ABSTRACT
Objectives:
A culturally adapted and validated Oral Health-Related Quality of Life (OHRQoL) inventory helps to reliably compare patient perceptions among different populations. The Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ) evaluates the impact of dental aesthetics on OHRQoL. This study aimed to develop a regional version of PIDAQ (PIDAQMal) for the Indian population and to assess differences in perceptions due to malocclusion in different population groups.
Materials and Methods:
PIDAQMal was derived through the translation process and pilot-tested to assess test–retest reliability. Psychometric properties were tested on 285 subjects (31.2% males, 68.8% females; age range 18–25 years). Normative treatment need was assessed using Index of Orthodontic Treatment Need (IOTN)-Dental Health Component and subjective assessment using IOTN-Aesthetic Component (AC) and Perception of Occlusion Scale (POS). PIDAQMal mean domain scores were compared with those of the previously validated versions to assess difference in perceptions.
Results:
Internal consistency and test–retest reliability were good (Cronbach’s α = 0.83–0.88; Intraclass Correlation Coefficient = 0.74–0.91). IOTN-AC and POS scores showed significant correlation with PIDAQMal scores ensuring convergent validity (P < 0.001). Discriminant validity was confirmed by statistically significant differences (P < 0.001) in PIDAQMal scores between subjects with no treatment need and moderate/definite need. Factor analysis derived four domains with one item showing cross-loading. Difference in mean domain scores among the previously validated versions of PIDAQ confirmed socio-cultural differences in perceptions due to malocclusion.
Conclusion:
PIDAQMal was found to be reliable and valid for the Indian subjects and can be used as a condition-specific OHRQoL measure. Socio-cultural differences in perceptions were brought to light using the translated scale.
KEYWORDS: Oral health-related quality of life, perception, psychosocial, translation, validity
INTRODUCTION
The orofacial region is an area of prime concern to individuals as it draws major attention during interpersonal communications.[1] Quality of life (QoL) is an individual’s perception of well-being that results from satisfaction/dissatisfaction with the aspects of life that are of greater significance to him/her.[2] Oral health forms a vital part of general health which is crucial for well-being and is a determining factor of QoL; whereas Oral Health-Related Quality of Life (OHRQoL) is a subset of QoL pertaining to the health of oral tissues. Malocclusion comprises a broad array of dental malalignments such as protruded teeth, crowding, spacing, rotations, etc. It is one of the most prevalent oral conditions, next to dental caries and periodontal disease, and ranks third among the worldwide dental health problems.
Most patients seek orthodontic care for aesthetic reasons which are reflected in their psychosocial well-being. This indicates a need for psychometric scales to assess the impact of malocclusion on OHRQoL. The Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ) developed by Klages et al.[3] is a condition-specific (CS) scale that evaluates the psychosocial impacts of dental aesthetics on OHRQoL similar to the Orthognathic Quality of Life Questionnaire (OQLQ)[4] for subjects undergoing orthognathic surgery and the Malocclusion Impact Questionnaire (MIQ)[5] for young adolescents seeking orthodontic treatment.
The final version of PIDAQ[3] contains 23 questions in four domains, viz., Dental Self-Confidence (DSC) with six items that measure the influence of dental aesthetics on an optimistic self-image; Social Impact (SI) comprises eight items which weigh stress levels of subjects toward others’ reaction when the individual’s teeth get exposed; Psychological Impact (PI) domain consists of six items that quantify negative feelings toward one’s own dental appearance; and Aesthetic Concern (AC) with three items that evaluate the subject’s discontent toward his/her dentition getting exposed in different situations. Initially drafted in German for use among young adults aged between 18 and 30 years, it was soon professionally translated into English for its worldwide application[3] and subsequently adapted for younger adolescents.[6]
The use of a CS scale in a different geographical area calls for its translation, cross-cultural adaptation, and validation prior to use. This ensures regional comparison of the psychosocial impacts of malocclusions across populations using a standardized scale. PIDAQ has been previously translated into and validated in various languages.[7,8,9,10,11,12,13,14,15,16,17] However, the scale is not available in any of the native languages of the Indian subcontinent except Hindi.[18] Hence, the present study aimed to derive a culturally and semantically equivalent South-Indian version of PIDAQ (PIDAQMal) and to compare the perceptions among subjects of previously validated groups.
MATERIALS AND METHODS
The study commenced after obtaining Institution Ethics Committee approval (IEC/M/14/2017/DCK) and was conducted at the Department of Orthodontics, Government Dental College, Kottayam, Kerala, India. Individuals aged between 18 and 25 years, who reported for orthodontic treatment, were included in the study after obtaining informed consent. Subjects undergoing or with a previous history of orthodontic treatment and those with structural, functional, or cognitive abnormalities were excluded.
