Abstract
Purpose
This review provides literature views on ocular trauma, with emphasis on common causes of injury, occupational risk, socio-economic factors, management peculiarities and some implications on overall care approach, from prevention to treatment.
Methods
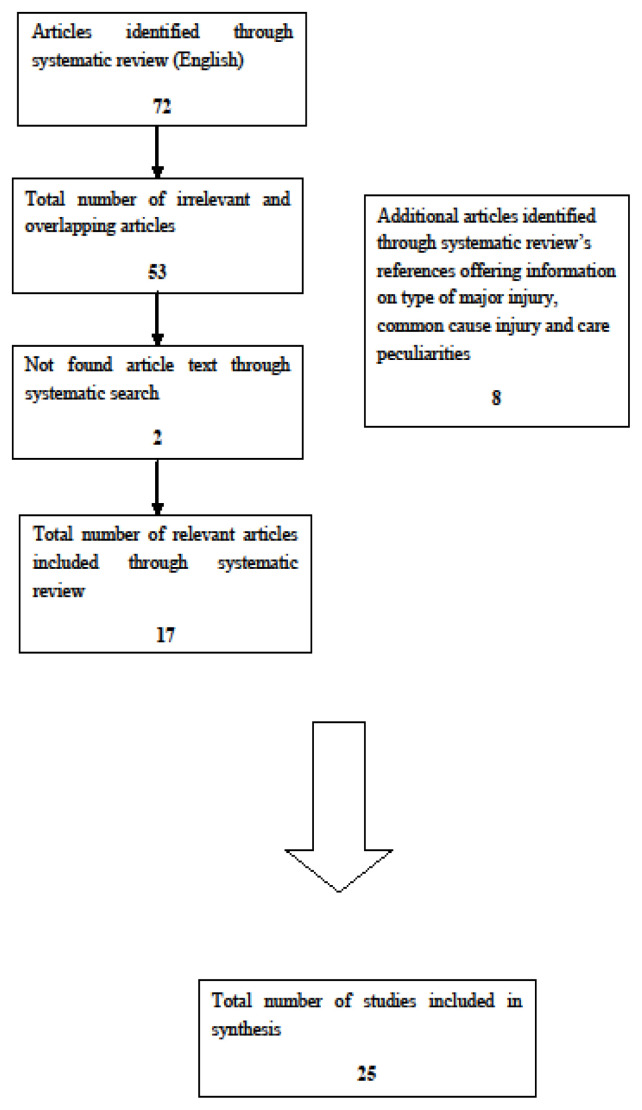
A literature search was performed using key words in PubMed to extract the most relevant articles on ocular injuries, from an occupational point of view. Seventeen relevant articles were included out of seventy-two. Eight relevant articles were found from the references of the articles included and were also added. The total number of articles for this systematic search analysis was twenty-five. Collected information was tabulated in the Appendix.
Results
Most of the included publications were original articles. Many studies were retrospective and cross-sectional with a satisfactory rate of participant recruitment when reported. Most of eye injuries occurred in the workplace. Common eye injuries were due to foreign bodies and corneal abrasions. High-risk occupations included welders, farmers, metalworkers and grinding, construction and manufacturing workers. Most of the injuries could be preventable by using suitable protective eye devices (PED) but appropriate protection is a more complex process than it appears.
Conclusions
Findings of this review showed that it is compulsory to inform people about the risk and consequences of eye injuries. Eye care services should be designed keeping in mind geo-epidemiologic trauma etiology patterns and local health system capacity. Issues of adherence to prevention measures remain object of knowledge dissemination, educational planning and cultural appraisal. Modernizing equipment and respecting workplace regulations are tasks that deserve continuous attention.
Keywords: ocular trauma, systematic review, workers, occupation, ocular injuries, protection
Introduction
During the last fifty years, despite much improvement in terms of prevention and management of ocular injuries in the workplace, ocular trauma still remains one of the most common causes of blindness in the world [1]. According to World Health Organization (WHO), in 1998 evidence across the most developed countries showed that there were almost 1.6 million of blind people globally, due to ocular injuries [1]. About 2.3 million people were diagnosed with bilateral low vision and almost 1.9 million persons with monocular blindness or low vision suffered due to ocular trauma [1].
According to American Optometric Association, the most common professions with increased susceptibility to ocular injury lesions included manufacturing, industry, mining, plumbing electrical, welding and maintenance working activity [2]. However, as it is expected, most of the ocular injuries could be preventable by using suitable protective eye devices (PED) and strict employee’s compliance with the safety rules [2]. Several types of PED are available and a suitable design is based on risk type in the workplace [2]. Finally, non-usage of ocular protective devices is mostly result of unavailability in the workplace or erroneous human decision-making process [3].
Based on the Birmingham Eye Trauma Terminology (BETT), ocular trauma refers to any injury of the eyes due to mechanic wound, chemical factors or radiation and they can be classified to open-globe and closed-globe injuries [4]. Open-globe injuries are full thickness wound of the eye globe and are subdivided into lacerations (caused by sharp objects) and ruptures (caused by blunt objects). Lacerations are subdivided into perforating, penetrating injuries and intraocular foreign bodies [4]. Closed-globe injury is a partial thickness wound (lamellar laceration). It is divided into lesions caused by blunt objects of cornea or sclera tissue and partial thickness wounds caused by sharp objects [5].
Many of the ocular injuries occur in the workplace, without omitting agricultural activities, during sport events, assaults, car accidents, and domestic works. Occupational ocular injuries are defined as those exclusively occurring in the workplace [6]. Ocular injuries occur mainly in men because they are employed in high risk occupations more frequently than females and they tend to work outdoors or more aggressively [7], but an overall ‘snowball’ effect on personal autonomy, family regular living, productivity and demand of community services is always reported in all cases of serious ocular injuries.
The purpose of this study was to conduct a review by providing literature views on ocular trauma occurrence, with emphasis on common causes of injury, occupational risk, socio-economic features, management peculiarities and some implications on overall care approach, from prevention to treatment.
