Abstract
Objective
In the context of an ongoing debate on the potential risks of hypoxemia and hyperoxemia, it seems prudent to maintain the partial arterial oxygen pressure (PaO2) in a physiological range during administration of supplemental oxygen. The PaO2 and peripheral oxygen saturation (SpO2) are closely related and both are used to monitor oxygenation status. However, SpO2 values cannot be used as an exact substitute for PaO2. The aim of this study in acutely ill and stable patients was to determine at which SpO2 level PaO2 is more or less certain to be in the physiological range.
Methods
This is an observational study prospectively collecting data pairs of PaO2 and SpO2 values in patients admitted to the emergency room or intensive care unit (Prospective Inpatient Acutely ill cohort; PIA cohort). A second cohort of retrospective data of patients who underwent pulmonary function testing was also included (Retrospective Outpatient Pulmonary cohort; ROP cohort). Arterial hypoxemia was defined as PaO2 < 60 mmHg and hyperoxemia as PaO2 > 125 mmHg. The SpO2 cut-off values with the lowest risk of hypoxemia and hyperoxemia were determined as the 95th percentile of the observed SpO2 values corresponding with the observed hypoxemic and hyperoxemic PaO2 values.
Results
220 data pairs were collected in the PIA cohort. 95% of hypoxemic PaO2 measurements occurred in patients with an SpO2 below 94%, and 95% of hyperoxemic PaO2 measurements occurred in patients with an SpO2 above 96%. Additionally in the 1379 data pairs of the ROP cohort, 95% of hypoxemic PaO2 measurements occurred in patients with an SpO2 below 93%.
Conclusion
The SpO2 level marking an increased risk of arterial hypoxemia is not substantially different in acutely ill versus stable patients. In acutely ill patients receiving supplemental oxygen an SpO2 target of 95% maximizes the likelihood of maintaining PaO2 in the physiological range.
Introduction
The administration of oxygen in acutely ill patients is one of the most frequently used therapeutic interventions, but the optimal target of the partial arterial oxygen pressure (PaO2) and peripheral oxygen saturation (SpO2) remains a topic of ongoing debate [1–3]. Some studies suggest that supra-physiological levels of PaO2, commonly referred to as hyperoxemia, may increase morbidity and mortality in critically ill patients [4–7], whilst for example a study in patients after cardiac arrest showed no negative effects of hyperoxia on mortality [8].The risk of hypoxemia has long been acknowledged, which commonly results in very liberal oxygen administration to acutely ill patients. Recent large randomized controlled trials in mechanically ventilated patients, however, showed no difference in mortality or other clinical outcomes between a mild hypoxemic and normoxemic protocol of oxygen therapy [9–12].
Non-invasive measurement of SpO2 by pulse oximetry is a derivative of arterial oxygen saturation (SaO2) and is used as a rapid and easy way to assess oxygenation. PaO2 on the other hand is the parameter of primary interest, since it reflects the balance between oxygen delivery and consumption [13, 14]. SaO2 and PaO2 are closely related, the nature of which is reflected by the oxyhemoglobin dissociation curve [15]. However SaO2 or SpO2 cannot be interpreted as an exact substitute of PaO2 [16, 17]. Lower hemoglobin levels, acid–base disturbances and altered temperature all influence the correlation between SaO2 and PaO2 [18] and altered cardiac output, peripheral tissue perfusion, sepsis and the use of vasoactive medication disturb the accuracy of SpO2 measurements [19–24]. Also, the measurement of saturation is intrinsically limited in that it cannot detect hyperoxemia if SpO2 is close to or at its maximum value of 100%. Indeed, corresponding PaO2 values for any given SpO2 value may range widely [24–27].
In order to prevent hypoxemia and hyperoxemia and its possible associated risks, the British Thoracic Society Guideline recommends a target SpO2 of 94–98% in adults in healthcare and emergency settings [28]. Others guidelines, however, caution against administering oxygen to obtain an SpO2 above 96% and advocate a lower SpO2 range [29, 30]. A recent pilot study by our group in a small cohort of Intensive Care Unit (ICU) patients determined that the risk of arterial hyperoxemia (> 125 mmHg), was negligible when SpO2 was 96% or lower [31].
In light of the debate on the trade-off between the risks of arterial hypoxemia and hyperoxemia, it is important to increase our understanding of the SpO2–PaO2 relationship, particularly in acutely ill patients receiving oxygen. In this study, we aim to identify a target SpO2 value, with relative safety margins, resulting in a high likelihood of maintaining PaO2 within a physiological range while administering oxygen [32].
Materials and methods
Study design
We performed a prospective observational study collecting simultaneously measured PaO2 and SpO2 values in two different patient cohorts. The study was registered at clinicaltrials.gov (NCT02666937). This cohort consists of acutely ill patients admitted to the Emergency Room (ER) and the ICU and is referred to as the Prospective Inpatient Acutely ill cohort (PIA cohort).
