Abstract
Objective
This study aimed to investigate association between conspiracy beliefs, trusts in media and authoritative information sources, with COVID-19 vaccine acceptance.
Methods
We conducted online survey on adult resident of Bali Province, Indonesia in September 14th to October 31st 2020 collecting data on demographics, impacts of the pandemic, conspiracy beliefs, trusts in conventional media and authoritative sources, as well as vaccine acceptance. We conducted bivariate and multivariate analysis for determinants of vaccine acceptance with SPSS 23.0.
Results
We recruited 779 respondents with 38.9% male and median age of 24 years old (IQR 20 – 26). The result showed vaccine acceptance of 60.8%. Vaccine acceptance was correlated with conspiracy beliefs, trusts in conventional media and authoritative sources with Spearman's rho of −0.350, 0.269, and 0.287 respectively. Controlling for demographics and impacts of pandemic, showed strong conspiracy beliefs and trust in conventional media as the only independent determinants with OR of 0.33 (CI95% 0.20–0.54) and 1.91 (CI95% 1.37–2.65) respectively.
Conclusion
The results indicated considerable impacts of infodemic, represented by conspiracy beliefs, trust in media, and in authoritative sources, toward COVID-19 vaccine acceptance. Effective public health messaging should be conducted concurrent with vaccine rollout to improve acceptance and achieve herd immunity.
Keywords: COVID-19, Vaccine acceptance, Trust, Media, Institutions, Conspiracy
1. Introduction
WHO situation report in December 13th 2020 showed a cumulative case of over 70 million with 1.6 million cumulative mortality (WHO, 2020b). In Indonesia alone, as of December 18th 2020, there has been cumulative case of over 650 thousand with over 19 thousand mortality(COVID-19 Response Acceleration Task Force, 2020). Throughout the pandemic, government institutions have responded to the crises with a slew of public health policies. These policies included discouragement from mass gathering and endorsement of physical distancing, hand hygiene, and mask wearing in public (WHO, 2020c). Health official has also been recommended to conduct stringent contact tracing and quarantine measures to those exposed (WHO, 2020a). Evidence showed these measures could effectively prevent transmission up to 81% and mortality by 63% (Girum et al., 2020). However, the results varied between communities and there are gaps left behind.
Vaccine development for SARS-CoV-2 was hoped to fill in these gaps. Fortunately, there was been fortunate news of effective COVID-19 vaccines developed by Pfizer/BioNTech (USA), Moderna (USA), and AstraZeneca/Oxford (UK) with over 90% efficacy(Knoll & Wonodi, 2020; Mahase, 2020; Polack et al., 2020). As such, discourse now shifted to administrative and legal requirement for approval of these vaccines, as well as logistics of distributing the vaccine. A large proportion of the population should be vaccinated to achieve herd immunity. Evidence from previous influenza pandemics showed 80–90% vaccine coverage was adequate to establish herd immunity, while 75% coverage or lower was not (Plans-Rubió, 2012). For COVID-19, it is estimated a minimum coverage of 60–70% would be required (Anderson et al., 2020).
However, even after we figure out optimal distribution chain for the vaccine, there remains one hurdle to overcome: acceptance. A global survey in July 2020 involving 13 thousand respondents in 19 countries showed 71.5% likely acceptance of COVID-19 vaccine should it become generally available although this rate varies from under 55% to over 90% in different countries (Lazarus et al., 2020). In Indonesia itself, a differently worder survey showed over 90% acceptance for a 95% effective COVID-19 vaccine (Harapan et al., 2020a, Harapan et al., 2020b). Although these figures are high, the data was obtained months earlier and the situation may have changed by the time the vaccine rolled out.
Among factors found affecting vaccine acceptance was trust in government (Lazarus et al., 2020) which take us to another longstanding issue in COVID-19 pandemic response: infodemic. Unverified information has been widely disseminated in various media resulting a considerable proportion of the population to held conspiracy beliefs surrounding COVID-19 pandemic. Two recent studies found a moderate level of conspiracy beliefs among their respondents (Earnshaw et al., 2020; Georgiou et al., 2020). There has been evidence of conspiracy beliefs negatively associated with adherence to COVID-19 preventive behaviors (Allington et al., 2020; Earnshaw et al., 2020). Similar infodemic has previously observed surrounding vaccination programs, although to lesser degrees. These theories ranged from cover-ups of health risks related to vaccine to how vaccination was a plot to control and track the population. Evidence from other vaccines showed that these conspiracy beliefs were associated with distrust in government and reduced vaccination intent (Goldberg & Richey, 2020; Jolley & Douglas, 2014).
The rapid changes associated with COVID-19 pandemic mitigation efforts, compounded by the infodemic, have been linked with increased mistrust in institutions as well as conspiracy beliefs (Ezeibe et al., 2020; Freeman et al., 2020). While there is evidence how these conspiracy beliefs may affect adherence to endorsed preventive behaviors, there are fewer evidence on how it affects acceptance of COVID-19 vaccines now that we are on the brink of mass vaccination. There are also few evidences on how these factors would interact with other factors associated with vaccine acceptance such as demographics, education, and prior exposure to COVID-19 (Lazarus et al., 2020). As such, we conduct this study to shed more evidence on these topics.