Methods
Literature search
A systematic literature search, through four search attempts in order to cover all possible term meaning equivalents was conducted to identify articles using the following English key words in MEDLINE (PubMed):
((“eye injuries” [MeSH Terms] OR (“eye” [All Fields] AND “injuries” [All Fields]) OR “eye injuries” [All Fields] OR (“ocular” [All Fields] AND “injury” [All Fields]) OR “ocular injury” [All Fields]) AND (“social class” [MeSH Terms] OR (“social” [All Fields] AND “class” [All Fields]) OR “social class” [All Fields] OR (“socioeconomic” [All Fields] AND “status” [All Fields]) OR “socioeconomic status” All Fields])) AND (“2009/10/21” [PDat]:”2019/10/18” [PDat] AND “humans” [MeSH Terms] AND English[lang]) AND “adult” [MeSH Terms]),
((“eye injuries” [MeSH Terms] OR (“eye” [All Fields] AND “injuries” [All Fields]) OR “eye injuries” [All Fields] OR (“eye” [All Fields] AND “injury” [All Fields]) OR “eye injury” [All Fields]) AND (“social class” [MeSH Terms] OR (“social” [All Fields] AND “class” [All Fields]) OR “social class” [All Fields] OR (“socioeconomic” [All Fields] AND “status” [All Fields]) OR “socioeconomic status” [All Fields])) AND (“2009/10/21” [PDat]: “2019/10/18” [PDat] AND “humans” [MeSH Terms] AND English [lang] AND “adult” [MeSH Terms]),
((“eye injuries” [MeSH Terms] OR (“eye” [All Fields] AND “injuries” [All Fields]) OR “eye injuries” [All Fields] OR (“ocular” [All Fields] AND “injury” [All Fields]) OR “ocular injury” [All Fields]) AND (“employment” [MeSH Terms] OR “employment” [All Fields] OR (“occupational” [All Fields] AND “status” [All Fields]) OR “occupational status” [All Fields])) AND (“2009/10/21” [PDat]: “2019/10/18” [PDat] AND “humans” [MeSH Terms] AND English [lang] AND “adult” [MeSH Terms]),
((“eye injuries” [MeSH Terms] OR (“eye” [All Fields] AND “injuries” [All Fields]) OR “eye injuries” [All Fields] OR (“eye” [All Fields] AND “injury” [All Fields]) OR “eye injury” [All Fields]) AND (“employment” [MeSH Terms] OR “employment” [All Fields] OR (“occupational” [All Fields] AND “status” [All Fields]) OR “occupational status” [All Fields])) AND (“2009/10/21” [PDat]: “2019/10/18” [PDat] AND “humans” [MeSH Terms] AND English [lang] AND “adult” [MeSH Terms]).
Apart from articles retrieved by the search, included in Appendix, we also looked into their reference lists and kept all the articles related to ocular trauma (references 25–32 in the Appendix).
Eligibility criteria
Two researchers (EDOK and EKS) screened the key words, the titles and the abstracts to firstly assess content compatibility. All included articles offered information on ocular trauma. There were several articles irrelevant to ocular injuries and they were excluded from this study. Articles that generally described the risk factors on patient’s health of some occupational categories were also excluded. Articles dealing with ocular injuries among specific professions in relation to social aspects were also included.
Data extraction and analysis
Reported information included authorship, publication year and country of each study, publication type, sample size and response rate when available, study design, type of major ocular injury, common cause of injury and care peculiarities (Appendix). Almost all studies fulfilled the details described except from three that care peculiarities were not reported. From all the articles through reference screening, we focused on the type of major injury reported the common cause of injury and care peculiarities.
Results
Literature screening
Systematic search of the literature retrieved 72 articles of which 17 were included in this study and were eligible for all data requirements regarding patients’ characteristics, type and common cause of ocular injuries [8–24]. Overlapping publications through all search attempts made in this systematic review were isolated. Eight studies with ocular injuries were identified through reference tracking tactic and also included in the review [25–32], based on three specific variables that were analyzed: the type of major injuries, the common cause of injury and management peculiarities (Figure 1). These articles are also presented in Appendix [25–32]. The total number of articles included in this review was 25 (Figure 1).
Figure 1.
Systematic review flowchart (PubMed).
Study characteristics and quality figures
All articles, as shown in the Appendix, were published mostly during the last decade and were conducted in countries with different levels of development. Most of the publication types were original and study design was mainly retrospective (n=10), cross-sectional (n=6) and prospective (n=4). Two of the studies included in the Appendix were cohort studies [10,15], while a national survey to identify risk factors of eye injuries among Greek endodontists was identified [12]. One study was descriptive, relating the epidemiology of traumatic lenticular subluxation to low visual loss in Indians, caused by sports activities [9]. A pragmatic randomized trial was also included in the Appendix, investigating the most common cause of injury among quarry workers, as many Indians are employed in quarries from an early age to contribute to their family income [13]. Reported response rate of included studies was over 50%.
Outcome measurements
Eye injuries, causes and care services
Studies included in the Appendix concluded that most eye injuries were work-related [8,10–16,18,20,21–24,26–29]. Working environment and eye injuries is a challenging issue of literature discussion, as workplace is related with serious eye trauma. Most common types of ocular injuries are corneal foreign bodies [8,12,15,22,23,28–30], globe ruptures [24], lamellar lacerations [30], hyphema of the anterior chamber [26] and traumatic cataract [8,13]. It was also shown that severe work-related ocular injuries occur due to chemical burns and they cause serious eye disorders as they destroy all globe tissues, frequently leading to blindness [11,14,16,22]. Many eye injuries also occur during sport activities, especially in childhood (9), assaults mainly in males [25,31] and falls at home in females [25]. High-risk occupations related to eye traumas include metal workers, welders, grinding and construction workers [8,12,23,27–30,32] and workers occupied in chemical industries [11,14,16,22].
Many patients have visited clinics and hospitals [12,16,23], whilst others have delayed to seek medical care because of the distance between their residence and hospital [9]. In a study from USA, about 60% of the reported eye injuries were penetrating lesions and six out of 10 patients admitted to hospital in less than 6 hours [27], while a study in Australia showed that 70% of eye injuries were due to intraocular foreign bodies and admission to hospital was registered in less than 30 minutes [28]. Moreover, patients with corneal lacerations sought for medical treatment with a delay of more than 24 hours, due to the fact that sufferers were unaware of their trauma consequences [31]. Time of recovery or hospital stay depends on type of eye injury. From the available information, average time of recovery among patients with chemical burns was 22 days [16] and in cases of hyphema of the anterior chamber the mean duration of hospital stay was 3–5 days [26]. Patients with chemical burns, corneal abrasions and corneal foreign bodies, being the most common sufferers, needed a follow-up within 6 days [22]. Many eye injuries registered to occur during early and late afternoon [24,31].
Barriers and attitudes towards protective measures
Most of the articles reported that eye injuries occurred in the workplace when use of protective eye devices (PED) is poor [8,10–13,15,16,18,21,23,26–28,30]. It was also suggested that some workers did not use PED due to unavailability [8,21] and ‘unaffordability’ [21]. Another study found that there was low workers’ compliance with safety regulations [23]. Furthermore, two studies found that Indian workers did not wear PED because of the climatic conditions [26] and cultural, mostly language driven, limitations [30]. It was also reported that using faulty devices does not protect [12,22]. Finally, most of the studies supported that educating workers and promoting protective eyewear are essential factors, if attention is paid to all safety regulations.
In detail, as shown in table I, two studies were conducted among cocoa Indian farmers and it was reported that reasons of not using PED were because they were unavailable or faulty [8,21]. Cocoa farmers were also of low education, with poor skills, and they were unaware of ocular trauma risks [8,21]. A study conducted among quarry workers assumed that the reason of not trying PED was due to non-compliance with safety work regulations [13]. Another reason was due to weather conditions (high temperature), so workers felt uncomfortable with PED [26]. Cultural determinants among workers may influence the process of decision making by using or not PED [30]. Language was a limitation among foreign workers to read and understand instructions of using PED, which means that they inevitably ignored a risky situation as not being practically informed [30]. Nationality, as independent risk determinant, does not seem to affect the reasons of not using PED as shown in table I, while educational level and lower social status appear more likely to affect the use of PED.
Table I.
