Abstract
We describe an uncommon cause of paraneoplastic optic neuropathy in adenocarcinoma of the lung. A 45-year-old healthy woman presented with seizure and encephalitis, followed by an acute visual loss in both eyes for 1 week. Her visual acuity was no perception of light in the right eye and hand movement in the left eye. There was a generalised restriction of extraocular muscle movements in both eyes. Funduscopy showed a bilateral pale optic disc. A paraneoplastic antigen autoimmune profile showed a positive anti-CV2/CRMP-5 antibody. CT of the thorax revealed the presence of right apical lung mass, confirmed to be adenocarcinoma through a biopsy. She was scheduled for lung lobectomy and chemotherapy. Unfortunately, her health deteriorated and she passed away eventually.
Keywords: cancer intervention, neuro-oncology, neuro-ophthalmology, lung cancer (oncology)
Background
The paraneoplastic syndromes are a group of rare immune-mediated disorders associated with cancer.1 It may present in the course of cancer due to remote effects of an ectopic hormone released by tumour or autoantibody production directed against cancer or a primary tumour which may precede the cancer diagnosis. The autoantibodies may be found in the patient’s serum and cerebrospinal fluid (CSF) and may cross-react with cells of the nervous system, causing neuronal damage. Hence, although patients with paraneoplastic optic neuropathy (PON) may present with isolated unilateral or bilateral optic neuropathy, the disease can be complicated by various neurological associations. A vast majority of PON has been reported to be associated with small cell lung carcinoma. Less commonly reported tumour associations include B cell lymphoma, cutaneous melanoma, pancreatic glucagonoma, neuroblastoma and uterine sarcoma, and breast, prostate, nasopharyngeal, papillary thyroid lung, non-small lung cell and renal cell carcinomas.2 Prompt recognition of this disorder allows the window of opportunity to diagnose and treat the cancer. We describe a unique case of PON associated with ophthalmoplegia, recurrent seizures and encephalitis secondary to lung adenocarcinoma.
Case presentation
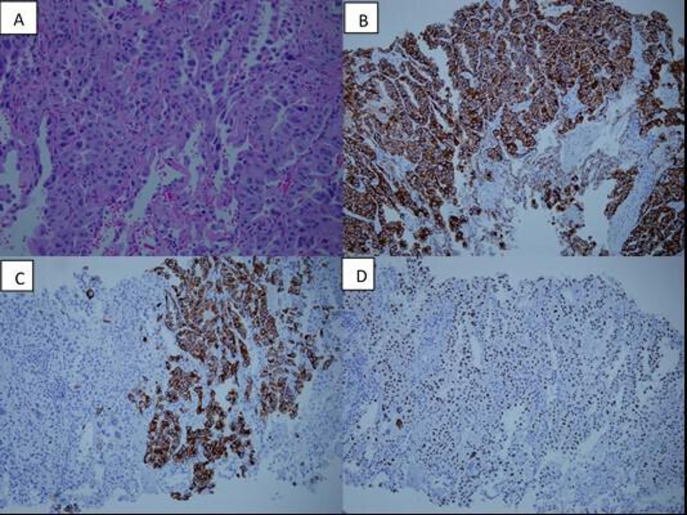
A 45-year-old healthy woman, non-smoker, presented with the sudden onset of persistent severe occipital headaches, followed by several episodes of generalised tonic clonic seizures. There were also episodes of incoherent speech and visual hallucination. It was followed by acute bilateral loss of vision for a week. On presentation, the visual acuity was no perception of light in the right eye and hand movement in the left eye. There was a relative afferent pupillary defect on the right. There was a generalised restriction of extraocular muscle movements in both eyes. Both anterior segments’ examination was unremarkable. Funduscopy showed bilateral pale optic disc with a cup disc ratio of 0.5 (figure 1). Neurological examinations revealed mild agitation with occasional incoherent speech. There was no limb weakness or dyskinesia. Other cranial nerves’ examinations were normal. There was no lymphadenopathy. Other examinations including respiratory, breast, abdomen and gynaecological examinations were normal.
Figure 1.