The medical research ethics committee of the Amsterdam University Medical Centers (Amsterdam UMC) approved the study protocol. The patients in the PIA cohort were informed about the use of their data and could object to their data being used through an opt-out procedure. The medical research ethics committee specifically approved the use of opt-out consent for these patients.
We also included a second cohort of patients with simultaneously measured PaO2 and SpO2 values. This was a retrospective dataset of patients undergoing pulmonary function testing. This dataset was used to gain more insight into the lower range of SpO2 and PaO2 values in a larger population. This cohort of patients is referred to as the Retrospective Outpatients Pulmonary cohort (ROP cohort). The medical research ethics committee granted a waiver of consent for the use of this data.
The Prospective Inpatient Acutely Ill cohort (PIA cohort)
For the PIA cohort, data was collected prospectively from December 2015 to August 2017 in mechanically ventilated ICU-patients and acutely ill patients visiting the ER at the Amsterdam UMC. This cohort consisted of a convenience sample, based on the availability of researchers. Adult patients were eligible for inclusion if they required arterial blood gas analysis (ABGA) as part of routine care. Up to 10 data pairs could be collected per patient with a time interval of at least two hours between samples. A data pair is one single measurement of a combined SpO2 and PaO2 value.
Simultaneous with the ABGA the SpO2 was measured with the use of a Nellcor OxiMax DS-100A (Covidien, Mansfield, USA) pulse oximeter. Reliability of the SpO2 curve was assessed and defined as a curve showing complete pulsatile tracing of the beat-to-beat arterial pulse wave on the pulse oximeter. On the ICU, PaO2 was measured using a combined blood gas analyzer and CO-oximeter (ABL825, pH-stat, Radiometer, Copenhagen, Denmark). The samples were analyzed immediately after sampling.
Patients with methemoglobinemia (> 1.5%), carboxyhemoglobinemia (> 1.5%) or known hyperbilirubinemia (> 20 μmol/L) were excluded. Additionally, ICU patients were only included if they had an arterial cannula and required mechanical ventilation, and were excluded when undergoing extracorporeal membrane oxygenation or therapeutic hypothermia. Oxygen was titrated to achieve a stable arterial oxygen saturation of ≥ 92% in the ICU during routine clinical care. ER patients were included upon presentation when they required ABGA. Most ER patients were stabilized with a non-rebreather mask with 15 liter O2/min when at risk for insufficient oxygenation, according to local guidelines.
The Retrospective Outpatient Pulmonary cohort (ROP cohort)
For the ROP cohort, a dataset was used containing adult patients performing a pulmonary function test at the Amsterdam UMC between 1995 and 2014 and at the Northwest Clinics between 2016 and 2017. A researcher accessed the database to obtain the retrospective data in July 2017. All patients having performed a test were screened for eligibility and were included if they had had an ABGA and a simultaneous SpO2 measurement. Per patient between one and four ABGA’s were collected during each pulmonary function test. The pulmonary function test consisted of a cycling protocol without supplemental oxygen. The arterial puncture was performed by a pulmonary function technician in the radial artery. SpO2 was measured with a NONIN Avant 9600 (Nonin Inc., Plymouth, MN) pulse oximeter at the Amsterdam UMC and a NONIN 8000S (Nonin Inc., Plymouth, MN) pulse oximeter at the Northwest Clinics.
Defining hypoxemia and hyperoxemia
The exact cut-offs for hypoxemia and hyperoxemia are relatively arbitrary and not well defined in literature. For example hyperoxemia is defined in a range from > 120 mmHg [33] up to > 300 mmHg [34], although the latter is clearly far above the physiological value when breathing a normal air mixture. In a multinational survey, most ICU-doctors stated they would accept a PaO2 of 60 mmHg or lower in a clinical trial of oxygenation targets [35]. We therefore pragmatically defined hypoxemia as a PaO2 < 60 mmHg [33, 34, 36] and hyperoxemia as a PaO2 > 125 mmHg [31, 37, 38].
Statistical analysis
Data were analyzed using SPSS (version 22, IBM, Armonk, NY, USA) and RStudio (version 3.5.3, R Foundation for Statistical Computing, Vienna, Austria). Values are presented as mean with standard deviation (SD) unless otherwise stated.
SpO2 and PaO2 data were first visually assessed with a scatterplot. We determined a hypoxemic and hyperoxemic SpO2 limit for the PIA cohort. The hypoxemic SpO2 limit was determined as the 95th percentile of the observed SpO2 values corresponding with the observed hypoxemic PaO2. The hyperoxemic SpO2 limit was determined as the 5th percentile of the observed SpO2 values corresponding with the hyperoxemic PaO2 values. For the ROP cohort we only defined a hypoxemic SpO2 limit, since the patients did not receive supplementary oxygen.
Since multiple measurements were available for most patients, we constructed a mixed linear model in both cohorts. This included a random effect for each patient. First SpO2 and PaO2 values were transformed such that relation between the SpO2 and PaO2 became linear (ln(1—SpO2/100) and ln(PaO2)). The transformed SpO2 was the dependent variable and the transformed PaO2 was included as a covariate with fixed effect. A two-sided 95% prediction interval was constructed for each specific value of PaO2. The upper and lower limit of the prediction interval and the predicted mean value for SpO2 were then transformed back to the original scale.