Barriers reported for not using PED classified by environment/occupation and nationality.
| Environment/occupation | Nationality | Barrier |
|---|---|---|
| Workplace (cocoa farmers) | South African | Unavailability and unaffordability, high cost of PED equipment (8) |
| Workplace (chemical workers) | Chinese | Low educational level, luck of safety consciousness and risk awareness (11) |
| Workplace (endododists) | Greek | Inadequacy at the time of injury (12) |
| Workplace (quarry workers) | Indian | Non-compliance with PED regulations in the workplace (13) |
| Workplace (craft, repair and precision production workers) | English | Lack of need for PED (15) |
| Workplace (factory and construction workers) | Chinese | PED was regarded as a routine procedure (16) |
| Workplace (not reported) | Americans | Low education level in addition with improper use of PED (18) |
| Workplace (cocoa farmers) | South African | Lack of economic funds, uncomfortable, unavailability, not seeing well, lack of training and ignorance (21) |
| Workplace (chemical and grinding workers) | Canadian | Inappropriate for specific tasks undertaken, failure to required standards (22) |
| Workplace (grinding workers) | Australian | Poor compliance with PED use and inappropriate for the task undertaken (23) |
| Workplace (not reorted) | Asians | Hot weather and uncomfortable PED (26) |
| Workplace (not reported) | American | The risk for performing a specific task was undertaken (27) |
| Workplace (grinding workers) | Australian | Inadequate protection while grinding. The use of PED supplies only frontal or frontal-side protection (28) |
| Workplace (grinding workers) | Indian | Racial or cultural variations, inappropriate PED and not correctly fitted (30) |
Discussion
Most injuries are occupational and most sufferers are men at a productive period of their life. Nationality does not affect ocular injuries, as shown in table I. However, a study of 2008, in Singapore, showed that racial variation among workers of Indian ethnicity was identified as a barrier for not using PED [30]. Almost limited PED usage is common and reasons differ due to geographic factors, culture determinants, educational level and socio-economic status. Injuries are related to specific occupational activity, being of high risk, such as welders, farmers, metalworkers, manufacturers and grinding workers [8,13,23,27–30,32]. Many ocular injuries were also caused by chemical burns, which seem to be a common cause of ocular injuries [11,14,16,22].
They frequently lead to complete destruction to all globe surface tissues and they cause serious global disorders. As a result, sufferers have important limitations in their daily activities [14]. In a recent study in China, it is shown that 8 out of 10 eye injuries occurred due to inappropriate chemical handling and machine functionality [11]. Moreover, workers were unaware of the risks and safety regulations due to a low educational level [11]. It is expected that educating chemical workers and their employers is essential in order to provide help at a first aid level and reduce complications. In another survey conducted to investigate ocular injuries in the workplace, it was found that workers from low socio-economic and educational level have increased risk of suffering eye injuries, being disproportionally exposed in high risk occupations [8]. Poor knowledge or information on potential eye injury consequences lead to increased risk whilst performing their duties [27]. As shown in table I, there is a variety of barriers for not using PED, and this is independent of nationality. However, it is interesting that workers coming from countries with different development level may not use PED due to difficulty to read or understand PED regulations in the workplace. It is essential for employers to actively undertake efforts to properly inform employees before they perform their duties.
Another study showed that ocular injuries occur during sport activities to younger people and they could be preventable by using PED [9]. There are many children suffering an eye injury, so it is essential to use suitable PED when participating in high risk for ocular trauma sports [9]. Proper PED design and suitable protection is another factor to be taken into consideration. In a survey conducted among Greek endododists, it was found that many eye injuries occur during performing their private practice activity and caused by amalgam particles [12]. It is noted that PED were used at the time of injury, but those were not accurately designed to offer full protection [12].
It is interesting that workers tend to change eye protection behavior after an injury [15]. As work related eye protection behavior improves, the likelihood to use PED when performing a similar task increases due to a then better safety regulation adherence [15]. In a study focusing on socio-economic deprivation and eye trauma, researchers found that one quarter of workers who reported to be intoxicated at the time of injury suffered an ocular injury and those from deprived areas had higher risks [19]. Employers should enhance strict work regulations and alcohol should be prohibited during their working duties, possibly with randomly frequent site testing and penalties. As behavior determinants appear to be interlinked, expression of violence, in many of its forms, is likely to lead to eye traumatic events. Ocular injuries were often caused by assaults particularly in males, while in females eye traumas were caused by falls at home [25, 31].
In some cases, patients seek medical treatment late because of long distances between their residence and hospital, being access affected due to financial limitations as well [9], combined with unawareness about the severity of the injury and its complications [9,31]. There is a need of ‘smartly’ skilled doctors at local primary care units to provide help at a first aid level and perform referrals, when necessary, by facilitating access in terms of good clinical practicing. Types of work related injuries reported to be corneal foreign bodies [8,12,15,22,23,28–30], traumatic cataract [8,13], chemical burns which may cause complete destruction of the globe tissues [15,22], globe ruptures [24], hyphema of the anterior chamber [26], and lamellar lacerations [30]. It was also observed through this systematic review that traumatic cataract was the most common cause of ocular trauma in South Africa and India [8,13]. Moreover, many children suffered an eye injury while working in quarries in India, but quarry owners refused that they employ children [13]. It is worth to be mentioned that many eye injuries caused by chemical burns occurred more often a seasonal occurrence, mostly during summer and autumn than winter and spring [11]. In addition, in a study conducted in Egypt, it was described that 8 out of 10 open globe injuries, occurred between 12:00–5:59 pm [31]. It is expected that as the most common causes of injuries are violent behavior related, some mainly occur at an urban environment. Elaborating similar information, geo-temporal, lesion and cause related, details [2,3,4,6,31,33,34] could be offered, to develop management algorithms, as predictive elements to facilitate proper care access.
As shown in the Appendix, average hospital stay or recovery time is related to the severity of an eye injury. Eye injuries caused by chemical burns have an average recovery period of 22 days [16]. Corneal abrasions and corneal foreign bodies need a follow-up surveillance within 6 days on average [22], hyphema of the anterior chamber, vitreous hemorrhage and corneal perforations of 3–5 day average hospital stay [26]. In Australia, it was reported that 26% of the injured patients sustained another injury in the past during domestic activities such as grinding, and vision loss from a previous trauma in the past was rare but possible [32]. Training initiatives, focused on first aid measures, should be introduced to deal with ocular trauma in order to not lose critical time, especially in those caused by chemical burns [11,14,28] and those occurring during sport activities [9]. In a survey conducted across 21 military hospitals in China, to record ocular injuries at a wide range of occurrence, it was found that the most common listed were due to sports activities [35]. As second cause eye injuries were work-related, in armed police and army during skill training, and it was observed that military training-related eye injuries decreased when personnel were educated [35]. In a survey conducted among Nigerian metal arc welders, the major risk factor for cataract was a past eye injury episode [36]. In countries with increased rates of criminality, where the most common cause of ocular injuries are assaults caused, public opinion should be informed about the consequences of violent behaviors [31], covering issues from socio-economic deprivation effects to substance abuse. Future research is needed to be undertaken in order to provide evidence of how better eye care service design can be supported from preventative to curative actions in regards to ocular trauma. Focusing on a better overall management approach of those injuries it may be useful to discuss some ‘hotspots’ for prospective health planning (Box 1).