2. Method
2.1. Research design and setting
This study utilized cross-sectional design with a single online survey-based data collection for each respondent. Online survey was conducted in 6 weeks September to October 2020 period. It was conducted prior to any announcement of effective vaccine from any pharmaceutical company or research groups. However, in the same period, there has been news on potential impending public vaccination in Indonesia as early as November or December 2020, using Chinese-made vaccine developed by Sinovac (Soeriaatmadja, 2020). At the same time, we also observe higher support of COVID-19 conspiracy theories, fueled by celebrity openly endorsing it in social media (Nugroho, 2020). It culminated in protests against mask and screening mandate in July 2020 (The Jakarta Post, 2020a) and a criminal case launched against a prominent celebrity proponent of COVID-19 conspiracy theory in Bali (The Jakarta Post, 2020b).
Meanwhile, in the same period Indonesia almost doubled the number of confirmed cases, from 221 thousand in September 14th to 410 thousand in October 31st. In the same period, mortality rose from 8 thousand to 13 thousand. Similar pattern was also observed in Bali where confirmed case rose form 5 thousand to 10 thousand and mortality rose from 179 to 387 (COVID-19 Response Acceleration Task Force, 2020). Indonesian economy, and especially Balinese, was also severely impacted with contraction of 6.8% announced in early November 2020 (Hendartyo, 2020), days after the survey was closed.
2.2. Data collection
Data collection was conducted by online survey made on Google Form for 6 weeks, from September 14th to October 31st 2020. Online survey promotion materials, including online pamphlets and URLs, was distributed through researchers' social media networks, including Facebook, Instagram, WhatsApp, and Twitter, with respondents and other viewers encouraged to forward the content to their network.
Recruitment materials, in form of pamphlet and URL to the online survey were shared online at least once per day. A coordinated ‘blast’ of recruitment material was scheduled biweekly along with updated pamphlets. Respondents were incentivized with chance to win a lottery worth IDR 100,000 (around USD 7) in electronic money for 20 lucky respondents.
Eligibility for inclusion in analysis was respondents aged 18 or older and have been resident of Bali since July 2019 at the latest. We exclude duplicate entries, identified by their mobile phone numbers entered as prerequisite for lottery inclusion. We also exclude respondents with incomplete responses from analyses.
2.3. Variables and measurements
The survey collected data on respondents' demographic information, health, social, and economic impact of COVID-19 pandemic, as well as trust in media and authoritative information sources, conspiracy beliefs, and vaccine acceptance.
Conspiracy beliefs were measured with a 12-itemed questionnaire based on the work of Miller (2020). Trust in media and authoritative sources was measured by 4-itemed questionnaire each. Cronbach alpha values for conspiracy beliefs, trust in conventional media, and in authoritative sources was 0.933, 0.897, and 0.900, respectively. Details on measures can be seen in Table 1 .
Table 1.
Measures for conspiracy beliefs and trust variables.
| Measures | Statements | Cronbach α |
|---|---|---|
| Conspiracy beliefs | COVID-19 is a manmade disease COVID-19 is a biological weapon COVID-19 is caused by 5G signal Actually COVID-19 is just a normal flu COVID-19 is a ploy to force everyone to be vaccinated Bill Gates funded COVID-19 conspiracy COVID-19 is not as deadly as portrayed Media intentionally overblown COVID-19 dangers Government intentionally overblown COVID-19 dangers COVID-19 vaccine and medication has been invented but is covered up Healthcare workers financially benefited from COVID-19 pandemic Government use COVID-19 pandemic to grab more power |
0.933 |
| Trust in conventional media | How much do you trust COVID-19 information from: - Television - Radio - Print media - Online media with a printed version |
0.897 |
| Trust in authoritative sources | How much do you trust COVID-19 information from: - Government institutions - Government officials - Healthcare workers - Academics |
0.900 |
Respondents responded in form of 5-itemed Likert scale from ‘disagree’ to ‘strongly agree’ with assigned score from 0 to 4. Conspiracy beliefs was measured by total score from all 12 questions with range from 0 to 48 which corresponds to 0% to 100% of maximum score. Meanwhile, each trust scale has score range from 0 to 16 which correspond to 0% and 100% of maximum score. Further, respondents were dichotomized based on all three scales into strong and weak categories with cutoff point of over 50% to be categorized into strong conspiracy belief or strong trust groups.
Meanwhile, vaccine acceptance was measured with a single question with 5-itemed Likert scale response. The question was ‘When COVID-19 vaccine is available, would you accept to be vaccinated?’ Responses was recorded in an ordinal scale ranged in likelihood from ‘would not accept’ to ‘would accept’ the vaccine.
2.4. Analyses
Bivariate analyses for conspiracy beliefs and trust variables with vaccine acceptance variables was conducted with non-parametric correlation and Kruskal-Wallis analyses. For multivariate analyses, vaccine acceptance variables were dichotomized, and analyses was conducted with multiple binomial logistic regression. All analyses were conducted on IBM SPSS 23.0.
