Abstract
SUMMARY: Interventional neuroradiology procedures are a valuable asset in the diagnosis, treatment, and surgical management of various disorders affecting the extracranial head and neck. A detailed understanding of cross-sectional and vascular anatomy and an awareness of potential collateral pathways between extracranial and intracranial vessels are essential for ensuring safe and successful procedures. With the use of high-quality imaging and a meticulous technique, the incidence of major complications is extremely low.
Interventional neuroradiology has undergone a rapid evolution in the last 2 decades. Continuing advances in imaging technology and the introduction of newer tools, including more trackable microcatheters and safer embolic materials, have resulted in expanding applications of this discipline in the treatment of intracranial as well as head and neck lesions. Compared with open surgical methods, interventional neuroradiology techniques offer minimally invasive alternatives for many head and neck disorders.
Interventions in the head and neck can be performed via percutaneous, endovascular, or a combination of these approaches. Procedures that predominantly require percutaneous access include biopsies and aspirations, sclerotherapy, and newer techniques like radio-frequency ablation and cryoablation. On the other hand, a transarterial (or endovascular) approach forms the mainstay of treatment for head and neck bleeding as well as for transarterial chemotherapy for head and neck neoplasms. A combination of percutaneous and transarterial approaches may be needed in the embolization of high-flow craniofacial vascular malformations (VMs) and hypervascular tumors. This article provides a review of the current clinical applications of a variety of percutaneous and endovascular interventional procedures of the extracranial head and neck.
Image-Guided Biopsies
Percutaneous image-guided biopsies play an important part in the diagnosis and management of deep-seated head and neck lesions. Superficial and palpable masses are often accessible to clinical examination and can be safely biopsied in the office by an otolaryngologist or cytopathologist without image guidance. On the other hand, the facial skeleton, airway, and major vessels may prevent a direct access to the deep-seated lesions. CT is the technique of choice for image-guided biopsies of these deep-seated lesions,1,2 though sonography and interventional MR imaging systems can also be used.
With knowledge of cross-sectional anatomy and careful attention to the anatomic structures that could potentially be in the needle path, safe needle trajectories can be planned to almost all the major spaces of the head and neck. Although contrast injection is often not needed, it may be helpful when the mass to be biopsied is in close relationship to the vascular structures (Fig 1C, -D). Most of biopsies can be performed with local anesthesia and conscious sedation, but transoral biopsies of prevertebral and upper cervical vertebral lesions need general anesthesia.1
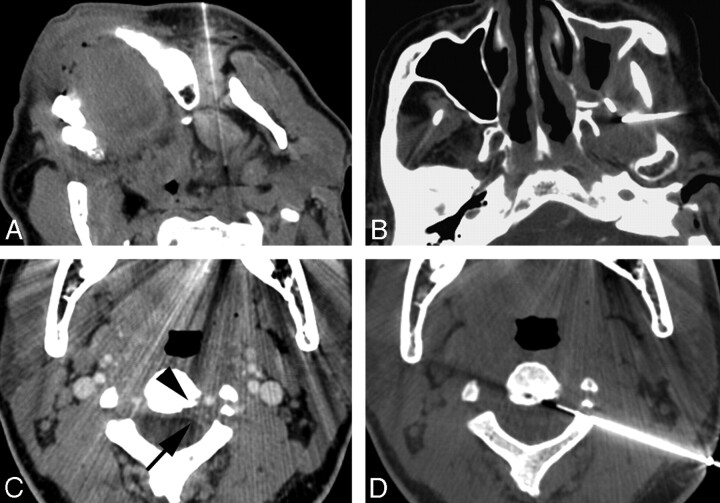
Fig 1.
A, Paramaxillary approach to the left parapharyngeal space mass, proven to be an oncocytoma. Slight turning of the head to the opposite side simplifies the approach to this parapharyngeal space lesion. B, Subzygomatic approach to the masticator space mass via the intercondylar notch. The core specimens in this patient with previously treated squamous cell carcinoma revealed scar tissue with no evidence of malignant cells. C, CT image in a patient with a mass at the C2 level reveals a subtle left-sided epidural soft-tissue (arrow) and cortical irregularity of the vertebral body (arrowhead). This image was acquired with contrast to map the location of the adjacent vertebral artery. D, A posterolateral approach to the epidural mass was planned. A 22-gauge Franseen needle is advanced through a guiding needle, and aspiration biopsy is performed. Aspiration biopsy was consistent with a diagnosis of chordoma.
A coaxial needle technique is very useful, with placement of an 18- to 19-gauge guiding (introducer) needle close to the target mass and subsequent advancement of the biopsy needle into the mass. We use thin 20- to 22-gauge Chiba or Franseen needles for obtaining aspirates for the cytologic analysis and, if required, 20-gauge cutting needles for obtaining core specimens. Injury to vascular structures and nerves can be avoided by using the Hawkins-Akins needle (Meditech, Westwood, Mass) with a blunt trocar.1,3,4 Modifications of the head position and opening the jaw with a bite block can be very helpful in permitting and facilitating access to many sites in the head and neck (Fig 1A). For example, mild hyperextension of the head can provide easier access to the skull base lesions via a paramaxillary or transbuccal approach. We often prefer to turn the patient's head contralateral to the side of the lesion. Suprahyoid neck, skull base, and upper cervical vertebral lesions can be biopsied via subzygomatic, retromandibular, paramaxillary, submastoid, transoral, and posterior approaches (Fig 1). Infrahyoid neck masses and lower cervical vertebrae require anterolateral, posterolateral, or posterior approaches. A detailed discussion of these approaches is beyond the scope of this article. However, the interested reader is referred to a recent article by Gupta et al,1 which discusses different approaches along with their particular anatomic considerations.
Percutaneous aspiration and biopsy techniques have a very high yield of diagnostic samples approaching 90%, with very few reported complications.2,5 Minor complications include pain, limited infection, or bleeding and vasovagal reactions.1 Injury to blood vessels and nerves is a theoretic concern but is very rarely encountered if careful attention is paid to needle-trajectory planning and small-caliber needles are used.
Radio-frequency Ablation and Cryoablation for Tumors
Radio-frequency and cryoablation represent focal tumor ablation strategies, most often used for the palliative treatment of unresectable malignancies or resectable lesions in patients with poor surgical risk. Radio-frequency ablation uses an alternating electric current to create ionic agitation, which produces frictional heat and subsequent tissue necrosis6 and is performed by using small percutaneous probes that produce heat, resulting in electrocauterization. This technique is gaining wide acceptance in the treatment of solid tumors of the liver, lung, kidney, and bone. The complication and postablation bleeding rates are fairly low.7 On the other hand, cryoablation produces rapid freezing of tissue, with resultant cell death due to ice crystallization, desiccation, and ischemic injury during thawing.8 Percutaneous cryoablation has been reported in the treatment of primary as well as metastatic tumors, most notably in the liver and the prostate.9
The advantages of radio-frequency ablation and cryoablative techniques include absence of a surgical scar, reduced recovery time, and the ability to visualize the treated tumor both during and after the procedure to determine treatment success. With cryoablation, direct visualization of the ice ball can be performed with sonography, CT, or MR imaging, and the treatment margins can be monitored in real time. Experience with radio-frequency ablation and cryoablation techniques in the head and neck is still in the very early stages, and only a handful of case descriptions exist, for example in the treatment of circumscribed solitary fibrous tumor,9 adenoid cystic carcinoma,10 and recurrent thyroid cancer.11
Recently Brook et al6 have reported the use of this technique in 14 patients with advanced unresectable head and neck cancers, in which radio-frequency ablation was performed with the intent of palliative therapy (Fig 2). The technical success of the procedure was reported to be 100%. The University of Washington quality-of-life surveys completed by 6 of the 14 patients (43%) showed an index increase by a median of 3.1 percentage points, with 4 of 6 patients (67%) demonstrating improvement. There were 3 major complications, all relating to proximity of the electrodes to the carotid artery. These included stroke, carotid blowout leading to death, and threatened carotid blowout with subsequent stroke. The authors cautioned that tumors surrounding or immediately adjacent to the carotid artery should not be treated at the energy levels used in their study. Additionally, a larger distance between the tumor and the electrodes may be helpful in preventing these complications.