The method involved deriving a regional version of the scale (PIDAQMal) followed by its application among the South-Indian population to assess the psychosocial impacts of malocclusion. The process of development of PIDAQMal included validation of both linguistic and psychometric properties. The linguistic validation process comprised a preliminary translation of the questionnaire into Malayalam, a pretest of this version in a sample of 15 subjects followed by back-translation to derive the draft questionnaire. The psychometric validation of the draft scale was performed to ensure its reproducibility, internal consistency, reliability, and construct validity.
TRANSLATIONAL VALIDATION AND CROSS-CULTURAL ADAPTATION OF PIDAQmal
The English version of PIDAQ[3] was translated into the target language by a team of three independent bilingual translators. The team of translators included a public health dentist who was an expert in OHRQoL measures, an orthodontist competent in the translation and validation process, and a college professor. The translations were analyzed with respect to diction and content, taking care of the item and conceptual equivalences between the published and translated versions. Special consideration was given to vernacular expressions and verb tenses. The best among the three translations was selected by consensus as the draft scale. This was pretested on a sample of 15 subjects who reported to the orthodontic outpatient department and the questionnaire was dictated to them individually for clarity of language, ambiguity, and need for any cultural modifications. Responses were collected and discussed with subjects to assess difficulties in understanding each item and the need for any modifications as a means to optimize face validity. The suggested changes were discussed among a panel of specialists from different fields and incorporated into the draft scale based on their recommendations.
The draft questionnaire was back-translated into English by another team of three bilinguals who had not seen the original version beforehand. The team of back-translators included a dentist efficient in the translation and validation process, an expert in QoL measures, and an English-teaching college professor. The three versions (published English, regional version, and back-translated English) were assessed by two postgraduate dental professionals trained in the validation process. Inconsistencies between the back-translated version and the published one were analyzed and rectified, ensuring that the final questionnaire was semantically and conceptually equivalent to the original version.
RELIABILITY TESTING
Test–retest reliability of PIDAQMal was ensured by conducting a pilot test on a class of 30 first-year undergraduate dental students. The same exercise was repeated after 15 days without prior intimation. An insight into the average time needed to complete the questionnaire was also obtained.
CONSTRUCT VALIDATION
Validation was subsequently carried out in 288 subjects who fulfilled the inclusion criteria. The sample size was calculated using the rule of thumb suggested by Plichta and Kelvin[19]: N= number of items in the scale × 10 subjects; hence 23 × 10= 230 was the required number of participants. Accounting for 25% data loss due to incomplete questionnaires, the final sample size was decided to be 288. Sociodemographic data of participants were also collected. The draft questionnaire was administered to subjects in a separate room and adequate time was given to fill the response sheet. Response to each item was rated using a five-point Likert scale as in the original version: 0 = “not at all,” 1 = “a little,” 2 = “somewhat,” 3 = “strongly,” and 4 = “very strongly.”[3] All items in the DSC domain which were positively worded were reverse-scored to bring the direction of scoring in line with other subscales.[9,15,16,17]
EVALUATION OF TREATMENT NEED
Normative treatment need was assessed using Dental Health Component (DHC) and subjective need using Aesthetic Component (AC) of the Index of Orthodontic Treatment Need (IOTN) and Perception of Occlusion Scale (POS). The sample was divided into three IOTN-DHC groups (Group 1 with grades 1 and 2 denoting no need for treatment, Group 2 included grade 3 representing moderate need, and Group 3 with grades 4 and 5 denoting definite treatment need). For assessing IOTN-AC, 10 photographs of anterior teeth depicting different levels of malocclusion were presented to subjects and asked to select the one that most closely simulated their dentition. The photographs were graded on a 10-point scale from the most attractive to the least. The POS includes six items that describe the upper and lower anterior occlusal traits. The response was rated on a five-point Likert scale ranging from 0—“not at all” to 4—“very strongly.”
Convergent validation was performed by comparing PIDAQMal scores with self-rated IOTN-AC and POS scores and discriminant validity by comparing PIDAQMal with the normative assessment of malocclusion status.
Mean domain scores of the available translated versions of PIDAQ were extracted and tabulated for each domain and compared with domain scores of the present study to bring out the sociocultural differences in perceptions.
Data were analyzed using SPSS software (version 16.0, Chicago, IL, USA). Internal consistency was analyzed using Cronbach’s alpha coefficient and test–retest reliability using Intraclass Correlation Coefficient (ICC). Psychometric properties were assessed by performing Exploratory Factor Analysis (EFA) using Principal Component Analysis (PCA) with varimax rotation and Kaiser normalization.[20] One-way analysis of variance (ANOVA) with post hoc Tukey test and Spearman’s correlation were used to validate the scale. Independent t-test compared the difference in perceptions between genders in the sample. The level of significance was set at 5% (P < 0.05).
RESULTS
The study included 288 participants (31.2% males and 68.8% females) with an age range of 18–25 years (mean = 20.43, SD = 2.185). Three questionnaires (1.04%) were incomplete, resulting in a final count of 285 samples. The sociodemographic data are shown in Table 1.
Table 1.