Study limitations
A possible limitation of this review is that some relevant articles may have been missed as it is often occurring when a literature search is undertaken [37]. Strict criteria may reduce the ability to expand inclusion sometimes. To minimize this eventuality, all articles were screened and checked by two researchers. Another limitation is that systematic review was based on a single but major database search and to buffer this limitation emphasis was given to all reported references of the included studies by screening them one by one. Due to the study setting and methodology variety, a major effort to offer homogeneous and compact information has been made. For this reason, information was listed in subtopics as shown in the Appendix, in order to better collect research “puzzles” of each study included and offer a more detailed ‘panorama’ of results section. “Minor” trauma such as corneal abrasions and corneal foreign bodies usually heal with no consequences on the visual function, as opposed to open globe injuries, ocular burns and severe closed globe injuries that may be associated with significant visual disability. For this reason, not all eye injury types equally affect sufferers’ quality of life and care demand. Additionally, this review does not analyze the impact of the delayed diagnosis or treatment of patients with ocular trauma, but it focuses on determinants related to the absence or inadequacy of protection measures. This paper mostly addresses issues of occupational medicine rather than clinical information related to ocular trauma. We acknowledge that emphasis is not given on factors determining the outcome of an ocular trauma from a clinical or surgical standpoint as our search offered little information on lesion type distinction (such as the involvement of the anterior or posterior ocular segment or the presence of sight-threatening findings including central corneal lacerations, damage to the macula, the optic disc or the optic nerve). Instead, emphasis is given on the occupational and socio-economic impact of ocular trauma and the need to provide related information to employers, employees, health professionals and health care providers. Retrospective and prospective research projects are required in order to match clinical and outcome information from secondary and tertiary hospital units with better prevention and social care initiatives.
Conclusions
Occupational eye injuries can be major causes of morbidity and disability. Severe ocular wounds such as globe ruptures, corneal foreign bodies, lamellar lacerations, traumatic cataract are grouped among such lesions. Just listing the previously mentioned injuries one can think that proper eye protection is a more complex issue than it appears. Sometimes, PED were not available in the workplace, or they were faulty and not suitable for the task undertaken or the climate, not to mention ignorance, inertia, underestimation, poor education, and other parameters that could influence workers’ decision-making to take cautions. It has been also emerged that most eye injuries could be preventable by using appropriate PED. Educational initiatives by offering information on types of traumas and time of recovery or risk of permanent lesion would be useful. Summarizing information from this review, it appears challenging to promote first aid level services, interlinking primary, secondary and tertiary care through flexible, effective and cost analysis driven decision algorithms, by observing geo-spatial eye care needs, in order to improve outcomes.
APPENDIX *. Summary of studies included from the systematic review
| Author/Year/Country | Publication Type | Sample size/response rate | Study Design | Type of major injury reported | Common cause of injury | Care peculiarities | Main Findings | Implications |
|---|---|---|---|---|---|---|---|---|
| Boadi-Kusi et al/2014/South Africa (8) | Letter | N=185 / (125 males cocoa farmers, 60 females) RR=80,4% (Total number:230) |
Cross-sectional study | The most common type of visual impairment and blindness among cocoa farmers was reported cataract (51.6%) | The most common cause of injuries reported were weeding (40.5%) during farm activity, with flying stones and sand (25.8%). | Of the total number of patients, 79.6% visited hospitals and clinics. | Cocoa farmers are at high risk to suffer an ocular injury in the rural community in Ghana. They are also at high risk on farm related vision disorders. There was found poor use of eye protective devices, probably due to unavailability and high cost. | It is necessary the introduction of an eye care program to educate cocoa farmers in the use of protective eye devices. Government interventions through strict legislation are fundamental in the agricultural industry to minimize the risk of ocular injuries among cocoa farmers in rural Ghana. |
| Khokhar et al/2014/India (9) | Original | N=150 from October 2009 to September 2011 | Descriptive, non-interventional, non-comparative study | The most common type of disorder was lenticular subluxation. | The most common cause of subluxation was blunt trauma (89%) during sport activities by wooden objects. Arrows and bows are the most common causes of injuries among children during sport activities. | The patients delay to seek for medical treatment because of the long distance between their residence and the hospital, due to lack of financial means, and their ignorance about the severity of the injury. | Traumatic lens subluxation is usually related to low visual acuity. Trauma during playing cricket and gulli danda is most frequently seen and blunt trauma contributes to the maximum number of these cases. The ocular morbidity related to ocular trauma has a huge impact because of severe vision loss occurring in a relatively younger population. The study also found that most of the injuries 46.5% happened while doing sports and it is remarkable that none of the children were wearing PED. Patients of high socio-economic classes seek for medical treatment in private units to avoid queues at government-run hospitals. | The survey suggests educating parents and children to avoid risk factors while playing sports. Public awareness campaigns are important to educate all the involved to athletic activities, regarding specific ocular hazards and their prevention. Players must be obligated to wear protective eye glasses, as injury can cause considerable ocular damage. It is also important a training program to deal with ocular trauma at a first aid level before seeking specialized care at the hospital. |
| Asharlous et al/2018/Tehran, Iran (10) | Original | N=140 welders and N=172 non-welders were selected as study groups | Historical Cohort study | The most common type of disorder was tear film secretion and dry eyes in welders due to exposure to ultraviolet light. | The most common cause of tear film problems in welders was due to ultraviolet light exposure in the workplace. | Not reported | Dry eye in welders is much higher than non-welders. Furthermore, there is a high percentage of welders suffering from severe dry eye and low tear production in addition to tear film instability. Aqueous-deficient is the most common cause of dry eyes in welders. | The results of the survey suggest that the workplace of welders should be improved while designing and employing safety equipment is essential. Work safety equipment should be mandatory in the workplace of the welders, as it reduces tear vaporization and UV radiation. |
| Ye et al/2016/China (11) | Original | N=690/ (619 males and 71 females)/years 2004–2013 | Retrospective study | The survey was conducted to document the epidemiology of chemical burns | The most common cause of chemical burns occurred in the workplace by acidic substances. | According to the results of the survey, chemical burns were more frequent during summer and autumn, than in winter or spring. One-fifth of patients underwent surgery. | .This study found that 86.24% of chemical burns occurred due to inappropriate chemical handling, machine operation and functioning problems in private and state-owned enterprises. The majority (94%) of chemical burns occurred in work-age workers. The most common burn sites were the head, neck and extremities. Most of the patients had low educational level so they were not safety conscious or danger awareness. | A long-term strategic plan should be established to improve education of the workers and improve the management of chemical burns. Private and state-owned enterprises should provide safe and protective eye equipment for workers to reduce the risk of suffering a chemical burn. Improvement of medical treatment for chemical burns is also considered essential. |
