Abstract
Introduction
International evidence has found large mental health inequities among transgender people and demonstrates that mental health outcomes are associated with enacted stigma experiences and protective factors. This study aimed to examine the extent of associations of enacted stigma experiences specific to transgender people alongside protective factors with mental health of transgender people in Aotearoa/New Zealand.
Methods
The 2018 Counting Ourselves survey was a nationwide community-based study of transgender people (N = 1178, Mage = 29.5) living in Aotearoa/New Zealand. The survey assessed a wide range of gender minority stress experiences and protective factors that comprised primary (support from friends and family) and secondary social ties (neighborhood and transgender community belongingness). We calculated the predicted probabilities that transgender people exhibit very high psychological distress level, non-suicidal self-injury, and suicidal risks with different combinations and exposure profiles of enacted stigma and protective factors.
Results
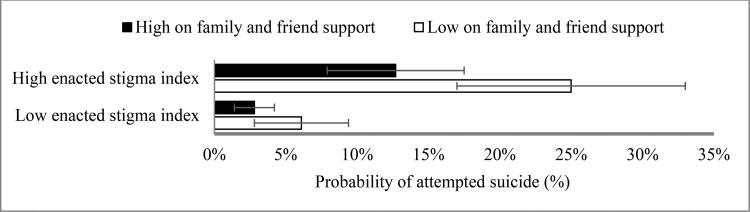
Our findings demonstrated that enacted stigma was associated with negative mental health, and support of friends and family was linked to better outcomes across all mental health measures. Beyond primary social ties, sense of belongingness to neighborhood and transgender communities were linked to reduced odds of psychological distress and suicidal ideation. For those scoring high on enacted stigma and low on protective factors, our model revealed a 25% probability of attempting suicide in the last year compared to 3% for those scoring low on enacted stigma and high on protective factors.
Conclusions
Echoing previous findings, this study demonstrates that transgender people across Aotearoa/New Zealand are less likely to manifest life-threatening mental health outcomes if they experience low levels of enacted stigma and high levels of access to protective factors. Our findings suggest a need to address the enacted stigma that transgender people face across interpersonal and structural settings, and also to enhance social supports that are gender affirmative for this population.
Keywords: Transgender, minority stress, enacted stigma, protective factors, mental health
Introduction
Transgender is an umbrella term that refers to people whose gender identity does not correspond with their sex assigned at birth. This term includes trans men, trans women, and people with non-binary genders, as well as the various gender diverse identities of non-Western cultural backgrounds. For example, in Aotearoa/New Zealand, the transgender population includes indigenous Māori tangata ira tane and whakawahine and people with Pasifika genders such as Samoan fa’afāfine and Tongan fakaleiti (Tan et al., 2019). Not all transgender people seek medical care, such as hormones or surgery to affirm their gender (Schulz, 2018), but all transgender people have a right to the highest standard of gender-affirming care (O’Flaherty & Fisher, 2008; The Yogyakarta Principles, 2007).
Mental health inequities, risk factors, and minority stress
International studies have identified significant health inequities affecting transgender people, with this population consistently found to have an increased prevalence of mental health difficulties, including psychological distress symptoms and suicidality (James et al., 2016; Veale, Watson, et al., 2017; see Valentine & Shipherd (2018) for a review). An example of such studies is the Youth’12 study, a population-based health survey of high school students in Aotearoa/New Zealand, which found a stark contrast in the prevalence of current significant depressive symptoms (41% vs 12%), and non-suicidal self-injury (NSSI; 46% vs 23%) and suicide attempts (20% vs 4%) in the past year among transgender adolescents compared to their cisgender counterparts (Clark et al., 2014).
In recent years, the focus of research on mental health inequities affecting transgender people has shifted from pathologizing models that conceptualize transgender identities as being mentally disordered to the understanding that it is broader social environment that hinder this population from achieving mental health equities (Schulz, 2018; Tan et al., 2019). An increasing number of studies have employed Gender Minority Stress Theory (Meyer, 2003; Tan et al., 2020; Testa et al., 2015) to delineate the processes in which marginalizing social environments lead to adverse mental health outcomes for transgender people. This theory attributes the disproportionate mental health burdens faced by transgender people to the negative consequences of cisgenderism (Tan et al., 2020), which is a prejudice that delegitimizes transgender people (Riggs et al., 2015) and exposes them to a specific form of stress, gender minority stress (Tan et al., 2020; Testa et al., 2015).
Transgender people have been described as one of the most marginalized populations around the world (O’Flaherty & Fisher, 2008), and even in relatively liberal countries like Aotearoa/New Zealand, transgender people report experiencing a multitude of gender minority stress experiences. To date, the legal framework protecting the human rights of transgender people in this country is limited to the Human Rights Act that prohibits discrimination on the grounds of sex (New Zealand Human Rights Commission, 2020). It is unclear if transgender people are provided legal protection from discrimination due to the lack of explicit acknowledgement of gender identity and expression in the Act. A recent review study that collated existing transgender research in Aotearoa/New Zealand proposed that gender minority stress is prevalent in the everyday lives of transgender people at individual (e.g., internalized transphobia), interpersonal (e.g., discrimination, harassment, and violence), and structural levels (e.g., barriers in changing gender marker on legal documents) (Tan et al., 2019).
In this article, we refer to risk factor experiences specific to transgender people as enacted stigma (actual or overt experiences of gender minority stressors). Empirical studies that have examined the association between enacted stigma experiences and mental health found transgender people who had been discriminated against or victimized on the basis of their gender were more likely to manifest symptoms of psychological distress (e.g., Bockting et al., 2013; Wilson et al., 2016). Studies involving transgender youth have also found those who had experienced bullying and abuse at school were more likely to engage in NSSI and suicidality (Peng et al., 2019; Strauss et al., 2020).