Results
Included patients and data pairs characteristics
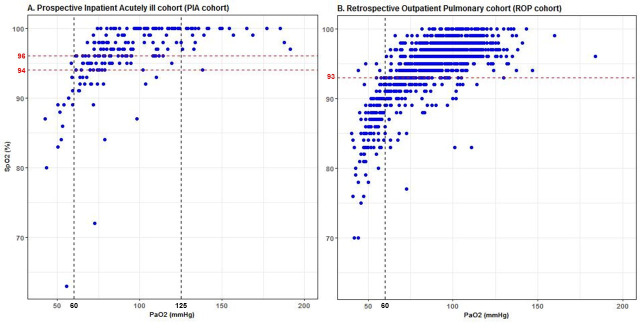
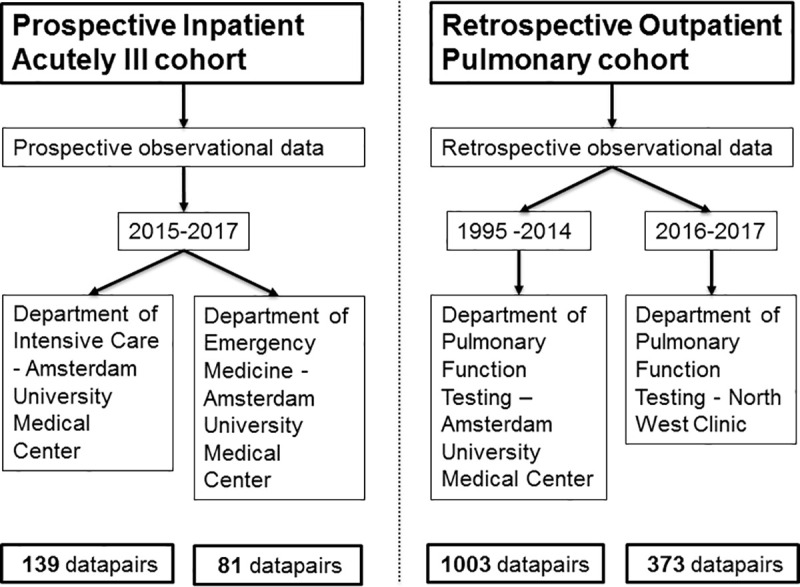
We screened 152 patients in the PIA cohort for eligibility. One patient was excluded because of hyperbilirubinemia and five were excluded because of unreliable SpO2 curves, resulting in the inclusion of 220 data pairs in 146 patients. 139 data pairs were collected at the ICU and 81 at the ER. We screened 693 patients in the retrospective database for eligibility in the ROP cohort. Thirteen patients were excluded because of no or unreliable SpO2 measurements, resulting in the inclusion of 1379 data pairs in 680 patients. 1003 data pairs were collected at the Amsterdam UMC, and 376 pairs at the North West Clinic. Fig 1 shows a visual representation of the different cohorts.
Fig 1. Visual representation of the included cohorts.
Demographics of the included patients and characteristics of the collected data pairs are shown in Table 1. In the PIA cohort, 6.4% of the data pairs had a hypoxemic PaO2 < 60 mmHg, and 20.5% had a PaO2 > 125 mmHg. In the ROP cohort 10.7% of the data pairs had a PaO2 value < 60 mmHg.
Table 1. Demographics of included patients and data pairs characteristics.
| Prospective Inpatient Acutely Ill (PIA) cohort | Retrospective Outpatient Pulmonary (ROP) cohort | |||||
|---|---|---|---|---|---|---|
| Demographics patients | N = 146 | N = 680 | ||||
| Age in years | 63 | (17) | 58 | (15) | ||
| Male | 96 | 66% | 362 | 53% | ||
| Intensive Care Unit Amsterdam UMC | 68 | 47% | - | |||
| Emergency Room Amsterdam UMC | 78 | 53% | - | |||
| Pulmonary function department NWC | - | 68 | 47% | |||
| Pulmonary function department Amsterdam UMC | - | 78 | 53% | |||
| Collected data pairs | N = | N = | ||||
| SpO2 (%) | 96.6 | (4.6) | 220 | 94.7 | (4.4) | 1379 |
| SaO2 (%) | 96.1 | (4.5) | 212 | 95.4 | (5.5) | 1357 |
| PaO2 (mmHg) | 110.9 | (64.6) | 220 | 88.6 | (20.6) | 1379 |
| PaO2 < 60 mmHg | 14 | 6.4% | 220 | 148 | 10.7% | 1379 |
| PaO2 > 125 mmHg | 45 | 20.5% | 220 | 31 | 2.2% | 1379 |
| PaCO2 (mmHg) | 43.6 | (13.2) | 220 | 36.8 | (6.1) | 1377 |
| pH | 7.36 | (0.13) | 218 | 7.37 | (0.06) | 1378 |
| Arterial Bicarbonate (mmol/l) | 24.1 | (5.3) | 216 | 21.7 | (3.8) | 1359 |
| Arterial Lactate (mmol/l) | 2.37 | (2.9) | 210 | |||
| Hemoglobin (mmol/l) | 6.9 | (1.4) | 183 | |||
| Systolic blood pressure (mmHg) | 127 | (28) | 214 | 179 | (38) | 1043 |
| Diastolic blood pressure (mmHg) | 68 | (17) | 214 | 88 | (16) | 1041 |
| Supplemental oxygen (%) | 191 | 87% | 219 | 0 | 0% | 1379 |
Data are presented as a mean (standard deviation) or number with % of total.