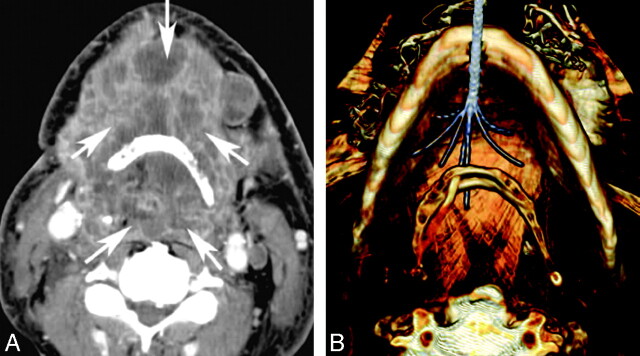
Fig 2.
A 59-year-old man with severe dyspnea and dysphagia secondary to a large squamous cell carcinoma treated with radio-frequency ablation. A, Axial contrast-enhanced CT scan demonstrates a large necrotic tumor (arrows) in the floor of the mouth and hypopharynx. B, 3D volume-rendered reconstruction demonstrates the radio-frequency probe (Starburst XLi; RITA Medical Systems, Mountainview, Calif) and electrode deployment within the tumor by means of a submental approach. Note that the tumor anterior and posterior to the hyoid bone could be ablated simultaneously. Reproduced with permission from the Journal of Vascular and Interventional Radiology.6 Copyright 2008, Elsevier.
Percutaneous Sclerotherapy
Percutaneous sclerotherapy (ST) is a technique that can be used to treat a variety of abnormalities in the head and neck, including low-flow VMs, plunging ranulas, sialoceles, and other benign cysts of the head and neck. Percutaneous catheterization of vascular channels or cysts is generally performed under direct visualization or sonography by using a needle or Teflon (Dupont, Wilmington, Del)–sheathed needle cannula.
The procedure is typically performed in the interventional suite with conscious sedation or general anesthesia. We prefer to use general anesthesia in children or when the lesion is large and may involve the airway. Contrast material is first injected under fluoroscopic guidance to assess the lesion and its venous drainage, exclude arterial cannulation, and calculate the volume of the sclerosant that can be injected before filling the draining vein (Fig 3). Injected contrast material is then aspirated out of the malformation and replaced with a slightly lower amount of the sclerosing agent. Commonly used sclerosants include the following: absolute alcohol, sodium tetradecyl sulfate (STS), polidocanol, sodium morrhuate, and doxycycline. Foaming the sclerosant agent can be performed by mixing it with air. Theoretically, foaming allows more prolonged displacement of the blood within the lesion and better contact of the sclerosant with the venous wall.
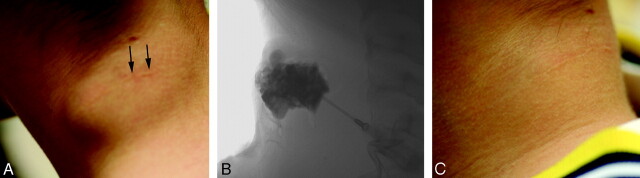
Fig 3.
A, Clinical photograph of the posterior aspect of the neck in an adolescent with a known venous malformation. The arrows in the picture point to the scar from a previous attempt at resection. Note the soft-tissue bulge of the residual venous malformation. B, Percutaneous injection of contrast into the venous malformation performed via an 18-gauge Teflon cannula shows the clustered and dilated venous spaces. The malformation was treated by using 3% STS that was injected after aspiration of the contrast. C, Clinical photograph on a follow-up visit shows complete disappearance of the soft-tissue bulge.
Low-Flow VMs
Low-flow VMs (LFVMs) of the head and neck include venous, lymphatic, and capillary malformations.12 They represent congenital defects in vascular morphogenesis. A discussion of capillary malformations is beyond the scope of this article and will be deferred because treatment is rarely performed with endovascular or percutaneous techniques. Venous and lymphatic malformations constitute the most common indication for ST of the head and neck.
Symptoms can range from pain, swelling, infection, or bleeding; or the problem can be a cosmetic.12,13 Functional impairment may be present, depending on the size, location, hemodynamic effects, and type of vessel involved. Large lesions may compress the aerodigestive tract and can sometimes present with compromise of the airway. Venous malformations consist of dilated venous channels that enlarge in a dependent position or with the Valsalva maneuver.14 The overlying skin may have a bluish-purple discoloration, and the lesions are compressible on palpation. Lymphatic malformations (LMs) are similar, except that the overlying skin does not show discoloration.
Evaluation is best performed with MR imaging. Sequences should include T1-weighted with fat-saturation before and after the infusion of gadolinium, inversion-recovery or T2-weighted with fat-saturation, and gradient-echo. We additionally prefer to obtain dynamic MR imaging with gadolinium to study the dynamics of contrast uptake within these lesions.
Venous malformations demonstrate high signal intensity with septations on T2-weighted images.15 Phleboliths may be evident as areas of signal-intensity void and are best seen on the gradient-echo images or on CT. Contrast administration results in a variable enhancement pattern, ranging from attenuated enhancement similar to that in adjacent veins to nonhomogeneous or delayed enhancement. LMs are generally classified as macrocystic, microcystic, or mixed. On MR imaging, lesions are generally of high signal intensity on T2-weighted and isointense to fluid on T1-weighted sequences.16 Unlike venous malformations, LMs generally do not enhance.
Treatment of LFVMs is challenging and often multidisciplinary, with involvement of the plastic surgeon, pediatric surgeon, otolaryngologist, and radiologist. Therapeutic options include compression, laser photocoagulation, resection, radio-frequency ablation, and obliteration of the lesion by percutaneous injection of a sclerosant agent.17,18 The most commonly used sclerosant agents are ethanol, STS, and polidocanol for VMs. LMs may be treated with OK-432 or doxycycline.19 At our center, we prefer to use ethanol and STS for venous malformations and doxycycline for LMs. For larger lesions, the sclerotherapy sessions are usually spaced 6–12 weeks apart, until there is no further recanalization or swelling.