Protective factors for transgender people
Previous studies have identified protective factors that may mitigate the negative effects of enacted stigma experiences by promoting individual resilience (Bockting et al., 2013; Puckett et al., 2019), and are associated with higher levels of mental health and wellbeing (Barr et al., 2016; Pflum et al., 2015; Puckett et al., 2019; Veale, Peter, et al., 2017; Weinhardt et al., 2019; Wilson et al., 2016). For instance, positive connections to family members have been shown as a crucial protective factor for transgender people with benefits such as affirmation of transgender people’s identity (Weinhardt et al., 2019) and offsetting the negative mental health impacts of enacted stigma (Veale, Peter, et al., 2017).
Studies have shown that social support at a community level is also important for transgender people. A recent study of transgender people in the United States found that those with high levels of support from family and friends and high levels of connectedness with transgender community had the lowest levels of depression and anxiety symptoms (Puckett et al., 2019). Another United States study found transgender people who lived in neighborhoods that were tolerant of their gender manifested fewer depressive symptoms (Owen-Smith et al., 2017). These findings are congruent with Gender Minority Stress Theory, which proposes that group and community level protective factors can potentially offer important mental health benefits for transgender people through providing opportunities to socialize, tangible resources that enhance personal coping, and platforms that allow community members with similar experiences to validate and reappraise their enacted stigma encounters (Meyer, 2003; Testa et al., 2015).
Objectives and hypotheses
There has been little research identifying the mental health influences of risk and protective factors specific to transgender people either globally or in Aotearoa/New Zealand. This study seeks to examine the associations of enacted stigma and protective factors with the mental health inequities that transgender people in this country face. As well as testing hypotheses of Gender Minority Stress Theory, it is important to understand the extent to which the manifestation of mental health difficulties is related to different risk and protective factors in different parts of the world. While studies have been conducted to examine the negative impacts of enacted stigma on transgender people’s mental health, a recent systematic review found that few of these have focused specifically on gender minority stressors as well as protective factors (Valentine & Shipherd, 2018).
Our study examined the associations of risk (transgender-specific enacted stigma) and protective factors (family and friend support, neighborhood belongingness, and transgender community belongingness), with psychological distress, NSSI, and suicidality in our sample of transgender people in Aotearoa/New Zealand. We hypothesized that enacted stigma experiences will be associated with a greater risk of mental health problems, whereas friend and family support, neighborhood belongingness, and transgender community belongingness will be predictive of a lower occurrence of mental health problems.
Method
Design and consultation
This study used data from Counting Ourselves: the Aotearoa New Zealand Trans and Non-Binary Health Survey, which was open for participation from June to September 2018. The anonymous survey was designed to provide a comprehensive understanding of health of transgender people. It comprised questions related to multiple aspects of health, such as physical and mental health, healthcare access, and experiences of risk and protective factors that could influence health.
General health and mental health questions were taken from Aotearoa/New Zealand population-based health surveys (e.g., the New Zealand Health Survey 2016/17; Ministry of Health, 2017). Questions specific to the lived experiences of transgender people were taken from other transgender studies (e.g., the U.S. Transgender Survey; James et al. (2016)) or developed by the research team. The study structure and content were developed in consultation with a community advisory group of ten transgender people of diverse backgrounds (e.g., ages, ethnic groups, and regions).
The study was advertised on online platforms (e.g., Facebook), billboards in the community, and spread through word of mouth with support from our networks of transgender community organizations, academic researchers, and health professionals working in transgender health. Participants were eligible to take part if they identified as transgender, were at least 14 years of age, and were residing in Aotearoa/New Zealand. Participants were presented with a list of gender options (e.g., trans man, trans woman, and non-binary) and transgender identities were confirmed if their self-identified gender(s) differed from their sex assigned at birth. The study received ethical approval from the New Zealand Health and Disability Ethics Committee (18/NTB/66/AM01).
Participants
There were 1380 initial responses to the survey, but some were removed for being duplicates (n = 22), younger than 14 years old (n = 2), not residing in Aotearoa/New Zealand (n = 12), not responding beyond the survey’s questions on gender identity to indicate that they were transgender (n = 161), or not genuine (e.g., provided illogical responses such as current age was younger than the age of realizing their transgender identity) (n = 5), leaving a final sample of 1178 responses.
Table 1 presents participants’ demographic information. The sample had a mean age of just under 30 years. Our sample consisted of a high proportion of younger and Pākehā (White) participants. Almost half of the participants were non-binary, and there was a similar proportion of trans women and trans men. It is not known whether this is representative of all transgender people in Aotearoa/New Zealand. The demographic make-up of participants in the current study, however, is very similar to survey research with transgender people in the same region (Treharne et al., 2020) and overseas (James et al., 2016; Strauss et al., 2020). More details of the sample demographics and survey method are given in the published report based on the survey dataset (Veale et al., 2019).1
Table 1.
Demographic details of Counting Ourselves participants (n = 1178).
| n (%)/M (SD; range) | |
|---|---|
| Age | 29.54 (13.31; 14–83) |
| Gender groups | |
| Trans men | 324 (27.6) |
| Trans women | 328 (27.9) |
| Non-binary AFAB | 397 (33.8) |
| Non-binary AMAB | 126 (10.7) |
| Race/ethnicity | |
| New Zealand European/Pākehā | 920 (82.4) |
| Māori | 160 (14.3) |
| Samoan | 21 (1.9) |
| Chinese | 17 (1.5) |
| Others | 211 (18.9) |
| Regions | |
| Auckland | 368 (31.9) |
| Wellington | 321 (27.7) |
| Other regions in the North Island | 216 (18.6) |
| Canterbury | 121 (10.4) |
| Other regions in the South Island | 132 (11.4) |
Note. Participants were allowed to select more than one race/ethnicity group and these were reported using the concept of total response (see Ministry of Health, 2017). AFAB = assigned female at birth; AMAB = assigned male at birth.