Amsterdam UMC, Amsterdam University Medical Center; N, number of patients; NWC, North West Clinic; PaCO2, partial arterial carbon dioxide pressure; PaO2, partial arterial oxygen pressure; SaO2, peripheral oxygen saturation; SpO2, peripheral oxygen saturation
Relationship between SpO2 and PaO2
Fig 2 shows the scatterplots of the data pairs of PaO2 and SpO2 measurements for both cohorts. In the PIA cohort 95% of data pairs corresponding to hypoxemia had SpO2 values below 94%, and 95% of data pairs corresponding to hyperoxemia had SpO2 values exceeding 96%. The horizontal red dotted lines in Fig 2 reflect the hypoxemic and hyperoxemic SpO2 limits. The patients in the ROP cohort have more hypoxemic PaO2 values and did not receive supplemental oxygen. In the ROP cohort, 95% of data pairs corresponding to a hypoxemic PaO2 had SpO2 values below 93%.
Fig 2. Scatterplots of the data pairs of the Prospective Inpatient Acutely ill cohorts and Retrospective Outpatient Pulmonary cohort.
A. Prospective Inpatient Acutely ill cohort (PIA cohort) and B. Retrospective Outpatient Pulmonary cohort (ROP cohort). The black dashed vertical lines reflect the PaO2 values of 60 mmHg and 125 mmHg. The red dashed vertical lines reflect the calculated lower and upper bounds to avoid hypoxemic and hyperoxemic PaO2 measurements.
A multilevel analysis was performed for each cohort, taking into account that multiple measurements could be included per patients (see Fig 3). The curve of the PIA cohort runs slightly left of the ROP curve. There are more measurements with a PaO2 >125 mmHg in the PIA cohort and more measurements with a PaO2 < 60 mmHg in the ROP cohort
Fig 3. Multilevel analysis of the Prospective Inpatient Acutely ill and Retrospective Outpatient Pulmonary cohort.
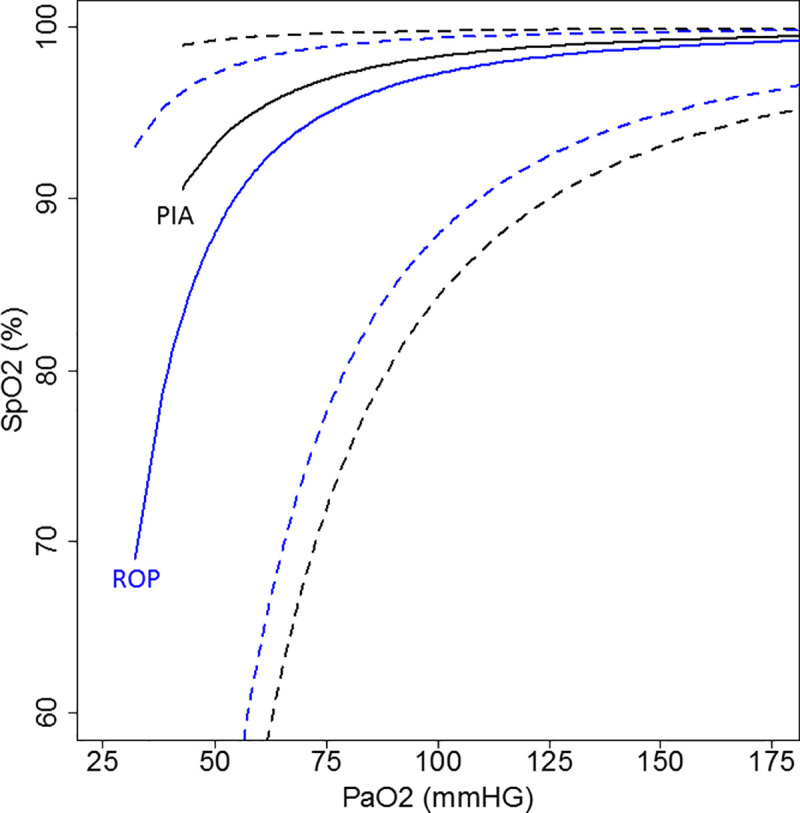
PIA, Prospective Inpatient Acutely ill cohort. ROP, Retrospective Outpatient Pulmonary cohort. The black curve represents the Prospective Inpatient Acutely Ill cohort with a 95% prediction interval (black dashed line). The blue curve represents the Retrospective Outpatient Pulmonary cohort with a 95% prediction interval (blue dashed line).