2.5. Ethical consideration
All respondents were given informed consent in the form of the first page of the online survey. Respondents have to answer affirmative in consenting to participate to progress to the main questionnaires. Respondents was also given chance to stop their participation at any stage data collection either by discontinuing response to the questionnaire or by contacting research team to notify their wish to discontinue participation. Ethical considerations for this survey have been reviewed and approved by appropriate ethical committee with Ethical Clearance no. 1918/UN14.2.2.VII.14/LT/2020.
3. Result
There were 842 responses to the online survey, 60 was excluded as duplicates and further 3 responses were excluded due to incomplete data. As visible in Table 2 , a total of 779 respondents was included for analyses, which include 303 (38.9%) male and 476 (61.1%) females. Median age was 24 (IQR 20–26) years old with native Balinese making up 80.4% of respondents. A majority (63.8%) of respondents have some form of college education while employment data showed 310 (39.8%) of respondents reported as students. As much as 297 (38.1%) reported to have full-time employment. By income, 385 (49.4%) of respondents reported monthly income of less than IDR 1 million.
Table 2.
Sociodemographic and COVID-19 pandemic impacts among respondents.
| Variables | |
|---|---|
| Sex, n (%) | |
| Male | 303 (38.9) |
| Female | 476 (61.1) |
| Age, median (IQR) | 24 years (20–26) |
| Ethnicity, n (%) | |
| Balinese | 626 (80.4) |
| Non-Balinese | 153 (19.6) |
| Education, n (%) | |
| Without higher education | 282 (36.2) |
| With higher education | 497 (63.8) |
| Employment, n (%) | |
| Unemployed | 42 (5.4) |
| Student | 310 (39.8) |
| Part-time employment | 130 (16.7) |
| Full-time employment | 297 (38.1) |
| Monthly income, n (%) | |
| ≤ IDR 1 million | 385 (49.4) |
| IDR 1 million – IDR 3 million | 184 (23.6) |
| > IDR 3 million | 210 (27.0) |
| History of COVID-19 infection, n (%) | |
| Never | 688 (88.3) |
| Suspected | 74 (9.5) |
| Confirmed | 17 (2.2) |
| COVID-19 infection in social circle, n (%) | |
| Never | 324 (41.6) |
| Suspected | 136 (17.5) |
| Confirmed | 319 (40.9) |
| COVID-19 related mortality in social circle, n (%) | |
| No | 616 (79.1) |
| Yes | 163 (20.9) |
| Impact to employment, n (%) | |
| No impact | 387 (49.7) |
| Hours and pay reduction | 200 (25.7) |
| Furloughed | 163 (20.9) |
| Termination | 29 (3.7) |
| Impact to income, n (%) | |
| Increased/no change | 261 (33.5) |
| Mild reduction | 178 (22.8) |
| Severe reduction | 340 (43.6) |
Some respondents reported have had COVID-19, either suspected or confirmed, amounting to 9.5% and 2.2% respectively. However, 136 (17.5%) and 319 (40.9%) respondents, respectively, reported have had someone in their social circle suspected or confirmed with COVID-19 with 163 (20.9%) reported have had someone in their social circle died with causes related to COVID-19 infection. Majority of respondents also reported economic impact of COVID-19 pandemic with only 387 (49.7%) and 261 (33.5%), respectively, reported no impact to either their employment status or income.
As can be seen in Table 3 , median score for conspiracy beliefs was 22.92% while for trusts in conventional media and authoritative sources was 50.00% and 75.00% respectively. Only 12.2% of respondents was categorized with strong belief in COVID-19 conspiracy theories while 48.8% and 79.2% respondents were categorized with strong trust in conventional media and authoritative sources, respectively. The majority of respondents (60.8%) also reported they would certainly accept COVID-19 vaccine when it becomes available. The remaining respondents were more inclined to accept, although not certain, with 15.1% reported likely to accept and 15.0% reported probably would accept.
Table 3.
Conspiracy belief, trusts, and vaccine acceptance.