Sociodemographic data of participants
| Demographics | n (%) |
|---|---|
| Gender | |
| Male | 89 (31.2) |
| Female | 196 (68.8) |
| Socioeconomic status | |
| BPL* | 72 (25.3) |
| APL* | 213 (74.7) |
| IOTN-DHC grades | |
| Little need for treatment (grades 1 and 2) | 169 (59.3) |
| Moderate need (grade 3) | 77 (27) |
| Definite need (grades 4 and 5) | 39 (13.7) |
| IOTN-AC grades | |
| Little need for treatment (grades 1–4) | 202 (70.9) |
| Moderate need (grades 5–7) | 62 (21.7) |
| Definite need (grades 8–10) | 21 (7.4) |
| POS scores | |
| 0–1 | 73 (25.6) |
| 2–4 | 42 (14.7) |
| 5–8 | 86 (30.2) |
| ≥ 9 | 84 (29.5) |
*Government criteria for socioeconomic status applied in the surveyed region
BPL: below poverty line, APL: above poverty line
During the pretest, few participants had difficulty in understanding the item “I hold myself back when I smile so my teeth don’t show so much.” Following discussion with experts, minor linguistic modifications were made, which were incorporated into the final version.
Cronbach’s alpha coefficient of the scale was 0.926 and that of the domains ranged from 0.827 for PI to 0.883 for SI [Table 2]. Alpha if item deleted for 23 items and corrected item total correlations are shown in Table 2. The test–retest reliability estimate (ICC) ranged from 0.74 to 0.91.
Table 2.
Item-wise factor loading after Principal Component Analysis and varimax rotation with Kaiser normalization, amount and percentages of explained variance, Cronbach’s alpha if item deleted, and reliability of each subscale
| Items | Components | Cronbach’s alpha if item deleted | |||
|---|---|---|---|---|---|
| SI | DSC | PI | AC | ||
| Proud of teeth | 0.254 | 0.789* | −0.065 | 0.061 | 0.924 |
| Like to show teeth | 0.176 | 0.641* | −0.333 | 0.337 | 0.926 |
| Pleased to see teeth in the mirror | 0.169 | 0.783* | 0.273 | 0.100 | 0.922 |
| Teeth are attractive | 0.071 | 0.753* | 0.248 | 0.193 | 0.923 |
| Satisfied with appearance | 0.17 | 0.740* | 0.303 | 0.039 | 0.923 |
| Find tooth position nice | 0.098 | 0.713* | 0.278 | −0.054 | 0.925 |
| Hold back when I smile | 0.379* | 0.199 | 0.026 | 0.356 | 0.925 |
| What others think | 0.712* | 0.132 | 0.157 | 0.148 | 0.922 |
| Offensive remarks | 0.741* | 0.123 | 0.232 | 0.183 | 0.921 |
| Inhibited in social contacts | 0.801* | 0.063 | 0.039 | 0.166 | 0.922 |
| Hide my teeth | 0.718* | 0.12 | 0.078 | 0.142 | 0.922 |
| People stare | 0.698* | 0.195 | 0.081 | 0.050 | 0.923 |
| Irritated on remarks | 0.741* | 0.071 | 0.224 | 0.127 | 0.922 |
| Worry about opposite sex | 0.712* | 0.207 | 0.164 | 0.137 | 0.921 |
| Envy | 0.356 | 0.024 | 0.564* | 0.254 | 0.924 |
| Somewhat distressed | 0.462 | 0.134 | 0.531* | 0.229 | 0.922 |
| Somewhat unhappy | 0.176 | 0.395 | 0.624* | 0.052 | 0.923 |
| Others have nicer teeth | 0.407 | 0.225 | 0.552* | 0.017 | 0.923 |
| Feel bad | 0.711* | 0.191 | 0.358 | 0.232 | 0.919 |
| Wish teeth looked better | 0.076 | 0.184 | 0.734* | 0.207 | 0.924 |
| Don’t like teeth in mirror | 0.498 | 0.163 | 0.243 | 0.416* | 0.922 |
| Don’t like teeth in photo | 0.269 | 0.109 | 0.219 | 0.842* | 0.923 |
| Don’t like teeth on video | 0.264 | 0.088 | 0.207 | 0.856* | 0.923 |
| Amount of variance explained (initial solution) | 8.29 | 2.52 | 1.48 | 1.28 | |
| Percentage of variance explained (initial solution) | 37.70 | 11.44 | 6.71 | 5.83 | |
| Percentage of variance explained (rotated solution) | 22.44 | 17.06 | 11.95 | 10.23 | |
| Cronbach’s α | 0.86 | 0.88 | 0.83 | 0.83 | |
*Salient factor loading
The values in bold indicate the items showing similar factor loading under a particular domain
The Kaiser–Meyer–Olkin measure of sampling adequacy (0.89) ensured the sample size to be adequate. Data were found to be factorizable as Bartlett’s test of sphericity was significant (P < 0.001). PCA extracted four factors in accordance with the Kaiser–Guttman criterion, each with an eigenvalue more than 1.0. The factor loading of each item following varimax orthogonal rotation along with the amount and percentages of explained variance is listed in Table 2. The first factor contained items belonging to the SI subscale (items 7–14 and 19) which explained 38.86% of the variance. Factor 2 embodied items 1–6 of the DSC subscale and explained 11.12% of the variance. Factor 3 contained items of the PI subscale (15–18 and 20) explaining 6.42% of the variance. Finally, the fourth factor contained items 21–23 of the AC subscale explaining 5.61% of the variance. The four components together accounted for 62.01% of the total variance.