Measures
All of the measures discussed below had a completion rate of 98% or higher within their respective sections of the survey, indicating the relative acceptability of these questions for our participants.
Enacted stigma
We modeled previous research (Poon et al., 2011; Veale, Peter, et al., 2017) to generate an enacted stigma index that collated a wide range of gender minority stress experiences reported by participants. The index consisted of 11 items and included minority stress events specific to our participants’ transgender identities such as discrimination and unfair treatment at various contexts, as well as cyberbullying (see Table 2). Each item was scored 0 (no or don’t know) or 1 (yes), and the sum of scores for each participant indicated the sum of enacted stigma experiences that they had encountered.
Table 2.
Prevalence of enacted stigma experiences among Counting Ourselves participants in their lifetime.
| n (%) | |
|---|---|
| Experienced discrimination based on gender | 436 (51) |
| Treated unfairly | 254 (33) |
| Verbally harassed | 175 (23) |
| Physically attacked | 23 (3) |
| Cyberbullying through phone or internet | |
| Sent nasty or threatening message | 325 (39) |
| Sent unwanted sexual messages | 240 (30) |
| Rejected by religious communities | 106 (13) |
| Housing experiences | |
| Evicted from home or apartment | 34 (4) |
| Rejected from home or apartment | 61 (7) |
| Homeless because of violence | 32 (4) |
| Prevented from identifying as a transgender person by a health professional | 154 (19) |
| Total (n = 859) | Mean = 2.23; Median = 2; SD = 2.13 |
Note. All items on the enacted stigma index asked specifically about the experience due to them being transgender. ns may vary for each item due to different number of responses.
Mental health
Psychological distress
The Kessler Psychological Distress Scale (K10; Kessler et al., 2003) measured the presence of depression and anxiety symptoms in the past 4 weeks. This scale comprises of 10 items with 5-point response scales from none of the time (0) to all of the time (4). Total scores range from 0 to 40, with a score of 20 or more indicating the presence of very high levels of psychological distress (Ministry of Health, 2017). In the present study, the K10 demonstrated good internal reliability consistency (α = .94).
NSSI and suicidality
These were assessed using questions from the Aotearoa/New Zealand Youth’12 study (Clark et al., 2012). NSSI was measured using a question asking “During the last 12 months, have you deliberately hurt yourself or done anything you knew might have harmed you (but not kill you)?” with response options from not at all to more than 5 times. Suicidal ideation was measured using a question asking “In the last 12 months, have you seriously thought about killing yourself (attempting suicide)?” and suicide attempt was measured using a question asking “In the last 12 months, have you tried to kill yourself (attempted suicide)?”; with three response options: not at all, once or twice, and three or more times.
Protective factors
Friend and family support
This was measured using a single item, “I can always rely on a friend or family or whānau2 member for support if I need it,” with a 5-point response scale from strongly disagree to strongly agree. This item was used as one of the social connectedness indicators in New Zealand Mental Health Survey (Health Promotion Agency, 2016).
Community belongingness
The relationship between sense of belongingness and mental health has been addressed in past research (e.g., Barr et al., 2016; Hagerty et al., 1992; Van Orden et al., 2010). For this study, we were interested in the experiences of transgender people’s involvement within neighborhood and transgender communities that allow them to feel accepted, valued, and to be an integral part of these support systems (Hagerty et al., 1992). Neighborhood belongingness was assessed with a single question from the New Zealand General Social Survey (Statistics New Zealand, 2016), in which participants were asked “On the scale of zero to ten, how would you describe your sense of belonging to neighborhood?”. We also created a separate question with the same wording to identify participants’ sense of belonging to “trans or non-binary community” on the same scale.
Data analysis
IBM SPSS Statistics version 25 was used for descriptive statistics and imputation of missing values. Questions that were later in the survey had a lower number of participants—this was likely to be due to length (over 330 questions). We imputed missingness due to participant attrition, as we had no reason to believe that these missing data were missing not at random; in other words, not related to specific covariates and outcomes that could not be evaluated (Schlomer et al., 2010). Missing values ranged from 0.2% to 1.1% of responses for the K10 scale and from 1.5% to 9.5% of responses for the enacted stigma index. The high percentage of missingness in the index included items that were not applicable to some participants. Missing values were imputed using the expectation maximization method through the estimation of means and covariances of available data in regression models (Schlomer et al., 2010).
To explore the relation of enacted stigma and protective factors on each mental health outcome among our participants, we used STATA’s margins command (MP2 version 16) to carry out probability profiling. This method is used to illustrate the differences in mental health patterns with various combinations of low (10th percentile) and high (90th percentile) levels of gender minority stress-related risk and protective factors. As per the original procedure (Rubenstein et al., 1989), the first step involved conducting bivariate logistic regression models of each of the single risk and protective factors (along with age) predicting each of the binarized mental health variables: very high psychological distress (K10 value of 20 or more) and affirmative responses to NSSI, suicidal ideation, and suicide attempts (see also Poon et al., 2011; Veale, Peter, et al., 2017; Watson et al., 2019 for recent studies employing this method).
Next, we carried forward the risk and protective factors that significantly predicted mental health variables in the bivariate models and entered them into multivariate logistic regression models which included age along with multiple risk and protective factors predicting each mental health variable. Risk and protective factors that were significantly associated with mental health variables in multivariate models were identified, and regression equations which included parameter estimates of these factors were then used to determine probability profiles. The results of these profiles are based on the analysis of all participants, and these can be interpreted as the probability that a transgender person would exhibit a mental health problem based on a specific combination of low and high levels of risk and protective factors.