This figure shows a bilateral pale optic disc, especially at the temporal site. The edges of the disc were well defined.
Investigations
On admission, her full blood count, renal profile, liver function test and peripheral blood film were normal. She was also screened for tuberculosis, syphilis and autoimmune disorders which turned out normal as well. Visual evoked potential (VEP) showed flattening of P100 waves in both eyes, pointing towards pre-chiasmatic optic nerve dysfunction. Contrast enhanced CT and MRI of the brain were normal. Serum aquaporin-4 antibody and myelin oligodendrocyte glycoprotein (MOG) antibody were negative. Chest X-ray and tumour markers including carcinoembryonic antigen, alpha-fetoprotein, CA19-9 and CA125 were within normal limit. In addition, based on the CSF analysis, the opening pressure of the lumbar puncture was 15 cmH2O with clear appearance. The protein and glucose levels were 0.32 g/L and 3.0 (ratio to serum glucose is 0.65), respectively. Minimal white cells were observed (less than 1). Besides, CSF analysis revealed negative results for infective parameters, atypical cells and autoimmune encephalitis panel. However, the serum paraneoplastic antigen autoimmune profile for an anti-collapsing response-mediating protein (anti-CV2/CRMP-5) antibody was positive. Other paraneoplastic antigen autoimmune profiles including anti-amphiphysin, anti-paraneoplastic antigen Ma2, anti-Ri, anti-Yo, anti-Hu, anti-SOX1 and anti-Titin were all negative. The results were suggestive of a paraneoplastic neurological disorder with PON.
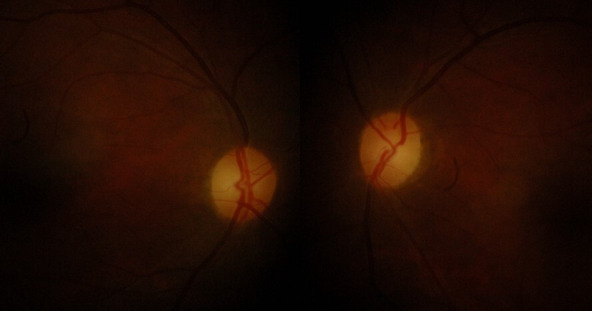
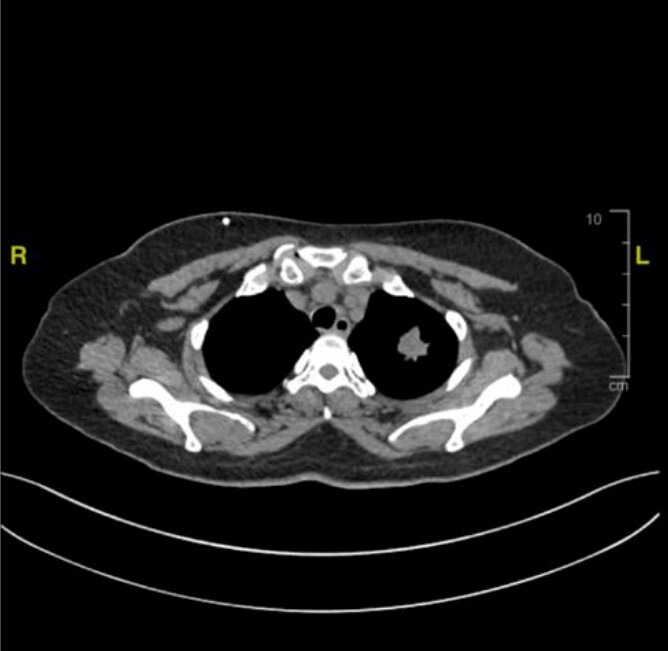
To date, the most common associated malignancies with the positive anti-CV2/CRMP-5 antibody are small cell lung malignancies and gynaecological malignancies. Therefore, CT of the thorax and pelvis (CT-TAP) was performed to screen for primary site of malignancy. CT-TAP showed the presence of multiple enhancing lung lesions at the apicoposterior segment of the left upper lobe with intrapulmonary metastasis into the contralateral lung (figure 2). A positron emission tomography (PET) scan was subsequently performed and further confirmed the presence of a lung malignancy on the left upper lobe with bilateral suprahilar lymph node involvement as well as metastasis at T3 and T4 vertebral bodies. In addition to that, a CT-guided biopsy of the lung mass revealed a malignant epithelial tumour consistent with adenocarcinoma (figure 3).3
Figure 2.