A statistically significant difference (P < 0.001) in the total PIDAQMal scores (mean = 60.42, SE = 1.057) among the IOTN-DHC subgroups tested using ANOVA with post hoc Tukey test ensured discriminant validity of PIDAQMal [Table 3].
Table 3.
Comparison of scores among the DHC of the IOTN categorized groups using one-way ANOVA with post hoc Tukey test
| One-way ANOVA | Post hoc Tukey test | ||||||
|---|---|---|---|---|---|---|---|
| IOTN-DHC categorized groups | N | PIDAQ score mean (SE) | p-value | Intergroup comparison | Difference in PIDAQ score, mean (SE) | p-value | 95% CI of mean difference |
| No need of treatment | 169 | 56.19 (1.353) | No need–moderate need | 8.29 (2.343) | 0.001** | −13.81, −2.77 | |
| Moderate need | 77 | 64.48 (1.796) | <0.001** | Moderate need– definite need | 6.26 (3.350) | 0.149 | −14.16, 1.63 |
| Definite need | 39 | 70.74 (2.735) | No need–definite need | 14.55 (3.028) | <0.001** | −21.69, −7.42 | |
| Total | 285 | 60.42 (1.057) | |||||
A significant correlation (P < 0.001) between PIDAQMal scores and self-rated IOTN-AC (ρ = 0.317) and POS scores (ρ = 0.354) ensured convergent validity [Table 4].
Table 4.
Comparison and correlation of the domain and total scores in subjects with different self-rated ACs of the IOTN scores and POS scores using one-way ANOVA and Spearman’s correlation
| IOTN-AC scores | Dental Self- Confidence | Social impact | Psychological impact | Aesthetic Concern | PIDAQ total | POS scores | Dental Self- Confidence | Social impact | Psychological impact | Aesthetic Concern | PIDAQ total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | ||
| 1–4 (n = 240) | 19.00 (0.362) | 17.07 (0.463) | 16.04 (5.488) | 6.45 (0.220) | 58.55 (1.119) | 0–1 (n = 73) | 16.55 (0.626) | 15.10 (0.658) | 14.23 (0.558) | 5.34 (0.332) | 51.22 (1.589) |
| 5–7 (n = 28) | 23.36 (0.884) | 21.21 (1.479) | 18.86 (1.028) | 7.82 (0.807) | 71.25 (3.495) | 2–4 (n = 42) | 18.17 (0.812) | 17.71 (1.075) | 16.29 (0.890) | 6.79 (0.512) | 58.95 (2.623) |
| 8–10 (n = 17) | 21.18 (1.158) | 20.59 (1.881) | 18.53 (1.295) | 8.65 (0.737) | 68.94 (3.822) | 5–8 (n = 86) ≥ 9 (n = 84) | 20.28 (0.585) 22.12 (0.531) | 17.99 (0.871) 19.62 (0.837) | 17.27 (0.657) 17.68 (0.540) | 7.07 (0.405) 7.50 (0.398) | 62.60 (2.127) 66.92 (1.775) |
| F | 8.728** | 5.505* | 4.598* | 4.744* | 8.880** | F | 8.728** | 5.505* | 4.598* | 4.744* | 8.880** |
| Spearman’s correlation | 0.319** | 0.215** | 0.261** | 0.191** | 0.317** | Spearman’s correlation | 0.398** | 0.231** | 0.252** | 0.243** | 0.354** |
SE: Standard Error, F: statistics and level of significance
*p < 0.05
**p < 0.001
There were no statistically significant differences (P > 0.05) in the mean PIDAQMal scores between males (60.48, SE = 1.71) and females (60.39, SE = 1.33).