| Variables | |
|---|---|
| Conspiracy belief score, median (IQR) | 22.92% (8.33%–35.42%) |
| Conspiracy belief category, n (%) | |
| Weak belief | 684 (87.8) |
| Strong belief | 95 (12.2) |
| Trust in conventional media score, median (IQR) | 50.00% (43.75% - 75.00%) |
| Trust in conventional media category, n (%) | |
| Weak trust | 402 (51.6) |
| Strong trust | 377 (48.8) |
| Trust in authoritative source score, median (IQR) | 75.00% (56.25% - 87.50%) |
| Trust in authoritative source category, n (%) | |
| Weak trust | 162 (20.8) |
| Strong trust | 617 (79.2) |
| Vaccine acceptance, n (%) | |
| Would not accept | 23 (3.0) |
| Unlikely to accept | 47 (6.0) |
| Probably accept | 117 (15.0) |
| Likely to accept | 118 (15.1) |
| Would accept | 474 (60.8) |
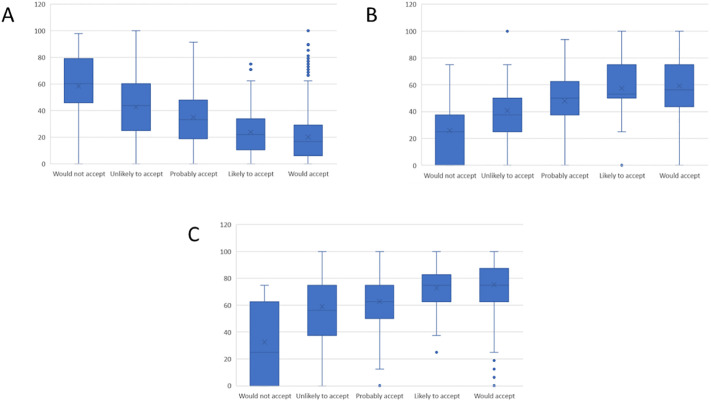
Bivariate analyses showed correlation between vaccine acceptance with conspiracy beliefs and trusts, as shown in Fig. 1 . Non-parametric correlation analyses for ordinal variables showed statistically significant correlation between vaccine acceptance with conspiracy beliefs and trust in conventional media as well as authoritative sources with Spearman's rho value of −0.350, 0.269, and 0.287 respectively.
Fig. 1.
Boxplot showing correlation of vaccine acceptance with A) conspiracy beliefs, B) trust in conventional media, and C) authoritative information sources.
We also observe intercorrelation between conspiracy beliefs and trusts. Conspiracy beliefs was inversely correlated with trusts in conventional media and authoritative sources with Spearman's rho of −0.248 and -0.358 respectively. Meanwhile, trust in conventional media was positively associated with trust in authoritative source with Spearman's rho of 0.520.
For multivariate analyses, we dichotomized vaccine acceptance into those who would accept. Multivariate analyses were conducted with multiple binomial logistic regression and controlled demographics, economic, and social impacts of the pandemic.
Table 4 showed multivariate analyses between conspiracy beliefs and trusts with vaccine acceptance, controlling for demographics and impacts for COVID-19 pandemic. The results showed strong conspiracy beliefs and trust in conventional media was independently associated with vaccine acceptance although in opposite directions. Strong trust in conventional media was associated with higher likelihood for vaccine acceptance with OR of 1.91 (CI95% 1.37–2.65) while strong conspiracy beliefs was associated with lower vaccine acceptance with OR of 0.33 (CI95% 0.20–0.54).
Table 4.
Multivariate binomial logistic regression for vaccine acceptance.
| Variables | OR (95% confidence interval) | p |
|---|---|---|
| Sex | ||
| Male | Ref. | |
| Female | 1.13 (0.82–1.57) | 0.460 |
| Age | 1.02 (0.99–1.05) | 0.148 |
| Ethnicity | ||
| Balinese | Ref. | |
| Non-Balinese | 0.93 (0.63–1.37) | 0.928 |
| Education | ||
| Without higher education | Ref. | |
| With higher education | 1.38 (0.89–2.14) | 0.149 |
| Employment | ||
| Full-time employment | Ref. | |
| Part-time employment | 2.06 (0.89–4.81) | 0.094 |
| Student | 1.54 (0.83–2.86) | 0.172 |
| Unemployed | 0.89 (0.55–1.42) | 0.621 |
| Monthly income | ||
| ≤ IDR 1 million | Ref. | |
| IDR 1 million – IDR 3 million | 1.16 (0.70–1.94) | 0.562 |
| > IDR 3 million | 1.26 (0.70–2.24) | 0.441 |
| History of COVID-19 infection | ||
| Never | Ref. | |
| Suspected | 1.67 (0.94–2.97) | 0.081 |
| Confirmed | 1.03 (0.35–3.04) | 0.951 |
| COVID-19 infection in social circle | ||
| Never | Ref. | |
| Suspected | 0.93 (0.59–1.47) | 0.759 |
| Confirmed | 0.89 (0.61–1.30) | 0.558 |
| COVID-19 mortality in social circle | ||
| No | Ref. | |
| Yes | 1.18 (0.79–1.177) | 0.411 |
| Impact to employment | ||
| No impact | Ref. | |
| Hours and pay reduction | 0.83 (0.53–1.31) | 0.418 |
| Furloughed | 1.04 (0.66–1.65) | 0.867 |
| Termination | 1.30 (0.51–3.29) | 0.580 |
| Impact to income | ||
| Increased/no change | Ref. | |
| Mild reduction | 0.82 (0.52–1.28) | 0.383 |
| Severe reduction | 0.78 (0.50–1.22) | 0.282 |
| Conspiracy belief category | ||
| Weak belief | Ref. | |
| Strong belief | 0.33 (0.20–0.54) | < 0.001⁎ |
| Trust in conventional media category | ||
| Weak trust | Ref. | |
| Strong trust | 1.91 (1.37–2.65) | < 0.001⁎ |
| Trust in authoritative source category | ||
| Weak trust | Ref. | |
| Strong trust | 1.34 (0.88–2.03) | 0.171 |
p < 0.05.