| Zarra et al/2013/Greece (12) | Original | N=147 endodontists with response rate 84% | National questionnaire survey | The most common type of eye injury was foreign bodies caused by amalgam particles. | Most eye injuries were work related and occurred during private practice (n=99, 82.5%) | Medical assistance was sought in 16% of the most recent accidents. Endodontists did the first aid provision in the majority of cases (80%), by irrigating the injured eye with tap water or normal saline. Patients with normal vision sought ocular treatment less frequently than those with eyesight deficiencies. | Significant predictors of ocular accidents among Endodontists were reported clinical practice and use of magnification since graduation. The majority of the sample reported that they were using eye protection, but it was considered inadequate at the time of the eye injury. There was reported no permanent eye damage among Endodontists. | Visual impairment should be timely corrected among Endodontists, because their profession is one of the highest visual demands. |
| Adams et al/2013/India (13) | Original | N=204 consenting adult stone quarry workers from 6 quarries between September 2006 and March 2007. | Randomised trial | The most common type of injury among quarry-workers, was traumatic cataract, intraocular foreign bodies, corneal tear suturing and retinal detachments requiring surgery. | The survey conducted among stone-quarry workers with the most common cause of ocular injury to occur whilst cutting stones in the workplace (quarry). | There were many children working in quarries in India. They start working there from an early age to contribute to their family income. So, there were many children with eye injuries, but frequencies are difficult to be measured, because of the refusal of quarry owners and the children’s family to identify them as quarry workers. In addition, none of the quarry owners accepted the fact that they employ kids. | Providing protective eyewear and specific education programs will be helpful to reduce ocular trauma among stone-quarry workers. It was found that the main reason of not wearing PED was non-compliance with work safety regulations. Wearing protective eyewear should be mandatory, and should be provided by the owners of quarries. They should also encourage employees to wear them during all working activities in the quarries. | Educational and motivational interventions among individuals and groups should be provided to encourage the use of protective eyewear. Furthermore, protective eye devices should be made of polycarbonate lenses in order to provide better eye protection against projectile injuries. |
| Le et al/2011/China (14) | Original | N=87 from January 1st through May 31st, 2010 | Prospective study | Chemical burns lead to permanent vision loss due to complete destruction of the globe surface. It is also reported cornea opacification. | The most injured eyes were due to chemical burns in the workplace | Chemical burns lead to complete destruction to all globe surface tissues. Chemical burns also cause more serious global disorders such as limitation in daily activities and limitation in mobility, than any other ocular injury. | Chemical burn has a significant and extensive impact on patients’ visual function outcomes and vision-related QOL. Chemical burns cause complete globe surface destruction whilst total loss of the eye is rarely reported. | Visual acuity outcomes should be translated into areas of well-being and functioning. That is more meaningful to ophthalmologists, patients and their families. Immediate irrigation after the chemical burn is essential in order to minimize the consequences of the injured eye. |
| lackburn et al/2012/Birmingham (15) | Original | N=77 respondents, N=124 non-respondents from August 2008 through September 2010 | Cohort study | The most common injuries involved corneal foreign bodies (26,7%) and corneal abrasions (23,7%) | The majority of ocular injuries (66%) 724 patients out of 1101 between August 2008 and September 2010, were work related. | Most participants (66.2%) reported that they were more likely to wear eye protective devices after the injury. It was also observed a stronger likelihood to use eye protection when performing a similar task among workers who were using protective devices the time they were injured (87,5%). | This study found that workers are more ready to change safety behaviors by always wearing protective eye equipment and increase its use among some workers. Primary prevention is also essential. Almost one third of workers indicated that their employers had also initiated more strict strategies in wearing protective eye equipment since the injury. It is generally accepted that protective devices is an effective mean to prevent occupational eye injuries, while primary measures in prevention of ocular injuries could minimize the risk of injury. The use of PED is rather low even after the eye injury, and lack of need in using PED is an obstacle in wearing PED. | Health care providers should encourage the use of eye protective devices and educate workers about appropriate equipment given the specific nature of each occupation. Obligatory use of eye protection is a significant preventive factor of ocular trauma. Future research should be conducted to investigate if the eye injured workers could influence coworkers intensive use of protective eye equipment. |
| Le et al/2012/China (16) | Original | N=56 (55 males, 1 female) from 1st January to April 30th 2010 | Retrospective cross-sectional study | Chemical burns | The majority of injured patients (62,5%) were factory workers, and most of the chemical burns occurred at the workplace. | 53 out of 56 patients with chemical burns were cared in the impatient department, with median time of recovery 22 days. | Medical expense was a big economic burden to most patients suffering a chemical burn in East China. Personal and household per capita income of the injured patients decreased more after the eye injury. Both the household and the personal income with the eye injury severity had a close relationship. None of the patients were wearing PED regarding it as a routine procedure despite the fact that they considered it helpful and required. | Employers should be obligated by strict legislation to purchase injury and medical insurance. They should also compel to provide more protective eye equipment to those employees working in high risk professions. In addition, instructions and psychological counseling in the aid and treatment of the victims is essential. The society should give patients more care, support and help. |
| Ghaedi et al/2012/Tehran Iran (17) | Original | N=149/ with eye injuries due to sulfur mustard exposure | Descriptive Cross-sectional study | Chemical warfare injuries | Chemical warfare survivors with ocular complications | Outpatient cares and a positive psychological history of hospitalization were referred in 58.4% of the cases and a negative in 41.6%. | Sulfur mustard induced ocular injury can cause changes and destructive effects on psychological health and life status of victims. | Bearing fewer children and increasing educational level in addition with creation of appropriate jobs may provide a better life to the victims. Reducing mental stress may help victims to improve psychological health status. |