The results of sclerotherapy are difficult to analyze because most citations in the literature report the results of patient questionnaires as the assessment of treatment outcome. Lee et al20 advocated the use of ethanol and demonstrated a 95% fair-to-good clinical response after treatment. Cabrera et al21 performed the largest study of polidocanol foam in the treatment of VMs and showed a 92% beneficial response rate. Seventy-five percent of patients with facial lesions report good or excellent results with ethanol or STS.17 Poor outcomes have been reported with diffuse VMs. Complete cure is unusual with diffuse lesions, and multiple treatment sessions are often necessary.17,20
Other Applications for Sclerosants
The mechanism of action of sclerosant agents involves producing an inflammatory reaction of the adjacent tissue as well as endothelial necrosis. Because of these properties, sclerosant agents have been used with variable success in many other cystic lesions of the head and neck, including plunging ranulas, sialoceles, benign lymphoepithelial cysts of the parotid gland, branchial cysts, and other benign cysts of the head and neck.22–24 Complications are generally minor, including fever and tender swelling for few days. Extracystic extravasation of sclerosants should be avoided, especially in the oral cavity and oropharynx because it can cause mucosal swelling, discomfort, and swallowing difficulties. The sclerotherapy should be withheld for the acutely infected cysts, and the infection should be controlled first.22
Preoperative Tumor Embolization
The tumors that require embolization in the head and neck most commonly include glomus tumors, angiofibromas, and meningiomas. Many other types of tumors that may also require preoperative embolization include the following: hypervascular metastases, esthesioneuroblastomas, schwannomas, rhabdomyosarcomas, plasmacytomas, chordomas, and hemangiopericytomas.
The goal of tumor embolization is to occlude selectively the external carotid artery (ECA) feeders through intratumoral deposition of embolic material. The embolic agents in common use are polyvinyl alcohol (PVA), Embospheres (BioSphere Medical, Rockland, Mass), liquid embolic agents (glue, ethylvinyl alcohol copolymer [EVOH], or Onyx [ev3, Irvine, Calif]), gelatin sponge (Gelfoam; Phadia, Uppsala, Sweden), and coils. The embolization is ideally performed 24–72 hours before surgical resection to allow maximal thrombosis of the occluded vessels and prevent recanalization of the occluded arteries or formation of collateral arterial channels. Preoperative embolization is cost-effective and tends to shorten operative time by reducing blood loss and the period of recovery.25,26
Treatment consists of performing a detailed cerebral angiography including selective injections of the internal carotid artery (ICA) and the ECA. A microcatheter is advanced into the artery supplying the tumor and angiography is performed checking for dangerous anastomoses between the ECA and ICA and or vertebral branches. The appropriate embolic agent is then injected under constant fluoroscopic monitoring, making sure to avoid reflux of embolic material and opening up of any dangerous anastomoses. If critical anastomoses are present, the anastomotic connection is first occluded with coils and then the particulate embolization is performed. Ideally, the embolic material is deposited at the arteriolar/capillary level. If there is arteriovenous shunting, particle size may need to be increased to prevent passage into the venous side. Proximal occlusion is inadequate because it allows arterial collateralization and may make surgical removal more difficult.
Embospheres of 100–300 μm are preferred by the authors because these particles allow more distal penetration into the tumor bed and better devascularization.27 However, one should always be aware of the possible risk of devascularizing the cranial nerves (the vasa nervorum are usually smaller than 150 μm) and the skin. Smaller particles may also increase the risk of tumoral hemorrhage and swelling.28 Therefore, when embolizing the arterial pedicles that might also supply the cranial nerves (for example the stylomastoid branch of the occipital artery or neuromeningeal trunk of the ascending pharyngeal artery), we upsize the particle size to 300–500 μm. We generally do not use liquid embolic agents via a transarterial approach because they can potentially occlude the arterial supply to the cranial nerves and may pass through tiny anastomoses into the intracranial circulation.
Direct percutaneous puncture under fluoroscopic guidance, CT, or sonography has also been described to embolize a number of different types of tumors. This method was initially reported for use in tumors in which conventional transarterial embolization was technically impossible due to the small size of the arterial feeders (Fig 4) or the posed risks that were considered too high.29 Examples include large tumors with supply from the ICA or ophthalmic artery, where devascularization from an intra-arterial approach with a microcatheter may not be possible or there may be significant risk of reflux of particles into the intracranial circulation or the retina. Excellent results obtained by this technique have extended its application to smaller and less complex tumors.30 Direct and easy access to the vascular tumor bed that is not hampered by arterial tortuosity, the small size of the feeders, atherosclerotic disease, or induced vasospasm is the main advantage of this technique (Fig 4).
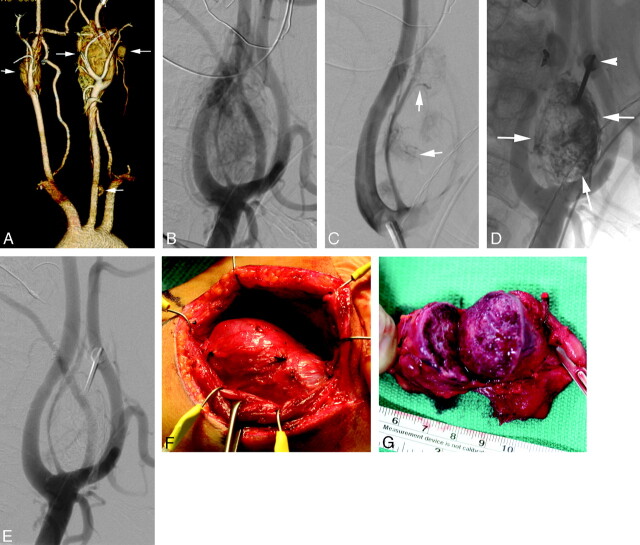
Fig 4.
A 33-year-old man with a family history of multiple paragangliomas and a palpable left neck mass. Preoperative embolization was planned before resection of the left carotid body tumor. A, Volume-rendered reconstruction of a CTA of the neck shows bilateral carotid body tumors as well as 2 other glomus tumors along the left carotid sheath (arrows). B, Lateral view of the left common carotid angiogram reveals a large carotid body tumor supplied by multiple external carotid branches and splaying the ICA and ECA. C, After transarterial embolization of the occipital and ascending pharyngeal contributions to the tumor, residual tumor blush is noted. The vessels that remain are too small to be catheterized with a microcatheter (arrows). D, Fluoroscopic puncture of the tumor performed with an 18-gauge needle (arrowhead) and tumor embolized percutaneously by using a 30% mixture of n-BCA glue and ethiodol oil (arrows). E, Postembolization angiogram reveals near-complete devascularization of the carotid body tumor. F, Intraoperative photograph shows the exposed carotid body tumor. Intraoperative bleeding was <130 mL for the entire procedure. G, The cut surface of the excised specimen shows grossly a thrombosed tumor.