4. Discussion
The main finding in this study is the level of vaccine acceptance, which is moderately high with 60.8% reported they would accept the vaccine and 15.1% reported they were likely to accept. Meanwhile, we observed low but significant, level of conspiracy beliefs with median score of 22.92% and 12.2% of respondents classified as having strong conspiracy beliefs. We also observe moderate trust in conventional media, with median score of 50% and almost fifty-fifty divide between weak, and strong trust groups, accompanied by high level of trust in authoritative sources, with median score of 75%.
There is considerable similarity of level of vaccine acceptance between our September–October survey with previous surveys conducted in April–May period (Freeman et al., 2020; Lazarus et al., 2020). Interestingly, our observed vaccine acceptance was considerably higher than other Indonesian surveys conducted in similar timeframe to ours. One set of surveys conducted in October–December period in Indonesia showed acceptance rate hovering around 35–40% mark with the highest being 54% in a survey conducted in December 2nd to 5th period (KedaiKopi Survey Institution, 2020; Saiful Mujani Research and Consulting, 2020). The difference can be attributed to respondents' characteristics. Our respondents consist mostly of younger and with higher education than other Indonesian surveys (KedaiKopi Survey Institution, 2020; Saiful Mujani Research and Consulting, 2020), which may contributed to higher vaccine acceptance.
Another potential factor is the difference in religious demographic characteristics. As is commonly known, Indonesia is a Muslim-majority country. Many controversies regarding vaccine was based on Islamic beliefs, especially on the halal status of the vaccine (i.e., whether the vaccine production and handling subscribe to Islamic religious rules) (Harapan et al., 2016; Pronyk et al., 2019). Bali, meanwhile, is a Hindu-majority region in Indonesia. With over 80% of respondents identifying as native Balinese, the difference in religious demographic between our data and aforementioned studies may also play a role in different vaccine acceptance.
On level of trusts in conventional media and institutions, however, we observed more consistency between our data and previous studies, including aforementioned Indonesian surveys. While there are some reports on diminishing trust in public institutions and media, the level of trusts remain moderate to high (Earnshaw et al., 2020), including in Indonesia (KedaiKopi Survey Institution, 2020; Saiful Mujani Research and Consulting, 2020). This is especially true in countries whose government's policy successfully suppress transmission, such as New Zealand (Sibley et al., 2020).
Consistency was also observed in level of conspiracy beliefs. One study reporting data from the United States measures conspiracy similarly to our study, showing mean score of 27 in a scale from 9 to 53 (Georgiou et al., 2020). Another, more recent, survey in Indonesia also showed considerably higher conspiracy beliefs. Based on five-itemed questionnaire, around 30–40% of respondents admitted they agree or strongly agree with conspiracy-related statements (KedaiKopi Survey Institution, 2020). Other data also showed the conspiracy to take hold even among university students, as study in Jordan showed 16.4% university student believe in COVID-19 conspiracy. Even among students in medical and scientific schools, the belief was held by 13.6% of student (Sallam et al., 2020).
Another main finding in this study was the correlation between vaccine acceptance with conspiracy beliefs, trusts in conventional media, authoritative sources. We found weak to moderate, statistically significant, correlations for all these four variables. Bivariate analysis with other covariate also found sex, personal history of COVID-19 infection, and pandemic impact to income as determinant to vaccine acceptance (Supp. File 1). Interestingly, only conspiracy beliefs and trust in conventional media was found as independent determinants of vaccine acceptance on multivariate analysis.
There has also been evidences of inverse correlation between levels of trust in government, media, academics, and other authority figures toward COVID-19 conspiracy beliefs. One study in UK showed inverse correlation between trust in government, doctors, and scientists with COVID-19 conspiracy beliefs. Curiously the same study showed positive correlation between trust in mainstream media and conspiracy beliefs, contrary to our findings in this study (Earnshaw et al., 2020; Freeman et al., 2020).
The observed inverse correlation between conspiracy beliefs and vaccine acceptance can be explained with cost-benefit analysis framework. Trust and valuation of vaccine benefits has been shown as important factors driving vaccine acceptance. In this framework, perceived benefits of vaccine diminish as the dangers of the disease it prevents became less visible due to successful vaccination programs (Ozawa & Stack, 2013). In this framework, perceived dangers that come with vaccine conspiracy beliefs ends up overpowering the slim and diminishing perceived benefits, reducing intent to vaccinate (Jolley & Douglas, 2014).
This led us to the paradox of COVID-19. With the pandemic still raging, the benefits of the vaccine should be obvious. However, the very nature of COVID-19 conspiracy theories was not on the danger of the vaccine but on the underlying facts of the disease itself. COVID-19 conspiracy mostly doubt the origin, nature, severity, and risk posed by the disease (Miller, 2020; Oleksy et al., 2021; Stephens, 2020). As such, conspiracy beliefs may explain lower perceived dangers from COVID-19 thus diminishing perceived benefits from its prevention through vaccine (Karlsson et al., 2020).