| Luo et al/2012/US (18) | Original | N=43.510/respondents aged 50 years or older from 2005–2007 collected with random-digit dialed telephone surveys from BRESS | Cross-sectional study | Not reported. The study investigated the factors associated with ocular injuries in the workplace. | Work related eye injuries. | Not reported | Education level and annual household income are two socio-economic indicators associated with eye injuries for patients 50 years or older. These population groups of the lowest socioeconomic level are at increased risk of work-related eye injuries. That happens because they are disproportionately exposed in high risk occupations and they do not wear or they use improperly PED. | Specific eye protective policies and interventions in addition with eye safety training and education should be taken into account on the prevention of ocular trauma. Risk for work-related eye injuries should be better understood to contribute to initiate more effective public health policies. An additional research into these influencing factors is also essential. |
| Low et al/2017/Scotland (19) | Original | N=104 with a subgroup of 25 intoxicated patients admitted to hospital during November 2008 to October 2009 | Prospective study | Penetrating eye injuries (n=44) | The common cause of eye trauma within the intoxicated patients was reported assaults in public areas and to no intoxicated patients was due to other reasons at home. | The percentage of mean time of presentation to hospital in more than 24 was 21.3% against 19.1% for those for presentation in less than 24 hours. | The main finding of the study shows that intoxicated patients at the time of injury were at a higher frequency of suffering an eye injury than those who were not intoxicated. The study also found that the frequencies were higher in patients from more deprived areas. The study also found that the higher risk communities to ocular trauma would benefit more from implementation and intervention strategies in preventing ocular injuries. | Additional funding in educational training in deprived areas is needed to highlight the awareness of risk which leads to ocular trauma. Health strategies to prevent health inequalities in prevention and management of ocular trauma are fundamental. |
| Chua et al/2011/USA (20) | Original | N=3.400 (from August 2007 to October 2009) out of 4.497 eligible to participate/RR=75,6% | Population based survey | Trauma was the cause 3.8% (n=15) of the visual loss. Most of the cases of visual disorder were due to corneal scars (80.0%). | A percentage of 42.0% (n=68) of the eye injuries resulted from a blunt object, while most of the ocular injuries occurred in people working in an indoor environment (79.5%, n=128) | Not reported | In Singapore, the majority of ocular injuries and severe ocular trauma has been found to result from work-related events and involve predominantly Indians, but it is unlikely to be related to socioeconomic differences. There is also a relatively low prevalence of ocular trauma in urban adult population. The higher prevalence is observed in men between 40–49 ages and suggests that physical activities are still the main risk factors for eye trauma. | Cigarette smoking was found from this study to be an independent risk factor of ocular trauma, but further studies are needed to be conducted to determine the association between smoking and ocular trauma. |
| Boadi-Kusi et al/2016/South Africa (21) | Original | N=556 (out of 576)/359 males, 197 females/RR=96,5% | Cross-sectional survey | Not reported | The most common cause of ocular injuries among cocoa farmers was the work place during cocoa farming. The injuries were caused by farm tools, dust, airborne soil and particulates, pollen and plant components. | The main type of eye protection among cocoa farmers was reported being goggles (n=24, 70.6%) and the main reason of not using it was due to unavailability (34.4%). | The use of protective eye devices was low among cocoa farmers in Ghana due to unavailability and unaffordability. The use of such devices could reduce the risk factors of eye injuries among cocoa farmers. 82.4% of those who were generally used PED reported that they were not used them at the time of injury because they regarded it as a routine. Another reason was due to unavailability and lack of economic means, lack of training and due to ignorance. | Provision of eye protective devices by the government/employers and the Ghana Cocoa Board could reduce the risk of ocular injuries among cocoa farmers in Ghana. An ocular health educational program and policy initiatives are also needed to minimize the risk of ocular injuries. |
| Zakrzewski et al/2017/Canada (22) | Original | N=169/(156 males, 13 females)/from October 1st 2013–November 30th 2014 | Case-control study | Corneal foreign bodies (33.7%) and corneal abrasions (22.5%) were reported the most common types of eye injuries. | The most common etiologies of work-related injuries were reported chemical exposures (31.4%) and grinding (17.9%). | The majority of the patients (69.1%) required follow up within a median duration of 6 days from initial assessment. | Young males were more affected by occupational eye injuries. It was also found that previous ocular injury was positively influenced the use of PED. A percentage of 33,1% of the participants sustained an eye injury despite the use of protective equipment. In addition, the use of protective eye devices among workers who suffered an occupational eye trauma was poor because it was inappropriate for the specific task and failure to the required standards. | The study suggests that using appropriate protective eye devices in the work place should be encouraged by public policies. Further prospective surveys are required to promote health strategies to prevent occupational eye trauma in Canada. |
| Northey et al/2014/Australia (23) | Original | Retrospective: N=411 (1st May 2001 to 30th April 2012/Prospective: N=117 (2nd May 2012 to 20th July 2012) | Retrospective and Prospective case series study | The most common type of eye injury was corneal foreign body. | Most of the injuries retrospectively and prospectively were work related and the series of eye trauma was grinding (22.1% and 27.4% respectively) | 12 patients (2.9%) were admitted in the Retrospective case series and 8 patients (6.8%) in the Prospective case series. | Young males represented a higher proportion of eye injuries in the workplace. Trades workers and technicians are the most vulnerable category to ocular injuries as they are more involved in angle-grinding activities. Protective eye devices are not used in the workplace and compliance in wearing such devices is rather low and the PED used was inappropriate for the task undertaken. | Risk populations should be identified to initiate interventions in order to reduce ocular trauma in the workplace. Future studies should be conducted with emphasis in management of ocular cases beyond hospitals. |
| Ahmed et al/2013/Egypt (24) | Original | N=237(total number of cases during the year 2011) | Retrospective epidemio-logical and clinical study | During the year 2011 patients presenting with open globe injuries were 88,6% (210 eyes) and 11,3% with close globe injuries. The type of major injury reported was globe ruptures 38.81% (92 eyes) | The most common cause of injury as means between the years 2006–2011 were occurring at work (25.4%) | During afternoon more injuries reported (26.4%) within emergency department visits as means of the last 5 years. | The study aimed at identifying factors involved in ocular trauma. The most affected in ocular trauma were male students in street activities, because they are less likely to be involved at work, sport and homes. They have also relatively violent behavior in Egypt’s streets. | High-risk ocular trauma groups should be a priority in eye health strategies to prevent blindness due to ocular trauma. Prevented studies should be initiated to reduce ocular trauma. All the population should be educated in wearing protective eyewear in the workplace. Workers should also be informed about the sequences of eye injuries. There should be strict legislation so as all violent instruments such as guns to be condemned and to be allowed under certain licensing and authorization. |