Complete devascularization of the tumor can be obtained with decreased risk to the patient by direct tumoral injection of n-butyl cyanoacrylate (n-BCA, Trufill; Cordis, Miami Lakes, Fla) or Onyx (ev3).29,30 Onyx is a recent US Food and Drug Administration–approved nonadhesive embolic agent, which is supplied in ready-to-use vials with a mixture of EVOH, dimethyl sulfoxide solvent (DMSO), and tantalum. Currently 6% (Onyx 18) and 8% (Onyx 34) EVOH concentrations (dissolved in DMSO) are available in the United States for presurgical cerebral arteriovenous malformation (AVM) embolization. Onyx is mechanically occlusive but nonadherent to the vessel wall. Its nonadherent properties allow a slow single injection of the embolic agent over a long period of time. During direct injection, if unfavorable filling of the normal vascular structures occurs, the injection can be stopped and resumed after 30 seconds to 2 minutes. Solidification will occur in the embolized portion of the tumor. The injection can then be restarted with Onyx taking the path of least resistance and filling another portion of the tumor. Due to its properties, Onyx may potentially allow a more controlled injection with better penetration into the tumor bed compared with n-BCA. Another benefit is that it advances in a single column, thus reducing the risk of involuntary venous migration.
Serious complications occur in <2% of patients.29,31 These are usually related to particle reflux, poor technique, or nonvisualization of dangerous anastomoses resulting in blindness or irreversible neurologic deficits.
Embolization of Cervicofacial High-Flow Malformations
AVMs of the head and neck are rare in contrast to low-flow vascular anomalies. These can involve the soft-tissue structures of the face and neck and/or the maxillofacial skeleton. The clinical presentation can be cosmetic defects, pain, bleeding, ischemic ulceration, and congestive heart failure.
The management of high-flow vascular anomalies is challenging because of their unpredictable biologic behavior and a relatively high incidence of recurrence if not managed correctly.32 A multidisciplinary team approach is required for the assessment and optimal treatment of high-flow VMs. Although smaller lesions can be managed by endovascular embolization alone, larger and complex lesions may require additional surgical resection.
Angiographically, the craniofacial high-flow VMs may consist of a nidus (AVMs) or direct communications between arteries and veins (arteriovenus fistulas),33 though the precise distinction between these 2 types may not always be possible. A variety of embolic agents have been used for the treatment of high-flow lesions, including ethanol, n-BCA, Onyx (Contour PVA particles; Boston Scientific, Natick, Mass), and coils.33,34 Transarterial endovascular embolization of high-flow lesions with particles is generally not effective because of frequently incomplete closure as well as recurrence of the AVM. Transarterial n-BCA is more effective and permanent,35 but staged procedures may be necessary and distal microcatheter access may be difficult when there is excessive vascular tortuosity.
Direct-puncture (percutaneous) embolization is used for direct access into the vascular nidus or the adjacent vein.33,35,36 The nidus and/or the draining vein can be embolized with n-BCA or Onyx by using this approach (Fig 5). Flow-modification techniques are frequently required to limit the venous egress of the embolic material and to facilitate complete filling of the nidus. This can be accomplished by manual compression of the vein if there is a single large outflow channel. However, when an AVM has multiple venous drainage channels, a compression device for circumferential flow reduction can be more effective than manual digital compression.37 Alternatively, a temporary balloon may be inflated in the feeding artery33 to decrease the rate of shunt surgery and limit the backward reflux of embolic material in the feeding vessel. Direct-puncture embolization of an AVM is technically easier compared with transarterial embolization, reduces the procedure time, and has the advantage of reducing the risk of ischemic complications (skin necrosis and brain or retinal ischemia).37 If Onyx is used for the percutaneous injection, care should be taken to avoid subcutaneous extravasation because it can result in black skin discoloration.
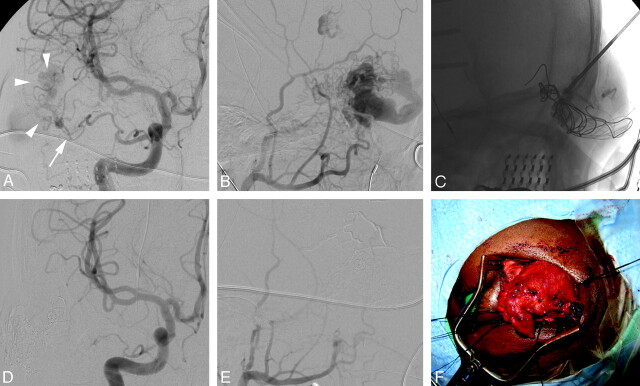
Fig 5.
A 12-year-old girl with a large periorbital AVM. A, Anteroposterior view of the right ICA shows the arterial supply to the AVM (arrowheads) via small branches of the ophthalmic artery (arrow). B, External carotid angiogram in the lateral projections demonstrates a large AVM fed by multiple branches of the internal maxillary artery and the anterior branch of the superficial temporal artery. A large venous varix is seen early in the arterial phase draining into the supraorbital and facial veins. C, Percutaneous access to the venous varix is shown with placement of coils and injection of a 1:1 mixture of n-BCA glue and ethiodol oil. Small remaining feeders were then embolized transarterially with Onyx (not shown). D, Postembolizarion right ICA angiogram shows complete cessation of supply from the ophthalmic artery. E, Right external carotid angiogram also demonstrates near-complete thrombosis of the AVM and the venous varix. F, Intraoperative photograph showing the thrombosed AVM mass. Total blood loss at surgery was <200 mL. Intraoperative photograph courtesy of A. Kahana, MD, Department of Ophthalmology, University of Michigan, Ann Arbor, Mich.
Because of the rarity of high-flow VMs, there is a lack of consensus on the optimal method of treatment. However, embolization forms an integral part of treatment. The fistulous lesions are cured more often by embolization compared with the AVMs.37
Management of Bleeding from the Head and Neck
Transarterial Embolization for Epistaxis
Epistaxis is a common clinical problem, with 60% of the normal population experiencing an episode of varying severity in their lifetime.38 Only 6% of patients require medical or surgical attention, and intractable epistaxis is relatively uncommon.39 Causes of epistaxis include hereditary hemorrhagic telangiectasia (HHT), craniofacial trauma, infections, tumors, bleeding disorders, vascular abnormalities, and anticoagulation therapy.39,40 In some patients, no definite cause can be identified, and it is labeled as idiopathic.
Uncontrolled epistaxis can be a life-threatening condition. The treatment is variable and often depends on institutional preference and available expertise. If the bleeding source is identified, it can be treated with electrocautery. Nasal packing can be useful if the bleeding source is occult. Nasal packing, with or without balloon tamponade, is however associated with risks of necrosis of the nasal cartilage, infections, aspiration, hypoxia, cardiac arrhythmia, and sepsis. Although transantral ligation of the internal maxillary arteries can be performed, a failure rate of up to 24% has been described with this technique.39
Endovascular embolization for epistaxis is an attractive therapeutic option for the patients with intractable epistaxis. This technique is safe and effective and is associated with very few complications.39,40 At our institution, we prefer to use general anesthesia for the embolization procedures and use conscious sedation only if the patient is a high risk for general anesthesia. Selective angiography of bilateral ICAs and ECAs is first performed with 4F or 5F catheters. ICA angiography is useful for evaluating any dangerous collateral vessels between the ECA and ICA as well as to delineate the predominant supply to the ophthalmic artery. Moreover, ICA injection also helps to delineate the ethmoidal artery supply to the nasal cavity. It is generally unsafe to embolize the anterior ethmoidal arteries with particulate agents because of the associated risk of blindness.