Fig 4 shows the number of PaO2 measurements within a certain PaO2 range for each SpO2 level in both cohorts. In the PIA cohort at an SpO2 value of 95%, 94,4% of the data pairs had a PaO2 value between 60 and 125 mmHg. For an SpO2 value of 96% and 98%, the corresponding rates of hyperoxemic values were 3.8% and 17.4%, respectively. In the ROP cohort at an SpO2 value of 93%, 4% of the data pairs had a hypoxemic PaO2 value. For an SpO2 value of 92%, the corresponding rate was 11.5%.
Fig 4. Stacked bar plots of the number and percentage of PaO2 values at every SpO2 value.
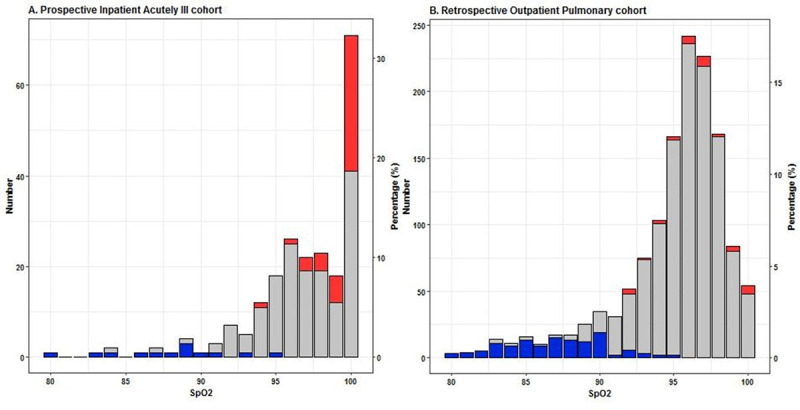
A. Prospective Inpatient Acutely ill cohort (PIA cohort) and B. Retrospective Outpatient Pulmonary cohort (ROP cohort). The left y-axis represents the number of data points and the right y-axis represents the percentage of data points per SpO2 value of the total number of measurements in the whole cohort. PaO2 values are divided into three groups: < 60 mmHg (blue), 60–125 mmHg (gray) and > 125 mmHg (red).
Discussion
In the PIA cohort with SpO2 values of 94–96% both hypoxemia and hyperoxemia can be effectively excluded. In the ROP cohort hypoxemia can be excluded with a lower SpO2 target of 93%. The lower PIA and ROP targets excluding hypoxemia are not substantially different. Combining these cut-offs, we recommend an SpO2 target of 95%, which clearly has margins of relative safety. This target SpO2 results in the highest likelihood of physiological PaO2 values for the average patient.
Our findings are supported by data from an uncontrolled study, aiming at a target SpO2 range between 92–95% that indeed resulted in a significant decrease of the number of hyperoxemic episodes, while hypoxemic episodes remained unchanged [39]. Moreover, an observational study in mechanically ventilated ICU patients by our group also suggested a safe upper SpO2 level excluding hyperoxia of 96% [31]. As for safety in terms of clinical outcomes, a recent systematic review of randomised studies in acutely ill patients showed that, in a variety of acute clinical conditions, mortality increased in patients with an SpO2 levels above 96% [29]. The British Thoracic Society Guideline (2017) recommends more liberal use of oxygen and an upper limit for SpO2 of 98% for acutely ill patients [28]. Our data suggest that this recommended SpO2 target of 98% may result in more hyperoxemia, without being associated with a meaningful lower risk of hypoxemia.
In the ROP cohort an SpO2 value below 93% results in a higher risk of hypoxemia, for the PIA cohort this is the case below 94%. The lower limits are quite similar in these different cohorts of acutely ill and stable patients. These lower safe limits are in line with recent clinical guidelines recommending a lower SpO2 limit of 92–94% [28, 29]. Aiming for even lower SpO2 values increases the risk for hypoxemia.
This observational study has some limitations. Different oximeters were used for the two cohorts and potential differences between measurements can depend on the oximeter used. The Nellcor oximeters, used in the PIA cohort, slightly overestimate SaO2 [40, 41], while Nonin oximeters, used in the ROP cohort, might underestimate SaO2 [41]. Since the lower limit in the PIA cohort was possibly overestimated and the lower limit in the ROP cohort was possibly underestimated, the lower limit for the two cohorts are probably the same. This strengthens the assumption that the hypoxemic safe margin of SpO2 is not heavily influenced by specific pulmonary morbidity.