This figure shows the CT of the thorax of our patient with an apical mass over the left upper lobe of the lung. The size of the mass was 2.4×2.3 cm.
Figure 3.
This figure shows the histological changes in lung tissue from the biopsy. (A) Shows lung tissue with neoplastic cells arranged in a complex glandular, acinar and lepidic pattern. The tumour cells exhibit markedly pleomorphic nuclei with prominent nucleoli and a moderate amount of eosinophilic cytoplasm. (B–D) Show malignant cells from the lung tissue, diffusely positive for CK7, CK20 and TTF-1, respectively. The positive results from these immunohistochemical changes indicate that the tumour was a primary lung adenocarcinoma.
Differential diagnosis
The most important differential diagnosis to exclude is space-occupying lesions as the initial presentation was severe headache and seizure. Thus, a neuroimaging investigation is vital in this case. Cerebrovascular accidents with cortical blindness or meningitis with infective optic neuritis are also high in the list of differential diagnoses. However, as all the related investigations turned out normal, all of the above differential diagnoses can be ruled out.
Based on age group and clinical presentation, the diagnosis of autoimmune disease complicated with neurological and ocular presentation should also be considered. Autoimmune diseases such as autoimmune encephalitis, systemic lupus erythematosus, MOG antibody disease, neuromyelitis optica and multiple sclerosis may present as above. However, serology investigations for autoimmune diseases including aquaporin-4 receptor antibodies and MOG markers of this patient were negative.
As the above investigations did not reveal any other clues, further investigations were performed to rule out paraneoplastic neurological syndrome with optic neuropathy. Specific serological markers anti-CV2/CRMP-5 antibody turned out positive. The primary location of the tumour was eventually identified after the CT scan and PET scan revealed a lung malignancy with vertebral metastasis. A histopathological examination of the lung biopsy confirmed adenocarcinoma. All the results led towards a final diagnosis of stage IV adenocarcinoma of the lung with paraneoplastic encephalitis and PON.
Treatment
The patient was started on high-dose intravenous methylprednisolone 250 mg four times per day for 5 days, followed by intravenous immunoglobulin (IVIG) 0.4 g/kg for 5 days. At the same time, she was prescribed with anti-epileptics for the seizure control. After the primary site of malignancy was discovered, she was scheduled for left upper lung lobectomy via video-assisted thoracoscopic surgery. The patient was also counselled for adjuvant chemotherapy after surgery.
Outcome and follow-up
Two weeks after the initial treatment with high dose of corticosteroids and IVIG, her visual acuity improved to hand movement in the right eye and 20/25 in the left eye. Extraocular movements improved as well. However, she remained indecisive with the proposed surgery and chemotherapy by her doctors. Her general condition deteriorated slowly and she passed away after 4 months.
Discussion
PON is one of the paraneoplastic neuro-ophthalmic syndromes associated with systemic malignancies. Other paraneoplastic visual syndromes include cancer-associated retinopathy, melanoma-associated retinopathy, bilateral diffuse uveal melanocytic proliferation, paraneoplastic tonic pupil and ocular movement disorders.1 Paraneoplastic syndromes can be found in up to 10% of patients with malignancies. However, only 0.01% of these patients will present with neurological and visual symptoms.2 Studies have shown that the most common associated systemic malignancy is small cell lung carcinoma, followed by ovarian cancer, B cell lymphoma, neuroblastoma, papillary thyroid cancer, colon cancer, non-small cell lung carcinoma and breast ductal carcinoma.1 2 4 5 In a series by Cohen et al,4 up to 70% of patients can present with neuro-ophthalmic symptoms prior to the diagnosis of malignancies which was similar to our patient’s presentation.3 The disease is also highly associated with smokers but this was not seen in our case.