The embolization is generally performed under systemic anticoagulation and with superselective catheterization of target vessels. We generally prefer microcatheters with larger bores (0.019–0.021 inches) and use 100–300 or 300–500 μm particles (Embospheres) for embolization. The microcatheter is positioned just proximal to the branches supplying the nasal mucosa, and care is taken to avoid nontargeted vessel embolization. If smaller particles (100–300 μm) are chosen, they are typically used in small quantities because aggressive embolization with small particles is associated with a risk of necrosis of the embolized territory. Gelfoam pledgets may be placed in the vessel lumen after completing embolization with particulate agents. Permanent occlusion of vessels is avoided in patients with epistaxis unless the bleeding is related to trauma, pseudoaneurysm, and nasal VMs.
Embolization is highly effective for treatment of intractable epistaxis with reported success rates ranging from 71% to 100%.39,41 The most common cause of the failure of this technique is bleeding from the anterior ethmoidal artery.39,42 Recurrent bleeding is not uncommon in patients with HHT; however, embolization often decreases the severity of hemorrhage and improves the quality of life in these patients.40
Complications resulting from the treatment are usually minor, including groin hematoma, facial numbness, mucosal necrosis, and sinusitis. A cerebrovascular accident or blindness can occasionally occur as a complication of the treatment, though the incidence of this complication is very low.41,43
Bleeding from Carcinoma of the Head and Neck
Traditional management of hemorrhage in a patient with head and neck carcinoma consists of open surgical exploration and ligation of the involved vessel. The hemorrhage can be difficult to control because of associated problems such as recurrent tumor, postsurgical anatomic changes, fistulas, infection, and radiation necrosis. Endovascular embolization may be a better alternative due to decreased morbidity, a shorter hospital stay, and greater efficacy.44,45
Patients who present with severe bleeding should be managed as if they were hemodynamically unstable (blowout precautions). A large-bore intravenous catheter line should be established, and hemodynamic parameters should be closely monitored. The blood should be typed and cross-matched, and complete blood count and coagulation studies should be obtained. A head and neck examination, including careful fiberoptic examination of the nasal cavity, nasopharynx, oropharynx, larynx, and hypopharynx, frequently can help in determining the site and/or the side of hemorrhage.
CT angiography (CTA) of the neck is a very useful technique and often the first imaging study performed at our institution. CTA can help identify the location of the hemorrhage and provides valuable information regarding the integrity of the carotid artery (Fig 6). Initial CTA examination may demonstrate a pseudoaneurysm or an area of active hemorrhage.46 CTA can also determine the location and the extent of the tumor and its relation to the major neck vessels.
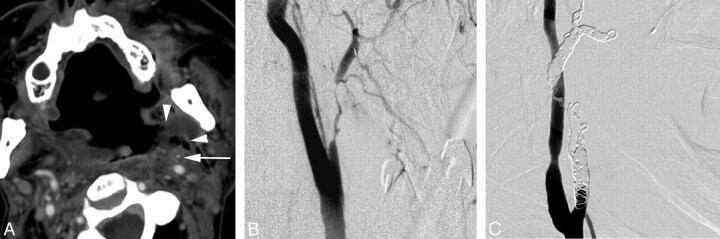
Fig 6.
An elderly man with a recurrent head and neck cancer presenting with pulsatile bleeding through the oral cavity. A, CT angiogram of the neck shows an ulcerated left oropharyngeal mass (arrowheads) that encases the left ECA (arrow). B, Common carotid angiogram reveals a long-segment tumor encasement of the left ECA. C, The ECA is embolized with fibered and detachable platinum coils. The patient did not have additional episodes of bleeding after the embolization.
Treatment consists of obtaining a detailed cerebral angiogram, including an aortic arch and selective injections of the common carotid artery, ICA, and ECA, as well as the bilateral thyrocervical trunks. An active site of hemorrhage is uncommonly seen on the angiogram. However, focal arterial narrowing and irregularity from tumor erosion or encasement of the artery can point toward the possible site of arterial hemorrhage. If a definite area of hemorrhage is not identified, on the basis of the location of the tumor on CT, a microcatheter is advanced into the artery supplying the tumor. Particles form the mainstay of tumor embolization. Embolization is initially performed with the particles in the 150- to 250-μm range. This can be followed with larger particles and/or Gelfoam pledgets until the main arterial branches to the tumor are occluded. The goal of embolization is tumor devascularization through intratumoral deposition of embolic material at the arteriolar/capillary level.
To our knowledge, data from large series comparing different techniques and results for endovascular treatment are lacking. In our institutional experience (unpublished data; D. Gandhi, University of Michigan, June 2008) and in a few reported small series, this technique has good efficacy with minimal risk of complications.47,48
Carotid Blowout Syndrome
Carotid blowout syndrome (CBS) refers to rupture of the carotid artery and its branches.49,50 It is a life-threatening delayed complication of extensive or recurrent squamous cell carcinoma of the head and neck. The cause may be related to tumor involvement of the vessel wall, postoperative radiation, or prior surgical exposure. The reported morbidity and mortality rates associated with this complication are 40% and 60% respectively.51,52 Survival is usually <2 years.
Surgical ligation of the carotid artery with or without a bypass is the traditional form of treatment. This is technically demanding because exploration and repair of a previous surgical and irradiated field can be difficult. Endovascular therapy is an excellent alternative to surgery and the method of choice. The use of a covered stent has been reported in this condition, and a high rate of technical success is reported in achieving immediate hemostasis.53,54 However, several recently published series have shown unfavorable long-term outcomes due to rebleeding, delayed thrombosis, and abscess formation from contamination of the stent with the skin or oral flora.54–56 The poor long-term patency of the stent-grafts and the delayed complications like infection and rebleeding suggest that stent-graft placement may be beneficial for temporary rather than permanent management for patients with CBS (Fig 7). Appropriate candidates for the use of stent-grafts may include those at high risk of neurologic morbidity from carotid occlusion, patients with acute massive bleed that prevents temporary balloon test occlusion, or those with a short life expectancy.54
Fig 7.