It is important to note, that there is no clear definition of hypoxemia and hyperoxemia available. We therefore pragmatically defined hypoxemia in line with literature and clinical practice as PaO2 < 60 mmHg [33, 34, 36] and hyperoxemia as PaO2 > 125 mmHg [31, 37, 38]. Different definitions would have resulted in different outcomes of this study. It should be noted that the potential risks of hyperoxemia remain unclear. Some studies do [4–7] and some studies do not [8] show an effect of hyperoxemia on mortality. However in view of the controversy on the definitions and clinical hazards of hypoxemia and hyperoxemia, it seems prudent to maintain PaO2 in a physiological range, defined as between 60 and 125 mmHg [32].
The PIA cohort consisted of a convenience sample. The patient profiles in the PIA cohort varied, with mechanically ventilated patients at the ICU and patients requiring blood gas analysis at the ER. In both cohorts, the number of patients with hypoxemia was relatively small, because of oxygen administration. The ROP cohort consisted of retrospective data of patients performing a pulmonary function test with a cycling protocol. There are very few alternatives to the ROP cohort to obtain more insight in hypoxemic PaO2 values, since stable patients without pulmonary pathology will hardly ever be hypoxemic. Thus, this limitation is intrinsic to the study question of whether the safe SpO2 margin is different in acutely ill versus stable patients.
This study did not explore the clinical variables potentially modifying the relation between PaO2 and SaO2 or the accuracy of SpO2 measurements, so we cannot provide separate recommendations about specific conditions, such as sepsis, hypotension, heart failure, or acute respiratory failure. The generalizability of the results of this study should be confirmed with sufficiently powered studies in patients with specific conditions with different oximeters to define how clinical variables might change SpO2 targets. Also the different definitions of hypoxemia and hyperoxemia and clinical outcome variables should be taken into account in future studies.
In conclusion, we recommend an SpO2-target of 95%, or as close to this level as possible, to avoid the occurrence of either hypoxemia or hyperoxemia in acutely ill patients receiving supplementary oxygen.
Supporting information
(XLSX)
Acknowledgments
The authors would like to thank dr. ir. Peter M. van der Ven for the help with the statistical analyses.
Abbreviations
- ABGA
Arterial blood gas analysis
- Amsterdam UMC
Amsterdam University Medical Centres
- ER
Emergency Room
- ICU
Intensive Care Unit
- NWC
Northwest Clinics
- PaCO2
Partial arterial carbon dioxide pressure
- PaO2
Partial arterial oxygen pressure
- PFD
Pulmonary function department
- PIA cohort
Prospective Inpatient Acutely Ill cohort
- ROP cohort
Retrospective Outpatient Pulmonary cohort
- SaO2
Arterial oxygen saturation
- SBP
Systolic blood pressure
- SD
Standard deviation
- SpO2
Peripheral oxygen saturation
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Damiani E, Adrario E, Girardis M, Romano R, Pelaia P, Singer M, et al. Arterial hyperoxia and mortality in critically ill patients: a systematic review and meta-analysis. Critical care (London, England). 2014;18(6):711. 10.1186/s13054-014-0711-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cornet AD, Kooter AJ, Peters MJ, Smulders YM. Supplemental oxygen therapy in medical emergencies: more harm than benefit? Archives of internal medicine. 2012;172(3):289–90. 10.1001/archinternmed.2011.624 [DOI] [PubMed] [Google Scholar]
- 3.Wetterslev J, Meyhoff CS, Jørgensen LN, Gluud C, Lindschou J, Rasmussen LS. The effects of high perioperative inspiratory oxygen fraction for adult surgical patients. The Cochrane database of systematic reviews. 2015;2015(6):1465–858. 10.1002/14651858.CD008884.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chu DK, Kim LH, Young PJ, Zamiri N, Almenawer SA, Jaeschke R, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet (London, England). 2018;391(10131):1693–705. 10.1016/S0140-6736(18)30479-3 [DOI] [PubMed] [Google Scholar]
- 5.Girardis M, Busani S, Damiani E, Donati A, Rinaldi L, Marudi A, et al. Effect of Conservative vs Conventional Oxygen Therapy on Mortality Among Patients in an Intensive Care Unit: The Oxygen-ICU Randomized Clinical Trial. Jama. 2016;316(15):1583–9. 10.1001/jama.2016.11993 [DOI] [PubMed] [Google Scholar]
- 6.Rincon F, Kang J, Maltenfort M, Vibbert M, Urtecho J, Athar MK, et al. Association between hyperoxia and mortality after stroke: a multicenter cohort study. Critical care medicine. 2014;42(2):387–96. 10.1097/CCM.0b013e3182a27732 [DOI] [PubMed] [Google Scholar]
