Abstract
SUMMARY: A 43-year-old patient with a basilar apex aneurysm had a 4.5-mm × 14-mm Enterprise stent placed from the midbasilar artery to the left P1 segment of the posterior cerebral artery. The patient experienced vertigo 4 months after stent placement and 1 week after stopping clopidogrel. At 5 months postembolization, angiography showed stent migration into the proximal basilar artery. This is the first described case of the spontaneous delayed migration of a self-expanding intracranial microstent.
The use of self-expanding microstents for the treatment of cerebral aneurysms continues to evolve.1-3 This technical evolution has allowed for previously uncoilable aneurysms to be successfully treated. Intracranial microstents may also produce flow redirection and parent vessel remodeling, ultimately improving the durability of aneurysm embolization.4 We report the first case of a spontaneous, delayed, symptomatic migration of a self-expanding intracranial microstent.
Case Report
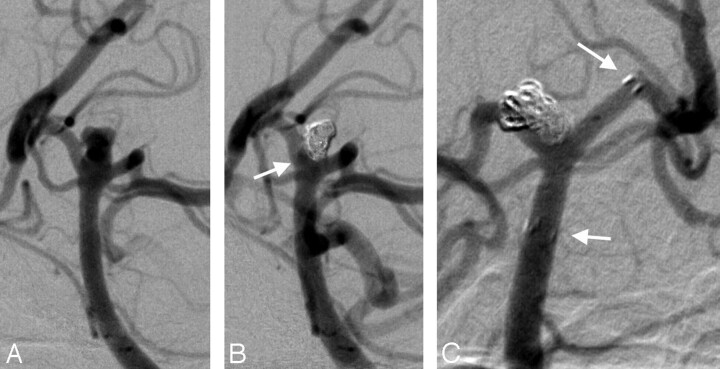
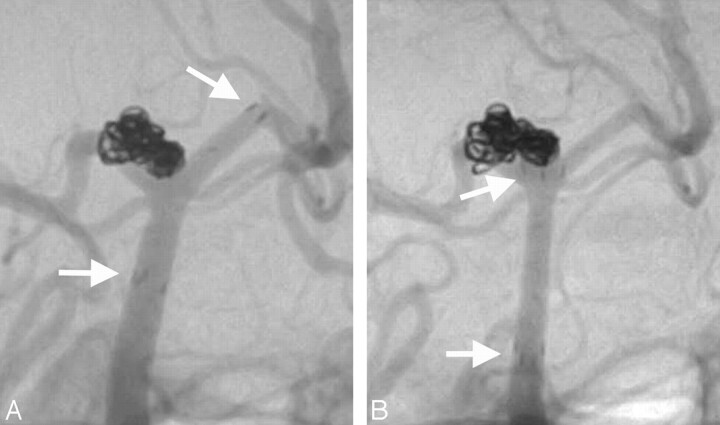
A 43-year-old woman presented with a Hunt and Hess II, Fisher grade III subarachnoid hemorrhage from a ruptured basilar apex aneurysm (Fig 1A). The aneurysm measured 4.0 × 2.5 × 2.0 mm. She was initially treated with balloon-assisted coiling, and 3 coils were placed (Fig 1B). A small residual at the base of the aneurysm was not occluded at the time of the initial treatment (Fig 1B, arrow). The patient made a full neurologic recovery after the subarachnoid hemorrhage. She returned 3 months later for treatment of the small residual aneurysm. A balloon-assisted coiling technique was again used to achieve complete occlusion of the remnant, which was broad necked relative to its small size (Fig 1C). At the conclusion of the coiling, a 4.5-mm × 14-mm Enterprise stent (Cordis Neurovascular, Miami Lakes, Fla) was placed, extending from the midbasilar artery to the P1 segment of the left posterior cerebral artery (PCA) (Fig 2A) to stabilize the new coil mass. Clopidogrel was discontinued 4 months after implantation of the stent. One week later, the patient experienced a brief onset of vertigo that resolved. She had a second episode of vertigo 1 week later and was given clopidogrel, after which she remained asymptomatic. The patient underwent another cerebral angiogram 5 months after coiling, which demonstrated proximal migration of the stent end markers from the P1 segment of the PCA into the distal basilar artery (Fig 2B). The patient remains neurologically intact and continues on dual antiplatelet therapy.
Fig 1.