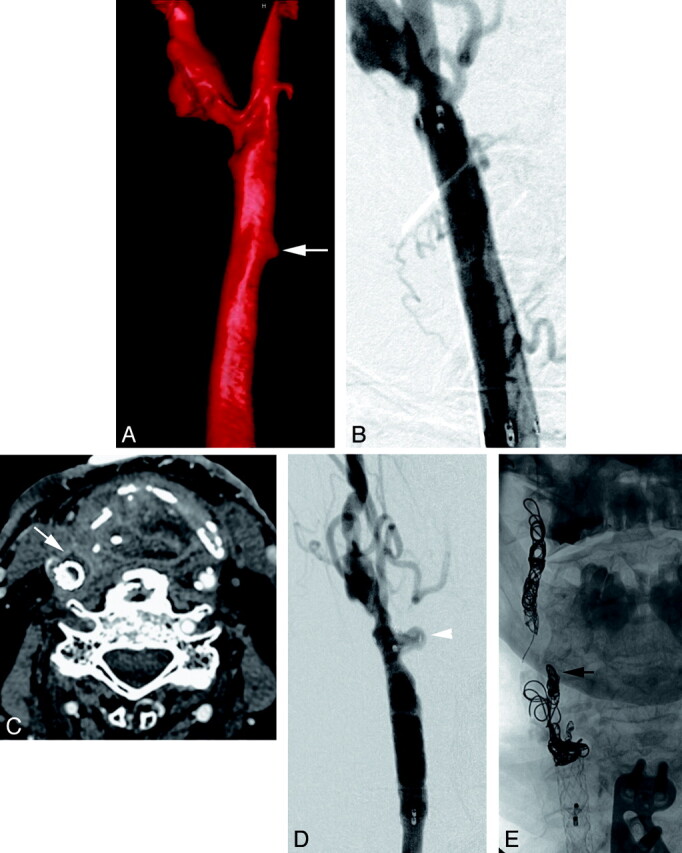
A 65-year-old patient with a previously treated supraglottic laryngeal carcinoma presenting with profuse hemoptysis. A, A volume-rendered 3D digital subtraction angiogram reveals a small pseudoaneurysm (arrow) arising from the medial aspect of the right common carotid artery. Also note the atherosclerotic changes at the carotid bifurcation. B, This image was obtained following deployment of an 8 × 40 mm stent-graft in the common carotid artery and excluding the pseduoaneurysm. C, The patient presented 11 weeks later with a recurrent hemorrhage from his tracheostomy site. Neck CT shows a rim-enhancing fluid collection (arrow) adjacent to the stent-graft suggestive of infection. D, Common carotid angiogram at this time shows a recurrent carotid blowout (arrowhead) at the distal end of the stent-graft. E, Following a successful temporary balloon occlusion test, the ICA and ECA (black arrow) were occluded with coils, and the common carotid artery was sacrificed proximal to the pseudoaneurysm. The patient has not had another bleed in the following 5 months.
Permanent occlusion of the carotid artery is usually performed with a detachable balloon or coils. Approximately 15%–20% of patients treated with permanent vessel occlusion may have an immediate or delayed cerebral ischemia.52,53 A temporary balloon occlusion test can be performed before sacrificing the carotid artery and may help in identifying patients at risk for immediate or delayed ischemic complications from occlusion of the carotid artery.
Intra-Arterial Chemotherapy for Head and Neck Carcinoma
The prognosis for patients with advanced head and neck cancer treated conventionally with surgery, radiation, or both is extremely poor, with a long-term survival of 15%–40%.57,58 Patients who are fortunate to survive their cancer often face a lifetime of significant morbidity, predominantly because of cosmetic and functional disabilities from extensive resection of the aerodigestive tract. Radiation therapy alone has the advantage of organ preservation; however, its use in advanced disease only shows benefit with surgical resection.59 Intravenous chemotherapy for advanced disease has shown little benefit as a single-technique treatment, and the use of concurrent chemoradiation is limited by severe toxicity with higher doses.60 A large prospective study of 332 patients with stage III or IV laryngeal cancer showed no difference in survival when induction intravenous chemotherapy followed by radiation therapy was compared with surgical resection and radiation therapy (P = .98).61
The radiation and platinum (RADPLAT) protocol was developed at the University of California, San Diego and the University of Tennessee, Memphis, to address these limitations.62 The basis of this approach is to deliver an extremely high dose of the anticancer drug directly into the artery supplying the tumor, while circulating the antagonist of the drug in the venous system. This approach increases the amount of cisplatin delivered to the tumor, thus increasing its cytotoxic effects. In addition, the cisplatin also acts as a radio-sensitization agent, increasing the effectiveness of the concurrent radiation. The drug's antagonist thiosulfate neutralizes the effects of cisplatin, thus minimizing the systemic toxicity.
Transfemoral carotid arteriography is carried out to assess the vascular anatomy before superselective catheterization of the tumor's dominant vascular supply. A microcatheter is then placed coaxially into the ECA at the level of the orifice of the dominant artery supplying the tumor. This procedure allows local intra-arterial infusion of cisplatin (150 mg/m2 for 3–5 minutes) in conjunction with an intravenous infusion of sodium thiosulfate (9 g/m2 for 3–5 minutes, followed by 12 g/m2 for 6 hours). Bilateral catheterizations and infusions are performed in patients with disease extending across the midline. The goal of intra-arterial infusion is to target the portion of the tumor considered bulky or infiltrative and likely to fail treatment with radiation therapy alone.63
Four cycles of intra-arterial chemotherapy are administered on days 1, 8, 15, and 22. Radiation therapy is started on day 1 before chemotherapy and continued once daily 5 days a week. Opposed lateral fields are used to encompass the primary and overt nodal disease at 2.0 Gy per fraction once daily 5 days a week to a planned total dose of 70.0 Gy. Uninvolved lower neck is treated with a single anteroposterior supraclavicular field at 50.0 Gy at 2.0 Gy per fraction once daily. Several studies have evaluated the response rate and survival of patients using this technique.62,64–66 Although this form of therapy has been studied for many years, the results have been variable, with heterogeneous use of this technique depending on institution or practitioner preference. However, several trials, particularly those using cisplatin-based regimens, indicate that a high response rate can be achieved. Additionally, there has been 1 phase II trial evaluating the feasibility and effectiveness of this form of treatment in a multi-institutional setting.67 The results have been encouraging, with reported complete response rates ranging from 55% to 90%. Locoregional control rates of 57%–96% have been quoted at 2–5 years. Survival has ranged from 32%–63% between 2 and 5 years.
