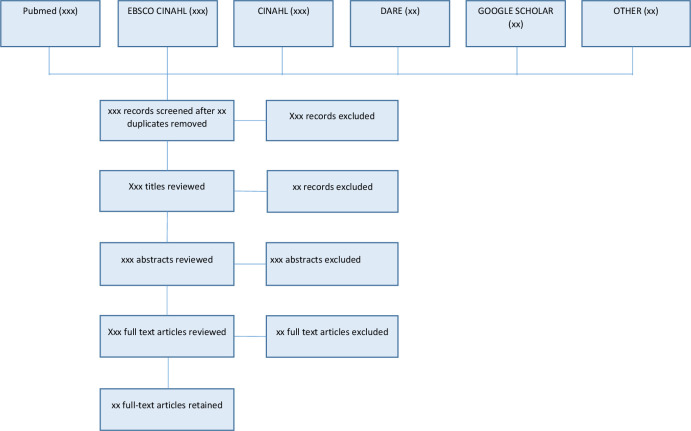
Step D—full text review. Articles retained if they comply with inclusion and exclusion criteria. This will be performed by all authors of the research team. The numbers of retrieved, assessed, excluded and retained articles will be documented using a PRISMA flowchart (template in figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart.
Within this step, we will first pilot a sample of 10 studies to ensure that our methods are robust, following to Stage 4, then re-running a full search again.
Stage 4: charting the data
An excel spreadsheet and/or covidence will be used to chart the data. This database will record the title and year of the publication, authors, study location, intervention type, study population, aims of the study, overview of methods, outcome measures and results. Duplicates will be removed via Endnote’s duplicate detecting function.
Stage 5: collating, summarising and reporting the results
Full texts that are retained will undergo study quality assessment and critical appraisal in order to determine the applicability of findings to clinical practice. We will use the Critical Skills Appraisal Programme (CASP).56 Retained articles will be examined for any qualitative or quantitative descriptions. Findings will be presented in a table that outlines the study type, year the study was undertaken, sample size, study location and patient characteristics.
In order to assess the first research question, we will examine each study against two types of HL: general HL (knowledge or skills) and VLU-specific HL (knowledge or skills). Findings and critical appraisal of the included articles will be provided in a summary of findings and reported in CASP evidence profile table. This table will indicate whether the paper suggested the majority of their sample lacked HL (general or specific). We anticipate that there will be a highly heterogeneous definition of HL in these papers, meaning that authors will be required to use their judgements as to whether or not the paper is relevant, as a degree of simplification will be needed. All entries will be checked by two authors. The lead author will resolve disagreements (if any) independently.
We aim to identify research gaps in the field of VLU treatments by displaying a possible deficit in HL, which translates to lower abilities to adhere to self-management in the form of compression and exercise. The findings are also expected to yield a number of ways HL deficits in VLU patients can be addressed, thereby adding to care and improving standards of care.
Stage 6: consultation—patient and public involvement
This ScR is the first phase in a multistage research programme aimed at developing a feasibility exercise programme as an adjunct to compression intervention for patients with VLUs. During the consultation phase, we will discuss with people with VLUs and their families and caregivers from an established Consumer Wounds Group whether the results of the ScR reflect their needs. The consultation process will take place at the time of a regular consumer group meeting. Data will be gathered using a group interview and Delphi methods. We will map the evidence and identify research gaps and report on compression and exercise treatments by investigating HL, which translates to lower abilities to adhere to self-management in the form of compression and exercise.
Ethics and dissemination
All articles will be sourced from publicly available platforms. As such, this ScR will not require ethical approval. The findings from the ScR will be reported in a separate article and submitted to an open-access peer-reviewed journal. The results of this article will provide an outline of the literature, which will be used to inform future research into HL in patients with VLU. To facilitate knowledge translation and our findings, we will liaise with consumer wounds group. The published protocol and final review will be promoted through social media platforms including Twitter and LinkedIn. We will submit the final review at National and International Wound and Health professional Conferences.
Supplementary Material
Acknowledgments
We would like to acknowledge Ms Cassandra Freeman, a librarian from Hargrave-Andrew library, Monash University, for her support with the development a search strategy.