- 7.de Jonge E, Peelen L, Keijzers PJ, Joore H, de Lange D, van der Voort PH, et al. Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Critical care (London, England). 2008;12(6):R156. 10.1186/cc7150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jakkula P, Reinikainen M, Hästbacka J, Loisa P, Tiainen M, Pettilä V, et al. Targeting two different levels of both arterial carbon dioxide and arterial oxygen after cardiac arrest and resuscitation: a randomised pilot trial. Intensive Care Med. 2018;44(12):2112–21. Epub 2018/11/16. 10.1007/s00134-018-5453-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barrot L, Asfar P, Mauny F, Winiszewski H, Montini F, Badie J, et al. Liberal or Conservative Oxygen Therapy for Acute Respiratory Distress Syndrome. The New England journal of medicine. 2020;382(11):999–1008. 10.1056/NEJMoa1916431 [DOI] [PubMed] [Google Scholar]
- 10.Mackle D, Bellomo R, Bailey M, Beasley R, Deane A, Eastwood G, et al. Conservative Oxygen Therapy during Mechanical Ventilation in the ICU. The New England journal of medicine. 2020;382(11):989–98. 10.1056/NEJMoa1903297 [DOI] [PubMed] [Google Scholar]
- 11.Schjørring OL, Klitgaard TL, Perner A, Wetterslev J, Lange T, Siegemund M, et al. Lower or Higher Oxygenation Targets for Acute Hypoxemic Respiratory Failure. The New England journal of medicine. 2021. Epub 2021/01/21. 10.1056/NEJMoa2032510 . [DOI] [PubMed] [Google Scholar]
- 12.Panwar R, Hardie M, Bellomo R, Barrot L, Eastwood GM, Young PJ, et al. Conservative versus Liberal Oxygenation Targets for Mechanically Ventilated Patients. A Pilot Multicenter Randomized Controlled Trial. American journal of respiratory and critical care medicine. 2016;193(1):43–51. Epub 2015/09/04. 10.1164/rccm.201505-1019OC . [DOI] [PubMed] [Google Scholar]
- 13.Carreau A, El Hafny-Rahbi B, Matejuk A, Grillon C, Kieda C. Why is the partial oxygen pressure of human tissues a crucial parameter? Small molecules and hypoxia. J Cell Mol Med. 2011;15(6):1239–53. 10.1111/j.1582-4934.2011.01258.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rogers K, McCutcheon K. Four Steps to Interpreting Arterial Blood Gases. Journal of Perioperative Practice. 2015;25(3):46–52. 10.1177/175045891502500304 [DOI] [PubMed] [Google Scholar]
- 15.Jubran A. Pulse oximetry. Critical care (London, England). 2015;19(1):272. 10.1186/s13054-015-0984-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Madan A. Correlation between the levels of SpO(2)and PaO(2). Lung India: official organ of Indian Chest Society. 2017;34(3):307–8. 10.4103/lungindia.lungindia_106_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dunn J-O, Mythen M, Grocott MPW. Physiology of oxygen transport. BJA Education. 2016;16:341–8. [Google Scholar]
- 18.Larkin BG, Zimmanck RJ. Interpreting Arterial Blood Gases Successfully. AORN Journal. 2015;102(4):343–57. 10.1016/j.aorn.2015.08.002 [DOI] [PubMed] [Google Scholar]
- 19.Collins J-A, Rudenski A, Gibson J, Howard L, O’Driscoll R. Relating oxygen partial pressure, saturation and content: the haemoglobin-oxygen dissociation curve. Breathe (Sheff). 2015;11(3):194–201. 10.1183/20734735.001415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibáñez J, Velasco J, Raurich JM. The accuracy of the biox 3700 pulse oximeter in patients receiving vasoactive therapy. Intensive Care Med. 1991;17(8):484–6. 10.1007/BF01690773 [DOI] [PubMed] [Google Scholar]
- 21.Jensen LA, Onyskiw JE, Prasad NG. Meta-analysis of arterial oxygen saturation monitoring by pulse oximetry in adults. Heart & lung: the journal of critical care. 1998;27(6):387–408. 10.1016/s0147-9563(98)90086-3 [DOI] [PubMed] [Google Scholar]
- 22.Wilson BJ, Cowan HJ, Lord JA, Zuege DJ, Zygun DA. The accuracy of pulse oximetry in emergency department patients with severe sepsis and septic shock: a retrospective cohort study. BMC emergency medicine. 2010;10:9. Epub 2010/05/07. 10.1186/1471-227X-10-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thijssen M, Janssen L, le Noble J, Foudraine N. Facing SpO2 and SaO2 discrepancies in ICU patients: is the perfusion index helpful? Journal of clinical monitoring and computing. 2019. 10.1007/s10877-019-00371-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farrell KS, Hopper K, Cagle LA, Epstein SE. Evaluation of pulse oximetry as a surrogate for PaO2 in awake dogs breathing room air and anesthetized dogs on mechanical ventilation. Journal of veterinary emergency and critical care (San Antonio, Tex: 2001). 2019. 10.1111/vec.12898 [DOI] [PubMed] [Google Scholar]