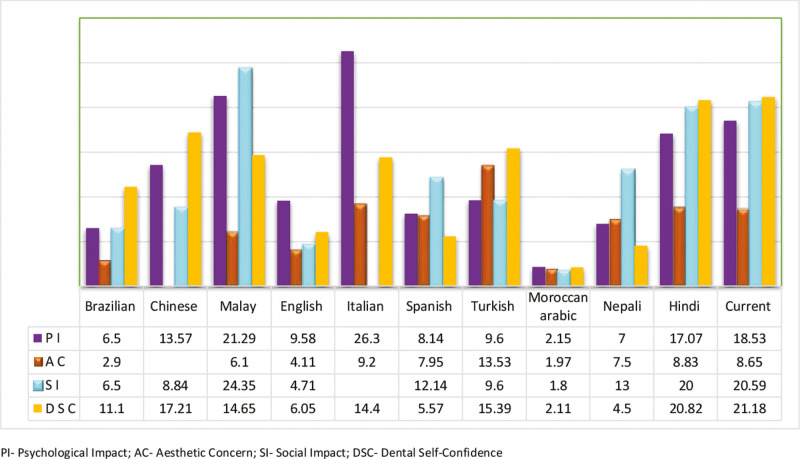
Data extracted from the currently available versions of PIDAQ for PI, SI, AC, and DSC domains are presented in Figure 1. A notable difference in psychosocial impact was evident across the European, Asian, and South American populations. DSC trait, being a positive protective factor against negative impacts of malocclusion, also showed similar variations.
Figure 1.
Comparison of PI, AC, SI, and DSC among the currently available versions of the questionnaire and the present study
DISCUSSION
The importance given to patient-reported outcome measures in clinical studies by international agencies like the World Health Organization paved way for a rise in QoL research over the last two decades. Several OHRQoL assessment scales have been introduced to assess the impact of oral conditions on QoL, which require cross-cultural adaptation and validation prior to use.[4,5,21,22]
PIDAQ is a CS scale that evaluates the self-reported influence of dental aesthetics on OHRQoL.[3] Translation into the native language was performed meticulously, following the guidelines of Guillemin et al.[23] The original and back-translated versions were made similar following minor modifications in the initial translation, which was subsequently pilot-tested to assess test–retest reliability.
The sample size selected based on the rule of thumb was similar to other studies.[7,8,12,15] As PIDAQ was primarily developed for young adults, subjects in the age group of 18–25 years were selected.[7,12,13]
The process of cross-cultural adaptation involves ensuring equivalence between the original and translated versions. It was done according to the steps outlined by Herdman et al.,[24] the same protocol being used in other versions.[7,16,17] The team of experts confirmed the presence of conceptual equivalence between the two versions. Semantic equivalence was attained by transferring the meaning of concepts from the original version to the translated one, thereby achieving similar responses from individuals belonging to different ethnic backgrounds.
With respect to item equivalence, there was difficulty in understanding the item “I hold myself back when I smile so my teeth don’t show so much” during the pretest. This was because an exact linguistic equivalence could not be obtained for the phrase “hold myself back”; hence, words that convey similar meaning were used. This was discussed among the panel of translators. As there were differences among the three translators, the item was presented to another team of two experts who analyzed the three versions and derived a final one by consensus. Malay PIDAQ depicted a similar problem.[16] Recently, when MIQ was cross-culturally adapted to Chinese, an east-west difference in culture was attributed to such issues.[25]
Operational equivalence was ensured using pilot test which confirmed that the mode of administration, format, and response options were acceptable. The questionnaire was effortless to answer and suitable for self-administration with an average response time of 14.5 min per subject. The response time for the Moroccan Arabic version of MIQ which had fewer items than PIDAQ was 10–17 min.[26]
Internal consistency of PIDAQMal was good with Cronbach’s alpha ranging from 0.83 to 0.88, which was higher than the Malaysian English (0.56–0.84)[17] and French PIDAQ (0.67–0.87)[10] while similar to other versions.[3,7,13,14,16] Cronbach’s α of 0.70 or greater is considered acceptable for a new scale and above 0.80 for established scales.[20] Alpha if item deleted remained constant for all items, ensuring the importance of each item contributing to the internal consistency of the scale.
The test–retest reliability was ensured by a repeated measure analysis (ICC) with a 15 days interval. ICC of PIDAQMal (0.74–0.91) was marginally greater than that of Malay PIDAQ (0.72–0.89)[16] and equivalent to the Spanish version (0.76–0.90).[11] The time interval suggested for test–retest reliability ranges from few days to a month.[27] Most previously validated versions have used a similar time interval.[5,7,9,16,17]
When subjected to PCA, PIDAQMal was found to have a similar structure to the original version with four common factors extracted, accounting for 62.01% of the total variance. This is above the minimum value (60%) suggested for the factor solution to be stable.[20] Unlike the present study, the Chinese[9] and Italian[14] versions had three and Nepali PIDAQ[12] had five common factors extracted. The item “I feel bad when I think about what my teeth look like” originally included in the PI domain showed good factor loading under the SI domain in the current study. This might be due to differences in understanding and perception of concepts by the study population compared with other groups. Such cross-loading of items was also reported in other versions.[12,15] The item that faced problems during the pretest, however, showed factor loading under its original domain. But, the loading threshold (0.379) was comparatively lower.