Results
Table 2 outlines the broad range of gender minority stress experiences that our participants had encountered. While some experiences such as being evicted from home or apartment, and rejected by religious communities for being transgender were only reported by a small minority of participants, a third had been treated unfairly, victimized through on the phone or the internet, and discriminated against for being transgender.
Table 3 presents the prevalence of mental health outcomes and the results of bivariate and multivariate regression models with risk and protective factors predicting very high levels of psychological distress in the past 4 weeks, or at least one instance of NSSI, suicidal ideation, or suicide attempts in the past year. In the bivariate models, enacted stigma experiences were positively associated with all negative mental health outcomes. The enacted stigma index also demonstrated statistically significant associations with mental health in the multivariate models.
Table 3.
Prevalence of mental health outcomes and results of bivariate and multivariate logistic regression models.
| Bivariate model Odds ratio (95% CIs) |
Multivariate model Odds ratio (95% CIs) |
|
|---|---|---|
| K10 (very high psychological distress) past 4 weeks | Very high n = 418; total n = 904 | |
| Enacted stigma index | 1.30 (1.21–1.40)** | 1.26 (1.17–1.37)** |
| Friend and family support | 0.67 (0.58–0.77)** | 0.75 (0.65–0.88)** |
| Neighborhood belongingness | 0.84 (0.79–0.88)** | 0.88 (0.83–0.94)** |
| Trans community belongingness | 0.94 (0.90–0.99)* | 0.99 (0.93–1.04) |
| Age | 0.94 (0.93–0.95)** | 0.94 (0.92–0.95)** |
| Non-suicidal self-injury past year | Yes n = 377; total n = 898 | |
| Enacted stigma index | 1.29 (1.20–1.39)** | 1.25 (1.15–1.35)** |
| Friend and family support | 0.78 (0.68–0.90)** | 0.85 (0.74–0.99)* |
| Neighborhood belongingness | 0.90 (0.85–0.95)** | 0.93 (0.88–0.99)* |
| Trans community belongingness | 0.98 (0.93–1.03) | —a |
| Age | 0.93 (0.92–0.94)** | 0.92 (0.90–0.94)** |
| Suicidal ideation past year | Yes n = 500; total n = 891 | |
| Enacted stigma index | 1.22 (1.14–1.31)** | 1.19 (1.11–1.29)** |
| Friend and family support | 0.71 (0.62–0.82)** | 0.78 (0.67–0.91)** |
| Neighborhood belongingness | 0.89 (0.84–0.94)** | 0.93 (0.88–0.99)* |
| Trans community belongingness | 0.93 (0.88–0.97)** | 0.95 (0.90–1.00) |
| Age | 0.96 (0.95–0.97)** | 0.96 (0.94–0.98)** |
| Suicide attempts past year | Yes n = 95; total n = 866 | |
| Enacted stigma index | 1.41 (1.28–1.55)** | 1.39 (1.25–1.54)** |
| Friend and family support | 0.71 (0.59–0.86)** | 0.76 (0.62–0.92)** |
| Neighborhood belongingness | 0.96 (0.89–1.05) | —a |
| Trans community belongingness | 1.04 (0.96–1.12) | —a |
| Age | 0.95 (0.93–0.97)** | 0.94 (0.92–0.96)** |
Note. A score of 20 or more on the K10 scale denotes very high psychological distress. Bivariate models included single risk or protective factor. Multivariate models included all risk and protective factors.
Excluded from the multivariate analysis as it was a nonsignificant predictor;
p < .05;
p < .01.
As expected, the protective factors were negatively associated with most mental health variables (see Table 3). Friend and family support was significantly related to every mental health variable, so we included this protective factor in all multivariate models. Other protective factors were excluded from multivariate models when they were not significantly associated with the respective mental health variable.
Table 4 displays predicted probability profiles for each mental health outcome. Probability profiles were calculated based on the regression equations for the multivariate models in Table 3. The models predicted that participants with high (90th percentile) enacted stigma and low (10th percentile) family and friend support had the highest probability of manifesting all of the negative mental health outcomes we assessed. Conversely, when participants had low enacted stigma and high levels of protective factors, the probabilities of having these mental health outcomes were lowest. Predicted probabilities for different combinations of levels of risk and protective factors fell between these extremes. Figure 1 provides a graphical representation of these probabilities for suicide attempt.
Table 4.
Predicted probabilities of mental health outcomes by low/high enacted stigma and protective factors.
| Low (10th percentile) enacted stigma index % (95% CIs) | High (90th percentile) enacted stigma index % (95% CIs) | |
|---|---|---|
| K10 (very high psychological distress) | ||
| High on both protective factors | 15.3 (10.3–20.4) | 36.9 (27.1–46.7) |
| Low on family and friend support, high neighborhood belongingness | 29.9 (19.4–40.5) | 58.0 (45.6–70.3) |
| High on family and friend support, low neighborhood belongingness | 33.7 (25.2–42.2) | 62.1 (52.8–71.4) |
| Low on both protective factors | 54.5 (44.1–65.0) | 79.5 (72.8–86.1) |
| Non-suicidal self-injury (yes; no) | ||
| High on both protective factors | 18.1 (12.5–23.7) | 39.8 (30.0–49.6) |
| Low on family and friend support, high neighborhood belongingness | 26.2 (16.5–36.0) | 51.6 (39.1–64.1) |
| High on family and friend support, low neighborhood belongingness | 28.2 (20.4–36.0) | 54.0 (44.3–63.7) |
| Low on both protective factors | 38.7 (29.0–48.5) | 65.4 (56.7–74.1) |
| Suicidal ideation (yes; no) | ||
| High on both protective factors | 32.7 (25.5–39.9) | 53.4 (43.8–63.0) |
| Low on family and friend support, high neighborhood belongingness | 51.4 (40.0–63.1) | 71.4 (61.3–81.4) |
| High on family and friend support, low neighborhood belongingness | 47.3 (38.3–56.2) | 67.9 (59.5–76.4) |
| Low on both protective factors | 66.1 (57.3–75.0) | 82.2 (76.3–88.0) |
| Suicide attempt (yes; no) | ||
| High on family and friend support | 2.8 (1.3–4.2) | 12.7 (7.9–17.5) |
| Low on family and friend support | 6.1 (2.9–9.4) | 25.0 (17.0–33.0) |
Note. Enacted stigma index: Range = 0–11, 10th percentile = 0, 90th percentile = 5. Family and friend support: Range = 1–5, 10th percentile = 2, 90th percentile = 5. Neighborhood belongingness: Range = 0–10, 10th percentile = 0, 90th percentile = 8. Trans community belongingness: Range = 0–10, 10th percentile = 2, 90th percentile = 10.