| Raymond et al/2010/Victoria, Australia (25) | Original | N=10.500 admissions during a four-year period (2001–2005) | Cross Sectional study | The most common type of eye injury reported was wounds of the eyelid and periocular area (54%) | The most common cause for eye injury for males was by assaults (27%) and for females was at home because of falls (55%) | Patients admitted to hospital with eye injuries due to falls and assaults, are often suffer for multiple injury types apart from an isolated eye wound. An effective preventative strategy to reduce eye injuries is difficult because most of the eye injuries occur due to assaults and at home. | Eye injuries requiring hospital care have increased the last years in Victoria, Australia. It is not clear if this increasing rate of eye injuries is real or it refers to doctor’s increasing trend to admit less severe eye injuries in Victoria’s hospitals. | It is a difficult task for protective measures to be taken due to the fact that most eye injuries occur at home and in streets as a result of assaults. |
| Chang et al/2008/South-Eastern Asia (26) | Original | N=657 between January 2001 to December 2002 | Retrospective study | The most common type of injury was hyphema of the anterior chamber (23.1%) | 48.1% of the ocular trauma cases were work-related | 46.8% of the patients stayed in the hospital from 3 to 5 days. Meanwhile, the mean duration of stay in hospital were 3–5 days for all eye injuries, 7 days of work-related and 5 days for non-work-related eye traumas. | The study found that work-related injuries are a major cause of severe ocular trauma in South-Eastern Asia. The most common type of eye injury was open globe traumas (86%). The use of protective eye devices could not be investigated. Safety regulations had not implemented. It was also found that because of the hot weather in Taiwan, workers do not feel comfortable to wear PED. | Work-related open globe injuries could be preventable in the industrial city of South-Eastern Asia, by the use of protective eye devices. Comparing the cost of treatment, rehabilitation and days off work with the cost of prevention, the latter is significantly lower. |
| Kanoff et al/2010/Massachusetts (27) | Original | N=812 patients between 1999 and 2008 | Retrospective chart review | The most common type of injury reported was penetrating injuries (56.8%) | Most of the injuries were work related and caused by other projectiles (32%) apart from nails, woods, knives, wires or glasses. | 60% of the patients admitted to hospital in less than 6 hours. Only 16.9% of the patients admitted to emergencies in more than 12 hours. | Other ruptured globes have a worst prognosis than open globe injuries investigated in this study. Some patients also suffered from endophthalmitis, and that caused delays in their surgical interventions. The risk of performing the specific task was undertaken, so workers did not wear PED. | Work-related open globe injuries could be preventable by using appropriate eye protection devices. Employers should initiate restrict safety regulations in the use of eye protection devices. |
| Shepherd et al/2006/Australia (28) | Original | N=6625 between January 1998 to December 2004 | Retrospective study | The most common type of injury was foreign bodies (71%) | Most of the eye injuries were work-related. Most of the injuries were caused during grinding activities (31%). | Most of the injured patients were admitted to Emergency Eye Department in less than 30 minutes. | Most of the Emergency Eye Clinic presentations were accounted by construction industry. The higher risk activity was grinding. Working with metal was found to be the occupation at higher risk for ocular injuries. There was not used appropriate PED for such tasks, as it provides only frontal or frontal-side protection and that is unable to prevent the impact of foreign bodies. | Education programs should be a priority of employers with replacement of all damaged and old equipment. Employees should be trained to irrigate their eyes in case of chemical accidents, and should be informed about the necessity of wearing protective eye devices. |
| McCall et al/2009/Texas, USA (29) | Original | N=10.545 between 1994–2003 | Retrospective study | The most common type of injury was foreign bodies (46.7%) | Most of the ocular injuries were work-related. The occupations at higher risk were found to be craft, production and precision (26.2%) | The recovery time of 2.3% of the injured patients was a week or more. | The industries at higher risk of ocular injuries were that of construction, mining and manufacturing. It is estimated that injuries may be higher because information the data used is specific sometimes. | Employers should be informed of what are the most problematic work areas in order to develop certain measures to address them and reduce eye injuries in the future. |
| Ngo et al/2008/Singapore (30) | Original | N=300 patients out of 1460 from March to September 2006 | Retrospective study | The most common type of injury reported was lamellar lacerations 71.3% and superficial corneal foreign bodies | Most of the eye injuries were work-related (20.5%), and 60% of the eye injuries were caused by high-speed machineries used during hacking and grinding works | Most of the patients were diagnosed with lamellar laceration, and the treatment involved the removal of the foreign body. | Industrial eye injuries have increased despite the safety regulations and legislative lows in the workplace. The majority of ocular injuries were caused by high-speed machineries. By using protective eye devices most of the injuries could be preventable. There was found that the racial variation is an important barrier of not wearing protective eyewear, as Indians were found to be at higher risk of sustaining an eye trauma. | By the use of protective eyewear well-fitted and with good visibility, most of the injuries could be preventable. Strict reinforcement on implementation of eye safety programs in workplace would be essential, especially among foreigners. |
| Soliman et al/2008/Egypt (31) | Original | N=147 patients admitted at Kasr El Aini Cairo Hospital from January to June 2000. | Prospective Epidemio-logical study | The most common type of injury was Corneal laceration (53.6%). The majority of the patients suffered from open globe injuries (80.4%). | Most of the injured patients were students (37%). The injuries occurred during day and the most common cause of injury was with sharp instruments (38%). | Most of the injuries happened between 12:00–5:59 PM. The patients delayed their admission to hospital for more than 24 hours (60%). Delay was not due to the distance between the place of injury and the hospital, but because of negligence. | Most of the eye injuries in this survey were on students during the day. That occurs because there is violent behavior in the streets by throwing stones, guns, fist fights. It couldn’t be found a link between increased risk of eye injury and a specific profession. None of the patients sustained an ocular trauma (3.3%) were wearing PED and they were not workers. | People should be educated for the risk of not admitting to hospital after an eye injury. The public should be informed about the consequences of violent behaviors. All violent instruments should be condemned and should be used only after certain licensing. |
| Raymond et al/2009/Victoria, Australia (32) | Original | N=435 patients with eye injuries in 2004 | Retrospective study | The most common type of injury reported was Corneal foreign body (31%) | The most common place of injury reported was at home (47.3%) and during grinding (24.2%). | 26% of the injured patients suffered another eye injury in the past. Two of the total number of patients had already lost their vision due to an eye injury in the past. | Eye injuries occurring at home have increased during 2004 (study period), so it is essential that protective eye measures should be taken. | Most of the eye injuries occurred at home, so the home handyman should be prohibited by legislation. Legislation should only allow to qualified tradesmen to buy tools and machinery, while safety eyewear should be mandatory with the sale of such tools and machineries. |
For the needs of this Table, authentic information was partly provided from the pertinent literature sources after reporting the related reference
References
- 1.Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5:143–169. doi: 10.1076/opep.5.3.143.8364. [DOI] [PubMed] [Google Scholar]