The translated scale demonstrated good convergent validity since its subscales correlated well with self-rated IOTN-AC and POS groups with subjects having higher domain and total scores exhibiting higher IOTN-AC and POS scores. Similar findings were observed in other versions of PIDAQ.[3,12,14] One of the shortcomings of IOTN-AC is that it has no image depicting Class III malocclusion, which represented 9% of the subjects in the present study. Nevertheless, it has been used extensively in studies validating PIDAQ.[3,9,11,12,13,14,15]
The current study had a relatively lesser number of subjects in the moderate and definite treatment need category. However, the results of one-way ANOVA showed that PIDAQMal was able to differentiate individuals with no need for treatment from those with moderate and definite need, thereby demonstrating good discriminant validity. But, it failed to distinguish individuals with moderate need from definite, with the results being statistically not significant (P > 0.05). This represents the dichotomy between normative and psychometric assessments of malocclusion.[1]
Females contribute to majority of participants in this study. This could be attributed to the fact that females are more concerned about their facial appearance and dental aesthetics than males.[28] Also, the last census reports showed a high female to male ratio in the studied region unlike many other regions in the subcontinent. There were no statistically significant gender differences in the domain and total PIDAQMal scores, which is similar to the Nepali version (P > 0.05).[12] This is, however, not in accordance with other studies in which females expressed more concern and dissatisfaction about their dental appearance than males.[28]
A novel feature of this study was an attempt to perform a domain-wise comparison of the mean scores among the previously validated versions of PIDAQ with the current study. This is the purported advantage of calibrating a scale and applying it across populations rather than using different generic scales to measure similar construct.
The psychological impact due to malocclusion among those in the definite malocclusion category was found to be the highest among the Italians (26.3 ± 9.5),[14] followed by the Malay population (21.29 ± 4.92)[16] and least among Brazilians (6.5 ± 4.9).[7] The previously validated Hindi version (17.07 ± 5.14)[18] and the present study (18.53 ± 1.29) showed similar PI demonstrating regional equivalence.
AC was found to be the highest among the Turkish (13.53 ± 8.0)[15] and least with the Brazilians (2.9 ± 3.3).[7] The current study showed a level of concern (8.65) similar to that of the Spanish population (7.95).[11] Few items under PI were loaded under the Aesthetics Attitude domain in the Chinese version[9]; hence, a domain-wise distinction was impossible. The level of social impact due to malocclusion was also high among the Malay version (24.35 ± 7.32),[16] followed by the present and Hindi versions[18] (20.59 ± 1.88 and 20.00 ± 6.96). However, the least SI was observed with the English version (4.71 ± 5.28).[3]
The unique feature of PIDAQ was its attempt to include DSC, a measure of positive attributes due to one’s own dentition. Since the items in this domain were reverse-scored, a low score indicates subjects with a high level of self-confidence due to their dental appearance and vice versa. Moroccan Arabic (2.11 ± 0.82)[13] and Nepali version (4.5)[12] showed the highest DSC among participants. The current study (21.18 ± 1.15), Hindi (20.82 ± 4.8),[18] and Chinese (18.07 ± 3.93)[9] had similar DSC domain score ranges showing cultural similarity among Asians. However, DSC being a subscale that warranted score reversal, we noted the greatest inconsistency in this domain score among versions. The Malay version,[16] though reported reverse-scoring, was not evident from the scores where subjects in the severe malocclusion category showed lesser DSC scores. Whether this was an error in scoring or the real mystery of OHRQoL when compared with normative assessment is unknown. A word of caution while applying DSC should not be overlooked.
Differences in perceptions due to malocclusion across different population groups have been reported in the literature.[29,30,31,32] Kragt et al.[29] in their systematic review found cultural differences in the relationship between malocclusion and OHRQoL. The difference existed both in the perception of malocclusion and in the interpretation of OHRQoL. The reasons attributed were the differences in the prevalence of other oral conditions and the importance given to dentofacial aesthetics in different socio-cultural backgrounds, and variations in the local healthcare system, which are also applicable to the present study.
PIDAQ has been validated for the Malayalam-speaking South-Indian population constituting more than 35 million and those in this category scattered across the globe. PIDAQMal will now be available as a ready-to-use scale to assess the psychosocial impacts due to malocclusion and the improvement after treatment for the above-mentioned population. Also, regional comparisons in the psychosocial impacts can be made using the translated scale.
However, the present study was not without drawbacks. The convenience sample selected did not account for a true representation of the population because the percentage of subjects with definite treatment need was low (13.7%). The responsiveness of the scale could not be studied due to the cross-sectional nature of the study. It necessitates a longitudinal study to ensure this dimension. A malocclusion-specific evaluation of PI would have been more ideal to bring out the perceptions across populations; however, this was not possible due to lack of specific details in the published versions.
CONCLUSION
The English version of PIDAQ was adapted for the Indian population following linguistic and cultural adaptations. The translated and cross-culturally adapted version was found to demonstrate good reliability and validity. A geographical comparison across population groups regarding their psychosocial impacts due to malocclusion demonstrated significant variations. The study provides evidence for the applicability of PIDAQMal as a condition-specific OHRQoL measure to assess the psychosocial impacts of malocclusion among young adults.