References
- 1.Gupta S, Henningsen JA, Wallace MJ, et al. Percutaneous biopsy of head and neck lesions with CT guidance: various approaches and relevant anatomic and technical considerations. Radiographics 2007;272:371–90 [DOI] [PubMed] [Google Scholar]
- 2.Sherman PM, Yousem DM, Loevner LA. CT-guided aspirations in the head and neck: assessment of the first 216 cases. AJNR Am J Neuroradiol 2004;25:1603–07 [PMC free article] [PubMed] [Google Scholar]
- 3.Akins EW, Hawkins IF Jr, Mladinich C, et al. The blunt needle: a new percutaneous access device. AJR Am J Roentgenol 1989;152:181–82 [DOI] [PubMed] [Google Scholar]
- 4.Mukherji SK, Turetsky D, Tart RP, et al. A technique for core biopsies of head and neck masses. AJNR Am J Neuroradiol 1994;15:518–20 [PMC free article] [PubMed] [Google Scholar]
- 5.DelGaudio JM, Dillard DG, Albritton FD, et al. Computed tomography–guided needle biopsy of head and neck lesions. Arch Otolaryngol Head Neck Surg 2000;126:366–70 [DOI] [PubMed] [Google Scholar]
- 6.Brook A, Gold MM, Miller TS. CT-guided radiofrequency ablation in the palliative treatment of recurrent advanced head and neck malignancies. J Vasc Interv Radiol 2008;19:725–35. Epub 2008 Mar 17 [DOI] [PubMed] [Google Scholar]
- 7.Rhim H, Dodd GD 3rd. Radiofrequency thermal ablation of liver tumors. J Clin Ultrasound 1999;27:221–29 [DOI] [PubMed] [Google Scholar]
- 8.Shafir M, Shapiro R, Sung M, et al. Cryoablation of unresectable malignant liver tumors. Am J Surg 1996;171:27–31 [DOI] [PubMed] [Google Scholar]
- 9.Schirmang TC, Davis LM, Nigri PT, et al. Solitary fibrous tumor of the buccal space: treatment with percutaneous cryoablation. AJNR Am J Neuroradiol 2007;28:1728–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bui Q, Dupuy DE. Percutaneous CT-guided radiofrequency ablation of an adenoid cystic carcinoma of the head and neck. AJR Am J Roentgenol 2002;179:1333–35 [DOI] [PubMed] [Google Scholar]
- 11.Monchik JM, Donatini G, Iannuccilli J, et al. Radiofrequency ablation and percutaneous ethanol injection treatment for recurrent local and distant well-differentiated thyroid carcinoma. Ann Surg 2006;244:296–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412–20 [DOI] [PubMed] [Google Scholar]
- 13.Enjolras O, Mulliken JB. Clinical and laboratory investigations: the current management of vascular birthmarks. Pediatr Dermatol 1993;10:311–33 [DOI] [PubMed] [Google Scholar]
- 14.Yakes WF. Extremity venous malformations: diagnosis and management. Semin Intervention Radiol 1994;11:332–39 [Google Scholar]
- 15.Claudon M, Upton J, Burrows PE. Diffuse venous malformations of the upper limb: morphologic characterization by MRI and venography. Pediatr Radiol 2001;31:507–14 [DOI] [PubMed] [Google Scholar]
- 16.Burrows PE, Laor T, Paltiel H, et al. Diagnostic imaging in the evaluation of vascular birthmarks. Dermatol Clin 1998;16:455–88 [DOI] [PubMed] [Google Scholar]
- 17.Berenguer B, Burrows PE, Zurakowski D, et al. Sclerotherapy of craniofacial venous malformations: complications and results. Plast Reconstr Surg 1999;104:1–11, discussion 12–15 [PubMed] [Google Scholar]
- 18.Choi YH, Han MH, O-Ki K, et al. Craniofacial cavernous venous malformations: percutaneous sclerotherapy with use of ethanolamine oleate. J Vasc Interv Radiol 2002;13:475–82 [DOI] [PubMed] [Google Scholar]
- 19.Cordes BM, Seidel FG, Sulek M, et al. Doxycycline sclerotherapy as the primary treatment for head and neck lymphatic malformations. Otolaryngol Head Neck Surg 2007;137:962–64 [DOI] [PubMed] [Google Scholar]
- 20.Lee BB, Do YS, Byun HS, et al. Advanced management of venous malformation with ethanol sclerotherapy: mid-term results. J Vasc Surg 2003;37:533–38 [DOI] [PubMed] [Google Scholar]
- 21.Cabrera J, Cabrera J Jr, Garcia-Olmedo A, et al. Treatment of venous malformations with sclerosant in microfoam form. Arch Dermatol 2003;139:1409–16 [DOI] [PubMed] [Google Scholar]
- 22.Rho MH, Kim DW, Kwon JS, et al. OK-432 sclerotherapy of plunging ranula in 21 patients: it can be a substitute for surgery. AJNR Am J Neuroradiol 2006;27:1090–95 [PMC free article] [PubMed] [Google Scholar]
- 23.Kim KH, Sung MN, Rho JL, et al. Sclerotherapy for congenital lesions in the head and neck. Otolaryngol Head Neck Surg 2004;131:307–16 [DOI] [PubMed] [Google Scholar]
- 24.Chang HS, Yoon JH, Chung WY, et al. Sclerotherapy with OK-432 for recurrent cystic thyroid nodule. Yonsei Med J 1998;39:367–71 [DOI] [PubMed] [Google Scholar]
- 25.Macpherson P. The value of pre-operative embolization of meningiomas estimated subjectively and objectively. Neuroradiology 1991;33:334–37 [DOI] [PubMed] [Google Scholar]
- 26.Dean BL, Flom RA, Wallace RC, et al. Efficacy of endovascular treatment of meningiomas: evaluation with matched samples. AJNR Am J Neuroradiol 1994;15:1675–80 [PMC free article] [PubMed] [Google Scholar]
- 27.Wakhloo AK, Juengling FD, Delthoven VV. Extended preoperative polyvinyl alcohol microembolization of intracranial meningiomas: assessment of two embolization techniques. AJNR Am J Neuroradiol 1993;14:571–82 [PMC free article] [PubMed] [Google Scholar]
- 28.Kallmes DF, Evans AJ, Kaptain GJ, et al. Hemorrhagic complications in embolization of a meningioma: case report and review of the literature. Neuroradiology 1997;39:877–80 [DOI] [PubMed] [Google Scholar]
- 29.Quadros RS, Gallas S, Delcourt C, et al. Preoperative embolization of a cervicodorsal paraganglioma by direct percutaneous injection of Onyx and endovascular delivery of particles. AJNR Am J Neuroradiol 2006;27:1907–09 [PMC free article] [PubMed] [Google Scholar]
- 30.Abud DG, Mounayer C, Benndorf G, et al. Intratumoral injection of cyanoacrylate glue in head and neck paragangliomas. AJNR Am J Neuroradiol 2004;25:1457–62 [PMC free article] [PubMed] [Google Scholar]
- 31.Gruber A, Bavinzski G, Killer M, et al. Preoperative embolization of hypervascular skull base tumors. Minim Invasive Neurosurg 2000;43:62–71 [DOI] [PubMed] [Google Scholar]
- 32.Erdmann MW, Jackson JE, Davies DM, et al. Multidisciplinary approach to the management of head and neck arteriovenous malformations. Ann R Coll Surg Engl 1995;77:53–59 [PMC free article] [PubMed] [Google Scholar]
- 33.Arat A, Cil BE, Vargel I, et al. Embolization of high-flow craniofacial vascular malformations with Onyx. AJNR Am J Neuroradiol 2007;28:1409–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee BB, Do YS, Yakes W, et al. Management of arteriovenous malformations: a multidisciplinary approach. J Vasc Surg 2004;39:590–600 [DOI] [PubMed] [Google Scholar]
- 35.Rodesch G, Soupre V, Vazquez MP, et al. Arteriovenous malformations of the dental arcades: the place of endovascular therapy—results in 12 cases are presented. J Craniomaxillofac Surg 1998;26:306–13 [DOI] [PubMed] [Google Scholar]
- 36.Resnick SA, Russell EJ, Hanson DH, et al. Embolization of a life-threatening mandibular vascular malformation by direct percutaneous transmandibular puncture. Head Neck 1992;14:372–79 [DOI] [PubMed] [Google Scholar]