Footnotes
Twitter: @CarolinaDWeller
Contributors: CDW, SP, GG, JS and LT provided substantial contributions to the conception and design of the work, revisited it critically for important intellectual content, provided final approval of the submitted version and an agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. VT and AB provided substantial contributions to the conception and design of the work, produced the first draft, revisited it critically for important intellectual content, provided final approval of the submitted version and an agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. CR provided substantial contributions to the conception and design of the work, produced the first draft, with the support of a librarian has developed a search strategy, provided final approval of the submitted version and an agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: CDW was supported by the grant from the Australian National Health and Medical Research Council (APP1069329). Other co-authors received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Guarantor of the review: Professor Carolina Weller.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Australian Wound Management Association Inc, New Zealand Wound Care Society Inc . Australian and New Zealand clinical practice guideline for prevention and management of venous leg ulcers. Barton, ACT: Cambridge Publishing, 2011. [Google Scholar]
- 2.Domingues EAR, Kaizer UAO, Lima MHM. Effectiveness of the strategies of an orientation programme for the lifestyle and wound-healing process in patients with venous ulcer: a randomised controlled trial. Int Wound J 2018;15:798–806. 10.1111/iwj.12930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Graves N, Zheng H. The prevalence and incidence of chronic wounds: a literature review. Wound Practice Res 2014;22:4–12. [Google Scholar]
- 4.Xie T, Ye J, Rerkasem K, et al. The venous ulcer continues to be a clinical challenge: an update. Burns Trauma 2018;6:18. 10.1186/s41038-018-0119-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meulendijks AM, Franssen WMA, Schoonhoven L, et al. A scoping review on chronic venous disease and the development of a venous leg ulcer: the role of obesity and mobility. J Tissue Viability 2020;29:190–6. 10.1016/j.jtv.2019.10.002 [DOI] [PubMed] [Google Scholar]
- 6.Weller CD, Team V, Ivory JD, et al. ABPI reporting and compression recommendations in global clinical practice guidelines on venous leg ulcer management: a scoping review. Int Wound J 2019;16:406–19. 10.1111/iwj.13048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pérez MB, López‐Casanova P, Lavín RS. Recent Reports from University of Alicante Highlight Findings in Leg Ulcers [Epidemiology of venous leg ulcers in primary health care: Incidence and prevalence in a health centre-A time series study (2010-2014)] Citation metadata. Int Wound J 2018;16:256–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jockenhöfer F, Gollnick H, Herberger K, et al. Aetiology, comorbidities and cofactors of chronic leg ulcers: retrospective evaluation of 1 000 patients from 10 specialised dermatological wound care centers in Germany. Int Wound J 2016;13:821–8. 10.1111/iwj.12387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thistlethwaite KR, Finlayson KJ, Cooper PD, et al. The effectiveness of hyperbaric oxygen therapy for healing chronic venous leg ulcers: a randomized, double-blind, placebo-controlled trial. Wound Repair Regen 2018;26:324–31. 10.1111/wrr.12657 [DOI] [PubMed] [Google Scholar]
- 10.Finlayson KJ, Parker CN, Miller C, et al. Predicting the likelihood of venous leg ulcer recurrence: the diagnostic accuracy of a newly developed risk assessment tool. Int Wound J 2018;15:686–94. 10.1111/iwj.12911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santler B, Goerge T. Chronic venous insufficiency - a review of pathophysiology, diagnosis, and treatment. J Dtsch Dermatol Ges 2017;15:538–56. 10.1111/ddg.13242 [DOI] [PubMed] [Google Scholar]
- 12.Weller C, Ademi Z, Makarounas-Kirchmann K. Economic evaluation of compression therapy in venous leg ulcer randomised controlled trials: a systematic review. Wound Practice Res 2012;20:21. [Google Scholar]
- 13.Cheng Q, Gibb M, Graves N, et al. Cost-Effectiveness analysis of guideline-based optimal care for venous leg ulcers in Australia. BMC Health Serv Res 2018;18:421. 10.1186/s12913-018-3234-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nussbaum SR, Carter MJ, Fife CE, et al. An economic evaluation of the impact, cost, and Medicare policy implications of chronic nonhealing wounds. Value Health 2018;21:27–32. 10.1016/j.jval.2017.07.007 [DOI] [PubMed] [Google Scholar]