FINANCIAL SUPPORT AND SPONSORSHIP
Self-funded.
CONFLICTS OF INTEREST
Nil.
AUTHOR CONTRIBUTIONS
J. M.: Investigation, data curation, writing-original draft preparation
E. P.: Conceptualization, methodology, reviewing, and editing
S. G. A.: Supervision
ETHICAL POLICY AND INSTITUTIONAL REVIEW BOARD STATEMENT
Not applicable.
PATIENT DECLARATION OF CONSENT
Not applicable.
DATA AVAILABILITY STATEMENT
Data used in the current study will be made available on request to the corresponding author.
ACKNOWLEDGEMENTS
We hereby express our sincere thanks to the Kerala University of Health Sciences (KUHS) for reviewing the protocol, research work, and for the final approval.
REFERENCES
- 1.Kiyak AH. Does orthodontic treatment affect patients’ quality of life? J Dent Educ. 2008;72:886–94. [PubMed] [Google Scholar]
- 2.Cunningham SJ, Hunt NP. Quality of life and its importance in orthodontics. J Orthod. 2001;28:152–8. doi: 10.1093/ortho/28.2.152. [DOI] [PubMed] [Google Scholar]
- 3.Klages U, Claus N, Wehrbein H, Zentner A. Development of a questionnaire for assessment of the psychosocial impact of dental aesthetics in young adults. Eur J Orthod. 2006;28:103–11. doi: 10.1093/ejo/cji083. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham SJ, Garratt AM, Hunt NP. Development of a condition-specific quality of life measure for patients with dentofacial deformity: I. Reliability of the instrument. Community Dent Oral Epidemiol. 2000;28:195–201. doi: 10.1034/j.1600-0528.2000.280305.x. [DOI] [PubMed] [Google Scholar]
- 5.Benson PE, Cunningham SJ, Shah N, Gilchrist F, Baker SR, Hodges SJ, et al. Development of the Malocclusion Impact Questionnaire (MIQ) to measure the oral health-related quality of life of young people with malocclusion: Part 2—Cross-sectional validation. J Orthod. 2016;43:14–23. doi: 10.1080/14653125.2015.1114223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klages U, Erbe C, Sandru SD, Brüllman D, Wehrbein H. Psychosocial impact of dental aesthetics in adolescence: Validity and reliability of a questionnaire across age-groups. Qual Life Res. 2015;24:379–90. doi: 10.1007/s11136-014-0767-8. [DOI] [PubMed] [Google Scholar]
- 7.Sardenberg F, Oliveira AC, Paiva SM, Auad SM, Vale MP. Validity and reliability of the Brazilian version of the Psychosocial Impact of Dental Aesthetics Questionnaire. Eur J Orthod. 2011;33:270–5. doi: 10.1093/ejo/cjq066. [DOI] [PubMed] [Google Scholar]
- 8.Spalj S, Lajnert V, Ivankovic L. The psychosocial impact of dental aesthetics questionnaire—Translation and cross-cultural validation in Croatia. Qual Life Res. 2014;23:1267–71. doi: 10.1007/s11136-013-0547-x. [DOI] [PubMed] [Google Scholar]
- 9.Lin H, Quan C, Guo C, Zhou C, Wang Y, Bao B. Translation and validation of the chinese version of the Psychosocial Impact of Dental Aesthetics Questionnaire. Eur J Orthod. 2013;35:354–60. doi: 10.1093/ejo/cjr136. [DOI] [PubMed] [Google Scholar]
- 10.Ngom PI, Attebi P, Diouf JS, Diop Ba K, Badiane A, Diagne F. [Translation and cultural adaptation of a French version of the Psychosocial Impact of Dental Aesthetics Questionnaire: PIDAQ] Orthod Fr. 2013;84:319–31. doi: 10.1051/orthodfr/2013066. [DOI] [PubMed] [Google Scholar]
- 11.Montiel-Company JM, Bellot-Arcis C, Almerich-Silla JM. Validation of the Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ) in Spanish adolescents. Med Oral Patol Oral Cirugia Bucal. 2013:e168–73. doi: 10.4317/medoral.18324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh VP, Singh R. Translation and validation of a Nepalese version of the Psychosocial Impact of Dental Aesthetic Questionnaire (PIDAQ) J Orthod. 2014;41:6–12. doi: 10.1179/1465313313Y.0000000079. [DOI] [PubMed] [Google Scholar]
- 13.Bourzgui F, Serhier Z, Sebbar M, Diouny S, Bennani Othmani M, Ngom PI. Adaptation and validation of the moroccan Arabic version of the Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ) Saudi Dent J. 2015;27:180–6. doi: 10.1016/j.sdentj.2014.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bucci R, Rongo R, Zito E, Valletta R, Michelotti A, D’anto V. Translation and validation of the Italian version of the Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ) among adolescents. Eur J Paediatr Dent. 2017;18:158–62. doi: 10.23804/ejpd.2017.18.02.13. [DOI] [PubMed] [Google Scholar]