- 37.Ryu CW, Whang SM, Suh DC, et al. Percutaneous direct puncture glue embolization of high-flow craniofacial arteriovenous lesions: a new circular ring compression device with a beveled edge. AJNR Am J Neuroradiol 2007;28:528–30 [PMC free article] [PubMed] [Google Scholar]
- 38.Turowski B, Zanella FE. Interventional neuroradiology of the head and neck. Neuroimaging Clin N Am 2003;13:619–45 [DOI] [PubMed] [Google Scholar]
- 39.Andersen PJ, Kjeldsen AD, Nepper-Rasmussen J. Selective embolization in the treatment of intractable epistaxis. Acta Otolaryngol 2005;125:293–97 [DOI] [PubMed] [Google Scholar]
- 40.Layton KF, Kallmes DF, Gray LA, et al. Endovascular treatment of epistaxis in patients with hereditary hemorrhagic telangiectasia. AJNR Am J Neuroradiol 2007;28:885–88 [PMC free article] [PubMed] [Google Scholar]
- 41.Strutz J, Schumacher M. Uncontrollable epistaxis, angiographic localization and embolization. Arch Otolaryngol Head Neck Surg 1990;116:697–99 [DOI] [PubMed] [Google Scholar]
- 42.Tseng EY, Narducci CA, Willing SJ, et al. Angiographic embolization for epistaxis: a review of 114 cases. Laryngoscope 1998;108:615–19 [DOI] [PubMed] [Google Scholar]
- 43.Christensen NP, Smith DS, Barnwell SL, et al. Arterial embolization in the management of posterior epistaxis. Otolaryngol Head Neck Surg 2005;133:748–53 [DOI] [PubMed] [Google Scholar]
- 44.Remonda L, Schroth G, Caversaccio M, et al. Endovascular treatment of acute and subacute hemorrhage in the head and neck. Arch Otolaryngol Head Neck Surg 2000;126:1255–62 [DOI] [PubMed] [Google Scholar]
- 45.Morrissey DD, Anderson PE, Nesbit GM, et al. Endovascular management of hemorrhage in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 1997;123:15–19 [DOI] [PubMed] [Google Scholar]
- 46.Goodman DN, Hoh BL, Rabinov JD, et al. CT angiography before embolization for hemorrhage in head and neck cancer. AJNR Am J Neuroradiol 2003;24:140–42 [PMC free article] [PubMed] [Google Scholar]
- 47.Sittel C, Jungelhulsing M, Gossmann A, et al. Superselective embolization as palliative treatment of recurrent hemorrhage in advanced carcinoma of the head and neck. Ann Otol Rhinol Laryngol 2001;110:1126–28 [DOI] [PubMed] [Google Scholar]
- 48.Wilner HI, Lazo A, Metes JJ, et al. Embolization in cataclysmal hemorrhage caused by squamous cell carcinoma of the head and neck. Radiology 1987;163:759–62 [DOI] [PubMed] [Google Scholar]
- 49.Chaloupka JC, Roth TC, Putman CM, et al. Recurrent carotid blowout syndrome: diagnosis and therapeutic challenges in a newly recognized subgroup of patients. AJNR Am J Neuroradiol 1999;30:1069–77 [PMC free article] [PubMed] [Google Scholar]
- 50.Mcdonald S, Gan J, Mckay AJ, et al. Endovascular treatment of acute carotid blowout syndrome. J Vasc Interv Radiol 2000;11:1184–88 [DOI] [PubMed] [Google Scholar]
- 51.Citardi MJ, Chaloupka JC, Son YH, et al. Management of carotid artery rupture by monitored endovascular therapeutic occlusion (1988–1994). Laryngoscope 1995;105:1086–92 [DOI] [PubMed] [Google Scholar]
- 52.Chaloupka JC, Putnam CM, Citardi MJ, et al. Endovascular therapy for the carotid blowout syndrome in head and neck surgical patients: diagnostic and managerial considerations. AJNR Am J Neuroradiol 1996;17:843–52 [PMC free article] [PubMed] [Google Scholar]
- 53.Lesley WS, Chaloupka JC, Weigele JB, et al. Preliminary experience with endovascular reconstruction for the management of carotid blowout syndrome. AJNR Am J Neuroradiol 2003;24:975–81 [PMC free article] [PubMed] [Google Scholar]
- 54.Chang FC, Lirng JF, Luo CB, et al. Carotid blowout syndrome in patients with head-and-neck cancers: reconstructive management by self-expandable stent-grafts. AJNR Am J Neuroradiol 2007;28:181–88 [PMC free article] [PubMed] [Google Scholar]
- 55.Chang FC, Lirng JF, Tai SK, et al. Brain abscess formation: a delayed complication of carotid blowout syndrome treated by self-expandable stent-graft. AJNR Am J Neuroradiol 2006;27:1543–45 [PMC free article] [PubMed] [Google Scholar]
- 56.Pyun HW, Lee DH, Yoo HM, et al. Placement of covered stents for carotid blowout in patients with head and neck cancer: follow-up results after rescue treatments. AJNR Am J Neuroradiol 2007;28:1594–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marcial VA, Pajak TF. Radiation therapy alone or in combination with surgery in head and neck cancer. Cancer 1985;55:2259–65 [DOI] [PubMed] [Google Scholar]
- 58.Laramore GE, Scott CB, Al-Sarraf M, et al. Adjuvant chemotherapy for resectable squamous cell carcinoma of the head and neck: report on Intergroup Study 0034. Int J Radiat Oncol Biol Phys 1992;23:705–13 [DOI] [PubMed] [Google Scholar]
- 59.Robertson AG, Soutar DS, Paul J, et al. Early closure of a randomized trial: surgery and postoperative radiotherapy versus radiotherapy in the management of intra-oral tumours. Clin Oncol (R Coll Radiol) 1998;10:155–60 [DOI] [PubMed] [Google Scholar]
- 60.Vokes EE, Weichselbaum RR. Concomitant chemotherapy: rationale and clinical experience in patients with solid tumors. J Clin Oncol 1990;8:911–34 [DOI] [PubMed] [Google Scholar]
- 61.Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer: The Department of Veterans Affairs Laryngeal Cancer Study Group. N Engl J Med 1991;324:1685–90 [DOI] [PubMed] [Google Scholar]
- 62.Robbins KT, Kumar P, Wong FS, et al. Targeted chemoradiation for advanced head and neck cancer: analysis of 213 patients. Head Neck 2000;22:687–93 [DOI] [PubMed] [Google Scholar]
- 63.Kumar P, Robbins KT. Treatment of advanced head and neck cancer with intra-arterial cisplatin and concurrent radiation therapy: the “RADPLAT” protocol. Curr Oncol Rep 2001;3:59–65 [DOI] [PubMed] [Google Scholar]
- 64.Robbins KT, Kumar P, Regine WF, et al. Efficacy of targeted supradose cisplatin and concomitant radiation therapy for advanced head and neck cancer: the Memphis experience. Int J Radiat Oncol Biol Phys 1997;38:263–71 [DOI] [PubMed] [Google Scholar]
- 65.Robbins KT, Wong FS, Kumar P, et al. Efficacy of targeted chemoradiation and planned selective neck dissection to control bulky nodal disease in advanced head and neck cancer. Arch Otolaryngol Head Neck Surg 1999;125:670–75 [DOI] [PubMed] [Google Scholar]
- 66.Balm AJ, Rasch CR, Schornagel JH, et al. High dose superselective intra-arterial cisplatin and concomitant radiation (RADPLAT) for advanced head and neck cancer. Head Neck 2004;26:485–93 [DOI] [PubMed] [Google Scholar]
- 67.Robbins KT, Kumar P, Harris J, et al. Supradose intra-arterial cisplatin and concurrent radiation therapy for the treatment of stage IV head and neck squamous cell carcinoma is feasible and efficacious in a multi-institutional setting: results of Radiation Therapy Oncology Group Trial 9615. J Clin Oncol 2005;23:1447–54 [DOI] [PubMed] [Google Scholar]