A, Oblique view, left vertebral artery injection showing a 4.0 × 2.5 × 2.0-mm basilar apex aneurysm. B, The patient underwent balloon-assisted coiling. There is a small (1.5-mm) residual at the base noted (arrow). C, Oblique view, left vertebral artery injection. The patient returned for balloon-assisted coiling of the aneurysm with near-complete occlusion of the aneurysm. An Enterprise stent was placed at the conclusion of the coiling to assist with flow redirection. (Arrows denote distal and proximal stent markers.) The P1 segment of the PCA measured 1.40 mm, the distal basilar artery at the level of the superior cerebellar arteries measured 2.33 mm, the distal basilar trunk measured 1.96 mm, and the proximal basilar trunk measured 2.55 mm.
Fig 2.
A, Oblique view, left vertebral artery injection. The patient was brought back 3 months after initial treatment for additional treatment. She underwent another balloon-assisted coiling procedure with near-complete occlusion of the aneurysm and had an Enterprise stent placed from the left P1 segment of the PCA to the midbasilar artery trunk. (The distal and proximal tines of the stent are shown by the arrows.) B, Oblique view, left vertebral artery injection. Another angiogram performed 5 months after placement of the Enterprise stent shows clear migration of the stent from the left P1 PCA to the distal basilar artery. (The distal and proximal stent tines are shown by the arrows.) The aneurysm remains well occluded.
Discussion
This case report represents the first published case of the delayed migration of a self-expanding intracranial stent used for the embolization of an intracranial aneurysm. Spontaneous migration of the stent occurred some time between the control angiogram performed at the conclusion of the procedure and the 5-month follow-up. The presence of symptoms 4 months after treatment suggests that the migration occurred at or before this time. The correlation of the neurologic symptoms with the discontinuation of clopidogrel can be attributed to the unopposed distal aspect of the migrated stent within the basilar apex, which very likely requires a longer period to become “passivated” (ie, nonthrombogenic) or endothelialized.
Self-expanding stents are delicate devices that are maintained in position within the cerebral vasculature by relatively low-level chronic outward radial forces. These stents are easily inadvertently displaced in the context of aneurysm embolization when attempts are made to manipulate other devices (eg, microcatheters, balloons, additional stent delivery systems) through or beyond them. For this reason, some operators prefer to either perform staged procedures, where embolization is performed at some interval after stent implantation to allow for “endothelialization” to occur, or to place the stent at the conclusion of the coiling procedure to minimize the amount of trans-stent manipulation.
At our institution, more than 200 Neuroform (Boston Scientific, Freemont, Calif) stents have been placed since 2003, and we have never observed a case of delayed spontaneous stent migration. In addition, no cases of spontaneous Neuroform migration have been reported in the literature. The closed-cell Enterprise (Cordis) stent is structurally different from Neuroform, which has an open-cell design. As such, forces exerted on 1 segment of the Enterprise are transmitted directly to the entire device. In our present case, the differential sizes of the PCA and basilar artery caused the distal aspect of the stent to be constrained to a greater degree than the proximal portion. We hypothesize that this differential constraint may have transferred a constant retrograde force to the stent, which ultimately caused it to “watermelon seed” backward into the basilar artery. Placement of the distal aspect of this stent into an artery measuring slightly less than 2 mm may have contributed to the proximal migration of this device. In a vessel of this size, the capacity of the “flared” distal segment of the Enterprise to engage the parent artery and adequately stabilize the stent may have been limited. We urge caution when deploying the Enterprise device in similar anatomic configurations.
References
- 1.Fiorella D, Albuquerque FC, Deshmukh VR, et al. Usefulness of the Neuroform stent for the treatment of cerebral aneurysms: results at initial (3–6-mo) follow-up. Neurosurgery 2005;56:1191–201; discussion 1201–02 [DOI] [PubMed] [Google Scholar]
- 2.Fiorella D, Albuquerque FC, Han P, et al. Preliminary experience using the Neuroform stent for the treatment of cerebral aneurysms. Neurosurgery 2004;54:6–16; discussion 16–17 [DOI] [PubMed] [Google Scholar]
- 3.Benitez RP, Silva MT, Klem J, et al. Endovascular occlusion of wide-necked aneurysms with a new intracranial microstent (Neuroform) and detachable coils. Neurosurgery 2004;54:1359–67; discussion 1368 [DOI] [PubMed] [Google Scholar]
- 4.Canton G, Levy DI, Lasheras JC, et al. Flow changes caused by the sequential placement of stents across the neck of sidewall cerebral aneurysms. J Neurosurg 2005;103:891–902 [DOI] [PubMed] [Google Scholar]