Our results can also be explained using vaccine hesitancy determinants, which included confidence, convenience, and complacency (MacDonald et al., 2015). While the convenience of COVID-19 vaccine was not yet apparent at the time of survey, the complacency and confidence can be linked to our variables. Misinformation on the nature of the COVID-19 disease create complacency, lowering perceived risk and severity of the disease (Kim & Kim, 2021). Meanwhile, distrust in media and authoritative information sources may also contribute to distrust in vaccine-related information coming from these sources.
Further analysis also found bivariate determinants of conspiracy beliefs and trust (Supp. File 1). Several covariates are consistent in their association with conspiracy beliefs and trust. Students are found less likely to believe in conspiracy theories and to have higher trust in media and authoritative figures. COVID-19 infection history in social circle also seems to increase trust. Meanwhile, loss of employment and/or income during the pandemic seems to erode trust and boost conspiracy beliefs.
These results were in line with previous studies. There has been studies that showed vulnerability, including health and economic vulnerability in the time of COVID-19 pandemic erode trust in authorities, including government figures and media (Devine et al., 2020; Gozgor, 2021). Furthermore, another study has also revealed students, especially college and university students, as less at risk to conspiracy beliefs (Duplaga, 2020).
This result is relevant to the problem of vaccine rollout that we face today. Although our results indicates a 60–70% acceptance rate, which is rather high, we still have to address conspiracy beliefs and trust which was found as significant factors. Stakeholders, public and private, should not give in to the infodemic in this crucial phase of COVID-19 vaccine public rollout. Attempt to mitigate conspiracy beliefs and to strengthen trust in our institutions should be implemented. The main objective is to increase exposure of science-based information to general public and stop treating unverified information as equal to established science-based facts. It can be achieved through cooperation between academics, public health official, and media corporation (Mheidly & Fares, 2020).
Attempts should also be made to address public concerns that may influence their trust in media and authorities as well as conspiracy beliefs, which underpins the reluctance to vaccinate. These efforts could include improvement to social security programs to alleviate concerns of economic insecurity during the pandemic (Guest et al., 2020). Improving inter-departmental and central-regional policy integration and communicating it to the public could also improve trust in authority and the media (Suwarno & Rahayu, 2021).
Lastly, we would like to highlight the strengths of this study. Our study was one of few studies to investigate the impact of conspiracy beliefs and trust to COVID-19 vaccine acceptance, which has become increasingly relevant as we begin to roll out the vaccine to the public. It is also of increasing relevance as previous studies on the topics of COVID-19 conspiracy beliefs, trust, and vaccine acceptance mostly conduct their data gathering early in the pandemic. Our survey, which was conducted in September–October period could show more recent development on the issues.
However, we must also state the caveats of this study. Non-random sampling method we employ in this study is subject to risk of systematic recruitment bias whereas certain group of people are more likely to response while others are less likely. The incentive given may also affect the decision to response although this is minimized by the fact that the amount is non-significant.
As visible in Table 1, age distribution of this study mostly covered young adults aged 20 to 26 years old due to data collection process which relied on social media. As such, this would be the most appropriate generalizable population of our findings. However, we believe generalizable data on vaccine acceptance of this segment of the population is important due to their tendency to facilitate COVID-19 transmission due to high mobility and higher proportion of undetected asymptomatic infections (Guilamo-Ramos et al., 2020).
We also need to point out the simple ordinal scale we employ in vaccine acceptance and willingness to pay measurement may oversimplify these concepts. Although similar ordinal measurement was employed by other large-scale survey in Indonesia (KedaiKopi Survey Institution, 2020; Saiful Mujani Research & Consulting, 2020), we were unable to capture to potential difference of acceptance based on vaccine effectivity, brand, country of origin, and others as was measured in some other studies (Harapan et al., 2020a, Harapan et al., 2020b).
5. Conclusion
We found adequately high level of COVID-19 vaccine acceptance among Balinese residents. Meanwhile, we observe low but significant level of COVID-19 conspiracy beliefs with moderate level of trust in conventional media and high level of trust in authoritative information sources. Conspiracy beliefs and trust was significantly and independently associated with vaccine acceptance. Our results imply the need of strong and clear public health messaging in the crucial months of COVID-19 vaccine public rollout.
Funding
None.
CRediT authorship contribution statement
Gede Benny Setia Wirawan: Conceptualization, Methodology, Data curation, Formal analysis, Writing – original draft. Putu Nandika Tungga Yudanti Mahardani: Investigation, Writing – review & editing. Made Ratna Komala Cahyani: Investigation, Writing – review & editing. Ni Luh Prema Shantika Putri Laksmi: Investigation, Writing – review & editing. Pande Putu Januraga: Conceptualization, Methodology, Writing – review & editing, Supervision, Funding acquisition.
Declaration of competing interest
The authors have no conflict of interest to declare related to materials presented in this paper.
Acknowledgments
Acknowledgement
We would like to acknowledge Center for Public Health Innovation (CPHI), Faculty of Medicine, Udayana University, for the funding of this study. We would also like to convey our appreciation to all respondents for their participation in this study.