Figure 1.
Probability profile of Counting Ourselves participants who tried to kill themselves (attempted suicide) during the last 12 months with different combinations of risk and protective factors. Error bars indicate 95% confidence intervals.
Discussion
The present study provides novel insights into both risk and protective factors together and illustrates the extent of these associations on negative mental health outcomes for transgender people using predicted probabilities. Using a large national sample, we found high rates of transgender-specific enacted stigma experiences ranging from discrimination, verbal harassment to cyberbullying, affecting transgender people in Aotearoa/New Zealand. Consistent with findings from existent national community-based studies such as the Transgender Inquiry (Human Rights Commission, 2008), as well as overseas studies such as the United States Transgender Survey (James et al., 2016), our study evinced how transgender people commonly face discrimination and victimization in everyday life, as well as the lack of inclusive legislative frameworks in place to protect transgender people from enacted stigma.
In line with findings of previous studies (Bockting et al., 2013; Liu & Mustanski, 2012; Strauss et al., 2020; Treharne et al., 2020; Veale, Peter, et al., 2017; Wilson et al., 2016), our findings are consistent with Gender Minority Stress Theory (Tan et al., 2020; Testa et al., 2015) that enacted stigma experiences resulting from marginalizing social environments (i.e., cisgenderism) are acting as drivers of mental health inequities. This study showed that the mental health problems affecting transgender people have strong associations with the gender minority stress that they experience. These findings were illustrated by the predicted probabilities of reporting psychological distress symptoms, NSSI risk, suicidal ideation, and suicide attempts which were statistically significantly higher and clinically meaningfully higher for those reporting high levels of enacted stigma compared with those reporting low enacted stigma.
Our bivariate models indicated that higher degrees of friend and family support, neighborhood belongingness, and transgender community belongingness were related to lower odds of reporting mental health problems. These findings were in accordance with other transgender studies that noted support from family and friends was associated with better mental health and lower suicidal risks (Puckett et al., 2019; Veale, Peter, et al., 2017; Wilson et al., 2016). For example, a study in the United States found that parental closeness (e.g., satisfaction with relationships with parents), and parental acceptance of transgender identities, were associated with lower risks for psychological stress and suicidal ideation among transgender youth (Wilson et al., 2016). Benefits of positive relationships with family and friends also extend to aspects of social wellbeing, with studies showing increased resilience to counteract negative effects of enacted stigma (Puckett et al., 2019) and heightened quality of life (Weinhardt et al., 2019) among transgender people who have adequate access to support from family and friends.
The provision of social support for transgender people, however, has mostly been demonstrated around the context of primary social ties (e.g., connections with close friends and family members), and there is a considerably less attention paid to the mental health benefits of secondary social ties (e.g., neighborhood and transgender communities). Existent finding on the importance of neighborhood environments for transgender people has been limited to one study which examined neighborhood tolerance levels of transgender people (Owen-Smith et al., 2017); our study demonstrated a novel positive association between neighborhood belongingness and mental health outcomes among transgender people. Sense of neighborhood belongingness includes the presence of reciprocally caring relationships with those living in close proximity that are essential in reducing social isolation (Van Orden et al., 2010), and previous studies with cisgender people have proposed that neighborhood belongingness is an important predictor of good mental health and wellbeing (Aminzadeh et al., 2013; Aneshensel & Sucoff, 1996). For example, a study of cisgender youth in Aotearoa/New Zealand found those who were living in neighborhoods of high levels social cohesion (characterized by participants’ rating of how much they liked and felt that they belonged to their neighborhood) had better mental health (Aminzadeh et al., 2013). Moreover, our results indicated neighborhood belongingness may provide additional protection for transgender people above primary social ties. Future studies could explore how transgender people develop a sense of community within their neighborhoods and the barriers that hinder them from accessing neighborhood support networks.
Our findings echoed recent studies in the United States which found transgender people with higher degrees of belongingness to transgender communities were less likely to experience mental health difficulties (Barr et al., 2016; Pflum et al., 2015; Puckett et al., 2019). This finding also aligns with Gender Minority Stress Theory which posits that access to social and emotional support from others with similar identities or experiences could buffer the negative influences of enacted stigma (Meyer, 2003; Testa et al., 2015). Particularly, social ties with secondary group members have been proposed as an alternative form of social support that is especially pertinent for those who have been victimized and rejected by their primary members (Thoits, 2011). The relatively weak associations of transgender community belongingness with specific mental health outcomes in our study were also reported in previous studies (Pflum et al., 2015; Puckett et al., 2019), and could be partly explained by our participants’ prime reliance on friends and family members for relevant information and social support. It could also be that many participants had transgender friends and included them when reporting about support from family and friends, meaning that the transgender community belongingness could not add any meaningful prediction above support from family and friends.