- 15.Ruseckaite R, Richards C, Rutherford C, et al. A conceptual framework of patient-reported outcomes in people with venous leg ulcers. Wound Repair Regen 2020;28:355–63. 10.1111/wrr.12787 [DOI] [PubMed] [Google Scholar]
- 16.Cheng Q, Kularatna S, Lee XJ, et al. Comparison of EQ-5D-5L and SPVU-5D for measuring quality of life in patients with venous leg ulcers in an Australian setting. Qual Life Res 2019;28:1903–11. 10.1007/s11136-019-02128-6 [DOI] [PubMed] [Google Scholar]
- 17.Barnsbee L, Cheng Q, Tulleners R, et al. Measuring costs and quality of life for venous leg ulcers. Int Wound J 2019;16:112–21. 10.1111/iwj.13000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pacella R, Tulleners R, Cheng Q. Solutions to the chronic wounds problem in Australia: a call to action. Wound Practice Res 2018;26:84–98. [Google Scholar]
- 19.Australian Wound Management Association . KPMG Health Economics report: An economic evaluation of compression therapy for venous leg ulcers. Canberra: Australian Wound Management Association, 2013. [Google Scholar]
- 20.Andriessen A, Apelqvist J, Mosti G, et al. Compression therapy for venous leg ulcers: risk factors for adverse events and complications, contraindications - a review of present guidelines. J Eur Acad Dermatol Venereol 2017;31:1562–8. 10.1111/jdv.14390 [DOI] [PubMed] [Google Scholar]
- 21.O'Meara S, Cullum N, Nelson EA, et al. Compression for venous leg ulcers. Cochrane Database Syst Rev 2012;11:CD000265. 10.1002/14651858.CD000265.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Team V, Chandler PG, Weller CD. Adjuvant therapies in venous leg ulcer management: a scoping review. Wound Repair Regen 2019;27:562–90. 10.1111/wrr.12724 [DOI] [PubMed] [Google Scholar]
- 23.Klonizakis M, Tew GA, Gumber A, et al. Supervised exercise training as an adjunct therapy for venous leg ulcers: a randomized controlled feasibility trial. Br J Dermatol 2018;178:1072–82. 10.1111/bjd.16089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jull A, Slark J, Parsons J. Prescribed exercise with compression vs compression alone in treating patients with venous leg ulcers: a systematic review and meta-analysis. JAMA Dermatol 2018;154:1304–11. 10.1001/jamadermatol.2018.3281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orr L, Klement KA, McCrossin L, et al. A systematic review and meta-analysis of exercise intervention for the treatment of calf muscle pump impairment in individuals with chronic venous insufficiency. Ostomy Wound Manage 2017;63:30–43. 10.25270/owm.2017.08.3043 [DOI] [PubMed] [Google Scholar]
- 26.Franks PJ, Barker J, Collier M, et al. Management of patients with venous leg ulcers: challenges and current best practice. J Wound Care 2016;25 Suppl 6:S1–67. 10.12968/jowc.2016.25.Sup6.S1 [DOI] [PubMed] [Google Scholar]
- 27.Gethin G, Probst S, Stryja J, et al. Evidence for person-centred care in chronic wound care: a systematic review and recommendations for practice. J Wound Care 2020;29:S1–22. 10.12968/jowc.2020.29.Sup9b.S1 [DOI] [PubMed] [Google Scholar]
- 28.Boxall S, Carville K, Leslie G, et al. Compression bandaging: identification of factors contributing to non-concordance. Wound Practice Res 2019;27:6–20. 10.33235/wpr.27.1.6-20 [DOI] [Google Scholar]
- 29.Yamashita T, Kart CS. Is diabetes-specific health literacy associated with diabetes-related outcomes in older adults? J Diabetes 2011;3:138–46. 10.1111/j.1753-0407.2011.00112.x [DOI] [PubMed] [Google Scholar]
- 30.Muldoon J. Compression hosiery for venous conditions: a literature review. J Community Nurs 2019;33:29–34. [Google Scholar]
- 31.Sørensen K, Pelikan JM, Röthlin F, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health 2015;25:1053–8. 10.1093/eurpub/ckv043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shi C, Dumville JC, Cullum N, et al. Compression bandages or stockings versus no compression for treating venous leg ulcers. Cochrane Database Syst Rev 2019;18. 10.1002/14651858.CD013397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Australian Institute of Health and Welfare . Australia’s health 2018. Australia’s health series no. 16 AUS 221. Canberra: AIHW, 2018. [Google Scholar]