- 15.Aglarci C, Baysal A, Demirci K, Dikmen F, Aglarci AV. Translation and validation of the Turkish version of the Psychosocial Impact of Dental Aesthetics Questionnaire. Korean J Orthod. 2016;46:220–7. doi: 10.4041/kjod.2016.46.4.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wan Hassan WN, Yusof ZY, Shahidan SS, Mohd Ali SF, Makhbul MZ. Validation and reliability of the translated Malay version of the Psychosocial Impact of Dental Aesthetics Questionnaire for adolescents. Health Qual Life Outcomes. 2017;15:23. doi: 10.1186/s12955-017-0600-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wan Hassan WN, Yusof ZY, Makhbul MZ, Shahidan SS, Mohd Ali SF, Burhanudin R, et al. Validation and reliability of the Malaysian English version of the Psychosocial Impact of Dental Aesthetics Questionnaire for adolescents. Health Qual Life Outcomes. 2017;15:54. doi: 10.1186/s12955-017-0632-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garg K, Tripathi T, Rai P, Sharma N, Kanase A. Prospective evaluation of psychosocial impact after one year of orthodontic treatment using PIDAQ adapted for Indian population. J Clin Diagn Res. 2017;11:ZC44–8. doi: 10.7860/JCDR/2017/28720.10376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Plichta SB, Kelvin EA. Munro’s Statistical Methods for Health Care Research. London: Philadelphia, PA; 2013. [Google Scholar]
- 20.Streiner DL. Figuring out factors: The use and misuse of factor analysis. Can J Psychiatry. 1994;39:135–40. doi: 10.1177/070674379403900303. [DOI] [PubMed] [Google Scholar]
- 21.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81:459–63. doi: 10.1177/154405910208100705. [DOI] [PubMed] [Google Scholar]
- 22.Adulyanon S, Vourapukjaru J, Sheiham A. Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol. 1996;24:385–9. doi: 10.1111/j.1600-0528.1996.tb00884.x. [DOI] [PubMed] [Google Scholar]
- 23.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J Clin Epidemiol. 1993;46:1417–32. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- 24.Herdman M, Fox-Rushby J, Badia X. A model of equivalence in the cultural adaptation of HRQoL instruments: The universalist approach. Qual Life Res. 1998;7:323–35. doi: 10.1023/a:1024985930536. [DOI] [PubMed] [Google Scholar]
- 25.Li M-Y, He S-L, Wang J-H. Validation of the Chinese version of the Malocclusion Impact Questionnaire (MIQ) Clin Oral Investig. 2020 doi: 10.1007/s00784-020-03565-1. doi: 10.1007/s00784-020-03565-1. [DOI] [PubMed] [Google Scholar]
- 26.Bourzgui F, Diouny S, Mkhantar H, Serhier Z, Bennani Othmani M. Cross-cultural adaptation and validation of “Malocclusion Impact Questionnaire” into Moroccan Arabic. Int J Dent. 2020;2020:8854922. doi: 10.1155/2020/8854922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Norquist JM, Girman C, Fehnel S, DeMuro-Mercon C, Santanello N. Choice of recall period for patient-reported outcome (PRO) measures: Criteria for consideration. Qual Life Res. 2012;21:1013–20. doi: 10.1007/s11136-011-0003-8. [DOI] [PubMed] [Google Scholar]
- 28.Shaw WC. Factors influencing the desire for orthodontic treatment. Eur J Orthod. 1981;3:151–62. doi: 10.1093/ejo/3.3.151. [DOI] [PubMed] [Google Scholar]
- 29.Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM. The impact of malocclusions on oral health-related quality of life in children—A systematic review and meta-analysis. Clin Oral Investig. 2016;20:1881–94. doi: 10.1007/s00784-015-1681-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Volpato GH, de Almeida-Pedrin RR, Oltramari PVP, Freire Fernandes TM, de Almeida MR, de Castro Ferreira Conti AC. Self-perception of facial esthetics by patients with different profiles compared with assessments of orthodontists and lay people. Am J Orthod Dentofac Orthop. 2020;158:840–8. doi: 10.1016/j.ajodo.2019.10.027. [DOI] [PubMed] [Google Scholar]
- 31.Aldhorae K, Alqadasi B, Altawili ZM, Assiry A, Shamalah A, Al-Haidari SA. Perception of dental students and laypersons to altered dentofacial aesthetics. J Int Soc Prev Community Dent. 2020;10:85–95. doi: 10.4103/jispcd.JISPCD_340_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jadav C, Lakshmi MN, Venkataramana I, Srinivasulu E, Mohan C, Babu A. Dental student’s perception of malocclusion and comparison with layman in Hyderabad. Int J Sci Res. 2019;8:23. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used in the current study will be made available on request to the corresponding author.