While our question on transgender community belongingness did not distinguish between online or in-person connections, a report using the same dataset as the current article found that 74% of participants socialized with other transgender people online (Veale et al., 2019). A study in the United States involving transgender youth found online platforms to be useful in compensating for limitations in accessing offline resources and relationships, especially for those who are “stealth” and do not regularly disclose their transgender history (DeHaan et al., 2013). Although the presence of online-based transgender support groups in Aotearoa/New Zealand facilitates opportunities for transgender people from non-urban regions to connect with each other, many transgender people socialize with each other in other ways, such as friendships, in political activism, and transgender community organizations (Veale et al., 2019). Nonetheless, our findings point to a need to shed light on how online platforms can empower transgender people who had experienced enacted stigma. This empowerment might be achieved by facilitating collective activism to address this stigma, peer support, or through provision of relevant resources.
Strengths and limitations
While a strength of this study is the large sample size, our use of nonprobability sampling means that the generalizability of our results to the wider transgender population in Aotearoa/New Zealand and beyond should be interpreted with caution. Our sample consisted of a high proportion of younger and Pākehā (White) participants. Our survey’s promotion was most successful via internet groups and transgender community organizations; those who were less connected to transgender community would have undoubtedly been more difficult to reach.
The cross-sectional nature of our findings means that causality cannot necessarily be inferred. Nonetheless, we expect that the reported gender minority stress events had temporal precedence over the mental health outcomes (Liu & Mustanski, 2012). Lifetime enacted stigma experiences were likely to have occurred before the development of psychological distress in past month, and NSSI and suicidality in past year among our participants, favoring the conclusion that minority stress is a significant contributor to mental health distress (Meyer, 2003; Testa et al., 2015).
Because we conducted a large survey encompassing a broad range of topics (a total of 330 questions), we needed to use single-item measures for many constructs to reduce participants’ response burden. It was difficult to ascertain the validity of constructs that were measured using only one item (NSSI, suicidality, family support, belongingness). On the other hand, single-item measures similar to these, with good face validity, are widely used in Aotearoa/New Zealand and overseas population-based surveys, and these constructs—especially NSSI, suicidal ideation, and suicide attempts—do not usually require multiple questions to reliably measure the entirety of the construct.
While the use of probability profiling in the current study was valuable for revealing how various combinations of co-occurring risk and protective factors contribute to mental health outcomes, its usage came with limitations. Probability profiling only allowed us to present results pertaining to those outcomes at low (10th) and high (90th) percentiles. Finally, there were likely to be within-group differences (e.g., gender, race/ethnicity, religion, and socioeconomic status) among transgender people that were beyond the scope of the current study. Future research should examine potential differences between subgroups of transgender people who may experience risk and protective factors in different manners, and the associations of these demographic variables with mental health outcomes.
Conclusion and implications
The striking prevalence of enacted stigma experiences reported in this study was consistent with those documented in the research available on transgender people in many countries (e.g., James et al., 2016; Strauss et al., 2020; Veale, Peter, et al., 2017) urging numerous agencies to consider immediate actions to diminish the mental health inequities affecting transgender people in Aotearoa/New Zealand and globally. There is a need for clinicians, practitioners, educators, and researchers who work in the field of transgender health to acknowledge the wider context of sociocultural cisgenderism. This includes deepening their understandings on how the impacts of cisgenderism can create a stressful and harmful environment for transgender people, as well as how cisgenderism is linked to the various forms of enacted stigma (e.g., discrimination and sexual violence) that may give rise to gender minority stress with subsequent negative mental health consequences. Specifically, the present findings suggest efforts to address cisgenderism at interpersonal and structural levels, including awareness education, support for community advocacy, and inclusive policy initiatives may help to reduce transgender people’s exposure to enacted stigma to reduce the risk of these life-threatening mental health problems.
The finding of Youth’12 study, which has reported that transgender students in Aotearoa/New Zealand were less likely to have family members to care about them, is a serious concern (Clark et al., 2014). Our findings highlight the crucial role that primary social ties play in providing transgender people with not just general support that they need. Transgender-specific support could include expressing affirmation of a transgender person’s gender that has been found to be associated with promotion of personal resilience and reduced negative impacts of enacted stigma (Puckett et al., 2019; Weinhardt et al., 2019). In relation to this, comprehensive resources and training for family members about understandings of transgender-specific needs should be made widely available, such as through social media, healthcare providers, and community organizations.
Given the potential role of secondary social ties (including connections to neighborhood and transgender communities) in providing mental health benefits for transgender people, opportunities for fostering positive relationships among transgender people and between trans and wider communities should be expanded by identifying and reducing barriers to neighborhood engagement. Resources should also be provided for the work that transgender community organizations do to allow transgender people to develop a sense of belonging within their communities.
Acknowledgment
The first author would like to acknowledge the financial support received through a University of Waikato Doctoral Scholarship. The authors would like to acknowledge the work of Counting Ourselves research team, and give special thanks to the community advisory group members and to the survey participants.
Funding Statement
This work was supported by the Health Research Council of New Zealand [J.F.V., 17/587], the Rule Foundation; and the University of Waikato.
Notes
Note that these demographic details may differ slightly from the published findings from the same survey dataset (Veale et al., 2019) which were weighted by ethnic groups to match the Aotearoa/New Zealand general population.
The Māori term “whānau” translates as family members, including those from an extended kinship system (Durie, 1985).
Conflict of interest
The authors have no other conflict of interest to declare.