- 34.Baker DW, Wolf MS, Feinglass J, et al. Health literacy, cognitive abilities, and mortality among elderly persons. J Gen Intern Med 2008;23:723–6. 10.1007/s11606-008-0566-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamashita T, Bardo AR, Liu D, et al. Literacy, numeracy, and health information seeking among middle-aged and older adults in the United States. J Aging Health 2020;32:33–41. 10.1177/0898264318800918 [DOI] [PubMed] [Google Scholar]
- 36.Turner AM, Osterhage KP, Taylor JO, et al., . A closer look at health information seeking by older adults and involved family and friends: design considerations for health information technologies. AMIA annual symposium proceedings. Maryland: American Medical Informatics Association, 2018. [PMC free article] [PubMed] [Google Scholar]
- 37.Chaudhuri S, Le T, White C, et al. Examining health information–seeking behaviors of older adults. Comput Informatics Nurs 2013;31:547–53. 10.1097/01.NCN.0000432131.92020.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chase SK, Melloni M, Savage A. A forever healing: the lived experience of venous ulcer disease. J Vasc Nurs 1997;15:73–8. 10.1016/s1062-0303(97)90004-2 [DOI] [PubMed] [Google Scholar]
- 39.Shanley E, Moore Z, Patton D, et al. Patient education for preventing recurrence of venous leg ulcers: a systematic review. J Wound Care 2020;29:79–91. 10.12968/jowc.2020.29.2.79 [DOI] [PubMed] [Google Scholar]
- 40.Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- 41.MacLeod S, Musich S, Gulyas S, et al. The impact of inadequate health literacy on patient satisfaction, healthcare utilization, and expenditures among older adults. Geriatr Nurs 2017;38:334–41. 10.1016/j.gerinurse.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 42.Graham S, Brookey J. Do patients understand? Perm J 2008;12:67. 10.7812/tpp/07-144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Walshe C. Living with a venous leg ulcer: a descriptive study of patients' experiences. J Adv Nurs 1995;22:1092–100. 10.1111/j.1365-2648.1995.tb03110.x [DOI] [PubMed] [Google Scholar]
- 44.Chase SK, Whittemore R, Crosby N, et al. Living with chronic venous leg ulcers: a descriptive study of knowledge and functional health status. J Commun Health Nurs 2000;17:1–13. 10.1207/S15327655JCHN1701_01 [DOI] [PubMed] [Google Scholar]
- 45.Probst S, Séchaud L, Bobbink P, et al. The lived experience of recurrence prevention in patients with venous leg ulcers: an interpretative phenomenological study. J Tissue Viability 2020;29:176–9. 10.1016/j.jtv.2020.01.001 [DOI] [PubMed] [Google Scholar]
- 46.CLARKE C, WHITMORE L, WEBB A. Patient education pictorial boards: improving patients' understanding of venous leg ulcer and compression therapy. Wounds UK 2020;16:54–60. [Google Scholar]
- 47.Margolis DJ, Hampton M, Hoffstad O, et al. Health literacy and diabetic foot ulcer healing. Wound Repair Regen 2015;23:299–301. 10.1111/wrr.12311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lael-Monfared E, Tehrani H, Moghaddam ZE, et al. Health literacy, knowledge and self-care behaviors to take care of diabetic foot in low-income individuals: application of extended parallel process model. Diabetes Metab Syndr 2019;13:1535–41. 10.1016/j.dsx.2019.03.008 [DOI] [PubMed] [Google Scholar]
- 49.Boren SA. A review of health literacy and diabetes: opportunities for technology. J Diabetes Sci Technol 2009;3:202–9. 10.1177/193229680900300124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xu XY, Leung AYM, Chau PH. Health literacy, self-efficacy, and associated factors among patients with diabetes. Health Lit Res Pract 2018;2:e67–77. 10.3928/24748307-20180313-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pham MT, Rajić A, Greig JD, et al. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods 2014;5:371–85. 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 53.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Choi TST, Walker KZ, Ralston RA, et al. Diabetes education needs of Chinese Australians: a qualitative study. Health Educ J 2015;74:197–208. 10.1177/0017896914523276 [DOI] [Google Scholar]
- 55.Walker C, Weeks A, McAvoy B, et al. Exploring the role of self-management programmes in caring for people from culturally and linguistically diverse backgrounds in Melbourne, Australia. Health Expect 2005;8:315–23. 10.1111/j.1369-7625.2005.00343.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Singh J. Critical appraisal skills programme. J Pharmacol Pharmacother 2013;4:76. 10.4103/0976-500X.107697 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-044604supp001.pdf (21.1KB, pdf)