References
- Allington D., Duffy B., Wessely S., Dhavan N., Rubin J. Health-protective behaviour, social media usage, and conspiracy belief during the COVID-19 public health emergency. Psychological Medicine. 2020 doi: 10.1017/S003329172000224X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R.M., Vegvari C., Truscott J., Collyer B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. The Lancet. 2020;396(10263):1614–1616. doi: 10.1016/S0140-6736(20)32318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Response Acceleration Task Force. (2020). Distribution maps (Indonesian). Retrieved January 31, 2021, from https://covid19.go.id/peta-sebaran.
- Devine D., Gaskell J., Jennings W., Stoker G. Trust and the coronavirus pandemic: What are the consequences of and for trust? An early review of the literature. Political Studies Review. 2020:1–12. doi: 10.1177/1478929920948684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duplaga M. The determinants of conspiracy beliefs related to the COVID-19 pandemic in a nationally representative sample of internet users. International Journal of Environmental Research and Public Health. 2020;17(21):1–18. doi: 10.3390/ijerph17217818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V.A., Eaton L.A., Kalichman S.C., Brousseau N.M., Hill E.C., Fox A.B. COVID-19 conspiracy beliefs, health behaviors, and policy support. Translational Behavioral Medicine. 2020;10(4):850–856. doi: 10.1093/tbm/ibaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezeibe C.C., Ilo C., Ezeibe E.N., Oguonu C.N., Nwankwo N.A., Ajaero C.K., Osadebe N. Political distrust and the spread of COVID-19 in Nigeria. Global Public Health. 2020;15(12):1753–1766. doi: 10.1080/17441692.2020.1828987. [DOI] [PubMed] [Google Scholar]
- Freeman D., Waite F., Rosebrock L., Petit A., Causier C., East A.…Lambe S. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychological Medicine. 2020 doi: 10.1017/S0033291720001890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgiou N., Delfabbro P., Balzan R. COVID-19-related conspiracy beliefs and their relationship with perceived stress and pre-existing conspiracy beliefs. Personality and Individual Differences. 2020;166(110201) doi: 10.1016/j.paid.2020.110201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girum T., Lentiro K., Geremew M., Migora B., Shewamare S. Global strategies and effectiveness for COVID-19 prevention through contact tracing, screening, quarantine, and isolation: A systematic review. Tropical Medicine and Health. 2020;48(1) doi: 10.1186/s41182-020-00285-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg Z.J., Richey S. Anti-vaccination beliefs and unrelated conspiracy theories. World Affairs. 2020;183(2):105–124. doi: 10.1177/0043820020920554. [DOI] [Google Scholar]
- Gozgor G. Global evidence on the determinants of public trust in governments during the COVID-19. Applied Research in Quality of Life. 2021 doi: 10.1007/s11482-020-09902-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest J.L., del Rio C., Sanchez T. The three steps needed to end the COVID-19 pandemic: Bold public health leadership, rapid innovations, and courageous political will. JMIR Public Health and Surveillance. 2020;6(2) doi: 10.2196/19043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilamo-Ramos, V., Benzekri, A., Thimm-Kaiser, M., Hidalgo, A., & Perlman, D. C. (2020). Reconsidering assumptions of adolescent and young adult severe acute respiratory syndrome coronavirus 2 transmission dynamics. Clinical Infectious Diseases, (Suppl XX), 1–8. doi: 10.1093/cid/ciaa1348. [DOI] [PMC free article] [PubMed]
- Harapan H., Anwar S., Setiawan A.M., Sasmono R.T. Dengue vaccine acceptance and associated factors in Indonesia: A community-based cross-sectional survey in Aceh. Vaccine. 2016;34(32):3670–3675. doi: 10.1016/j.vaccine.2016.05.026. [DOI] [PubMed] [Google Scholar]
- Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K.…Mudatsir M. Acceptance of a COVID-19 vaccine in Southeast Asia: A cross-sectional study in Indonesia. Frontiers in Public Health. 2020;8(July):1–8. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K.…Mudatsir M. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Human Vaccines & Immunotherapeutics. 2020;00(00):1–7. doi: 10.1080/21645515.2020.1819741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendartyo M. Nusa Tenggara economies hit the hardest. 2020, November 6. Indonesia in recession; Bali.https://en.tempo.co/read/1402714/indonesia-in-recession-bali-nusa-tenggara-economies-hit-the-hardest Retrieved December 19, 2020, from. [Google Scholar]
- Jolley D., Douglas K.M. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS One. 2014;9(2) doi: 10.1371/journal.pone.0089177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson, L. C., Soveri, A., Lewandowsky, S., Karlsson, L., Karlsson, H., Nolvi, S., … 1Department. (2020). Fearing the disease or the vaccine: The case of COVID-19. (Preprint), 172, 110590. doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed]
- KedaiKopi Survey Institution . 2020. COVID-19 vaccine perception survey. (Jakarta) [Google Scholar]
- Kim, S., & Kim, S. (2021). Searching for general model of conspiracy theories and its implication for public health policy: Analysis of the impacts of political, psychological, structural factors on conspiracy beliefs about the COVID-19 pandemic. [DOI] [PMC free article] [PubMed]
- Knoll M.D., Wonodi C. Oxford-AstraZeneca COVID-19 vaccine efficacy. Lancet. 2020;2(20):19–21. doi: 10.1016/S0140-6736(20)32623-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K.…El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine. 2020 doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald N.E., Eskola J., Liang X., Chaudhuri M., Dube E., Gellin B.…Schuster M. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Mahase E. Covid-19: Vaccine candidate may be more than 90% effective, interim results indicate. BMJ (Clinical Research Ed.) 2020;371(November 2020):m4347. doi: 10.1136/bmj.m4347. [DOI] [PubMed] [Google Scholar]
- Mheidly N., Fares J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. Journal of Public Health Policy. 2020;41(4):410–420. doi: 10.1057/s41271-020-00247-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J.M. Do covid-19 conspiracy theory beliefs form a monological belief system? Canadian Journal of Political Science. 2020;53(2):319–326. doi: 10.1017/S0008423920000517. [DOI] [Google Scholar]
- Nugroho, J. (2020, August 19). Indonesia's COVID-19 conspiracy theories. Retrieved December 19, 2020, from New Naratif website: https://newnaratif.com/journalism/indonesias-covid-19-conspiracy-theories/share/revxanqve/ac54acb4b5289a1342f6e71089288e0b/.