References
- Aminzadeh, K., Denny, S., Utter, J., Milfont, T. L., Ameratunga, S., Teevale, T., & Clark, T. (2013). Neighbourhood social capital and adolescent self-reported wellbeing in New Zealand: A multilevel analysis. Social Science & Medicine (1982), 84, 13–21. 10.1016/j.socscimed.2013.02.012 [DOI] [PubMed] [Google Scholar]
- Aneshensel, C. S., & Sucoff, C. A. (1996). The neighborhood context of adolescent mental health. Journal of Health and Social Behavior, 37(4), 293–310. 10.2307/2137258 [DOI] [PubMed] [Google Scholar]
- Barr, S. M., Budge, S. L., & Adelson, J. L. (2016). Transgender community belongingness as a mediator between strength of transgender identity and well-being. Journal of Counseling Psychology, 63(1), 87–97. 10.1037/cou0000127 [DOI] [PubMed] [Google Scholar]
- Bockting, W., Miner, M., Romine, R., Hamilton, A., & Coleman, E. (2013). Stigma, mental health, and resilience in an online sample of the US transgender population. American Journal of Public Health, 103(5), 943–951. 10.2105/AJPH.2013.301241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, T. C., Fleming, T., Bullen, P. D. S., Crengle, S., Dyson, B., Fortune, S., Lucassen, M., Peiris-John, R., Robinson, E., Rossen, F., Sheridan, J., Teevale, T., & Utter, J. (2012). Youth’12 Overview: The health and wellbeing of New Zealand secondary school students in 2012. The University of Auckland. [Google Scholar]
- Clark, T. C., Lucassen, M. F. G., Bullen, P., Denny, S. J., Fleming, T. M., Robinson, E. M., & Rossen, F. V. (2014). The health and well-being of transgender high school students: Results from the New Zealand Adolescent Health Survey (Youth'12). The Journal of Adolescent Health, 55(1), 93–99. 10.1016/j.jadohealth.2013.11.008 [DOI] [PubMed] [Google Scholar]
- DeHaan, S., Kuper, L. E., Magee, J. C., Bigelow, L., & Mustanski, B. S. (2013). The interplay between online and offline explorations of identity, relationships, and sex: A mixed-methods study with LGBT youth. Journal of Sex Research, 50(5), 421–434. 10.1080/00224499.2012.661489 [DOI] [PubMed] [Google Scholar]
- Durie, M. H. (1985). A Maori perspective of health. Social Science & Medicine, 20(5), 483–486. 10.1016/0277-9536(85)90363-6 [DOI] [PubMed] [Google Scholar]
- Hagerty, B. M. K., Lynch-Sauer, J., Patusky, K. L., Bouwsema, M., & Collier, P. (1992). Sense of belonging: A vital mental health concept. Archives of Psychiatric Nursing, 6(3), 172–177. 10.1016/0883-9417(92)90028-H [DOI] [PubMed] [Google Scholar]
- Health Promotion Agency . (2016). 2016 New Zealand Mental Health Survey questionnaire. Health Promotion Agency. [Google Scholar]
- Human Rights Commission . (2008). To be who I am: Report of the inquiry into discrimination experienced by transgender people. Human Rights Commission. [Google Scholar]
- James, S. E., Herman, J. L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality. [Google Scholar]
- Kessler, R. C., Barker, P. R., Colpe, L. J., Epstein, J. F., Gfroerer, J. C., Hiripi, E., Howes, M. J., Normand, S.-L T., Manderscheid, R. W., Walters, E. E., & Zaslavsky, A. M. &. (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60(2), 184–189. 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- Liu, R. T., & Mustanski, B. (2012). Suicidal ideation and self-harm in lesbian, gay, bisexual, and transgender youth. American Journal of Preventive Medicine, 42(3), 221–228. 10.1016/j.amepre.2011.10.023 [DOI] [PubMed] [Google Scholar]
- Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health. (2017). Methodology report 2016/17: New Zealand Health Survey. Ministry of Health. [Google Scholar]
- New Zealand Human Rights Commission . (2020). Prism: Human rights issues relating to sexual orientation, gender identity and expression, and sex characteristics (SOGIESC) in Aotearoa New Zealand- A report with recommendations. New Zealand Human Rights Commission. [Google Scholar]
- O’Flaherty, M., & Fisher, J. (2008). Sexual orientation, gender identity and international human rights law: Contextualising the Yogyakarta Principles. Human Rights Law Review, 8(2), 207–248. 10.1093/hrlr/ngn009 [DOI] [Google Scholar]
- Owen-Smith, A. A., Sineath, C., Sanchez, T., Dea, R., Giammattei, S., Gillespie, T., Helms, M. F., Hunkeler, E. M., Quinn, V. P., Roblin, D., Slovis, J., Stephenson, R., Sullivan, P. S., Tangpricha, V., Woodyatt, C., & Goodman, M. (2017). Perception of community tolerance and prevalence of depression among transgender persons. Journal of Gay & Lesbian Mental Health, 21(1), 64–76. 10.1080/19359705.2016.1228553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng, K., Zhu, X., Gillespie, A., Wang, Y., Gao, Y., Xin, Y., Qi, J., Ou, J., Zhong, S., Zhao, L., Liu, J., Wang, C., & Chen, R. (2019). Self-reported rates of abuse, neglect, and bullying experienced by transgender and gender-nonbinary adolescents in China. JAMA Network Open, 2(9), e1911058. 10.1001/jamanetworkopen.2019.11058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pflum, S. R., Testa, R. J., Balsam, K. F., Goldblum, P. B., & Bongar, B. (2015). Social support, trans community connectedness, and mental health symptoms among transgender and gender nonconforming adults. Psychology of Sexual Orientation and Gender Diversity, 2(3), 281–286. 10.1037/sgd0000122 [DOI] [Google Scholar]