There are two proposed mechanisms in the pathophysiology of paraneoplastic syndrome: immune-mediated cross-reactivity by the tumour antigen resulting in collateral damage to the normal host tissue, or ectopic secretion of hormones or growth factors resulting in endocrinological abnormalities.1 In PON, an abnormal regulatory protein of neurogenesis, neoplastic CV2/CRMP-5, was found to cross-react with host immune response at optic nerve or may also involve the central and peripheral nervous system.6 The primary tumour produces large amount of this abnormal regulatory protein and leads to extensive damage to the optic nerve and other neurological tissues.2 In our patient, anti-CV2/CRMP-5 antibodies were detected, pointing towards the diagnosis of PON which is most commonly associated with small cell lung carcinoma and sometimes in lung adenocarcinoma as well.
In patients with PON, common ocular presenting signs include bilateral gradual painless loss of vision (ranging from 20/20 up to no perception of light) ranging from days to weeks, gradual constriction of visual fields, optic disc oedema or pallor, as well as associated extraocular motility dysfunction or nystagmus.1 5 At the initial stage of the disease, fundus may show periphlebitis and mild vitritis.1 These may not be clinically symptomatic. Subsequently, in the later stages, there may be arteriolar attenuation together with retinal pigment epithelial pigmentation and thinning in which patients will start to note blurred vision.1 These can be observed on the optical coherence tomography as thinned out central macular thickness with loss of retinal structures and diminished ellipsoid and interdigitation zone.1 Unfortunately, we were unable to demonstrate the findings in this patient due to her unstable clinical condition throughout the treatment in our facilities. In addition, Humphrey visual field (HVF) may show enlarged blind spot, paracentral scotoma, arcuate or altitudinal field defects, and field constriction leading to tunnel vision.7 In our case, the patient rapidly lost her vision within 1 week and her optic disc was pale on presentation together with generalised reduced ocular motility. Other than visual symptoms, PON commonly coexists with neurological dysfunction. Common neurological features include peripheral neuropathy, autonomic dysfunction, limbic encephalitis, cerebellar ataxia, subacute dementia, cranial nerve dysfunction, neuromuscular junction disorder, opsoclonus-myoclonus syndrome and chorea.4 8–10 Patients can have more than one of these neurological presenting signs in paraneoplastic syndrome. Our patient developed severe headache, seizures and encephalitis consistent with neurological presentation.
Further investigations should be carried out early to obtain the definite diagnosis of PON and identify the primary site of malignancy. Late diagnosis will lead to a very poor visual prognosis and mortality rate can be extremely high.4 VEP may show reduced conduction in optic nerve represented by flattening of the P1007 wave which was seen in this particular patient. Moreover, MRI of the brain may show meningeal enhancement in some cases.7 However, there was no evidence of encephalitis or meningitis in our case. A paraneoplastic antigen autoimmune profile can be done either using peripheral blood or CSF.9 It is used to identify the presence of a tumour in remote location which does not have significant physical presentation. There are many forms of antigens and antibodies which represent different types of tumours.7 In our case, anti-CV2/CRMP-5 antibodies were detected and they were highly suggestive of small cell lung carcinoma up to 87% in a cohort study.4 However, based on the biopsy result, this patient had adenocarcinoma (non-small cell lung carcinoma). The CT-TAP and PET scans used to confirm the primary and metastatic lesions in our patient were consistent with previous reports.
The treatment strategy for PON includes symptomatic treatment for visual recovery and definitive cancer-targeted therapy. For symptomatic therapy, immunosuppressants such as high-dose corticosteroids, IVIG, plasma exchange, anti-metabolites such as cyclophosphamide, and intraocular steroid injections have been reported as potential treatment for PON with variable results.4 Our patient had minimal visual improvement with corticosteroids and IVIG. However, her ocular motility was fully restored after treatment. Definitive treatment depends on the stage of the cancer. In our case, the patient was scheduled for lung lobectomy followed by adjuvant chemotherapy. Unfortunately, the patient deteriorated and passed away eventually before definitive treatment could be given to her. Death rate was reported to be up to 58% within 5 years of diagnosis with median of 9.8 months.4 In conclusion, unexplained atypical optic neuropathy associated with other neurological associations should raise the suspicions of PON, after infective and autoimmune aetiologies have been ruled out. Extensive work-out, including tumour and paraneoplastic markers, and radiology investigations, might help in detecting the primary site of malignancy or metastasis (if any). Early stage cancer may be curable. However, PON can be a manifestation of advanced disease, such has been demonstrated in our case. The prognosis in such cases is guarded, which can be fatal most of the time.