- 2.Almoosa A, Asal A, Atif M, Ayachit S. Occupational Eye Injury: The Neglected Role of Eye Protection. Bahrain Med Bull. 2017;39:82–84. [Google Scholar]
- 3.Dannenberg AL, Parver LM, Brechner RJ, Khoo L. Penetrating eye injuries in the workplace The National Eye Trauma System Registry. Arch Ophthalmol. 1992;110:843–848. doi: 10.1001/archopht.1992.01080180115038. [DOI] [PubMed] [Google Scholar]
- 4.Mela EK, Dvorak GJ, Mantzouranis GA, Giakoumis AP, Blatsios G, Andrikopoulos GK, et al. Ocular trauma in a Greek population: review of 899 cases resulting in hospitalization. Ophthalmic Epidemiol. 2005;12:185–190. doi: 10.1080/09286580590964801. [DOI] [PubMed] [Google Scholar]
- 5.Kuhn F, Morris R, Mester V, Witherspoon CD, Mann L, Maisiak R. Epidemiology and socioeconomics. Ophthalmol Clin North Am. 2002;15:145–151. doi: 10.1016/s0896-1549(02)00005-6. [DOI] [PubMed] [Google Scholar]
- 6.Thompson GJ, Mollan SP. Occupational eye injuries: a continuing problem. Occup Med (Lond) 2009;59:123–125. doi: 10.1093/occmed/kqn168. [DOI] [PubMed] [Google Scholar]
- 7.Yalcin Tök O, Tok L, Eraslan E, Ozkaya D, Ornek F, Bardak Y. Prognostic factors influencing final visual acuity in open globe injuries. J Trauma. 2011;71:1794–1800. doi: 10.1097/TA.0b013e31822b46af. [DOI] [PubMed] [Google Scholar]
- 8.Boadi-Kusi SB, Hansraj R, Kumi-Kyereme A, Mashige K, Awusabo-Asare K, Ocansey S, et al. Ocular health assessment of cocoa farmers in a rural community in Ghana. J Agromedicine. 2014;19:171–180. doi: 10.1080/1059924X.2014.886537. [DOI] [PubMed] [Google Scholar]
- 9.Khokhar S, Agrawal S, Gupta S, Gogia V, Agarwal T. Edidemiology of traumatic lenticular subluxation in India. Int Ophthalmol. 2014;34:197–204. doi: 10.1007/s10792-013-9813-8. [DOI] [PubMed] [Google Scholar]
- 10.Asharlous A, Hashemi H, Yekta A, Ostadimoghaddam H, Gharaee H, Khabazkhoob M. Tear film secretion and stability in welders. Cont Lens Anterior Eye. 2018;41:426–429. doi: 10.1016/j.clae.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Ye C, Wang X, Zhang Y, Ni L, Jiang R, Liu L, et al. Ten-year epidemiology of chemical burns in western Zhejiang Province, China. Burns. 2016;42:668–674. doi: 10.1016/j.burns.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Zarra T, Lambrianidis T. Occupational ocular accidents amongst Greek endodontists: a national questionnaire survey. Int Endod J. 2013;46:710–719. doi: 10.1111/iej.12048. [DOI] [PubMed] [Google Scholar]
- 13.Adams JS, Raju R, Solomon V, Samuel P, Dutta AK, Rose JS, et al. Increasing compliance with protective eyewear to reduce ocular injuries in stone-quarry workers in Tamil Nadu, India: a pragmatic, cluster randomized trial of a single education session versus an enhanced education package delivered over six months. Injury. 2013;44:118–125. doi: 10.1016/j.injury.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Le Q, Chen Y, Wang X, Li Y, Hong J, Xu J. Vision-related quality of life in patients with ocular chemical burns. Invest Ophthalmol Vis Sci. 2011;52:8951–8956. doi: 10.1167/iovs.11-8355. [DOI] [PubMed] [Google Scholar]
- 15.Blackburn JL, Levitan EB, MacLennan PA, Owsley C, McGwin G., Jr Changes in eye protection behavior following an occupational eye injury. Workplace Health Saf. 2012;60:393–400. doi: 10.1177/216507991206000904. [DOI] [PubMed] [Google Scholar]
- 16.Le Q, Chen Y, Wang X, Hong J, Sun X, Xu J. Analysis of medical expenditure and socio-economic status in patients with ocular chemical burns in East China: a retrospective study. BMC Public Health. 2012;12:409. doi: 10.1186/1471-2458-12-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghaedi G, Ghasemi H, Mousavi B, Soroush MR, Rahnama P, Jafari F, et al. Impact of psychological problems in chemical warfare survivors with severe ophthalmologic complication, a cross sectional study. Health Qual Life Outcomes. 2012;10:36. doi: 10.1186/1477-7525-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luo H, Beckles GL, Fang X, Crews JE, Saaddine JB, Zhang X. Socioeconomic status and lifetime risk for workplace eye injury by a us population aged 50 years and over. Ophthalmic Epidemiol. 2012;19:103–110. doi: 10.3109/09286586.2011.639977. [DOI] [PubMed] [Google Scholar]
- 19.Low L, Hodson J, Morris D, Desai P, MacEwen C. Socioeconomic deprivation and serious ocular trauma in Scotland: a national prospective study. Br J Ophthalmol. 2017;101:1395–1398. doi: 10.1136/bjophthalmol-2016-309875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chua D, Wong W, Lamoureux EL, Aung T, Saw SM, Wong TY. The prevalence and risk factors of ocular trauma: the Singapore Indian eye study. Ophthalmic Epidemiol. 2011;18:281–287. doi: 10.3109/09286586.2011.628775. [DOI] [PubMed] [Google Scholar]
- 21.Boadi-Kusi SB, Hansraj R, Mashige KP, Ilechie AA. Factors associated with protective eyewear use among cocoa farmers in Ghana. Inj Prev. 2016;22:365–369. doi: 10.1136/injuryprev-2014-041531. [DOI] [PubMed] [Google Scholar]
- 22.Zakrewski H, Chung H, Sanders E, Hanson C, Ford B. Evaluation of occupational ocular trauma: are we doing enough to promote eye safety in the workplace? Can J Ophthalmol. 2017;52:338–342. doi: 10.1016/j.jcjo.2016.11.034. [DOI] [PubMed] [Google Scholar]
- 23.Northey LC, Bhardwaj G, Curran S, McGirr J. Eye trauma epidemiology in regional Australia. Ophthalmic Epidemiol. 2014;21:237–246. doi: 10.3109/09286586.2014.928825. [DOI] [PubMed] [Google Scholar]
- 24.Ahmed SA, Zaki RG. Forensic analysis of ocular injuries during the 2011 revolution in Egypt. Forensic Sci Int. 2013;233:348–354. doi: 10.1016/j.forsciint.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 25.Raymond S, Jenkins M, Favilla I, Rajeswaran D. Hospital-admitted eye injury in Victoria, Australia. Clin Exp Ophthalmol. 2010;38:566–571. doi: 10.1111/j.1442-9071.2010.02296.x. [DOI] [PubMed] [Google Scholar]
- 26.Chang CH, Chen CL, Ho CK, Lai YH, Hu RC, Yen YL. Hospitalized eye injury in a large industrial city of South-Eastern Asia. Graefes Arch Clin Exp Ophthalmol. 2008;246:223–228. doi: 10.1007/s00417-007-0733-z. [DOI] [PubMed] [Google Scholar]
- 27.Kanoff JM, Turalba AV, Andreoli MT, Andreoli CM. Characteristics and outcomes of work-related open globe injuries. Am J Ophthalmol. 2010;150:265–269.e2. doi: 10.1016/j.ajo.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 28.Shepherd M, Barker R, Scott D, Hocjey R, Spinks D, Pitt R. Occupational Eye Injuries. Queensland Injury Surveillance Unit. 2006 [Google Scholar]
- 29.McCall BP, Horwitz IB, Taylor OA. Occupational eye injury and risk reduction: Kentucky workers’ compensation claim analysis 1994–2003. Inj Prev. 2009;15:176–182. doi: 10.1136/ip.2008.020024. [DOI] [PubMed] [Google Scholar]
- 30.Ngo CS, Leo SW. Industrial accident-related ocular emergencies in a tertiary hospital in Singapore. Singapore Med J. 2008;49:280–285. [PubMed] [Google Scholar]
- 31.Soliman MM, Macky TA. Pattern of ocular trauma in Egypt. Graefes Arch Clin Exp Ophthalmol. 2008;246:205–212. doi: 10.1007/s00417-007-0720-4. [DOI] [PubMed] [Google Scholar]
- 32.Raymond S, Favilla I, Nguyen A, Jenkins M, Mason G. Eye injuries in rural Victoria, Australia. Clin Exp Ophthalmol. 2009;37:698–702. doi: 10.1111/j.1442-9071.2009.02110.x. [DOI] [PubMed] [Google Scholar]
- 33.Hasset PD, Kelleher CC. The epidemiology of occupational penetrating eye injuries in Ireland. Occup Med (Lond) 1994;44:209–211. doi: 10.1093/occmed/44.4.209. [DOI] [PubMed] [Google Scholar]
- 34.Voon LW, See J, Wong TY. The epidemiology of ocular trauma in Singapore: perspective from the emergency service of a large tertiary hospital. Eye (Lond) 2001;15(Pt 1):75–81. doi: 10.1038/eye.2001.18. [DOI] [PubMed] [Google Scholar]
- 35.Qiu HY, Zhang MN, Zhang Y, Jiang CH. The survey of the causes of eye injury of various services in China. Mil Med. 2011;176:1051–1055. doi: 10.7205/milmed-d-10-00472. [DOI] [PubMed] [Google Scholar]
- 36.Megbele Y, Lam KB, Sadhra S. Risks of cataract in Nigerian metal arc welders. Occup Med (Lond) 2012;62:331–336. doi: 10.1093/occmed/kqs034. [DOI] [PubMed] [Google Scholar]
- 37.Ganann R, Ciliska D, Thomas H. Expending systematic reviews: methods and implications of rapid reviews. Implement Sci. 2010;5:56. doi: 10.1186/1748-5908-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]