- Poon, C., Saewyc, E. M., & Chen, W. (2011). Enacted stigma, problem substance use, and protective factors among Asian sexual minority youth in British Columbia. Canadian Journal of Community Mental Health, 30(2), 47–64. 10.7870/cjcmh-2011-0016 [DOI] [Google Scholar]
- Puckett, J. A., Matsuno, E., Dyar, C., Mustanski, B., & Newcomb, M. E. (2019). Mental health and resilience in transgender individuals: What type of support makes a difference? Journal of Family Psychology, 33(8), 954–964. 10.1037/fam0000561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs, D. W., Ansara, G. Y., & Treharne, G. J. (2015). An evidence-based model for understanding the mental health experiences of transgender Australians. Australian Psychologist, 50(1), 32–39. 10.1111/ap.12088 [DOI] [Google Scholar]
- Rubenstein, J. L., Heeren, T., Housman, D., Rubin, C., & Stechler, G. (1989). Suicidal behavior in “normal” adolescents: Risk and protective factors. The American Journal of Orthopsychiatry, 59(1), 59–71. 10.1111/j.1939-0025.1989.tb01635.x [DOI] [PubMed] [Google Scholar]
- Schlomer, G. L., Bauman, S., & Card, N. A. (2010). Best practices for missing data management in counseling psychology. Journal of Counseling Psychology, 57(1), 1–10. 10.1037/a0018082 [DOI] [PubMed] [Google Scholar]
- Schulz, S. L. (2018). The informed consent model of transgender care: An alternative to the diagnosis of gender dysphoria. Journal of Humanistic Psychology, 58(1), 72–92. 10.1177/0022167817745217 [DOI] [Google Scholar]
- Statistics New Zealand . (2016). New Zealand General Social Survey 2016. Statistics New Zealand. [Google Scholar]
- Strauss, P., Cook, A., Winter, S., Watson, V., Wright Toussaint, D., & Lin, A. (2020). Associations between negative life experiences and the mental health of trans and gender diverse young people in Australia: findings from Trans Pathways. Psychological Medicine, 50(5), 808–817. 10.1017/S0033291719000643 [DOI] [PubMed] [Google Scholar]
- Tan, K. K. H., Schmidt, J. M., Ellis, S. J., & Veale, J. F. (2019). Mental health of trans and gender diverse people in Aotearoa/New Zealand: A review of the social determinants of inequities. New Zealand Journal of Psychology, 48(2), 64–72. [Google Scholar]
- Tan, K. K. H., Treharne, G. J., Ellis, S. J., Schmidt, J. M., & Veale, J. F. (2020). Gender minority stress: A critical review. Journal of Homosexuality, 67(10), 1471–1489. 10.1080/00918369.2019.1591789 [DOI] [PubMed] [Google Scholar]
- Testa, R. J., Habarth, J., Peta, J., Balsam, K., & Bockting, W. (2015). Development of the gender minority stress and resilience measure. Psychology of Sexual Orientation and Gender Diversity, 2(1), 65–77. 10.1037/sgd0000081 [DOI] [Google Scholar]
- The Yogyakarta Principles . (2007). Principles on the application of international human rights law in relation to sexual orientation and gender identity. http://yogyakartaprinciples.org/wp-content/uploads/2016/08/principles_en.pdf
- Thoits, P. A. (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145–161. 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- Treharne, G. J., Riggs, D. W., Ellis, S. J., Flett, J. A. M., & Bartholomaeus, C. (2020). Suicidality, self-harm, and their correlates among transgender and cisgender people living in Aotearoa/New Zealand or Australia. International Journal of Transgender Health, In Press. 10.1080/26895269.2020.1795959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine, S. E., & Shipherd, J. C. (2018). A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clinical Psychology Review, 66, 24–38. 10.1016/j.cpr.2018.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden, K. A., Witte, T. K., Cukrowicz, K. C., Braithwaite, S. R., Selby, E. A., & Joiner, T. E. Jr, (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veale, J. F., Byrne, J., Tan, K. K. H., Guy, S., Yee, A., Nopera, T., & Bentham, R. (2019). Counting Ourselves: The health and wellbeing of trans and non-binary people in Aotearoa New Zealand. Transgender Health Research Lab, University of Waikato. [Google Scholar]
- Veale, J. F., Peter, T., Travers, R., & Saewyc, E. M. (2017). Enacted stigma, mental health, and protective factors among transgender youth in Canada. Transgender Health, 2(1), 207–216. 10.1089/trgh.2017.0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veale, J. F., Watson, R. J., Peter, T., & Saewyc, E. M. (2017). Mental health disparities among Canadian transgender youth. The Journal of Adolescent Health, 60(1), 44–49. 10.1016/j.jadohealth.2016.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson, R. J., Veale, J. F., Gordon, A. R., Clark, B. A., & Saewyc, E. M. (2019). Risk and protective factors for transgender youths' substance use. Preventive Medicine Reports, 15, 100905. 10.1016/j.pmedr.2019.100905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt, L. S., Xie, H., Wesp, L. M., Murray, J. R., Apchemengich, I., Kioko, D., Weinhardt, C. B., & Cook-Daniels, L. (2019). The role of family, friend, and significant other support in well-being among transgender and non-binary youth. Journal of GLBT Family Studies, 15(4), 311–325. 10.1080/1550428X.2018.1522606 [DOI] [Google Scholar]
- Wilson, E. C., Chen, Y. H., Arayasirikul, S., Raymond, H. F., & McFarland, W. (2016). The impact of discrimination on the mental health of trans*female youth and the protective effect of parental support. AIDS and Behavior, 20(10), 2203–2211. 10.1007/s10461-016-1409-7 [DOI] [PMC free article] [PubMed] [Google Scholar]