Learning points.
Understanding the basic pathophysiology of this rare paraneoplastic disorder is important for a better understanding of the disease.
Recognising the common clinical features of paraneoplastic optic neuropathy is key for early investigation and detection of a remote malignancy.
Performing specific investigations is crucial to rule out possible differential diagnoses to come to the final diagnosis of paraneoplastic optic neuropathy.
Learning the current trend of management for paraneoplastic optic neuropathy is paramount.
Footnotes
Contributors: JYY was one of the physicians in charge of the patient we reported; responsible for writing up the case presentation and data collection, including the consent taking and obtaining the images;and involved in the literature review of the case report as well. W-HWH was the main physician in charge of the patient; provided important intellectual content for the discussion of the write up of the case presentation; and finalised the case report before submission. SAH was the neurologist in charge of the patient; provided expert opinion to co-manage the patient; and provided important intellectual content for the discussion of the case report. NAM was the physician in charge of the patient; assisted in data collection and provided intellectual content for the discussion of the case report.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Przeździecka-Dołyk J, Brzecka A, Ejma M, et al. Ocular paraneoplastic syndromes. Biomedicines 2020;8:490–17. 10.3390/biomedicines8110490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rahimy E, Sarraf D. Paraneoplastic and non-paraneoplastic retinopathy and optic neuropathy: evaluation and management. Surv Ophthalmol 2013;58:430–58. 10.1016/j.survophthal.2012.09.001 [DOI] [PubMed] [Google Scholar]
- 3.Su Y-C, Hsu Y-C, Chai C-Y. Role of TTF-1, CK20, and CK7 immunohistochemistry for diagnosis of primary and secondary lung adenocarcinoma. Kaohsiung J Med Sci 2006;22:14–19. 10.1016/S1607-551X(09)70214-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen DA, Bhatti MT, Pulido JS, et al. Collapsin Response-Mediator protein 5-Associated retinitis, vitritis, and optic disc edema. Ophthalmology 2020;127:221–9. 10.1016/j.ophtha.2019.09.012 [DOI] [PubMed] [Google Scholar]
- 5.Xu Q, Du W, Zhou H, et al. Distinct clinical characteristics of paraneoplastic optic neuropathy. Br J Ophthalmol 2019;103:797–801. 10.1136/bjophthalmol-2018-312046 [DOI] [PubMed] [Google Scholar]
- 6.Nakajima M, Uchibori A, Ogawa Y, et al. CV2/CRMP5-antibody-related paraneoplastic optic neuropathy associated with small-cell lung cancer. Intern Med 2018;57:1645–9. 10.2169/internalmedicine.9736-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cross SA, Salomao DR, Parisi JE, et al. Paraneoplastic autoimmune optic neuritis with retinitis defined by CRMP-5-IgG. Ann Neurol 2003;54:38–50. 10.1002/ana.10587 [DOI] [PubMed] [Google Scholar]
- 8.Dalmau J, Rosenfeld MR. Paraneoplastic syndromes of the CNS. Lancet Neurol 2008;7:327–40. 10.1016/S1474-4422(08)70060-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rogemond V, Honnorat J. Anti-CV2 autoantibodies and paraneoplastic neurological syndromes. Clin Rev Allergy Immunol 2000;19:51–60. 10.1385/CRIAI:19:1:51 [DOI] [PubMed] [Google Scholar]
- 10.Voltz R. Paraneoplastic neurological syndromes: an update on diagnosis, pathogenesis, and therapy. Lancet Neurol 2002;1:294–305. 10.1016/S1474-4422(02)00135-7 [DOI] [PubMed] [Google Scholar]