- Oleksy, T., Wnuk, A., Maison, D., & Łyś, A. (2021). Content matters. Different predictors and social consequences of general and government-related conspiracy theories on COVID-19. Personality and Individual Differences, 168(110289). [DOI] [PMC free article] [PubMed]
- Ozawa S., Stack M.L. Public trust and vaccine acceptance-international perspectives. Human Vaccines & Immunotherapeutics. 2013;9(8):1774–1778. doi: 10.4161/hv.24961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plans-Rubió P. The vaccination coverage required to establish herd immunity against influenza viruses. Preventive Medicine. 2012;55(1):72–77. doi: 10.1016/j.ypmed.2012.02.015. [DOI] [PubMed] [Google Scholar]
- Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S.…C4591001 Clinical Trial Group Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. The New England Journal of Medicine. 2020:1–13. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronyk P., Sugihantono A., Sitohang V., Moran T., Kadandale S., Muller S.…Kezaala R. Vaccine hesitancy in Indonesia. The Lancet Planetary Health. 2019;3(3):e114–e115. doi: 10.1016/S2542-5196(18)30287-0. [DOI] [PubMed] [Google Scholar]
- Saiful Mujani Research & Consulting . 2020. National Public Trust in Covid-19 vaccines and vaccinations. (Jakarta) [Google Scholar]
- Sallam M., Dababseh D., Yaseen A., Al-Haidar A., Ababneh N.A., Bakri F.G., Mahafzah A. Conspiracy beliefs are associated with lower knowledge and higher anxiety levels regarding covid-19 among students at the university of Jordan. International Journal of Environmental Research and Public Health. 2020;17(14):1–15. doi: 10.3390/ijerph17144915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley C.G., Greaves L.M., Satherley N., Wilson M.S., Overall N.C., Lee C.H.J.…Barlow F.K. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. American Psychologist. 2020;75(5):618–630. doi: 10.1037/amp0000662. [DOI] [PubMed] [Google Scholar]
- Soeriaatmadja, W. (2020, October 12). Indonesia aims to start administering coronavirus vaccines in early November. Retrieved December 19, 2020, from The Strait Times website: https://www.straitstimes.com/asia/se-asia/indonesia-aims-to-start-administering-coronavirus-vaccines-in-early-november.
- Stephens M. A geospatial infodemic: Mapping Twitter conspiracy theories of COVID-19. Dialogues in Human Geography. 2020;10(2):276–281. doi: 10.1177/2043820620935683. [DOI] [Google Scholar]
- Suwarno, Y., & Rahayu, N. S. (2021). LS policy integration real in policy practice? Critical review on how government of Indonesia respond to Covid-19 pandemic. IOP conference series: Earth and Environmental science, 717(1), 012041. doi: 10.1088/1755-1315/717/1/012041. [DOI]
- The Jakarta Post. (2020a, July 27). In Bali, hundreds rally without masks to protest rapid, swab test requirement. Retrieved December 19, 2020, from The Jakarta Post website: https://www.thejakartapost.com/travel/2020/07/27/in-bali-hundreds-rally-without-masks-to-protest-rapid-swab-test-requirement.html.
- The Jakarta Post. (2020b, November 3). Prosecutors demand 3 years for drummer Jerinx in IDI defamation case. Retrieved December 19, 2020, from The Jakarta Post website: https://www.thejakartapost.com/news/2020/11/03/prosecutors-demand-3-years-for-drummer-jerinx-in-idi-defamation-case.html.
- WHO. (2020a). Contact tracing in the context of COVID-19. Retrieved from https://www.who.int/publications-detail/contact-tracing-in-the-context-of-covid-19.
- WHO. (2020b). Coronavirus disease (COVID-19) weekly epidemiological update. Geneva.
- WHO. (2020c). Transmission of SARS-CoV-2: Implications for infection prevention precautions. Geneva.