- 25.Eytan D, Mazwi ML, Goodwin AJ, Goodfellow SD, Assadi A, Greer RW, et al. Revisiting oxygen dissociation curves and bedside measured arterial saturation in critically ill children. Intensive Care Med. 2019. 10.1007/s00134-019-05792-x [DOI] [PubMed] [Google Scholar]
- 26.Morgan TJ. The oxyhaemoglobin dissociation curve in critical illness. Critical care and resuscitation: journal of the Australasian Academy of Critical Care Medicine. 1999;1(1):93–100. . [PubMed] [Google Scholar]
- 27.Louw A, Cracco C, Cerf C, Harf A, Duvaldestin P, Lemaire F, et al. Accuracy of pulse oximetry in the intensive care unit. Intensive Care Med. 2001;27(10):1606–13. 10.1007/s001340101064 [DOI] [PubMed] [Google Scholar]
- 28.O’Driscoll BR, Howard LS, Earis J, Mak V. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax. 2017;72(Suppl 1):ii1–ii90. 10.1136/thoraxjnl-2016-209729 [DOI] [PubMed] [Google Scholar]
- 29.Siemieniuk RAC, Chu DK, Kim LH, Güell-Rous MR, Alhazzani W, Soccal PM, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ (Clinical research ed). 2018;363:k4169. 10.1136/bmj.k4169 [DOI] [PubMed] [Google Scholar]
- 30.Beasley R, Chien J, Douglas J, Eastlake L, Farah C, King G, et al. Target oxygen saturation range: 92–96% Versus 94–98%. Respirology. 2017;22(1):200–2. 10.1111/resp.12879 [DOI] [PubMed] [Google Scholar]
- 31.Durlinger EMJ, Spoelstra-de Man AME, Smit B, de Grooth HJ, Girbes ARJ, Oudemans-van Straaten HM, et al. Hyperoxia: At what level of SpO(2) is a patient safe? A study in mechanically ventilated ICU patients. Journal of critical care. 2017;39:199–204. 10.1016/j.jcrc.2017.02.031 [DOI] [PubMed] [Google Scholar]
- 32.Robba C, Ball L, Pelosi P. Between hypoxia or hyperoxia: not perfect but more physiologic. J Thorac Dis. 2018;10(Suppl 17):S2052–S4. 10.21037/jtd.2018.05.129 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Page D, Ablordeppey E, Wessman BT, Mohr NM, Trzeciak S, Kollef MH, et al. Emergency department hyperoxia is associated with increased mortality in mechanically ventilated patients: a cohort study. Critical care (London, England). 2018;22(1):9–. 10.1186/s13054-017-1926-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rincon F, Kang J, Vibbert M, Urtecho J, Athar MK, Jallo J. Significance of arterial hyperoxia and relationship with case fatality in traumatic brain injury: a multicentre cohort study. Journal of Neurology, Neurosurgery & Psychiatry. 2014;85(7):799–805. 10.1136/jnnp-2013-305505 [DOI] [PubMed] [Google Scholar]
- 35.Schjørring OL, Toft-Petersen AP, Kusk KH, Mouncey P, Sørensen EE, Berezowicz P, et al. Intensive care doctors’ preferences for arterial oxygen tension levels in mechanically ventilated patients. Acta anaesthesiologica Scandinavica. 2018;62(10):1443–51. Epub 2018/06/22. 10.1111/aas.13171 . [DOI] [PubMed] [Google Scholar]
- 36.Considine J. The reliability of clinical indicators of oxygenation: a literature review. Contemporary nurse. 2005;18(3):258–67. 10.5172/conu.18.3.258 [DOI] [PubMed] [Google Scholar]
- 37.Hafner S, Beloncle F, Koch A, Radermacher P, Asfar P. Hyperoxia in intensive care, emergency, and peri-operative medicine: Dr. Jekyll or Mr. Hyde? A 2015 update. Ann Intensive Care. 2015;5(1):42–. Epub 2015/11/19. 10.1186/s13613-015-0084-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Graaff AE, Dongelmans DA, Binnekade JM, de Jonge E. Clinicians’ response to hyperoxia in ventilated patients in a Dutch ICU depends on the level of FiO2. Intensive Care Med. 2011;37(1):46–51. Epub 2010/09/28. 10.1007/s00134-010-2025-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Helmerhorst HJ, Schultz MJ, van der Voort PH, Bosman RJ, Juffermans NP, de Wilde RB, et al. Effectiveness and Clinical Outcomes of a Two-Step Implementation of Conservative Oxygenation Targets in Critically Ill Patients: A Before and After Trial. Critical care medicine. 2016;44(3):554–63. 10.1097/CCM.0000000000001461 [DOI] [PubMed] [Google Scholar]
- 40.Bickler PE, Feiner JR, Severinghaus JW. Effects of skin pigmentation on pulse oximeter accuracy at low saturation. Anesthesiology. 2005;102(4):715–9. Epub 2005/03/26. 10.1097/00000542-200504000-00004 . [DOI] [PubMed] [Google Scholar]
- 41.Feiner JR, Severinghaus JW, Bickler PE. Dark skin decreases the accuracy of pulse oximeters at low oxygen saturation: the effects of oximeter probe type and gender. Anesthesia and analgesia. 2007;105(6 Suppl):S18–23, tables of contents. Epub 2007/12/06. 10.1213/01.ane.0000285988.35174.d9 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.